Abstract
Background and Hypothesis
Quantitative models of psychopathology can empirically guide subclassification of heterogeneous clinical presentations such as psychosis; they are particularly well-equipped to capture the nuanced symptomatology observed in first-episode psychosis. As well, components may be better aligned with biological variables. The current study sought to confirm and extend knowledge of the hierarchical structure of psychosis symptoms in first-episode psychosis. Based on past hierarchical work, we hypothesized that a 4 component level would be most closely associated with longitudinal disability.
Study Design
Participants with early-stage psychosis (N = 370) underwent clinical assessment with the scale for the assessment of positive symptoms (SAPS), scale for assessment of negative symptoms (SANS), and global assessment scale(GAS). A subset was assessed at 6 months (N = 221) and 1 year (N = 207). Hierarchical symptom components were extracted at 12 levels. The predictive utility of the components for global functioning was tested.
Study Results
As predicted, the 4-component model (reality distortion, thought disorder, inexpressivity, apathy/asociality) provided a superior prediction of functioning over other levels of the hierarchy. Baseline apathy/asociality longitudinally predicted functioning beyond the shared variance of the components at 6 months (b = −4.83, t(216) = −5.37, p < .001, R2adj = 0.12) and 1-year (b = −4.49, t(202) = −4.38, p < .001, R2adj = 0.09).
Conclusions
The hierarchical structure of psychotic symptomatology and its external validity have been robustly established in independent, longitudinal first-episode psychosis samples. The established model incorporates multiple levels of granularity that can be flexibly applied based on the level that offers the greatest predictive utility for external validators.
Keywords: schizophrenia, principal component analysis (PCA), dimensional classification, functional impairment
Introduction
Psychosis is a heterogeneous spectrum of psychopathology. It has traditionally been defined by categorical diagnoses: Schizophrenia spectrum disorders, bipolar disorders, and major depressive disorders with psychotic features. Contemporary taxonomical models quantify symptoms dimensionally, from subclinical to clinical severity, then group related symptoms into empirically-based spectra.1 This approach offers a robust, reliable structure that is inclusive of emerging and severe symptom expression; it also reduces arbitrary boundaries between highly overlapping diagnostic phenotypes. Research has robustly demonstrated that the psychosis spectrum has shared risk factors, genetics, neural and cognitive deficits, and prognostic features, supporting a transdiagnostic approach across multiple measurement domains. Dimensional models may be particularly useful in guiding assessment and treatment in the early stages of illness when some symptoms are subtle and do not reach clinical thresholds.
Psychosis has often been discussed in terms of 2 (positive, negative) or 3 (positive, negative, disorganized/cognitive) symptom domains with various symptoms loading onto these factors.2–7 However, factor solutions vary, and thus the underlying dimensional structure of the psychotic spectrum is debated.3,8 Hierarchical models establish a structure that incorporates multiple levels so that various degrees of specificity can be considered within a cohesive structure. Hierarchical Taxonomy of Psychopathology (HiTOP) is one of the most well-developed, prominent, and empirically supported classification systems.9,10 Psychosis is 1 of 3 overarching spectra (“super spectra”) in HiTOP. The psychosis super spectrum splits into thought disorder, inclusive of positive and disorganized symptoms, and detachment, which includes negative symptoms, with more specific traits and symptom components at lower levels. The delineations align with previous factor analyses and widen the psychosis phenotype to include subclinical experiences such as fantasy proneness.
As dimensional models become more established, it is important to examine signs, symptoms, and behavior in first-episode psychosis when symptom expression is relatively subtle and can extend beyond the strict boundaries of taxonomic approaches described in diagnostic manuals. Categorical diagnoses for psychosis are particularly unstable in the early stages of illness or when symptoms are less severe.11–13 In contrast, dimensions show good longitudinal reliability.14,15 Furthermore, a hierarchical dimensional approach provides enough detail to identify the domain in which symptom changes occur and the degree to which the change affects the overall clinical profile. Expanding research on the psychosis spectrum through replication and a wide range of samples, ages, and symptom severity will buoy the empirical support and clinical utility of the model.
We sought to extend previous work investigating whether the Scale for the Assessment of Negative Symptoms (SANS)16 and Scale for the Assessment of Positive Symptoms (SAPS),17 some of the most broadly used psychosis symptom rating instruments, would form a symptom hierarchy in first-episode psychosis individuals aligned with contemporary dimensional models of psychosis. Our central aims were to: (1) derive a hierarchical model that articulates grouping of symptom items at various levels of detail, from broad to fine-grained; (2) examine the utility of each level of the hierarchy in predicting functioning at future time points; (3) establish whether the hierarchical components and the predictive utility of the components are consistent over time; (4) lastly, demonstrate how existing instruments are relevant to dimensional applications so that past and future work in the field can be bridged. Only 1 previous study, Kotov et al. (2016), performed a hierarchical analysis of psychotic symptoms at first hospital admission and linked symptom factors to longitudinal disability. The current analysis extends that work by recruiting a sample that is uniformly early in the illness course (mean age < 25 years), known to have minimal antipsychotic exposure, and more racially diverse. We hypothesized that we would derive a structure consistent with past work that has shown a reliable structure across illness trajectory, with 4 components providing the best predictive utility for functional outcome. Among the components, we expected negative symptoms to predict functioning most strongly, replicating Kotov et al and past work by the authors showing the predictive utility of affective and negative symptoms for functioning over and above acute psychotic symptoms in long-term recovery.
