Abstract
Purpose
To characterize the shoulder injuries experienced by baseball batters and position players (nonpitchers); to quantify the outcomes of these injuries with respect to time out of play, recurrence, and surgery rates; and to identify any injury patterns that are associated with worse outcomes.
Methods
Between 2011 and 2017, all Major League Baseball (MLB) and Minor League Baseball (MiLB) players who sustained shoulder injuries were identified using the MLB Health and Injury Tracking System (HITS). Injuries were included if they were sustained during baseball activity, resulted in at least 1 day missed (DM), and occurred in position players (nonpitchers).
Results
Over the study period, a total of 3,414 shoulder injuries occurred in batters, resulting in a sum of 68,808 DM and a mean of 22 DM per injury. Most injuries were a result of acute trauma (n = 2125; 62.2%) with throwing as the predominant activity (n = 1292; 38%). Rotator cuff strain/tears was the most common diagnosis (n = 790; 23.1%), and SLAP tears had the highest season-ending rate (35.3%) and need for surgery (45.1%). There was a lower frequency of surgery (6.2% vs 9.2%; P = .002) and reinjury (2.03% vs 3.62%; P = .007) in the throwing shoulder vs the nonthrowing shoulder. There was an increased frequency of surgery for the front versus the back batting shoulder (8.2% vs 6.2%; P = .031) with similar DM (20.7 vs 22.2; P = .333) and return to play rates (94.0% vs 92.2%; P = .135).
Conclusions
During the 7-season study period, there were a total of 3,414 shoulder injuries that resulted in nearly 70,000 days of out of play in professional baseball position players/batters (nonpitchers). Although pitchers were intentionally excluded from the analysis, throwing was still the most common mechanism of injury, and rotator cuff injuries were the most common injury. Labral tears were the most likely injury to be season ending and require surgery.
Clinical Relevance
This study is meant to help determine characteristics of shoulder injuries that occur in non-pitchers by focusing on professional baseball batters and position players. This information could be helpful to sports medicine practitioners and shoulder specialists to better prognosticate injury recovery.
Musculoskeletal injuries are a common problem for professional baseball players, where despite continued injury-prevention efforts, there has been no significant decline of events in recent years.1,2 A commonly reported injured body region is the shoulder.1,3,4 With regard to shoulder injuries in professional baseball players, they have historically been described as a result of overuse mechanisms secondary to overhead throwing.5 Anatomically, 6 (12%) of the top 50 most common injury diagnoses in professional baseball occur in the shoulder.1 Shoulder injuries have been reported to occur at greater rates in pitchers, with previous work demonstrating greater proportions of days missed and eventual surgery for pitchers as compared with position players.3,6 As a result, there has been a predominant focus on shoulder injuries in pitchers, whereas less is known about shoulder injuries in position players and batters.
One mechanism of injury specific to batters includes the “batter’s shoulder,” defined as posterior instability of the lead shoulder during a baseball swing. It is a relatively uncommon form of instability, but the injury mechanism is specific to the baseball batter. Fortunately, it has been demonstrated to have relatively high return to play (RTP) rates after arthroscopic management.7 Being hit by pitch is an additional pattern specific to batters that has been reported to result in a mean of 8.4 days missed per injury.8 More specifically, shoulder injuries ranked 11 of 18 among the various body regions, with shoulder contusions as the most common shoulder injury when hit by pitch. Similarly, previous data on the top 50 most common injuries in professional baseball found batting to be the most common injury activity at 19.7% followed by pitching at 19.3%, and fielding at 18%.1 However, there is still a lack of specific data examining shoulder injuries occurring in professional batting athletes. Given the high demands of the hitting motion and the stress placed on the shoulders during the swing, additional work is needed to better understand the epidemiology and impact of these injuries. Accordingly, the purpose of this study was to develop a deeper understanding of the injury risk conferred to the batter’s shoulder due to the unique forces and stresses it experiences during the batting motion. More specifically, we sought to characterize the shoulder injuries experienced by baseball position players/batters; to quantify the outcomes of these injuries with respect to time out of play, recurrence, and surgery rates; and to identify any injury patterns that are associated with worse outcomes. We hypothesized that injuries to batting athletes would be unique compared to those already described for pitchers, and that the type and severity of injuries would be different for the front and back batting shoulder.
Methods
This work was approved by our institutional review board (Mayo institutional review board #17-006455) and the Major League Baseball (MLB) Commissioner’s Office prior to beginning. Following approval, the MLB Health and Injury Tracking System (HITS) database was used to identify all shoulder injuries occurring in MLB and Minor League Baseball (MiLB) position players/batters (i.e., nonpitchers) during the 2011-2017 seasons. As previously mentioned, the HITS medical record database contains deidentified medical information of all professional baseball players (MLB and MiLB) recorded by official team athletic trainers.9
Injuries had to meet the following criteria to be included in the study: primary body region was shoulder, occurred during baseball activity (pre, regular, or postseason), player was primarily a position player (i.e., nonpitcher) or batter, resulted in at least 1 day out of play, and each player had to be active on an MLB or MiLB roster at the time of injury. Injuries were excluded if they resulted in less than 1 day out of play or did not occur during normal baseball activity. Season-ending injuries were defined as injuries that resulted in days missed (DM) beyond a baseball year. A baseball year was defined as the 4 consecutive sessions within a baseball season: spring training, regular season, postseason, and offseason.
