Abstract
Purpose
The purpose of this study was to evaluate three different methods of attachment of continuous loop suspensory cortical preparation of all soft tissue central quad tendon grafts compared to a bone block control for anterior cruciate ligament reconstruction on construct displacement and load to failure.
Methods
Thirty-two cadaveric central quadriceps tendon (CQT) specimens were harvested, using three clinical techniques for graft fixation: cortical button alone (BTB EB), BTB cortical button with rip-stop suture (BTB RS), and continuous loop cortical button (BTB CL). A control group was also included that consisted of a bone block secured within testing clamps (BTB CON). Specimens were preloaded to 150 N. Tendons were then cyclically loaded between 50 N and 250 N for 1,000 cycles at .5 Hz. Displacement was measured at the point of fixation of the CQT after the 150 N preload, 250 N initial load and every 100th cycle. The specimens were loaded to failure after 1,000 cycles.
Results
There was a significant increase in displacement from .32 ± .56 mm for the BTB CON to 1.91 ± 1.13 mm for the BTB RS (P = .014) and 3.85 ± 2.32 mm for the BTB CL condition (P = .023). There was no significant increase in displacement for BTB EB (P = .182). Failure occurred for all of the BTB CL and 62.5% of the BTB EB specimens within the first 50 cycles. Twenty-five percent of the BTB CON specimens and 12.5% BTB RS failed at ∼400 and 500 cycles, respectively. Similar failure loads were observed for the BTB CON and the BTB RS (446.4 ± 151.46 N vs 505.74 ± 131.41 N; P = .99) Failure testing was not feasible for the BTB CL and BTB EB preparation methods.
Conclusion
In response to cyclic loading, the three all-soft tissue suspensory conditions experienced significantly greater displacement compared to the bone block controls. None of the soft-tissue conditions appeared superior when compared to each other.
Clinical Relevance
It remains unknown which method of soft-tissue suspensory provides optimal fixation. As these autografts become more common, it is essential to evaluate which fixation methods provide superior outcomes
Keywords: ACL, bone block, quadriceps tendon, soft tissue fixation
Introduction
Central quadriceps tendon (CQT) autograft has been gaining popularity for anterior cruciate ligament (ACL) reconstruction. The reported rate of CQT as a graft choice for ACL reconstruction increased from 2.5% in 2010 to 11% in 2014.1,2 In a recent publication from the ACL Study Group, surveying orthopaedic surgeons on their graft preferences, 13% responded that quad tendon was their secondary graft choice.3 In addition, 33% and 10% predicted that bone-tendon-bone autograft and quad-tendon autograft will be the most commonly used grafts 10 years from now, respectively.3 This trend may be related to several factors such as hamstring tendon (HT) grafts having a higher rate of infection and a greater risk of rerupture.4,5 CQT grafts are also larger and stronger than bone-patella tendon-bone (BPTB) grafts,6 and the CQT autograft has a low donor site morbidity profile compared to BPTB, while offering favorable anatomical and biomechanical properties.7
Biomechanical studies have shown that the CQT has a higher maximum tensile load (2,173–2,352 N),6,8,9 compared to the BPTB graft (1,580 N) and native ACL (1,725–2,106 N).6,10,11 Histologically, the CQT has 20% more collagen fibrils per cross-sectional area than the patellar tendon.7 Clinically, the CQT autograft has shown favorable results as a choice for ACL reconstruction while avoiding some of the postoperative complications associated with BPTB and HT autografts.12,13 A 2015 systematic review of 14 studies showed no difference between CQT graft reconstructions when compared to other graft choices with regard to arthrometric, Lachman, or pivot shift testing.14 Five of the 14 studies indicated less donor site morbidity, including anterior knee pain and patellar fracture, with CQT compared to BPTB. A 2014 prospective study comparing CQT to BPTB tendon grafts showed no significant difference in laxity as measured by KT-1000 at 2 years postoperation.13 Additionally, the CQT group had a significantly lower rate of pivot-shift compared to the BPTB group (14% vs 38%, respectively).13 This study also demonstrated lower rates of anterior knee pain for CQT patients (7%) compared to BTB patients (34%). When compared to HT grafts, the CQT grafts preserves the function of the hamstrings, which serve as an ACL agonist, suggesting that CQT harvest results in a protective hamstring to quadriceps muscle strength ratio, which may result in lower stress rates on the ACL.12
Multiple techniques have been described for the harvest and fixation of CQT for ACL reconstruction.15, 16, 17, 18, 19, 20, 21 Techniques include full and partial thickness tendon harvest, both with and without the harvest of a bone block from the superior pole of the patella. The use of a bone block has the advantage of bony healing within the tunnel.22 All soft tissue grafts have the advantage of a smaller incision and decreased anterior knee pain, and they remove the risk of potential patella fracture.7 However, soft tissue-based CQT grafts rely on the strength of the graft preparation technique, often using high-strength sutures with or without a suspensory fixation device, which is often the weak point in the construct that may contribute to failure18,23 These factors have created controversy as to what is the optimal fixation method for CQT autografts.
The purpose of this study was to evaluate three different clinical methods of attachment of continuous loop suspensory cortical preparation of all soft tissue CQT grafts for ACL reconstruction on construct displacement and load to failure. We hypothesised that the addition of a rip-stop suture to a BTB Endobutton (Smith and Nephew, Inc., Andover, MA) passed through the soft tissue graft would provide similar cyclic and load to failure characteristics to a graft remaining attached to a patellar bone block.