Method
Participants
The sample consisted of 370 individuals in the acute phase of the first-episode of a psychotic disorder who completed an initial clinical research assessment with the University of Pittsburgh Department of Psychiatry Psychosis Research Clinical Core from 1990 to 2019. Participants were recruited via UPMC Western Psychiatric Hospital inpatient and outpatient services. A subsample was assessed 6 months (n = 221) and 1 year (n = 207) later. At the baseline and follow-up visits, participants underwent a diagnostic evaluation that included a clinical interview and symptom assessment. Psychotic diagnoses were determined by the Structured Clinical Interview for DSM-IV (SCID-IV)18,19 and consensus conference review. Participants who were enrolled 1990–1994, prior to release of DSM-IV, underwent structured clinical interviews for DSM-III-R; diagnoses were later converted to DSM-IV codes via consensus conference review. Participants with diagnoses of schizophreniform, schizoaffective disorder, schizophrenia, brief psychotic disorder, delusional disorder, psychotic disorder NOS, bipolar I disorder, bipolar II disorder, bipolar NOS, and major depressive disorder with psychotic features were included (see table 1). First-episode was defined as individuals within their initial psychotic episode, and with less than 2 months duration of antipsychotic use in their lifetime.
Table 1.
Sample Characteristics
| Baseline | Six Months | One Year | |
|---|---|---|---|
| n = 370 | n = 221 | n = 207 | |
| Sex | |||
| Male | 229 (62%) | 138 (62%) | 135 (65%) |
| Female | 141 (38%) | 83 (38%) | 72 (35%) |
| Age | 24.25 (7.49) | 24.76 (7.58) | 25.25 (7.83) |
| Race/ethnicity | |||
| White | 214 (58%) | 136 (62%) | 125 (60%) |
| Black/African American | 127 (34%) | 70 (32%) | 66 (32%) |
| Asian/Pacific Islander | 19 (5%) | 12 (5%) | 12 (6%) |
| LatinX/Hispanic | 2 (1%) | 0 (0%) | 0 (0%) |
| Native American/Hawaiian Native | 3 (1%) | 2 (1%) | 2 (1%) |
| Other | 4 (1%) | 1 (1%) | 2 (1%) |
| Diagnosis | |||
| Schizophrenia | 157 (42%) | 96 (43%) | 83 (40%) |
| Schizoaffective disorder | 32 (9%) | 23 (10%) | 24 (12%) |
| Schizophreniform | 33 (9%) | 22 (10%) | 20 (10%) |
| Psychotic disorder NOS | 61 (16%) | 33 (15%) | 30 (14%) |
| Brief psychotic disorder | 4 (1%) | 2 (1%) | 3 (1%) |
| Delusional disorder | 16 (4%) | 9 (4%) | 10 (5%) |
| Bipolar I disorder | 23 (6%) | 14 (6%) | 16 (8%) |
| Bipolar II disorder | 2 (1%) | 0 (0%) | 0 (0%) |
| Bipolar disorder NOS | 1 (0%) | 1 (0%) | 0 (0%) |
| Major depressive disorder | 41 (11%) | 21 (10%) | 21 (10%) |
Notes: Standard deviation is listed in parentheses for age. Sex, race, and diagnoses are listed as counts. Participants can identify as more than 1 race, thus numbers may be greater than the sample size at a given time point. Percentages may not sum to 100% due to rounding.
All participants were fluent English speakers, 12 to 50 years old, with normal, or corrected hearing and vision, and intelligence quotient (IQ) of at least 70 years. On average, participants reported the start of the prodromal period began at age 20.63 (SD = 8.02; median = 18.86). The estimated time between prodrome onset and onset of the first psychotic episode was 1.84 years (SD = 3.46; median = 0.34). For those who were admitted to the hospital for treatment of psychosis, the age of initial psychiatric hospitalization for psychosis was 23.26 (SD = 7.64; median = 21).1 Research procedures aligned with the Declaration of Helsinki and were approved by the University of Pittsburgh Institutional Review Board. All participants provided written informed consent, and received compensation for participation.
Measures
Clinical interviewers rated current symptomatology using the semi-structured SANS and SAPS interviews. The NIMH Modified SANS version was used, which does not include “Inappropriate Affect,” for a total of 23 items. Consistent with the NIMH Modified SANS version, SANS items were rated on a scale of 1 (None) to 5 (Severe). SAPS items were rated on the standard scale of 0 (None) to 5 (Severe). A total of 48 items (29 SAPS, 19 SANS) were included in the analysis. SAPS item “Clanging” was excluded from analysis because there was no variation in scores (all ratings were 0). As well, SANS and SAPS global symptom rating scores were excluded from analysis. Global functioning was estimated using the global assessment scale (GAS), a brief clinical rating of overall functioning. Measures were assessed at each time point.
