Abstract
Objective/Background:
The current study describes insomnia precipitating events reported by women Veterans and examines differences in sleep and psychological distress variables in those who endorsed traumatic, nontraumatic, or no insomnia precipitating events.
Participants:
Baseline data were collected from 347 women Veterans enrolled in a behavioral sleep intervention study (NCT02076165).
Methods:
Participants completed self-report measures of insomnia symptoms, sleep quality, sleep efficiency (SE), nightmare frequency, and depression and posttraumatic stress disorder (PTSD) symptoms; SE was also assessed by wrist actigraphy. Participants responded to 2 open-ended questions assessing stressful life events and health changes that coincided with insomnia symptom onset. Responses were coded as traumatic, nontraumatic, and no events. Analyses of covariance examined the effect of insomnia precipitating event type on sleep and psychological symptom variables after controlling for sociodemographic factors.
Results:
Overall, 25.80% of participants endorsed traumatic events, 65.80% endorsed only nontraumatic events, and 8.41% endorsed no events. Participants who endorsed traumatic events reported more severe insomnia (p = .003), PTSD (p = .001), and depression symptoms (p = .012), and poorer quality of sleep (p = .042) than participants who endorsed no events. Participants who endorsed traumatic events reported more severe PTSD symptoms (p = .004), a longer duration of sleep problems (p = .001), and poorer quality of sleep (p = .039) than participants who endorsed nontraumatic events. Participants who endorsed nontraumatic events reported more severe insomnia (p = .029) and PTSD (p = .049) symptoms than participants who endorsed no events.
Conclusions:
Trauma as a precipitant for insomnia may be related to higher symptom severity in women Veterans. Implications for treatment engagement and effectiveness remain unstudied.
Introduction
Women represent a rapidly growing portion of the Veteran population. It is estimated that the number of women Veterans will grow to 2.4 million by 2020 (National Center for Veterans Analysis and Statistics, 2013). More than 44% of Operation Enduring Freedom and Operation Iraqi Freedom (OEF/OIF) women Veterans are enrolled in VA healthcare, with women Veterans utilizing VA healthcare at higher rates than men Veterans (Haskell et al., 2011; Hayes & Krauthamer, 2009). Given women Veterans’ increased healthcare utilization, research to identify the unique healthcare needs of this growing population is greatly needed.
A consistent finding is the unique trauma history of women in the military. While exposure to traumatic events is common, the development of clinically significant trauma-related symptoms is less common. It is estimated that 89.7% of the population will be exposed to a posttraumatic stress disorder (PTSD) criterion A event, but only 8.3% will meet diagnostic criteria for PTSD during their lifetime (Kilpatrick et al., 2013). Research has demonstrated that certain types of stressful/traumatic events contribute to higher levels of psychological distress (Ehring & Quack, 2010; Shakespeare-Finch & Armstrong, 2010). It is estimated that 38% of women Veterans experience military sexual trauma (MST) and MST is consistently associated with higher levels of distress, greater medical/psychiatric comorbidities, and poorer functioning compared to other stressful and traumatic events (Kimerling et al., 2016; Surís & Lind, 2008; Wilson, 2018). It stands to reason that traumatic events may result in more severe sleep disturbance than nontraumatic events, but no study has examined the impact of traumatic and nontraumatic insomnia precipitants on sleep and psychological distress among women Veterans. These differences may inform the treatment women Veterans receive. Lehavot et al. (2018) examined lifetime trauma exposure and past-year stressful life events (i.e., health-related, social, job, and legal stress) among men and women Veterans as well as women civilians. Women Veterans reported a greater number of lifetime traumatic events (2.21) than women civilians (1.65) and a greater number of stressful life events (2.01) than women civilians (1.63) and men Veterans (1.29). These collective findings suggest that women Veterans are not only at an increased risk for experiencing traumatic events, but also for experiencing a variety of other stressful life events.
One of the most commonly reported symptoms following traumatic events and stressful life events is sleep disturbance. Bastien et al. (2004) examined the types of stressful life events that precipitate insomnia in the general population in Canada and found that 78.3% of patients identified a specific insomnia precipitating event. The authors categorized events into the following domains: work/school, family, physical and psychological health, and indeterminate, and these events were furthered categorized according to negative or positive affective valence. Sixty-five percent of insomnia precipitating events were of a negative valence, with events related to family, health, and work/school most frequently reported. LeBlanc et al. (2009) examined life events in patients with good sleep (i.e., endorsed satisfaction with sleep, denied insomnia symptoms, and denied use of sleep-promoting agents), patients with insomnia syndrome (i.e., met DSM-IV-TR diagnostic criteria for primary insomnia or used a sleep-promoting agent ≥3 nights per week), and patients with insomnia symptoms (i.e., endorsed symptoms without fulfilling all diagnostic criteria for primary insomnia or endorsed dissatisfaction with sleep or used prescribed medication to promote sleep < 3 nights per or over-the-counter medication ≥ 1 night per week). Results revealed that patients with insomnia symptoms and insomnia syndrome reported significantly more total life events than good sleepers over a 6-month period. Patients with insomnia syndrome also reported significantly more negative life events and rated these events as higher in intensity than good sleepers. These collective results suggest that stressful life events are an important predictor of insomnia symptoms.
The relationship between stressful life events and insomnia onset is frequently referenced in the sleep literature. The “3-Ps” model is a widely accepted model of insomnia development and underlies the rationale for Cognitive Behavioral Therapy for Insomnia (CBT-I), the first-line treatment for insomnia disorder (Qaseem et al., 2016; Spielman et al., 1987). The “3-Ps” model proposes that sleep problems develop from and are maintained by three factors, (1) predisposing factors (e.g., genetic, physiological, and psychological vulnerabilities), (2) precipitating factors (e.g., environmental, physiological, or psychological stressors), and (3) perpetuating factors (e.g., behaviors, environmental circumstances, and physiological or psychological conditions). The nature of these events has received limited research attention.
PTSD and major depressive disorder (MDD) symptoms are among the most frequently reported mental health symptoms following the experience of a traumatic event (O’Donnell et al., 2004; Rytwinski et al., 2013), yet the conditions are not well studied in the context of insomnia onset. PTSD and MDD are also the most prevalent psychiatric service-connected disabilities among women Veterans and (National Center for Veterans Analysis and Statistics, 2015). Despite their high prevalence, PTSD and MDD treatment rates vary widely. Women Veterans who obtain care outside the VA are less likely than VA users to receive care (Washington et al., 2013). Seventy percent of individuals with PTSD experience sleep disturbance and 90% of individuals with depression report sleep quality complaints (Ohayon & Shapiro, 2000; Tsuno et al., 2005). Within the context of posttraumatic responses, sleep disturbance is the norm and not the exception. Among women Veterans, more than a quarter meet concurrent diagnostic criteria for insomnia disorder and probable PTSD (Hughes et al., 2013; Martin et al., 2017). Kelly et al. (2011) examined mental and physical health among 135 women Veterans, and found elevated rates of clinically significant PTSD and depression symptoms, and every participant reported disturbed sleep. Given the high rate at which women Veterans experience traumatic events, it is likely that these events contribute to insomnia symptoms for many women Veterans.
The aims of the current analyses were to: (1) describe the traumatic and nontraumatic events that women Veterans link to insomnia symptom onset, (2) examine differences in sleep characteristics among women Veterans who endorsed traumatic, nontraumatic, or no insomnia precipitating events, and (3) examine differences in PTSD and depression symptoms among women Veterans who endorsed traumatic, nontraumatic, and no insomnia precipitating events. The following hypotheses were proposed: (1) most women Veterans will identify insomnia precipitating events and (2) women Veterans who endorse traumatic insomnia precipitating events will demonstrate greater sleep disturbance and more severe PTSD and depression symptoms than women Veterans who endorse nontraumatic insomnia precipitating events or no insomnia precipitating events.
Methods
Recruitment and participants
The sample for the current study was drawn from the population of women Veterans who received care at the VA Greater Los Angeles Healthcare System (VGLAHS). Women Veterans were recruited through a three-step process. Women Veterans with insomnia symptoms were identified using a postal survey, which contained items addressing the diagnostic criteria for insomnia disorder (Martin et al., 2017). In total, 1,372 women Veterans were considered as potentially eligible based on survey responses, 788 of whom were contacted to complete a telephone eligibility screening, and 347, of those screened were enrolled in the study. Exclusion criteria included: those who self-described as too ill to participate, did not have access to transportation to the medical center, were unable to provide self-consent for participation, or were without stable housing. All other women Veterans who endorsed insomnia symptoms on the survey, defined as one or more symptoms of poor sleep and daytime consequences at least three times per week, were invited to participate in the study. Interested women Veterans provided written informed consent and competed baseline assessment to participate in the behavioral sleep intervention trial (NCT02076165).
