Abstract
Objectives
Meditation practices positively influence the neural, hormonal and autonomic systems. We have demonstrated that long-term practice of mindfulness meditation increases N3 and rapid eye movement (REM) sleep stages and bring efficient autonomic modulation during sleep. In the present study, the probable humoral correlation that could bring about these changes is evaluated.
Material and Methods
Long-term Vipassana meditators (n=41) and controls (n=24) (males, 30-60 years of age) underwent a two-day consecutive whole night polysomnography recording. During the second day, with exposure to 100Lux brightness, blood was sampled from the antecubital vein between 8-9 PM and in subsequent early morning. Sleep stage was scored as per American Society of Sleep Medicine (ASSM) guidelines for the second-day recording. Sleep-related hormones were estimated - melatonin by radioimmunoassay; dehydroepiandrosterone (DHEA), cortisol, growth hormone (GH) and prolactin with enzyme-linked immunosorbent assay (ELISA); DHEA/cortisol ratio was calculated. Percentage of sleep stages and hormonal levels were compared between both groups using independent ‘t’ test and Pearson’s correlation was estimated between sleep stages and hormonal levels.
Results
Meditators showed increased N3, REM sleep stages. Though evening cortisol was comparable between the two groups; early morning cortisol, diurnal DHEA and melatonin were significantly higher in meditators. Diurnal DHEA correlated significantly with the N3 sleep stage in meditators.
Discussion
Higher diurnal DHEA despite variations in corresponding cortisol in meditators demonstrates that long-term Vipassana meditation practice modulates the hypothalamicpituitary-adrenal (HPA) axis and thereby influences sleep. Thus, the study provides evidence to explore the mechanism most likely involved with mindfulness meditation intervention in insomnia.
Keywords: Mindfulness; Sleep; Dehydroepiandrosterone; Hydrocortisone; Melatonin; Sleep, Slow-Wave
INTRODUCTION
Sleep quality is one of the important determining components associated with health and well-being1. Growing evidence demonstrates that mindfulness meditation practice modulates various psycho-physiological processes and moderately facilitate proper sleep. These effects are reported in both general and clinical populations2-4. Most of the studies evaluate sleep either by questionnaire, sleep diary or actigraphy5-8, however, the whole night polysomnography is the gold standard for evaluation of sleep architecture.
The foremost polysomnography evaluation on the effect of meditation on sleep was conducted among transcendental meditation (TM) practitioners9 and showed that the senior TM practitioners have higher slow-wave sleep and rapid eye movement (REM) sleep when compared to the age-matched nonmeditating controls. Further, during slow-wave sleep, meditators showed higher theta-alpha power, which the authors ascribe to a higher state of consciousness during sleep. We have reported the differential effect of breath-based meditation practice (Sudarshan kriya yoga) and mindfulness meditation practice (Vipassana meditation) on sleep architecture. The former enhances slowwave sleep but has no effect on REM sleep; whereas the latter increases both slow-wave sleep and REM sleep even in the older age group and enhances REM density10-12. Despite attenuation of slow-wave generating mechanism with the normal ageing process13, our observation of retaining slow-wave sleep even in elderly long-term Vipassana meditation practitioners11 is attributed to the meditation-induced neural plasticity changes. Effective thalamocortical and corticocortical interactions are reported among meditators, which facilitates the generation of slow waves14. Even short-term Vipassana meditation practice is reported to enhance slow frequency oscillations during NREM sleep, implying neural plasticity changes15. Further, effective buffering of overt sympathetic surges during sleep is observed in long-term Vipassana meditation practitioners that could also facilitate a stable sleep16.
In addition to the neural and autonomic influences, sleep is also modulated by the hormonal system. Meditation practices induce both immediate and long-term effects on the hormonal milieu. In general, the practice of meditation reduces cortisol and catecholamines17,18, increases dehydroepiandrosterone (DHEA), melatonin, growth hormone (GH), thyroid-stimulating hormone (TSH) and prolactin19-24. Among various hormones, DHEA, cortisol and melatonin are considered as a metric to assess the effect of meditation practice on the humoral system25 and these hormones are also involved in the regulation of sleep26. An increase in melatonin levels23,24,27,28 and reduction in the cortisol response to a stressor17,22,29,30 is reported immediately after a meditation session. However, with the long-term practice of mindfulness meditation, enhanced melatonin and reduced cortisol are observed at the basal level31-33. On the contrary, long-term practice of TM is known to increase DHEA; reduce prolactin, growth hormone and TSH, without much changes in cortisol levels19,21,34. Mindfulness meditation intervention in cancer patients improves sleep quality and is associated with reduced random cortisol levels without affecting melatonin and DHEA25. But higher early morning cortisol levels is attributed to adequate sleep and is observed in yoga and mindfulness practitioners but not with TM practice35-37. These inconsistencies on the effect of meditation practices on hormones are not yet resolved though it was first reported decades back38, and the influence of meditation practice on sleep-associated hormonal profiles is sparingly evaluated. Our earlier studies have shown that long-term Vipassana meditation practice, by inducing neural plasticity changes and modulating cardiac autonomic activity will positively influence sleep architecture16,39. In the present manuscript, we have evaluated sleep-related hormones and their correlation with sleep stages among long-term practitioners of Vipassana meditation.
MATERIAL AND METHODS
The data for the study were from a subgroup of participants from our earlier report comprising of 91 subjects (mindfulness meditators and controls) who underwent consecutive two whole night polysomnography recordings11. Out of 91 subjects, 65 of them gave written consent for hormonal assay along with whole night polysomnography recordings. The sleep data and hormonal assessment of these subjects, i.e., mindfulness meditators (n=41) and non-meditating controls (n=24) are being reported here. The study was initiated after obtaining approval from the Institute Human Ethics Committee (NIMHANS/XXXVII/IEC/2005).
The meditators were practising Vipassana meditation regularly for more than three years, daily for 2-4 hours, i.e.,1-2 hours, in the morning (between 6-8 A.M.) and 1-2 hours in the evening (between 6-8 P.M.). The details of meditation training have been elaborated on in our earlier publication11. In brief, Vipassana meditation is possibly the most ancient form of mindfulness-based meditative technique. Presently the technique follows the tradition of Sayagyi U Ba Khin as taught by S. N. Goenka all over the globe. The word ‘Vipassana’ in the Pali language means ‘to see things as they are’. Vipassana meditation practice involves the strategy of mindfulness wherein, the meditators learn to notice and witness the perceptions of the senses and the thoughts arising in the mind without reacting to them, like an onlooker, and to focus their attention on their bodily activities in their true perspective, in their true nature. The Vipassana meditators in the present study were recruited through the Vipassana Research Institute at Igathpuri, India, the world headquarters for Vipassana meditation. All the meditators were employed in various private and public sector institutions and leading normal social life, none of them were monks nor lived in a monastery. The control subjects were recruited from various private and public sector institutions. Participants who were practising any other form of meditation, yoga, or regular physical activity were excluded. Subjects from both groups who consumed tobacco, alcohol, and regular medications that could potentially influence sleep and hormonal profile were excluded. Subjects from both groups were matched for demographic characteristics such as age, socioeconomic and educational status. Before recruitment, the clinical history of participants was obtained; their routine sleep habits were assessed and were examined for medical, psychiatric, neurological and other disease conditions. Participants maintained a sleep log for a week before the study. Those with a history of sleep disorders for three months and beyond, sleep-log showing sleep disturbance/ restriction or deprivation, on regular medications for neuropsychiatric conditions were excluded from the study.
