Abstract
Background
Avascular necrosis (AVN) is a rare albeit serious condition that has a high risk for long term morbidity given the risk of chronic pain and arthroplasty after diagnoses. The recent rise in sports participation in the pediatric population demonstrates the importance of evaluating functional limitations after AVN treatment. Return to sport (RTS) rates after treatment for AVN have not been evaluated in pediatric or adolescent populations.
It is necessary to evaluate all joints impacted by AVN due to heterogenous nature of the disease and the variety of sports that could be impacted by disease specific activity restrictions. Thus, this present study aimed to characterize RTS rate after AVN treatment, determine if there was a difference in RTS rates after operative versus nonoperative management, and identify demographic and treatment factors associated with RTS rates.
Methods
This retrospective cohort study evaluated patients ages eight to twenty years old who were treated for symptomatic AVN of any joint between January 2005 and August 2021. Patient records were reviewed for demographic, disease, and treatment variables. Standard descriptive statistics and bivariate analyses were performed to describe and compare groups who did and did not RTS. A generalized estimating model was used to determine variables that were associated with better RTS rates.
Results
A total of 144 patients and 190 lesions were evaluated in the study, 60 patients (43%) were female with a mean age of 14.36+/-3.24 years. The overall RTS rate after AVN treatment was 67% (64/96). Roughly 8% of patients (5/64) were able to return to multiple sports, however of those that returned to sports, 6% (4/64) reported playing at a lower level of competition. There was not a significant difference between the RTS rate for those who underwent operative versus nonoperative management (70% versus 62%, p=0.38). Males were almost 2.5 times more likely to return to sport than females (OR: 2.46, p=0.018).
Conclusion
The ability to return to sports after AVN treatment has largely remained unknown in the pediatric and adolescent populations. Our data suggests that a majority of patients are able to RTS in the short term follow up with males being twice as likely to RTS compared to females. Physicians should maintain awareness of the long-term morbidity of AVN and understand the unique patient and disease characteristics that optimize functional outcomes in this population.
Level of Evidence: III
Keywords: AVN, avascular necrosis, sports, return to sport, pediatrics, lesion, RTS, adolescent, arthroplasty
Introduction
Avascular necrosis (AVN) is a morbid condition that can be understood as a final shared pathway where blood supply to the bone is impaired causing necrosis. Numerous etiologies lead to this shared pathway, including Legg-Calve-Perthes disease,1 sickle cell disease,2 corticosteroid exposure,3 slipped capitol femoral epiphysis,4 and idiopathic causes.5-7 Although relatively rare in the general population, estimates place new diagnoses of AVN around 10,000 to 30,000 a year in the U.S.7,8 While AVN is often diagnosed in older patients aged 30 to 65, children and adolescents with the aforementioned conditions are at higher risk of developing AVN than their healthy counterparts.9
In this younger at-risk population, the outcomes and long-term prognosis are less than ideal. Lesions in weight-bearing joints, like the hip, commonly cause symptoms of pain and can eventually progress to joint collapse.5 While there are many nonoperative and operative treatments for AVN such as hyperbaric-oxygen,10 bisphosphonate therapy,11 zoledronic acid,11,12 osteotomy, core decompression with or without bone marrow aspirate concentrate (BMAC),13,14 many patients will require a joint arthroplasty for definitive treatment.15
Previous literature examining AVN outcomes have evaluated pain, rates of arthroplasty, and rates of hardware survival.15-17 However, there is a need to better understand functional outcomes for those diagnosed with AVN in any joint, especially in pediatric and adolescent populations. Given the increasing amount of youth sport participation and earlier ages of sports specialization,18,19 there is a need to evaluate return to sports (RTS) rates in pediatric and adolescent patients treated for AVN. Furthermore, it is critical to evaluate all joints impacted by AVN due to the heterogeneous nature of the disease and the variety of sports that could be impacted by disease specific activity restrictions. To address this gap in literature, this study aims to characterize RTS rates after AVN treatment in any joint, determine if there was a difference in RTS rates after operative versus nonoperative management, and identify demographic and treatment factors associated with better RTS rates in pediatric and adolescent patient populations.