Procedure
This was a cross-sectional study. Participants completed a 9-day pre-treatment baseline assessment consisting of three visits to the Sepulveda Ambulatory Care Center within VAGLAHS, during which time interviews and questionnaire assessments were completed in private offices used for research purposes by trained study assessment staff. During visit 1, participants completed an informed consent to participate in the clinical trial and provided demographic information. During visit 2, participants answered questions about mental health symptoms and were provided with an actigraph to wear at home for a week and a sleep diary to complete each day. During visit 3, participants returned the actigraph and sleep diary and completed self-report sleep measures. A psychologist or social worker administered the PTSD Checklist for the DSM-5 (PCL-5) (Bovin et al., 2016). All other measures were administered by either a psychologist, a social worker, or an experienced Bachelor’s level research assistant, who completed a standardized training. The Institutional Review Board at the VGLAHS reviewed and approved the study procedures.
Measures
Sociodemographic variables
Age in years was calculated using each participant’s birth date. Participants reported their race/ethnicity, number of years of education, annual household income, relationship status, and employment status.
Insomnia precipitating events
Participants were asked two questions regarding insomnia precipitating events in an open response format; identify any (1) health changes or (2) stressful life events that coincided with insomnia symptom onset. For description of items, see Figure 1. Responses were categorized as identified traumatic events, identified nontraumatic events, or no identified events. For a visual depiction of precipitating event categorization, see Figure 2. Two authors (GCC and MRK) achieved high interrater agreement (92%) on all event ratings in the sample. Disagreements among raters (n = 28) were adjudicated during a face-to-face meeting. To confirm the reliability of the insomnia precipitating event coding system, a third rater (AMG) recoded 10% of the sample and achieved adequate agreement (82.86%) across all event categories (i.e., no event, all nontraumatic event subcategories, and all traumatic event subcategories) and high agreement (91.28%) regarding classification into the three broader event groups (i.e., no events, nontraumatic events, and traumatic events). Disagreements among raters (n = 6) were adjudicated during a second face-to-face meeting. The third rater (AMG) recoded another 10% of the sample and, again, achieved adequate interrater agreement (82.86%) across all event subcategories and high interrater agreement on the three event groups (97.14%). Disagreements among raters (n = 6) were adjudicated during a third and final face-to-face meeting. All discrepancies were resolved by consensus.
Figure 1.
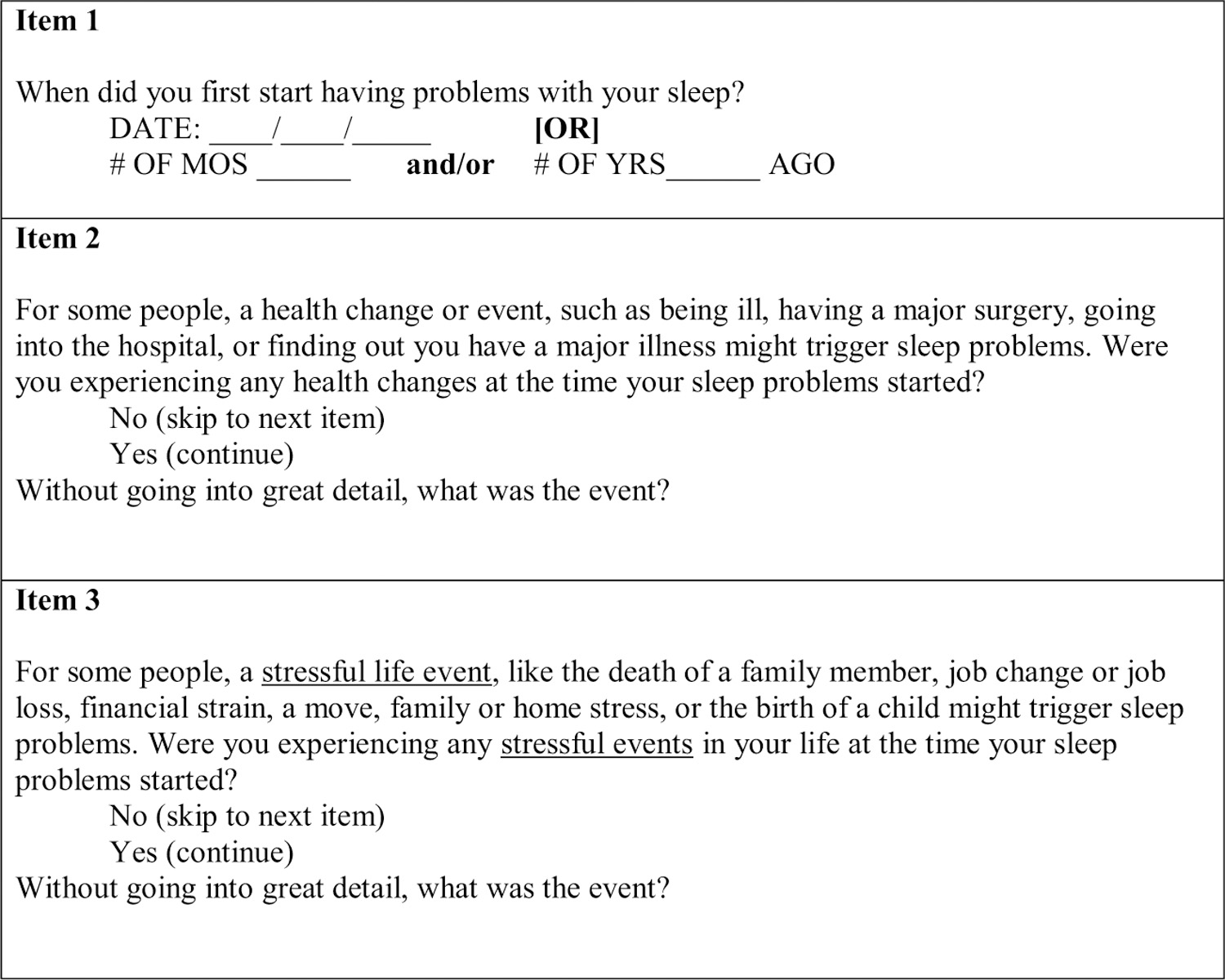
Items used to assess the duration of sleep problems and insomnia precipitating events.
Figure 2.
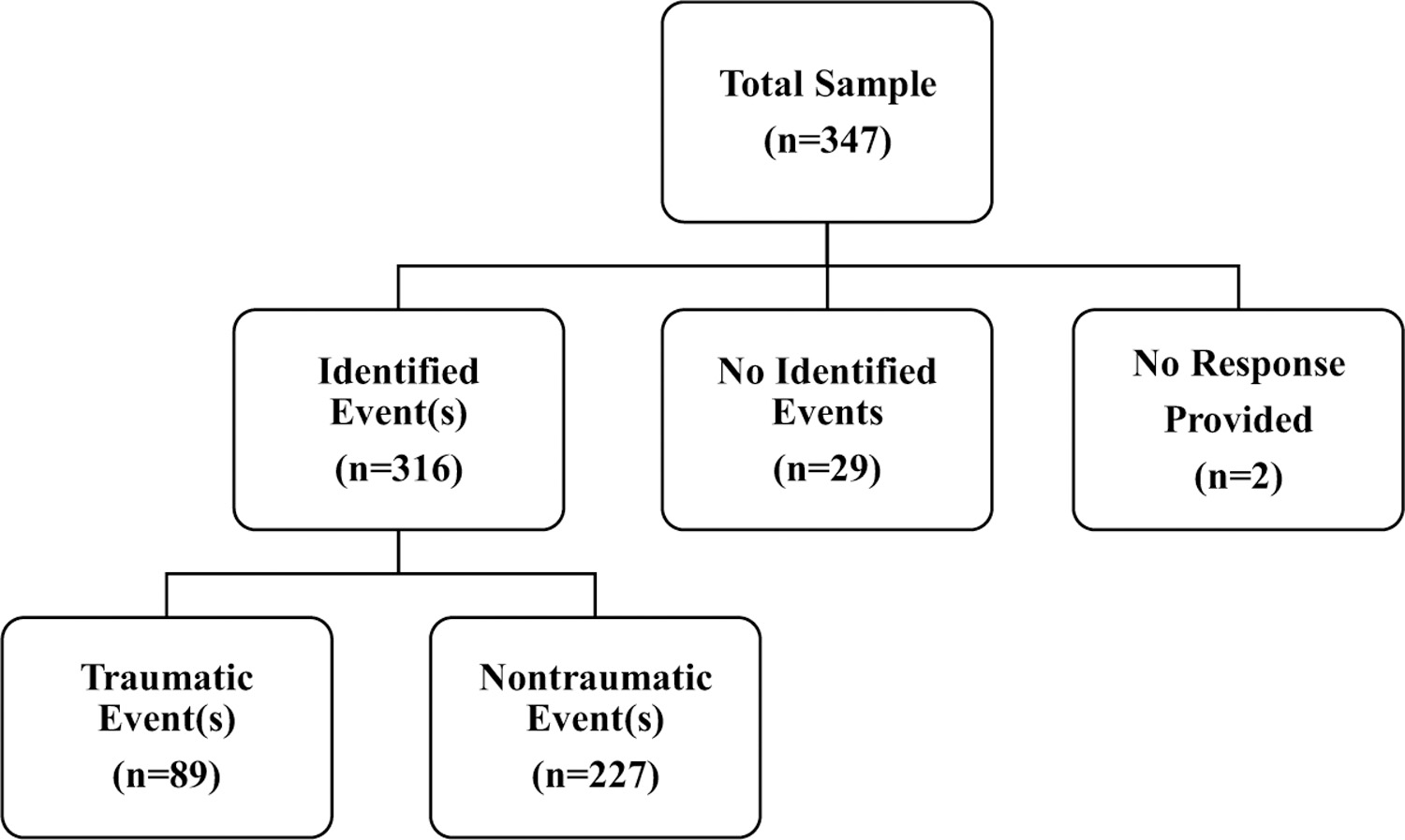
Endorsement of insomnia precipitating events among participants.