Participants were housed in the institute guesthouse with a uniform diet. They were instructed to refrain from the consumption of coffee or tea after 4 p.m. and asked to report to the Human Sleep Research Laboratory after their dinner. With all the precautions, 5ml of blood from the antecubital vein was drawn between 8-9 P.M. before sleep recordings. Subjects woke up the next morning without an alarm and after half an hour the blood was drawn. Blood was collected in uniform conditions with the subject being seated and the room being illumined with the intensity of about 100Lux. Blood samples were immediately centrifuged at 3000rpm for 15min and serum was separated, aliquot in 5ml vials, and stored at-800ºC.
The whole night polysomnography was recorded using a 32-channel digital EEG system (EEG- 2110, Nihon Kohden Corporation, Japan) with EEG, EOG, and chin EMG electrodes. The technical details are elaborated elsewhere11. The recording was carried out until the subjects woke spontaneously by themselves in the morning. The offline scoring of sleep was carried with ASSM criteria40. The sleep scoring was carried independently by two experienced sleep scorers and the reliability of scoring from both of them was about 95.04%. Sleep efficiency index (SEI) was calculated using the formula (TST + TIB) x100, where, TST is total sleep time and TIB is the total time in bed. The recordings which had SEI of more than 85% were selected for the analysis. SEI based selection ensures the exclusion of possible sleep-related problems so that the analysis is carried out only among good sleepers.
Melatonin was estimated by radioimmunoassay (RIA)41. Radioimmunoassay (Biosource Europe SA, Belgium) involves competition between a radioactive and non-radioactive antigen for a fixed number of antibody binding sites. The amount of I125 labelled antigen bound to the antibody is inversely proportional to the analyte concentration of the sample. When the system is in equilibrium, the antibody-bound radioactivity is precipitated with a second antibody in the presence of polyethylene glycol. The precipitate is counted using a gamma counter. Quantification is achieved by comparing their activity with a reference curve prepared with a known standard. The intra-assay coefficient of variation of melatonin is 12.3%.
DHEA, cortisol, GH, and prolactin were analyzed by enzyme-linked chemiluminescence (ELISA) (Immulite of Siemens Medical Solutions). The general principle of ELISA is applied for the assay of hormones, wherein the hormone specific antibodies are used. Beads coated with the specific hormone antibody are mixed with a reagent containing alkaline phosphatase, conjugated with a rabbit antibody. Reagent with serum is incubated with antibody-coated beads. Antigen (hormone) in the serum forms a complex with antibody sandwitched with the reagent. The unbound enzyme is removed by centrifugal wash and a chemiluminescence’s substrate is added to the bead. The signal is generated in proportion to the bound enzyme. Intra-assay coefficient variation for prolactin and DHEA is 9.5%, GH is 5.3%, and cortisol is 8.8%. Subsequently, the DHEA/cortisol ratio was calculated.
Statistics
The statistical test was applied using SPSS version 24. Descriptive statistics of sleep variables (mean and standard deviation) and hormonal profile (mean and standard error) were calculated. The hormonal levels were positively skewed (skewness >2); therefore, the values were log-transformed for statistical analysis. However, in the results, the original values are depicted.
Independent ‘t’ test was used to compare the percentage of sleep stages and logarithmic values of hormonal profile between the two groups. A paired ‘t’ test was used to compare the diurnal differences in logarithmic hormonal levels within controls and meditators. The correlation was estimated between various sleep stages and hormonal profiles using Pearson’s correlation. And p<0.05 is the level of significance.
RESULTS
Both the groups were comparable for their age [controls = 44.67±9.72 years, meditators = 45.04±9.56 years, t=0.63, p=0.52]. No significant difference in the duration of sleep is observed between the two groups [controls = 357.14±63.36 minutes, meditators = 375.98±62.07 minutes, t=1.30, p=0.25]. Sleep efficiency index even though was above 90% in both, meditators showed significantly higher value [controls = 91.85±4.19 percentage, meditators = 93.98±3.43 percentage, t=2.1, p=0.036]. Whereas microarousal index during sleep was comparable between two groups [controls = 15.26±8.01, meditators = 16.42±8.01, t=0.41, p=0.68].
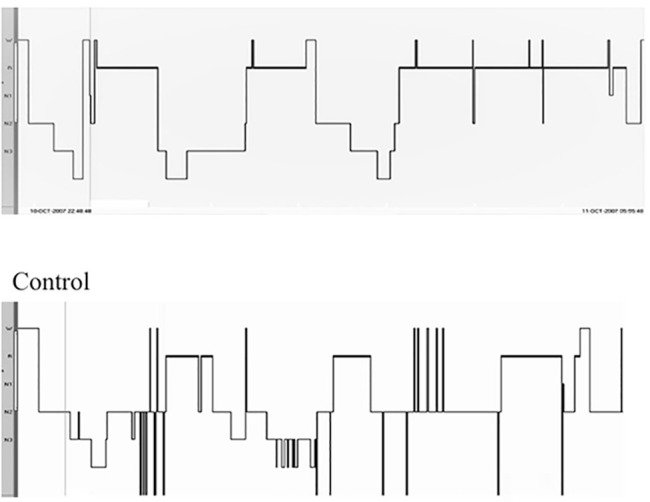
In meditators, the percentage of sleep stage N1 [controls = 19.29±11.18, meditators = 12.00±8.55, t=2.85, p=0.006] and N2 [controls = 50.43±11.55, meditators = 42.09±11.75, t=2.71, p=0.009] was less, whereas, percentage of N3 [controls = 6.86±1.39, meditators = 15.57±9.06, t=4.01, p=0.000] and REM sleep stages [controls = 22.40±7.76, meditators = 32.20±8.89, t=4.39, p=0.000] were significantly higher when compared to controls. The representative hypnogram of a meditator and control is given in Figure 1.
Figure 1.
Representative hypnogram of meditator and control subject.
Notes: Representative hypnogram of meditator and control; meditator shows enhanced N3 and REM sleep state than control.
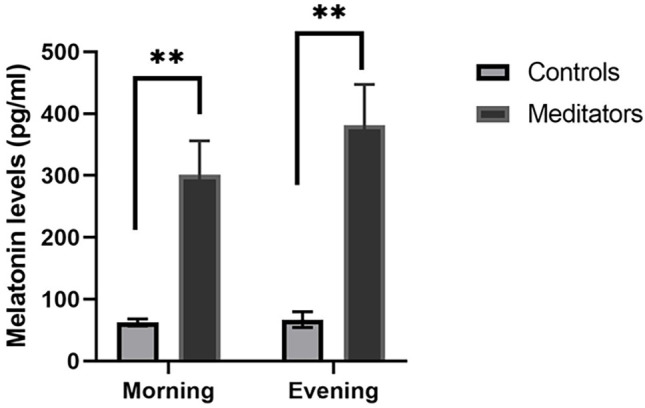
The details of the hormonal levels are provided in Table 1. Diurnal melatonin levels were significantly higher in meditators than controls [morning t=4.05, p=0.00, evening t=4.05, p=0.00] (Figure 2), but, did not show any significant differences within controls and meditators. Similarly, DHEA levels both during morning and in the evening were higher among meditators than controls [morning t=3.16, p=0.04, evening t=3.08, p=0.04] without significant diurnal variations within each group. Cortisol levels in meditators, when compared to controls, showed higher levels in morning sample [t=2.04, p=0.04], but, evening levels was comparable [t=0.37, p=0.70]. Whereas, significantly higher evening cortisol levels were observed in both controls and meditators when compared to their own morning levels. Both GH [morning t=1.38, p=0.19, evening t=0.09, p=0.56] and prolactin [morning t=0.08, p=0.99, evening t=1.62, p=0.20] did not show any significant difference between the two groups. Diurnal variations of prolactin in both controls [t=3.34, p=0.003] and meditators [t=4.38, p=0.00] showed increased levels in the evening, however, neither of the groups showed any diurnal difference in GH levels. DHEA/ cortisol ratio was comparable between the groups [morning= t=0.45, p=0.65, evening t=0.96, p=0.33] and the ratio was significantly less in the evening in both controls and meditators.