Methods
Following institutional review board-approval, we performed a retrospective cohort study evaluating patients who were diagnosed with avascular necrosis (AVN) of any joint at a single tertiary pediatric hospital. Patients eight to twenty years old who were treated for symptomatic AVN between 1/1/2005 and 12/31/2021 were included. Patients who were asymptomatic, did not have AVN confirmed by radiographs or advanced imaging, or did not have at least 12 months of follow up were excluded from the study.
AVN diagnosis was confirmed based on EMR documentation, radiographs, and the following ICD-9 and ICD-10 codes: 733.4, 733.41, 733.42, 733.43, 733.44, 733.49, M87, M87.0, M87.00, M87.01, M87.01, M87.012, M87.019, M87.02, M87.021, M87.022, M87.029, M87.03, M87.031, M87.032, M87.033, M87.034, M87.035, M87.036, M87.037, M87.038, M87.039, M87.05, M87.050, M87.051, M87.052, M87.059, M87.06, M87.061, M87.062, M87.063, M87.064, M87.065, M87.066, M87.07, M87.071, M87.072, M87.073, M87.074, M87.075, M87.076, M87.08, M87.09, M87.8, M87.80.
Authors collected demographic and treatment data for all patients who met inclusion criteria, including variables such as age, sex, AVN location, treatment type (operative vs. nonoperative), and etiology of AVN. Data was also collected on the patient’s ability to RTS, the type of sport returned to, and impact level of the sport. Each patient’s sport involvement status was based on chart review of all Orthopedic specific visits combined with a complimentary text search of all hospital encounters that referenced sports during their treatment. As per routine institutional practice, treating physicians documented each patient’s baseline activity level and the activities they are involved in, including sports. Patients were classified as returned to sport if there was post-treatment documentation of sport involvement or the treatment plan referenced sport specific advancements in activity levels. Common post-treatment visit statements included, “patient returned to…” and “patient is now involved in…”. Patients underwent routine clinical follow up at intervals based on current treatment of AVN.
Standard descriptive statistics were used to report demographic variables. Bivariate analyses of the primary outcomes of interest (RTS) were performed using Chi-square, Fisher’s test, Mann-Whitney U, and Kruskal-Wallis tests. Considering that some patients had multiple AVN-affected joints, we utilized generalized estimating equations model (GEE model) for regression to account for correlated repeated measures among our study population. All statistical analysis was completed with Stata 15 (College Station, TX) and statistical significance was considered to be p< 0.05.
Results
Demographics
Over the sixteen-year period ending in 2021, 265 patients were initially identified as eligible (Figure 1). There were 47 patients excluded for having asymptomatic AVN or being outside the age range, leaving 218 for review. A total of 74 patients were removed for having less than 1 year of follow up, leaving a total of 144 patients with 190 AVN-affected joints available for study. Of the 144 patients, 60 (43%) were female with a mean age of 14.36 +/- 3.24 years (Table 1). AVN lesions were most commonly located in the hips (57%, 108/190), followed by the knees (23%, 43/190), ankles (11%, 21/190), and shoulders (6%, 12/190). High dose courses of steroids were the most common etiology for AVN lesions followed by sickle cell anemia and idiopathic causes (Table 1). Over 50% of lesions (56%, 106/190) underwent operative treatment, whereas 44% (84/190) received nonoperative management with physical therapy and observation. The majority of patients who underwent operative treatment received core decompression and bone marrow aspiration (Table 2).
Figure 1.
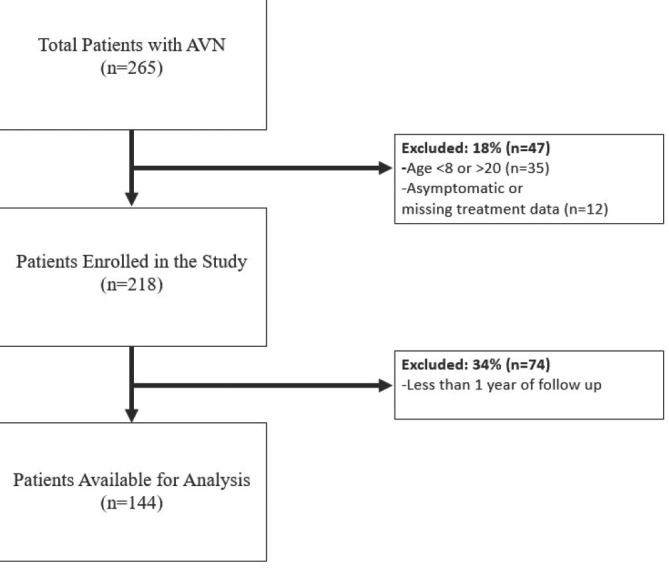
The STROBE flow chart of inclusion criteria.