Analysis
The hierarchical structure of SANS and SAPS symptoms at baseline was estimated with a “bass-Ackwards” model,20 which allowed us to examine the relationship between multiple levels of specificity. We iteratively extracted all levels from 1 to 12 components using the bassAckward function in the psych package (v1.9.2) of R.21 Twelve components were chosen as the upper limit based on parallel analysis,22 interpretability, and direct comparison with previous work (eg, Kotov et al., 2016). Components were extracted using the principal component analysis (PCA) method, which is consistent with the original Goldberg bass-Ackwards application,20 and promax rotation. Correlations were specified as “mixed” to allow for a mixture of continuous, dichotomous, and polytomous variables, a method that minimizes bias in zero-inflated data that is common to symptom measures.23 Items with primary component loadings ≥ 0.4 were assigned to that component; when cross-loadings occurred, items were assigned to the component on which the loading was highest.
Component scores were calculated for all time points by applying the baseline loadings using the Thurstone regression method. Missing data were imputed using median values. At baseline, 337 of 370 participants had complete data; missing values amounted to 0.52% of the baseline item-level data. Among participants with longitudinal data, less than 1% were missing at each time point. We investigated convergence across time points by calculating correlations between the same component at baseline and 6 months, and baseline and 1 year. We also examined correlations between different components to ensure convergence (correlation of the same component across time) was greater than divergence (correlation of different components with each other across time points).
Lastly, we tested the predictive utility of each level of the hierarchical model using hierarchical linear regressions at all 3 time points. Each regression model tested the proportion of variance in functioning, as measured by GAS, predicted by the symptom components at a given level. For each time point, the levels were then compared by ANOVA which indicated whether each level incrementally predicted a greater degree of variance in functioning, as quantified by a significant change in adjusted R-squared. Bonferroni corrections for multiple comparisons were applied.
Results
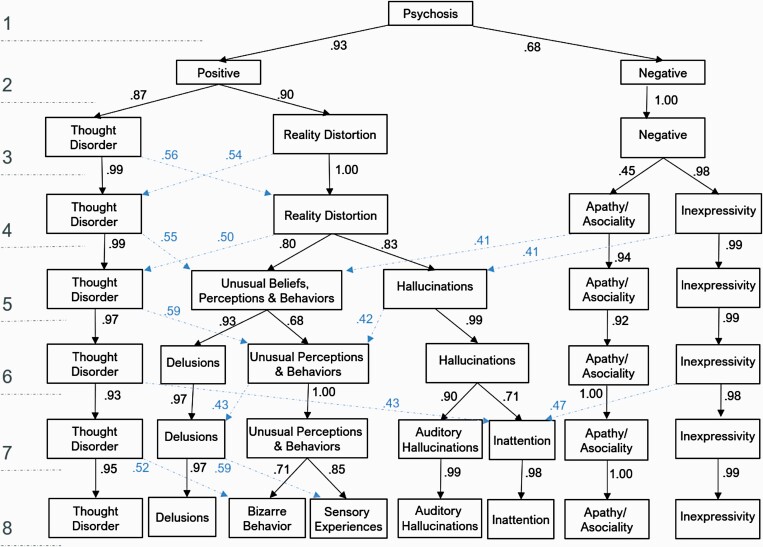
Baseline SANS and SAPS data were extracted to form a hierarchical model with up to 12 components. However, interpretability and stability of the components deteriorated with 9 or more components. Beginning at level 9, components contained fewer than 3 items, which is below the guidelines for PCA and factor analysis, and items inconsistently shifted between components, which suggests that components beyond level 9 were over-extracted.24 Parallel analysis also suggested that the optimal number of components was 8. Thus, we focused on levels 1 through 8 (see figure 1). At upper levels of the hierarchy, symptoms formed components that have been widely demonstrated in the schizophrenia literature. At level 2, positive and negative components emerged. At level 3, positive symptoms split into reality distortion (unusual beliefs, perceptions, and behaviors including hallucinations and delusions) and thought disorder (problems expressing thought content). At level 4, negative symptoms split into inexpressivity (reduced facial expressions, speech, gestures, and movement) and apathy/asociality (anergia, anhedonia, and interpersonal activities). The items contributing to the 4-component level—the most informative level of the hierarchy for the current analysis—are detailed in table 2; coefficients for other levels of the hierarchy can be found in Supplementary tables S3-S9. Components I—IV are reality distortion, inexpressivity, thought disorder, and apathy/asociality, respectively. At lower levels of the hierarchy thought disorder, apathy/asociality, and inexpressivity remained intact while reality distortion (within positive symptoms) was partitioned into more fine-grained components. The 4-component structure at baseline had convergent correlations higher than discriminant correlations for all 4 components at the 6-month and 1-year timepoints, meaning that each component was more similar to itself over time than to the other components (Supplementary table S1). Convergence between baseline and 6 months was highest for reality distortion (r = 0.35) and lowest for thought disorder (r = 0.27). Convergence at 1 year was highest for thought disorder (r = 0.31) and lowest for apathy/asociality (r = 0.27).