Identified traumatic events.
Events were categorized as identified traumatic events if they corresponded to the first 16 items included on the Life Events Checklist (LEC) for the Diagnostic and Statistical Manual of Mental Disorders 5th Edition (DSM-5) (Weathers et al., 2013). In the current study, “traumatic illness or injury” (LEC item #12) was limited to cancer, heart conditions, autoimmune disorders (e.g., lupus), neurodegenerative disorders (e.g., Parkinson’s disease), major injury/medical procedure involving the abdomen, chest, or spine, and injuries that resulted in lasting disability.
Identified nontraumatic events.
Consistent with Bastien et al. (2004), events that were identified as nontraumatic were further categorized into the following content domains: health, psychopathology, work/school, family, and other. The health content domain included all other health-related conditions not previously categorized as a traumatic illness or injury as described above. The psychopathology domain included mental health diagnoses, alcohol/substance use problems, and emotional distress. The work/school domain included: stress at work/school, rotating shift, employment change, retirement, and financial problems. In the current study, the family domain was relabeled “interpersonal” to more accurately describe the breadth of events reported within this domain. Given the diversity of the interpersonal domain, the following interpersonal subcategories were also examined: illness of significant person, bereavement, pregnancy/childbirth, child caregiving, adult caregiving, relationship problems, divorce/separation/romantic breakup, and interpersonal-other (e.g., stress at home, family stress). A military domain was added to include deployment and training experiences, excluding combat and military sexual trauma. Events were categorized as “other” if they did not fall into the previously described domains (e.g., moving, litigation).
No identified events.
If participants denied experiencing a health change or a stressful life event that coincided with the onset of their sleep problems, the participant was categorized as identifying no insomnia precipitating events.
Insomnia
The Insomnia Severity Index (ISI) is a 7-item instrument using Likert-type scales that measure perceived severity of insomnia symptoms from 0 (not at all) to 4 (very much). Individual items are summed to calculate a total score for each participant. The total score ranges from 0 to 28, with higher score indicating greater insomnia severity. The ISI correlates well with scores on the Pittsburgh Sleep Quality Index (r =.67) and with sleep diary measures (r’s = 0.32–0.91) (Bastien, Vallières & Morin, 2001).
Sleep quality
The Pittsburgh Sleep Quality Index (PSQI) is a widely used 18-item questionnaire that assesses sleep quality and disturbances over the last month (Buysse et al., 1989). Subscale scores are calculated from individual items, then summed to calculate the PSQI global score for each participant. PSQI global scores range from 0 to 21 with higher scores indicating worse sleep quality. The PSQI has a sensitivity for distinguishing between normal and abnormal sleepers of 89.6% and a specificity of 86.5% (kappa = 0.75, p < .001) (Buysse et al., 1989). Sleep quality will hence forth be referred to has PSQI sleep quality.
Sleep efficiency
Participants completed a sleep diary for one week as a measure of subjective sleep efficiency. The sleep diary was based on the American Academy of Sleep Medicine Consensus Sleep Diary and was adapted for use in the current study using a cognitive interviewing process (Carney et al., 2012). Cognitive interviewing involves asking individuals to answer questions, then asking them to describe how they arrived at their answer (see Collins (2003); Drennan (2003)). In this way, construct validity for survey questionnaires can be improved. We used this process to improve readability and understanding of the question wording on the diary. Sleep efficiency (percent of time asleep out of total time in bed) was the key outcome, with higher values indicating greater sleep efficacy (Carney et al., 2012; Willis et al., 1991). Objective sleep efficiency data were collected via actigraphy (Actiwatch Spectrum, Minimitter/Respironics, Bend, OR) worn on the nondominant wrist for 7 consecutive days and nights Activity levels were collected in 1-minute epochs. Wrist actigraphy has been validated as an objective measure of sleep in numerous studies, and evidence-based guidelines direct the use of this technology (Morgenthaler et al., 2007). Sleep efficacy data was calculated by the Philips Actiware software, Version 6.0.8 automated scoring algorithm utilizing the default algorithms with medium threshold settings. To clean actigraphy data, we calculated summary measures of sleep and wake. Intervals corresponding to time periods of interest were created based on the bedtimes and out of bed times noted on each participant’s sleep diary for every night the watch was worn. If there was an apparent discrepancy between the sleep diary and actigraphy recording, these were reviewed by two trained scorers and the Principal Investigator (JLM) and a consensus was reached about the bedtime and rise time for that night.
Nightmare frequency
The Disturbing Dream and Nightmare Severity Index (DDNSI) is a 5-item expanded version of the Nightmare Frequency Questionnaire (Krakow et al., 2000, 2002). The DDNSI included in the current study assessed the number of nights (during the previous week) in which participants experienced nightmares. This item was used as the measure of nightmare frequency.
Depression symptoms
Patient Health Questionnaire-9 (PHQ-9) is a 9-item depression module in the Patient Health Questionnaire, a-self-administered diagnostic instrument for common mental health disorders (Kroenke et al., 2010). Individual items are summed to calculate a total score for each participant. The total score ranges from 0 to 27, with higher score indicating greater depression symptoms. The PHQ-9 has a sensitivity of 88% and a specificity of 88% for major depression (Kroenke et al., 2001).
PTSD symptoms
The PTSD Checklist for the DSM-5 (PCL-5) (Bovin et al., 2016) was administered to assess PTSD symptoms. The PCL-5 is a 20-item self-report measure of PTSD symptoms. Individual items are summed to calculate a total score for each participant. The total score ranges from 0 to 80, with higher score indicating greater PTSD symptoms. The PCL-5 has demonstrated strong internal reliability (α = .94), test-retest reliability (r = .82), and convergent validity (rs = 74 to .85) (Blevins et al., 2015).
Data analysis
All analyses were conducted using Stata/MP version 15.1 (StataCorp, 2017). Descriptive statistics examined the frequency of traumatic, nontraumatic, or no events endorsed by participants. Participants who endorsed one or more traumatic event(s) were categorized as having a traumatic event. Participants who endorsed one or more stressful life events but no traumatic event(s) were categorized as having a nontraumatic event. Participants who did not endorse any events were categorized as having no event. For each analysis, two-sided testing was performed with an alpha of 0.05.
