Abstract
Purpose
To compare the axial plane orientation and width and length of the acromial resections required to reduce the critical shoulder angle (CSA) using lateral acromioplasty (LA) techniques that are based on the lateral acromial border with an ideal resection that is oriented parallel to the glenoid.
Methods
This was a retrospective observational cohort study of symptomatic patients that were investigated for shoulder pain, instability, or fracture with high-quality computed tomography (CT). The CT scan data were used to create 3-dimensional meshes, and a series of LA resection planes were mapped. The orientation, width, and length of each resection based on the lateral acromial border (lateral, anterolateral, posterolateral, and image guided) to reduce the measured CSA to 35° or 30° was compared with an ideal resection that was oriented parallel to the glenoid.
Results
23 models had CSA 30.1° to 35°, and 13 had CSA >35°. In the models with CSA >35°, there was no angular difference between the resection planes of the lateral, anterolateral, or image-guided resections compared with the ideal technique; there were differences in the required width and length of the resections to reduce the CSA to 35° (additional width/length: lateral, 3.2/14.8 mm; anterolateral, 2.8/10.6 mm; posterolateral, 6.9/19.2 mm; image guided, 2.4/10.3 mm). Width and length differences were also present in the models with CSA >30° when the resections aimed to reduce the CSA to 30° (additional width/length: lateral, 2.5/12.5 mm; anterolateral, 1.9/8.8 mm; posterolateral, 7.4/19.0 mm; image guided, 1.6/8.8 mm).
Conclusions
LA techniques based on the lateral acromial border did not replicate the ideal resection and may lead to excessive deltoid release which could adversely affect clinical results.
Clinical relevance
Our findings do not support LA techniques based on the lateral acromial border.
The critical shoulder angle (CSA) measured on a true anteroposterior radiograph of the shoulder is the angle between a line connecting the superior and inferior aspects of the glenoid fossa and another line connecting the inferior aspect of the glenoid with the most inferolateral point on the acromion.1 The acromial side of the angular measurement is defined by the most lateral part of the acromion on the radiograph. This has been termed the critical acromial point (CAP) and is located 21% ± 10% of the acromial anterior-posterior length from its anterolateral corner.2
Measurement of the CSA is affected by scapular rotation.3 The use of only well-oriented images results in an 89% likelihood that the measured CSA is <2° from the true CSA.3 Suter et al.3 classified the radiographic image quality used for CSA measurement according to the degree of overlap of the anterior and posterior glenoid rims (Fig 1). In an A1 image, there is no glenoid double contour, and there is overlap of the coracoid process and the upper glenoid rim (Fig 1).
Fig 1.
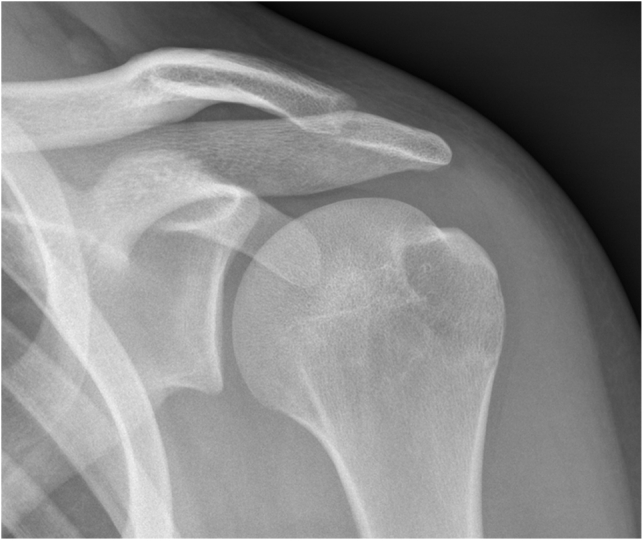
Suter-Henninger A1 type anteroposterior radiograph of a left shoulder characterized by no glenoid double contour and overlap of the coracoid process and the upper glenoid rim.3
The normal CSA range is 30° to 35°, with values >35° linked to the development of full-thickness rotator cuff (RC) tears.1,4 Biomechanical analyses have demonstrated that an increase in the CSA increases the vertical force vector of the deltoid muscle during arm abduction. This results in a greater shear force acting at the glenohumeral joint. To maintain stability, a greater compressive force is required from the rotator cuff.5,6 It is hypothesized that chronic overload and overuse of the supraspinatus could then predispose to an RC tear.7
A lateral acromioplasty (LA) aiming to remove the most lateral part of the acromion has been proposed to reduce high CSA, thereby reducing the vertical component of the deltoid force vector.2,8, 9, 10, 11 This contrasts with anterolateral or anterior acromioplasty, in which the aim is to reduce impingement. The middle deltoid originates from the entire vertical extent of the lateral wall of the acromion.12 An LA may therefore release the middle deltoid origin with the potential for weakness or deltoid dehiscence.
