Abstract
Background
The mental health of the Italian population declined at the onset of the COVID-19 pandemic. However, nationwide population prevalence estimates may not effectively reproduce the heterogeneity in distress responses to the pandemic. In particular, contextual determinants specific to COVID-19 pandemic need to be considered. We thus aimed to explore the association between local COVID-19 mortality rates and mental health response among the general population.
Methods
We capitalised on data (N = 17,628) from a large, cross-sectional, national survey, the COMET study, run between March and May 2020. While psychological distress was measured by General Health Questionnaire–12 (GHQ-12), the Depression, Anxiety and Stress Scale-21 Items (DASS-21) was used to assess relevant domains. In addition, a Covid-19 mortality ratio was built to compare single regional mortality rates to the national estimate and official statistics were used to control for other area-level determinants.
Results
Adjusted ordered regression analyses showed an association between mortality ratio and moderate (OR = 1.10, 95%CI 1.03–1.18) and severe (OR = 1.11, 95%CI 1.03–1.21) DASS-21 anxiety levels. No effects of mortality ratio on GHQ-12 scores and DASS-21 depression and stress levels, uniformly high across the country, were estimated.
Conclusions
Although we could not find any association between regional COVID-19 mortality ratio and depression or psychological distress, anxiety levels were significantly increased among subjects from areas with the highest mortality rates. Local mortality rate seems a meaningful driver for anxiety among the general population. Considering the potentially long-lasting scenario, local public health authorities should provide neighbouring communities with preventive interventions reducing psychological isolation and anxiety levels.
Keywords: Anxiety, Depression, Psychological distress, Mortality rate, COVID-19
1. Introduction
Since the beginning of the coronavirus outbreak a large number of surveys have been carried out to determine the impact of the pandemic and of related containment measures on the mental health of general population (Unützer et al., 2020; Ghebreyesus, 2020). Research has documented at an unprecedented pace increased levels of psychological distress (e.g., Li et al., 2020, McGinty et al., 2020), in particular anxiety and depression, though with considerable variations across countries (COVID-19 Mental Disorders Collaborators, 2021).
However, reported increased prevalence of common mental disorders during the early stages of the pandemic gradually ameliorated with the passage of weeks, contradicting media claiming a mental health ‘tsunami’ of mental ill-health (Shevlin et al., 2021; Pierce et al., 2020a). Indeed, recent longitudinal research has shown that mental health response to the pandemic seems heterogeneous and likely to be influenced by individual (Sampogna et al., 2021; Pompili et al., 2021; Wasserman et al., 2020; McIntyre and Lee, 2020; Wang et al., 2021; Rooksby et al., 2020) and area-level determinants linked also to the differential severity of containment measures and to the related process of living adjustment and adaptation (Shevlin et al., 2021; Pierce et al., 2020a; Ahrens et al., 2021). If before the COVID-19 pandemic literature had clearly shown that many characteristics (including socio-demographic factors such as age, gender, household type, employment, region of residence, and previous mental and physical health problems) significantly influence the likelihood of experiencing common mental disorders, it seems reasonable this remained true also during the pandemic (McManus et al., 2016). However, COVID-19 pandemic has probably introduced in mental health research a previously infrequently considered, area-level determinant, which is intrinsic to the classical paradigm of infectious diseases. At least in the early stages of the pandemic, different parts of the various countries became impacted at different times, since there were differences across geographic areas in the local prevalence rates and in the severity of the lockdowns; it thus seems plausible that also mental health responses to differential pandemic impacts followed similar paths.
Understanding local variations in mental health impact of the pandemic, is important because overall prevalence figures or other summary statistics are of little public health usefulness, as they cannot point to where mental health service and preventive assets should be allocated in this and future global emergencies.
The spread of SARS-CoV-2 in Italy showed a strikingly uneven geographic distribution during the first wave of the pandemic (March–April 2020), with the northern regions (Lombardy, Emilia Romagna, Piedmont, and Veneto) disproportionately affected by the pandemic, in terms of both severe cases and deceased persons, as compared with the central and southern regions (Pluchino et al., 2021). Although the Italian government placed 60 million people under a nationwide lockdown from March 8, to May 3, 2020, daily mortality figures were astonishingly high just in the northern regions, where nearly all families experienced severe cases and/or victims of SARS-COVID-19 within their circle of acquaintances (Sanfelici, 2020).
Research has shown that exposure to disasters is associated with an array of mental health consequences and the collective experience of the pandemic can be considered as a mass trauma (Miller and Rasmussen, 2010; Horesh and Brown, 2020; Fiorillo and Gorwood, 2020). For example, in war exposures, daily, enduring stressors play a key role leading to poor mental health outcomes (Goldmann and Galea, 2014). Similarly, information from relevant circle of acquaintances, social networks, as well as news from ongoing media coverage on daily deaths and hospitalizations, which in Italy hit highs across the peak on March 27 up to May 3, 2020, may well be considered daily stressors, possibly inducing specific emotional reactions among those living in the most affected geographic areas.
The COvid Mental hEalth Trial (COMET) study was specifically set up to evaluate the impact of COVID-19 pandemic and its containment measures on the mental health of the Italian population (Giallonardo et al., 2020). Data were collected nationwide over a period of three months by an online survey conducted between March and May 2020. It therefore provided a valuable opportunity to test the hypothesis that levels of anxiety, depression and psychological distress were mostly increased in areas where the highest COVID -19 mortality rates were daily experienced and reported to people living in relevant geographic communities during the lockdown.
2. Material and methods
2.1. Participants
The COMET study is a naturalistic, cross-sectional study, coordinated by the University of Campania “Luigi Vanvitelli” (Naples), purposively sampling the general population as well as different special groups. Procedures, sampling strategies and inclusion/exclusion criteria are fully described elsewhere (Fiorillo et al., 2020). The study was approved by the Ethical Review Board of the coordinating centre (protocol number: 0007593/i). In total, 20,720 participants completed the survey, although we here consider only subjects from the general population (N = 17,628), excluding any special populations (i.e., health care staff; users of mental health services and people who had already been diagnosed with a mental disorder; those living in institutional settings such as care homes, offender institutions, prisons, or in temporary housing or sleeping rough; and those who were staying in hospital for SARS-COVID-19 or other serious physical health conditions).
2.2. Measures
Socio-demographic characteristics (e.g., gender, age, regional geographic location of residence, working and housing conditions, including a measure for household financial situation) and clinical information were collected. In addition, an extensive battery of instruments was used to collect information from the survey. Only those relevant to this study are presented here.