Table 1.
Population Demographics for Patients with AVN Treatment in Surgical and Nonoperative Populations
| Variable | Total Population (n=144, lesions =190) | Surgical Treatment (n=89, lesions=106) | Nonoperative Treatment (n=55, lesions=84) | Chi Square | P value |
|---|---|---|---|---|---|
| Sex | 1.03 | 0.31a | |||
| Male | 84 (57%) | 49 (55%) | 35 (63%) | ||
| Female | 60 (43%) | 40 (45%) | 20 (37%) | ||
| Race | 10.87 | 0.055a | |||
| Caucasian | 49 (34%) | 38 (43%) | 11 (20%) | ||
| African American | 23 (16%) | 14 (16%) | 9 (16%) | ||
| Asian | 6 (4%) | 4 (4%) | 2 (4%) | ||
| Indian | 1 (1%) | 0 (0%) | 1 (2%) | ||
| Other | 8 (6%) | 3 (3%) | 5 (9%) | ||
| Unknown | 57 (39%) | 30 (34%) | 27 (49%) | ||
| Ethnicity | 4.303 | 0.116a | |||
| Non-Hispanic | 76 (52%) | 53 (60%) | 23 (42%) | ||
| Hispanic | 11 (8%) | 6 (6%) | 5 (9%) | ||
| Unknown | 57 (40%) | 30 (34%) | 27 (49%) | ||
| Age at First Lesion | 14.36 +/-3.24 | 13.88 +/- 3.08 | 14.96 +/- 3.35 | 0.023b | |
| Location of Lesion | 12.018 | 0.035a | |||
| Hip | 108 (57%) | 69 (65%) | 39 (47%) | ||
| Knee | 43 (23%) | 21 (20%) | 22 (26%) | ||
| Ankle | 21 (11%) | 10 (9%) | 11 (13%) | ||
| Shoulder | 12 (6%) | 3 (3%) | 9 (11%) | ||
| Elbow | 4 (2%) | 3 (3%) | 1 (1%) | ||
| Hand | 2 (1%) | 0 (0%) | 2 (2%) | ||
| Laterality | 1.176 | 0.555a | |||
| Right | 83 (44%) | 47 (44%) | 36 (43%) | ||
| Left | 77 (41%) | 40 (38%) | 37 (44%) | ||
| Both | 30 (15%) | 19 (18%) | 11 (13%) | ||
| Cause of Lesion | 14.628 | 0.102a | |||
| Steroid Induced (Cancer) | 59 (31%) | 34 (32%) | 25 (30%) | ||
| Sickle Cell Anemia | 48 (25%) | 23 (22%) | 25 (30%) | ||
| Idiopathic | 25 (13%) | 16 (14%) | 9 (11%) | ||
| Septic Arthritis | 9 (5%) | 2 (2%) | 7 (8%) | ||
| Trauma | 8 (4%) | 7 (7%) | 1 (1%) | ||
| DDH | 7 (3%) | 5 (5%) | 2 (2%) | ||
| Perthes | 4 (2%) | 3 (3%) | 1 (1%) | ||
| SCFE | 3 (2%) | 3 (3%) | 0 (0%) | ||
| Juvenile Idiopathic Arthritis | 1 (1%) | 0 (0%) | 1 (1%) | ||
| Length of Follow Up (months) | 27.50 (18 to 43.5) | 32.5 (23.5 to 51) | 24 (16 to 29) | 0.0001c | |
Data is presented as n(%), mean +/- SD, or median (IQR). a- chi square test, b- independent t test, c-Kruskal Wallis. P value less than 0.05 in bold.
Table 2.