The analysis consisted of a descriptive epidemiologic evaluation over a multitude of characteristics. Player specific variables included: age, level of play (MLB or MiLB), position, and hand dominance with respect to batting and throwing. Injury specific variables included: injury date, laterality (right or left), diagnosis, acuity of injury (acute or overuse), injury mechanism, subsequent surgical requirement, days missed, RTP to any level, and RTP at the same level. Batter’s shoulder was defined as posterior instability injury of the lead shoulder resulting from a baseball swing.7 If a batter experienced posterior instability by another mechanism (sliding, diving, collision, etc.), it was not considered to meet criteria as a batter’s shoulder. Comparisons of the front and back batting shoulder included athletes with clear determination of their dominant batting shoulder that were not switch hitters. DM away from play was defined as the time between the date of injury to the date of medical clearance for return to play. In the days missed analysis, athletes without a definitive medical clearance date or time greater than 1 full baseball year cycle were excluded. Reinjuries also were included and were defined as events where the same injury occurred at least once prior.
Statistical Analysis
Statistical analysis was performed with JMP Pro (v14.1.0; SAS Institute, Cary, NC). Descriptive statistics were used to report epidemiologic data: numbers, frequencies, percentages, means, medians, ranges, and standard deviations where appropriate. Specifically, these were used to generate an overview of shoulder injuries with respect to timing, specific diagnoses, and outcomes. Two-sample proportion statistical tests were performed between means of normally distributed variables. Wilcoxon signed rank analysis was used to compare means of continuous variables, and the Fisher exact test and χ2 test were used to compare nominal variables, when appropriate. This led to comparisons between injury mechanisms, involved shoulders, and professional level of play. Linear regression modeling was used to assess data trends over time, and were reported with their respective R2 and P values. Statistical significance was defined as a P value of ≤.05.
Results
Overview of Shoulder Injuries in Baseball Position Players/Batters
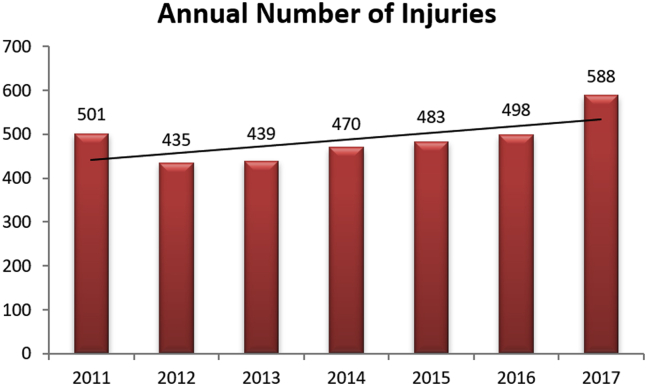
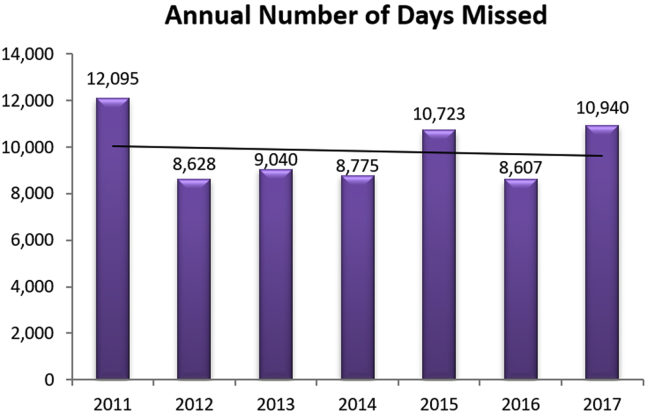
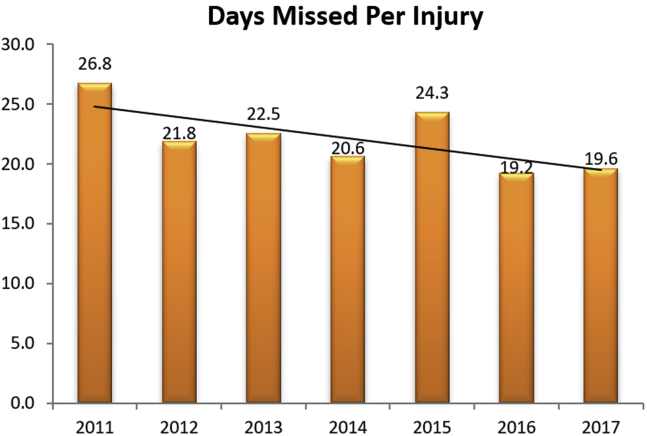
Over the 7-season study period (2011-2017) a total of 3,414 shoulder injuries occurred in professional batters. Of these, 483 (14.1%) occurred in MLB players and 2,931 (85.9%) occurred in MiLB players. A majority of injuries occurred during live game action (n = 2028; 59%) throughout the season (n = 2637; 77%). The annual number of injuries from 2011 to 2017 was relatively steady (R2 = 0.42, P = .116), ranging from a low of 435 in 2012 to a high of 588 in 2017 (Fig 1). A total of 3,121 of these shoulder injuries were non–season-ending injuries, with a cumulative total of 68,808 DM over the study period, and these did not significantly change over time (R2 = 0.01, P = .836) (Fig 2). The mean number of DM per injury was 22.0 with a median of 6 days, which also remained fairly steady during the study period (R2 = 0.003, P = .10) (Fig 3).