Fig. 1.
Hierarchical components of psychosis.The bass-Ackwards method was used to iteratively derive a hierarchical structure of symptoms based on SAPS and SANS item ratings made during a structured clinical interview. The hierarchy was readily interpretable up to 8 factors, as illustrated here. Level 4 offered the greatest predictive power in terms of global functioning scores. Intercorrelations of components at adjacent levels are reported by solid lines. Dotted lines note strong correlations ( ≥ 0.4) between levels (eg, reality distortion at level 3 with thought disorder at level 4).
Table 2.
Four Component Solution: Item-Level Loadings
| Item | I | II | III | IV |
|---|---|---|---|---|
| SAPS 1: Auditory hallucinations | 0.82 | 0.05 | −0.31 | −0.05 |
| SAPS 3: Voices conversing | 0.81 | 0.08 | −0.22 | −0.16 |
| SAPS 6: Visual hallucinations | 0.79 | 0.00 | −0.19 | −0.21 |
| SAPS 2: Voices commenting | 0.77 | 0.10 | −0.14 | −0.17 |
| SAPS 17: Thought broadcasting | 0.68 | 0.05 | −0.03 | 0.17 |
| SAPS 4: Somatic or tactile hallucinations | 0.67 | −0.05 | −0.11 | 0.03 |
| SAPS 18: Thought insertion | 0.65 | −0.04 | −0.03 | 0.32 |
| SAPS 5: Olfactory hallucinations | 0.64 | 0.04 | 0.02 | −0.12 |
| SAPS 16: Delusions of mind reading | 0.64 | −0.02 | −0.06 | 0.27 |
| SAPS 19: Thought withdrawal | 0.58 | 0.02 | 0.14 | 0.13 |
| SAPS 15: Delusions of being controlled | 0.47 | −0.22 | 0.16 | 0.35 |
| SAPS 11: Grandiose delusions | 0.41 | −0.25 | 0.27 | 0.03 |
| SANS 3: Paucity of expressive gesture | 0.05 | 0.88 | −0.07 | −0.01 |
| SANS 6: Lack of vocal inflections | −0.09 | 0.85 | 0.02 | 0.13 |
| SANS 9: Poverty of speech | 0.11 | 0.85 | −0.06 | −0.10 |
| SANS 5: Affective nonresponsivity | 0.03 | 0.84 | −0.08 | 0.14 |
| SANS 2: Decreased spontaneous movement | 0.01 | 0.83 | −0.11 | −0.02 |
| SANS 1: Unchanging facial expressions | −0.02 | 0.82 | −0.06 | 0.15 |
| SANS 12: Increased latency of response | 0.06 | 0.65 | 0.29 | −0.02 |
| SANS 4: Poor eye contact | −0.03 | 0.64 | 0.22 | 0.06 |
| SANS 23: Social inattentiveness | 0.12 | 0.46 | 0.40 | −0.13 |
| SAPS 26: Derailment | −0.11 | −0.05 | 0.85 | 0.13 |
| SANS 10: Poverty of speech content | −0.26 | −0.02 | 0.80 | 0.02 |
| SAPS 28: Incoherence | −0.21 | 0.27 | 0.78 | 0.08 |
| SAPS 27: Tangentiality | −0.09 | 0.02 | 0.76 | 0.16 |
| SAPS 31: Pressure of speech | −0.18 | -0.42 | 0.74 | −0.13 |
| SAPS 30: Circumstantiality | −0.13 | -0.40 | 0.74 | 0.05 |
| SAPS 29: Illogicality | −0.11 | 0.01 | 0.73 | 0.20 |
| SAPS 32: Distractible speech | 0.17 | 0.16 | 0.61 | −0.17 |
| SANS 11: Thought blocking | 0.15 | 0.34 | 0.48 | −0.11 |
| SAPS 22: Social and sexual behavior | 0.36 | 0.00 | 0.43 | −0.20 |
| SAPS 21: Clothing and appearance | 0.32 | 0.08 | 0.40 | −0.13 |
| SANS 21: Relationships with friends/Peers | −0.20 | 0.10 | 0.12 | 0.73 |
| SANS 20: Ability to feel intimacy/closeness | −0.18 | 0.11 | 0.06 | 0.67 |
| SAPS 8: Persecutory delusions | 0.16 | −0.20 | 0.02 | 0.61 |
| SANS 15: Impersistence at work/school | −0.09 | 0.13 | 0.15 | 0.54 |
| SANS 18: Recreational interests and activities | 0.21 | 0.28 | −0.23 | 0.48 |
| SANS 16: Physical anergia | 0.00 | 0.30 | 0.00 | 0.45 |
| SANS 19: Sexual interest and activity | 0.03 | 0.08 | 0.05 | 0.40 |
| SAPS 9: Delusions of jealousy | 0.39 | −0.03 | 0.18 | −0.03 |
| SAPS 13: Somatic delusions | 0.35 | −0.03 | 0.21 | 0.17 |
| SAPS 24: Repetitive or stereotyped behavior | 0.26 | 0.18 | 0.26 | -0.19 |
| SANS 24: Inattentiveness in MSE | 0.12 | 0.10 | 0.06 | 0.10 |
| SANS 14: Grooming and hygiene | −0.01 | 0.20 | 0.39 | 0.25 |
| SAPS 23: Aggressive and agitated behavior | 0.22 | -0.07 | 0.33 | −0.18 |
| SAPS 12: Religious delusions | 0.26 | −0.17 | 0.28 | 0.05 |
| SAPS 14: Delusions of reference | 0.36 | −0.32 | 0.04 | 0.39 |
| SAPS 10: Delusions of guilt or sin | 0.29 | 0.03 | 0.02 | 0.30 |
Note: Loadings ≥ 0.4 are bolded. Component I is Reality Distortion; II is Inexpressivity; III is Thought Disorder; IV is Apathy/Asociality. Nine items did not load sufficiently on any component (r < 0.4; see bottom of table); the highest loadings for these items are designated by italics. MSE = Mental Status Exam.