Surgical Treatment Type Overview
| Variable | Total Population (n=106) |
|---|---|
| Core Decompression with Bone Marrow Aspiration | 63 (59%) |
| Unknown | 12 (11%) |
| Joint Replacement | 9 (8%) |
| Osteotomy (femoral, tibial) | 7 (7%) |
| Hardware Removal | 4 (4%) |
| Pelvic Acetabular Osteotomy with Bone Graft | 3 (3%) |
| Surgical Debridement | 3 (3%) |
| Epiphysiodesis | 2 (2%) |
| Arthrogram | 1 (1%) |
| Surgical Dislocation with femoral neck lengthening | 1 (1%) |
| Screw Fixation with Allograft | 1 (1%) |
| Total | 106 |
Data is presented as n(%)
The median post treatment follow-up for all patients was 27.5 months (IQR: 18 to 43.5 months).
Return to Sport Rate After AVN Treatment
The overall return to sport rate after AVN treatment was 67% (64 of 96). Swimming, basketball, and baseball/softball were the most commonly played sports after treatment (Table 3). However, roughly 8% of patients (5/64) were able to return to multiple sports. Of those that returned to sports, 6% (4/64) reported playing at a lower level of competition and 5% (3/64) reported switching their primary sport after their treatment.
Table 3.
Return to Sport After AVN Treatment in Surgical and Nonoperative Populations
| Variable | Surgical Treatment (n=89) | Nonoperative Treatment (n=55) | Chi Square | P Value |
|---|---|---|---|---|
| Participation in Sport (After Treatment) | 0.78 | 0.38a | ||
| Yes | 40 (70%) | 24 (62%) | ||
| No | 17 (30%) | 15 (38%) | ||
| Sport Returned To | 12.413 | 0.19a | ||
| Multiple | 3 (16%) | 2 (22%) | ||
| Other (dance, lacrosse, cheerleading, equestrian, etc.) | 4 (22%) | 0 (0 %) | ||
| Swimming | 3 (16%) | 1 (11%) | ||
| Baseball/Softball | 2 (10%) | 2 (22%) | ||
| Basketball | 2 (10%) | 2 (22%) | ||
| Football | 3 (16%) | 0 (0 %) | ||
| Soccer | 0 (0 %) | 2 (22%) | ||
| Tennis | 1 (5%) | 0 (0 %) | ||
| Golf | 1 (5%) | 0 (0 %) | ||
| Impact of Sport | 0.92 | 0.34a | ||
| Low Impact | 14 (74%) | 5 (56%) | ||
| High Impact | 5 (26%) | 4 (44%) | ||
| Changed Sport | 0.49b | |||
| Yes | 3 (50%) | 0 (0 %) | ||
| No | 3 (50%) | 1 (100%) | ||
| Level of Competition after Treatment | 0.517b | |||
| Lower | 4 (50%) | 0 (0 %) | ||
| Same | 2 (25%) | 1 (33%) | ||
| Higher | 2 (25%) | 2 (67%) | ||
Data is presented as n(%). P values were calculated using the following: a-Chi Square Test, b-Fisher’s Exact Test
Difference in RTS Rates After Operative Versus Nonoperative Management
There was not a significant difference between the return to sport rate for those who underwent operative versus nonoperative management (70% [40/57] versus 62% [24/39] respectively, p=0.38). There also was no difference in the type of sport returned to or impact level of the sport between the two treatment cohorts (Table 3).
Demographic, Lesion, and Treatment Factors Associated With Better RTS Rates
Based on the GEE model, males were almost 2.5 times more likely to return to sport than females (OR: 2.46, 95% CI: 1.16 to 5.20, p=0.018). There was not a difference in proportion of patients who returned to sport based on age, race, ethnicity, location of the lesion, cause of the lesion, or type of treatment.
Discussion
Our study, a cohort of 144 patients and 190 joints, described the epidemiology and factors associated with return to sport rates among pediatric and adolescent patients treated for AVN. To our knowledge, this is the first study to evaluate return to sports rates, as a functional outcome, in this patient population. Our results suggest that a majority of patients are able to return to sport in some form in the short term and that males were significantly more likely to return to sport than females.
The epidemiologic results of our patient population mirror those found in prior studies. Most pediatric and adolescent literature report that common AVN-affected joints are the hips and knees, followed by the shoulders, ankles, and elbows.20-22 The majority of patients had a history of corticosteroid treatment which redemonstrates the risk of AVN following treatment for cancer or autoimmune conditions.21-23 A majority of the patients in the study cohort were able to return to sport. Given that the ability to return to activity after AVN treatment has largely remained unknown in the pediatric and adolescent populations, our study provides an importation foundation for postoperative expectations for both providers and patients. A recent study demonstrated that there is low return to impact activity after core decompression of femoral head AVN.24 However, this study was conducted in military members who were significantly older and had higher activity requirements than our study.24 Furthermore, our study also evaluated lesions in non-weightbearing joints where there may be less risk of joint collapse and quicker return to activity. Although our study did not find a difference between return to sport and AVN location, there may be a difference at mid to long term follow up.
