Abstract
Objective:
Guided by the Operating Conditions Framework, the goal of this study was to identify how and for whom an online sexual health program called Health Education and Relationship Training (HEART) worked.
Design:
Data come from a randomized controlled trial among 198 U.S. high school girls who completed HEART or an attention-matched control. We conducted mediation and moderated mediation models to determine if sexual self-efficacy was a mediator and if program acceptability and sexual activity status were moderators of HEART efficacy.
Main Outcome Measure:
Sexual communication skills were assessed with a behavioral role-play task.
Results:
HEART significantly improved sexual communication skills. These effects were fully mediated through sexual self-efficacy. Specifically, HEART improved sexual self-efficacy which in turn increased sexual communication skills. Also, when participants liked the program more, the effect of HEART on sexual self-efficacy was stronger. Further, among girls who had engaged in sexual activity, sexual self-efficacy was significantly associated with sexual communication skills.
Conclusion:
This study provides insights into the mechanisms of behavior change underlying HEART. Results highlight the need to further “unpack” the effects of other sexual health programs, as we showed that programs may work better under certain conditions.
Keywords: sexual communication, sexual self-efficacy, program acceptability, adolescent sexual health, moderated mediation
A growing body of research calls for behavioral and intervention research to move beyond a focus on testing the main effects of interventions, as intervention effects often vary across sub-groups and contexts (Bryan et al., 2021; Kenny & Judd, 2019). Understanding how and for whom an intervention works are critical next steps that can inform program theory, development, and broader implementation (Bryan et al., 2021; Rothman & Sheeran, 2020). Sexual health interventions are important for adolescents. They can provide knowledge and skills to help girls prevent sexually transmitted infections (STIs), HIV, and unplanned pregnancy, and they can promote optimal sexual health outcomes (for reviews, see Hall et al., 2016; Widman et al., 2018). Yet, research on how and for whom these sexual health programs work is more sparse (Morales et al., 2018). Thus, the purpose of this study is to extend the findings of one evidence-based sexual health promotion program developed for adolescent girls, called Health Education and Relationship Training (HEART; Widman et al., 2016). Specifically, we will examine if HEART: 1) improves sexual communication skills through sexual self-efficacy (i.e., test of mediation) and 2) works better or worse for certain adolescents based on their sexual activity status and endorsement of program acceptability (i.e., tests of moderation).
Program Mediator: Sexual Self-Efficacy
Sexual self-efficacy is a person’s confidence in their ability to manage sexual situations, including refusing unwanted sexual activities and negotiating sexual experiences with partners (Brar et al., 2020). Sexual self-efficacy is a construct situated within social cognitive theory, which suggests that self-efficacy, or a person’s beliefs about their ability to perform a behavior is the antecedent to behavioral action (Bandura, 1986; Fishbein & Ajzen, 2009). Self-efficacy is important because if people believe that they have agency to change a health behavior they are more likely to succeed, even in the face of challenges (Bandura, 1986). For example, previous literature has shown that contraception self-efficacy has been linked to contraceptive use at last sexual intercourse (Sieving et al., 2007) and condom self-efficacy has been linked to condom use (Crosby et al., 2013). Additionally, resistive efficacy has been linked with fewer sexual partners (Mitchell et al., 2005). Given the association between sexual self-efficacy and other sexual behaviors, we hypothesize that sexual self-efficacy could be a predictor of sexual communication. Understanding whether sexual self-efficacy is the mediator driving the increase of sexual communication seen in HEART may be critical for future adaptations of this specific program. In addition, it could inform the development of other sexual health promotion programs. More specifically, this knowledge provides critical insight for researchers and practitioners on the proximal role of sexual self-efficacy as an important ingredient to behavior change in sexual health promotion programs.
Program Outcome: Sexual Communication
Sexual communication is an exchange of verbal and nonverbal messages between partners about sexual beliefs or behaviors (Warren & Warren, 2015). Sexual communication is an important skill that adolescents can use to refuse unsafe sex behaviors and assertively communicate their sexual boundaries and preferences with a partner (Noar et al., 2006; Schmid et al., 2015). For example, assertive sexual communication among adolescents has been associated with increased condom and contraceptive use among adolescents (Gause et al., 2018; Lalas et al., 2020; Widman et al., 2014). Given the importance of developing sexual communication skills among adolescents, HEART was developed to increase adolescent girls’ skills to communicate assertively about sexual health topics and refuse unsafe sexual behaviors.
Moderators of the Mediation Pathway: Program Acceptability and Sexual Activity Status
There are numerous factors at the intervention-level that may moderate the impact of an intervention (Proctor et al., 2011; Rothman & Sheeran, 2020). The acceptability of an intervention – defined as affective attitudes toward an intervention (e.g., likeability; Sekhon et al., 2017) – is one such factor with important implications for program uptake. Participants who like an intervention may be more likely to fully engage with program content and internalize program messages, thereby improving their treatment outcomes (Fodor et al., 2020). Thus, in this study we will examine program acceptability as a potential intervention-level moderator of HEART.
We will also examine sexual activity status as a moderator. The Precaution Adoption Process Model (Weinstein et al., 2008) provides theoretical grounding for examining sexual activity status as a moderator. This model suggests that people make decisions about health behavior change only after they have become knowledgeable and then engaged by a particular issue. In line with this theory, adolescents who are sexually active demonstrate higher levels of sexual communication with both their partners and their peers compared to adolescents who are not sexually active (Widman et al., 2014). In the context of this study, it is possible that only participants who are sexually active have the experience and context needed to move to the next stage of behavior change and decide to engage in sexual communication with a partner. Whereas participants who are not sexually active may have less confidence or skills to communicate with a partner as they have had fewer opportunities to practice these communication skills. Thus, it is plausible that sexual activity may moderate both paths of the mediation model (see Figure 1).
Figure 1.