Table 1.
Comparison of diurnal levels of melatonin, DHEA, cortisol, GH, prolactin, and DHEA/cortisol ratio between controls and meditators.
| Control (n=24) | Meditators (n=41) | p-value | ||
|---|---|---|---|---|
| Melatonin (pg/mL) | Morning | 62.95±5.69 | 301.53±54.44 | <0.001 |
| Evening | 66.95±12.65 | 381.80±65.51 | <0.001 | |
| t=2.8, p=0.001 | t=1.28, p=0.21 | |||
| DHEA (pg/dL) | Morning | 169.39±36.23 | 192.37±24.21 | 0.04 |
| Evening | 156.72±36.22 | 213.25±33.14 | 0.04 | |
| t=0.83, p=0.041 | t=1.38, p=0.18 | |||
| Cortisol (Pg/dL) |
Morning | 7.52±0.88 | 10.26±0.90 | 0.04 |
| Evening | 15.31±1.02 | 15.85±0.93 | 0.70 | |
| t=4.83, p=0.00 | t=3.54, p=0.001 | |||
| Growth hormone (ng/dL) |
Morning Evening |
0.14±0.05 0.33±0.70 |
0.30±0.10 0.22±0.33 |
0.19 0.56 |
| t=1.41, p=0.17 | t=0.57, p=0.51 | |||
| Prolactin (ng/dL) |
Morning | 12.93±1.52 | 12.95±1.76 | 0.99 |
| Evening | 23.94±12.95 | 19.51±1.96 | 0.20 | |
| t=3.34, p=0.003 | t=4.38, p=0.00 | |||
| DHEA/Cortisol ratio |
Morning | 28.06±5.55 | 24.82±4.41 | 0.65 |
| Evening | 10.73±1.93 | 13.80±2.21 | 0.33 | |
| t=3.17, p=0.005 | t=2.26, p=0.02 |
Notes: Meditators show significantly higher diurnal levels of melatonin, DHEA, and morning levels of cortisol when compared to controls. Evening levels of melatonin, cortisol, and prolactin were higher in controls when compared to their morning levels. Meditators showed a significantly higher evening cortisol and prolactin levels than their morning levels. Values in mean ± SE, p<0.05 as significant level.
Figure 2.
Comparison of morning and evening levels of melatonin between controls and meditators.
Notes: Melatonin levels, both during morning and evening are significantly high in meditators than controls; **p<0.001.
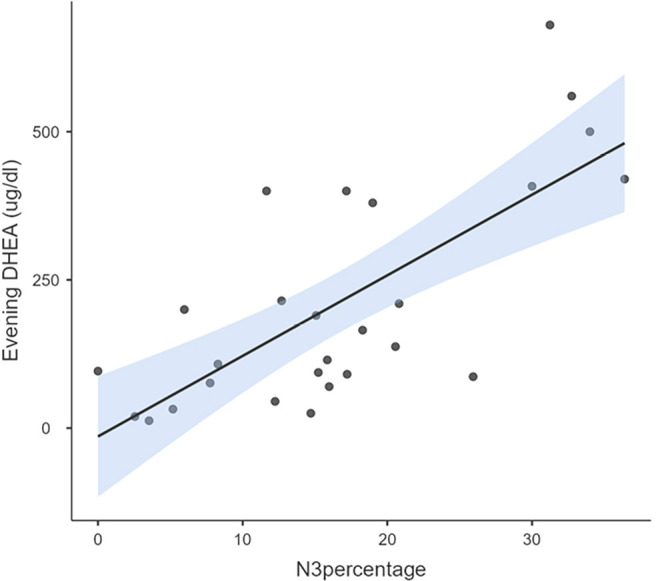
Average years of meditation practice by meditators was 7.29±2.32 years of practice. The Pearson’s correlation with meditation duration showed a positive relation with levels of DHEA (morning r=0.36, p=0.03), prolactin (morning r=0.73, p=0.00, evening r =0.52, p=0.002) and DHEA/cortisol ratio (morning r=0.41, p=0.02). Sleep stages in meditators showed a significant positive correlation between stage N3 with diurnal DHEA [morning r=0.68, p=0.00, evening r=0.72, p=0.00, (Figures 3 and 4)], morning melatonin [morning r=0.42, p=0.02] and DHEA/cortisol ratio [morning r=0.58, p=0.00]. Otherwise, no significant correlation was found with percentage of N1, N2 and REM sleep. Among controls, only morning cortisol levels showed significant negative correlation with percentage of N2 sleep stage (r=-0.58, p=0.003).
Figure 3.
Correlation between morning DHEA levels and N3 percentage in meditators.
Notes: Morning DHEA levels correlated significantly (r=3.16, p=0.04) with the percentage of N3 in meditators.
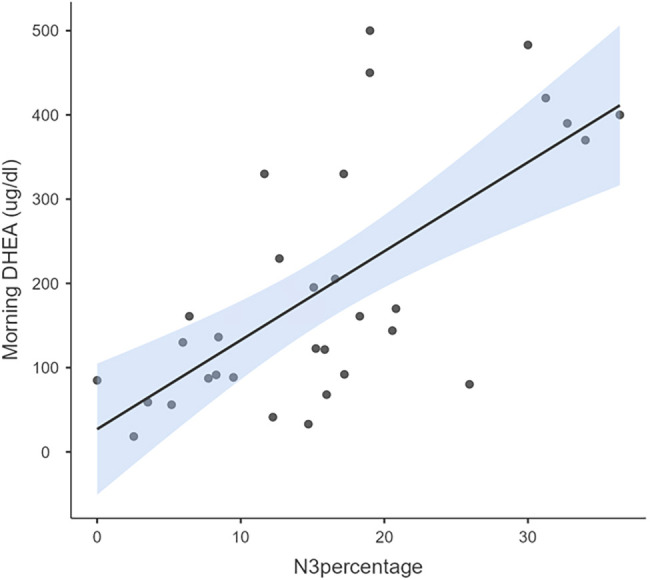
Figure 4.
Correlation between evening DHEA levels and N3 percentage among meditators.
Notes: Evening DHEA levels correlated significantly (r=3.08, p=0.04) with the percentage of N3 in meditators.
DISCUSSION
The present study assessed the levels of sleep-related hormonal profiles and their correlation with sleep stages among long-term practitioners of Vipassana meditation. Vipassana meditators showed significantly higher diurnal levels of DHEA, melatonin and morning cortisol levels, besides increased N3 sleep stage demonstrating a moderate to strong significant positive correlation with diurnal DHEA levels. There are consistent reports demonstrating a positive effect of meditation practice on subjective sleep quality despite the variability in its correlation with hormonal profiles2,38. However, to the best of our knowledge, this could be the first study to report the relationship between sleep-related hormones with whole night polysomnographic data among long-term Vipassana meditation practitioners.