Our study also surprisingly demonstrated that there was no difference in return to sport rates between those treated operatively and nonoperatively. Given that treatment outcomes for AVN are associated with disease severity, with most studies showing advanced disease has poorer outcomes,24,25 one might expect that those receiving operative care would have more advanced disease and lower likelihood of return to sport. However, our study demonstrated that a majority of operative patients return to sport in the short term follow up. Patients who received operative intervention were younger than those in the nonoperative cohort therefore there could be a treatment bias where the younger patients had more severe disease requiring surgery. However, the clinical influence of patient age is unclear since there is less than one year difference between the cohorts and no overall difference in return to sport rate. In addition, our study evaluated return to sport in patients with over a year of follow up, however there could be long term differences between those who undergo operative and nonoperative management.
The result that males are more likely to return to sport than females has been reported in other conditions, including concussions and anterior cruciate ligament reconstructions.26-28 A recent meta-analysis on anterior cruciate ligament reconstruction reported that females differed in both subjective and functional outcomes post reconstruction, and had lower return to sport rates than their male counterparts.28 One theory for the difference in return to sports rates between sexes is psychological and developmental differences between males and females. It is important to note that successful return to sport is a multifactorial outcome dependent on risk of re-injury, presence of clear athletic goals, and other psychosocial factors. Due to the heterogeneity of AVN lesions and the corresponding recovery timelines, further research is needed to identify subgroups at risk for worse recovery. However, our results can provide an initial framework for generalized recovery expectations after AVN treatment.
We were unable to identify any other patient, AVN lesion, or treatment characteristics to define a subgroup of patients that would be more likely to return to sport. Our findings suggest that it is difficult to predict which pediatric patients will return to sport, however other AVN lesion and treatment characteristics should be explored before definitive recommendations are issued. Specifically, outcome studies using lesion classification systems such as the Steinberg Classification System for AVN of the femoral head could be used to further define hip lesion specifics. Given the rare and heterogenous nature of AVN, randomized trials comparing return to sport after specific treatment may not be feasible, although future studies could investigate other aspects of treatment and recovery strategies such as frequency of physical therapy, types of surgery, cost-effectiveness of surgery, and psychosocial implications for patients.
Limitations
Foremost, our study is not designed to answer definitely the question of whether specific patient or operative interventions allow for long term return to sport after AVN treatment, as it does not account for other considerations such as the long-term morbidity associated with lesion size, nor have we performed a psychosocial evaluation of patients returning to sport. Second, this study is limited by the sample size related to the rarity and heterogeneity of AVN. In particular, our study may have been underpowered to detect difference in the type of sports played, impact of sport, or competition level. However, the inclusion of these variables was to provide an epidemiologic framework for future studies to use while evaluating patients. It is also likely that other factors we did not consider, such as poorly understood variables related to specific lesion biology, may be useful in identifying patients at risk for high recurrence and failure to return to sport. Thirdly, this study characterized return to sport after at least one year of follow, but future studies should look for long term return to sport rate and associated retention rates. It is possible some or many of these patients return to sport initially after treatment, only to worsen to the point of needing arthroplasty in the long-term. Finally, this study is limited by certain biases related to its retrospective design. While this study sought to use preexisting data to establish whether there are factors influencing return to sports rates, future studies could utilize patient callback or prospective study design to further characterize the results.
Conclusion
Rates of arthroplasty have been historically helpful in characterizing end stage outcomes of AVN, however functional outcome measures like return to sport provide valuable information to providers treating pediatric and adolescent patients. The ability to return to sports after AVN treatment has largely remained unknown in this population. Our data suggests that a majority of patients are able to return to sport in the short term follow up. Furthermore, males are over twice as likely to return to sport compared to females. We were unable to further define a subgroup that could return to sport in the short term follow up. Physicians should maintain awareness of the long-term morbidity of AVN and understand the unique patient and disease characteristics that optimize functional outcomes in this population.