The Depression, Anxiety and Stress Scale - 21 Items (DASS-21) (Lovibond and Lovibond, 1995) consists of 21 items, grouped in three subscales: depression, anxiety, and stress. Each item is rated on a 4-point Likert scale, from 0 (never) to 3 (almost always). The total score is calculated by adding together the response values of each item, with higher scores indicating more severe levels of depressive, anxiety, and stress symptoms. Scores ranges at the DASS-depression subscale are considered normal (0–9), rather than indicative of mild (10–12), moderate (13–20), severe (21–27), and extremely severe depression (28–42). Similarly, the anxiety subscale range scores map into normal (0–6), mild (7–9), moderate (10–14), severe (15–19), and extremely severe anxiety (20–42), whilst the stress subscale considers scores ranges as normal (0–10), either evidence of mild (11–18), moderate (19–26), severe (27–34), and extremely severe stress (35–42).
The General Health Questionnaire - 12 items (GHQ-12) version explores participants’ mental health status through six positively and six negatively worded items, respectively. Each item is rated on a four-point scale (less than usual, no more than usual, rather more than usual, or much more than usual). We used the standard bimodal GHQ scoring method (0-0-1-1), with a threshold≥4 recommended for caseness of mental health problems (Goldberg et al., 1997).
In addition, we included an area-level measure related to the consequences of the COVID-19 pandemic in terms of mortality in the single participant's region of residence, assuming this would represent a significant exposure for the neighbouring general population in terms of emotional distress (Delmastro and Zamariola, 2020). Taking into account available official statistics related to the number of COVID-19 confirmed deaths at regional level during the first pandemic wave in Italy (Dipartimento della Protezione Civile, 2020), we could derive regional mortality rates, defined as the number of deaths per 100,000 inhabitants in a single region. A COVID-19 mortality ratio (regional/national, mortality rates) was thus built and used to compare single regional mortality rates to the national estimate. Finally, we retrieved -as of January 2020- official regional, socio-demographic statistics from the Italian National Institute of Statistics population census (i.e., age, gender and employment rates), in order to control for area-level determinants which might influence -regardless of COVID-19 pandemic-mental health status variations across regions (Istituto nazionale di statistica (ISTAT), 2020a).
2.3. Statistics
Descriptive analyses were carried out to summarize main characteristics of survey participants. Standard statistics were provided for continuous and categorical variables based on the whole sample and by macro area-level stratifications, i.e., North-West (Aosta Valley, Liguria, Lombardy, Piedmont); North-East (Emilia-Romagna, Friuli Venezia Giulia, Trentino-South Tyrol, Veneto); Central (Lazio, Marche, Tuscany, Umbria); and Southern (Abruzzo, Apulia, Basilicata, Calabria, Campania, Molise, Sardinia, Sicily) Italy.
According to data distribution and relevant assumptions (e.g., normally distributed residuals), logistic regression and generalized ordered logit models were fitted exploring the association between area-level mortality ratios and the various measures of psychological distress explored, i.e., GHQ-12 caseness for a mental health problem and the three DASS-21 subscales scores ranges, respectively. In the generalized ordered logit models for DASS-21 subscales, three panels were used, summarizing comparisons between each level of distress and remaining, more severe, ones: Panel 1-Normal, Panel 2-Mild, and Panel 3-Moderate. Considering actual variables of interest in the ordered regression analyses, we handled multiple testing correction by using survey postestimation commands for panels’ joint-hypothesis evaluation and Bonferroni-adjusted p-values, where appropriate. A statistically significant positive coefficient would indicate an association between the local exposure to COVID-19 pandemic mortality ratio and levels of psychological distress, which would be higher than those expected from each single panel. Taking into account design-based differences across geographical areas, the final model was adjusted for several factors including age, gender, employment (either student) status, household financial situation, and regional-level employment rates, as well as previous contacts with mental health services (as proxy measure for pre-existing mental health conditions), along with estimates for depression prevalence rates per region from the 2017–2020 Italian Behavioural Risk Factor Surveillance System (PASSI), in order to take into account any COVID-19 independent regional differences in mental health (Gigantesco et al., 2022). Where appropriate, we checked for plausible relationships across independent variables, such as multicollinearity. All covariates had less than 1% missing data.
Analyses were carried out in Stata version 17. To take account of the survey design, the svy suite of commands was used, weighting for differential nonresponse to the COVID-19 web survey, according to key population variables (e.g., bias in terms of female over-representation). Finally, a post-stratification approach was followed, identifying different strata by using information from National Census (Istituto nazionale di statistica (ISTAT), 2020b) in terms of gender and age within regional populations.
3. Results
The sample included 17,628 participants aged 18 years and older (70.7% female) with a mean age (SD) of 40.2 (14.6) years. Considering the COVID-19 first wave in Italy (peaking during the first week of April 2020), COVID-19 regional mortality rates per 100,000 inhabitants, aggregated by geographic macro areas, were higher in Northern Regions as compared with Central and Southern Italy [mean (SE): North-West: 46.8 (0.47); North-East: 21.9 (0.21); Centre: 7.3 (0.12); South: 2.6 (0.02)].
Descriptive statistics for unweighted sample characteristics are summarized in Table 1 by geographic macro areas, reporting statistically significant differences (*p < 0.05; **p < 0.01; ***p < 0.001). Participants living in North-West and North-East regions were older and more likely to be employed and with higher educational attainments. On the other hand, people living in the South were more likely to report poor household financial situation.
Table 1.
Unweighted sample characteristics by geographic macro areas.