Fig 1.
The annual number of shoulder injuries in professional baseball batters remained steady over the course of the study (R2 = 0.42, P = .116).
Fig 2.
The annual number of days missed due to injury did not change significantly in Major League Baseball and Minor League Baseball players from 2011 to 2017 (R2 = 0.01, P = .836).
Fig 3.
Professional baseball players averaged 22.0 days missed per injury (median = 6 days), and this remained relatively steady during the course of the study (R2 = 0.003, P = .109).
Table 1 provides an overview of the player’s demographics and injury characteristics. For this cohort, the mean age for an MLB player was 28.9 ± 3.8 years and 22.0 ± 3.1 years for MiLB players (P < .001). Infielders were most often affected, with 1,463 (43%) injuries. Most of the athletes were right-handed throwers (n = 3036; 89%) and batters (n = 2059; 60%), with a predominance of injuries occurring on the players throwing (n = 2215; 65%) and back batting shoulder (n = 1723; 57%). Acute trauma was responsible for 2125 (62.2%) injuries. Throwing (n = 1292; 38%) was the predominant activity leading to injury, followed by fielding (n = 882; 26%) and batting (n = 618; 18%). Table 2 provides a more in-depth injury analysis, focusing on mechanisms, and activities at the time of injury.
Table 1.
Basic Characteristics and Demographics of Major League Baseball (MLB) and Minor League Baseball (MiLB) Batters Who Sustained Shoulder Injuries During the Study Period
| MLB | MiLB | Total (%) | |
|---|---|---|---|
| Throwing dominance | |||
| Right | 419 (86.7%) | 2617 (89.3%) | 3036 (88.9%) |
| Left | 64 (13.3%) | 309 (10.5%) | 373 (10.9%) |
| Both | 0 | 5 (0.2%) | 5 (0.2%) |
| Batting dominance | |||
| Right | 272 (56.3%) | 1787 (61.0%) | 2059 (60.3%) |
| Left | 154 (31.9%) | 786 (26.8%) | 940 (27.5%) |
| Both | 57 (11.8%) | 358 (12.2%) | 415 (12.2%) |
| Position | |||
| Catcher | 58 (12.0%) | 558 (19.0%) | 616 (18.0%) |
| Infielder | 213 (44.1%) | 1250 (42.6%) | 1463 (42.9%) |
| Outfielder | 208 (43.1%) | 1122 (38.3%) | 1330 (39.0%) |
| Designated hitter | 4 (0.8%) | 1 (0.03%) | 5 (0.1%) |
| Season | |||
| Preseason | 111 (23.0%) | 521 (17.8%) | 632 (18.5%) |
| Season | 358 (74.1%) | 2279 (77.8%) | 2637 (77.2%) |
| Postseason | 14 (2.9%) | 131 (4.5%) | 145 (4.3%) |
| Season-ending injury | |||
| Yes | 17 (10.2%) | 149 (9.0%) | 166 (5.0%) |
| No | 442 (14.2%) | 2679 (85.8%) | 3121 (95.0%) |
| Surgery required | |||
| Yes | 48 (9.9%) | 198 (6.8%) | 246 (7.2%) |
| No | 435 (90.1%) | 2733 (93.2%) | 3168 (92.8%) |
| Reinjury | |||
| Yes | 5 (1.0%) | 83 (2.8%) | 88 (2.6%) |
| No | 478 (99.0%) | 2848 (97.2%) | 3326 (97.4%) |
| Return to play (RTP) | |||
| Yes | 482 (99.8%) | 2676 (91.3%) | 3158 (92.5%) |
| No | 1 (0.2%) | 255 (8.7%) | 256 (7.5%) |
| Return to same level (RTSL) | |||
| Yes | 457 (94.6%) | 2601 (88.7%) | 3058 (91.8%) |
| No | 26 (5.4%) | 330 (11.3%) | 356 (10.4%) |
Table 2.
