Abstract
Complications related to open entry for laparoscopic procedures are relatively rare, and the incidence of closed entry-related complications is 0.4 per 1000 cases. We report a case of serosal injury to a distended stomach that was caused during open entry. A 37-year-old woman presented with a 1-year history of dysmenorrhea. Transvaginal ultrasonography revealed a uterine myoma and cesarean section (C/S) wound defect. Laparoscopic single-site myomectomy and repair of the C/S wound defect were planned. Open abdominal entry was achieved at the umbilicus, and the patient's stomach was distended and injured by the electric knife (30 watts). After identifying the injury, we inserted a nasogastric tube to deflate the stomach and repaired the gastric serosal injury. The laparoscopic myomectomy and C/S defect repair were subsequently performed without complications. The patient has remained free from complications during the 1-year follow-up. Gastric serosal injury during open entry is a rare complication. Insertion of a nasopharyngeal tube and routine percussion of the abdomen before entering the abdominal cavity are the most important steps to prevent this complication.
Keywords: Injury, open entry, serosa, single-site laparoscopy, stomach
INTRODUCTION
Laparoscopic-assisted surgery for benign gynecological diseases has become increasingly popular worldwide, as well as in Taiwan during the last two decades.[1] The first step in laparoscopic surgery involves creating pneumoperitoneum through an entry port. Although major complications are very rare after laparoscopic surgery, entry-related complications account for up to 50% of complications,[2] which include bowel injury and vascular injury. The major cause of death during or after laparoscopic surgery is an injury to major blood vessels, which typically occurs during trocar insertion and requires immediate repair to manage life-threatening hemorrhage. Bowel injury may not be immediately life threatening, although it can be difficult to identify and a delayed diagnosis can lead to postoperative death.[3]
We report a case of gastric serosal injury in which a woman's distended stomach was injured during open entry for laparoendoscopic single-site surgery.
CASE REPORT
A 37-year-old woman had previously delivered two children through cesarean section (C/S) and subsequently presented with a 1-year history of dysmenorrhea. Her menstrual cycles were regular and eumenorrhea was noted. A physical examination and blood tests revealed no specific findings. However, transvaginal ultrasonography revealed a uterine myoma [3.4 cm × 2.8 cm at the anterior wall, Figure 1a], a uterine wall C/S scar defect [Figure 1b], and normal bilateral adnexa. Therefore, laparoendoscopic single-site (LESS) myomectomy and C/S scar defect repair were planned.
Figure 1.
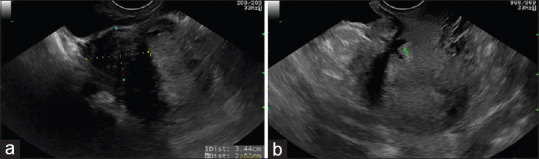
Ultrasonography revealed the uterine myoma and cesarean section scar defect. (a) The uterine myoma located at the anterior wall. (b) The cesarean section scar defect (arrow)
Open entry was achieved at the umbilicus using an electric knife (30 watts) for layer-by-layer incisions. However, during entry into the peritoneum, the surgeon suspected that a gastric serosal injury had been created. Therefore, after pneumoperitoneum was established, a laparoscopic examination was performed to identify any gastric injury, which revealed a distended stomach with a serosal injury [Figure 2]. A nasogastric tube was inserted to decompress the stomach, and the serosal injury was repaired using four stitches of 3-0 Vicryl suture. The LESS myomectomy and C/S defect repair were subsequently performed smoothly and without complication. The patient was discharged on the 4th postoperative day and has not experienced any complications during the 1-year follow-up.
Figure 2.