| Characteristics | North-West N = 2920 |
North-East N = 4266 |
Centre N = 5446 |
South N = 4986 |
Total N = 17,628 |
|---|---|---|---|---|---|
| Gender ** | |||||
| Female | 2092 (71.6%) | 2965 (69.5%) | 3788 (69.4%) | 3615 (72.5%) | 12,460 (70.7%) |
| Age, yrs. *** | |||||
| mean (SD) | 43.1 (14.5) | 40.0 (14.7) | 39.7 (14.9) | 39.2 (14.2) | 40.2 (14.6) |
| Median (IQR) | 43 (31–53) | 39 (26–52) | 38 (26–52) | 37 (27–49) | 39 (27–52) |
| Marital status *** | |||||
| In a relationship | 1670 (57.2%) | 2196 (51.5%) | 2664 (48.8%) | 2383 (47.8%) | 8813 (50.6%) |
| Education *** | |||||
| Degree | 1879 (64.4%) | 2402 (56.3%) | 3107 (56.9%) | 2813 (56.4%) | 10,201 (57.9%) |
| High school | 835 (28.6%) | 1544 (36.2%) | 1990 (36.5%) | 1879 (37.7%) | 6248 (35.4%) |
| Middle school | 206 (7.0%) | 320 (7.5%) | 359 (6.6%) | 294 (5.9%) | 1179 (6.7%) |
| Current Student *** | 440 (15.1%) | 1047 (24.5%) | 1641 (30.1%) | 1376 (27.6%) | 4504 (25.6%) |
| Employed *** | 2148 (73.6%) | 2955 (69.3%) | 3459 (63.4%) | 3014 (60.5%) | 11,576 (65.7%) |
| Poor Household Financial situation *** | 646 (22.1%) | 847 (19.9%) | 1325 (24.3%) | 1521 (30.5%) | 4339 (24.6%) |
| Comorbid major physical illnesses | 426 (14.6%) | 621 (14.6%) | 727 (13.3%) | 734 (14.7%) | 2508 (14.2%) |
| Isolated due to COVID-19 infection *** | 148 (5.1%) | 136 (3.2%) | 175 (3.2%) | 127 (2.6%) | 586 (3.3%) |
| Previous contacts with mental health services* | 284 (9.7%) | 344 (8.1%) | 525 (9.6%) | 464 (9.3%) | 1617 (9.2%) |
| GHQ-12 caseness ratio *** | 1124 (38.5%) | 1573 (36.9%) | 2155 (39.5%) | 2185 (43.8%) | 7037 (39.9%) |
| DASS-21 | |||||
| Depression *** | |||||
| Median (IQR) | 12 (6–18) | 12 (4–18) | 14 (8–18) | 14 (8–18) | 14 (8–18) |
| Normal | 1091 (37.4%) | 1687 (39.6%) | 1912 (35.0%) | 1534 (30.8%) | 6224 (35.3%) |
| Mild | 419 (14.4%) | 648 (15.2%) | 795 (14.6%) | 695 (13.9%) | 2557 (14.5%) |
| Moderate | 1064 (36.5%) | 1470 (34.5%) | 2030 (37.2%) | 2038 (40.9%) | 6602 (37.5%) |
| Severe-Extrem. severe | 344 (11.8%) | 458 (10.7%) | 718 (13.2%) | 719 (14.4%) | 2239 (12.7%) |
| Anxiety *** | |||||
| Median (IQR) | 4 (0–12) | 4 (0–12) | 4 (0–12) | 8 (4–14) | 6 (0–12) |
| Normal | 1601 (54.9%) | 2419 (56.7%) | 2910 (53.3%) | 2211 (44.3%) | 9141 (51.9%) |
| Mild | 393 (13.5%) | 571 (13.4%) | 719 (13.2%) | 695 (13.9%) | 2378 (13.5%) |
| Moderate | 486 (16.7%) | 672 (15.8%) | 914 (16.8%) | 921 (18.5%) | 2993 (17.0%) |
| Severe-Extrem. severe | 438 (15.0%) | 601 (14.1%) | 912 (16.7%) | 1158 (23.2%) | 3109 (17.6%) |
| Stress *** | |||||
| Median (IQR) | 16 (12–22) | 16 (12–22) | 18 (12–22) | 18 (14–22) | 18 (12–22) |
| Normal | 591 (20.2%) | 920 (21.6%) | 1067 (19.6%) | 759 (15.2%) | 3337 (18.9%) |
| Mild | 1121 (38.4%) | 1622 (38.0%) | 2099 (38.5%) | 2089 (41.9%) | 6931 (39.3%) |
| Moderate | 1079 (37.0%) | 1533 (36.0%) | 2077 (38.1%) | 1899 (38.1%) | 6588 (37.4%) |
| Severe-Extrem. severe | 127 (4.3%) | 188 (4.4%) | 212 (3.9%) | 239 (4.8%) | 766 (4.3%) |
IQR = interquartile range; statistically significant differences across regions: *p < 0.05 **p < 0.01 ***p < 0.001.
On average, participants scored high on GHQ-12 according to the standard threshold (total sample mean GHQ-12 score = 3.12, SD = 1.98), and roughly 40% of them reported scores indicative of likely mental ill health. There were no significant variations across geographic macro areas on GHQ-12 average scores in terms of median (IQR): North-West = 3 (3), North-East = 3 (2), Centre = 3 (2), and South = 3 (3). On the other hand, participants were likely to score at most mild on DASS-21 (Anxiety: 65.4%; Stress: 58.2%; Depression: 49.8% of the entire sample) with limited variations across geographic macro areas.
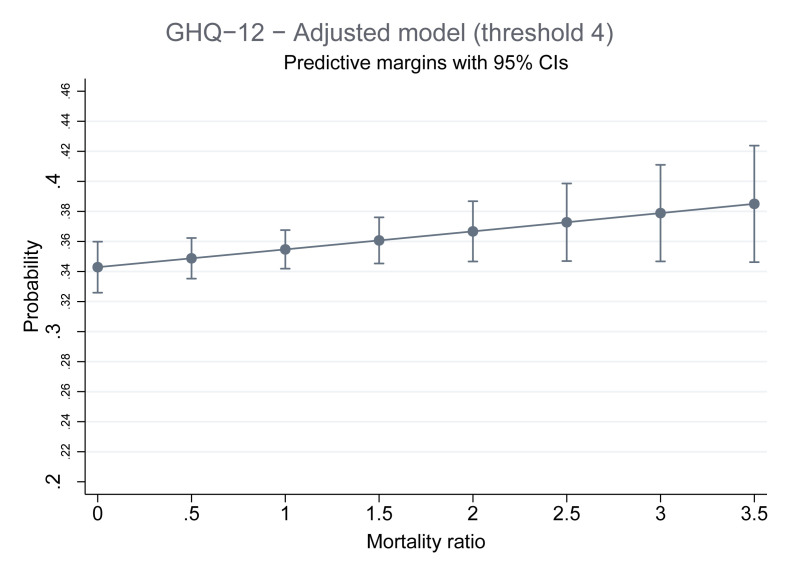
Table 2 presents the results of the logistic regression analyses for GHQ-12 caseness on weighted data. Although psychological distress, as assessed by GHQ-12, was more likely among women and younger people, as well as in those who reported a poor household financial situation, mortality ratio was not associated with GHQ-12 caseness (OR = 1.06, 95%CI 0.99–1.12, p = 0.082).
Table 2.
Adjusted regression analysis showing the association between psychological distress (GHQ-12 score ≥4) and COVID-19 mortality ratio.
| Characteristics | Coefficient (95% CI) | p-value |
|---|---|---|
| Mortality ratio | 0.054 (−0.007; 0.115) | 0.082 |
| Gender (women vs. men) | 0.265 (0.146; 0.384) | <0.001 |
| Age (years) | −0.013 (−0.017; −0.008) | <0.001 |
| Previous contact with mental health services | 0.380 (0.172; 0.587) | <0.001 |
| Employed | −0.114 (−0.251; 0.023) | 0.104 |
| Student | 0.037 (−0.141; 0.216) | 0.682 |
| Poor household financial situation | 0.612 (0.480; 0.744) | <0.001 |
| Regional-level employment rates | −0.010 (−0.020; 0.001) | 0.070 |
GHQ-12 = 12-item General Health Questionnaire (threshold: ≥4).
In addition, Fig. 1 shows profile plot of probability for GHQ-12 caseness, based on the logistic regression analysis and holding mortality ratio at fixed values. The model was adjusted for age, gender, current student/employment status (both at an individual- and at a regional-level), household financial situation, and previous contacts with mental health services. Increase in probability was not significant.
