Abstract
Purpose
To determine the percent maximal outcome improvement willingness thresholds (MOWTs) for the Nonarthritic Hip Score (NAHS) and the visual analog scale (VAS) for pain that were associated with a patient’s willingness to undergo surgery, in retrospect, given the known outcome of their primary hip arthroscopy with concomitant endoscopy for gluteus medius (GM) tear repair.
Methods
An anchor question was provided to patients who underwent primary hip arthroscopy for femoroacetabular impingement syndrome with concomitant endoscopic GM tear repair between April 2008 to April 2020. Patients were included if they answered the anchor question and had baseline and postoperative minimum 1-year follow-up scores for the NAHS and VAS. Patients were excluded if they had a previous ipsilateral hip surgery, Tönnis grade >1, hip dysplasia, previous hip conditions, or a preoperative score that was already at the maximum value for the NAHS and VAS scores. Receiver operating characteristic (ROC) analysis was used to determine the MOWT. Significance was indicated by a P value <.05.
Results
A total of 107 patients (107 hips) were included, with 101 (94.4%) females and 6 (5.6%) males. The average age and body mass index was 56.20 ± 9.88 years and 28.80 ± 4.92 kg/m2, respectively. The average follow-up time was 54.89 ± 29.52 months. The ROC analysis determined that the MOWT for the mHHS and VAS were 54.7%, and 62.6%, respectively. The probability of a patient being willing to undergo surgery again if they met the MOWT was 85.8% and 85.6% for the NAHS and VAS, respectively.
Conclusion
The MOWTs that were predictive of willingness to undergo surgery again following primary hip arthroscopy with concomitant endoscopy for GM tear repair were 54.7% and 62.6% for the NAHS, and VAS, respectively.
Clinical Relevance
Outcome assessment has been a point of increasing emphasis in hip preservation surgery. Having a tool to measure whether patients would go through the process of surgery again knowing their current outcome status is important to understanding outcomes after surgery.
Introduction
Femoroacetabular syndrome (FAIS) in combination with a symptomatic gluteus medius (GM) tear is relatively uncommon. In a cross-sectional study that included 2,452 patients with FAIS diagnosis, Meghpara et al. determined that 3.5% had symptomatic partial-thickness tears, and 0.4% had symptomatic full-thickness tears.1 Hence, this is an injury in which age also is reported to play a role with patients over 40 years having 2.11 relative risk of GM pathology compared with patients younger than 40 years.1 Nevertheless, combined FAIS arthroscopic management with endoscopic GM repair has been demonstrated to be a safe and valid procedure with significant improvements in patient-reported outcome scores (PROs) in the short-and-mid-term follow-up.2,3
Clinically, outcome assessment has been a point of increasing emphasis in hip preservation surgery.4, 5, 6 Moving forward from the statistical significance of improvement in PROs,7 psychometric tools, such as the patient-acceptable symptomatic state (PASS),8 the minimal clinically important difference (MCID),9 and the substantial clinical benefit (SCB) have been used to report clinical improvement. More recently, the concept of the maximal outcome improvement (MOI) and a MOI threshold have also been reported as a useful additional option for this task following FAIS arthroscopic surgery.10
The MOI is defined as the patient’s change in functional score divided by their total possible improvement.11 One advantage of the MOI is that it limits the ceiling effects associated with other psychometric tools by accounting for the total possible improvement.11 By using ROC analysis, an MOI threshold can also be created with MOI values and an anchor question, which ascertains satisfaction with surgery. In a similar fashion as PASS, previous studies have used this as a supplementary tool that attempts to estimate patient satisfaction using PROs, while also controlling for ceiling effects.10,12,13 Maldonado et al. determined that 52.5% and 55.5% of MOI were the thresholds for maximal predictability of satisfaction for the Nonarthritic Hip Score (NAHS) and the visual analog scale for pain (VAS), respectively.12 However, if the MOI calculation is combined with an anchor question that assesses patient willingness to undergo surgery again, the maximal outcome improvement willingness threshold (MOWT) is obtained. This metric is different from PASS since the anchor question for PASS focuses on satisfaction following surgery rather than willingness to undergo surgery again.