Among the 8 levels, the 4-component model (reality distortion, thought disorder, inexpressivity, apathy/asociality) provided superior external validity. The 3-component (F3, 365 = 31.17, p < .01, R2adj = 0.20), 4-component (F4, 364 = 33.85, p < .001, R2adj = 0.26) and 5-component (F5, 353 = 32.98, p < .001, R2adj = 0.30) models accounted for significantly more variance than other levels of the symptom hierarchy in explaining concurrent baseline functioning (Supplementary table S2). However, only the 4-component model demonstrated significant predictive validity over other levels of the hierarchy at 6-months (F4, 215 = 8.23, p < .001, R2adj = 0.12) and 1-year (F4, 202 = 6.07, p < .001, R2adj = 0.09). While baseline thought disorder predicted a small portion of baseline functioning (b = −2.02, t(364) = −3.95, p < .001, R2 = 0.003 in the 4-component model), it did not predict future functioning. Apathy/asociality persisted in accounting for significant variance beyond that shared by other components in concurrent (b = −3.49, t(364) = −7.48, p < .001, R2 = 0.11) and prospective functioning levels (6-months: b = −4.83, t(215) = −5.37, p < .001, R2 = 0.11; 1-year: b = −4.49, t(202) = −4.38, p < .001, R2 = 0.08). The other 2 components at level 4 of the hierarchy—reality distortion and inexpressivity—did not uniquely predict functioning levels at initial assessment, 6-months, or 1-year. Regressions for all levels are reported in Supplementary table S2; zero-order correlations between level 4 components and functioning are in Supplementary table S1.
Discussion
We derived a hierarchical model of symptoms of psychosis that illustrated how items form complementary groupings from broad to fine-grained within a single multi-level structure. The components were theoretically and analytically supported up to level 8, ranging from 1 to 8 symptom components. Models with more than 8 components were minimally interpretable and decomposed into patterns of variance that did not clearly map onto conceptual units or follow empirical guidelines for factor analysis. As found by Kotov et al., our level 4 of the hierarchy (eg, reality distortion, thought disorder, inexpressivity, and apathy/asociality) provided the best balance of reliability and external validity.25
The model we derived is consistent with previous symptom models.2–7,9 At level 2, symptoms formed a positive and negative component, with positive symptoms splitting into 2 components (reality distortion and thought disorder) at level 3. Many 3-factor models characterize positive symptoms, disorganization, and negative symptoms. The content in our thought disorder component differed slightly from what is generally a broader disorganization component. Aspects typically seen in disorganization, such as bizarre behaviors and poor grooming, instead emerged from the reality distortion component suggesting that symptoms covary slightly differently early in illness.
Level 4 of our model was the most powerful predictor of future functioning, adding to the evidence that 4 components offer superior utility to other levels in predicting longitudinal functioning. At level 4, negative symptoms branched into 2 components (apathy/asociality and inexpressivity), with the unique variance of apathy/asociality providing the strongest predictor of future global functioning levels. Multiple large-scale analyses of clinical assessment scales with broader content coverage of psychopathology have also indicated 4 factors in psychotic disorders, with 2 factors reflecting positive symptoms and 2 reflecting negative or affective symptoms.26–28 Within the existing HiTOP hierarchical model, inexpressivity largely aligns with the detachment spectra whereas there are 2 possibilities for apathy/asociality. First, the apathy/asociality component likely shares variance with broad definitions of internalizing due to the focus on intimacy and relationships with others. SANS content does not provide sufficient coverage of internalizing, such as anxious and depressive symptoms, leaving apathy/asociality as the most closely aligned component. Second, the content of apathy/asociality includes intimacy avoidance and social withdrawal, which suggests that both the subcomponents of negative symptoms in the current model could reflect the detachment spectra. While much research has shown the association between detachment and functional outcome, few studies have investigated the contribution of internalizing to recovery in psychosis.29 Without the inclusion of both internalizing and detachment, it is unclear which contributes a unique effect. Importantly, the findings here, along with previously published findings,29,30 emphasize that, though acute positive symptoms are highly distressing, affective and negative symptoms have strong, enduring effects on the outcome. The external validity of our findings is important in the context of existing 3-factor models of psychosis. Level 4 offered greater specificity and larger effect sizes than level 3 in predicting global functioning, specifically showing that high levels of interpersonal withdrawal—rather than negative symptoms broadly—lead to functional impairment. Additionally, our findings offer some resolution to the debate over the number of symptom factors.