Methods
Specimen Preparation
Thirty-two fresh-frozen extensor mechanisms, including quadriceps tendon and patella, were harvested from human cadaveric knee specimens (mean [SD] age = 68.6 [6.0] years; 16 males) that were procured from an independent and anonymous body donation program (ScienceCare, Inc., Phoenix AZ). The study protocol was reviewed and approved in adherence with the tissue use and ethical guidelines of deidentified cadaveric tissue. The tendons were wrapped in saline-soaked gauze, plastic wrap, and sealed in a plastic bag for storage in a freezer (−18°C) prior to testing. The quadriceps tendon specimens were thawed for approximately 3 hours prior to preparation and testing. Any remaining quadriceps muscle and adipose tissue were carefully dissected from the final graft. The specimens were moistened with a saline solution throughout preparation and testing to minimize soft tissue desecration.
Graft Preparation
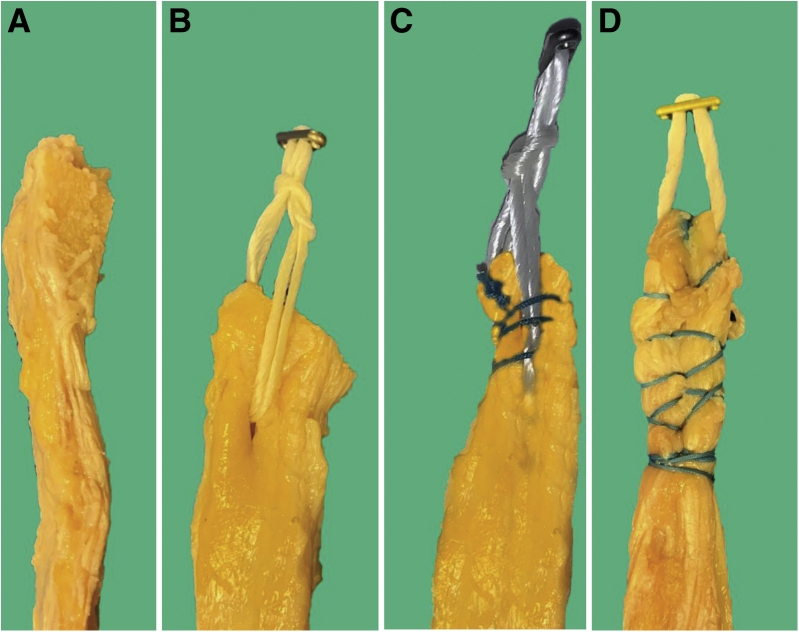
The specimens were randomly allocated into 1 of 4 groups: (1) CQT with bone block that served as a control group (BTB CON; n = 8); (2) all soft tissue CQT with BTB Endobutton alone (BTB EB; n = 8); (3) all soft tissue CQT with BTB Endobutton with rip-stop suture (BTB RS; n = 8); and (4) all soft tissue CQT with continuous loop Endobutton (BTB CL; n = 8) (Fig 1). For the BTB CON group, a partial-thickness tendon graft of rectus femoris was harvested measuring 12 mm × 6 mm with a 12 mm × 10mm × 6 mm patellar bone. For the BTB EB group a 40-mm BTB Endobutton (Smith & Nephew, Andover, MA) was passed through a 12 mm × 6 mm partial-thickness tendon harvested without bone or periosteal flap. The mean (SD) length of the grafts was 60.1 (20.9) mm. A small puncture was made through the central portion of the tendon 2 cm from the distal end of the tendon. For the BTB RS group, the partial-thickness tendon graft was prepared in an identical fashion as group two, with the addition of a no. 2 Ethibond (Ethicon Inc., Somerville, NJ) suture. The suture was passed through the tendon 3 times in a whip stitch fashion from distal to proximal and then proximal to distal that tubularized the distal portion of the graft, acting as a rip-stop stitch for the Endobutton. For the BTB CL group, a 12 mm × 6 mm partial thickness tendon graft was harvested along with a 2-cm periosteal flap from the superior aspect of the patella. A no. 2 high-strength looped suture (Ultrabraid, Smith & Nephew) was passed three times through the tendon starting 2 cm proximal to the distal aspect of the tendon. The periosteal flap was then passed through a 20-mm CL Endobutton and folded over onto the tendon. The same looped suture was then passed 3 times around the loop of the Endobutton, securing the periosteal flap to the tendon. A final 3 throws of the loop suture were passed to return to the starting point of the suture. Each CQT tendon was harvested and prepared by a single fellowship-trained orthopaedic surgeon, and all of the soft tissue graft preparation techniques are representative of the clinical preparation.24
Fig 1.
Demonstration of the different tendon preparations bone block (A), BTB with Endobutton alone (B), BTB Endobutton with rip-stop suture (C), and continuous loop Endobutton (D).