To determine the percent MOWTs for the NAHS and the VAS for pain that were associated with a patient’s willingness to undergo surgery, in retrospect, given the known outcome of their primary hip arthroscopy with concomitant endoscopy for GM tear repair. It was hypothesized that MOWT thresholds, which were predictive of willingness to undergo surgery again following primary hip arthroscopy for FAIS with concomitant endoscopy for GM tear repair, would be determined.
Methods
Patient Selection Criteria
This study was performed in accordance with the ethical standards in the 1964 Declaration of Helsinki. This study was carried out in accordance with relevant regulations of the US Health Insurance Portability and Accountability Act (or HIPAA). Details that might disclose the identity of the subjects under study have been omitted. This study was approved by the Institutional Review Board (IRB ID: 5276). This study was performed at the American Hip Institute Research Foundation.
Since August of 2019, all patients who underwent hip arthroscopy by the senior author (B.D.G.) between April 2008 and April 2020 received an anchor question that read: “Taking into account the outcome of your surgery, would you choose to undergo the surgery again?” Patients could respond with either “yes” or “no” to this question. Patients were included in this study if they underwent primary hip arthroscopy for FAIS and labral tears with a concomitant endoscopic repair of symptomatic GM tear, had completed a questionnaire containing the anchor question, and had minimum 1-year follow-up. This questionnaire included the NAHS14 and the VAS for pain.2 Patients who had a preoperative score that was already at the maximum value for the NAHS and VAS were excluded. Patients were excluded if they had a previously diagnosed ipsilateral hip conditions (such as Legg-Calvé-Perthes disease, avascular necrosis, or slipped capital femoral epiphysis), previous ipsilateral hip surgery, hip osteoarthritis (Tönnis grade ≥2), or Ehlers-Danlos syndrome. Patients were also excluded if they marked themselves as unwilling to participate in the study. The data collection received approval from an Institutional Review Board.
A comprehensive physical examination before surgery was performed by the senior author. The physical exam included assessment of the range of motion, gait, and signs of FAIS. For GM pathology, peritrochanteric pain and tenderness was assessed. The modified resisted internal rotation test was performed.15 Presence of Trendelenburg sign was documented. Abductor strength was measured with patient lying on their unaffected side with the affected leg abducted, extended at the hip and knee, and slightly internally rotated. Gluteal and concomitant FAIS were then confirmed with radiographic imaging (45° modified Dunn view, anteroposterior pelvis view in the upright and supine positions, and a false profile view) and magnetic resonance arthrography. Cam-type morphology was defined as an alpha angle >55°. GM pathology on magnetic resonance imaging (MRI) was graded as tendinosis, partial-thickness tear, or full-thickness tear.16
Before being recommended for surgery, all patients underwent a minimum of 3 months of conservative treatment such as rest, physical therapy, activity modification, anti-inflammatory medications, and ultrasound-guided therapeutic injections. If a patient failed all nonoperative measures, the senior author recommended them for surgery The surgical technique for hip arthroscopy, endoscopic GM repair, and rehabilitation protocol have been described in prior publications.3,17, 18, 19, 20
Patient-Reported Outcome Scores Evaluation
Patients were assessed preoperatively, 3 months postoperatively, and annually thereafter. All patients had reported preoperative and minimum 1-year scores for the NAHS and VAS. Patients also all completed the anchor question. The MOI is calculated as described in previous studies using the following formula:11,21,22
The MOWTs were determined using receiver operating characteristic (ROC) analysis with the area under the curve (AUC).21 The AUC with 95% confidence intervals was used to identify patients willing to undergo surgery again and those unwilling.23 An AUC ≥0.7 was considered acceptable. An AUC ≥0.8 was considered exceptional.24,25 Using the Youden index and maximizing specificity and sensitivity, we determined the thresholds for both NAHS and VAS.26
Statistical Analysis
Categorical variables were assessed with a chi-square or Fisher exact test. Continuous variables were evaluated for variance and normality using F tests and Shapiro-Wilk tests, respectively. T-tests and nonparametric equivalent tests were used to calculate statistical significance. Statistical significance was indicated by a P value <.05. Continuous variables were reported as means with 95% confidence intervals. Categorical variables were reported as number and percentage. Statistical analyses were performed using Microsoft Excel and RStudio Desktop (version 1.2.1093; R Studio).