The ideal target CSA for the LA is not known. The axial orientation of the LA is also incompletely described. Given that the aim of a lateral resection is to reduce the 2-dimensional (2D) measurement of the CSA, the plane of the resection should be dictated by the glenoid plane. However, it is not possible to reference the glenoid plane while viewing from the subacromial space at the time of arthroscopy unless there is a massive RC tear. Therefore, authors have described an LA that uses an undersurface view of the acromion as a reference for the resection. Typically, the stated aim is to resect the entire lateral border of the acromion of a fixed width extending from the anterolateral corner of the acromion to the posterolateral corner.2,8, 9, 10 The orientation of this resection is therefore dictated by the lateral border of the acromion rather than the glenoid plane. This would be a precise technique if the lateral border of the acromion were parallel to the glenoid plane and the lateral border of the acromion were straight. However, the lateral border is not parallel to the glenoid face in patients with RC tears, in whom the axial tilt of the acromion relative to the glenoid is 36.4° (range 8° to 54°; standard deviation [SD] 9.4°).13 Also, the lateral border of the acromion is not straight in patients with RC tears.13 As a result, it would likely be difficult to identify the anterolateral and posterolateral corners of the acromion. Therefore, the shape and orientation of the acromion may render the described techniques for LA imprecise and lead to excessive resection of bone, thereby jeopardizing more deltoid fibers than required.
The ideal LA would diminish the CSA to the normal range, thereby reducing the vertical component of the deltoid force vector while minimizing the additional risk to the deltoid origin by resecting the minimal amount of bone. This would necessitate a resection parallel to the glenoid in the axial orientation. The amount of bone resection would also depend on whether the aim was to change the CSA to the upper or lower end of the normal range. The extent to which the currently described technique replicates the ideal resection has not been established.
The purpose of this study was to compare axial plane orientation and required width and length of the resultant acromial resections required to reduce the CSA using LA techniques that are based on the lateral acromial border with an ideal resection that is oriented parallel to the glenoid. The hypothesis was that there was no difference in the orientation or the required width and length of the acromial resections required compared with an ideal resection that is oriented parallel to the glenoid.
Methods
Ethics approval was obtained from the University of New South Wales Human Research Ethics Committee (HC180247). This was a retrospective observational cohort study of a diagnostic test. The clinical records of a single surgeon (G.S.) were searched over a 6-year period (January 2013 to September 2018) for those patients who underwent computed tomography (CT) scan of the shoulder. CT was performed routinely for all patients undergoing arthroplasty (anatomic and reverse), glenohumeral instability, and some fractures during the study period. Exclusion criteria were insufficient resolution (slice thickness >1 mm); gross glenoid or acromial deformity (e.g., fracture, bone loss); artifact (beam hardening, CT arthrography); or incomplete capturing of the entire scapula. The digital imaging and communications in medicine (DICOM) data from the included CT scans were imported into InVesalius (version 3.1.1, Renato Archer Information Technology Centre, Brazil), which was used to segment bone from the CT raw data and to create 3D meshes. The meshes were then imported into Meshmixer (3.4.35, Autodesk, San Rafael, CA) for cleaning and analysis. All angular measurements were acquired using the software’s orthographic view, eliminating any angular distortion that would otherwise arise from changes in perspective. The viewing perspective or a plane can be marked with a visible grid. The grid can then be used as a reference to orient the mesh, because when the mesh is viewed perpendicularly to a grid, it will appear as a line. A viewing perspective can also be saved to allow future reorientation of the mesh to the same position.
The mesh was first oriented into the Suter-Henninger (S-H) A1 view,3 and the CSA was measured as originally described.1 The viewing perspective was marked with a grid. This grid was therefore oriented in the glenoid plane (glenoid plane grid). A series of LA resection planes were then mapped by a specialist fellowship-trained shoulder surgeon (G.S.). The coronal orientation of all the resections was perpendicular to the undersurface of the acromion. The axial orientation of the resection varied according to the technique.
Ideal Resection
The mesh was initially viewed in the S-H A1 position. The glenoid plane grid was tilted while keeping the grid fixed at the inferior-most point of the glenoid so that it intersected the undersurface of the acromion (Fig 2). The mesh was reoriented until the view was perpendicular to the undersurface of the acromion (Fig 3). The orientation of the ideal resection was defined by the tilted glenoid plane grid after the mesh was reoriented (Fig 3).