References
- 1.Leroux J, Abu Amara S, Lechevallier J. Legg-Calvé-Perthes disease. Orthop Traumatol Surg Res. 2018;104(1) doi: 10.1016/j.otsr.2017.04.012. [DOI] [PubMed] [Google Scholar]
- 2.Adesina O, Brunson A, Keegan THM, Wun T. Osteonecrosis of the femoral head in sickle cell disease: prevalence, comorbidities, and surgical outcomes in California. Blood Adv. 2017;1(16):1287–1295. doi: 10.1182/bloodadvances.2017005256. Jul 11; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McAvoy S, Baker KS, Mulrooney D, Blaes A, Arora M, Burns LJ, Majhail NS. Corticosteroid dose as a risk factor for avascular necrosis of the bone after hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2010;16(9):1231–6. doi: 10.1016/j.bbmt.2010.03.008. Sep; [DOI] [PubMed] [Google Scholar]
- 4.Mullins MM, Sood M, Hashemi-Nejad A, Catterall A. The management of avascular necrosis after slipped capital femoral epiphysis. J Bone Joint Surg Br. 2005;87(12):1669–74. doi: 10.1302/0301-620X.87B12.16665. Dec; [DOI] [PubMed] [Google Scholar]
- 5.Lespasio MJ, Sodhi N, Mont MA. Osteonecrosis of the Hip: A Primer. Perm J. 2019;23:18–100. doi: 10.7812/TPP/18-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lafforgue P. Pathophysiology and natural history of avascular necrosis of bone. Joint Bone Spine. 2006;73(5):500–7. doi: 10.1016/j.jbspin.2006.01.025. Oct; [DOI] [PubMed] [Google Scholar]
- 7.Moya-Angeler J, Gianakos AL, Villa JC, Ni A, Lane JM. Current concepts on osteonecrosis of the femoral head. World J Orthop. 2015;6(8):590601. doi: 10.5312/wjo.v6.i8.590. Sep 18; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am. 1995;77(3):459–74. doi: 10.2106/00004623-199503000-00018. [DOI] [PubMed] [Google Scholar]
- 9.Kadan-Lottick NS, Dinu I, Wasilewski-Masker K, Kaste S, Meacham LR, Mahajan A, et al. Osteonecrosis in adult survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol. 2008;26(18):3038–45. doi: 10.1200/JCO.2007.14.9088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Camporesi EM, Vezzani G, Bosco G, Mangar D, Bernasek TL. Hyperbaric oxygen therapy in femoral head necrosis. J Arthroplasty. 2010;25(6 Suppl):118–23. doi: 10.1016/j.arth.2010.05.005. Sep; [DOI] [PubMed] [Google Scholar]
- 11.Agarwala S, Banavali SD, Vijayvargiya M. Bisphosphonate Combination Therapy in the Management of Postchemotherapy Avascular Necrosis of the Femoral Head in Adolescents and Young Adults: A Retrospective Study From India. J Glob Oncol. 2018;4:1–11. doi: 10.1200/JGO.17.00083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Padhye B, Dalla-Pozza L, Little DG, Munns CF. Use of zoledronic acid for treatment of chemotherapy related osteonecrosis in children and adolescents: a retrospective analysis. Pediatr Blood Cancer. 2013;60(9):1539–45. doi: 10.1002/pbc.24563. [DOI] [PubMed] [Google Scholar]
- 13.Arbeloa-Gutierrez L, Dean CS, Chahla J, Pascu-al-Garrido C. Core Decompression Augmented With Autologous Bone Marrow Aspiration Concentrate for Early Avascular Necrosis of the Femoral Head. Arthrosc Tech. 2016;5(3):e615–20. doi: 10.1016/j.eats.2016.02.009. Jun 13; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pilge H, Bittersohl B, Schneppendahl J, Hesper T, Zilkens C, Ruppert M, Krauspe R, Jäger M. Bone Marrow Aspirate Concentrate in Combination With Intravenous Iloprost Increases Bone Healing in Patients With Avascular Necrosis of the Femoral Head: A Matched Pair Analysis. Orthop Rev (Pavia). 2017;8(4):6902. doi: 10.4081/or.2016.6902. Jan 4; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Waewsawangwong W, Ruchiwit P, Huddleston JI, Goodman SB. Hip arthroplasty for treatment of advanced osteonecrosis: comprehensive review of implant options, outcomes and complications. Orthop Res Rev. 2016;8:13–29. doi: 10.2147/ORR.S35547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karimova EJ, Rai SN, Howard SC, Neel M, Britton L, Pui CH, et al. Femoral head osteonecrosis in pediatric and young adult patients with leukemia or lymphoma. J Clin Oncol. 2007;25(12):1525–31. doi: 10.1200/JCO.2006.07.9947. [DOI] [PubMed] [Google Scholar]