Results
Patient Demographics
A total of 119 patients were identified for inclusion. Four of these were excluded for having the maximal preoperative scores preoperatively, and 8 were excluded because of inadequate follow-up, leaving 107 patients (107 hips) to be included in the study. The group consisted of 101 (94.4%) females and 6 (5.6%) males. The average age was 56.20 ± 9.88 years, and the average body mass index was 28.80 ± 4.92 kg/m2. The group’s average follow-up time was 54.89 ± 29.52 months. Patient demographics and characteristics are detailed in Table 1.
Table 1.
Patient Demographics
| Parameter | Value |
|---|---|
| Hips included in study | |
| Right | 57 (53.3) |
| Left | 50 (46.7) |
| Sex | |
| Male | 6 (5.6) |
| Female | 101 (94.4) |
| Age at surgery, years | 56.20 [54.32, 58.07] |
| BMI, kg/m2 | 28.80 [27.87, 29.73] |
| Follow-up time, months | 54.89 [49.29, 60.48] |
Values are presented as number (%) or mean [95% confidence interval].
BMI, body mass index.
Patient-Reported Outcome Scores
Patients reported statistically significant improvements in both NAHS (P < .001) and VAS (P < .001). Eighty-nine (83.2%) patients reported that they would be willing to undergo the surgery again, taking into account the outcome of their surgery. Complete PRO data can be found in Table 2.
Table 2.
Patient-Reported Outcome Scores
| Parameter | Score |
|---|---|
| NAHS (means ± SD, CI) | |
| Preoperative | 57.72 [55.18, 60.26] |
| Latest | 82.99 [79.87, 86.11] |
| Pre-Postoperative P value | <0.001 |
| Improvement | 25.27 [21.54, 29.00] |
| VAS (means ± SD, CI) | |
| Preoperative | 5.49 [5.13, 5.84] |
| Latest | 2.12 [1.67, 2.58] |
| Pre-Postoperative P value | <0.001 |
| Improvement | -3.36 [-3.88, -2.85] |
| Patient Willingness | |
| Would choose to undergo surgery again | 89 (83.2) |
| Would not choose to undergo surgery again | 18 (16.8) |
Values are presented as number (%) or mean [95% confidence interval (CI)].
NAHS, nonarthritic hip score; VAS, visual analog scale for pain.
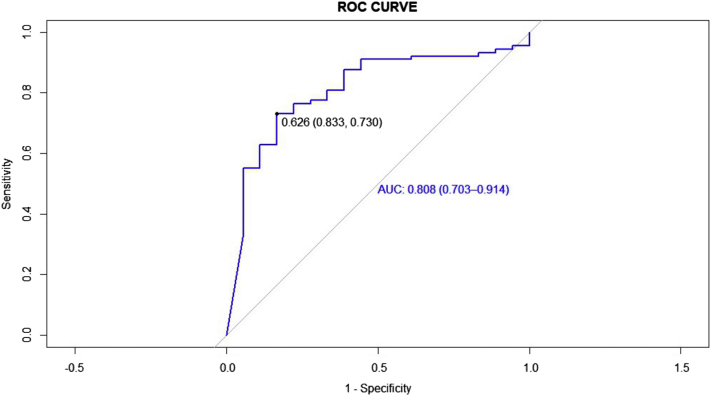
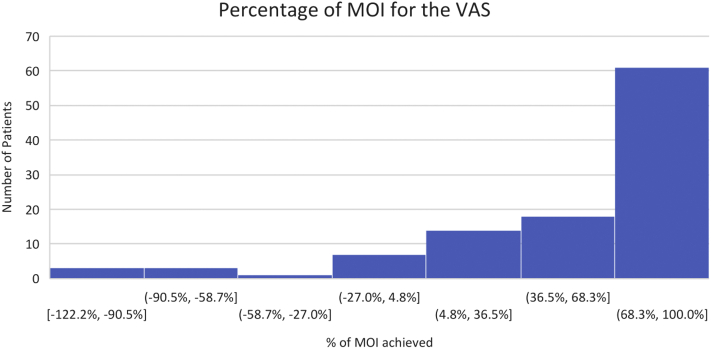
The ROC analysis determined that the MOWT for the NAHS was 54.7% (AUC: 0.847; 95% CI: 0.77-0.93). The MOWT for the VAS was 62.6% (AUC: 0.808; 95% CI: 0.70-0.91) (Figs 1 and 2, Table 3). Both AUC values for the curves were greater than 0.8, which indicates strong discrimination. The distribution of the percentage of MOI reached per score is reported in Figs 3 and 4. The probability of a patient being willing to undergo surgery again if they met the MOI threshold was 85.8% and 85.6% for the NAHS and VAS, respectively.