Experimental Set-Up
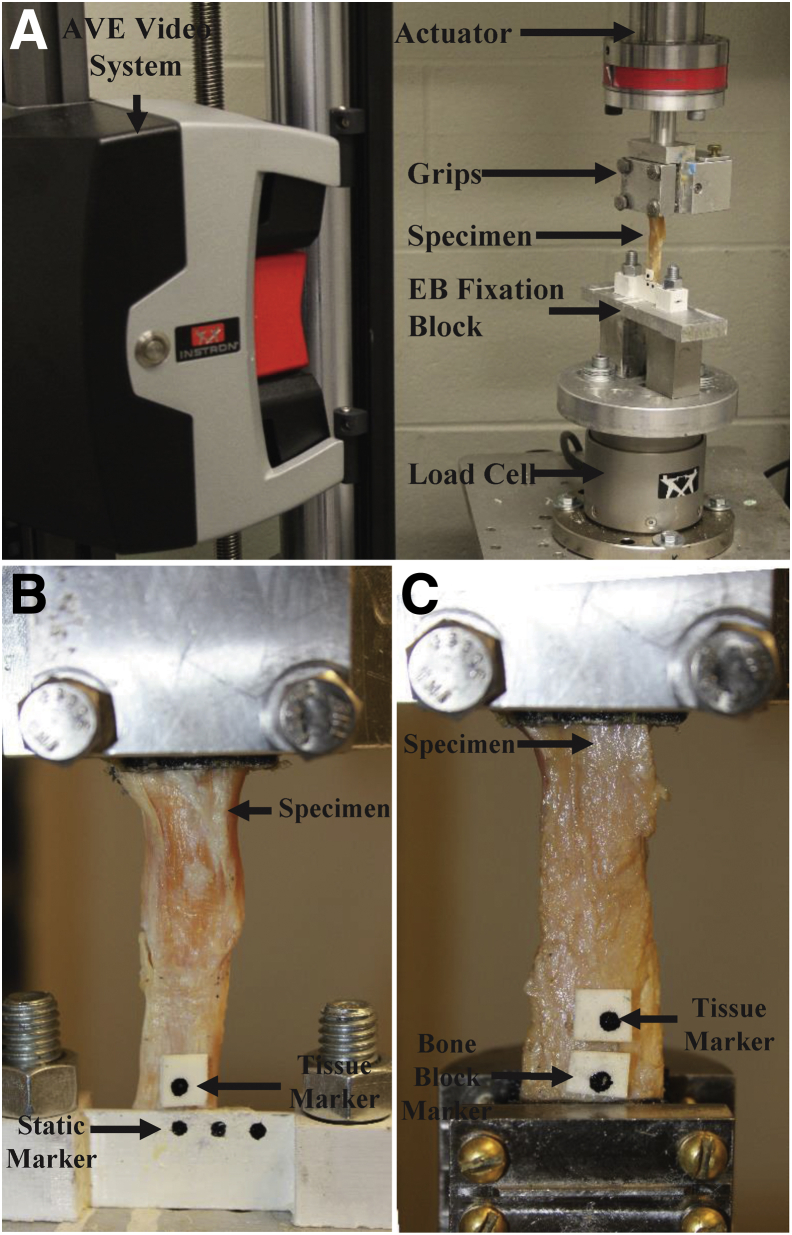
The musculotendinous end of the CQT was secured within a set of custom tissue grips that were connected to a 10 kN load cell (Dynacell 2527-207; Instron, Norwood MA), subsequently attached to the actuator of an Instron materials testing system (Eletropuls E10000; Instron). For the all-soft tissue grafts using suspensory preparation, the cortical button was passed through a hole in a custom steel block (95 mm × 45 mm × 15 mm). For the BTB CON specimens, custom grips were used to rigidly secure the bone block during testing (Fig 2A).
Fig 2.
Biomechanical testing set up. (A) For the all-soft tissue grafts using suspensory fixation, the cortical button was passed through a hole in a custom steel block (95 mm × 45 mm × 15 mm). For the bone-block specimens, custom grips were used to rigidly secure the bone block during testing. (B) An advanced video system was used to measure the displacement between the end of the tendon and static markers. (C) For the Bone Block Group, the markers were placed on the bone block while a second was attached to the soft tissue, directly adjacent to the bone block.
Markers were affixed to the end of the tendon grafts and a custom-designed marker block was used as a static marker and was rigidly secured to the steel block. For the BTB CON specimens, one marker was attached to the bone block, while a second was attached to the soft tissue, adjacent to the bone block (Fig 2B). A line was placed on the bone block at the level of the grips, with an indelible marker, to visually monitor if any slippage occurred within the grips during testing. Overall, the specimens were not observed to move relative to the grips throughout the cyclic testing protocol. An advanced video extensometer system (AVE 2; Instron; focal length = 35 mm; 0.5-μm resolution) was used to monitor the motion of the tendon throughout loading (see below) and to measure the displacement between the tendon and the static markers (Fig 2C). The AVE was calibrated using a standardized calibration plate as per the manufacturer’s recommendations, and the initial gauge length was measured, while a 10-N load was applied. To ensure that the physical characteristics of the specimens were homogenous across conditions, the width and thickness of the tendons were measured.
Loading Protocol
The specimens were preloaded to 150 N for 10 s. The tendons were then cyclically loaded between 50 N and 250 N for 1,000 cycles at .5 Hz. The test was only stopped if catastrophic failure occurred to any component of the system; otherwise, the specimens were loaded for the duration of the 1,000 cycles.25,26 Video was recorded (10 frames/s) throughout the entirety of testing. After the 1000th cycle, the specimens were tested to failure by applying a tensile load at 50 mm/min until failure (e.g., suture breakage, suture pull-out, tendon-grip slippage) was detected.26 For the specimens that failed prior to the cyclic testing, the force they failed at was used as their failure force (less than 250 N), while the specimens that failed during the cyclic testing protocol were considered to have failed at 250 N.
Data Analysis
The displacement of the CQT was measured at the 150-N preload, the initial 250-N load (0 cycles), the 20th cycle, the 50th cycle, and every 100th cycle; these data points were used in further analysis. The displacements at the 150-N preload and 250-N initial load states were calculated as the change from the resting state when only a 10-N load was being applied. The cyclic loading displacements were zeroed/adjusted, according to the displacement observed at the initial 250-N load, and these values were used for the statistical analysis. For the failure trials, the load at failure was determined from the force-time curve, and the location of failure was recorded and documented with pictures. To determine the effect of the four configurations on displacement at the 150-N preload and the initial 250-N load, a one-way ANOVA was used. To statistically compare the displacement that occurred across the entire cyclic loading protocol a two-way mixed repeated-measures ANOVA was performed; preparation type was the between-specimen variable, while cycles were the within-specimen variable. Finally, a one-way ANOVA was completed to statistically analyze the failure force data, as well as to compare the physical characteristics of the CQT specimens. Post hoc effect sizes and power were calculated and assessed according to Levine and Hullett,27 and all statistical tests were performed in IBM SPSS version 23 (IBM, Armonk, NY). A Bonferroni adjustment was used for all post hoc tests, and alpha was set at .05.