Meditation practice is known to increase DHEA in men (45-70 years) and women (20-74 years) demonstrating the robust effect even after adjusting for other confounding variables like diet, body mass index, and physical activity19. Increased diurnal DHEA levels in the middle-aged male meditators corroborate with this report. A healthier shift of DHEA is observed in patients who practised mindfulness meditation and yoga for 2 months; however, mindfulness practice also showed improvement in sleep quality25,42. In contrast, three years of yoga practice showed improvement in sleep quality, without any changes in DHEA43. Thus, reinforcing the observation that type and duration of meditation practice have a differential effect on hormonal profiles44. In the present study, long-term practitioners of Vipassana meditation have shown high levels of diurnal DHEA with a significant positive correlation with N3 sleep stage. Lower DHEA levels, in healthy individuals, is known to induce sleep disturbance and reduces slow-wave sleep in patients with obstructive sleep apnea45,46. However, few studies have observed no significant relationship between DHEA levels either with sleep duration and other polysomnography variables47,48. These contrasting observations could be due to the influence of DHEA on multiple pathways associated with sleep-promoting or inhibiting mechanisms49. These mechanisms may include DHEA-driven variations in testosterone and estradiol secretion which promotes or inhibits sleep respectively50 or influencing agonistic and antagonistic action on GABAergic activity which influences NREM and REM sleep49,51. Therefore, DHEA at appropriate dosage is considered as supplementation therapy for various sleep disorders52. Further, DHEA is known to have an antiaging effect53,54 and the observation of a positive correlation between DHEA and N3 sleep stage among meditators in the present study is in accordance with our earlier finding of mitigating age-associated changes in sleep architecture among long-term Vipassana meditation practitioners11.
In the present study, meditators, when compared to controls, showed a higher level of cortisol in the morning. Whereas, evening cortisol levels were comparable between them. Our observation of higher cortisol levels in the morning appears to be counterintuitive where meditation practice is expected to decrease the cortisol levels18. Though higher morning cortisol levels, was reported to be proportional to perceived stress55, studies consistently have demonstrated a blunted response to chronic stress conditions in apparently healthy individuals56,57 and also in various medical and psychiatric conditions58. The blunted response is attributed to the reduced sensitivity of adrenals to circulating adrenocorticotropin (ACTH) hormone which is regulated by the hypothalamic-pituitary-adrenal (HPA) axis59,60. Therefore, impaired early morning cortisol is considered to be the marker of alteration in the function of the HPA axis due to prolonged stress61.
The most accepted functional role of early morning cortisol is that it serves as an allostatic boost on awakening to prime the neural network to modulate cognition anticipating the demands of the day62 and facilitates wakefulness with better resilience59,63. This allostatic boost appears to be more in the early morning riser64,65 irrespective of the mode of waking up, i.e., spontaneously or by an alarm66 and chronotype of the person67. There are reports showing higher morning cortisol levels with mindfulness meditation practice36,68. However, the latest report on TM practice in young adults shows no increase in early morning cortisol levels when compared to the waitlist control group37. It could be attributed that type and duration of meditation practice will differently influence HPA activity. In response to cortisol, the sensitive HPA axis secretes DHEA to mitigate the adverse actions of cortisol69. This protective response is reduced with prolonged stress70. In the present study, meditators showed higher diurnal DHEA levels. It is to be noted that though evening cortisol levels were comparable between both groups, meditators showed higher DHEA levels. Evening cortisol reflects the stress levels of the day71. This demonstrates that the HPA axis in meditators is more sensitive than controls. Our observation of higher DHEA levels in meditators and its correlation with N3 sleep stage provides a clue that the long-term Vipassana meditation practice could possibly influence the HPA axis to be more resilient and dynamic, and favourably influence sleep. However, the cortisol response to early morning wake is known to vary on situational factors like prior day experiences, the anticipation of the day ahead and its related stress and changes in weather/seasonal conditions58,71. More studies are warranted in this direction accounting for other factors influencing morning cortisol levels.
Melatonin is the most versatile hormone preserved through evolution72. In the present study, we observed significantly higher diurnal melatonin levels in meditators and N3 sleep stage showed a positive correlation with morning melatonin levels. Whereas, among controls, no correlation was observed between melatonin levels and sleep stages. Various types of meditation practices like mindfulness, TM, Omkar meditation has been shown to increase nocturnal melatonin levels (both saliva and plasma) immediately after a meditation session and high salivary levels are maintained for long hours after meditation23,24,27,28. It is to be noted that long-term meditators have shown higher basal melatonin73, thus, showing the duration of meditation practice differently influence melatonin. Further, melatonin levels depend on the type of biological specimen and methodology used to estimate. Melatonin in plasma is ten times more than in the other biological specimens. In the present study, plasma levels of melatonin were estimated using a more sensitive method the radioimmunoassay with I125 labelled iodomelatonin41. Other confounding factors that can influence melatonin levels like circadian variations, exposure to light and diet were relatively taken care of. All participants were housed in the guesthouse with a uniform diet and blood was drawn during the same clock hours exposed to 100Lux brightness in the laboratory. Both controls and meditators were with their normal social and professional responsibilities with no shift work. This demonstrates that circadian phase shifts were not present in the participants, which otherwise would have been a major confound. As per the norms73, the melatonin levels were within the normal range in controls and acceptable maximal upper limit in meditators.
Melatonin administration in normal healthy volunteers and in various clinical conditions is known to improve sleep by reducing sleep onset latency, increasing sleep duration and efficiency74-78. On the contrary, there are reports showing no effect79 or influences only by reducing the sleep onset latency80. Similarly, variable effects of melatonin on sleep stages are reported. Studies have shown reduced slow-wave sleep with either decrease81 and increase82 of sleep stage N2 with enhanced81 or no changes82 in REM sleep. Few have shown no effects of melatonin on sleep stages83-86 except one study demonstrating only reduction in REM onset latency87. The reasons for inconsistent results could be due to variations in the dosage, timing and mode of administration. Further, the methodology used to acquire sleep data could also influence the outcome, where variations in the quantification of few sleep variables are reported between actigraphy and polysomnography88. In the present study, polysomnographically (gold standard method) scored N3 sleep stage in meditators showed a positive correlation with morning melatonin levels. Whereas, controls did not show any correlation between their melatonin level and sleep stages. The reason for such observation cannot be deciphered from the present protocol. It is recommended to have a serial blood sampling throughout the night for melatonin estimation to capture the circadian variations along with other physiological variables like temperature for a deeper insight. However, it is important to mention that meditation practice significantly increases melatonin levels. Three reasons have been hypothesized for enhanced melatonin levels in meditators viz., reduced hepatic metabolism of melatonin or meditationinduced higher serotonin and noradrenaline levels, which are essential for melatonin synthesis89 or meditation-induced heightened activity of the pineal gland itself90. In the present study, meditation was not preceded before sleep nor prior to blood collection in the morning. Therefore, the immediate effect of meditation on hormone level is ruled out. Hence, high circulating melatonin levels observed in the study could possibly be a trait effect of intense meditation practice.
Melatonin is known to synergistically influence DHEA and enhances the inhibitory effect of GABA to improve sleep91. There is evidence to demonstrate the increased production of GABA in the brain with meditation practice92-96. With this background, we speculate that meditation-induced effects like higher levels of DHEA, melatonin and enhanced inhibitory effect of GABA could cumulatively have facilitated the slow-wave generation thereby enhancing N3 sleep stage. In addition, DHEA and melatonin are shown to have anxiolytic, antioxidant, anti-stress, antiaging, immuno-modulation and other hosts of physiological and psychological benefits21,73-75 could have also influenced sleep in meditators. More studies are warranted especially in assessing the circadian variations of hormones with serial sampling and estimating GABA levels to establish the causal relationship between hormonal levels and sleep architecture in meditators. Other hormones like growth hormone and prolactin did not show any correlation with sleep stages in both controls and meditators.