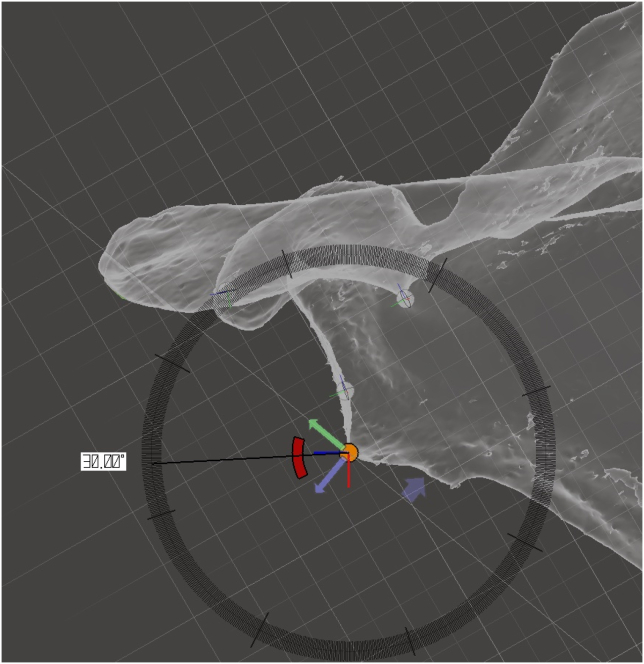
Fig 2.
The right shoulder 3D mesh has been oriented in the Suter-Henninger A1 (S-H A1) view.3 The glenoid plane grid has been tilted while keeping the grid fixed at the inferior-most point of the glenoid so that the grid intersects the undersurface of the acromion (in this case at an angle of 30°).
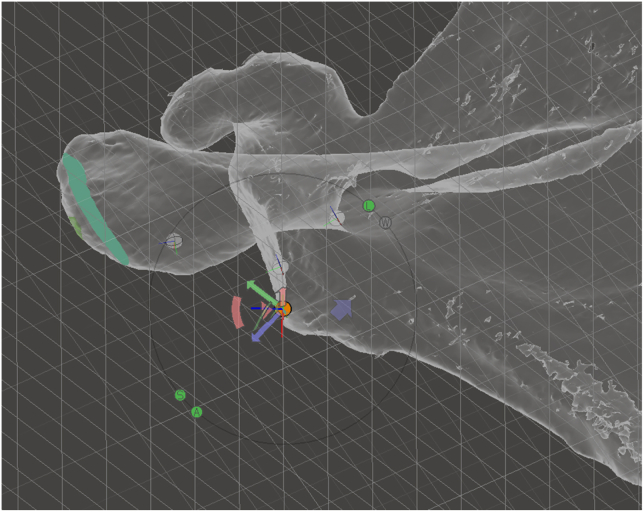
Fig 3.
The right shoulder 3D mesh has been reoriented perpendicular to the undersurface of the acromion. The original glenoid plane grid and the tilted glenoid plane grid are visible. In this transparent view of the 3D mesh, the ideal resection (green area) appears broad, as the resection plane is displayed though the entire thickness of the acromion.
Resections Based on the Lateral Acromial Border
The lateral border of the acromion was used to define the orientation of 3 other resections. The mesh remained oriented perpendicular to the undersurface of the acromion (Fig 4), and resection planes were inserted parallel to this viewing plane.
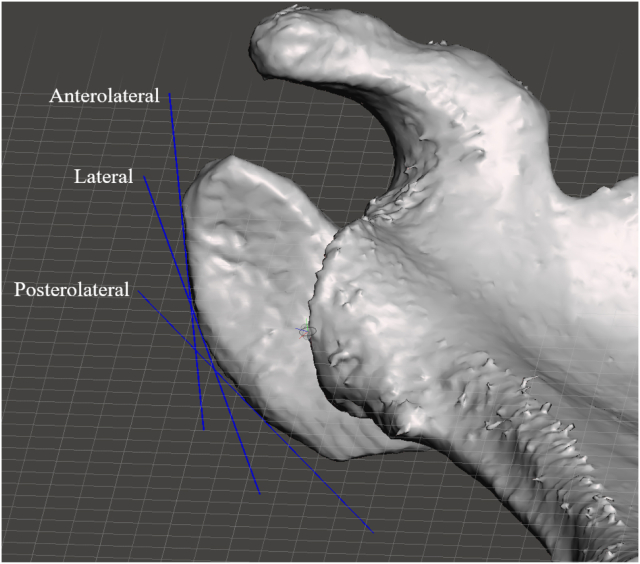
Fig 4.