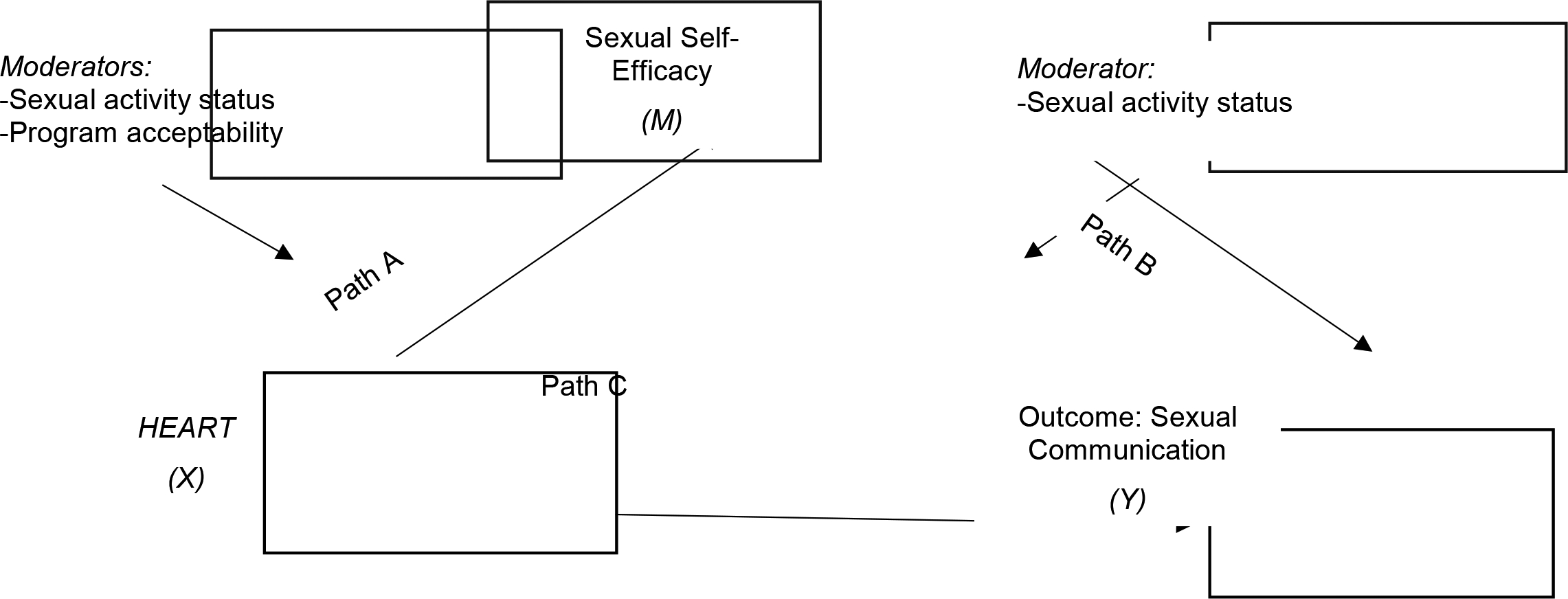
Conceptual Model of Moderated Mediation Adapted from Rothman & Sheeran, 2020
Theoretical Underpinning and Objectives of this Study
Two critical next steps after determining the efficacy of any program are to identify the mechanism underlying the intervention outcomes (e.g., mediators) and to determine for whom the intervention is most effective (e.g., moderators; Lightfoot, 2012; Rothman & Sheeran, 2020). The theoretical underpinning for this study is the Operating Conditions Framework (Rothman & Sheeran, 2020), which posits that there is need for an evidence base that explains both the mediating mechanisms underlying interventions and the moderating conditions under which interventions are effective. According to the Operating Conditions Framework, the first step is to examine mediators driving the main outcome. Second, researchers must explore intervention moderation in two parts as shown in Figure 1: (1) What factors influence the impact of the intervention on the mediator (path A)? (2) What factors influence the impact of the mediator on the behavior/outcome (path B)? The analytic process guided by this framework allows us to unpack the mechanism of change and understand who the program works for.
First, we examined whether sexual self-efficacy mediates the effect of the intervention on a behavioral measure of sexual communication skills. In other words, was sexual self-efficacy the component of HEART responsible for changes in sexual communication skills. Next, we examined moderators on both pathways of the mediation model. We examined sexual activity status as a moderator on: 1) path A from HEART to sexual self-efficacy (Figure 1) and 2) path B from sexual self-efficacy to sexual communication among the full sample of adolescents (Figure 1). In other words, was HEART more effective for sexually active participants and participants who liked the program more. We assessed program acceptability as a moderator only on path A from HEART to the mediator variable.1 The hypotheses we examine are:
Figure 2.
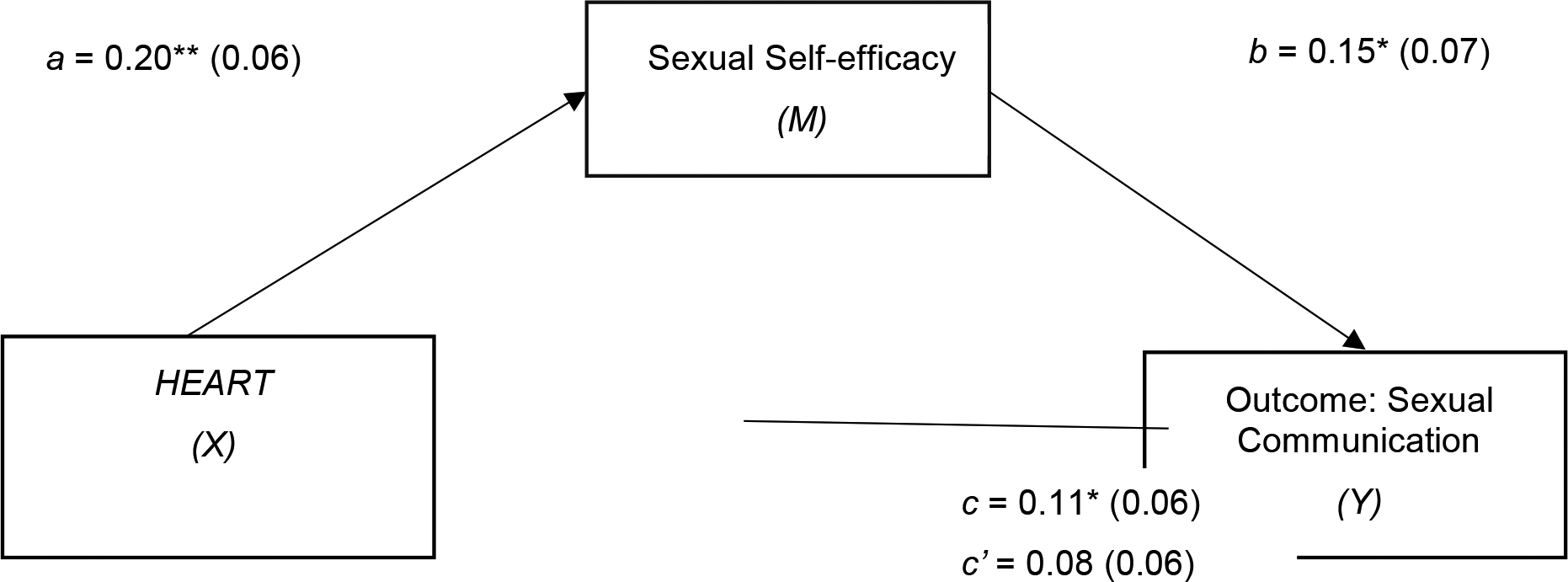
Mediating Effect of Sexual Self-efficacy in the Association Between HEART and Sexual Communication
Note. n = 197; all presented effects are unstandardized; a is the effect of HEART on sexual self-efficacy; participants in HEART are coded as 1 and control group participants as 0; b is the effect of sexual self-efficacy on sexual communication; c’ is the direct effect of HEART on sexual communication; c is the total effect of HEART on sexual communication.