Injury Mechanisms, Activities, and On-Field Location in Professional Baseball Batters Sustaining Shoulder Injuries
| MLB | MiLB | Total (%) | |
|---|---|---|---|
| Timing of injury | |||
| Acute | 314 (65.0%) | 1811 (61.8%) | 2125 (62.2%) |
| Overuse | 115 (23.8%) | 776 (26.5%) | 891 (26.1%) |
| Unlisted | 54 (11.2%) | 344 (11.7%) | 398 (11.7%) |
| Injury mechanism | |||
| Noncontact | 224 (47.3%) | 1716 (59.5%) | 1940 (57.7%) |
| Contact with ground | 133 (28.1%) | 634 (22.0%) | 767 (22.8%) |
| Contact with ball | 30 (6.3%) | 222 (7.7%) | 252 (7.5%) |
| Contact with person | 31 (6.5%) | 121 (4.2%) | 152 (4.5%) |
| Contact with boundary | 37 (7.8%) | 63 (2.2%) | 100 (3.0%) |
| Contact with bat | 2 (0.4%) | 5 (0.2%) | 7 (0.21%) |
| Other | 17 (3.6%) | 125 (4.3%) | 142 (4.2%) |
| Injury activity | |||
| Throwing | 124 (26.2%) | 1168 (40.5%) | 1292 (38.4%) |
| Fielding | 188 (39.7%) | 696 (24.1%) | 884 (26.3%) |
| Batting | 88 (18.6%) | 530 (18.4%) | 618 (18.4%) |
| Sliding | 33 (7.0%) | 274 (9.5%) | 307 (9.1%) |
| Base running | 9 (1.9%) | 45 (1.6%) | 54 (1.6%) |
| Weight training/conditioning | 10 (2.1%) | 36 (1.2%) | 46 (1.4%) |
| Pitching | 0 (0%) | 21 (0.7%) | 21 (0.63%) |
| Other | 22 (4.6%) | 116 (4.0%) | 138 (4.1%) |
| Injury location on field | |||
| Home plate area | 112 (23.6%) | 760 (26.3%) | 872 (25.9%) |
| Middle infield area | 61 (12.9%) | 433 (15.0%) | 494 (14.7%) |
| Left field | 55 (11.6%) | 234 (8.1%) | 289 (8.6%) |
| Center field | 57 (12.0%) | 217 (7.5%) | 274 (8.1%) |
| Right field | 38 (8.0%) | 230 (8.0%) | 268 (8.0%) |
| First base | 35 (7.4%) | 194 (6.7%) | 229 (6.8%) |
| Third base | 39 (8.2%) | 172 (6.0%) | 211 (6.3%) |
| Foul territory | 6 (1.3%) | 96 (3.3%) | 102 (3.0%) |
| Pitcher's mound | 0 (%) | 18 (0.6%) | 18 (0.54%) |
| Other: outfield | 6 (1.3%) | 61 (2.1%) | 67 (2.0%) |
| Other: infield | 6 (1.3%) | 28 (1.0%) | 34 (1.0%) |
| Other | 55 (11.6%) | 408 (14.1%) | 463 (13.8%) |
MiLB, Minor League Baseball; MLB, Major League Baseball.
Characterization of Injury Diagnoses and Outcomes
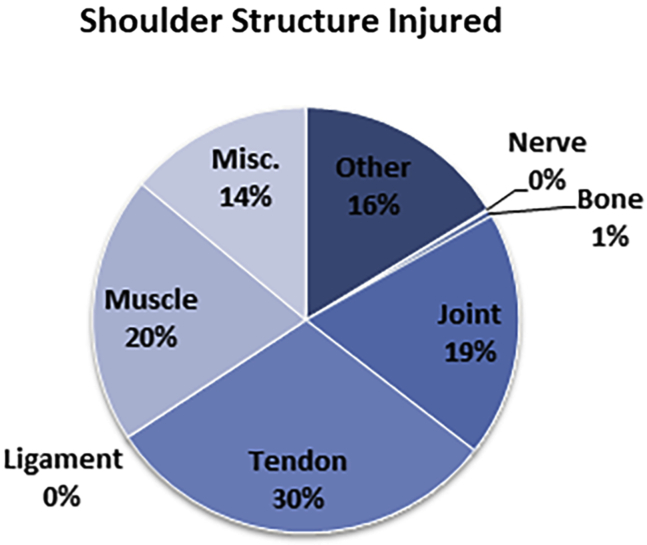
A detailed breakdown of injury types by structure is provided in Figure 4, with tendons as the most common injured structure (n = 1032, 30%) followed by muscle (n = 693, 20%) and joints (n = 637, 19%) (Table 3). When focusing on injuries affecting at least 10 players, SLAP tears had the highest season-ending rate (35.3%) and need for surgical intervention (45.1%) (Table 3). Second in this category was anterior instability with labral tear with a season-ending rate of 23.8% and a surgical frequency of 28.5%. Third was multidirectional instability, with a season-ending rate of 12.2% and a surgical frequency of 14.6%. Fourth was batter’s shoulder (posterior instability of the lead shoulder) with a 15.4% season-ending rate and 15.4% of injuries needing surgical intervention. Fifth was posterior instability with an 11.8% season-ending rate and 13.2% rate for surgical intervention. With respect to recurrence rates, multidirectional instability (12.2%), SLAP tears (10.8%), anterior instability with labral tear (9.4%), and posterior instability (7.4%) had the highest frequencies, with an associated mean DM of 17.8 ± 32.6, 85.4 ± 85.1, 52.3 ± 69.4, and 35.3 ± 57.3 days, respectively.