The right shoulder 3D mesh has been oriented perpendicular to the undersurface of the acromion. The mesh has been rendered opaque. The lines of best fit for the anterolateral, lateral, and posterolateral acromial-based resections have been superimposed on the image.
Entire lateral border resection (lateral): The orientation of the resection plane was parallel to the lateral border of the acromion using a line of best fit (LOBF) of the entire lateral border of the acromion (Fig 4). Anterolateral lateral border resection (anterolateral): The orientation of the resection plane was parallel to the anterior half of the lateral border of the acromion in a similar way to the entire lateral border resection (Fig 4). Posterolateral lateral border resection (posterolateral): The orientation of the resection plane was parallel to the posterior half of the lateral border of the acromion in a similar way to the entire lateral border resection (Fig 4). Image-guided lateral border resection (image guided): The mesh was viewed perpendicular to the undersurface of the acromion. Subsequently, the CAP was estimated as being either in the anterior, middle, or posterior third of the lateral acromial border by 1 of the investigators (G.S.) on 2 occasions, 1 month apart. Subsequently either the anterolateral, lateral or posterolateral lateral border resections were assigned to that model.
Only those cases in which the measured CSA was >30° were included. The resections that reduced the measured CSA to 35° (if the initial CSA was >35°) or to 30° (if the measured CSA was >30°) were mapped. The length and width of the bone requiring resection to reduce the CSA to 35° and 30° were measured. The angle between the orientation of the ideal cut and the resections based on the lateral acromial border were also measured while viewing perpendicular to the undersurface of the acromion (Fig 5).
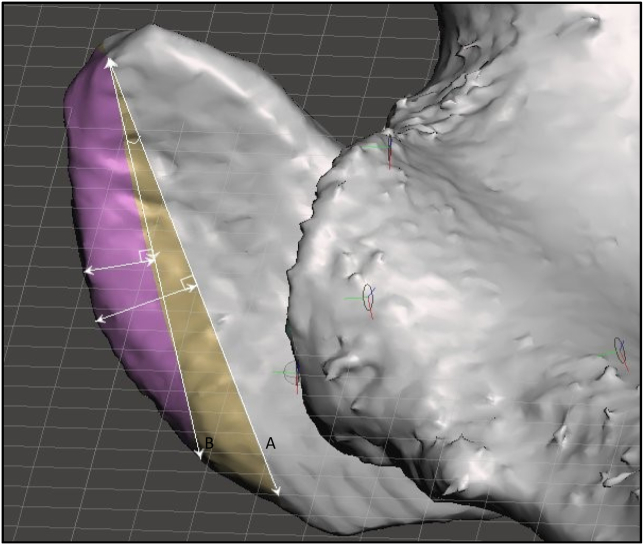
Fig 5.
The right shoulder 3D mesh has been oriented perpendicular to the undersurface of the acromion. The entire lateral border (A) and ideal resection (B) planes have been superimposed on the image. The axial angular difference angle between 2 resection planes, as well as the width and length of both the resections, are measured.
Statistical analysis was conducted using SPSS (IBM SPSS Statistics for Windows, version 26.0; IBM Corp., Armonk, NY). Data were tested for normality using the Kolmogorov-Smirnov test. Normally distributed data are expressed using means and standard deviation (SD). Angular differences between the ideal resection and the other techniques were calculated and comparisons performed with paired t tests. Two comparisons were made: models with CSA >35° and models with CSA >30°. Pearson’s correlation coefficient was used to assess the relationship between CSA value and the angular difference between the ideal resection and the other methods. Comparisons of the mean length and width of the ideal resection to the other techniques were carried out with paired t tests. Two comparisons were made: models with CSA >35° reducing the CSA to 35° and models with CSA >30° reducing the CSA to 30°.
Results
After initial exclusion, there were 53 CT scans. The mean CSA was 32.8° (SD 4.7°). 17 cases had a CSA ≤30° and were excluded. The study group consisted of 23 models (23 patients) with a CSA of 30.1° to 35° and 13 with a CSA >35°. The demographic data of the patients and their diagnoses are presented in Table 1.
Table 1.