*p < .05, **p < .01
Hypothesis 1: Sexual self-efficacy will mediate the program effects on sexual communication.
Hypothesis 2: Program acceptability will moderate the effect of HEART on sexual self-efficacy. Specifically, the association between HEART and sexual self-efficacy will be stronger among participants who liked the program more.
Hypothesis 3: Sexual activity status will moderate the effect of the HEART on sexual self-efficacy and the effect of sexual self-efficacy on sexual communication. Specifically, the associations between the HEART and sexual self-efficacy and sexual self-efficacy and sexual communication will be stronger among sexually active participants.
Methodology
HEART Overview and Objectives
HEART is a brief online program grounded in health behavior change and developmental theory (Fishbein & Ajzen, 2010; Reyna & Brainerd, 2011). The program targets five domains of sexual health behavior change: 1) safer sex motivation, 2) STI/HIV knowledge, 3) sexual attitudes and norms, 4) safer sex self-efficacy, and 5) sexual communication skills. Sexual communication skills are emphasized throughout the program, but particularly in the communication module where users receive didactic training and modeling from same-age peers. Users can also practice skills through an audio-recording and playback feature (Widman et al., 2016). HEART has now been evaluated in several studies with nearly 1,000 adolescents, with results demonstrating improvements in sexual communication skills, along with several secondary outcomes (e.g., sexual self-efficacy, safer sex attitudes and beliefs, and communication and condom intentions; Javidi et al., 2021; Kamke et al., 2020; Widman et al., 2020; Widman, Golin, et al., 2018).
Participants and Procedure
We recruited participants from four rural, low-income high schools in the southeastern United States to take part in HEART (Widman, Golin, et al., 2018). We randomly assigned participants to the sexual health promotion program or an attention-matched control (clinicaltrials.gov registration number: NCT02579135). An investigator not associated with the study team conducted random assignment by using random sampling and allocation procedures in SPSS. Randomization was stratified within school and based on participants’ sexual activity status that was obtained during the pretest. Further details of methods and results of the randomized control trial study have been published elsewhere (Widman, Golin, et al., 2018). We invited all 10th grade girls (n = 371) to participate in the study. Of these girls, 229 received written parental consent for the study and 222 girls provided written assent. Only participants whom we obtained consent and assent were eligible to participate. After we obtained parental consent and student assent, participants completed confidential pre-test and immediate post-test surveys using computer-assisted self-interviews (CASIs) in a small-group classroom setting. CASIs have been shown to reduce social desirability biases and increase the validity of self-report data when collecting sensitive data about sexual behavior from youth (Dolezal et al., 2012). Of the 222 girls from whom we obtained consent and assent, 24 participants were excluded because they did not follow directions for the sexual communication behavioral skills activity and were missing data on this key outcome assessment. There were no differences in sexual self-efficacy, program acceptability, or sexual activity status between participants who completed the sexual communication behavioral skills measure versus those who did not complete the measure (all ps > .20). Thus, our final analytic sample for this study is 198 girls. The University Institutional Review Board approved all study procedures.
Instruments
Participant Characteristics.
Participants self-reported several demographic characteristics in a pre-test survey using a CASI. Data collected included their age, race/ethnicity, sexual orientation, whether they had a current or recent dating partner (defined as someone they are dating casually, a sexual relationship, or a boyfriend or girlfriend), or had ever had vaginal sexual intercourse.
Sexual Self-Efficacy.
Ten items from the Self-Efficacy for HIV Prevention Scale (Brown et al., 2014) were used to assess participants self-efficacy for sexual communication and condom use. We collected data using a CASI and used the immediate post-test measure of sexual self-efficacy in study analyses. Seven items assessed participants self-efficacy for sexual communication (e.g., “How sure are you that you could talk to your partner about safer sex?”) and three items assessed self-efficacy for obtaining and using condoms (e.g., “How sure are you that you could have condoms available when you need them?”). Participants responded on a 4-point Likert scale from 1 = (Couldn’t do it) to 4 = (Very sure). We averaged the item responses to create an overall sexual self-efficacy measure (Cronbach’s α = .79), with higher scores indicating greater sexual self-efficacy.
Behavioral Assessment of Assertive Sexual Communication Skills.
Participants’ communication skills at refusing unwanted sexual activity and negotiating condom use were assessed with an audio-recorded role-play methodology adapted from a validated behavioral assessment (Forsyth et al., 1997). This behavioral assessment was originally developed and tested among undergraduate students where they listened to five audiotaped scenarios and were scored across four dimensions; all scores were reliable (kappas .76 to .90) and it was determined to be an effective behavioral measure of assertive communication (Forsyth et al., 1997). In this study, participants listened to and responded out loud to 3-role play scenarios. An example of a scenario was: “You’ve been with your boyfriend for several months. He wants to have sex but you’re not ready. He says, ‘I know you want to wait to have sex, but haven’t we waited long enough? I really think it will make our relationship stronger.’” Responses were recorded, transcribed, and rated on 3 dimensions (Forsyth et al., 1997; Gordon et al., 1997): (1) refusal of unsafe behavior, (2) providing a reason for the refusal, and (3) verbal assertiveness. The range for each code included: 0 = absent; 1 = moderate; 2 = high. Four trained coders masked to study condition coded the responses (interrater reliability = 84%). We averaged scores across codes to obtain an index of sexual communication skills. We used the immediate post-test measure of sexual communication skills in study analyses.
Sexual Activity Status.
Participants self-reported their sexual activity status in a pre-test survey using a CASI. Sexual activity was assessed with one question, “Have you ever engaged in sexual activity (like sexual touching, oral sex, or sexual intercourse)?” with answer choices 0 (No) and 1 (Yes). The instructions for this question about sexual activity explicitly asked participants to report only consensual sexual activity.
Program Acceptability.
Participants self-reported whether they liked the program in an immediate post-test survey using a CASI. Participants answered one question to assess program acceptability: “How much did you like the program?” They rated this item on a 4-point Likert-type scale from 0 (Not at all) to 3 (A lot).