Analyses of covariance (ANCOVAs) were performed to examine differences in insomnia symptoms, PSQI sleep quality, sleep efficiency, nightmare frequency, depression symptoms, and PTSD symptoms among participants who endorsed traumatic events, nontraumatic events, and no events, controlling for the effects of sociodemographic variables. We chose to focus on sleep efficiency as our main diary-based outcome measure as it is used to inform insomnia treatment. To further explore this finding, we conducted post hoc analyses of the variables that comprise sleep efficiency including: total sleep time, sleep onset latency, and wake after sleep onset from the sleep diary as well as sleep efficiency calculated from the PSQI (i.e., [number of hours slept/number of hours spent in bed] x 100; see Supplemental Table 1). Given the specific between-group study hypotheses, no omnibus tests were performed. Instead, three planned comparisons were tested, 1) comparing traumatic events vs. nontraumatic events groups, 2) comparing traumatic events vs. no events groups, and 3) comparing nontraumatic events and no events groups. The ANCOVA model was fit using the regress command, while the planned comparisons were performed with the contrast command. Adjusted means were computed as a function of precipitating event type, adjusting for covariates, using the margins command.
The effect size for these planned comparisons was estimated using Cohen’s d. Cohen’s d was computed from the ANCOVA analyses by dividing the difference in the adjusted means by the pooled standard deviation (i.e., mean squared error [MSE]) from the unadjusted analysis (i.e., the MSE arising from the analysis in which insomnia precipitating event group is the only predictor in the model) (Olejnik & Algina, 2000).
Follow-up logistic regression analyses were performed to examine differences in ISI, PCL-5, and PHQ-9 clinical cutoff scores among participants who endorse traumatic events, nontraumatic events, or no events, controlling for the effects of sociodemographic variables. Within the no events group, no participants had an ISI total score of >21 (severe insomnia); therefore, the clinical cutoff score of >14 (moderately severe insomnia) was used (Bastien et al., 2001). The PCL-5 cutoff score was >32 (clinically significant PTSD symptoms) (Blevins et al., 2015). Within the no events group, only 1 participants had a PHQ-9 total score of >19 (severe depression), therefore, the clinical cutoff score of >14 (moderately severe depression) and >9 (moderate depression) were used (Kroenke et al., 2001).
The logistic regression model was fit using the logistic command and the results of planned contrasts comparing precipitating event types are reported using odds ratios. To further aid in the interpretation of the results, the adjusted proportions, by precipitating event type, adjusting for the covariates were computed (using the margins command).
Results
Insomnia precipitating event frequency
Regarding participants’ reports of events coinciding with insomnia onset, 8.41% (n = 29) reported no event, 25.80% (n = 89) reported one or more traumatic events, and 65.80% (n = 227) reported one or more nontraumatic events, but no traumatic event. Within the traumatic event group, 89.89% (n = 80) reported one traumatic event, 8.99% (n = 8) reported two traumatic events, and 1.12% (n = 1) reported three traumatic events. Within the nontraumatic event group, 44.49% (n = 101) reported one nontraumatic event, 36.56% (n = 83) reported two nontraumatic events, 15.42% (n = 35) reported three nontraumatic events, 3.08% (n = 7) reported four nontraumatic events, 0.44% (n = 1) reported five nontraumatic events. The specific types of traumatic and nontraumatic insomnia precipitating events and the frequencies are presented in Table 1.
Table 1.
Types and frequencies of traumatic and nontraumatic precipitating events.
| Traumatic insomnia precipitating event types | |
|---|---|
| Life threatening injury/illness | 50.56% (n = 45) |
| Sexual assault | 30.34% (n = 27) |
| Physical assault | 8.99% (n = 8) |
| Combat or exposure to war zone | 7.87% (n = 7) |
| Transportation accident | 4.49% (n = 4) |
| Sudden violent death (e.g., suicide or homicide) | 4.49% (n = 4) |
| Unwanted or uncomfortable sexual experience | 2.25% (n = 2) |
| Natural disaster | 1.12% (n = 1) |
| Assault with a weapon | 1.12% (n = 1) |
| Nontraumatic insomnia precipitating event types | |
| Interpersonal events | 46.26% (n = 105) |
| Military events | 44.93% (n = 102) |
| Health events | 29.96% (n = 68) |
| Work/school events | 29.52% (n = 67) |
| Psychopathology events | 13.22% (n = 30) |
| Other nontraumatic events | 14.54% (n = 33) |
| Nontraumatic interpersonal event types* | |
| Pregnancy/childbirth | 28.57% (n = 30) |
| Bereavement | 27.62% (n = 29) |
| Illness of a significant person | 12.38% (n = 13) |
| Relationship problems | 9.52% (n = 10) |
| Divorce/separation/romantic breakups | 9.52% (n = 10) |
| Child caregiving | 3.81% (n = 4) |
| Adult caregiving | 3.81% (n = 4) |
| Other interpersonal events | 27.62% (n = 29) |
Note. Among the 105 women Veterans who reported nontraumatic interpersonal insomnia precipitating events
indicates the types of interpersonal events reported.
Differences in sleep variables by insomnia precipitating event type
Sociodemographic variable descriptive statistics for participants who endorsed traumatic events, nontraumatic events, and no events are included in Table 2. Sleep and psychological distress variable descriptive statistics, adjusted for sociodemographic covariates, are presented in Table 3.
Table 2.
Sociodemographic variables among participants.
| Total Sample M or % n |
No Events M or % n |
Nontraumatic Event(s) M or % n |
Traumatic Event(s) M or % n |
p | |
|---|---|---|---|---|---|
| Age (Years) | 47.12 | 47.66 | 45.26 | 51.40 | <0.001 |
| 345 | 29 | 226 | 88 | ||
| Race/Ethnicity† | |||||
| Non-Hispanic/Latina White | 41.16% | 34.48% | 39.65% | 47.19% | 0.35 |
| 142 | 10 | 90 | 42 | ||
| Non-Hispanic/Latina Back/African American | 32.17% | 24.14% | 31.28% | 37.08% | 0.38 |
| 111 | 7 | 71 | 33 | ||
| Hispanic/Latina | 27.54% | 31.03% | 30.84% | 17.98% | 0.06 |
| 95 | 9 | 70 | 16 | ||
| Non-Hispanic/Latina American Indian/Native Alaskan | 6.09% | 0.00% | 7.05% | 5.62% | 0.40 |
| 21 | 0 | 16 | 5 | ||
| Non-Hispanic/Latina Asian | 4.64% | 3.45% | 5.29% | 3.37% | 0.84 |
| 16 | 1 | 12 | 3 | ||
| Education (Years) | 16.03 | 16.80 | 16.03 | 15.77 | 0.14 |
| 344 | 28 | 227 | 89 | ||
| Income | 0.17 | ||||
| <$10,000 | 8.26% | 0.00% | 10.81% | 4.55% | |
| 28 | 0 | 24 | 4 | ||
| $10,000–20,000 | 11.21% | 17.24% | 9.01% | 14.77% | |
| 38 | 5 | 20 | 13 | ||
| $20,000–30,000 | 13.57% | 20.69% | 11.26% | 17.05% | |
| 46 | 6 | 25 | 15 | ||
| $30,000–40,000 | 11.80% | 13.79% | 11.71% | 11.36% | |
| 40 | 4 | 26 | 10 | ||
| $40,000–50,000 | 14.16% | 3.45% | 13.96% | 18.18% | |
| 48 | 1 | 31 | 16 | ||
| $50,000-$100,000 | 26.25% | 31.03% | 27.03% | 22.73% | |
| 89 | 9 | 60 | 20 | ||
| >$100,000 | 14.75% | 13.79% | 16.22% | 11.36% | |
| 50 | 4 | 36 | 10 | ||
| Relationship status | 0.71 | ||||
| Married | 33.43% | 20.69% | 36.41% | 30.12% | |
| 110 | 6 | 79 | 25 | ||
| Divorced | 24.92% | 31.03% | 23.50% | 26.51% | |
| 82 | 9 | 51 | 22 | ||
| Separated | 4.56% | 3.45% | 4.15% | 6.02% | |
| 15 | 1 | 9 | 5 | ||
| Widowed | 4.26% | 3.45% | 3.69% | 6.02% | |
| 14 | 1 | 8 | 5 | ||
| Single/Never | 32.83% | 41.38% | 32.26% | 31.33% | |
| 108 | 12 | 70 | 26 | ||
| Employment | 0.08 | ||||
| Unemployed | 50.43% | 44.83% | 47.14% | 60.67% | |
| 174 | 13 | 107 | 54 | ||
| Employed for wages | 49.57% | 55.17% | 52.86% | 39.33% | |
| 171 | 16 | 120 | 35 |
Valid N varies according to variable, from n = 329 to n = 347.
Multiple response options can be selected, and thus percentages do not sum to 100%.
Table 3.