Fig 1.
Receiver operating characteristic (ROC) analysis with the area under the curve (AUC) for the Nonarthritic Hip Score.
Fig 2.
Receiver operating characteristic (ROC) analysis with the area under the curve (AUC) for the visual analog scale for pain.
Table 3.
Receiver Operating Characteristic Analysis
| core | Threshold | Sensitivity | Specificity | AUC (95% CI) | Cases Achieving MOWT, n (%) |
|---|---|---|---|---|---|
| NAHS | 54.7% | .708 | .889 | 0.847 (.0766-.929) | 65 (60.7%) |
| VAS | 62.6% | .730 | .833 | 0.808 (.703-.914) | 68 (63.6%) |
NAHS, Nonarthritic Hip Score; VAS, Visual Analog Scale for pain; MOWT, maximal outcome improvement willingness threshold; AUC, area under the curve; CI, confidence interval.
Fig 3.
Histogram of the percentage of maximal outcome improvement (MOI) for the Nonarthritic Hip Score (NAHS).
Fig 4.
Histogram of the percentage of maximal outcome improvement (MOI) for the visual analog score for pain (VAS).
Discussion
The main finding of the present study was that MOWTs were determined for the NAHS and VAS following hip arthroscopy with hip endoscopy for the surgical treatment of FAIS and GM tear, respectively that were predictive of willingness to undergo surgery again. Specifically, the MOI thresholds were 54.7% for the NAHS and 62.6% for the VAS. Further, 85.8% and 85.6% of the patients who met the MOI threshold for the NAHS and VAS, respectively, were willing to undergo surgery again. The use of the MOWTs does not imply the exclusion of the PASS, MCID or SCB, in fact, these clinical assessment tools can supplement each other.13
In a retrospective study that included 2,851 hips, Meghpara et al.1 reported that the prevalence of asymptomatic GM pathologies in patients with the diagnosis of FAIS and labral tear was 16.0% on MRI. Moreover, 1.7% had partial-thickness GM tears, whereas none had full-thickness tears. The addition of surgical GM pathology management on the FAIS population must be based on a complete clinical evaluation rather than exclusively on MRI findings. However, in FAIS patients with symptomatic GM partial-thickness tears, determining which are compensatory and which are actually pathologic is still a conundrum.27
Combined hip arthroscopy, in the context of arthroscopic FAIS and labral tear, with endoscopic GM repair, reported significant improvement in several PROs, and high patient satisfaction at a minimum 5-year follow-up. Regardless of the GM tear severity, comparable PROs were found at the latest follow-up. Furthermore, when patients with GM repair were propensity-matched (age, body mass index, sex, labral treatment, acetabular, and femoral head Outerbridge grade) to a group with only arthroscopic labral treatment, and mid-term results were reported to be similar.3
Previously, the validity of the MOI threshold assessing patient satisfaction has been proven for arthroscopic rotator cuff tear repair.11 This finding has also been demonstrated within the hip preservation realm. Maldonado et al. reported the MOI threshold for several PROs, including NAHS and VAS in patients who underwent hip arthroscopy for FAIS and labral tear treatment.12 The values associated with satisfaction were 52.5% and 55.5%, for the NAHS and VAS, respectively.
The greater trochanteric pain syndrome, which includes GM pathology,28 has been described as a debilitating condition for lateral hip pain more commonly seen in women with a higher incidence between the fourth and sixth decades of life,29, 30, 31, 32, 33 as reflected in the present investigation. These patient demographic characteristics do not represent the common denominator for patients undergoing hip arthroscopy for solely FAIS. Therefore, extrapolated clinical metrics, particularly the MOI within the context of this study, between these groups is inaccurate. The present investigation is one of the few providing MOWTs, for the NAHS and VAS, specifically for patients with the diagnosis of FAIS and symptomatic GM tears, following combined hip arthroscopy and hip endoscopy, respectively.