Analysis Plan
First, we conducted descriptive analyses to characterize the sample. Second, in line with the Operating Conditions Framework (Figure 1), we ran mediation and moderated mediation models in SPSS using the PROCESS macro version 3.5 developed by Hayes (Hayes, 2017). Mediation analysis was selected because we wanted to understand whether sexual self-efficacy explained the relationship between HEART and sexual communication skills. Moderated mediation analysis was selected as we wanted to understand whether the moderators affect the strength of the relationship between HEART and sexual self-efficacy (mediator) in addition to the relationship between sexual self-efficacy (mediator) and sexual communication (outcome). PROCESS macro was selected for analysis as this approach uses a percentile bootstrap confidence interval – an approach that has become the widely recommended method for making an inference about an indirect effect while balancing power and validity considerations (Hayes, 2017). We selected 95% confidence intervals to determine significance of the indirect effect and had confidence intervals resampled 5000 times for each analysis (Hayes, 2017). To test our first hypothesis, we selected Hayes’ Model 4 and entered the intervention condition as the independent variable, sexual self-efficacy measured at post-test as the potential mediator, and sexual communication skills measured at post-test as the dependent variable (Hayes, 2017). To test our second hypothesis, we used Hayes’ Model 7 to test moderated mediation on path A for program acceptability. To test our third hypothesis, we selected Hayes’ Model 58 to test moderated mediation on paths A and B for sexual activity status. The moderated mediation models in PROCESS is a justified statistical technique when attempting to model the mechanisms linking X to Y (i.e., HEART to sexual communication) while simultaneously allowing those effects to be contingent on individual differences (Hayes, 2017). For both moderated mediation models, we entered the intervention condition as the independent variable, sexual self-efficacy as the mediator, sexual communication as the dependent variable, and the moderator variable. We mean centered all continuous predictors for the moderated mediation models. Lastly, we used a pick-a-point approach and computed simple slopes to estimate the conditional effect of each independent variable on the outcome or mediator variable (Hayes, 2017). In total, one mediation model and two moderated mediation models were conducted.
Results
Sample Characteristics
Participants were between the ages of 14–17 (Mage = 15.3 years; SD = 0.49). As shown in the top of Table 1, the sample was racially/ethnically diverse including 37.9% White, 30.3% Latina, 23.2% Black, 8.6% other or mixed race/ethnicity. Most participants (78.7%) identified their sexual orientation as heterosexual, and half of participants (50.5%) reported having a dating partner in the past three months. Further, 23.4% had ever engaged in vaginal intercourse and 41.6% had ever engaged in any form of sexual activity.
Table 1.
Participant Characteristics and Study Variables
| Variable | Full Sample (n = 198) |
HEART (n = 104) |
Control Program (n = 94) |
|---|---|---|---|
| Descriptive Characteristics | % | % | % |
| Race/Ethnicity | |||
| White | 37.9% | 35.6% | 40.4% |
| Latina | 30.3% | 29.8% | 30.9% |
| Black | 23.2% | 26.9% | 19.1% |
| Other/Mixed | 8.6% | 7.7% | 9.6% |
| Sexual Orientation | |||
| Heterosexual | 78.7% | 78.8% | 78.5% |
| Bisexual | 13.2% | 11.5% | 15.1% |
| Lesbian | 4.1% | 3.8% | 4.3% |
| Other | 4.1% | 5.8% | 2.2% |
| Current dating Partner | 50.5% | 52.9% | 47.9% |
| Had vaginal sexual intercourse | 23.4% | 25.2% | 21.3% |
| Age - M (SD) | 15.25 (0.49) | 15.26 (0.48) | 15.23 (0.50) |
| Primary Study Variables | M (SD) | M (SD) | M (SD) |
| Sexual Communication Skills | 1.12 (0.40) | 1.17 (0.38) | 1.06 (0.42) |
| Sexual Self-Efficacy | 3.27 (0.44) | 3.37 (0.45) | 3.17 (0.41) |
| Sexually Active | 41.6% | 41.8% | 41.5% |
| Program Acceptability | 2.41 (0.66) | 2.51 (0.59) | 2.30 (0.72) |
Note. Sexual communication skills, sexual self-efficacy, and program acceptability were measured at immediate posttest; all other variables were measured at pre-test. Had vaginal sexual intercourse defined as ever having vaginal sex. Sexually active defined as ever having engaged in sexual activity (sexual touching, oral sex, intercourse).
Mediation Results
Compared to the control, we found HEART was efficacious at improving sexual communication skills (b = .11, SE =.06, p = .049). Further, the results indicated that the HEART was a significant predictor of sexual self-efficacy (b = 0.20, SE = 0.06, p = .001), and that sexual self-efficacy was a significant predictor of sexual communication (b = 0.15, SE = 0.07, p = .028). HEART was no longer a significant predictor of sexual communication after controlling for the mediator, sexual self-efficacy (b = 0.08, SE = 0.06, p = .15), indicating full mediation. The indirect effect was tested using a percentile bootstrap with 5000 samples. These results indicated that the indirect effect of X on Y was significant, b = 0.03, Boot SE = 0.02, 95% CI = .0017, .0690 (Figure 2).
Moderated Mediation Results
Program Acceptability
The interaction between the intervention group and program acceptability was significant (b = 0.24, SE = 0.09, p = .013), suggesting that how much participants liked the program impacted the effects of HEART on sexual self-efficacy (Table 2). For participants who liked the program more (1 SD above the mean), the effect of the intervention on sexual self-efficacy was positive and significant (b = 0.33, SE = 0.08, p = .0001). In contrast, among participants who liked the program less (1 SD below the mean), the effect was not significant (b = −0.66, SE = 0.09, p = .73; Figure 3).
Table 2.
Moderated Mediation Model: Examining Paths A and B
| Sexual Activity Status n = 196 |
Program Acceptability n = 195 |
|||
|---|---|---|---|---|
| Mediator Model: Path A | b (SE) | t | b (SE) | t |
| Constant | −0.11 (0.06) | −1.91 | 3.16 (0.05) | 69.90*** |
| Intervention | 0.20 (0.08) | 2.48* | 0.19 (0.06) | 3.02** |
| Moderatora | 0.02 (0.09) | 0.18 | −0.06 (0.06) | −0.95 |
| Intervention x Moderatora | −0.00 (0.13) | −0.00 | 0.24 (0.09) | 2.50* |
| Outcome Model: Path B | ||||
| Constant | 1.06 (0.05) | 22.17*** | ||
| Intervention | 0.09 (0.06) | 1.55 | ||
| Sexual Self-Efficacy | 0.03 (0.08) | 0.33 | ||
| Moderator – Sexual Activity Status | 0.04 (0.06) | 0.62 | ||
| Sexual Self-Efficacy x Sexual Activity Status | 0.28 (0.13) | 2.16* | ||
| Conditional Effects of Sexual Self-Efficacy at Values of Sexual Activity Status | Conditional Effects of HEART at Values of Program Acceptability | |||||||
|---|---|---|---|---|---|---|---|---|
| b (SE) | LLCI | ULCI | b (SE) | LLCI | ULCI | |||
| Not sexually active | 0.03 (0.08) | −0.14 | 0.19 | −1 SD (−0.66) | 0.03 (0.09) | −0.14 | 0.21 | |
| Sexually active | 0.31 (0.10) | 0.11 | 0.50 | Mean (0.00) | 0.19 (0.06) | 0.06 | 0.31 | |
| +1 SD (0.59) | 0.33 (0.08) | 0.16 | 0.49 | |||||
Note. Unstandardized coefficients are reported. Bootstrap sample size = 5000. The mediator model (path A, Figure 1) is presented first, followed by the outcome model (path B, Figure 1) second. The two moderators are listed across the top of the table. The bottom half of the table contains the conditional effects of the moderators for significant interactions. LL = low limit. UL = upper limit. CI = confidence interval.