Demographic details and diagnoses of the patients in the study
| Characteristic | CSA >30° to 35° (n = 23) | CSA >35° (n = 13) |
|---|---|---|
| Age (y) | 54.6 (21.7) | 59.2 (14.2) |
| Gender | ||
| M:F | 13:10 | 6:7 |
| % male | 56.5 | 46.2 |
| Side | ||
| Right:left | 13:10 | 7:6 |
| % right | 56.5 | 53.8 |
| Diagnosis | ||
| Glenohumeral instability | 8 (34.8) | 2 (15.4) |
| Fracture | 7 (30.4) | 9 (69.2) |
| Glenohumeral osteoarthritis | 7 (30.4) | 1 (7.7) |
| Rotator cuff arthropathy | 1 (4.3) | 1 (7.7) |
Data are mean (standard deviation) or n (%).
Abbreviation: CSA, critical shoulder angle.
There were no discrepancies between each of the allocations of the perceived best image-guided resection technique. 33 models were allocated to the anterolateral resection and 3 to the lateral resection. The mean width and length of the resections required to reduce the CSA using the ideal orientation are shown in Table 2. The mean angular differences between the resection planes of each of the techniques and the ideal resection plane are shown in Table 3 (angular difference of ideal compared to lateral, anterolateral, posterolateral, and image guided). The results of the assessment of the correlation between CSA value and the angular difference between the ideal resection and the other methods are shown in Table 4. Results of the assessment of the width and length of the acromial resections and the pairwise comparisons of the techniques are shown in Tables 5 and 6.
Table 2.
Mean width and length of the lateral acromial resections required to reduce the CSA using the ideal orientation technique
| Angle | Width of Resection (mm) | Length of Resection (mm) |
|---|---|---|
| CSA>35° reducing CSA to 35° | 4.7 (2.2) | 27.1 (10.6) |
| CSA >30° reducing CSA to 30° | 5.5 (3.4) | 29.2 (11.2) |
Data are mean (standard deviation).
Abbreviation: CSA, critical shoulder angle.
Table 3.
Axial angular difference between the ideal resection plane and the resections based on the lateral acromial border for those models with CSA >35° and CSA >30°
| Angle | Axial angular Difference |
|||
|---|---|---|---|---|
| Lateral | Anterolateral | Posterolateral | Image Guided | |
| CSA >35° | ||||
| Ideal | 7.5 (17.5), P = .146 | –2.7 (13.6), P = .496 | 19.7 (17.3), P = .001 | –1.7 (13.1), P = .656 |
| CSA >30° | ||||
| Ideal | 8.6 (12.7), P < .001 | 0.5 (11.1), P = .805 | 21.7 (14.4), P < .001 | 0.5 (10.5), P = .792 |
Data are mean (standard deviation).
Abbreviation: CSA, critical shoulder angle.
Table 4.
Assessment of the correlation between CSA value and the axial angular difference between the ideal resection and the resections based on the lateral acromial border
| Resection Method | Pearson’s Correlation Coefficient |
|---|---|
| Lateral | –0.225, P = .168 |
| Anterolateral | –0.325, P = .044 |
| Posterolateral | –0.193, P = .238 |
| Image Guided | –0.294, P = .082 |
Abbreviation: CSA, critical shoulder angle.
Table 5.
Results and pairwise comparison of width and length of the acromial resections required to correct the CSA to 35° for those models with CSA >35° (n = 13) using the ideal resection and the resections based on the lateral acromial border
| Technique | Resection Width (mm) | Comparative Technique | Mean Difference (mm) | SEM | P | 95% Confidence Interval |
|---|---|---|---|---|---|---|
| Width | ||||||
| Ideal | 4.7 (2.2) | Lateral | –3.2 | 0.9 | .041 | –6.3 to –0.1 |
| Anterolateral | –2.8 | 0.6 | .006 | –4.8 to –0.7 | ||
| Posterolateral | –6.9 | 0.9 | <.001 | –9.9 to –3.9 | ||
| Image guided | –2.4 | 0.5 | .009 | –4.3 to –0.5 | ||
| Length | ||||||
| Ideal | 27.1 (10.6) | Lateral | –14.8 | 3.2 | .005 | –25.6 to –4.0 |
| Anterolateral | –10.6 | 3.0 | .040 | –20.8 to –0.4 | ||
| Posterolateral | –19.2 | 2.8 | <.001 | –28.7 to –9.6 | ||
| Image guided | -–10.3 | 3.0 | .050 | –20.6 to 0.0 |
Data for resection width and length are mean (standard deviation).
Abbreviation: CSA, critical shoulder angle; SEM, standard error of the mean.
Table 6.