Fig. 1.
Prediction for psychological distress in terms of GHQ-12 scores by COVID-19 mortality ratio.
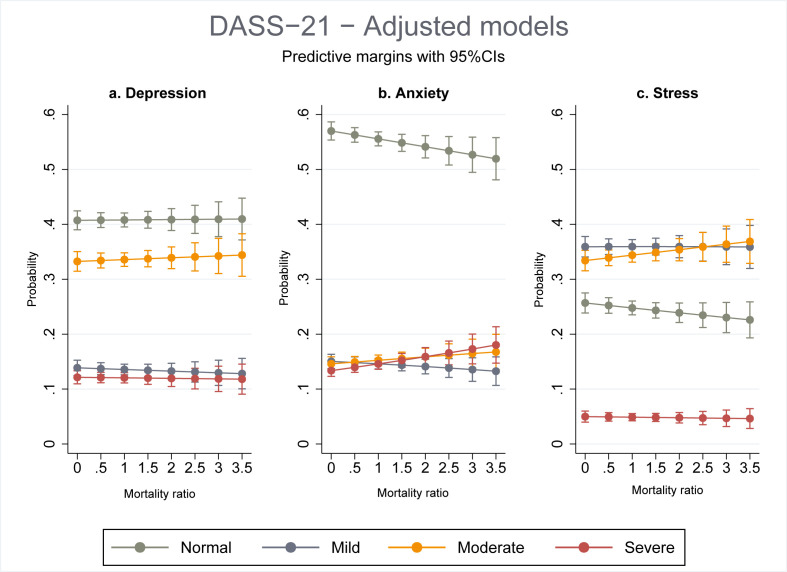
Female gender, younger age, previous contacts with mental health services, unemployment, and financial dissatisfaction were all predictors of DASS-21 depression scores, considering the probability of being categorized as having a mild or moderate depression. However, the relevant regression model did not uncover any relationship between the COVID-19 mortality ratio and DASS-21 depression scores (Table 3 - Model 1, Panel 1: OR = 0.99, 95%CI 0.94–1.05; Panel 2: OR = 1.01, 95%CI 0.94–1.07; Panel 3: OR = 0.99, 95%CI 0.91–1.09). Similarly, the plot based on this model did not show any changes in probabilities of suffering from normal, mild, moderate, and severe depression, holding estimated mortality ratio at fixed values. In addition, according to the adjusted model, and independently of mortality ratio variations, participants were more likely to score within the normal ranges on DASS-21 Depression subscale (Fig. 2 a).
Table 3.
Adjusted ordered regression analysis exploring the association between DASS-21 Depression, Anxiety, Stress scores and mortality ratio.
| Characteristics by DASS-21 contrast panels | Model 1-Depression |
Model 2-Anxiety |
Model 3-Stress |
|||
|---|---|---|---|---|---|---|
| Coefficient (95% CI) | p-value | Coefficient (95% CI) | p-value | Coefficient (95% CI) | p-value | |
| Panel 1: Normal(Normal vs Mild + Moderate + Severe) | ||||||
| Mortality ratio | −0.006 (−0.067; 0.053) | 0.831 | 0.062 (0.004; 0.121) | 0.036 #0.108 |
0.050 (−0.022; 0.123) | 0.175 |
| Gender (women vs men) | 0.597 (0.480; 0.713) | <0.001 | 0.697 (0.583; 0.811) | <0.001 | 0.599 (0.455; 0.743) | <0.001 |
| Age (years) | −0.012 (−0.016; −0.008) | <0.001 | −0.007 (−0.011; −0.003) | 0.001 | −0.016 (−0.021; −0.011) | <0.001 |
| Previous contact with mental health services | 0.823 (0.607; 1.040) | <0.001 | 0.872 (0.669; 1.076) | <0.001 | 0.482 (0.211; 0.752) | <0.001 |
| Employed | −0.442 (−0.582; −0.303) | <0.001 | −0.282 (−0.416; −0.147) | <0.001 | 0.005 (−0.160; 0.170) | 0.950 |
| Student | −0.033 (−0.223; 0.157) | 0.735 | −0.052 (−0.227; 0.122) | 0.556 | 0.081 (−0.172; 0.335) | 0.531 |
| Financial dissatisfaction | 0.799 (0.658; 0.940) | <0.001 | 0.432 (0.304; 0.560) | <0.001 | 0.427 (0.263; 0.591) | <0.001 |
| Regional-level employment rates | −0.002 (−0.013; 0.008) | 0.645 | −0.031 (−0.040; −0.021) | <0.001 | −0.023 (−0.036; −0.009) | 0.001 |
| Regional-level depression prevalence rates | 0.065 (0.023; 0.107) | 0.002 | – | – | ||
| Panel 2: Mild(Normal + Mild vs Moderate + Severe) | ||||||
| Mortality ratio | 0.006 (−0.057; 0.070) | 0.840 | 0.098 (0.034; 0.162) | 0.003 #0.008 |
0.037 (−0.024; 0.099) | 0.231 |
| Gender (women vs men) | 0.416 (0.298; 0.533) | <0.001 | 0.626 (0.500; 0.751) | <0.001 | 0.339 (0.222; 0.456) | <0.001 |
| Age (years) | −0.010 (−0.014; −0.005) | <0.001 | −0.012 (−0.017; −0.008) | <0.001 | −0.003 (−0.007; 0.001) | 0.203 |
| Previous contact with mental health services | 0.760 (0.532; 0.989) | <0.001 | 0.973 (0.763; 1.183) | <0.001 | −0.132 (0.334; 0.069) | 0.199 |
| Employed | −0.469 (−0.607; −0.332) | <0.001 | −0.244 (−0.395; −0.093) | 0.002 | 0.006 (−0.132; 0.145) | 0.927 |
| Student | −0.020 (−0.204; 0.163) | 0.830 | −0.051 (−0.241; 0.140) | 0.601 | −0.164 (−0.344; 0.015) | 0.072 |
| Financial dissatisfaction | 0.731 (0.584; 0.878) | <0.001 | 0.531 (0.398; 0.663) | <0.001 | 0.119 (−0.014; 0.253) | 0.080 |
| Regional-level employment rates | −0.007 (−0.018; 0.004) | 0.225 | −0.035 (−0.046; −0.025) | <0.001 | −0.011 (−0.022; −0.001) | 0.031 |
| Regional-level depression prevalence rates | 0.064 (0.023; 0.105) | 0.002 | – | – | ||
| Panel 3: Moderate(Normal + Mild + Moderate vs Severe) | ||||||
| Mortality ratio | −0.006 (−0.096; 0.084) | 0.891 | 0.107 (0.028; 0.187) | 0.008 #0.025 |
−0.022 (−0.177; 0.132) | 0.776 |
| Gender (women vs men) | 0.207 (0.030; 0.384) | 0.022 | 0.582 (0.417; 0.748) | <0.001 | 0.070 (−0.230; 0.370) | 0.646 |
| Age (years) | −0.002 (−0.008; 0.005) | 0.619 | −0.016 (−0.022; −0.010) | <0.001 | 0.009 (−0.002; 0.019) | 0.101 |
| Previous contact with mental health services | 0.262 (−0.0005; 0.524) | 0.050 | 0.788 (0.567; 1.009) | <0.001 | −0.321 (−0.819; 0.177) | 0.207 |
| Employed | 0.016 (−0.191; 0.222) | 0.881 | −0.185 (−0.371; 0.001) | 0.051 | −0.269 (−0.629; 0.091) | 0.143 |
| Student | 0.061 (−0.201; 0.324) | 0.648 | −0.201 (−0.413; 0.010) | 0.062 | −0.360 (−0.985; 0.266) | 0.260 |
| Financial dissatisfaction | 0.592 (0.417; 0.767) | <0.001 | 0.556 (0.390; 0.723) | <0.001 | −0.046 (−0.352; 0.259) | 0.767 |
| Regional-level employment rates | −0.015 (−0.030; −0.0006) | 0.041 | −0.047 (−0.059; −0.035) | <0.001 | −0.011 (−0.037; 0.015) | 0.406 |
| Regional-level depression prevalence rates | −0.036 (−0.101; 0.030) | 0.287 | – | – | ||
DASS-21 = Depression, Anxiety and Stress Scale - 21 Items.