Fig 4.
A subclassification of injuries based on the shoulder structure in professional baseball batters.
Table 3.
All Shoulder Injury Diagnoses in Professional Baseball Batters
| Diagnosis | N | % | Age | Total DM∗ | Mean DM∗ | SD | Min | Max | Med | % Requiring Surgery | % Season Ending | % Recurrent | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Rotator cuff Injury | 790 | 23.1% | 23.1 | 13,650 | 18.5 | 35.9 | 1 | 325 | 6 | 4.3% | 6.7% | 1.5% |
| 2 | Other shoulder injury | 553 | 16.2% | 22.4 | 11,175 | 22.2 | 41.9 | 1 | 342 | 7 | 4.9% | 8.9% | 1.8% |
| 3 | Impingement/SA bursitis | 492 | 14.4% | 22.9 | 11,039 | 24.4 | 48.3 | 1 | 319 | 7 | 4.7% | 7.9% | 2.8% |
| 4 | Contusion - shoulder | 477 | 14.0% | 23.9 | 3,590 | 7.6 | 21.9 | 1 | 267 | 2 | 1.0% | 1.5% | 0.2% |
| 5 | LHBT injury | 304 | 8.9% | 21.9 | 4,904 | 17.2 | 33.4 | 1 | 317 | 7 | 3.0% | 6.3% | 2.0% |
| 6 | Anterior instability with labral tear | 235 | 6.9% | 22.4 | 9,466 | 52.3 | 69.4 | 1 | 320 | 23 | 28.5% | 23.8% | 9.4% |
| 7 | AC joint sprain | 155 | 4.5% | 25.1 | 3,282 | 22.5 | 35.7 | 1 | 320 | 12 | 2.6% | 5.8% | 0.0% |
| 8 | SLAP tear | 102 | 3.0% | 22.9 | 5,637 | 85.4 | 85.1 | 1 | 350 | 45.5 | 45.1% | 35.3% | 10.8% |
| 9 | Deltoid strain | 71 | 2.1% | 21.3 | 974 | 13.9 | 30.0 | 1 | 159 | 4 | 4.2% | 1.4% | 2.8% |
| 10 | Posterior instability | 68 | 2.0% | 22.4 | 2,118 | 35.3 | 57.3 | 1 | 242 | 13 | 13.2% | 11.8% | 7.4% |
| 11 | MDI | 41 | 1.2% | 23.1 | 640 | 17.8 | 32.6 | 1 | 167 | 6 | 14.6% | 12.2% | 12.2% |
| 12 | Pectoralis injury | 34 | 1.0% | 21.7 | 254 | 7.9 | 11.1 | 1 | 42 | 3 | 5.9% | 5.9% | 0.0% |
| 13 | Rhomboid strain | 34 | 1.0% | 24.0 | 488 | 14.4 | 28.9 | 1 | 157 | 4.5 | 0.0% | 0.0% | 0.0% |
| 14 | Batter’s shoulder | 13 | 0.4% | 19.5 | 577 | 44.4 | 61.7 | 3 | 204 | 18 | 15.4% | 15.4% | 7.7% |
| 15 | SC joint sprain | 13 | 0.4% | 24.8 | 260 | 21.7 | 34.7 | 1 | 125 | 10.5 | 0.0% | 7.7% | 0.0% |
| 16 | Scapulothoracic dysfunction | 11 | 0.3% | 23.7 | 186 | 18.6 | 15.3 | 1 | 46 | 21 | 0.0% | 9.1% | 0.0% |
AC, acromioclavicular; DM, day(s) missed; LHBT, long head biceps tendon; Max, maximum; MDI, multidirectional instability; Med, median; Min, minimum; SA, subacromial; SC, sternoclavicular; SD, standard deviation.
Days missed calculations do not include season-ending injuries.
Factors of Shoulder Injuries That Predict Outcomes
Table 4 contains subanalysis data for select shoulder injury factors (level of play, batting mechanism, batting shoulder, and throwing shoulder) with respective outcomes of number of injuries, days missed, frequency of surgery, and reinjury rates. In comparison of MLB versus MiLB players; MLB batters experienced a minority of the injuries (14.1%) and had a lower injury recurrence (1.0% vs 2.8%; P = .019) but had an increased frequency of surgery (9.9% vs 6.8%; P = .016) and mean days missed compared with MiLB batters (25.8 vs 21.7 days; P = .044). Focusing on injuries secondary to a throwing mechanism only, rotator cuff injuries were the most common (n = 428, 33.1%). For the throwing shoulder versus nonthrowing shoulder, a majority of these injuries occurred in the throwing shoulder (n = 2215, 65.1%) relative to the nonthrowing shoulder (n = 1188, 34.9%). Notably, there was a lower frequency of surgery (6.2% vs 9.2%; P = .002) and reinjury rate (2.03% vs 3.62%; P = .007) in the throwing shoulder of professional baseball batters. Focusing on injuries secondary to a batting mechanism only, rotator cuff injuries were the most common (n = 125, 20%). With respect to the front versus back batting shoulder, 42.4% of these injuries occurred on the front batting shoulder with 57.6% sustained in the back shoulder. There was an increased frequency of surgery for the front batting shoulder (8.2% vs 6.2%; P = .031).