- 17.Andronic O, Weiss O, Shoman H, Kriechling P, Khanduja V. What are the outcomes of core decompression without augmentation in patients with nontraumatic osteonecrosis of the femoral head? Int Orthop. 2021;45(3):605–613. doi: 10.1007/s00264-020-04790-9. Mar; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smucny M, Parikh SN, Pandya NK. Consequences of single sport specialization in the pediatric and adolescent athlete. Orthop Clin North Am. 2015;46(2):249–58. doi: 10.1016/j.ocl.2014.11.004. Apr; [DOI] [PubMed] [Google Scholar]
- 19.Brenner JS. COUNCIL ON SPORTS MEDICINE AND FITNESS. Sports Specialization and Intensive Training in Young Athletes. Pediatrics. 2016;138(3):e20162148. doi: 10.1542/peds.2016-2148. Sep; [DOI] [PubMed] [Google Scholar]
- 20.Matthews AH, Davis DD, Fish MJ, et al. StatPearls. Treasure Island (FL): StatPearls Publishing; Avascular Necrosis. updated 2021. Oct 9. [PubMed] [Google Scholar]
- 21.Mattano LA, Devidas M, Nachman JB, Sather HN, Hunger SP, Steinherz PG, et al. Effect of alternate-week versus continuous dexamethasone scheduling on the risk of osteonecrosis in paediatric patients with acute lymphoblastic leukaemia: results from the CCG-1961 randomised cohort trial. Lancet Oncol. 2012;13(9):906–15. doi: 10.1016/S1470-2045(12)70274-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Padhye B, Dalla-Pozza L, Little D, Munns C. Incidence and outcome of osteonecrosis in children and adolescents after intensive therapy for acute lymphoblastic leukemia (ALL). Cancer Med. 2016;5(5):960–7. doi: 10.1002/cam4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rao SS, El Abiad JM, Puvanesarajah V, Levin AS, Jones LC, Morris CD. Osteonecrosis in pediatric cancer survivors: Epidemiology, risk factors, and treatment. Surg Oncol. 2019;28:214–221. doi: 10.1016/j.suronc.2019.02.001. Mar; [DOI] [PubMed] [Google Scholar]
- 24.Shaw KA, Mottern E, Parada S, Burks R, Dumont G, et al. Low Rate of Return to Impact Activity Following Core Decompression for Femoral Head AVN in Military Servicemembers, Military Medicine. 2019;184(1-2) doi: 10.1093/milmed/usy163. Jan; [DOI] [PubMed] [Google Scholar]
- 25.Shah SN, Kapoor CS, Jhaveri MR, Golwala PP, Patel S. Analysis of outcome of avascular necrosis of femoral head treated by core decompression and bone grafting. J Clin Orthop Trauma. 2015;6(3):160166. doi: 10.1016/j.jcot.2015.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stone S, Lee B, Garrison JC, Blueitt D, Creed K. Sex Differences in Time to Return-to-Play Progression After Sport-Related Concussion. Sports Health. 2017;9(1):41–4. doi: 10.1177/1941738116672184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chand MR, Kanwar S, Calvo C, Peck E. Influence of Sex and Previous Concussion History on Postconcussive Recovery in Young Athletes. Clin J Sport Med. 2020;1(30 Suppl):S36–S41. doi: 10.1097/JSM.0000000000000554. Mar; [DOI] [PubMed] [Google Scholar]
- 28.Tan SH, Lau BP, Khin LW, Lingaraj K. The Importance of Patient Sex in the Outcomes of Anterior Cruciate Ligament Reconstructions: A Systematic Review and Meta-analysis. Am J Sports Med. 2016;44(1):242–54. doi: 10.1177/0363546515573008. [DOI] [PubMed] [Google Scholar]