Results and pairwise comparison of width and length of the acromial resections required to correct the CSA to 30° for those models with CSA >30° (n = 36) using the ideal resection and the resections based on the lateral acromial border
| Technique | Resection Width (mm) | Comparative Technique | Mean Difference (mm) | SEM | P | 95% Confidence Interval |
|---|---|---|---|---|---|---|
| Width | ||||||
| Ideal | 5.5 (3.4) | Lateral | –2.5 | 0.4 | <.001 | –3.7 to –1.2 |
| Anterolateral | –1.9 | 0.3 | <.001 | –2.8 to –0.9 | ||
| Posterolateral | –7.4 | 0.7 | <.001 | –9.4 to –5.4 | ||
| Image guided | –1.6 | 0.3 | <.001 | –2.4 to –0.8 | ||
| Length | ||||||
| Ideal | 29.2 (11.2) | Lateral | –12.5 | 1.6 | <.001 | –17.2 to –7.8 |
| Anterolateral | –8.8 | 1.8 | <.001 | –14.1 to –3.6 | ||
| Posterolateral | –19.0 | 1.6 | <.001 | –23.7 to –14.3 | ||
| Image guided | –8.8 | 1.7 | <.001 | –13.9 to –3.8 |
Data for resection width and length are mean (standard deviation).
Abbreviation: CSA, critical shoulder angle; SEM, standard error of the mean.
Discussion
The results of this study show that among scapulae with CSA >35°, there was no angular difference between the orientation of an ideal LA that aims to reduce the CSA (which necessitates that the plane of resection is based on the orientation of the glenoid) and the typically performed LA (entire lateral border resection). However, the standard deviation was high (17.5°), implying considerable variability in the shape and orientation of the lateral border of the acromion. A greater width and length of acromial resection was required to reduce the CSA to the upper end of the normal range using the entire lateral border resection compared with the ideal orientation, and these differences were clinically meaningful (additional width 3.2 mm, additional length 14.8 mm). The additional length and width of acromial resection mean that more of the deltoid origin would be released from the acromion than is necessary if the results are replicated in vivo. Therefore, alternative techniques that better replicate the ideal resection would be beneficial.
Three other potential techniques that were based on the lateral border of the acromion were evaluated in this study. The anterolateral technique reflects that the CAP is located on average 21% of AP length of the acromion posterior to its anterolateral corner.2 The posterolateral technique was included because, although the typical CAP location is anterolateral, it may range from 3% to 46% of AP length of the acromion posterior to its anterolateral corner.2 The image-guided resection technique aimed to replicate the surgeons’ selection of the orientation of the resection based on the location of the CAP on an axillary radiograph.
The results of this study demonstrated that in scapulae with CSA >35°, there is no angular difference between the orientation of an ideal LA and the anterolateral and image-guided resections. Again, this was subject to high SDs (anterolateral, 13.6°; image guided, 13.1°), and there were thus clinically relevant differences in the width and length of acromial resections (anterolateral, additional width 2.8 mm, additional length 10.6 mm; image guided, additional width 2.4 mm, additional length 10.3 mm). Given the typical location of the CAP, it is unsurprising that the posterolateral resection was angularly different from the ideal orientation and resulted in a greater required width and length of resection to reduce the CSA to 35°. As the models were allocated to the anterolateral resection in the majority of cases in the image-guided technique, the results are similar to the anterolateral technique, as would be expected.
The role of acromioplasty in the surgical treatment of subacromial impingement syndrome and rotator cuff tears is controversial. Anterolateral acromioplasty does not improve outcome after rotator cuff repair and does not lead to improved outcomes compared with nonoperative treatment of subacromial impingement syndrome.14, 15, 16 Although a high CSA value has been linked to a higher risk of retear after RC repair,17, 18, 19 there is no current evidence to demonstrate that an LA may diminish the risk of retear after RC repair. However, as the rationale for LA is based on cuff overload rather than mechanical impingement, the assumption that its results are likely to be equivalent to that of anterolateral acromioplasty may be erroneous. Further clinical studies are required to assess the role of LA.
The clinical relevance of this study is that none of the described or potential acromial-based lateral acromioplasty resection methods investigated in this study sufficiently replicate the ideal resection to recommend their routine use which may lead to excessive deltoid release which could adversely affect clinical results. Instead, the variability of the shape and orientation of the lateral acromion suggest that either a preoperative, patient-specific, CT-based plan of the orientation of the resection is required or an operative technique is used that enables referencing of the orientation of the glenoid rather than referencing the acromion. Further studies are required to assess whether a technique that closely replicates the ideal resection is possible. If an ideal orientation of the resection of the lateral acromial border is surgically possible, the commonly described 5-mm width seems appropriate to reduce the CSA to either the upper end of the normal range if the CSA is >35° (mean width of resection required using the ideal orientation is 4.7 mm) or to the lower end of the normal range if the CSA is >30° (mean width of resection required using the ideal orientation is 5.5 mm).