Sleep and psychological variables, adjusted for sociodemographic covariates.
| No Events M (95% CI) |
Nontraumatic Event(s) M (95% CI) |
Traumatic Event(s) M (95% CI) |
|
|---|---|---|---|
| Insomnia (ISI Total Score) | 11.88 | 14.16 | 15.30 |
| (9.96, 13.79) | (13.47, 14.84) | (14.16, 16.44) | |
| Sleep Quality (PSQI Total Score) | 10.02 | 10.66 | 11.70 |
| (8.63, 11.40) | (10.17, 11.16) | (10.87, 12.52) | |
| Diary Sleep Efficiency (%) | 79.56 | 78.03 | 78.10 |
| (74.30, 84.82) | (76.15, 79.91) | (74.92, 81.28) | |
| Objective Sleep Efficiency (%) | 80.86 | 79.82 | 80.73 |
| (77.70, 84.02) | (78.71, 80.93) | (78.86, 82.60) | |
| Duration of Sleep Problems (Years) | 15.37 | 14.88 | 19.59 |
| (11.35, 19.39) | (13.44, 16.32) | (17.21, 21.96) | |
| Nightmare Frequency (Nights/Week) | 1.30 | 2.04 | 2.34 |
| (0.11, 2.49) | (1.62, 2.45) | (1.64, 3.04) | |
| PTSD (PCL-5 Total Score) | 17.16 | 26.54 | 35.41 |
| (8.33, 25.98) | (23.57, 29.51) | (30.34, 40.47) | |
| Depression (PHQ-9 Total Score) | 8.75 | 10.70 | 12.12 |
| (6.49, 11.00) | (9.92, 11.49) | (10.80, 13.45) |
Number of observations vary according to variable, from n = 299 to n = 321.
Note. ISI = Insomnia Severity Index, PSQI = Pittsburgh Sleep Quality Index, PCL-5 = PTSD Checklist-5, and PHQ-9 = Patient Health Questionnaire-9. Lower values indicate poorer sleep efficiency and greater PSQI scores indicate poorer sleep quality; analyses controlled for the following covariates: age, race/ethnicity, years of education, income, relationship status, and employment status.
Planned comparisons revealed significant differences in insomnia symptom severity among groups. The traumatic events group reported more severe insomnia symptoms (M = 15.30) than the no events group (M = 11.88; p = .003; d = 0.66). The nontraumatic events group (M = 14.16) also reported more severe insomnia symptoms than the no events group (p = .029; d = 0.44). Comparisons also revealed significant differences in PSQI sleep quality among groups. The traumatic events group (M = 11.70) reported poorer PSQI sleep quality than the nontraumatic events group (M = 10.66; p = .039; d = 0.28) and the no events groups (M = 10.02; p = .042; d = 0.46). There were no significant group differences in diary sleep efficiency (M = 78.03–79.56; p = .59–0.97; d = −0.11–0.005), objective sleep efficiency, (M = 79.82–80.86; p = .42–0.95; d = −0.13–0.11), or nightmare frequency (M = 1.30–2.34; p = .14–0.47; d = 0.10–0.35). Comparisons revealed a significant difference in the duration of sleep problems, with the traumatic events group (M = 19.59 years) reporting a longer duration of sleep problems than the nontraumatic events group (M = 14.88 years p = .001, d = 0.41).
Differences in PTSD and depression symptoms by insomnia precipitating event type
Group comparisons revealed significant differences in PTSD symptom severity among groups. The traumatic events group (M = 35.41) reported more severe PTSD symptoms than the nontraumatic events group (M = 26.54; p = .004; d = 0.40) and the no events group (M = 17.16; p = .001; d = 0.83). The nontraumatic events group also reported more severe PTSD symptoms than the no events group (p = .049; d = 0.42). Group comparisons also revealed a significant difference in depression symptom severity, with the traumatic events group (M = 12.12) reporting more severe depression symptoms than the no events group (M = 8.75; p = .012; d = 0.57). Table 4 summarizes group differences.
Table 4.
Results of planned comparisons across groups according to precipitating event type.
| Nontraumatic Events vs. No Events |
Traumatic Events vs. No Events |
Traumatic Events vs. Nontraumatic Events |
|
|---|---|---|---|
| Insomnia (ISI Total Score) | 2.28 (0.23, 4.33) p = .029, d = 0.44 | 3.42 (1.17, 5.67) p = .003, d = 0.66 | 1.14 (−0.21, 2.50) p = .098, d = 0.22 |
| Sleep Quality (PSQI Total Score) | 0.65 (−0.83, 2.12) p = .39, d = 0.17 | 1.68 (0.06, 3.30) p = .042, d = 0.46 | 1.03 (0.053, 2.01) p = .039, d = 0.28 |
| Diary Sleep Efficiency (%) | −1.53 (−7.14, 4.08) p = .59, d = −0.11 | −1.46 (−7.66, 4.74) p = .64, d = ?0.11 | 0.07 (−3.68, 3.83) p = .97, d = 0.005 |
| Objective Sleep Efficiency (%) | −1.04 (−4.41, 2.32) p = .54, d = −0.13 | −0.13 (−3.84, 3.58) p = .95, d = −0.015 | 0.91 (−1.30, 3.12) p = .42, d = 0.11 |
| Duration of Sleep Problems (Years) | −0.49 (−4.78, 3.81) p = .82, d = −0.042 | 4.22 (−0.47, 8.91) p = .078, d = 0.37 | 4.70 (1.88, 7.53) p = .001, d = 0.41 |
| Nightmare Frequency (Nights/Week) | 0.74 (−0.53, 2.00) p = .25, d = 0.25 | 1.04 (−0.35, 2.44) p = .14, d = 0.35 | 0.30 (−0.52, 1.13) p = .47, d = 0.10 |
| PTSD (PCL-5 Total Score) | 9.39 (0.05, 18.73) p = .049, d = 0.42 | 18.25 (7.97, 28.53) p = .001, d = 0.83 | 8.86 (2.90, 14.83) p = .004, d = 0.40 |
| Depression (PHQ-9 Total Score) | 1.96 (−0.44, 4.35) p = .11, d = 0.33 | 3.38 (0.73, 6.02) p = .012, d = 0.57 | 1.42 (−0.15, 2.99) p = .075, d = 0.24 |
Note. Tabled values show differences in adjusted means, 95% confidence interval for the difference, p value of the comparison, and the effect size expressed as Cohen’s d.
Number of observations vary according to variable, from n = 299 to n = 321; ISI = Insomnia Severity Index, PSQI = Pittsburgh Sleep Quality Index, PCL-5 = PTSD Checklist-5, and PHQ-9 = Patient Health Questionnaire-9. Lower values indicate poorer sleep efficiency and greater PSQI scores indicate poorer sleep quality; analyses controlled for the following covariates: age, race/ethnicity, years of education, income, relationship status, and employment status.
Clinically significant symptom differences by insomnia precipitating event type
Insomnia symptoms
The odds for reporting moderately severe insomnia symptoms (i.e., ISI total score >14) was 3.97 times greater for the nontraumatic events group (OR 3.97, 95% CI = 1.34, 11.76, p = .013) and 6.61 times greater for the traumatic events group (OR 6.61, 95% CI = 2.06, 21.26, p = .002) compared to the no events group. There was no significant difference in the proportion of moderately severe insomnia cutoff scores between the traumatic events and the nontraumatic events groups (OR 1.67, 95% CI = 0.92, 3.04, p = .095). The adjusted probabilities of reporting moderately severe insomnia, PTSD, and depression symptoms by precipitating event type, adjusted for covariates, are shown in Table 5.
Table 5.
Adjusted probabilities of meeting clinical cutoffs for insomnia, PTSD, and depression symptoms by precipitating event type, adjusted for covariates, with 95% confidence intervals.
| OR (95% CI) |
||||||
|---|---|---|---|---|---|---|
| No Events | Nontraumatic Event(s) | Traumatic Event(s) | No Event(s) vs. Nontraumatic Event(s) |
No Events vs. Traumatic Event(s) |
Traumatic Event(s) vs. Nontraumatic Event(s) |
|
| Insomnia: ISI Total Score >14 (Moderately severe) |
0.19 (0.04, 0.34) | 0.45 (0.38, 0.51) | 0.56 (0.45, 0.67) | 3.97 (1.34, 11.76) | 6.61 (2.06, 21.26) | 1.67 (0.92, 3.04) |
| PTSD: PCL-5 Total Score >32 (Clinically significant) |
0.26 (0.09, 0.43) | 0.42 (0.35, 0.48) | 0.61 (0.50, 0.71) | 2.26 (0.80, 6.44) | 5.45 (1.75, 16.99) | 2.41 (1.30, 4.45) |
| Depression: PHQ-9 Total Score |
0.43 (0.24, 0.61) | 0.52 (0.45, 0.58) | 0.65 (0.55, 0.76) | 1.49 (0.61, 3.64 | 2.80 (1.04, 7.55) | 1.87 (1.03, 3.42) |
| >9 (Moderate) | ||||||
| >14 (Moderately severe) | 0.13 (−0.002, 0.26) | 0.28 (0.22, 0.34) | 0.37 (0.26, 0.48) | 2.81 (0.77, 10.23) | 4.55 (1.18, 17.59) | 1.62 (0.87, 3.03) |
Note. ISI = Insomnia Severity Index, PCL-5 = PTSD Checklist-5, and PHQ-9 = Patient Health Questionnaire-9; analyses controlled for the following covariates: age, race/ethnicity, years of education, income, relationship status, and employment status.