In conclusion, long-term Vipassana meditation practice increases diurnal DHEA, melatonin and morning cortisol levels. Though all three hormones are known to influence sleep, we observed a positive correlation of N3 sleep stage only with diurnal DHEA. An increase in DHEA with cortisol levels in meditators reflects the positive influence of meditation practice on the HPA axis. This humoral correlate with sleep architecture is in addition to the neural plasticity and autonomic modulatory effects of Vipassana meditation practice on sleep11,16,39. This study provides ample evidence to explore the mechanisms that probably could have been involved in the beneficial effect of mindfulness meditation intervention in insomnia. However, our observation is limited to long-term practitioners of Vipassana meditation. The circadian variations of these hormones and other related factors like core body temperature were not estimated in the study. To get more insight further experiments are warranted with varying duration of Vipassana meditation practice and estimating the circadian variations of hormones.
Acknowledgments
A special note of our gratitude to the Vipassana Research Institute, Igatpuri, India for their constant support and encouragement. We also thank all the participants for their support and co-operation to make the study possible. We greatly acknowledge the technical help provided by Mr. Ramachandra M, Mr. Nagaraj BG towards the completion of the study.
Funding Statement
The study was funded by CCRYN (Central Council for Research in Yoga and Naturopathy), Dept. of AYUSH, Ministry of Health and Family welfare Govt. of India, New Delhi (project no. 12-2/Res/CCRYN/2003-2004).
Footnotes
Data
The data will be made available on specific requests to the corresponding author.
Funding source
The study was funded by CCRYN (Central Council for Research in Yoga and Naturopathy), Dept. of AYUSH, Ministry of Health and Family welfare Govt. of India, New Delhi (project no. 12-2/Res/CCRYN/2003-2004).
REFERENCES
- 1.Mystakidou K, Parpa E, Tsilika E, Pathiaki M, Gennatas K, Smyrniotis V, et al. The relationship of subjective sleep quality, pain, and quality of life in advanced cancer patients. Sleep. 2007 Jun;30(6):737–42. doi: 10.1093/sleep/30.6.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rusch HL, Rosario M, Levison LM, Olivera A, Livingston WS, Wu T, et al. The effect of mindfulness meditation on sleep quality: a systematic review and meta-analysis of randomized controlled trials. Ann N Y Acad Sci. 2019 Jun;1445(1):5–16. doi: 10.1111/nyas.13996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ong JC, Ulmer CS, Manber R. Improving sleep with mindfulness and acceptance: a metacognitive model of insomnia. Behav Res Ther. 2012 Nov;50(11):651–60. doi: 10.1016/j.brat.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greeson JM, Zarrin H, Smoski MJ, Brantley JG, Lynch TR, Webber DM, et al. Mindfulness meditation targets transdiagnostic symptoms implicated in stress-related disorders: understanding relationships between changes in mindfulness, sleep quality, and physical symptoms. Evid Based Complement Alternat Med. 2018;2018:4505191. doi: 10.1155/2018/4505191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khalsa SBS. Treatment of chronic insomnia with yoga: a preliminary study with sleep-wake diaries. Appl Psychophysiol Biofeedback. 2004 Dec;29(4):269–78. doi: 10.1007/s10484-004-0387-0. [DOI] [PubMed] [Google Scholar]
- 6.Ong JC, Manber R, Segal Z, Xia Y, Shapiro S, Wyatt JK. A randomized controlled trial of mindfulness meditation for chronic insomnia. Sleep. 2014 Sep;37(9):1553–63. doi: 10.5665/sleep.4010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hubbling A, Reilly-Spong M, Kreitzer MJ, Gross CR. How mindfulness changed my sleep: focus groups with chronic insomnia patients. BMC Complement Altern Med. 2014 Feb;14(1):50. doi: 10.1186/1472-6882-14-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Irwin MR, Olmstead R, Motivala SJ. Improving sleep quality in older adults with moderate sleep complaints: a randomized controlled trial of Tai Chi Chih. Sleep. 2008 Jul;31(7):1001–8. [PMC free article] [PubMed] [Google Scholar]
- 9.Mason LI, Alexander CN, Travis FT, Marsh G, Orme-Johnson D, Gackenbach J, et al. Electrophysiological correlates of higher states of consciousness during sleep in long-term: Practitioners of the transcendental meditation program. Sleep. 1997 Feb;20(2):102–10. doi: 10.1093/sleep/20.2.102. [DOI] [PubMed] [Google Scholar]
- 10.Sulekha S, Thennarasu K, Vedamurthachar A, Raju TR, Kutty BM. Evaluation of sleep architecture in practitioners of Sudarshan Kriya yoga and Vipassana meditation. Sleep Biol Rhythms. 2006;4(3):207–14. [Google Scholar]
- 11.Pattanashetty R, Sathiamma S, Talakkad S, Nityananda P, Trichur R, Kutty BM. Practitioners of Vipassana meditation exhibit enhanced slow wave sleep and REM sleep states across different age groups. Sleep Biol Rhythms. 2010;8(1):34–41. [Google Scholar]
- 12.Maruthai N, Nagendra RP, Sasidharan A, Srikumar S, Datta K, Uchida S, et al. Senior Vipassana meditation practitioners exhibit distinct REM sleep organization from that of novice meditators and healthy controls. Int Rev Psychiatry. 2016 Jun;28(3):279–87. doi: 10.3109/09540261.2016.1159949. [DOI] [PubMed] [Google Scholar]
- 13.Mourtazaev MS, Kemp B, Zwinderman AH, Kamphuisen HA. Age and gender affect different characteristics of slow waves in the sleep EEG. Sleep. 1995 Sep;18(7):557–64. doi: 10.1093/sleep/18.7.557. [DOI] [PubMed] [Google Scholar]
- 14.Lutz A, Greischar LL, Rawlings NB, Ricard M, Davidson RJ. Longterm meditators self-induce higha mplitude gamma synchrony during mental practice. Proc Natl Acad Sci. 2004 Nov;101(46):16369–73. doi: 10.1073/pnas.0407401101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dentico D, Ferrarelli F, Riedner BA, Smith R, Zennig C, Lutz A, et al. Short meditation trainings enhance non-REM sleep low-frequency oscillations. PLoS One. 2016 Feb;11(2):e0148961. doi: 10.1371/journal.pone.0148961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nagendra R, Sulekha S, Sasidharan A, Sathyaprabha T, Pradhan N, Raju T, et al. Vipassana meditation practices enhance the parasympathetic activity during sleep: A case-control study of heart rate variability across sleep cycles. Int J Complement Alt Med. 2017;5(2):14–12. [Google Scholar]
- 17.Jevning R, Wilson AF, Davidson JM. Adrenocortical activity during meditation. Hormon Behav. 1978 Feb;10(1):54–60. doi: 10.1016/0018-506x(78)90024-7. [DOI] [PubMed] [Google Scholar]