Given the results of this study, the technique of any LA should be adequately described in all future clinical outcome studies. The LA techniques in this study involved a vertical resection of the lateral wall of the acromion perpendicular to the undersurface of the acromion. A less aggressive obliquely oriented beveling of the inferior aspect of the lateral acromion is also described.9 This would reduce the CSA measurement, but from a biomechanical perspective it would only partially release the middle deltoid. As a result, the vertical component of the deltoid force vector would be only partially changed. In contrast, a vertical LA would theoretically modify the described biomechanical link between high CSA and RC tears. Additionally, the present study reflects the theory that the reduction of the 2D measurement of the CSA should be the aim of a 3D resection. Instead, it may be that other scapular morphological factors that result in variances in the CSA may be more relevant to the high-risk acromion for the development of RC tears than the CSA value per se.
Limitations
The main limitation of this study is that the study population was defined by the acquisition of high-quality CT images rather than including only those patients with rotator cuff tears in whom an LA might be considered. Furthermore, the integrity of the rotator cuff in the included patients was not assessed. This study population was used because CT-based models were required for mesh generation and subsequent accurate assessment of the resections. Additionally, only 13 patients had a CSA >35°. However, the results of this study were not different when comparing resections of all patients with CSA >30° (36 scapulae), in whom the aim was to reduce the CSA to 30°, and just those with CSA >35° (13 scapulae), in whom the aim was to reduce the CSA to 35°. Additionally, some patients with RC tears do not have a CSA >35°, and the target CSA for an LA technique is not known. Also, there was no correlation between the CSA and the axial angular difference of the resection planes for the lateral, posterolateral, and image-guided resection technique, and therefore assessment of all patients with a CSA above the lower end of the normal range may be justified. There was a correlation between CSA value and the axial angular difference between the anterolateral resection and the ideal resection, which may be explained by scapulae with a high CSA having an acromion that is more externally rotated in the axial plane.13 But, considering the other results of this study, the anterolateral resection was not notably different from the other acromial-based resection methods.
Conclusions
LA techniques based on the lateral acromial border did not replicate the ideal resection and may lead to excessive deltoid release, which could adversely affect clinical results.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Moor B.K., Bouaicha S., Rothenfluh D.A., Sukthankar A., Gerber C. Is there an association between the individual anatomy of the scapula and the development of rotator cuff tears or osteoarthritis of the glenohumeral joint? A radiological study of the critical shoulder angle. Bone Joint J. 2013;95-B:935–941. doi: 10.1302/0301-620X.95B7.31028. [DOI] [PubMed] [Google Scholar]
- 2.Karns M.R., Jacxsens M., Uffmann W.J., Todd D.C., Henninger H.B., Burks R.T. The critical acromial point: The anatomic location of the lateral acromion in the critical shoulder angle. J Shoulder Elbow Surg. 2018;27:151–159. doi: 10.1016/j.jse.2017.08.025. [DOI] [PubMed] [Google Scholar]
- 3.Suter T., Gerber Popp A., Zhang Y., Zhang C., Tashjian R.Z., Henninger H.B. The influence of radiographic viewing perspective and demographics on the critical shoulder angle. J Shoulder Elbow Surg. 2015;24:e149–158. doi: 10.1016/j.jse.2014.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith G.C.S., Liu V., Lam P.H. The critical shoulder angle shows a reciprocal change in magnitude when evaluating symptomatic full-thickness rotator cuff tears versus primary glenohumeral osteoarthritis as compared with control subjects: A systematic review and meta-analysis. Arthroscopy. 2020;36:566–575. doi: 10.1016/j.arthro.2019.09.024. [DOI] [PubMed] [Google Scholar]