Limitations
The present study has limitations. The investigation used a retrospective methodology, which leads to recall bias. The analysis was based on a single institution/single surgeon database, which may compromise the reproducibility of the results presented. Patients were included only if they completed the anchor question, which led to response bias. Furthermore, the results presented were exclusively for patients who underwent hip arthroscopy with concomitant hip endoscopy for the treatment of FAIS and GM tear, respectively; however, these cannot be extrapolated to alternative treatment options, such as open GM tear repair with or without concomitant hip arthroscopy.
Conclusion
The MOWTs that were predictive of willingness to undergo surgery again following primary hip arthroscopy with concomitant endoscopy for GM tear repair were 54.7% and 62.6% for the NAHS, and VAS, respectively.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: D.R.M. is an editorial board member of the Journal of Arthroscopy; he reports nonfinancial support from Arthrex, Stryker, Smith & Nephew, and Ossur, outside the submitted work. B.R.S. reports grants from Arthrex and personal fees from DJO Global, outside the submitted work. A.C.L. reports grants, personal fees, and nonfinancial support from Arthrex, nonfinancial support from Iroko, nonfinancial support from Medwest, nonfinancial support from Smith & Nephew, grants and nonfinancial support from Stryker, nonfinancial support from Vericel, nonfinancial support from Zimmer Biomet, personal fees from Graymont Medical, outside the submitted work. B.G.D. reports grants and other from American Orthopedic Foundation, during the conduct of the study; personal fees from Amplitude, grants, personal fees and nonfinancial support from Arthrex, personal fees and a speaker fee from DJO Global, grants, personal fees and nonfinancial support from Medacta, grants, personal fees, nonfinancial support and other from Stryker, grants from Breg, personal fees from Orthomerica, grants and nonfinancial support from Medwest Associates, grants from ATI Physical Therapy, personal fees and nonfinancial support from St. Alexius Medical Center, grants from Ossur, outside the submitted work. In addition, he has a patent 8920497 - Method and instrumentation for acetabular labrum reconstruction with royalties paid to Arthrex, a patent 8708941 - Adjustable multi-component hip orthosis with royalties paid to Orthomerica and DJO Global, and a patent 9737292 - Knotless suture anchors and methods of tissue repair with royalties paid to Arthrex. He is also a board member of American Hip Institute Research Foundation, AANA Learning Center Committee, the Journal of Hip Preservation Surgery, the Journal of Arthroscopy; has had ownership interests in the American Hip Institute, Hinsdale Orthopedic Associates, Hinsdale Orthopedic Imaging, SCD#3, North Shore Surgical Suites, and Munster Specialty Surgery Center. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Meghpara M.B., Bheem R., Shah S., et al. Prevalence of gluteus medius pathology on magnetic resonance imaging in patients undergoing hip arthroscopy for femoroacetabular impingement: Asymptomatic tears are rare, whereas tendinosis is common. Am J Sports Med. 2020;48:2933–2938. doi: 10.1177/0363546520952766. [DOI] [PubMed] [Google Scholar]
- 2.Sun H, Huang HJ, Mamtimin M, et al. Isolated arthroscopic treatment of femoroacetabular impingement for patients with radiographic gluteus medius tear. Arthroscopy In press. https://doi.org/10.1016/j.arthro.2021.10.006.