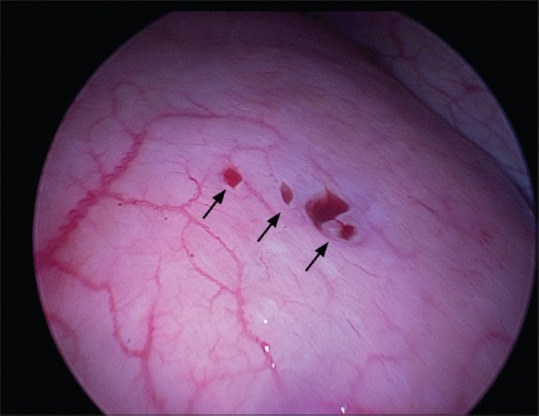
Laparoscopic view of the gastric serosal injury (arrows)
DISCUSSION
Laparoscopic-assisted surgery (e.g., myomectomy, ovarian cystectomy, and hysterectomy) is used to treat both benign conditions and malignant diseases.[4] Furthermore, minimally invasive surgery has many advantages, including shorter lengths of hospital stay, reduced pain, and better cosmesis.[5] Moreover, technical innovations have led to the development of single-port laparoscopic surgery techniques, which include embryonic natural orifice transumbilical endoscopic surgery, LESS, and single-incision laparoscopic surgery.[6,7]
The primary trocar entry for laparoscopic surgery is typically performed using the open (Hasson) technique or the classic closed technique (with a Veress needle).[8] During the classic closed technique, the Veress needle is blindly inserted through the subumbilical skin incision until a double click sound is heard, and then, insufflation is performed through the Veress needle after the saline drop test has been passed. During the open technique, a small umbilical laparotomy is performed by serially incising the skin, rectus sheath, and peritoneum under direct vision. Entry-related complications after laparoscopic procedures are rare. Risk factors for entry-related bowel injury include obesity or severe underweight status, previous abdominal and pelvic surgery, severe endometriosis, extensive bowel distention, and a very large abdominal or pelvic mass.[3]
Gastric injuries are a very rare type of gastrointestinal injury after trocar insertion. Gastric dilatation is a potential cause of entry-related gastric injury during laparoscopic surgery.[9] This type of dilatation may be related to difficult intubation, prolonged oxygenation maneuvers, peristaltic dysfunction in the colon, and the use of general anesthesia with a laryngeal mask airway.[9,10,11] Patients with an increased risk of gastric dilatation may exhibit upper abdominal distension or increased tympanism, and decompression in these cases may be achieved by inserting a nasogastric tube before pneumoperitoneum is established.[9] However, our patient did not have difficult intubation and it remains unclear why the exhibited gastric distension is unknown. Nevertheless, we identified the serosal injury during the procedure, inserted a nasogastric tube to achieve stomach decompression, repaired the injury, and completed the procedure without any long-term complications.
Gastrointestinal injury during trocar insertion can be difficult to identify, and a delayed diagnosis can increase the risk of comorbidity and mortality. Furthermore, the risk of gastrointestinal injury may increase if there is difficulty establishing pneumoperitoneum (e.g., because of multiple trocar insertions), and the surgeon must be aware of the possibility of bowel injury. The most common type of injury is superficial and involves a small hole (<2 cm) at one side of the intestine. Laparoscopic repair of the injury depends on the surgeon's experience and the size and nature of the wound. Primary closure can be achieved using Vicryl or silk sutures, depending on the degree of serosal injury,[3] and our patient was successfully treated by a general surgery specialist using four stitches of 3-0 Vicryl suture.
Parvaiz and Pervaiz have reviewed all case reports regarding gastric perforation during entry for laparoscopy between 1972 and 2008 and noted that all of these cases involved the classic closed technique, which prompted them to recommend the open entry technique.[11] In addition, a previous report has suggested that the open technique may be superior, as it provides a lower complication rate and greater safety because it is performed under direct vision.[12] Moreover, the open single-site entry has become a trend during recent years, and we are not aware of any reports regarding gastric injury caused by the electric knife during open entry. Nevertheless, the present case suggests that surgeons should consider the possibility of a distended stomach even when using the open entry technique, as there is a small risk of gastric injury.