Analyses are weighted, adjusting for non-response. #Bonferroni-adjusted p-values considering the panels in the ordered regression analysis. A statistically significant positive coefficient would indicate an association between the exposure and levels of psychological distress on DASS-21 Depression, Anxiety and Stress, which would be higher than those expected from each single panel.
Fig. 2.
Predictions for psychological distress in terms of DASS-21 Depression, Anxiety and Stress, by mortality ratio (adjusted ordered regression analysis).
Nonetheless, COVID-19 mortality ratio appeared to predict statistically significant, though small, differences in DASS-21 Anxiety scores (Table 3- Model 2). Exposure to higher mortality ratio made it more likely that a participant scored for anxiety at least on moderate (Panel 2: OR = 1.10, 95%CI 1.03–1.18), and severe (Panel 3: OR = 1.11, 95%CI 1.03–1.21) levels, as compared with less severe ones. Thus, participants living in regions exposed to a higher mortality ratio might be more likely to report more severe anxiety levels, as assessed by the DASS-21, as shown also in the related plot (Fig. 2b). Finally, as regards the DASS-21 Stress domain, according to contrast panels from the relevant model (Table 3-Model 3), we could not find any association between exposure to higher mortality ratio and stress levels (Panel 1: OR = 1.05, 95%CI 0.98–1.13; Panel 2: OR = 1.04, 95%CI 0.98–1.10; Panel 3: OR = 0.98, 95%CI 0.84–1.14). However, participants from regions with the highest mortality ratios were more likely to be classified with moderate rather than mild stress (Fig. 2c).
4. Discussion
This study explored the effects of local COVID-19 mortality on the mental health of the relevant geographic communities. Validated and reliable assessment instruments have been used in order to investigate several domains of mental health and psychological wellbeing, in a large, nationwide, sample from the general population. We could not find any association between COVID-19 mortality ratio and psychological distress as measured by GHQ-12. However, when considering symptoms in specific domains, DASS-21 anxiety levels were consistently higher in subjects living in areas with the highest mortality rates. Nonetheless, this was not true for DASS-21 stress and depression levels.
An increasing number of reports have shown high rates of symptoms of anxiety, depression, posttraumatic stress disorder, psychological distress, and stress during the first wave of the pandemic (Nochaiwong et al., 2021). In addition, research has focussed on individual-level, sociodemographic and pre-existing clinical correlates associated with increased mental health burden (Wang et al., 2020; Ruggeri et al., 2008; Carrà et al., 2014). We found comparable psychological distress rates and similar individual-level correlates (e.g., female gender, younger age, previous contacts with mental health services, unemployment, and financial dissatisfaction), as reported by several analogous surveys (Hyland et al., 2020; Puangsri et al., 2021; Tracy et al., 2020; Crocamo et al., 2021a). This general examination masks the very dissimilar experiences lived by people during the early stages of the pandemic, since they were differentially exposed to specific, local features. In fact, we could uncover an association with a contextual correlate – COVID-19 regional mortality ratio – which is meaningful in terms of impact of the pandemic on the mental health of local general population. Indeed, also early cross-sectional and longitudinal evidence has recently shown that some area-level correlates (e.g., deprivation) are likely risk factors for dwindling mental health during the pandemic (Hubbard et al., 2021; Sotomayor-Beltran et al., 2021; Pierce et al., 2021). Thus, also our findings support the hypothesis that the population response to the pandemic was not homogeneous (Shevlin et al., 2021), showing in particular that local mortality ratio was a meaningful driver for increased anxiety levels among the general population. However, this was not true for other, still related, mental health domains like DASS-21 depression and stress levels, as well as general psychological distress as measured by GHQ-12. There may be several alternative explanations for these apparent discrepancies. First, whilst anxiety is likely to quickly increase after exposure to tragic mass events like COVID-19 pandemic and related deaths, depressive reactions may require more time to develop, in order to fully show their interference with one's abilities and functioning (Hidaka, 2012; Maj et al., 2020; Reynolds, 2020). In addition, it could be argued that stress levels, as measured by DASS-21 in our study, were homogeneously high across the country, since these are likely to be associated with ubiquitously implemented, lock-down and containment measures (Mohler-Kuo et al., 2021). This was possibly true also for the GHQ-12 caseness construct, which probably needs sufficient time to be apparent, while this was hostage to the intervals between measurements of our design (Griffith and Jones, 2019).
The anxiety domain, conversely, with its moving boundaries and interfaces with threat appraisal and fear learning (Britton et al., 2011), was most likely particularly sensitive to the exposure to the relevant infodemic, involving newspapers, social media, and other digital platforms (World Health Organization (WHO), 2020), reporting rising daily victims. During the main lockdown from March 8, to May 3, 2020, a news cycle informed nationwide the general population about the exponential growth of daily mortality figures in the northern regions, where a significant proportion of the population personally lived the experience of severe cases and victims within their families and circle of acquaintances. In addition, at this stage mental health habituation was not in place yet, and the prevalent trajectory kept deteriorating until the revocation of national lockdown measures as recently shown in other European countries (Pierce et al., 2021). Thus, understandably, also anxiety levels hit highs, particularly in the geographic areas most affected in terms of COVID-19 mortality ratio.