- 3.Meghpara M.B., Yelton M.J., Annin S., et al. Mid-term outcomes of endoscopic gluteus medius repair with concomitant arthroscopic labral treatment: A propensity-matched controlled study. Arthroscopy. 2020;36:2856–2865. doi: 10.1016/j.arthro.2020.07.020. [DOI] [PubMed] [Google Scholar]
- 4.Beck E.C., Nwachukwu B.U., Kunze K.N., Chahla J., Nho S.J. How can we define clinically important improvement in pain scores after hip arthroscopy for femoroacetabular impingement syndrome? Minimum 2-year follow-up study. Am J Sports Med. 2019;47:3133–3140. doi: 10.1177/0363546519877861. [DOI] [PubMed] [Google Scholar]
- 5.Ueland T.E., Disantis A., Carreira D.S., Martin R.L. Patient-reported outcome measures and clinically important outcome values in hip arthroscopy: A systematic review. JBJS Rev. 2021;9 doi: 10.2106/JBJS.RVW.20.00084. [DOI] [PubMed] [Google Scholar]
- 6.Kunze K.N., Bart J.A., Ahmad M., Nho S.J., Chahla J. Large heterogeneity among minimal clinically important differences for hip arthroscopy outcomes: A systematic review of reporting trends and quantification methods. Arthroscopy. 2021;37:1028–1037.e6. doi: 10.1016/j.arthro.2020.10.050. [DOI] [PubMed] [Google Scholar]
- 7.Harris J.D., Brand J.C., Cote M.P., Faucett S.C., Dhawan A. Research pearls: The significance of statistics and perils of pooling. Part 1: Clinical versus statistical significance. Arthroscopy. 2017;33:1102–1112. doi: 10.1016/j.arthro.2017.01.053. [DOI] [PubMed] [Google Scholar]
- 8.Pham T., Tubach F. Patient acceptable symptomatic state (PASS) Joint Bone Spine. 2009;76:321–323. doi: 10.1016/j.jbspin.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 9.Kvien T.K., Heiberg T., Hagen K.B. Minimal clinically important improvement/difference (MCII/MCID) and patient acceptable symptom state (PASS): What do these concepts mean? Ann Rheum Dis. 2007;66(Suppl 3):iii40–iii41. doi: 10.1136/ard.2007.079798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nwachukwu B.U. Editorial commentary: Maximal outcome improvement: Another arrow in the quiver. Arthroscopy. 2021;37:1486–1487. doi: 10.1016/j.arthro.2021.03.001. [DOI] [PubMed] [Google Scholar]
- 11.Beck E.C., Gowd A.K., Liu J.N., et al. How is maximum outcome improvement defined in patients undergoing shoulder arthroscopy for rotator cuff repair? A 1-year follow-up study. Arthroscopy. 2020;36:1805–1810. doi: 10.1016/j.arthro.2020.02.047. [DOI] [PubMed] [Google Scholar]
- 12.Maldonado D.R., Kyin C., Shapira J., et al. Defining the maximum outcome improvement of the modified Harris hip score, the nonarthritic hip score, the visual analogue scale for pain, and the International Hip Outcome Tool-12 in the arthroscopic management for femoroacetabular impingement syndrome and labral tear. Arthroscopy. 2021;37:1477–1485. doi: 10.1016/j.arthro.2021.01.002. [DOI] [PubMed] [Google Scholar]
- 13.Lubowitz J.H., Brand J.C., Rossi M.J. Our measure of medical research should be appreciable benefit to the patient. Arthroscopy. 2019;35:1943–1944. doi: 10.1016/j.arthro.2019.04.033. [DOI] [PubMed] [Google Scholar]
- 14.Christensen C.P., Althausen P.L., Mittleman M.A., Lee J ann, McCarthy J.C. The nonarthritic hip score: Reliable and validated. Clin Orthop Relat Res. 2003;(406):75–83. doi: 10.1097/01.blo.0000043047.84315.4b. [DOI] [PubMed] [Google Scholar]
- 15.Walker-Santiago R., Ortiz-Declet V., Maldonado D.R., Wojnowski N.M., Domb B.G. The modified resisted internal rotation test for detection of gluteal tendon tears. Arthrosc Tech. 2019;8:e331–e334. doi: 10.1016/j.eats.2018.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosinsky P.J., Diulus S.C., Walsh J.P., et al. Development of a predictive algorithm for symptomatic hip abductor tears in patients undergoing primary hip arthroscopy. Am J Sports Med. 2021;49:497–504. doi: 10.1177/0363546520980461. [DOI] [PubMed] [Google Scholar]
- 17.Maldonado D.R., Rosinsky P.J., Shapira J., Domb B.G. Stepwise safe access in hip arthroscopy in the supine position: Tips and pearls from A to Z. J Am Acad Orthop Surg. 2020;28:651–659. doi: 10.5435/JAAOS-D-19-00856. [DOI] [PubMed] [Google Scholar]