Corresponds to either sexual activity status or program acceptability depending on column.
p < .05,
p < .01;
p < .001
Figure 3.
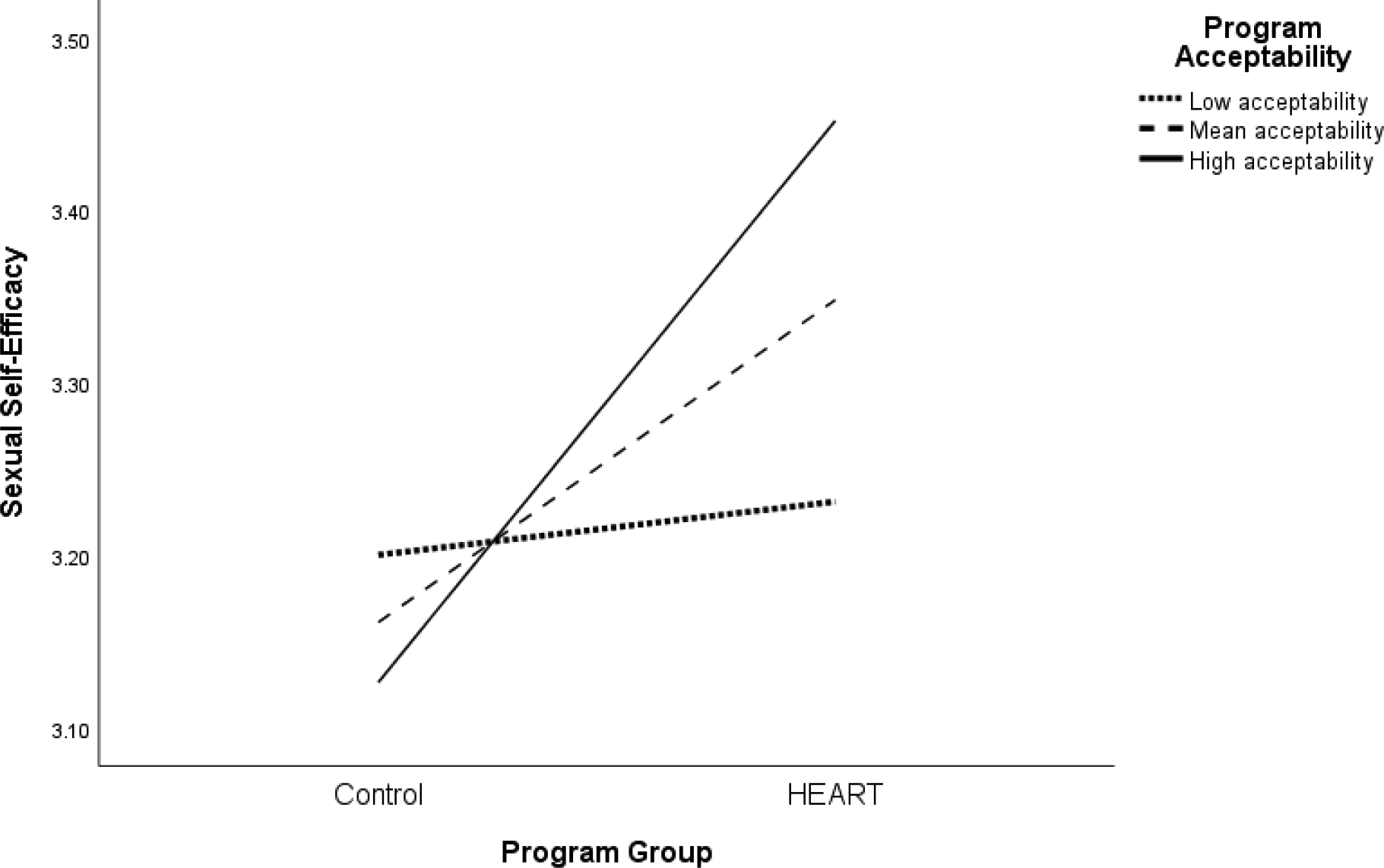
The Association Between the Program Condition (Predictor) and Sexual Self-efficacy (Mediator) by Program Acceptability (Moderator)
Sexual Activity
The interaction between the intervention group and sexual activity status on sexual self-efficacy was not statistically significant (b = −0.00, SE = 0.13, p = .997), indicating that HEART was equally efficacious at improving sexual self-efficacy for girls who were sexually active and those who were not yet sexually active. However, the interaction on the second path between self-efficacy and sexual communication was significant (b = 0.28, SE= 0.13, p = .032), indicating that sexual activity status moderated the association between sexual self-efficacy and sexual communication (Table 2). Simple slope tests indicated that among girls who had engaged in sexual activity, sexual self-efficacy was significantly associated with sexual communication (b = 0.31, SE = 0.10, p =.003). In contrast, among girls who had never engaged in sexual activity, sexual self-efficacy was not significantly associated with sexual communication (b = 0.03, SE= 0.08, p = .74; Figure 4).
Figure 4.