Our findings are thus in a position to account for heterogeneity in mental health response to the outbreak. We could show that area-level determinants like local mortality ratio are likely to play a key role to identify populations most in need of support for their increased levels of anxiety. There are significant suggestions for mental health policy makers and service planners. Taking into consideration the potentially long-lasting scenario, there is the need to surveil local exposures and sustain neighbouring communities to reduce psychological isolation and anxiety levels, promoting new mental health policies which may moderate the detrimental impact of the pandemic (Stewart and Appelbaum, 2020; Kuzman et al., 2020; McDaid, 2021). Under these circumstances timely preventive interventions on social, as well as on mainstream media, can be provided by local public health authorities (Crocamo et al., 2021b). Frequent, purposeful, comprehensible, and culturally appropriate contents, confronting anxiety increase as well as confusion and fear, may play an important role in deterring the emotional impact of local catastrophic features on individuals under lockdown and other containment measures like social distancing. These contents can help people coping with their anxiety levels, using focused communication strategies, despite tragic, ongoing, news they are exposed to (CSTS-Center for the Study of Traumatic Stress, 2020; Viviani et al., 2021).
In order to maintain public mental health advice grounded on evidence, we need continued investigation on circumstances like local lockdowns imposed in areas where there will be localised infectious disease, and on the related responses of the local populations in terms of anxiety and general psychological distress. In addition, likely changes in several individual- and area-level determinants (e.g. local infection rates, unemployment, religiosity, poverty, deprivation, etc.) have to be taken into account (Kimhi et al., 2021).
4.1. Limitations
Our findings should be interpreted within the context of several limitations. First, given the cross-sectional design of our study, causal relationships involving different characteristics, cannot be drawn. In addition, self-reports on which this study relies are influenced by various biases, including memory errors and under-reporting due to social desirability biases. Moreover, our online convenience sampling may have attracted volunteers who were already well engaged, interested in the topic, and who can access the internet; on the other hand, though we controlled for potential existing links between people and mental health services, we may not have been able to sufficiently account for some pre-existing conditions in psychological distress that were already occurring over time (Pierce et al., 2020a). Furthermore, we are aware that we did not use random sampling to reduce risk of bias, allowing quantification of non-response, since this was simply not feasible during the first wave, strict lock-down, when many official surveys were affected by physical distancing guidelines (Pierce et al., 2020b). Also, we used non-standardized (i.e., by age and gender) mortality rates, since relevant data were not available, and we were not able to carry out multilevel models since random effects are not allowed with a survey design with poststratification. Finally, based on the small number of people who reported COVID-19 infection, it is likely that sampled participants did not fully disclose COVID-19 exposure, making impossible to take into account the potential role of this exposure.
5. Conclusions
Our study shows essential variations in terms of public mental health across local communities as a consequence of the uneven severity of COVID- 19 pandemic regional impact. Clarifying these questions is crucial to planning focussed preventive interventions and to appropriately staffing local mental health services.
Compliance with ethical standards
The study has been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All persons gave their informed consent prior to their inclusion in the study. Details that might disclose the identity of the subjects under study were omitted.
Role of funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interests
None.
Author contributions
Conceptualization, G.C. and C.C; methodology, G.C. and C.C.; formal analysis, C.C.; data curation, G.S., M.L., U.A., C.Ca., F.C., B.D., G.M., M.G.N., M.P., G.San., U.V., A.F.; validation, G.C., C.C.; writing-original draft G.C., C.C., I.R., F.B; writing-review and editing, G.S., M.L., U.A., C.Ca., F.C., B.D., G.M., M.G.N., M.P., G.San., U.V., A.F; visualization, G.C.; supervision, G.C.; project administration, G.C. All authors have read and agreed to the published version of the manuscript.
References
- Ahrens K.F., Neumann R.J., Kollmann B., Plichta M.M., Lieb K., Tüscher O., Reif A. Differential impact of COVID-related lockdown on mental health in Germany. World Psychiatr. 2021;20:140–141. doi: 10.1002/wps.20830. https://doi:10.1002/wps.20830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britton J.C., Lissek S., Grillon C., Norcross M.A., Pine D.S. Development of anxiety: the role of threat appraisal and fear learning. Depress. Anxiety. 2011;28:5–17. doi: 10.1002/da.20733. https://doi:10.1002/da.20733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrà G., Bartoli F., Carretta D., Crocamo C., Bozzetti A., Clerici M., Bebbington P.E. The prevalence of metabolic syndrome in people with severe mental illness: a mediation analysis. Soc. Psychiatr. Psychiatr. Epidemiol. 2014;49:1739–1746. doi: 10.1007/s00127-014-0835-y. [DOI] [PubMed] [Google Scholar]
- COVID-19 Mental Disorders Collaborators Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;(21) doi: 10.1016/S0140-6736(21)02143-7. https://doi:10.1016/S0140-6736(21)02143-7 S0140-6736. 02143-02147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CSTS-Center for the Study of Traumatic Stress . Uniformed Services University; Bethesda: 2020. Mental health and behavioral guidelines for response to a pandemic flu outbreak: background on the mental health impact of natural disasters, including epidemics.https://www.cstsonline.org/resources/resource-master-list/mental-health-and-behavioral-guidelines-for-response-to-a-pandemic-flu-outbreak [Google Scholar]
- Crocamo C., Bachi B., Calabrese A., Callovini T., Cavaleri D., Cioni R.M., Moretti F., Bartoli F., Carrà G. Some of us are most at risk: systematic Review and Meta-Analysis of correlates of depressive symptoms among healthcare workers during the SARS-CoV-2 outbreak. Neurosci. Biobehav. Rev. 2021;131:912–922. doi: 10.1016/j.neubiorev.2021.10.010. https://doi:10.1016/j.neubiorev.2021.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crocamo C., Viviani M., Famiglini L., Bartoli F., Pasi G., Carrà G. Surveilling COVID-19 emotional contagion on Twitter by sentiment analysis. Eur. Psychiatr. 2021;64(1):e17. doi: 10.1192/j.eurpsy.2021.3. https://doi:10.1192/j.eurpsy.2021.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delmastro M., Zamariola G. Depressive symptoms in response to COVID-19 and lockdown: a cross-sectional study on the Italian population. Sci. Rep. 2020;10 doi: 10.1038/s41598-020-79850-6. https://doi:10.1038/s41598-020-79850-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dipartimento della Protezione Civile Dati COVID-19. 2020. https://opendatadpc.maps.arcgis.com/apps/dashboards/b0c68bce2cce478eaac82fe38d4138b1