- 18.Infante JR, Torres-Avisbal M, Pinel P, Vallejo JA, Peran F, Gonzalez F, et al. Catecholamine levels in practitioners of the transcendental meditation technique. Physiol Behav. 2001 Jan;72(1-2):141–6. doi: 10.1016/s0031-9384(00)00386-3. [DOI] [PubMed] [Google Scholar]
- 19.Glaser JL, Brind JL, Vogelman JH, Eisner MJ, Dillbeck MC, Wallace RK, et al. Elevated serum dehydroepiandrosterone sulfate levels in practitioners of the Transcendental Meditation (TM) and TM-Sidhi programs. J Behav Med. 1992 Aug;15(4):327–41. doi: 10.1007/BF00844726. [DOI] [PubMed] [Google Scholar]
- 20.Jevning R, Wallace RK, Beidebach M. The physiology of meditation: a review. A wakeful hypometabolic integrated response. Neurosci Biobehav Rev. 1992;16(3):415–24. doi: 10.1016/s0149-7634(05)80210-6. [DOI] [PubMed] [Google Scholar]
- 21.Werner OR, Wallace RK, Charles B, Janssen G, Stryker T, Chalmers RA. Long-term endocrinologic changes in subjects practicing the Transcendental Meditation and TM-Sidhi program. Psychosom Med. 1986;48(1-2):59–66. doi: 10.1097/00006842-198601000-00004. [DOI] [PubMed] [Google Scholar]
- 22.MacLean CR, Waltson KG, Wennenberg SR, Levitsky DK, Mandarino JV, Waziri R, et al. Altered responses of cortisol, GH, TSH and testosterone to acute stress after four months’ practice of transcendental meditation (TM) Ann N Y Acad Sci. 1995 Nov;746:381–4. doi: 10.1111/j.1749-6632.1994.tb39261.x. [DOI] [PubMed] [Google Scholar]
- 23.Massion AO, Teas J, Hebert JR, Wertheimer M, Kabat-Zinn J. Meditation, melatonin and breast/prostate cancer: hypothesis and preliminary data. Med Hypotheses. 1995 Jan;44(1):39–46. doi: 10.1016/0306-9877(95)90299-6. [DOI] [PubMed] [Google Scholar]
- 24.Tooley GA, Armstrong SM, Norman TR, Sali A. Acute increases in night-time plasma melatonin levels following a period of meditation. Biol Psychol. 2000 May;53(1):69–78. doi: 10.1016/s0301-0511(00)00035-1. [DOI] [PubMed] [Google Scholar]
- 25.Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology. 2004 May;29(4):448–74. doi: 10.1016/s0306-4530(03)00054-4. [DOI] [PubMed] [Google Scholar]
- 26.Krueger JM, Fang J, Hansen MK, Zhang J, Obal Junior F. Humoral regulation of sleep. News Physiol Sci. 1998 Aug;13(4):189–94. doi: 10.1152/physiologyonline.1998.13.4.189. [DOI] [PubMed] [Google Scholar]
- 27.Liou CH, Hsieh CW, Hsieh CH, Chen DY, Wang CH, Chen JH, et al. Detection of nighttime melatonin level in Chinese Original Quiet Sitting. J Form Med Assoc. 2010 Oct;109(10):694–701. doi: 10.1016/S0929-6646(10)60113-1. [DOI] [PubMed] [Google Scholar]
- 28.Harinath K, Malhotra AS, Pal K, Prasad R, Kumar R, Kain TC, et al. Effects of Hatha yoga and Omkar meditation on cardiorespiratory performance, psychologic profile, and melatonin secretion. J Altern Complement Med. 2004 Apr;10(2):261–8. doi: 10.1089/107555304323062257. [DOI] [PubMed] [Google Scholar]
- 29.Bottaccioli F, Carosella A, Cardone R, Mambelli M, Cemin M, D’Errico MM, et al. Brief training of psychoneuroendocrinoimmunology-based meditation (PNEIMED) reduces stress symptom ratings and improves control on salivary cortisol secretion under basal and stimulated conditions. Explore (NY) 2014 May/Jun;10(3):170–9. doi: 10.1016/j.explore.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 30.Turakitwanakan W, Mekseepralard C, Busarakumtragul P. Effects of mindfulness meditation on serum cortisol of medical students. J Med Assoc Thai. 2013 Jan;96(Suppl 1):S90–S5. [PubMed] [Google Scholar]
- 31.Solberg EE, Holen A, Ekeberg O, Osterud B, Halvorsen R, Sandvik L. The effects of long meditation on plasma melatonin and blood serotonin. Med Sci Monit. 2004 Mar;10(3):CR96–CR101. [PubMed] [Google Scholar]
- 32.Fernandes CA, Nóbrega YK, Tosta CE. Pranic meditation affects phagocyte functions and hormonal levels of recent practitioners. J Altern Complement Med. 2012 Aug;18(8):761–8. doi: 10.1089/acm.2010.0718. [DOI] [PubMed] [Google Scholar]
- 33.Jacobs TL, Shaver PR, Epel ES, Zanesco AP, Aichele SR, Bridwell DA, et al. Self-reported mindfulness and cortisol during a Shamatha meditation retreat. Health Psychol. 2013 Oct;32(10):1104–9. doi: 10.1037/a0031362. [DOI] [PubMed] [Google Scholar]
- 34.Walton KG, Pugh ND, Gelderloos P, Macrae P. Stress reduction and preventing hypertension: preliminary support for a psychoneuroendocrine mechanism. J Altern Complement Med. 1995;1(3):263–83. doi: 10.1089/acm.1995.1.263. [DOI] [PubMed] [Google Scholar]
- 35.Cahn BR, Goodman MS, Peterson CT, Maturi R, Mills PJ. Yoga, meditation and mind-body health: increased BDNF, cortisol awakening response, and altered inflammatory marker expression after a 3 month yoga and meditation retreat. Front Hum Neurosci. 2017 Jun;11:315. doi: 10.3389/fnhum.2017.00315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Robb SW, Haslam A, Wirth MD, Gay JL, Middleton L, Healy M, et al. Relationship between Meditation and waking salivary cortisol secretion among long-term MBSR Instructors. Complement Med Res. 2019;26(2):101–9. doi: 10.1159/000493124. [DOI] [PubMed] [Google Scholar]
- 37.Klimes-Dougan B, Chong LS, Samikoglu A, Thai M, Amatya P, Cullen KR, et al. Transcendental meditation and hypothalamic-pituitaryadrenal axis functioning: a pilot, randomized controlled trial with young adults. Stress. 2020 Jan;23(1):105–15. doi: 10.1080/10253890.2019.1656714. [DOI] [PubMed] [Google Scholar]
- 38.Delmonte MM. Biochemical indices associated with meditation practice: a literature review. Neurosci Biobehav Rev. 1985;9(4):557–61. doi: 10.1016/0149-7634(85)90002-8. [DOI] [PubMed] [Google Scholar]
- 39.Nagendra RP, Maruthai N, Kutty BM. Meditation and its regulatory role on sleep. Front Neurol. 2012;3:54. doi: 10.3389/fneur.2012.00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Silber MH, Ancoli-Israel S, Bonnet MH, Chokroverty S, GriggDamberger MM, Hirshkowitz M, et al. The visual scoring of sleep in adults. J Clin Sleep Med. 2007 Mar;3(2):121–31. [PubMed] [Google Scholar]