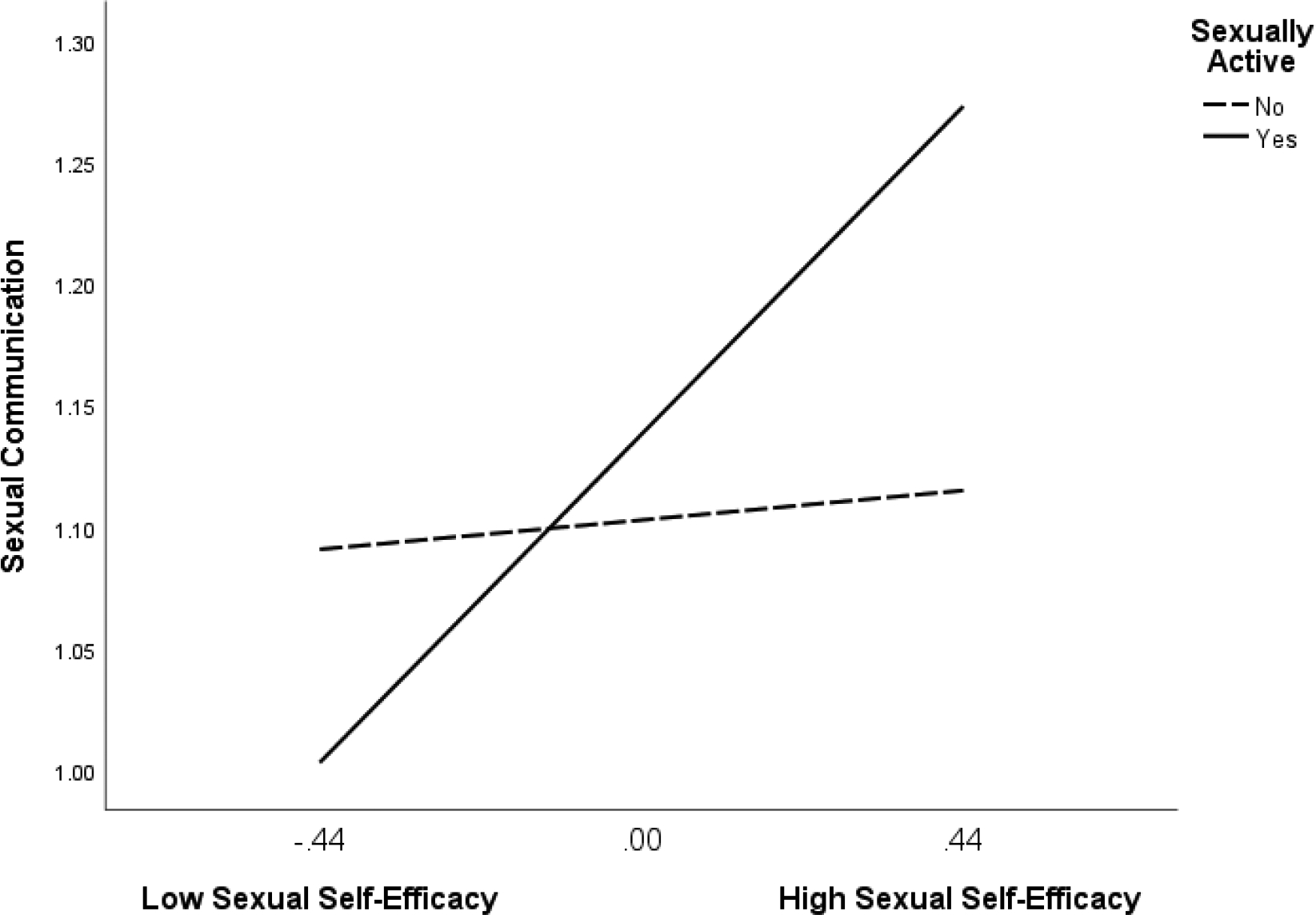
The Association Between Sexual Self-efficacy (Mediator) and Sexual Communication (Outcome) by Whether Teens Have Ever Engaged in Sexual Activity (Moderator)
Discussion
When adolescents receive comprehensive sex education, they feel more informed, make safer choices, and learn the sexual communication skills they need to advocate for their sexual health outcomes (Evans et al., 2020; Morales et al., 2018). The Operating Conditions Framework calls for more detailed analyses of program effects to examine the mechanism of behavior change and the conditional nature of this process (Rothman & Sheeran, 2020). Determining how a sexual health promotion program works and whether a program has different effects based on relevant factors provides critical information for program design, implementation, and efficacy (Hayes, 2017; Rothman & Sheeran, 2020). The purpose of this study was to determine if sexual self-efficacy was a significant mediator of one sexual health program, HEART, on sexual communication skills. In addition, we examined program acceptability and sexual activity status as moderators. We found a mediating effect of sexual self-efficacy on sexual communication and evidence of moderated mediation for program acceptability and sexual activity status.
The mediating effect of sexual self-efficacy is consistent with literature suggesting that sexual self-efficacy is a proximal cognitive predictor of sexual communication (Fishbein & Ajzen, 2009; Quinn-Nilas et al., 2016). Further, this finding complements empirical research showing that self-efficacy related to a variety of sexual behaviors (e.g., contraception self-efficacy, condom use self-efficacy, resistive self-efficacy) are predictors of the target sexual behavior (Crosby et al., 2013; Mitchell et al., 2005; Sieving et al., 2007). Practitioners could focus on increasing adolescent girls’ confidence in their ability to communicate about sexual topics through strategies such as role-plays, observational learning and modeling, and positive feedback (Boone et al., 2015; Javier et al., 2018); this confidence should in turn impact their actual sexual communication skills.
Additionally, we found evidence of moderated mediation for program acceptability and sexual activity status. On the first path of the mediation model from HEART to sexual self-efficacy (path A, Figure 1), we found that the program was more effective among adolescents who liked the HEART more. Researchers tend to examine acceptability of an intervention separately from efficacy; however, this result suggests that whether adolescents like the program also impacts the efficacy of a program. Future work should consider tailoring interventions so that they are acceptable to diverse groups of adolescents as this may impact the sexual health outcomes of the program.
We did not find evidence of moderation on the first path of the mediation model from HEART to sexual self-efficacy (path A, Figure 1) for sexual activity status. This finding indicates that the HEART is equally effective at increasing sexual self-efficacy among adolescent girls regardless of whether they are sexually active. This is important as it suggests that sexual health promotion programs can increase adolescent girls’ confidence in their ability to advocate for their sexual health before they become involved in sexual relationships.
On the second path of the mediation model from sexual self-efficacy to sexual communication (path B, Figure 1), we found that among sexually active girls, sexual self-efficacy was significantly associated with sexual communication. This finding indicates that increasing girls’ confidence in their ability to communicate with a sexual partner is a particularly effective strategy among girls who are sexually active. This is critical as girls who are sexually active may be the most in need of communication skills to communicate with a partner about safe sex (Shannon & Klausner, 2018). However, among girls who are not sexually active, sexual self-efficacy does not appear to be associated with sexual communication skill development. A possible explanation is that girls who are not yet sexually active do not have the prior relationship context and experience communicating about sexual topics with a partner; thus merely having higher sexual self-efficacy does not translate to sexual communication skills (Weinstein et al., 2008). Researchers and practitioners should consider increasing the confidence of sexually active girls to communicate about sex to aid in the development of sexual communication skills. More broadly, this study provides evidence of the need for researchers and practitioners to understand which underserved groups of people are not deriving benefit from intervention content. This information could inform adaptations and tailoring of sexual health interventions.
Limitations and Future Directions
This study has limitations that should be considered. First, the mediation analyses were conducted using pre and immediate post-test data and thus no conclusions about the role of sexual self-efficacy on sexual communication over time can be drawn. Longitudinal and experimental research are needed to tease out causality and how long intervention effects persist. Second, this sample includes only girls, of which the majority identified as heterosexual. Thus, future research examining this model among a more diverse sample of adolescents including boys and LGBTQ+ adolescents may be warranted. Research examining sexual communication skills specifically among LGBTQ+ adolescents is sparse and could be an important area to elucidate, given the significant sexual health disparities that LGBTQ+ adolescents experience (Centers for Disease Control and Prevention, 2019; Hafeez et al., 2017). Third, this study focused on understanding the effects of a sexual health intervention among individual adolescents. Since adolescents make sexual decisions within the context of dyadic relationships, future research would benefit from examining more robust dyadic factors. For example, trust and power differentials in relationships have been shown to significantly affect sexual communication and subsequent sexual health behaviors, such as condom use (Fortenberry, 2019; VanderDrift et al., 2013). Fourth, future research should consider the role of health risk perception literature, which suggests that when interventions change risk perceptions, they alter health behavior (Ferrer & Klein, 2015). More specifically, this literature indicates that self-efficacy is an important predictor of risk perception and people that have higher self-efficacy are more likely to actually adhere to health behaviors (Commodari et al., 2020; Ferrer & Klein, 2015). Thus, exploring the role of health risk perception and self-efficacy on adolescent sexual communication may be warranted.