Results
Preload Displacements
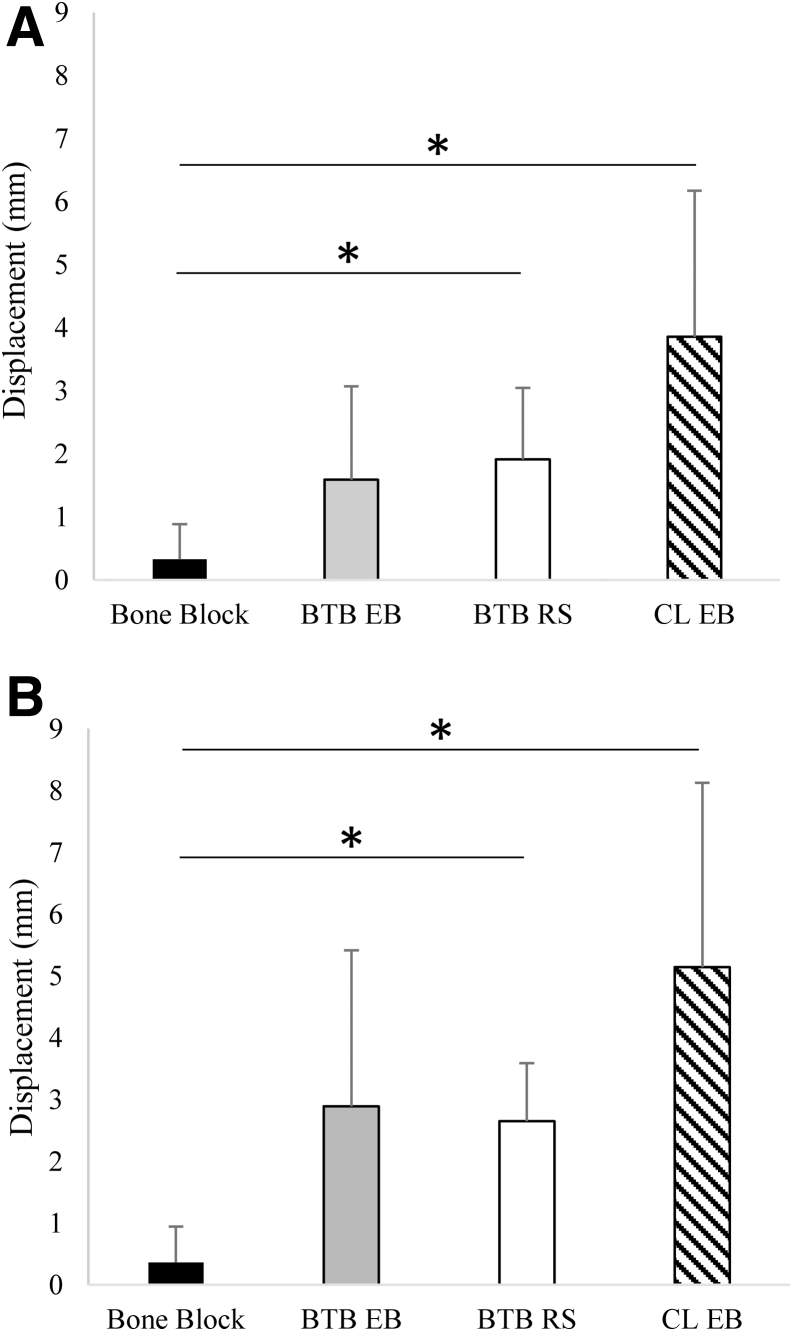
Following the 150 N preload, there was a statistically significant increase in the means ± SD displacement 0.32 ± .56 mm for the BTB CON condition to 1.91 ± 1.13 mm for the BTB RS (P = .014) and 3.85 ± 2.32 mm for the BTB CL condition (P = .023) (Fig 3A). Although not statistically significant (P =.182), there was a large difference (effect size = 1.13) in displacement between the BTB CON and the BTB EB (1.59 ± 1.48 mm) (Fig 3A). The means ± SD displacements were further increased in response to the 250 N load, and the differences between the BTB CON (0.36 ± .58 mm) and BTB RS (2.65 ± .94 mm) and the BTB CL (5.14 ± 2.99 mm) were statistically significant (P = .011 and P < .001, respectively) (Fig 3B). There was a large (effect size = 1.38), but nonsignificant (P = .186), difference between the bone block and the BTB EB (2.89 ± 2.52 mm) conditions (Fig 3B).
Fig 3.
Comparions of the mean (SD) disaplcements of the distal end of the tendon across fixation types in reponse to the 150-N preload (A) and the the initial 250-N load (B) ∗P < .05.
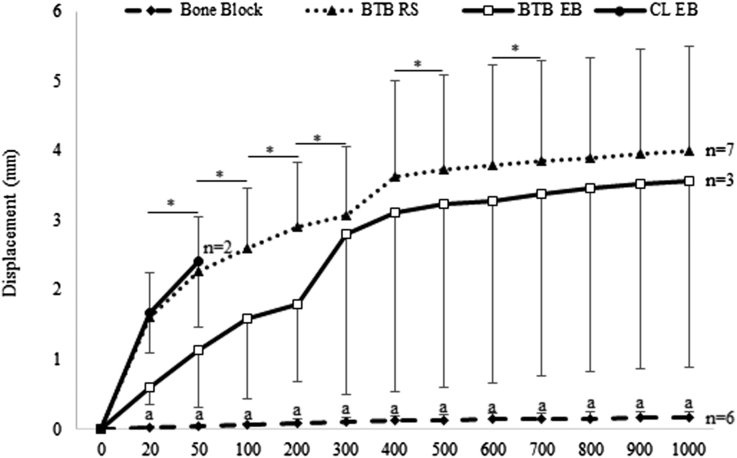
Cyclic Loading
All of the BTB CL and five of the BTB EB specimens failed within the first 50 cycles of the cyclic testing protocol. In addition, two of the bone block specimens and one of the BTB RS specimens failed at ∼400 and 500 cycles, respectively. Therefore, the statistical analysis of the cyclic testing data did not include the BTB CL or BTB EB specimens, and only six of the BTB CON and seven of the BTB RS tendons. There was a significant interaction between cycles and preparation type (P < .001; effect size = .435; power = 1.00) such that the displacement was significantly smaller in the bone block compared to the BTB RS conditions at all cycles (P < .001 at all cycles) (Fig 4). In addition, within the BTB CON condition, there were no significant differences in displacement between any subsequent number of cycles (P = 1.00 at all cycles). However, within the BTB RS condition, there were significant increases in the displacements between subsequent cycles at 200 versus 300 cycles (P = .001-.020) and again between 400 versus 500 (P = .015) and 600 versus 700 cycles (P = .010) (Fig 4).