Table 4.
Subanalyses of Various Shoulder Injury Factors and Outcomes (Days Missed, Surgery, and Reinjury Rate)
| Professional Level of Play | MLB | MiLB | P Value |
|---|---|---|---|
| Total no. of injuries (%) | 483 (14.1%) | 2,931 (85.9%) | |
| Total no. of days missed due to injury | 11,414 | 57,394 | |
| Mean (median) number of days missed per injury | 25.8 (4) | 21.4 (7) | .044 |
| No. of injuries requiring surgery (%) | 48 (9.9%) | 198 (6.8%) | .016 |
| Players who reinjured shoulder (%) | 5 (1.0%) | 83 (2.8%) | .019 |
| Return to play (%) | 482 (99.8%) | 2676 (91.3%) | < .001 |
| Return to same level of play (%) |
457 (94.6 %) |
2,601 (88.7%) |
< .001 |
| Throwing Versus Nonthrowing Shoulder Injuries |
Throwing |
Nonthrowing |
P Value |
| Total no. of injuries (%) | 2,215 (65.1%) | 1,188 (34.9%) | |
| Total no. of days missed due to injury | 44,050 | 24,674 | |
| Mean (median) number of days missed per injury | 21.9 (7) | 22.5 (6) | .768 |
| No. of Injuries requiring surgery (%) | 137 (6.2%) | 109 (9.2%) | .002 |
| Players who reinjured shoulder (%) | 45 (2.0%) | 43 (3.6%) | .007 |
| Return to play (%) | 2,028 (91.6%) | 1,119 (94.2%) | .005 |
| Return to same level of play (%) |
1,963 (88.6%) |
1,084 (91.3%) |
.016 |
| Batting Versus Nonbatting Injury Mechanism |
Batting |
Nonbatting |
P Value |
| Total no. of injuries (%) | 618 (18.4%) | 2,742 (81.6%) | |
| Total no. of days missed due to injury | 11,098 | 55,766 | |
| Mean (median) number of days missed per injury | 19.6 (5) | 22.6 (6) | .136 |
| No. of injuries requiring surgery (%) | 50 (8.1%) | 196 (7.1%) | .354 |
| Players who reinjured shoulder (%) | 19 (3.1%) | 69 (2.5%) | .400 |
| Return to play (%) | 581 (94.0%) | 2,577 (92.2%) | .106 |
| Return to same level of play (%) |
563 (91.1%) |
2,495 (89.2%) |
.162 |
| Front vs back batting shoulder injuries |
Front |
Back |
P value |
| Total no. of injuries (%) | 1,270 (42.4%) | 1,723 (57.6%) | |
| Total no. of days missed due to injury | 23,920 | 34,924 | |
| Mean (median) number of days missed per injury | 20.7 (5.5) | 22.2 (7) | .333 |
| No. of injuries requiring surgery (%) | 104 (8.2%) | 106 (6.2%) | .031 |
| Players who reinjured shoulder (%) | 33 (2.6%) | 38 (2.2%) | .139 |
| Return to play (%) | 1,182 (93.1%) | 1,582 (91.8%) | .200 |
| Return to same level of play (%) | 1,142 (89.9%) | 1,533 (89.0%) | .404 |
MiLB, Minor League Baseball; MLB, Major League Baseball.
Discussion
This review demonstrated 3,414 shoulder injuries leading to 68,808 days missed; the equivalent of nearly 400 full-length MLB seasons. Throwing was the most common injury activity followed by fielding and batting. Rotator cuff injury was the most common diagnosis; however, SLAP tears had both the highest season-ending rate and need for surgical intervention. With respect to the batting shoulder, the back shoulder was more often injured; however, the front shoulder more commonly required surgical intervention.
Of these 3,414 shoulder injuries, 483 (14.1%) occurred in MLB, and 2,931 (85.9%) occurred in MiLB. This pattern is consistent with the significantly larger pool of athletes across various levels of MiLB (i.e., AAA, AA, A), and similar findings have been previously observed in other professional baseball epidemiology reports.1,10 MLB batters experienced an additional 4.4 DM per injury, a 3.1% greater rate of required surgical intervention, and a 1.8% lower rate of reinjury compared with those in MiLB. These changes may suggest that the age difference is playing a role. However, there may also be some differences with diagnostic evaluation and treatment protocols with respect to level of play, especially as shoulder surgery for all professional baseball players (both batters and pitchers) is still more likely in MiLB players.3 Another potential explanation for these observations includes a talent bias at the MLB level where those players (and organizations) may be more willing to take the time off for surgery, as they anticipate a longer-term career. It could also be related to a potential reluctance of MiLB players to undergo surgical intervention if they feel that the surgical procedure, time needed for recovery, or more significant injury history could negatively impact their future value or potential to progress to greater levels of play.