Conclusion
Understanding how and for whom a program work are critical next steps for intervention science (Bryan et al., 2021; Lightfoot, 2012; Rothman & Sheeran, 2020). This study identified sexual self-efficacy as a cognitive mechanism underlying sexual communication skill development among girls who completed a sexual health program. Program acceptability and sexual activity status were also identified as significant moderators of treatment effects. We showed that programs may work better under certain conditions – when youth have higher sexual self-efficacy, like the program more, and for youth who are already sexually active. Understanding who is not benefitting from a program could inform adaptations of interventions.
Funding
This project was supported by NIH grants K99/R00 HD075654 and K24 HD069204. Clinicaltrials.gov registration number: NCT02579135
Footnotes
We assessed program acceptability only on path A from PROGRAM to the mediator variable because it is an intervention-specific factor and thus not interpretable and relevant if analyzed among path B, which is among the full sample.
Disclosure of Interest
The authors report no conflicts of interest.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, JB, upon reasonable request. The data are not publicly available due to restrictions from the North Carolina State University IRB.
References
- Bandura A (1986). Social foundations of thought and action: A social cognitive theory (pp. xiii, 617). Prentice-Hall, Inc. [Google Scholar]
- Boone MR, Cherenack EM, Wilson PA, & ATN 086/106 Protocol Team. (2015). Self-Efficacy for Sexual Risk Reduction and Partner HIV Status as Correlates of Sexual Risk Behavior Among HIV-Positive Adolescent Girls and Women. AIDS Patient Care and STDs, 29(6), 346–353. 10.1089/apc.2014.0175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brar P, Dworkin J, & Brady SS (2020). Adolescent Women’s Sexual Self-Efficacy: Associations with Personal and Perceived Partner Beliefs That Condoms Interfere with Pleasure. American Journal of Sexuality Education, 15(3), 336–356. 10.1080/15546128.2020.1763882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LK, Hadley W, Donenberg GR, DiClemente RJ, Lescano C, Lang D, Crosby R, Barker D, & Oster D (2014). Project STYLE: a multisite RCT for HIV prevention among youths in mental health treatment. Psychiatric Services, 65(3), 338–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan CJ, Tipton E, & Yeager DS (2021). Behavioural science is unlikely to change the world without a heterogeneity revolution. Nature Human Behaviour, 5(8), 980–989. 10.1038/s41562-021-01143-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2019, December 27). Health Considerations for LGBTQ Youth. https://www.cdc.gov/healthyyouth/disparities/health-considerations-lgbtq-youth.htm
- Commodari E, La Rosa VL, & Coniglio MA (2020). Health risk perceptions in the era of the new coronavirus: Are the Italian people ready for a novel virus? A cross-sectional study on perceived personal and comparative susceptibility for infectious diseases. Public Health, 187, 8–14. 10.1016/j.puhe.2020.07.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crosby RA, DiClemente RJ, Salazar LF, Wingood GM, McDermott-Sales J, Young AM, & Rose E (2013). Predictors of consistent condom use among young African American women. AIDS and Behavior, 17(3), 865–871. 10.1007/s10461-011-9998-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolezal C, Marhefka SL, Santamaria EK, Leu C-S, Brackis-Cott E, & Mellins CA (2012). A Comparison of Audio Computer-Assisted Self-Interviews to Face-to-Face Interviews of Sexual Behavior Among Perinatally HIV-Exposed Youth. Archives of Sexual Behavior, 41(2), 401–410. 10.1007/s10508-011-9769-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans R, Widman L, Stokes M, Javidi H, Hope E, & Brasileiro J (2020). Sexual Health Programs for Latinx Adolescents: A Meta-analysis. Pediatrics, 146(1). 10.1542/peds.2019-3572 [DOI] [PubMed] [Google Scholar]
- Ferrer R, & Klein WM (2015). Risk perceptions and health behavior. Current Opinion in Psychology, 5, 85–89. 10.1016/j.copsyc.2015.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishbein M, & Ajzen I (2009). Predicting and Changing Behavior: The Reasoned Action Approach (1st ed.). Psychology Press. [Google Scholar]
- Fodor MC, Grekin ER, Beatty JR, McGoron L, & Ondersma SJ (2020). Participant Satisfaction with Computer-Delivered Intervention Components and Its Relation to Alcohol Outcomes. Substance Use & Misuse, 55(14), 2332–2340. 10.1080/10826084.2020.1811343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsyth AD, Carey MP, & Fuqua RW (1997). Evaluation of the validity of the condom use self-efficacy scale (CUSES) in young men using two behavioral simulations. Health Psychology, 16(2), 175–178. 10.1037//0278-6133.16.2.175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortenberry JD (2019). Trust, Sexual Trust, and Sexual Health: An Interrogative Review. The Journal of Sex Research, 56(4–5), 425–439. 10.1080/00224499.2018.1523999 [DOI] [PubMed] [Google Scholar]
- Gause NK, Brown JL, Welge J, & Northern N (2018). Meta-analyses of HIV prevention interventions targeting improved partner communication: Effects on partner communication and condom use frequency outcomes. Journal of Behavioral Medicine, 41(4), 423–440. 10.1007/s10865-018-9916-9 [DOI] [PubMed] [Google Scholar]
- Gordon CM, Carey MP, & Carey KB (1997). Effects of a drinking event on behavioral skills and condom attitudes in men: Implications for HIV risk from a controlled experiment. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association, 16(5), 490–495. 10.1037//0278-6133.16.5.490 [DOI] [PubMed] [Google Scholar]
- Hafeez H, Zeshan M, Tahir MA, Jahan N, & Naveed S (2017). Health Care Disparities Among Lesbian, Gay, Bisexual, and Transgender Youth: A Literature Review. Cureus, 9(4). 10.7759/cureus.1184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall KS, Sales JM, Komro KA, & Santelli J (2016). The State of Sex Education in the United States. The Journal of Adolescent Health, 58(6), 595–597. 10.1016/j.jadohealth.2016.03.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2017). Introduction to Mediation, Moderation, and Conditional Process Analysis, Second Edition: A Regression-Based Approach. Guilford Publications. [Google Scholar]
- Javidi H, Widman L, Lipsey N, Brasileiro J, Jhala A, & Javidi F (2021). Adapting an online sexual health intervention for broader dissemination. AIDS Education and Prevention, In Press. [DOI] [PubMed] [Google Scholar]
- Javier SJ, Abrams JA, Moore MP, & Belgrave FZ (2018). Condom Use Efficacy and Sexual Communication Skills Among African American College Women. Health Promotion Practice, 19(2), 287–294. 10.1177/1524839916676253 [DOI] [PubMed] [Google Scholar]