- 5.Gerber C., Snedeker J.G., Baumgartner D., Viehofer A.F. Supraspinatus tendon load during abduction is dependent on the size of the critical shoulder angle: A biomechanical analysis. J Orthop Res. 2014;32:952–957. doi: 10.1002/jor.22621. [DOI] [PubMed] [Google Scholar]
- 6.Viehofer A.F., Gerber C., Favre P., Bachmann E., Snedeker J.G. A larger critical shoulder angle requires more rotator cuff activity to preserve joint stability. J Orthop Res. 2016;34:961–968. doi: 10.1002/jor.23104. [DOI] [PubMed] [Google Scholar]
- 7.Viehofer A.F., Snedeker J.G., Baumgartner D., Gerber C. Glenohumeral joint reaction forces increase with critical shoulder angles representative of osteoarthritis: A biomechanical analysis. J Orthop Res. 2016;34:1047–1052. doi: 10.1002/jor.23122. [DOI] [PubMed] [Google Scholar]
- 8.Gerber C., Catanzaro S., Betz M., Ernstbrunner L. Arthroscopic correction of the critical shoulder angle through lateral acromioplasty: A safe adjunct to rotator cuff repair. Arthroscopy. 2018;34:771–780. doi: 10.1016/j.arthro.2017.08.255. [DOI] [PubMed] [Google Scholar]
- 9.Katthagen J.C., Marchetti D.C., Tahal D.S., Turnbull T.L., Millett P.J. The effects of arthroscopic lateral acromioplasty on the critical shoulder angle and the anterolateral deltoid origin: An anatomic cadaveric study. Arthroscopy. 2016;32:569–575. doi: 10.1016/j.arthro.2015.12.019. [DOI] [PubMed] [Google Scholar]
- 10.Altintas B., Kaab M., Greiner S. Arthroscopic lateral acromion resection (ALAR) optimizes rotator cuff tear relevant scapula parameters. Arch Orthop Trauma Surg. 2016;136:799–804. doi: 10.1007/s00402-016-2431-y. [DOI] [PubMed] [Google Scholar]
- 11.Marchetti D.C., Katthagen J.C., Mikula J.D., et al. Impact of arthroscopic lateral acromioplasty on the mechanical and structural integrity of the lateral deltoid origin: A cadaveric study. Arthroscopy. 2017;33:511–517. doi: 10.1016/j.arthro.2016.08.015. [DOI] [PubMed] [Google Scholar]
- 12.Smith G.C.S., Liu V.K., Bonar S.F., Lam P.H. The lateral deltoid originates from the entire lateral wall of the acromion: MRI and histologic cadaveric analysis regarding vertical lateral acromioplasty. Arthrosc Sports Med Rehabil. 2020;2:e547–e552. doi: 10.1016/j.asmr.2020.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beeler S., Hasler A., Getzmann J., Weigelt L., Meyer D.C., Gerber C. Acromial roof in patients with concentric osteoarthritis and massive rotator cuff tears: Multiplanar analysis of 115 computed tomography scans. J Shoulder Elbow Surg. 2018;27:1866–1876. doi: 10.1016/j.jse.2018.03.014. [DOI] [PubMed] [Google Scholar]
- 14.Beard D.J., Rees J.L., Cook J.A., et al. Arthroscopic subacromial decompression for subacromial shoulder pain (CSAW): A multicentre, pragmatic, parallel group, placebo-controlled, three-group, randomised surgical trial. Lancet. 2018;391:329–338. doi: 10.1016/S0140-6736(17)32457-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Familiari F., Gonzalez-Zapata A., Ianno B., Galasso O., Gasparini G., McFarland E.G. Is acromioplasty necessary in the setting of full-thickness rotator cuff tears? A systematic review. J Orthop Traumatol. 2015;16:167–174. doi: 10.1007/s10195-015-0353-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paavola M., Malmivaara A., Taimela S., et al. Subacromial decompression versus diagnostic arthroscopy for shoulder impingement: Randomised, placebo surgery controlled clinical trial. BMJ. 2018;362 doi: 10.1136/bmj.k2860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garcia G.H., Liu J.N., Degen R.M., et al. Higher critical shoulder angle increases the risk of retear after rotator cuff repair. J Shoulder Elbow Surg. 2017;26:241–245. doi: 10.1016/j.jse.2016.07.009. [DOI] [PubMed] [Google Scholar]
- 18.Scheiderer B., Imhoff F.B., Johnson J.D., et al. Higher critical shoulder angle and acromion index are associated with increased retear risk after isolated supraspinatus tendon repair at short-term follow up. Arthroscopy. 2018;34:2748–2754. doi: 10.1016/j.arthro.2018.05.029. [DOI] [PubMed] [Google Scholar]
- 19.Sheean A.J., Sa D., Woolnough T., Cognetti D.J., Kay J., Burkhart S.S. Does an increased critical shoulder angle affect re-tear rates and clinical outcomes following primary rotator cuff repair? A systematic review. Arthroscopy. 2019;35:2938–2947. doi: 10.1016/j.arthro.2019.03.063. e2931. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.