- Fiorillo A., Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatr. 2020;63(1):e32. doi: 10.1192/j.eurpsy.2020.35. https://doi:10.1192/j.eurpsy.2020.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorillo A., Sampogna G., Giallonardo V., Del Vecchio V., Luciano M., Albert U., Carmassi C., Carrà G., Cirulli F., Dell'Osso B., Nanni M.G., Pompili M., Sani G., Tortorella A., Volpe U. Effects of the lockdown on the mental health of the general population during the COVID-19 pandemic in Italy: results from the COMET collaborative network. Eur. Psychiatr. 2020;28(1):e87. doi: 10.1192/j.eurpsy.2020.89. https://doi:10.1192/j.eurpsy.2020.89 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghebreyesus T.A. Addressing mental health needs: an integral part of COVID-19 response. World Psychiatr. 2020;19:129–130. doi: 10.1002/wps.20768. https://doi:10.1002/wps.20768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giallonardo V., Sampogna G., Del Vecchio V., Luciano M., Albert U., Carmassi C., Carrà G., Cirulli F., Dell'Osso B., Nanni M.G., Pompili M., Sani G., Tortorella A., Volpe U., Fiorillo A. The impact of quarantine and physical distancing following COVID-19 on mental health: study protocol of a multicentric Italian population trial. Front. Psychiatr. 2020;11:533. doi: 10.3389/fpsyt.2020.00533. https://doi:10.3389/fpsyt.2020.00533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gigantesco A., Minardi V., Contoli B., Masocco M. Depressive symptoms among adults in 2018-2019 and during the 2020 COVID-19 pandemic in Italy. J. Affect. Disord. 2022;15:1–8. doi: 10.1016/j.jad.2022.04.131. https://doi:10.1016/j.jad.2022.04.131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg D.P., Gater R., Sartorius N., Ustun T.B., Piccinelli M., Gureje O., Rutter C. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol. Med. 1997;27 doi: 10.1017/s0033291796004242. https://doi:10.1017/s0033291796004242 191-7. [DOI] [PubMed] [Google Scholar]
- Goldmann E., Galea S. Mental health consequences of disasters. Annu. Rev. Publ. Health. 2014;35:169–183. doi: 10.1146/annurev-publhealth-032013-182435. https://doi:10.1146/annurev-publhealth-032013-182435 [DOI] [PubMed] [Google Scholar]
- Griffith G.J., Jones K. Understanding the population structure of the GHQ-12: methodological considerations in dimensionally complex measurement outcomes. Soc. Sci. Med. 2019;243 doi: 10.1016/j.socscimed.2019.112638. https://doi:10.1016/j.socscimed.2019.112638 [DOI] [PubMed] [Google Scholar]
- Hidaka B.H. Depression as a disease of modernity: explanations for increasing prevalence. J. Affect. Disord. 2012;140:205–214. doi: 10.1016/j.jad.2011.12.036. https://doi:10.1016/j.jad.2011.12.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horesh D., Brown A.D. Traumatic stress in the age of COVID-19: a call to close critical gaps and adapt to new realities. Psychol Trauma. 2020;12:331–335. doi: 10.1037/tra0000592. https://doi:10.1037/tra0000592 [DOI] [PubMed] [Google Scholar]
- Hubbard G., Daas C.D., Johnston M., Murchie P., Thompson C.W., Dixon D. Are rurality, area deprivation, access to outside space, and green space associated with mental health during the COVID-19 pandemic? A cross sectional study (CHARIS-E) Int. J. Environ. Res. Publ. Health. 2021;18:3869. doi: 10.3390/ijerph18083869. https://doi:10.3390/ijerph18083869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland P., Shevlin M., McBride O., Murphy J., Karatzias T., Bentall R.P., Martinez A., Vallières F. Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. Acta Psychiatr. Scand. 2020;142:249–256. doi: 10.1111/acps.13219. https://doi:10.1111/acps.13219 [DOI] [PubMed] [Google Scholar]
- Istituto nazionale di statistica (ISTAT) Geodemo. 2020. https://demo.istat.it/index.php
- Istituto nazionale di statistica (ISTAT) 2020. National Census.https://demo.istat.it/popres/index.php?anno=2020&lingua=ita [Google Scholar]
- Kimhi S., Eshel Y., Marciano H., Adini B., Bonanno G.A. Trajectories of depression and anxiety during COVID-19 associations with religion, income, and economic difficulties. J. Psychiatr. Res. 2021;144:389–396. doi: 10.1016/j.jpsychires.2021.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuzman M.R., Curkovic M., Wasserman D. Principles of mental health care during the COVID-19 pandemic. Eur. Psychiatr. 2020;63(1):e45. doi: 10.1192/j.eurpsy.2020.54. https://doi:10.1192/j.eurpsy.2020.54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Yang Z., Qiu H., Wang Y., Jian L., Ji J., Li K. Anxiety and depression among general population in China at the peak of the COVID-19 epidemic. World Psychiatr. 2020;19:249–250. doi: 10.1002/wps.20758. https://doi:10.1002/wps.20758.PMID:32394560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond S.H., Lovibond P.F. second ed. Psychology Foundation; Sydney: 1995. Manual for the Depression Anxiety & Stress Scales. [Google Scholar]
- Maj M., Stein D.J., Parker G., Zimmerman M., Fava G.A., De Hert M., Demyttenaere K., McIntyre R.S., Widiger T., Wittchen H.U. The clinical characterization of the adult patient with depression aimed at personalization of management. World Psychiatr. 2020;19:269–293. doi: 10.1002/wps.20771. https://doi:10.1002/wps.20771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty E.E., Presskreischer R., Anderson K.E., Han H., Barry C.L. Psychological distress and COVID-19-related stressors reported in a longitudinal cohort of US adults in April and july 2020. JAMA. 2020;324:2555–2557. doi: 10.1001/jama.2020.21231. https://doi:10.1001/jama.2020.21231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDaid D. Viewpoint: investing in strategies to support mental health recovery from the COVID-19 pandemic. Eur. Psychiatr. 2021;26(1):e32. doi: 10.1192/j.eurpsy.2021.28. https://doi:10.1192/j.eurpsy.2021.28 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre R.S., Lee Y. Preventing suicide in the context of the COVID-19 pandemic. World Psychiatr. 2020;19:250–251. doi: 10.1002/wps.20767. https://doi:10.1002/wps.20767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McManus S., Bebbington P., Jenkins R., Brugha T. NHS digital; Leeds: 2016. Mental Health and Wellbeing in England: the Adult Psychiatric Morbidity Survey 2014. [Google Scholar]
- Miller K.E., Rasmussen A. War exposure, daily stressors, and mental health in conflict and post-conflict settings: bridging the divide between trauma-focused and psychosocial frameworks. Soc. Sci. Med. 2010;70:7–16. doi: 10.1016/j.socscimed.2009.09.029. https://doi:10.1016/j.socscimed.2009.09.029 [DOI] [PubMed] [Google Scholar]