Hierarchical models demonstrate that there is an advantage to dynamically considering multiple levels of specificity instead of determining a static number of factors that represent psychosis. That is, multiple levels of dimensional resolution can be simultaneously empirically supported. The appropriate level of specificity may be dependent on the context and research question. Here, 4 components were best at predicting future global functioning. Given other variables of interest, we might find utility from a different level. For example, associations with genetic variables are likely to exist at higher, broad levels.31,32
On the other hand, a more detailed level might be superior for considering specific neural processes; at level 7 auditory hallucinations form a component separate from other sensory experiences. Thus, a 7-component model might be relevant to an analysis examining variance unique to auditory processing. This split in sensory modalities also highlights symptom expression that may be distinctive to early stages of psychosis and overlooked in current models. Among positive symptoms of psychosis, auditory hallucinations are particularly prevalent in first-episode psychosis and are associated with a higher risk for conversion to psychosis in high-risk samples.33 Yet, most assessment tools cluster auditory, visual, somatic, tactile, and olfactory experiences without regard for sensory modality. Our findings suggest that sensory modalities may show a different pattern in early psychosis, with auditory hallucinations particularly prominent among positive symptoms. Furthermore, the findings emphasize the need for models that represent fine-grained symptom groupings that differentiate between sensory modalities.
Item covariance at different levels offer informative details within other symptom components as well. For example, persecutory delusions primarily load on the delusions factor at level 6 and beyond. However, among broader components the item loads most strongly on apathy/asociality, perhaps reflecting suspiciousness and feelings of social penalization at the core of the delusion. Other dimensional models have likewise shown that suspiciousness loads with negative symptoms or detachment.34,35 At level 7, unusual perceptions and behaviors and apathy/asociality both include interpersonal elements. However, apathy/asociality includes content related to engagement and closeness in social settings, such as the ability to feel intimacy, while unusual perceptions and behaviors captures a state that may influence social interactions such as agitated behavior and delusions of jealousy. Among a broader characterization of psychopathology, it is conceivable that elements of this low-level unusual perceptions and behaviors component would show a cross-loading with externalizing.
These findings extend the work by Kotov et al. (2016) by demonstrating a comparable hierarchical structure and external relevance in a second distinct and rigorously designed early psychosis protocols. Our sample is younger (median age of 24 years as compared to 29 years in the Suffolk County sample), and more racially diverse (White: 58% vs 77%; Black/African American: 34% vs 15%). As well, our exclusion criteria explicitly restricted duration of antipsychotic exposure, which resulted in a relatively high percentage of participants with minimal or no lifetime antipsychotic exposure. The findings not only replicate Kotov et al.’s findings, but show that the structure is generalizable across a wide array of people experiencing the early stages of psychosis.
The constrained symptom range of SANS and SAPS (eg, exclusion of mood symptomatology and emphasis of positive and disorganization symptoms) limits the degree to which the current study can be compared to broader models of psychopathology such as HiTOP. Future work can incorporate a full range of psychopathology to fully account for mania symptoms within affective psychotic disorders (eg, bipolar disorder), as well as depression, anxiety, and substance use problems that commonly co-occur with primary psychotic disorders. Utilizing a variety of scales will ensure that a similar hierarchy emerges regardless of the instrument. The external indicators were also limited in depth (eg, GAS is a brief snapshot of functioning) and breadth due to limitations in the measures administered in the sample. The GAS is weighted toward social outcomes while SANS embeds social behaviors and motivation in the symptom ratings. The common content on apathy/asociality items and the functioning measure results in a degree of overlap in the predictor and criterion measures. Both areas offer opportunities for extension that incorporates a rich array of social functioning, cognitive, and biological measures. For example, cognitive deficits have been shown to be one of the strongest predictors of functional outcome36 and could be incorporated alongside symptom variables in models predicting functional outcome. Currently, we are collecting more robust symptom ratings, personality measures, cognitive measures, and social functioning scales to capture a more nuanced and comprehensive picture of symptoms and functioning in first-episode psychosis and prodromal states.
In summary, we detected a multilevel hierarchy of symptom components that parsed psychosis at increasing levels of construct specificity. The hierarchical model was robust and indicated both a specific level and construct that best-predicted outcome. However, the benefit of the hierarchical model is that more (or less) fine-grained constructs and dimensions can be assessed for specific research and clinical questions. The findings are an important bridge between earlier dimensional approaches to measurement based on theoretically driven clustering of symptoms (eg, positive and negative dimensions), and contemporary empirically-based classifications of psychopathology. Few studies have considered both the intercorrelation of symptoms and how they predict real-world factors. Here, the relationship between symptom groupings and external validators is used as a guide to the most relevant level of the hierarchical model. Understanding the level of symptom specificity that best predicts different units of analysis has the potential to build mechanistic accounts for clinical profiles at varying levels of construct complexity. This approach may aid in identification of underlying system-level pathology and development of personalized interventions targeting these associated neurobiological systems.