CONCLUSION
It is important to identify any risk factors for gastrointestinal injury and take steps to minimize that risk when establishing pneumoperitoneum. For example, the possibility of injury should be considered and evaluated laparoscopically if it is difficult to establish the pneumoperitoneum, if repeated trocar insertions are necessary, or if there is a high risk of adhesions. Identification of the injury in this setting is important to prevent a delayed diagnosis, which can increase the risks of morbidity and mortality and can permit immediate primary repair by an experienced surgeon if an injury is identified.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This work was supported in part by grants from the Buddhist Tzu Chi Medical Foundation (TCMF-EP-108-02).
Conflicts of interest
Prof. Dah-Ching Ding, an editorial board member at Gynecology and Minimally Invasive Therapy, had no role in the peer review process of or decision to publish this article. The other authors declared no conflicts of interest in writing this paper.
REFERENCES
- 1.Wu MP, Lee CL. The trends of minimally invasive surgery for benign gynecologic lesions, 1997-2007 in Taiwan. Gynecol Minim Invasive Ther. 2012;1:3–8. [Google Scholar]
- 2.Ott J, Jaeger-Lansky A, Poschalko G, Promberger R, Rothschedl E, Wenzl R. Entry techniques in gynecologic laparoscopy – A review. Gynecol Surg. 2012;9:139–46. [Google Scholar]
- 3.Elbiss HM, Abu-Zidan FM. Bowel injury following gynecological laparoscopic surgery. Afr Health Sci. 2017;17:1237–45. doi: 10.4314/ahs.v17i4.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mandai M AOFOG MIGS Committee. AOFOG survey for the status of minimally invasive gynecologic surgery in the Asia/Oceania region. J Obstet Gynaecol Res. 2019;45:1091–5. doi: 10.1111/jog.13954. [DOI] [PubMed] [Google Scholar]
- 5.Koo YJ. Recent advances in minimally invasive surgery for gynecologic indications. Yeungnam Univ J Med. 2018;35:150–5. doi: 10.12701/yujm.2018.35.2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park HS, Kim TJ, Song T, Kim MK, Lee YY, Choi CH, et al. Single-port access (SPA) laparoscopic surgery in gynecology: A surgeon's experience with an initial 200 cases. Eur J Obstet Gynecol Reprod Biol. 2011;154:81–4. doi: 10.1016/j.ejogrb.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 7.Ding DC, Chu TY, Hong MK. Hysterectomy and ovarian cystectomy using natural orifice transluminal endoscopic surgery: An initial experience at Tzu Chi General Hospital. Tzu Chi Med J. 2017;29:208–12. doi: 10.4103/tcmj.tcmj_127_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Toro A, Mannino M, Cappello G, Di Stefano A, Di Carlo I. Comparison of two entry methods for laparoscopic port entry: Technical point of view. Diagn Ther Endosc. 2012;2012:305428. doi: 10.1155/2012/305428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abdullah Z, Nnochiri A. A rare case of gastric injury during routine laparoscopic surgery. Gynecol Surg. 2011;8:471–3. [Google Scholar]
- 10.El-Hossamy H, Morsi H. Recognition and prevention of gastric injury during gynecologic laparoscopy. J Gynecol Surg. 2014;30:181–3. doi: 10.1097/01.AOG.0000214680.33896.d0. [DOI] [PubMed] [Google Scholar]
- 11.Parvaiz MA, Pervaiz MA. Iatrogenic gastric perforation during laparoscopy presenting on anaesthesia monitor. Ann R Coll Surg Engl. 2014;96:e14–5. doi: 10.1308/003588414X13946184900129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taye MK, Fazal SA, Pegu D, Saikia D. Open versus closed laparoscopy: Yet an unresolved controversy. J Clin Diagn Res. 2016;10:C04–7. doi: 10.7860/JCDR/2016/18049.7252. [DOI] [PMC free article] [PubMed] [Google Scholar]