PTSD symptoms
The odds for reporting PTSD symptoms above the clinical cutoff (i.e., PCL-5 total score >32) was 5.45 times greater for the traumatic events group compared to the no events group (OR 5.45, 95% CI = 1.75, 16.99, p = .004) and 2.41 times greater for the traumatic events group compared to the nontraumatic events group (OR 2.41, 95% CI = 1.30, 4.45, p = .005). There was not a significant difference in the proportion of PTSD clinical cutoff scores between the nontraumatic events and the no events groups (OR 2.26, 95% CI = 0.80, 6.44, p = .13).
Depression symptoms
Using a PHQ-9 cutoff score of >14 (moderately severe depression), the odds for reporting moderately severe depression symptoms was 4.55 times greater for the traumatic events group compared to no events group (OR 4.55, 95% CI = 1.18, 17.59, p = .028). There were no significant differences in the proportions of moderately severe depression cutoff scores between the traumatic events and the nontraumatic events groups (OR 1.62, 95% CI = 0.87, 3.03, p = .13) or the nontraumatic events and the no events groups (OR 2.81, 95% CI = 0.77, 10.23, p = .12). Using a PHQ-9 cutoff score of >9 (moderate depression), the odds for reporting moderate depression symptoms was 2.80 times greater for the traumatic events group compared to the no events group (OR 2.80, 95% CI = 1.04, 7.55, p = .042). The odds for reporting moderate depression symptoms was 1.87 times greater for the traumatic events group compared to the nontraumatic events group (OR 1.87, 95% CI = 1.03, 3.42, p = .041). There was not a significant difference in the proportion of moderate depression cutoff scores between the nontraumatic events and the no events groups (OR 1.49, 95% CI = 0.61, 3.64, p = .38).
Discussion
The aims of the current study were to describe the traumatic and nontraumatic events that correspond with insomnia symptom onset in women Veterans and examine differences in sleep variables and PTSD and depression symptoms among women Veterans who endorsed traumatic events, nontraumatic events, or no events. The vast majority of women Veterans identified traumatic or nontraumatic events. Women Veterans who endorsed traumatic events reported significantly more severe insomnia, depression, and PTSD symptoms and poorer PSQI sleep quality than those who endorsed no events and significantly more severe PTSD symptoms, poorer PSQI sleep quality, and a longer duration of sleep problems than those who only endorsed nontraumatic events. Women Veterans who endorsed nontraumatic events reported significantly more severe insomnia and PTSD symptoms than women Veterans who endorsed no events. Significant group differences in insomnia, PTSD, and depression symptoms were observed across both total scores and clinical cutoff scores. No significant group differences were observed for diary and objective sleep efficiency or nightmare frequency.
The current findings are consistent with previous studies in demonstrating that most individuals with insomnia are able to link an event to the onset of their insomnia symptoms (Bastien et al., 2004; Healey et al., 1981). Our study builds upon prior work on the frequency and impact of traumatic and nontraumatic life events in women Veterans (Lehavot et al., 2018; Zinzow et al., 2007), suggesting that these events not only contribute to PTSD symptoms, but also to long-standing insomnia symptoms. The most commonly reported nontraumatic events in the current study (i.e., interpersonal, military, health, and work/school) correspond with the commonly reported events observed in the study by Bastien et al. (Bastien et al., 2004) (i.e., interpersonal, health, and work/school). The one difference between our findings and those of Bastien et al. (2004) can be attributed to the addition of the military events category in the current study, which is specific to a Veteran population.
The most commonly reported traumatic events were life threatening illness/injury and sexual assault. Previous studies have demonstrated that injury, pain, and illness are associated with greater sleep disturbance (Giannoccaro et al., 2013; Moldofsky, 2001; Taylor et al., 2007). Additionally, previous studies have found that women Veterans experience high rates of sexual assault (Maguen et al., 2012; Surís & Lind, 2008). Collectively, the findings suggest that women Veterans frequently link events involving health and interpersonal relationships to the onset of their insomnia symptoms. While comorbid medical conditions have received a great deal of attention in the sleep intervention literature, less research has focused on the role of interpersonal relationships in behavioral sleep interventions. This is an area that requires further exploration.
Results also showed that women Veterans who endorsed traumatic or nontraumatic events reported significantly more severe insomnia symptoms than those who endorsed no events. These findings suggest that insomnia symptoms are exacerbated in the presence of clear precipitating event(s), which is consistent with the “3-Ps” model of insomnia development (Spielman et al., 1987). The absence of a significant difference in insomnia symptoms between participants who endorsed traumatic events and those who only endorsed nontraumatic events suggests that the impact of life-threatening events may not always manifest in the form of more severe insomnia symptoms. Traumatic insomnia precipitating events may also be uniquely associated with insomnia chronicity and sleep quality. Women Veterans who endorsed traumatic events reported a longer duration of sleep problems than those who endorsed nontraumatic events and poorer PSQI sleep quality than women Veterans who reported nontraumatic events or no events. The findings may indicate that women Veterans who endorse traumatic insomnia precipitants go without insomnia treatment longer than women Veterans who endorse nontraumatic insomnia precipitants. While we cannot determine a causal relationship in the current study, it is possible that women Veterans who endorsed traumatic insomnia precipitating events also engage in more problematic sleep-related behaviors and have more factors contributing to sleep problems (i.e., worry, rumination, grief, and avoidance of sleep) than women Veterans who endorse nontraumatic events.
Traumatic insomnia precipitating events were also associated with the highest level of psychological distress. Women Veterans who endorsed traumatic events reported significantly greater PTSD symptoms than women Veterans who endorsed nontraumatic events or no events. Women Veterans who endorsed traumatic events also reported significantly greater depression symptoms than women Veterans who endorsed no events; however, there was no significant difference in depression symptom severity between women Veteran with traumatic and nontraumatic insomnia precipitating events. Collectively, the findings suggest that traumatic events are associated with increased insomnia and psychological distress symptom severity among women Veterans. It is unclear to what extent comorbid PTSD/depression symptoms moderate the course of insomnia symptoms. Additional research should examine whether women Veterans associate different events with their insomnia symptoms and symptoms of psychological distress. Women Veterans may perceive different events to precipitate different symptom sets. For example, some women Veterans in the current study endorsed multiple traumatic events, attributing their PTSD symptom onset to one traumatic event and their insomnia symptom onset to another traumatic event. These perceptions may impact both treatment preference and treatment response.
While multiple significant differences in sleep and psychological distress variables were observed in the expected direction among participants in the current study, no significant group differences were observed for objective and diary sleep efficiency or for nightmare frequency. The wrist actigraphy and the sleep diary used to assess sleep efficiency were distinct from the one-time, self-report measures used to assess all other outcome variables in that the actigraphy and sleep diary were collected prospectively over the course of a week. The nonsignificant differences for sleep efficiency may be partially attributed to these methodological differences. The findings may also indicate that traumatic and nontraumatic insomnia precipitants have a similar impact on sleep efficiency and their differences are better reflected in measures of patient-reported sleep quality, duration of sleep problems, and daytime impairment. The lack of significant differences may also be attributed to low sleep efficiency across all participants, regardless of insomnia precipitating event type (i.e., diary sleep efficiency = 78.03–79.56; objective sleep efficiency = 79.82–80.86). It is also well documented that depressed individuals are more likely to attend to negative information (Peckham et al., 2010). This may explain why group differences were only observed across subjective measures of sleep in the primary study analyses. Similarly, there are multiple methodological and conceptual explanations for the nonsignificant differences observed for nightmare frequency. A time frame of seven days may have been insufficient and not allowed for enough variability in nightmare frequency among groups. Another explanation may be that some women Veterans with insomnia symptoms avoid sleep as a strategy to avoid having nightmares, limiting the experience of nightmares in the current sample and the ability to detect significant difference in nightmare frequency. Future research is needed to better understand the effects of insomnia precipitating events on sleep efficiency and the experience of nightmares.