Supplementary Material
Acknowledgment
Thank you first and foremost to the research participants who so generously volunteered their time to advance our knowledge of first-episode psychosis. Additional thanks to the research staff who facilitated study administration and data collection, including the assessment core at Western Psychiatric Hospital. Lastly, thank you to Roman Kotov and Miri Forbes for their inspiration and feedback that led to this final product. Note that the contents of this article do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
Footnotes
Illness and treatment values are based on retrospective reporting during clinical interviews and a consensus conference review of medical records. Prodromal estimates were missing for 17 of 370 participants. Nearly half of the sample (n = 175) did not have data on hospitalization for psychosis, due to never having been hospitalized or not recalling historical dates of treatment.
Contributor Information
Julia M Longenecker, VISN 4 Mental Illness Research Education and Clinical Center (MIRECC), VA Pittsburgh Healthcare System, Pittsburgh, PA, USA; Department of Psychiatry, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA.
Gretchen L Haas, VISN 4 Mental Illness Research Education and Clinical Center (MIRECC), VA Pittsburgh Healthcare System, Pittsburgh, PA, USA; Department of Psychiatry, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA.
Dean F Salisbury, Department of Psychiatry, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA.
Funding
This research was supported by funding from the National Institutes of Mental Health (R01 MH108568, R01 MH113533); Dr. Longenecker received infrastructure support from the VISN 4 Mental Illness Research, Education and Clinical Center (MIRECC; Director: D. Oslin; Associate Director: G. Haas), VA Pittsburgh Healthcare System.
Conflict of Interest
The authors have no conflicts to report.
References
- 1. Kotov R, Jonas KG, Carpenter WT, et al. . Validity and utility of Hierarchical Taxonomy of Psychopathology (HiTOP): I. Psychosis superspectrum. World Psychiatry 2020;19(2):151–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Grube BS, Bilder RM, Goldman RS. Meta-analysis of symptom factors in schizophrenia. Schizophr Res. 1998;31(2–3):113–120. [DOI] [PubMed] [Google Scholar]
- 3. Dollfus S, Everitt B. Symptom structure in schizophrenia: two-, three- or four-factor models? Psychopathology 1998;31(3):120–130. [DOI] [PubMed] [Google Scholar]
- 4. Minas IH, Stuart GW, Klimidis S, Jackson HJ, Singh BS, Copolov DL. Positive and negative symptoms in the psychoses: multidimensional scaling of SAPS and SANS items. Schizophr Res. 1992;8(2):143–156. [DOI] [PubMed] [Google Scholar]
- 5. Crow TJ. Positive and negative schizophrenic symptoms and the role of dopamine. Br J Psychiatry. 1980;137(4):383–386. [PubMed] [Google Scholar]
- 6. Andreasen NC, Arndt S, Miller DD, Flaum M, Napoulos P. Correlational studies of the scale for the assessment of negative symptoms and the scale for the assessment of positive symptoms: an overview and update. Psychopathology. 1995;28(1):7–17. [DOI] [PubMed] [Google Scholar]
- 7. Toomey R, Faraone S, Simpson J, Tsuang M. Negative, positive, and disorganized symptom dimensions in schizophrenia, major depression and bipolar disorder. J Nerv Ment Dis. 1998;186(8):470–476. [DOI] [PubMed] [Google Scholar]
- 8. Peralta V, Cuesta MJ. Dimensional structure of psychotic symptoms: an item-level analysis of SAPS and SANS symptoms in psychotic disorders. Schizophr Res. 1999;38(1):13–26. [DOI] [PubMed] [Google Scholar]
- 9. Kotov R, Krueger RF, Watson D, et al. . The Hierarchical Taxonomy of Psychopathology (HiTOP): a quantitative nosology based on consensus of evidence. Annu Rev Clin Psychol. 2021;17:83–108. [DOI] [PubMed] [Google Scholar]
- 10. Krueger RF, Kotov R, Watson D, et al. . Progress in achieving quantitative classification of psychopathology. World Psychiatry. 2018;17(3):282–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Regier DA, Narrow WE, Clarke DE, et al. . DSM-5 field trials in the United States and Canada, part ii: test-retest reliability of selected categorical diagnoses. Am J Psychiatry. 2013;170(1):59–70. [DOI] [PubMed] [Google Scholar]
- 12. Addington J, Chaves A, Addington D. Diagnostic stability over one year in first-episode psychosis. Schizophr Res. 2006;86(1–3):71–75. [DOI] [PubMed] [Google Scholar]
- 13. Kim JS, Baek JH, Choi JS, Lee D, Kwon JS, Hong KS. Diagnostic stability of first-episode psychosis and predictors of diagnostic shift from non-affective psychosis to bipolar disorder: a retrospective evaluation after recurrence. Psychiatry Res. 2011;188(1):29–33. [DOI] [PubMed] [Google Scholar]
- 14. Hopwood CJ, Morey LC, Donnellan MB, et al. . Ten-year rank-order stability of personality traits and disorders in a clinical sample. J Pers. 2013;81(3):335–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Van Os J, Gilvarry C, Bale R, et al. . A comparison of the utility of dimensional and categorical representations of psychosis. Psychol Med. 1999;29(3):595–606. [DOI] [PubMed] [Google Scholar]
- 16. Andreasen NC. Scale for the Assessment of Negative Symptoms (SANS). Iowa: University of Iowa; 1983. [Google Scholar]
- 17. Andreasen NC. Scale for the Assessment of Positive Symptoms (SAPS). Iowa: University of Iowa; 1984. [Google Scholar]
- 18. First M, Spitzer R, Gibbon M, Williams J.. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I). Washington, DC: American Psychiatric Press, Inc.; 1997. [Google Scholar]
- 19. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Text Revision (DSM-IV-TR). Washington, DC: American Psychiatric Association; 4th ed. 2000. [Google Scholar]
- 20. Goldberg LR. Doing it all Bass-Ackwards: the development of hierarchical factor structures from the top down. J Res Pers. 2006;40(4):347–358. [Google Scholar]
- 21. Revelle W. An Introduction to the Psych Package: part I: data Entry and Data Description; 2019. http://www.personality-project.org/r/psych/HowTo/intro.pdf. Accessed May 14, 2021.