- 41.Almeida EA, Di Mascio P, Harumi T, Spence DW, Moscovitch A, Hardeland R, et al. Measurement of melatonin in body fluids: standards, protocols and procedures. Childs Nerv Syst. 2011 Jun;27(6):879–91. doi: 10.1007/s00381-010-1278-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Agarwal RP, Kumar A, Lewis JE. A pilot feasibility and acceptability study of yoga/meditation on the quality of life and markers of stress in persons living with HIV who also use crack cocaine. J Altern Complement Med. 2015 Mar;21(3):152–8. doi: 10.1089/acm.2014.0112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vera FM, Manzaneque JM, Maldonado EF, Carranque GA, Rodriguez FM, Blanca MJ, et al. Subjective sleep quality and hormonal modulation in long-term yoga practitioners. Biol Psychol. 2009 Jul;81(3):164–8. doi: 10.1016/j.biopsycho.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 44.Pascoe MC, Thompson DR, Ski CF. Meditation and endocrine health and wellbeing. Trends Endocrinol Metabol. 2020;31(7):469–77. doi: 10.1016/j.tem.2020.01.012. [DOI] [PubMed] [Google Scholar]
- 45.Jackowska M, Kumari M, Steptoe A. Sleep and biomarkers in the English Longitudinal Study of Ageing: associations with C-reactive protein, fibrinogen, dehydroepiandrosterone sulfate and hemoglobin. Psychoneuroendocrinology. 2013 Sep;38(9):1484–93. doi: 10.1016/j.psyneuen.2012.12.015. [DOI] [PubMed] [Google Scholar]
- 46.Makino S, Fujiwara M, Handa H, Fujie T, Aoki Y, Hashimoto K, et al. Plasma dehydroepiandrosterone sulphate and insulin-like growth factor I levels in obstructive sleep apnoea syndrome. Clin Endocrinol (Oxf) 2012 Apr;76(4):593–601. doi: 10.1111/j.1365-2265.2011.04237.x. [DOI] [PubMed] [Google Scholar]
- 47.Goh VH, Tong TY. Sleep, sex steroid hormones, sexual activities, and aging in Asian men. J Androl. 2010 Mar/Apr;31(2):131–7. doi: 10.2164/jandrol.109.007856. [DOI] [PubMed] [Google Scholar]
- 48.Sousa G, Schlüeter B, Menke T, Trowitzsch E, Andler W, Reinehr T. Relationships between polysomnographic variables, parameters of glucose metabolism, and serum androgens in obese adolescents with polycystic ovarian syndrome. J Sleep Res. 2011 Sep;20(3):472–8. doi: 10.1111/j.1365-2869.2010.00902.x. [DOI] [PubMed] [Google Scholar]
- 49.Schiffelholz T, Holsboer F, Lancel M. High doses of systemic DHEAsulfate do not affect sleep structure and elicit moderate changes in nonREM sleep EEG in rats. Physiol Behav. 2000 Jun;69(4-5):399–404. doi: 10.1016/s0031-9384(00)00218-3. [DOI] [PubMed] [Google Scholar]
- 50.Caufriez A, Leproult R, L’Hermite-Baleriaux M, Kerkhofs M, Copinschi G. Effects of a 3-week dehydroepiandrosterone administration on sleep, sex steroids and multiple 24-h hormonal profiles in postmenopausal women: a pilot study. Clin Endocrinol (Oxf) 2013;79(5):716–24. doi: 10.1111/cen.12201. [DOI] [PubMed] [Google Scholar]
- 51.Friess E, Trachsel L, Guldner J, Schier T, Steiger A, Holsboer F. DHEA administration increases rapid eye movement sleep and EEG power in the sigma frequency range. Am J Physiol. 1995 Jan;268(1):E107–13. doi: 10.1152/ajpendo.1995.268.1.E107. [DOI] [PubMed] [Google Scholar]
- 52.Goncharov NP, Katsiia GV, Nizhnik AN. Dehydroepiandrosterone and the cerebral functions. Vestn Ross Akad Med Nauk. 2006;(6):45–50. [PubMed] [Google Scholar]
- 53.Barrou Z, Charru P, Lidy C. Dehydroepiandrosterone (DHEA) and aging. Arch Gerontol Geriatr. 1997 May/Jun;24(3):233–41. doi: 10.1016/s0167-4943(96)00761-3. [DOI] [PubMed] [Google Scholar]
- 54.Yen SSC. Dehydroepiandrosterone sulfate and longevity: new clues for an old friend. Proc Natl Acad Sci. 2001 Jul;98(15):8167–9. doi: 10.1073/pnas.161278698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lindholm H, Ahlberg J, Sinisalo J, Hublin C, Hirvonen A, Partinen M, et al. Morning cortisol levels and perceived stress in irregular shift workers compared with regular daytime workers. Sleep Disord. 2012;2012:789274. doi: 10.1155/2012/789274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Duan H, Yuan Y, Zhang L, Qin S, Zhang K, Buchanan TW, et al. Chronic stress exposure decreases the cortisol awakening response in healthy young men. Stress. 2013 Nov;16(6):630–7. doi: 10.3109/10253890.2013.840579. [DOI] [PubMed] [Google Scholar]
- 57.Lovell B, Moss M, Wetherell MA. Perceived stress, common health complaints and diurnal patterns of cortisol secretion in young, otherwise healthy individuals. Horm Behav. 2011 Aug;60(3):301–5. doi: 10.1016/j.yhbeh.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 58.Fries E, Dettenborn L, Kirschbaum C. The cortisol awakening response (CAR): facts and future directions. Int J Psychophysiol. 2009 Apr;72(1):67–73. doi: 10.1016/j.ijpsycho.2008.03.014. [DOI] [PubMed] [Google Scholar]
- 59.Clow A, Hucklebridge F, Stalder T, Evans P, Thorn L. The cortisol awakening response: more than a measure of HPA axis function. Neurosci Biobehav Rev. 2010 Sep;35(1):97–103. doi: 10.1016/j.neubiorev.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 60.Guilliams TG, Edwards L. Chronic stress and the HPA axis. Standard. 2010;9(2):1–12. [Google Scholar]
- 61.Motzer SA, Hertig V. Stress, stress response, and health. Nurs Clin North Am. 2004 Mar;39(1):1–17. doi: 10.1016/j.cnur.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 62.Clow A, Law R, Evans P, Vallence AM, Hodyl NA, Goldsworthy MR, et al. Day differences in the cortisol awakening response predict day differences in synaptic plasticity in the brain. Stress. 2014 May;17(3):219–23. doi: 10.3109/10253890.2014.905533. [DOI] [PubMed] [Google Scholar]
- 63.Clow A, Hucklebridge F, Thorn L. The cortisol awakening response in context. Int Rev Neurobiol. 2010;93:153–75. doi: 10.1016/S0074-7742(10)93007-9. [DOI] [PubMed] [Google Scholar]
- 64.Kudielka B, Kirschbaum C. Awakening cortisol responses are influenced by health status and awakening time but not by menstrual cycle phase. Psychoneuroendocrinology. 2003 Jan;28(1):35–47. doi: 10.1016/s0306-4530(02)00008-2. [DOI] [PubMed] [Google Scholar]
- 65.Williams E, Magid K, Steptoe A. The impact of time of waking and concurrent subjective stress on the cortisol response to awakening. Psychoneuroendocrinology. 2005 Feb;30(2):139–48. doi: 10.1016/j.psyneuen.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 66.Wust S, Wolf J, Hellhammer DH, Federenko I, Schommer N, Kirschbaum C. The cortisol awakening response-normal values and confounds. Noise Health. 2000;2(7):79–88. [PubMed] [Google Scholar]
- 67.Petrowski K, Schmalbach B, Stalder T. Morning and evening type: the cortisol awakening response in a sleep laboratory. Psychoneuroendocrinology. 2020 Feb;112:104519. doi: 10.1016/j.psyneuen.2019.104519. [DOI] [PubMed] [Google Scholar]
- 68.Matousek RH, Pruessner JC, Dobkin PL. Changes in the cortisol awakening response (CAR) following participation in mindfulnessbased stress reduction in women who completed treatment for breast cancer. Complement Ther Clin Pract. 2011 May;17(2):65–70. doi: 10.1016/j.ctcp.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 69.Schmidt M, Naumann H, Weidler C, Schellenberg M, Anders S, Straub RH. Inflammation and sex hormone metabolism. Ann N Y Acad Sci. 2006 Jun;1069(1):236–46. doi: 10.1196/annals.1351.021. [DOI] [PubMed] [Google Scholar]