With regard to specific diagnoses, the most common of these injuries in descending order was: rotator cuff injury (23.1%), impingement/subacromial bursitis (14.4%), contusions (14.0%), and long head of the biceps tendon injuries (8.9%). This supports the findings of a previous summative report on the 50 most common injuries in professional baseball.1 Our study reviewed 28 shoulder-specific diagnoses, of which our previously mentioned top 5 also represent 3 of the top 10 injuries among all professional baseball players (rotator cuff injuries, impingement/subacromial bursitis and long head of the biceps tendon injuries).1 Furthermore, when analyzing injuries affecting at least 10 players, SLAP tears had both the highest season-ending rate and need for surgical intervention. This was followed by anterior instability with labral tear, multidirectional instability, batter’s shoulder, and posterior instability. This observation of glenoid labral pathology resulting in a greater surgical burden is consistent with the investigation of Chalmers et al.,3 where they identified the labrum as the most commonly injured anatomic location in the shoulder among professional baseball players at >60%. In their cohort, pitchers were the most common position to have shoulder surgery (60%), with the labrum being responsible for 51.7% of these cases. In the present investigation of batters, the glenoid labrum collectively was involved in 13.1% of injuries with 28.3% of these players requiring surgical intervention. Comparisons of these data suggest that professional batters are still substantially affected by glenoid labrum pathology but possibly at lower rates compared with pitching athletes.
Upper-extremity injuries sustained in professional baseball players have been typically described as noncontact, overuse injuries, with modifiable risk factors based on limiting excessive throwing or pitching.3,10, 11, 12, 13 This has led to implementation of many injury prevention programs14,15 whose efficacy remains unproven as overall injury rates have not demonstrated measurable decline in recent years.1,3 The current investigation noted that 57.7% of injuries were noncontact, but a majority (62.2%) of injuries were acute. Throwing was the most common injury activity and the throwing shoulder was most commonly injured. However, our findings demonstrated that the non-throwing shoulder had both an increased frequency of surgery (6.2% vs 9.2%; P = .002) and reinjury (2.0% vs 3.6%; P = .007); while the throwing shoulder had both lower RTP (91.6% vs 94.2%; P = .005) and RTP at the same level (88.6% vs 91.3%; P = .016). These findings may be suggestive of a tendency for surgeons to avoid surgery in the throwing shoulder given the less-than-optimal outcomes that have generally been reported when surgery is performed in the throwing shoulder.
Focusing on the batting motion, there continues to be limited literature evaluating the type of injuries experienced by professional batters and their consequences. In 2018, Camp et al.8 studied the effect of being hit by pitch in professional baseball. They demonstrated that the upper extremity was the most likely region to be affected with a majority of injuries in the hand (21.8%); however, only 2.4% of injuries affected the shoulder or clavicle. Alternatively, batter’s shoulder is an injury mechanism specific to batters affecting the posterior capsulolabral complex of the lead shoulder. This remains a relatively uncommon form of posterior instability but has been shown to have up to 92% return to play rates after surgical management.7 In the present study focusing only on shoulder injuries in professional batters the back batting shoulder was most commonly injured, however the front shoulder demonstrated an elevated frequency of surgery (8.2% vs 6.2%; P = .031). Interestingly, the data did not demonstrate any differences with respect to days missed, reinjury, or return to play between shoulders. It is important to note that the back batting shoulder is most often the throwing shoulder in these athletes, as such these findings may be altered due to concurrent management strategies of their throwing shoulder. This potentially could explain the similarities with days missed and once again an inclination to treat the back or throwing shoulder nonoperatively.
Limitations
This work is not without its limitations. First, this study focused on professional batters, which may not be as generalizable to nonprofessional players. The data available through the HITS database rely on the accurate diagnosis and classification of injuries by each of the 30 professional baseball clubs, which is subject to some variability and introduction of bias. Furthermore, though the club’s athletic trainers are well trained, the database contains “miscellaneous” and “other” categories which may include some injuries that could have been more accurately described in other specific categories. Finally, precise details regarding the diagnostic assessment of injuries, specific treatments pursued, and the contract status of athletes at the time of treatment were not available within the dataset. Moreover, the specificity regarding the determination of certain diagnoses especially those designated as other is not available. As such, this may limit the understanding of the observations within this cohort.
Conclusions
During the 7-season study period, there were a total of 3,414 shoulder injuries that resulted in nearly 70,000 days of out of play in professional baseball position players/batters (non-pitchers). Although pitchers were intentionally excluded from the analysis, throwing was still the most common mechanism of injury, and rotator cuff injuries were the most common injury. Labral tears were the most likely injury to be season ending and require surgery.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: E.M.M. reports other from Stryker Corp., United States, outside the submitted work. S.C. reports and Major League Baseball medical research, United States—consultant. J.A.S. reports other from Gemini Medical LLC and Arthrex, outside the submitted work. M.L.K. reports other from Arthrex and Gemini Medical LLC, outside the submitted work. A.J.K. reports grants from Aesculap/B. Braun, grants and other from Arthrex, United States, grants from Arthritis Foundation, grants from Ceterix, grants from Histogenics, United States, grants from DJO, LLC, personal fees from Gemini Mountain Medical, LLC, other from Vericel, and other from JRF Ortho, outside the submitted work, and American Journal of Sports Medicine—editorial or governing board, International Cartilage Regeneration & Joint Preservation Society—board or committee member, International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine— board or committee member, Minnesota orthopedic society—board or committee member, Musculoskeletal Transplantation Foundation—board or committee member, and Minnesota Timberwolves—team physician. C.L.C. reports personal fees from Arthrex, other from Zimmer Biomet Holdings, United States, and other from Gemini Medical LLC, outside the submitted work, and Minnesota Twins—team physician. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Primary location where this investigation was performed: Mayo Clinic, Rochester, Minnesota, U.S.A.