- Mohler-Kuo M., Dzemaili S., Foster S., Werlen L., Walitza S. Stress and mental health among children/adolescents, their parents, and young adults during the first COVID-19 lockdown in Switzerland. Int. J. Environ. Res. Publ. Health. 2021;18:4668. doi: 10.3390/ijerph18094668. https://doi:10.3390/ijerph18094668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nochaiwong S., Ruengorn C., Thavorn K., Hutton B., Awiphan R., Phosuya C., Ruanta Y., Wongpakaran N., Wongpakaran T. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis. Sci. Rep. 2021;11 doi: 10.1038/s41598-021-89700-8. https://doi:10.1038/s41598-021-89700-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., Kontopantelis E., Webb R., Wessely S., McManus S., Abel K.M. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatr. 2020;7:883–892. doi: 10.1016/S2215-0366(20)30308-4. https://doi:10.1016/S2215-0366(20)30308-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., McManus S., Jessop C., John A., Hotopf M., Ford T., Hatch S., Wessely S., Abel K.M. Says who? The significance of sampling in mental health surveys during COVID-19. The lancet. Psychiatry. 2020;7:567–568. doi: 10.1016/S2215-0366(20)30237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., McManus S., Hope H., Hotopf M., Ford T., Hatch S.L., John A., Kontopantelis E., Webb R.T., Wessely S., Abel K.M. Mental health responses to the COVID-19 pandemic: a latent class trajectory analysis using longitudinal UK data. Lancet Psychiatr. 2021;8:610–619. doi: 10.1016/S2215-0366(21)00151-6. https://doi:10.1016/S2215-0366(21)00151-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pluchino A., Biondo A.E., Giuffrida N., Inturri G., Latora V., Le Moli R., Rapisarda A., Russo G., Zappalà C. A novel methodology for epidemic risk assessment of COVID-19 outbreak. Sci. Rep. 2021;11:5304. doi: 10.1038/s41598-021-82310-4. https://doi:10.1038/s41598-021-82310-4 Erratum in: Sci Rep. 2021 Jul 28. 11, 15719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pompili M., Innamorati M., Sampogna G., Albert U., Carmassi C., Carrà G., Cirulli F., Erbuto D., Luciano M., Nanni M.G., Sani G., Tortorella A., Viganò C., Volpe U., Fiorillo A. The impact of Covid-19 on unemployment across Italy: consequences for those affected by psychiatric conditions. J. Affect. Disord. 2021;296:59–66. doi: 10.1016/j.jad.2021.09.035. https://doi:10.1016/j.jad.2021.09.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puangsri P., Jinanarong V., Wattanapisit A. Impacts on and care of psychiatric patients during the outbreak of COVID-19. Clin. Pract. Epidemiol. Ment. Health. 2021;17:52–60. doi: 10.2174/1745017902117010052. https://doi:10.2174/1745017902117010052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds C.F. Optimizing personalized management of depression: the importance of real-world contexts and the need for a new convergence paradigm in mental health. World Psychiatr. 2020;19:266–268. doi: 10.1002/wps.20770. https://doi:10.1002/wps.20770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rooksby M., Furuhashi T., McLeod H.J. Hikikomori: a hidden mental health need following the COVID-19 pandemic. World Psychiatr. 2020;19:399–400. doi: 10.1002/wps.20804. https://doi:10.1002/wps.20804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggeri M., Lora A., Semisa D., SIEP-DIRECT'S Group The SIEP-DIRECT'S Project on the discrepancy between routine practice and evidence. An outline of main findings and practical implications for the future of community based mental health services. Epidemiol. Psichiatr. Soc. 2008;17:358–368. [PubMed] [Google Scholar]
- Sampogna G., Del Vecchio V., Giallonardo V., Luciano M., Albert U., Carmassi C., Carrà G., Cirulli F., Dell'Osso B., Menculini G., Nanni M., Pompili M., Sani G., Volpe U., Bianchini V., Fiorillo A. What is the role of resilience and coping strategies on the mental health of the general population during the COVID-19 pandemic? Results from the Italian multicentric COMET study. Brain Sci. 2021;11:1231. doi: 10.3390/brainsci11091231. https://doi:10.3390/brainsci11091231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanfelici M. The Italian response to the COVID-19 crisis: lessons learned and future direction in social development. Int. J. Commun. Soc. Dev. 2020;2:191–210. https://doi:10.1177/2516602620936037 [Google Scholar]
- Shevlin M., Butter S., McBride O., Murphy J., Gibson-Miller J., Hartman T.K., Levita L., Mason L., Martinez A.P., McKay R., Stocks T.V.A., Bennett K., Hyland P., Bentall R.P. Refuting the myth of a 'tsunami' of mental ill-health in populations affected by COVID-19: evidence that response to the pandemic is heterogeneous, not homogeneous. Psychol. Med. 2021;20:1–9. doi: 10.1017/S0033291721001665. https://doi:10.1017/S0033291721001665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sotomayor-Beltran C., Matta-Solis H., Perez-Siguas R., Matta-Solis E., Matta-Zamudio L. Fear of COVID-19 among Peruvian people living in disadvantaged communities: a cross-sectional study. Clin. Pract. Epidemiol. Ment. Health. 2021;17:19–25. doi: 10.2174/1745017902117010019. https://doi:10.2174/1745017902117010019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart D.E., Appelbaum P.S. COVID-19 and psychiatrists' responsibilities: a WPA position paper. World Psychiatr. 2020;19:406–407. doi: 10.1002/wps.20803. https://doi:10.1002/wps.20803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tracy D.K., Tarn M., Eldridge R., Cooke J., Calder J.D.F., Greenberg N. What should be done to support the mental health of healthcare staff treating COVID-19 patients? Br. J. Psychiatry. 2020;217:537–539. doi: 10.1192/bjp.2020.109. https://doi:10.1192/bjp.2020.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unützer J., Kimmel R.J., Snowden M. Psychiatry in the age of COVID-19. World Psychiatr. 2020;19:130–131. doi: 10.1002/wps.20766. https://doi:10.1002/wps.20766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viviani M., Crocamo C., Mazzola M., Bartoli F., Carrà G., Pasi G. Assessing vulnerability to psychological distress during the COVID-19 pandemic through the analysis of microblogging content. Future Generat. Comput. Syst. 2021;125:446–459. doi: 10.1016/j.future.2021.06.044. https://doi:10.1016/j.future.2021.06.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q., Xu R., Volkow N.D. Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatr. 2021;20:124–130. doi: 10.1002/wps.20806. https://doi:10.1002/wps.20806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Kala M.P., Jafar T.H. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: a systematic review and meta-analysis. PLoS One. 2020;28(12) doi: 10.1371/journal.pone.0244630. https://doi:10.1371/journal.pone.0244630 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman D., Iosue M., Wuestefeld A., Carli V. Adaptation of evidence-based suicide prevention strategies during and after the COVID-19 pandemic. World Psychiatr. 2020;19:294–306. doi: 10.1002/wps.20801. https://doi:10.1002/wps.20801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2020. Situation Report 13, Novel Coronavirus (2019-nCov)https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200202-sitrep-13-ncov-v3.pdf?sfvrsn=195f4010_6 [Google Scholar]