Findings of the current study are limited to women Veterans and may not generalize to other populations. Unstable housing and transportation limitations were exclusion criteria in the current study, limiting the information gathered from particularly vulnerable women Veterans. Due to the cross-sectional nature of the current study, causal inferences cannot be determined and future studies should examine how insomnia precipitating events (traumatic vs. nontraumatic) impact changes in sleep and mental health symptoms over time. This was a secondary analysis of baseline data from a behavioral sleep intervention study and information regarding insomnia precipitating events was limited to concise descriptions of events provided in an open-response format. The retrospective reporting of insomnia precipitating events may also limit the accuracy of participants’ responses. More sophisticated strategies to gather information regarding insomnia precipitating events may be useful in future studies. That being said, an iterative process was undertaken to ensure the validity and reliability of the event coding system, adequate interrater reliability was achieved, and no previous study has examined the traumatic nature of insomnia precipitating events. The current study did not include an assessment of lifetime traumatic events, injuries, or illnesses. It is possible that experiences, which occurred prior to the event(s) coinciding with insomnia symptom onset, influenced sleep and mental health symptoms and the potential impact of lifetime traumatic/medical experiences should be examined in future studies. The sleep diary did not contain a sleep quality item completed daily. The PSQI was the only measure of sleep quality in the current study. Given the exploratory nature of the current study, alpha adjustments were not included as part of the analyses; however, the large number of significant differences observed in the current study cannot be explained by type errors I alone. Furthermore, on diagnostic measures, total scores and cutoff scores were examined to demonstrate that group differences were both statistically significant and clinically meaningful.
The current study has a number of implications for the treatment of insomnia in women Veterans. Findings suggest that women Veterans who attribute their insomnia symptom onset to traumatic events may demonstrate a greater need for insomnia treatment as evidenced by increased symptom severity and comorbid PTSD. Previous studies have demonstrated that CBT-I is effective at improving sleep patterns in individuals with comorbid psychiatric conditions, including PTSD (Talbot et al., 2014), and CBT-I has been shown to contribute to improvements in depression symptoms (Cunningham & Shapiro, 2018; Wu et al., 2015). Women Veterans with comorbid insomnia disorder and PTSD would likely benefit from insomnia treatment. If women Veterans have a positive experience with CBT-I, their willingness to engage in trauma-focused treatment may increase as well. Presenting women Veterans with comorbid PTSD and insomnia disorder with all evidence-based treatment options for PTSD and insomnia is consistent with the shared decision-making model of clinical practice (Elwyn et al., 2012). Shared decision-making interventions have been shown to increase Veterans’ initiation of evidence-base treatments for PTSD (Hessinger et al., 2018; Mott et al., 2014). Finally, given the high rates of sexual trauma among women Veterans, a greater emphasis on trauma-informed care should be considered in the delivery of behavioral sleep interventions to women Veterans. Specific considerations include: the presence of a bed partner, the perceived safety of the sleeping environment, and women Veterans’ daytime behaviors.
The current findings provide information about the types of events that contribute to insomnia symptoms among women Veterans and demonstrate that traumatic insomnia precipitating events are associated with greater symptom severity than nontraumatic events or no events. While traumatic events are associated with greater symptom severity, future research is needed to determine how insomnia precipitating events (traumatic or nontraumatic) impact women Veterans’ treatment preferences, treatment engagement, and their responses to behavioral sleep interventions. Additional research is also needed to determine how comorbid PTSD and depression symptoms moderate or mediate the relationship between insomnia precipitating events and treatment outcomes. Future studies should examine potential barriers to both insomnia assessment and treatment in women Veterans and greater efforts are needed to reach members of particularly vulnerable and/or underserved groups. A greater understanding of the circumstances that precipitated and/or perpetuate insomnia symptoms will optimize the delivery of care and improve treatment outcomes among women Veterans.
Supplementary Material
Funding
This project was funded by VA/HSR&D IIR-HX002300 (PI: Martin), NIH/NHLBI K24HL143055 (PI: Martin); Dr. Carlson and Dr. Kelly were supported by the VA Office of Academic Affiliations through the Advanced Fellowship Programs in HSR&D and Women’s Health and the Advanced Fellowship Programs in HSR&D, and Advanced Geriatrics. Dr. Yano’s effort is funded by a VA HSR&D Senior Research Career Scientist Award (Project # RCS 05-195). Support was also provided by the VA Greater Los Angeles Geriatric Research, Education and Clinical Center.
Footnotes
Supplemental data for this article can be accessed on the publisher’s website.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Bastien CH, Vallieres A, & Morin CM (2004). Precipitating factors of insomnia. Behavioral Sleep Medicine, 2(1), 50–62. 10.1207/s15402010bsm0201_5 [DOI] [PubMed] [Google Scholar]
- Bastien CH, Vallières A, & Morin CM (2001). Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Medicine, 2(4), 297–307. 10.1016/S1389-9457(00)00065-4 [DOI] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders–fifth edition (PCL-5) in veterans. Psychological Assessment, 28(11), 1379. 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF III, Monk TH, Berman SR, & Kupfer DJ (1989). The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- Carney CE, Buysse DJ, Ancoli-Israel S, Edinger JD, Krystal AD, Lichstein KL, & Morin CM (2012). The consensus sleep diary: Standardizing prospective sleep self-monitoring. Sleep, 35(2), 287–302. 10.5665/sleep.1642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins D (2003). Pretesting survey instruments: An overview of cognitive methods. Quality of Life Research, 12(3), 229–238. 10.1023/A:1023254226592 [DOI] [PubMed] [Google Scholar]
- Cunningham JE, & Shapiro CM (2018). Cognitive behavioural therapy for insomnia (CBT-I) to treat depression: A systematic review. Journal of Psychosomatic Research, 106, 1–12. 10.1016/j.jpsychores.2017.12.012 [DOI] [PubMed] [Google Scholar]
- Drennan J (2003). Cognitive interviewing: Verbal data in the design and pretesting of questionnaires. Journal of Advanced Nursing, 42(1), 57–63. 10.1046/j.1365-2648.2003.02579.x [DOI] [PubMed] [Google Scholar]
- Ehring T, & Quack D (2010). Emotion regulation difficulties in trauma survivors: The role of trauma type and PTSD symptom severity. Behavior Therapy, 41(4), 587–598. 10.1016/j.beth.2010.04.004 [DOI] [PubMed] [Google Scholar]
- Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P,… Rollnick S (2012). Shared decision making: A model for clinical practice. Journal of General Internal Medicine, 27(10), 1361–1367. 10.1007/s11606-012-2077-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giannoccaro MP, Moghadam KK, Pizza F, Boriani S, Maraldi NM, Avoni P,… Plazzi G (2013). Sleep disorders in patients with spinal cord injury. Sleep Medicine Reviews, 17(6), 399–409. 10.1016/j.smrv.2012.12.005 [DOI] [PubMed] [Google Scholar]
- Haskell SG, Mattocks K, Goulet JL, Krebs EE, Skanderson M, Leslie D, … Brandt C (2011). The burden of illness in the first year home: Do male and female VA users differ in health conditions and healthcare utilization. Women’s Health Issues, 21(1), 92–97. 10.1016/j.whi.2010.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes P, & Krauthamer M (2009). Changing the face of health care for women veterans. Federal Practitioner, 26(2), 8–10. [Google Scholar]