Fig 4.
Comparison of the mean (SD) distal tendon displacements between the bone block (n = 6) and the BTB RS (n = 7) fixation types and across cycles. (∗P < .05 between cycles within the BTB RS group. An asterisk (∗) denotes a significant difference between the bone block and BTB RS group at P < .05). It should be noted that the statistical analysis was only performed on the bone block and the BTB RS specimens.
Load to Failure
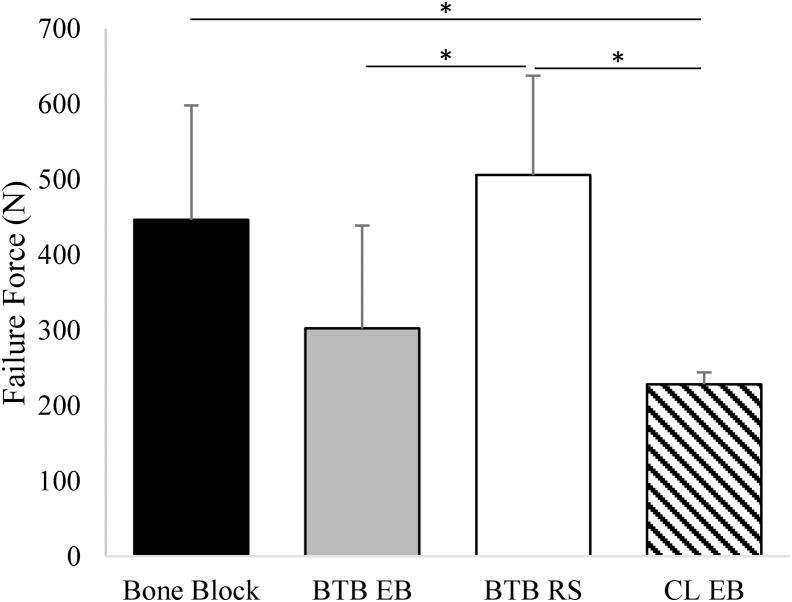
The BTB CON and the BTB RS grafts failed at mean ± SD load of 446.4 ± 151.46 N and 505.74 ± 131.41 N, respectively, and were not statistically different (P = .99) (Fig 5). However, the BTB EB failed at a significantly lower load (302.32 ± 136.20 N) compared to the BTB RS (P = .013) and the BTB CL failure load (227.87 ± 15.67 N) was significantly lower than both the bone block (P = .009) and the BTB RS (P = .001) conditions (Fig 5).
Fig 5.
Comparison of the mean (SD) load to failure between the different fixations. ∗P < .05.
Mechanism of Failure
All of the BTB CL specimens failed as a result of the suture pulling through the flap and suture construct, while all of the BTB EB specimens failed by having the loop pull through the tissue. The addition of the rip-stop to the BTB RS prevented the loop from pulling all of the way through the tissue initially, but failure occurred in 100% of the specimens as a result of the loop applying pressure to the rip-stop constricting the tissue and eventually pulling through. Finally, 57.1% of the BTB CON specimens failed at the bone block grip interface, 28.6% experienced a failure within the tendon tissue, and 14.3% experienced an avulsion off the bone block.
Discussion
The main finding of this study is that each of the all soft tissue suspensory preparation methods experienced significantly greater displacement with preload and cyclic loading compared to the BTB CON. Early failure was noted for the majority of specimens in the BTB CL and BTB EB groups during cyclic testing, while six of the BTB CON and all of the BTB RS groups completed the cyclic testing without complete tissue failure and were available for the failure testing. While the load-to-failure of the BTB RS was similar to that of the BTB CON, the all soft tissue preparation had already experienced significant displacement (>3 mm) that was representative of clinical failure.25 Importantly, all of the BTB CL group failed early in the cyclic testing (failure at the tissue flap), while only 37.5% of the BTB EB group completed the cyclic loading, with all failures involving the loop pulling through the tissue. Although the addition of the rip-stop improved the construct strength, all of the failures of the BTB RS involved the suture constricting the tissue and pulling the loop through the center of the tendon.