- 70.Ferrari E, Cravello L, Muzzoni B, Casarotti D, Paltro M, Solerte S, et al. Age-related changes of the hypothalamic-pituitary-adrenal axis: pathophysiological correlates. Eur J Endocrinol. 2001 Apr;144(4):319–29. doi: 10.1530/eje.0.1440319. [DOI] [PubMed] [Google Scholar]
- 71.Chida Y, Steptoe A. Cortisol awakening response and psychosocial factors: a systematic review and meta-analysis. Biol Psychol. 2009 Mar;80(3):265–78. doi: 10.1016/j.biopsycho.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 72.Pandi-Perumal SR, Srinivasan V, Maestroni GJM, Cardinali DP, Poeggeler B, Hardeland R. Melatonin: nature’s most versatile biological signal? FEBS J. 2006 Jul;273(13):2813–38. doi: 10.1111/j.1742-4658.2006.05322.x. [DOI] [PubMed] [Google Scholar]
- 73.Brzezinski A. Melatonin in humans. N Engl J Med. 1997 Jan;336(3):186–95. doi: 10.1056/NEJM199701163360306. [DOI] [PubMed] [Google Scholar]
- 74.Brzezinski A, Vangel MG, Wurtman RJ, Norrie G, Zhdanova I, BenShushan A, et al. Effects of exogenous melatonin on sleep: a metaanalysis. Sleep Med Rev. 2005 Feb;9(1):41–50. doi: 10.1016/j.smrv.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 75.Ferracioli-Oda E, Qawasmi A, Bloch MH. Meta-analysis: melatonin for the treatment of primary sleep disorders. PloS One. 2013 May;8(5):e63773. doi: 10.1371/journal.pone.0063773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shamir E, Laudon M, Barak Y, Anis Y, Rotenberg V, Elizur A, et al. Melatonin improves sleep quality of patients with chronic schizophrenia. J Clin Psychiatry. 2000 May;61(5):373–7. doi: 10.4088/jcp.v61n0509. [DOI] [PubMed] [Google Scholar]
- 77.Lemoine P, Nir T, Laudon M, Zisapel N. Prolonged-release melatonin improves sleep quality and morning alertness in insomnia patients aged 55 years and older and has no withdrawal effects. J Sleep Res. 2007 Dec;16(4):372–80. doi: 10.1111/j.1365-2869.2007.00613.x. [DOI] [PubMed] [Google Scholar]
- 78.Shilo L, Dagan Y, Smorjik Y, Weinberg U, Dolev S, Komptel B, et al. Effect of melatonin on sleep quality of COPD intensive care patients: a pilot study. Chronobiol Int. 2000 Jan;17(1):71–6. doi: 10.1081/cbi-100101033. [DOI] [PubMed] [Google Scholar]
- 79.Mendelson WB. Efficacy of melatonin as a hypnotic agent. J Biol Rhythms. 1997 Dec;12(6):651–6. doi: 10.1177/074873049701200621. [DOI] [PubMed] [Google Scholar]
- 80.Hughes RJ, Sack RL, Lewy AJ. The role of melatonin and circadian phase in age-related sleep maintenance insomnia: assessment in a clinical trial of melatonin replacement. Sleep. 1998;21(1):52–68. [PubMed] [Google Scholar]
- 81.Waldhauser F, Saletu B, Trinchard-Lugan I. Sleep laboratory investigations on hypnotic properties of melatonin. Psychopharmacology (Berl) 1990;100(2):222–6. doi: 10.1007/BF02244410. [DOI] [PubMed] [Google Scholar]
- 82.Hughes R, Badia P, French J, Santiago L, Plenzler S. Melatonin induced changes in body temperature and daytime sleep. Sleep Res. 1994;23:496. [Google Scholar]
- 83.James SP, Mendelson WB, Sack DA, Rosenthal NE, Wehr TA. The effect of melatonin on normal sleep. Neuropsychopharmacology. 1987;1(1):41–4. doi: 10.1016/0893-133x(87)90008-x. [DOI] [PubMed] [Google Scholar]
- 84.James SP, Sack DA, Rosenthal NE, Mendelson WB. Melatonin administration in insomnia. Neuropsychopharmacology. 1990 Feb;3(1):19–23. [PubMed] [Google Scholar]
- 85.Medeiros CAM, Bruin PFC, Lopes LA, Magalhães MC, Seabra ML, Bruin VMS. Effect of exogenous melatonin on sleep and motor dysfunction in Parkinson’s disease. J Neurol. 2007 Apr;254(4):459–64. doi: 10.1007/s00415-006-0390-x. [DOI] [PubMed] [Google Scholar]
- 86.Dawson D, Rogers NL, Van Den Heuvel CJ, Kennaway DJ, Lushington K. Effect of sustained nocturnal transbuccal melatonin administration on sleep and temperature in elderly insomniacs. J Biol Rhythms. 1998 Dec;13(6):532–8. doi: 10.1177/074873098129000354. [DOI] [PubMed] [Google Scholar]
- 87.Haimov I, Lavie P, Laudon M, Herer P, Vigder C, Zisapel N. Melatonin replacement therapy of elderly insomniacs. Sleep. 1995 Sep;18(7):598–603. doi: 10.1093/sleep/18.7.598. [DOI] [PubMed] [Google Scholar]
- 88.Rogers NL, Dinges DF, Kennaway DJ, Dawson D. Potential action of melatonin in insomnia. Sleep. 2003 Dec;26(8):1058–9. [PubMed] [Google Scholar]
- 89.Bujatti M, Biederer P. Serotonin, noradrenaline, dopamine metabolites in transcendental meditation-technique. J Neural Transm. 1976;39(3):257–67. doi: 10.1007/BF01256514. [DOI] [PubMed] [Google Scholar]
- 90.Liou CH, Hsieh CW, Hsieh CH, Chen JH, Wang CH, Lee SC. Studies of Chinese original quiet sitting by using functional magnetic resonance imaging. Conf Proc IEEE Eng Med Biol Soc. 2005;2005:5317–9. doi: 10.1109/IEMBS.2005.1615681. [DOI] [PubMed] [Google Scholar]
- 91.Pawlikowski M, Kolomecka M, Wojtczak A, Karasek M. Effects of six months melatonin treatment on sleep quality and serum concentrations of estradiol, cortisol, dehydroepiandrosterone sulfate, somatomedin C in elderly women. Neuro Endocrinol Lett. 2002;23(Suppl 1):S17–S9. [PubMed] [Google Scholar]
- 92.Elias AN, Wilson AF. Serum hormonal concentrations following transcendental meditation-- potential role of gamma aminobutyric acid. Med Hypotheses. 1995 Apr;44(4):287–91. doi: 10.1016/0306-9877(95)90181-7. [DOI] [PubMed] [Google Scholar]
- 93.Guglietti CL, Daskalakis ZJ, Radhu N, Fitzgerald PB, Ritvo P. Meditation-related increases in GABAB modulated cortical inhibition. Brain Stimul. 2013 May;6(3):397–402. doi: 10.1016/j.brs.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 94.Streeter CC, Jensen JE, Perlmutter RM, Cabral HJ, Tian H, Terhune DB, et al. Yoga Asana sessions increase brain GABA levels: a pilot study. J Altern Complement Med. 2007 May;13(4):419–26. doi: 10.1089/acm.2007.6338. [DOI] [PubMed] [Google Scholar]
- 95.MacLean CR, Walton KG, Wenneberg SR, Levitsky DK, Mandarino JP, Waziri R, et al. Effects of the transcendental meditation program on adaptive mechanisms: changes in hormone levels and responses to stress after 4 months of practice. Psychoneuroendocrinology. 1997 May;22(4):277–95. doi: 10.1016/s0306-4530(97)00003-6. [DOI] [PubMed] [Google Scholar]
- 96.Cooper R, Joffe B, Lamprey J, Botha A, Shires R, Baker S, et al. Hormonal and biochemical responses to transcendental meditation. Postgrad Med J. 1985 Apr;61(714):301–4. doi: 10.1136/pgmj.61.714.301. [DOI] [PMC free article] [PubMed] [Google Scholar]