- 22. Franklin SB, Gibson DJ, Robertson PA, Pohlmann JT, Fralish JS. Parallel Analysis: a method for determining significant principal components. J Veg Sci. 1995;6(1):99–106. [Google Scholar]
- 23. Holgado–Tello FP, Chacón–Moscoso S, Barbero–García I, Vila–Abad E. Polychoric versus Pearson correlations in exploratory and confirmatory factor analysis of ordinal variables. Qual Quant. 2010;44(1):153–166. [Google Scholar]
- 24. Tabachnick B, Fidell L, Ullman J. Using Multivariate Statistics; 2007. https://www.pearsonhighered.com/assets/preface/0/1/3/4/0134790545.pdf. Accessed November 9, 2021.
- 25. Kotov R, Foti D, Li K, Bromet EJ, Hajcak G, Ruggero CJ. Validating dimensions of psychosis symptomatology: neural correlates and 20-year outcomes. J Abnorm Psychol. 2016;125(8):1103–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Velligan D, Prihoda T, Dennehy E, et al. . Brief Psychiatric Rating Scale Expanded Version: how do new items affect factor structure? Psychiatry Res. 2005;135(3):217–228. [DOI] [PubMed] [Google Scholar]
- 27. Mueser KT, Curran PJ, McHugo GJ. Factor structure of the Brief Psychiatric Rating Scale in schizophrenia. Psychol Assess. 1997;9(3):196–204. [Google Scholar]
- 28. Shafer A, Dazzi F. Meta-analysis of the positive and Negative Syndrome Scale (PANSS) factor structure. J Psychiatr Res. 2019;115:113–120. [DOI] [PubMed] [Google Scholar]
- 29. Longenecker J, George TP, Voore P, et al. . Cross-cutting symptom domains predict functioning in the psychotic s pectrum. J Clin Psychiatry. 2021;82(2)e1:e7. doi: 10.4088/JCP.20m13288. [DOI] [PubMed] [Google Scholar]
- 30. Rabinowitz J, Levine SZ, Garibaldi G, Bugarski-Kirola D, Berardo CG, Kapur S. Negative symptoms have greater impact on functioning than positive symptoms in schizophrenia: analysis of CATIE data. Schizophr Res. 2012;137(1–3):147–150. [DOI] [PubMed] [Google Scholar]
- 31. Wright ZE, Pahlen S, Krueger RF. Genetic and environmental influences on Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (DSM-5) maladaptive personality traits and their connections with normative personality traits. J Abnorm Psychol. 2017;126(4):416–428. [DOI] [PubMed] [Google Scholar]
- 32. Zavos HMS, Freeman D, Haworth CMA, et al. . Consistent etiology of severe, frequent psychotic experiences and milder, less frequent manifestations: a twin study of specific psychotic experiences in adolescence. JAMA Psychiatry. 2014;71(9):1049–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lehembre-Shiah E, Leong W, Brucato G, et al. . Distinct relationships between visual and auditory perceptual abnormalities and conversion to psychosis in a clinical high-risk population. JAMA Psychiatry. 2017;74(1):104–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gore WL, Widiger TA. The DSM-5 dimensional trait model and five-factor models of general personality. J Abnorm Psychol. 2013;122(3):816–821. [DOI] [PubMed] [Google Scholar]
- 35. Kotov R, Krueger RF, Watson D, et al. . The Hierarchical Taxonomy of Psychopathology (HiTOP): a dimensional alternative to traditional nosologies. J Abnorm Psychol. 2017;126(4):454–477. [DOI] [PubMed] [Google Scholar]
- 36. Green MF, Kern RS, Heaton RK. Longitudinal studies of cognition and functional outcome in schizophrenia: implications for MATRICS. Schizophr Res. 2004;72(1):41–51. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.