- Kamke K, Widman L, & Desmarais SL (2020). Evaluation of an Online Sexual Health Program among Adolescent Girls with Emotional and Behavioral Difficulties. Journal of Child and Family Studies, 29(4), 1044–1054. 10.1007/s10826-019-01685-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny DA, & Judd CM (2019). The unappreciated heterogeneity of effect sizes: Implications for power, precision, planning of research, and replication. Psychological Methods, 24(5), 578–589. 10.1037/met0000209 [DOI] [PubMed] [Google Scholar]
- Lalas J, Garbers S, Gold MA, Allegrante JP, & Bell DL (2020). Young Men’s Communication With Partners and Contraception Use: A Systematic Review. Journal of Adolescent Health. 10.1016/j.jadohealth.2020.04.025 [DOI] [PubMed] [Google Scholar]
- Lightfoot M (2012). HIV prevention for adolescents: Where do we go from here? American Psychologist, 67(8), 661–671. 10.1037/a0029831 [DOI] [PubMed] [Google Scholar]
- Mitchell CM, Kaufman CE, & Beals J (2005). Resistive Efficacy and Multiple Sexual Partners Among American Indian Young Adults: A Parallel-Process Latent Growth Curve Model. Applied Developmental Science, 9(3), 160–171. 10.1207/s1532480xads0903_3 [DOI] [Google Scholar]
- Morales A, Espada JP, Orgilés M, Escribano S, Johnson BT, & Lightfoot M (2018). Interventions to reduce risk for sexually transmitted infections in adolescents: A meta-analysis of trials, 2008–2016. PloS One, 13(6), e0199421. 10.1371/journal.pone.0199421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noar SM, Carlyle K, & Cole C (2006). Why communication is crucial: Meta-analysis of the relationship between safer sexual communication and condom use. Journal of Health Communication, 11(4), 365–390. 10.1080/10810730600671862 [DOI] [PubMed] [Google Scholar]
- Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, Griffey R, & Hensley M (2011). Outcomes for Implementation Research: Conceptual Distinctions, Measurement Challenges, and Research Agenda. Administration and Policy in Mental Health and Mental Health Services Research, 38(2), 65–76. 10.1007/s10488-010-0319-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn-Nilas C, Milhausen RR, Breuer R, Bailey J, Pavlou M, DiClemente RJ, & Wingood GM (2016). Validation of the Sexual Communication Self-Efficacy Scale. Health Education & Behavior, 43(2), 165–171. 10.1177/1090198115598986 [DOI] [PubMed] [Google Scholar]
- Reyna VF, & Brainerd CJ (2011). Dual processes in decision making and developmental neuroscience: A fuzzy-trace model. Developmental Review, 31, 180–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rickert VI, Neal WP, Wiemann CM, & Berenson AB (2000). Prevalence and predictors of low sexual assertiveness. Journal of Pediatric and Adolescent Gynecology, 13(2), 88–89. 10.1016/S1083-3188(00)00016-4 [DOI] [PubMed] [Google Scholar]
- Rothman AJ, & Sheeran P (2020). The operating conditions framework: Integrating mechanisms and moderators in health behavior interventions. Health Psychology, Advance online publication. 10.1037/hea0001026 [DOI] [PubMed] [Google Scholar]
- Schmid A, Leonard NR, Ritchie AS, & Gwadz MV (2015). Assertive Communication in Condom Negotiation: Insights From Late Adolescent Couples’ Subjective Ratings of Self and Partner. Journal of Adolescent Health, 57(1), 94–99. 10.1016/j.jadohealth.2015.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sekhon M, Cartwright M, & Francis JJ (2017). Acceptability of healthcare interventions: An overview of reviews and development of a theoretical framework. BMC Health Services Research, 17(1), 88. 10.1186/s12913-017-2031-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shannon C, & Klausner J (2018). The Growing Epidemic of Sexually Transmitted Infections in Adolescents: A Neglected Population. Current Opinion in Pediatrics, 30(1), 137–143. 10.1097/MOP.0000000000000578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sieving RE, Bearinger LH, Resnick MD, Pettingell S, & Skay C (2007). Adolescent Dual Method Use: Relevant Attitudes, Normative Beliefs and Self-Efficacy. Journal of Adolescent Health, 40(3), 275.e15–275.e22. 10.1016/j.jadohealth.2006.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, & Sonenstein FL (1998). Adolescent Sexual Behavior, Drug Use, and Violence: Increased Reporting with Computer Survey Technology. Science, 280(5365), 867–873. JSTOR. [DOI] [PubMed] [Google Scholar]
- VanderDrift LE, Agnew CR, Harvey SM, & Warren JT (2013). Whose intentions predict? Power over condom use within heterosexual dyads. Health Psychology, 32(10), 1038–1046. 10.1037/a0030021 [DOI] [PubMed] [Google Scholar]
- Warren C, & Warren L (2015). Family and Partner Communication about Sex. In The Sage Handbook of Family Communication (pp. 184–202). 10.4135/9781483375366.n12 [DOI] [Google Scholar]
- Weinstein N, Sandman P, & Blalock S (2008). The Precaution Adoption Process Model. In Health Behavior and Health Education (4th ed., pp. 123–147). Jossey-Bass. https://cancercontrol.cancer.gov/brp/research/theories_project/theory.pdf [Google Scholar]
- Widman L, Choukas-Bradley S, Helms SW, Golin CE, & Prinstein MJ (2014). Sexual Communication Between Early Adolescents and Their Dating Partners, Parents, and Best Friends. The Journal of Sex Research, 51(7), 731–741. 10.1080/00224499.2013.843148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widman L, Golin CE, Kamke K, Burnette JL, & Prinstein MJ (2018). Sexual Assertiveness Skills and Sexual Decision-Making in Adolescent Girls: Randomized Controlled Trial of an Online Program. American Journal of Public Health, 108(1), 96–102. 10.2105/AJPH.2017.304106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widman L, Golin CE, Noar SM, Massey J, & Prinstein MJ (2016). ProjectHeartforGirls.com: Development of a Web-Based HIV/STD Prevention Program for Adolescent Girls Emphasizing Sexual Communication Skills. AIDS Education and Prevention, 28(5), 365–377. 10.1521/aeap.2016.28.5.365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widman L, Kamke K, Evans R, Stewart JL, Choukas-Bradley S, & Golin CE (2020). Feasibility, Acceptability, and Preliminary Efficacy of a Brief Online Sexual Health Program for Adolescents. The Journal of Sex Research, 57(2), 145–154. 10.1080/00224499.2019.1630800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widman L, Nesi J, Kamke K, Choukas-Bradley S, & Stewart JL (2018). Technology-Based Interventions to Reduce Sexually Transmitted Infections and Unintended Pregnancy Among Youth. Journal of Adolescent Health, 62(6), 651–660. 10.1016/j.jadohealth.2018.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, JB, upon reasonable request. The data are not publicly available due to restrictions from the North Carolina State University IRB.