Methods for securing all soft tissue quadriceps grafts have been previously studied.23,28 Michel et al. investigated suture type (doubled no. 2 vs single no. 5 composite suture) and stitch type (Krackow, whip and baseball), on cyclic and load-to-failure.23 The Krackow stitch with a doubled no. 2 suture was shown to have the most favorable characteristics; however, the magnitude of displacement (10.59 ± −2.63 mm) in response to cyclic loading was significantly greater than what we observed with the BTB RS and bone block CQT in our study. In a similar study, Hahn et al. compared Krackow and baseball stitches in porcine flexor tendons.28 They also found a significantly greater displacement (15 ± −4 mm) with the Krackow stich, which again is greater than the displacements that we observed in our study. The difference between these studies and ours may be due to our testing protocol. We adjusted our cyclic loading data with respect to the displacements that occurred following the preloading stages of testing. This represents the clinical scenario in which the prepared graft is preloaded on the back table to remove suture creep prior to inserting the graft into the knee. We also hypothesized that the use of the continuous loop device would reduce the amount of displacement in the construct, by removing the issue of suture creep within the soft tissue graft, as is observed with the more traditional Krakow and whip suture configurations. Furthermore, the weak link in soft tissue suture application is often the method of fixation of the suture to bone. Sutures tied over a cortical button or screw post have the potential for knot slippage and loss of graft fixation.29 Continuous loop cortical suspensory fixation devices, such as the Endobutton CL (Smith and Nephew, Inc.), have been shown to provide the strongest fixation properties for soft tissue grafts.25,26
Our soft tissue displacements are consistent with those reported in studies by Sakaguchi et al.30 and Eguchi et al.25 in both magnitude and pattern. In these studies, there was an abrupt increase in displacement between 0 and 200 cycles followed by a slow leveling out to 1,000 cycles.25,30 With respect to load to failure, Eguchi et al. compared soft tissue fixation of fixed loop versus adjustable loop devices.25 The fixed loop (Endobutton CL) failed at approximately 1,100 N compared to 870 N with the adjustable loop (Tightrope), with the majority of failures attributed to tendon rupture (Endobutton) and broken loops (Tightrope). Two other studies determined that the displacement or slippage of hamstring grafts was approximately .6 mm to 3 mm depending on the type of fixation that was used.31,32 Both of these studies used screws, washers, and anchors as their mode of fixation, which are mechanically different than the suspensory fixation devices that were tested in our study.
A previous study comparing CQT and BTB grafts observed load to failure to be 2,189 N and 1,580 N, respectively.6 These failure loads are larger than those reported in our study, with the differences potentially being attributed to the different experimental setups. For example, in the current study a partial thickness CQT graft used compared to the full-thickness graft used in the previous study. In addition, Shani et al. cemented their bone blocks while our BTB CON were secured with mechanical clamps.6 Although the pressure exerted by the clamps used in this investigation may be indicative of the pressure exerted by an interference screw, fixation of the bone blocks should not be interpreted clinically and was included to serve only as a control group. While using a fixation screw would better replicate the clinical scenario, we opted to use the mechanical grips to reduce the variability that would have been introduced by incorporating interreference screws. The loads to failure reported in our study fall within a range of those for four-strand hamstring tendon grafts reported to be from 445 N to 2,421 N depending on the type of fixation used,31, 32, 33 Finally, our results also agree favorably with a study that noted a failure load of 606.3 N when an interference screw was used for tibial side fixation.34
When compared to the BTB CON specimens, the BTB RS had the same load to failure but displayed significantly greater tendon displacement at all cycles. It should be reiterated that two of the BTB CON specimens and one of the BTB RS specimens failed at ∼400 and 500 cycles, respectively. However, it has been suggested that displacements greater than 3 mm represent a clinical failure of the fixation, as this inhibits graft healing.25 Even if bone-tendon healing still takes place, the progressive displacement may lead to decreased postoperative stability and failure of the reconstruction. Applying this failure criteria to the current study, all of the BTB RS would have failed between 200 and 300 cycles after accounting for the displacements incurred from the preload.
While caution must be used when interpreting the BTB CON results in comparison to the clinical environment using an interference screw, the results do suggest that fixation may be improved using a bone block. Although the BTB CON specimens exhibited significantly less displacement in response to the cyclic loading, this must be balanced with the risks associated with bone block harvesting, such as postoperative anterior knee pain or patella fracture.35, 36, 37 Fu et al. examined a series of 57 patients that underwent CQT harvest with bone block and found an incidence of 3.5% intraoperative patella fracture and 8.8% at 2 years follow-up; some of these fractures were only seen on computed tomography scan and, thus, may not be clinically relevant.36 After reviewing the fracture cases and imaging, the authors suggested that the risk of fracture was multifactorial and included eccentric harvest site (more lateral), harvesting >50% of anteroposterior thickness, harvesting >50% of mediolateral width, failure of bone graft incorporation, and stress risers at the corner of harvest site. Patellae that have less than 27% of their thickness harvested for a bone block are also less likely to fracture than those that have 42% of their thickness harvested.37 With appropriate harvesting technique and patient selection, the risk of patella fracture can be minimized, thus making CQT with bone plug potentially a safer and more stable graft choice.
Limitations
Limitations in this study include the small sample size for each testing group and the relatively older age of the specimens. Despite the small sample, effect sizes were large, and the post hoc power analysis indicated that it was adequately powered. Additionally, early failure during cyclic testing further reduced sample size and may limit the applicability of load-to-failure testing. With respect to the testing methodology, the line of pull in the current study does not necessarily reflect the physiological stresses placed on the grafts in a human knee. Previous studies have shown higher loads to failure in physiological stresses compared to a straight line of pull.10,11 Changing the orientation may have an effect on cyclic loading and rate of displacement. Our study also did not incorporate tibia-sided fixation. Although this could have altered graft behavior, this was outside of the scope of our study, as we were examining the difference in femur-sided suspensory fixation devices. Additionally, tibia-sided fixation would have been standard in all four groups and, thus, would not have added any additional between-group changes. Finally, it is difficult to interpret what the displacement in this biomechanical model would translate to in vivo and if this would create symptomatic laxity. The threshold for failure and revision surgery in the context of ACL reconstruction is generally regarded as persistent symptomatic laxity.
Conclusion
The bone block controls experienced significantly less displacement when compared to the 3 all-soft tissue fixation suspensory devices. However, the BTH RS specimens failed at similar forces compared to the BTB CON group.
Footnotes
This research was funded by Smith and Nephew Inc. (A17-ASDUS-GR-598).