- 18.Maldonado D.R., Chen S.L., Chen J.W., et al. Prospective analysis of arthroscopic hip anatomic labral repair utilizing knotless suture anchor technology: The controlled-tension anatomic technique at minimum 2-year follow-up. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120935079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Domb B.G., Nasser R.M., Botser I.B. Partial-thickness tears of the gluteus medius: Rationale and technique for trans-tendinous endoscopic repair. Arthroscopy. 2010;26:1697–1705. doi: 10.1016/j.arthro.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 20.Domb B.G., Carreira D.S. Endoscopic repair of full-thickness gluteus medius tears. Arthrosc Tech. 2013;2:e77–e81. doi: 10.1016/j.eats.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berglund D.D., Damodar D., Vakharia R.M., et al. Predicting outstanding results after anatomic total shoulder arthroplasty using percentage of maximal outcome improvement. J Shoulder Elbow Surg. 2019;28:349–356. doi: 10.1016/j.jse.2018.08.016. [DOI] [PubMed] [Google Scholar]
- 22.DeVito P., Damodar D., Berglund D., et al. Predicting outstanding results after reverse shoulder arthroplasty using percentage of maximal outcome improvement. J Shoulder Elbow Surg. 2019;28:1223–1231. doi: 10.1016/j.jse.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 23.Lasko T.A., Bhagwat J.G., Zou K.H., Ohno-Machado L. The use of receiver operating characteristic curves in biomedical informatics. J Biomed Inform. 2005;38:404–415. doi: 10.1016/j.jbi.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 24.Mandrekar J.N. Receiver operating characteristic curve in diagnostic test assessment. J Thor Oncol. 2010;5:1315–1316. doi: 10.1097/JTO.0b013e3181ec173d. [DOI] [PubMed] [Google Scholar]
- 25.Rosinsky P.J., Chen J.W., Lall A.C., Shapira J., Maldonado D.R., Domb B.G. Can we help patients forget their joint? Determining a threshold for successful outcome for the forgotten joint score. J Arthroplasty. 2020;35:153–159. doi: 10.1016/j.arth.2019.08.014. [DOI] [PubMed] [Google Scholar]
- 26.Martínez-Camblor P., Pardo-Fernández J.C. The Youden Index in the generalized receiver operating characteristic curve context. Int J Biostat. 2019;15 doi: 10.1515/ijb-2018-0060. https://doi.org/10.1515/ijb-2018-0060 /j/ijb.2019. [DOI] [PubMed] [Google Scholar]
- 27.Gruskay J.A., Philippon M.J. Editorial Commentary: Indications for concurrent procedures during hip femoroacetabular impingement arthroscopic treatment. Arthroscopy. 2021;37:1853–1855. doi: 10.1016/j.arthro.2021.03.004. [DOI] [PubMed] [Google Scholar]
- 28.Annin S., Lall A.C., Meghpara M.B., et al. Intraoperative classification system yields favorable outcomes for patients treated surgically for greater trochanteric pain syndrome. Arthroscopy. 2021;37:2123–2136. doi: 10.1016/j.arthro.2021.01.058. [DOI] [PubMed] [Google Scholar]
- 29.Meghpara M.B., Yelton M.J., Annin S., et al. Return to activity after gluteus medius repair in active patients older than 50 Years. Orthop J Sports Med. 2021;9 doi: 10.1177/2325967120967968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Meghpara M.B., Bheem R., Haden M., et al. Differences in clinical presentations and surgical outcomes of gluteus medius tears between men and women. Am J Sports Med. 2020;48:3594–3602. doi: 10.1177/0363546520966335. [DOI] [PubMed] [Google Scholar]
- 31.Byrd J.W.T. Gluteus medius repair with double-row fixation. Arthrosc Tech. 2013;2:e247–e250. doi: 10.1016/j.eats.2013.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maldonado D.R., Annin S., Chen J.W., et al. Full-thickness gluteus medius tears with or without concomitant hip arthroscopy: Minimum 2-year outcomes using an open approach and contemporary tendon repair techniques. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120929330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Parker E.A., Meyer A.M., Laskovski J.R., Westermann R.W. Endoscopic gluteus medius repair with an ITB-sparing versus ITB-splitting approach: A systematic review and meta-analysis. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120922196. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.