- Healey SE, Kales A, Monroe LJ, Bixler EO, Chamberlin K, & Soldatos CR (1981). Onset of insomnia: Role of life-stress events1. Psychosomatic Medicine, 43(5), 439–451. 10.1097/00006842-198110000-00007 [DOI] [PubMed] [Google Scholar]
- Hessinger JD, London MJ, & Baer SM (2018). Evaluation of a shared decision-making intervention on the utilization of evidence-based psychotherapy in a VA outpatient PTSD clinic. Psychological Services, 15(4), 437. 10.1037/ser0000141 [DOI] [PubMed] [Google Scholar]
- Hughes J, Jouldjian S, Washington DL, Alessi CA, & Martin JL (2013). Insomnia and symptoms of post-traumatic stress disorder among women veterans. Behavioral Sleep Medicine, 11(4), 258–274. 10.1080/15402002.2012.683903 [DOI] [PubMed] [Google Scholar]
- Kelly UA, Skelton K, Patel M, & Bradley B (2011). More than military sexual trauma: Interpersonal violence, PTSD, and mental health in women veterans. Research in Nursing & Health, 34(6), 457–467. 10.1002/nur.20453 [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, & Friedman MJ (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress, 26(5), 537–547. 10.1002/jts.21848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimerling R, Makin-Byrd K, Louzon S, Ignacio RV, & McCarthy JF (2016). Military sexual trauma and suicide mortality. American Journal of Preventive Medicine, 50(6), 684–691. 10.1016/j.amepre.2015.10.019 [DOI] [PubMed] [Google Scholar]
- Krakow B, Hollifield M, Schrader R, Koss M, Tandberg D, Lauriello J, … Edmond T (2000). A controlled study of imagery rehearsal for chronic nightmares in sexual assault survivors with PTSD: A preliminary report. Journal of Traumatic Stress, 13(4), 589–609. 10.1023/A:1007854015481 [DOI] [PubMed] [Google Scholar]
- Krakow B, Schrader R, Tandberg D, Hollifield M, Koss MP, Yau CL, & Cheng DT (2002). Nightmare frequency in sexual assault survivors with PTSD. Journal of Anxiety Disorders, 16(2), 175–190. 10.1016/S0887-6185(02)00093-2 [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB, & Löwe B (2010). The patient health questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. General Hospital Psychiatry, 32(4), 345–359. 10.1016/j.genhosppsych.2010.03.006 [DOI] [PubMed] [Google Scholar]
- LeBlanc M, Mérette C, Savard J, Ivers H, Baillargeon L, & Morin CM (2009). Incidence and risk factors of insomnia in a population-based sample. Sleep, 32(8), 1027–1037. 10.1093/sleep/32.8.1027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehavot K, Goldberg SB, Chen JA, Katon JG, Glass JE, Fortney JC, … Schnurr PP (2018). Do trauma type, stressful life events, and social support explain women veterans’ high prevalence of PTSD? Social Psychiatry and Psychiatric Epidemiology, 53(9), 943–953. 10.1007/s00127-018-1550-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maguen S, Cohen B, Ren L, Bosch J, Kimerling R, & Seal K (2012). Gender differences in military sexual trauma and mental health diagnoses among Iraq and Afghanistan veterans with posttraumatic stress disorder. Women’s Health Issues, 22(1), e61–e66. 10.1016/j.whi.2011.07.010 [DOI] [PubMed] [Google Scholar]
- Martin JL, Schweizer CA, Hughes JM, Fung CH, Dzierzewski JM, Washington DL, … Josephson KR (2017). Estimated prevalence of insomnia among women veterans: Results of a postal survey. Women’s Health Issues, 27(3), 366–373. 10.1016/j.whi.2016.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moldofsky H (2001). Sleep and pain. Sleep Medicine Reviews, 5(5), 385–396. 10.1053/smrv.2001.0179 [DOI] [PubMed] [Google Scholar]
- Morgenthaler T, Alessi C, Friedman L, Owens J, Kapur V, Boehlecke B, … Lee-Chiong T (2007). Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: An update for. Sleep, 30(4), 519–529. 10.1093/sleep/30.4.519 [DOI] [PubMed] [Google Scholar]
- Mott JM, Stanley MA, Street RL Jr, Grady RH, & Teng EJ (2014). Increasing engagement in evidence-based PTSD treatment through shared decision-making: A pilot study. Military Medicine, 179(2), 143–149. 10.7205/MILMED-D-13-00363 [DOI] [PubMed] [Google Scholar]
- National Center for Veterans Analysis and Statistics. (2013). National center for veterans analysis and statistics: Veteran population. 2013. www.va.gov/VETDATA/Veteran_Population.asp
- National Center for Veterans Analysis and Statistics. (2015). Figure 20. Ten most prevalent primary service-connected disabilities for women veterans: 2015. https://www.va.gov/vetdata/docs/SpecialReports/Women_Veterans_2015_Final.pdf
- O’Donnell ML, Creamer M, & Pattison P (2004). Posttraumatic stress disorder and depression following trauma: Understanding comorbidity. American Journal of Psychiatry, 161(8), 1390–1396. 10.1176/appi.ajp.161.8.1390 [DOI] [PubMed] [Google Scholar]
- Ohayon MM, & Shapiro CM (2000). Posttraumatic stress disorder in the general population. Comprehensive Psychiatry, 41(6), 469–478. 10.1053/comp.2000.16568 [DOI] [PubMed] [Google Scholar]
- Olejnik S, & Algina J (2000). Measures of effect size for comparative studies: Applications, interpretations, and limitations. Contemporary Educational Psychology, 25(3), 241–286. 10.1006/ceps.2000.1040 [DOI] [PubMed] [Google Scholar]
- Peckham AD, McHugh RK, & Otto MW (2010). A meta-analysis of the magnitude of biased attention in depression. Depression and Anxiety, 27(12), 1135–1142. 10.1002/da.20755 [DOI] [PubMed] [Google Scholar]
- Qaseem A, Kansagara D, Forciea MA, Cooke M, & Denberg TD (2016). Management of chronic insomnia disorder in adults: A clinical practice guideline from the American college of physicians. Annals of Internal Medicine, 165(2), 125–133. 10.7326/M15-2175 [DOI] [PubMed] [Google Scholar]
- Rytwinski NK, Scur MD, Feeny NC, & Youngstrom EA (2013). The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: A meta-analysis. Journal of Traumatic Stress, 26(3), 299–309. [DOI] [PubMed] [Google Scholar]
- Shakespeare-Finch J, & Armstrong D (2010). Trauma type and posttrauma outcomes: Differences between survivors of motor vehicle accidents, sexual assault, and bereavement. Journal of Loss & Trauma, 15(2), 69–82. 10.1080/15325020903373151 [DOI] [Google Scholar]
- Spielman AJ, Caruso LS, & Glovinsky PB (1987). A behavioral perspective on insomnia treatment. Psychiatric Clinics, 10(4), 541–553. [PubMed] [Google Scholar]
- StataCorp. (2017). Stata statistical software: Release: 15. [Google Scholar]
- Surís A, & Lind L (2008). Military sexual trauma: A review of prevalence and associated health consequences in veterans. Trauma, Violence & Abuse, 9(4), 250–269. 10.1177/1524838008324419 [DOI] [PubMed] [Google Scholar]
- Talbot LS, Maguen S, Metzler TJ, Schmitz M, McCaslin SE, Richards A, … Ruoff L (2014). Cognitive behavioral therapy for insomnia in posttraumatic stress disorder: A randomized controlled trial. Sleep, 37(2), 327–341. 10.5665/sleep.3408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor DJ, Mallory LJ, Lichstein KL, Durrence HH, Riedel BW, & Bush AJ (2007). Comorbidity of chronic insomnia with medical problems. Sleep, 30(2), 213–218. 10.1093/sleep/30.2.213 [DOI] [PubMed] [Google Scholar]
- Tsuno N, Besset A, & Ritchie K (2005). Sleep and depression. The Journal of Clinical Psychiatry, 66(10), 1254–1269. 10.4088/JCP.v66n1008 [DOI] [PubMed] [Google Scholar]
- Washington DL, Davis TD, Der-Martirosian C, & Yano EM (2013). PTSD risk and mental health care engagement in a multi-war era community sample of women veterans. Journal of General Internal Medicine, 28(7), 894–900. 10.1007/s11606-012-2303-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013). The life events checklist for DSM-5 (LEC-5). Instrument available from the national center for PTSD. www.ptsd.va.gov
- Willis GB, Royston P, & Bercini D (1991). The use of verbal report methods in the development and testing of survey questionnaires. Applied Cognitive Psychology, 5(3), 251–267. 10.1002/acp.2350050307 [DOI] [Google Scholar]
- Wilson LC (2018). The prevalence of military sexual trauma: A meta-analysis. Trauma, Violence & Abuse, 19(5), 584–597. 10.1177/1524838016683459 [DOI] [PubMed] [Google Scholar]
- Wu JQ, Appleman ER, Salazar RD, & Ong JC (2015). Cognitive behavioral therapy for insomnia comorbid with psychiatric and medical conditions: A meta-analysis. JAMA Internal Medicine, 175(9), 1461–1472. 10.1001/jamainternmed.2015.3006 [DOI] [PubMed] [Google Scholar]
- Zinzow HM, Grubaugh AL, Monnier J, Suffoletta-Maierle S, & Frueh BC (2007). Trauma among female veterans: A critical review. Trauma, Violence & Abuse, 8(4), 384–400. 10.1177/1524838007307295 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