Supplementary Data
References
- 1.Camp C.L., Dines J.S., van der List J.P., et al. Summative report on time out of play for major and minor league baseball: An analysis of 49,955 injuries from 2011 through 2016. Am J Sports Med. 2018;46:1727–1732. doi: 10.1177/0363546518765158. [DOI] [PubMed] [Google Scholar]
- 2.Swindell H.W., Coury J.R., Dantzker N., et al. A systematic review of the orthopaedic literature on truncal and lower extremity injuries in major league baseball players. J Am Acad Orthop Surg Glob Res Rev. 2021;5 doi: 10.5435/JAAOSGlobal-D-21-00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chalmers P.N., Erickson B.J., D’Angelo J., Ma K., Romeo A.A. Epidemiology of shoulder surgery among professional baseball players. Am J Sports Med. 2019;47:1068–1073. doi: 10.1177/0363546519832525. [DOI] [PubMed] [Google Scholar]
- 4.Conte S., Camp C.L., Dines J.S. Injury Trends in Major League Baseball Over 18 Seasons: 1998-2015. Am J Orthop (Belle Mead, NJ) 2016;45:116–123. [PubMed] [Google Scholar]
- 5.Agresta C.E., Krieg K., Freehill M.T. Risk factors for baseball-related arm injuries: A systematic review. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119825557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Posner M., Cameron K.L., Wolf J.M., Belmont P.J., Owens B.D. Epidemiology of Major League Baseball Injuries. Am J Sports Med. 2011;39:1675–1691. doi: 10.1177/0363546511411700. [DOI] [PubMed] [Google Scholar]
- 7.Wanich T., Dines J., Dines D., Gambardella R.A., Yocum L.A. ‘Batter's shoulder’: can athletes return to play at the same level after operative treatment? Clin Orthop Relat Res. 2012;470:1565–1570. doi: 10.1007/s11999-012-2264-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Camp C.L., Wang D., Sinatro A.S., et al. Getting hit by pitch in professional baseball: Analysis of injury patterns, risk factors, concussions, and days missed for batters. Am J Sports Med. 2018;46:1997–2003. doi: 10.1177/0363546518773048. [DOI] [PubMed] [Google Scholar]
- 9.Pollack K.M., D'Angelo J., Green G., et al. Developing and implementing major league baseball's health and injury tracking system. Am J Epidemiol. 2016;183:490–496. doi: 10.1093/aje/kwv348. [DOI] [PubMed] [Google Scholar]
- 10.Ciccotti M.G., Pollack K.M., Ciccotti M.C., et al. Elbow injuries in professional baseball: Epidemiological findings from the Major League Baseball injury surveillance system. Am J Sports Med. 2017;45:2319–2328. doi: 10.1177/0363546517706964. [DOI] [PubMed] [Google Scholar]
- 11.Byram I.R., Bushnell B.D., Dugger K., Charron K., Harrell F.E., Jr., Noonan T.J. Preseason shoulder strength measurements in professional baseball pitchers: Identifying players at risk for injury. Am J Sports Med. 2010;38:1375–1382. doi: 10.1177/0363546509360404. [DOI] [PubMed] [Google Scholar]
- 12.Chalmers P.N., Erickson B.J., Ball B., Romeo A.A., Verma N.N. Fastball pitch velocity helps predict ulnar collateral ligament reconstruction in Major League Baseball pitchers. Am J Sports Med. 2016;44:2130–2135. doi: 10.1177/0363546516634305. [DOI] [PubMed] [Google Scholar]
- 13.Melugin H.P., Leafblad N.D., Camp C.L., Conte S. Injury prevention in baseball: From youth to the pros. Curr Rev Musculoskelet Med. 2018;11:26–34. doi: 10.1007/s12178-018-9456-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Erickson B.J., Chalmers P.N., Bush-Joseph C.A., Romeo A.A. Predicting and preventing injury in Major League Baseball. Am J Orthop (Belle Mead, NJ) 2016;45:152–156. [PubMed] [Google Scholar]
- 15.Fleisig G.S., Diffendaffer A.Z., Aune K.T., Ivey B., Laughlin W.A. Biomechanical analysis of weighted-ball exercises for baseball pitchers. Sports Health. 2017;9:210–215. doi: 10.1177/1941738116679816. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.