The authors report the following potential conflicts of interest or sources of funding: T.A.B. reports grants from Smith and Nephew, during the conduct of the study. A.G. reports grants from Smith and Nephew, during the conduct of the study; grants and personal fees from Smith and Nephew, grants from Ossur, personal fees from Precision OS and personal fees from Xiros Ltd, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Van Eck C.F., Schreiber V.M., Mejia H.A., et al. Anatomic anterior cruciate ligament reconstruction: A systematic review of surgical techniques and reporting of surgical data. Arthroscopy. 2010;26:S2–S12(9 Suppl. 1). doi: 10.1016/j.arthro.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 2.Middleton K.K., Hamilton T., Irrgang J.J., Karlsson J., Harner C.D., Fu F.H. Anatomic anterior cruciate ligament (ACL) reconstruction: A global perspective. Part 1. Knee Surg Sport Traumatol Arthrosc. 2014;22:1467–1482. doi: 10.1007/s00167-014-2846-3. [DOI] [PubMed] [Google Scholar]
- 3.Sherman S.L., Calcei J., Ray T., et al. ACL Study Group presents the global trends in ACL reconstruction: Biennial survey of the ACL Study Group. J ISAKOS. 2021;6:322–328. doi: 10.1136/jisakos-2020-000567. [DOI] [PubMed] [Google Scholar]
- 4.Mariscalco M.W., Flanigan D.C., Mitchell J., et al. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: A Multicenter Orthopaedic Outcomes Network (MOON) Cohort Study. Arthroscopy. 2013;29:1948–1953. doi: 10.1016/j.arthro.2013.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Makhni E.C., Steinhaus M.E., Mehran N., Schulz B.S., Ahmad C.S. Functional outcome and graft retention in patients with septic arthritis after anterior cruciate ligament reconstruction: A systematic review. Arthroscopy. 2015;31:1392–1401. doi: 10.1016/j.arthro.2014.12.026. [DOI] [PubMed] [Google Scholar]
- 6.Shani R.H., Umpierez E., Nasert M., Hiza E.A., Xerogeanes J. Biomechanical comparison of quadriceps and patellar tendon grafts in anterior cruciate ligament reconstruction. Arthroscopy. 2015;32:1–5. doi: 10.1016/j.arthro.2015.06.051. [DOI] [PubMed] [Google Scholar]
- 7.Xerogeanes J.W. Quadriceps tendon graft for anterior cruciate ligament reconstruction: The graft of the future. Arthroscopy. 2019;35:696–697. doi: 10.1016/j.arthro.2019.01.011. [DOI] [PubMed] [Google Scholar]
- 8.West R.V., Harner C.D. Graft selection in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2005;13:197–207. doi: 10.1097/JSA.0000000000000265. [DOI] [PubMed] [Google Scholar]
- 9.Stäubli H.U., Schatzmann L., Brunner P., Rincón L., Nolte L.P. Quadriceps tendon and patellar ligament: Cryosectional anatomy and structural properties in young adults. Knee Surg Sport Traumatol Arthrosc. 1996;4:100–110. doi: 10.1007/bf01477262. [DOI] [PubMed] [Google Scholar]
- 10.Woo S., Hollis J.M., Adams D.J., Lyon R.M., Takai S. Tensile properties of the human femur- anterior cruciate ligament-tibia complex The effects of specimen age and orientation. Am J Sports Med. 1991;19:217–225. doi: 10.1177/036354659101900303. [DOI] [PubMed] [Google Scholar]
- 11.Noyes F.R., Butler D.L., Grood E.S., Zernicke R.F., Hefzy M.S. Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Jt Surg. 1984;66:344–352. [PubMed] [Google Scholar]
- 12.Fischer F., Fink C., Herbst E., et al. Higher hamstring-to-quadriceps isokinetic strength ratio during the first post-operative months in patients with quadriceps tendon compared to hamstring tendon graft following ACL reconstruction. Knee Surg, Sport Traumatol Arthrosc. 2018;26:418–425. doi: 10.1007/s00167-017-4522-x. [DOI] [PubMed] [Google Scholar]
- 13.Lund B., Nielsen T., Faunø P., Christiansen S.E., Lind M. Is quadriceps tendon a better graft choice than patellar tendon? A prospective randomized study. Arthroscopy. 2014;30:593–598. doi: 10.1016/j.arthro.2014.01.012. [DOI] [PubMed] [Google Scholar]
- 14.Slone H.S., Romine S.E., Premkumar A., Xerogeanes J.W. Quadriceps tendon autograft for anterior cruciate ligament reconstruction: A comprehensive review of current literature and systematic review of clinical results. Arthroscopy. 2015;31:541–554. doi: 10.1016/j.arthro.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 15.Lippe J., Armstrong A., Fulkerson J.P. Anatomic guidelines for harvesting a quadriceps free tendon autograft for anterior cruciate ligament reconstruction. Arthroscopy. 2012;28:980–984. doi: 10.1016/j.arthro.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 16.Fink C., Herbort M., Abermann E., Hoser C. Minimally invasive harvest of a quadriceps tendon graft with or without a bone block. Arthrosc Tech. 2014;3:e509–e513. doi: 10.1016/j.eats.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Slone H.S., Ashford W.B., Xerogeanes J.W. Minimally invasive quadriceps tendon harvest and graft preparation for all-inside anterior cruciate ligament reconstruction. Arthrosc Tech. 2016;5:e1049–e1056. doi: 10.1016/j.eats.2016.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sheean A.J., Musahl V., Slone H.S., et al. Quadriceps tendon autograft for arthroscopic knee ligament reconstruction: Use it now, use it often. Br J Sports Med. 2018;52:698–701. doi: 10.1136/bjsports-2017-098769. [DOI] [PubMed] [Google Scholar]
- 19.Fulkerson J.P., McKeon B.P., Donahue B.J., Tarinelli D.J. The central quadriceps tendon as a versatile graft alternative in anterior cruciate ligament reconstruction: Techniques and observations. Tech Orthop. 1998;13:367–374. [Google Scholar]
- 20.Akoto R., Hoeher J. Anterior cruciate ligament (ACL) reconstruction with quadriceps tendon autograft and press-fit fixation using an anteromedial portal technique. BMC Musculoskelet Disord. 2012;13 doi: 10.1186/1471-2474-13-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.DeAngelis J.P., Fulkerson J.P. Quadriceps tendon—a reliable alternative for reconstruction of the anterior cruciate ligament.itle. Clin Sports Med. 2007;26:587–596. doi: 10.1016/j.csm.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 22.Tomita F., Yasuda K., Mikami S., Sakai T., Yamazaki S., Tohyama H. Comparisons of intraosseous graft healing between the doubled flexor tendon graft and the bone-patellar tendon-bone graft in anterior cruciate ligament reconstruction. Arthroscopy. 2001;17:461–476. doi: 10.1053/jars.2001.24059. [DOI] [PubMed] [Google Scholar]
- 23.Michel P.A., Domnick C., Raschke M.J., et al. Soft tissue fixation strategies of human quadriceps tendon grafts: A biomechanical study. Arthroscopy. 2019;35:3069–3076. doi: 10.1016/j.arthro.2019.05.025. [DOI] [PubMed] [Google Scholar]
- 24.Hughes J.D., Vaswani R., Gibbs C.M., Tisherman R.T., Musahl V. Anterior cruciate ligament reconstruction with a partial-thickness quadriceps tendon graft secured with a continuous-loop fixation device. Arthrosc Tech. 2020;9:e603–e609. doi: 10.1016/j.eats.2020.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eguchi A., Ochi M., Adachi N., Deie M., Nakamae A., Usman M.A. Mechanical properties of suspensory fixation devices for anterior cruciate ligament reconstruction: Comparison of the fixed-length loop device versus the adjustable-length loop device. Knee. 2014;21:743–748. doi: 10.1016/j.knee.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 26.Petre B.M., Smith S.D., Jansson K.S., et al. Femoral cortical suspension devices for soft tissue anterior cruciate ligament reconstruction: A comparative biomechanical study. Am J Sports Med. 2013;41:416–422. doi: 10.1177/0363546512469875. [DOI] [PubMed] [Google Scholar]
- 27.Levine T.R., Hullett C.R. Eta-squared, partial eta-squared, and misreporting of effect size in communication research. Hum Commun Res. 2002;28:612–625. doi: 10.1111/j.1468-2958.2002.tb00828.x. [DOI] [Google Scholar]
- 28.Hahn J.M., Inceoʇlu S., Wongworawat M.D. Biomechanical comparison of Krackow locking stitch versus nonlocking loop stitch with varying number of throws. Am J Sports Med. 2014;42:3003–3008. doi: 10.1177/0363546514550989. [DOI] [PubMed] [Google Scholar]
- 29.Cole B.J., Sayegh E.T., Yanke A.B., Chalmers P.N., Frank R.M. Fixation of soft tissue to bone: Techniques and fundamentals. J Am Acad Orthop Surg. 2016;24:83–95. doi: 10.5435/JAAOS-D-14-00081. [DOI] [PubMed] [Google Scholar]
- 30.Sakaguchi K., Tachibana Y., Oda H. Biomechanical properties of porcine flexor tendon fixation with varying throws and stitch methods. Am J Sports Med. 2012;40:1641–1645. doi: 10.1177/0363546512450406. [DOI] [PubMed] [Google Scholar]
- 31.Coleridge S.D., Amis A.A. A comparison of five tibial-fixation systems in hamstring-graft anterior cruciate ligament reconstruction. Knee Surg Sport Traumatol Arthrosc. 2004;12:391–397. doi: 10.1007/s00167-003-0488-y. [DOI] [PubMed] [Google Scholar]
- 32.Giurea M., Zorilla P., Amis A.A., Aichroth P. Comparative pull-out and cyclic-loading strength tests of anchorage of hamstring tendon grafts in anterior cruciate ligament reconstruction. Am J Sports Med. 1999;27:621–625. doi: 10.1177/03635465990270051301. [DOI] [PubMed] [Google Scholar]
- 33.Wilson T.W., Zafuta M.P., Zobitz M. A biomechanical analysis of matched bone-patellar tendon-bone and double-looped semitendinosus and gracilis tendon grafts. Am J Sports Med. 1999;27:202–207. doi: 10.1177/03635465990270021501. [DOI] [PubMed] [Google Scholar]
- 34.Karkosch R.F., Ettinger M., Bachmaier S., Wijdicks C.A., Smith T. Adjustable-length loop cortical button versus interference screw fixation in quadriceps tendon anterior cruciate ligament reconstruction—A biomechanical in vitro study. Clin Biomech. 2018;60:60–65. doi: 10.1016/j.clinbiomech.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 35.Lee S., Sang C.S., Jo C.H., Hyuk S.H., Joon H.A., Myung C.L. Anterior cruciate ligament reconstruction with use of autologous quadriceps tendon graft. J Bone Jt Surg A. 2007;89(Suppl. 3):116–126. doi: 10.2106/JBJS.G.00632. [DOI] [PubMed] [Google Scholar]
- 36.Fu F.H., Rabuck S.J., West R.V., Tashman S., Irrgang J.J. Patellar fractures after the harvest of a quadriceps tendon autograft with a bone block: A case series. Orthop J Sport Med. 2019;7:1–6. doi: 10.1177/2325967119829051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ferrer G.A., Miller R.M., Murawski C.D., et al. Quantitative analysis of the patella following the harvest of a quadriceps tendon autograft with a bone block. Knee Surg Sport Traumatol Arthrosc. 2016;24:2899–2905. doi: 10.1007/s00167-015-3550-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.