Abstract
Objective
The purpose of this thematic review is to examine the literature on the publics’ preferences of scarce medical resource allocation during COVID-19.
Study design
Literature review.
Methods
A review of Ovid MEDLINE, Embase, CINAHL and Scopus was performed between December 2019 and June 2022 for eligible articles.
Results
Fifteen studies using three methodologies and spanning five continents were included. Five key themes were identified: (1) prioritise the youngest; (2) save the most lives; (3) egalitarian allocation approaches; (4) prioritise healthcare workers; and (5) bias against particular groups. The public gave high priority to allocation that saved the most lives, particularly to patients who are younger and healthcare workers. Themes present but not supported as broadly were giving priority to individuals with disabilities, high frailty or those with behaviours that may have contributed to their ill-health (e.g. smokers). Allocation involving egalitarian approaches received the least support among community members.
Conclusion
The general public prefer rationing scarce medical resources in the COVID-19 pandemic based on saving the most lives and giving priority to the youngest and frontline healthcare workers rather than giving preference to patients with disabilities, frailty or perceived behaviours that may have contributed to their own ill-health. There is also little public support for allocation based on egalitarian strategies.
Keywords: COVID-19, Pandemic, Healthcare allocation, Public preferences, Ethical principles
Background
Since the outbreak of the coronavirus (COVID-19) pandemic, there have been over 496 million confirmed cases and 6.17 million deaths.1 The rapid evolution of the virus saw a dramatic increase in patients, particularly the elderly and those with severe illness, which began to overwhelm the health systems in many countries, resulting in shortages of medical resources, such as ventilators and intensive care unit (ICU) beds and now vaccines.2 The surplus in demand exceeding the availability of healthcare resources led to the unavoidable rationing of medical equipment and interventions, most notably critical care resources which are challenging to expand in a short time.3, 4, 5, 6 How health services and clinicians respond to the need for rationing of scarce but vitally important resources could potentially be a life-and-death situation for patients.
Previous authors have highlighted that hospitals lack a standardized foundation on which to make these rationing decisions.7, 8, 9 In response, ethicists and healthcare policymakers developed guidelines and protocols to avoid health systems becoming overwhelmed10 as well as to help physicians make challenging decisions.3 , 5 , 10 , 11 These decision-making frameworks can have a direct impact on the access to services and health of the public. This process is not dissimilar to what has occurred in other fields where there are scarce health resources. Arguably the most prominent example is that of allocating donated organs, where previous work has synthesised the views of ethicists,3 , 12, 13, 14 clinicians15 , 16 and the public17, 18, 19, 20 as to how this allocation process should take place. However, none of the current COVID-19 guidelines involved community consultation;21, 22, 23, 24, 25, 26, 27 therefore, it is unknown to what extent the current COVID-19 allocation policies align with community preferences and values.
Allocation of scarce health care during pandemic conditions that can be guided by rules and recommendations that do not align with the public's opinions and values could create feelings of injustice and distrust of governments and health systems. This was shown in the UK where early in the pandemic, the UK's National Institute for Health and Care Excellence (NICE) drafted allocation guidelines proposing that all adults on admission to hospital, irrespective of COVID-19 status, be assessed for frailty and that comorbidities and underlying health conditions should be considered.27 This was eventually revised after concerns were raised by several patient groups that the policy would disadvantage some groups, such as those with disabilities.28 This example highlights the difficulty of balancing different ethical criteria, a difficulty exacerbated by the need to make urgent clinical decisions.3 It further highlights the importance of engaging the public in priority setting in health care, a principle that has been widely advocated for.29
As COVID-19 will not be the last pandemic to occur and challenge healthcare systems and in addition to preparing for future healthcare resource shortages, efficient allocation of resources need to be better planned. Therefore, it is necessary to involve the public in discussions before another healthcare crisis eventuates so that resource limitations would not lead to arbitrary allocation decisions, which can lead to public confidence in both health professionals and health systems.30, 31, 32, 33 To help inform such discussions, we conducted a synthesis of the literature that has examined the public's perceptions regarding scarce medical allocation during the COVID-19 pandemic.
Methods
Search strategy
A systematic search was carried out using Ovid MEDLINE, Embase, CINAHL and Scopus using the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) 2020 Statement.34 Specific search strategies were developed with expert librarian support using the search terms: ‘COVID-19’, ‘coronavirus’, ‘community’, ‘layperson∗’, ‘general public’, ‘decision making’, ‘preferences’, ‘healthcare resource allocation’, ‘rationing’ and ‘medical ethics’. Additional data were located with the use of Google Scholar and a search of the reference lists of included articles.
Eligibility criteria
Included were articles that met the following inclusion criteria:
-
1.
Studies published in a peer-reviewed source since December 2019 to coincide with the COVID-19 pandemic outbreak. Abstracts, comments, posters and editorials were excluded.
-
2.
Studies that assessed community preferences for allocation of scarce healthcare resources during the COVID-19 pandemic outbreak. Note: Healthcare resources are defined as any material (e.g. ventilator, ICU bed, vaccine) and facility (e.g. hospital) that can be used for providing healthcare services.
Article selection
The initial database searches were conducted by two researchers and the retrieved literature was imported into Endnote 9.1. Two researchers also independently screened the titles and abstracts of the search results and cross-checked. After initial screening, full texts were downloaded and two researchers read full texts. Disagreements between the researchers were resolved through discussions with a third researcher until consensus was reached.
Data charting process
Relevant data were extracted by two researchers using Excel (Microsoft Corporation), including the first author, country of origin, study design, sample size and key findings for each selected article.
Collation of results
The variation in study designs across articles meant that conducting a systematic review was not possible. Therefore, a thematic synthesis of the findings was conducted using inductive coding to identify emerging themes. As there are no formal guidelines for literature reviews with thematic synthesis, two researchers organised the review into paragraphs that present the themes and identified trends relevant to our topic. Following this, descriptive themes were developed to group common preferences and named accordingly.
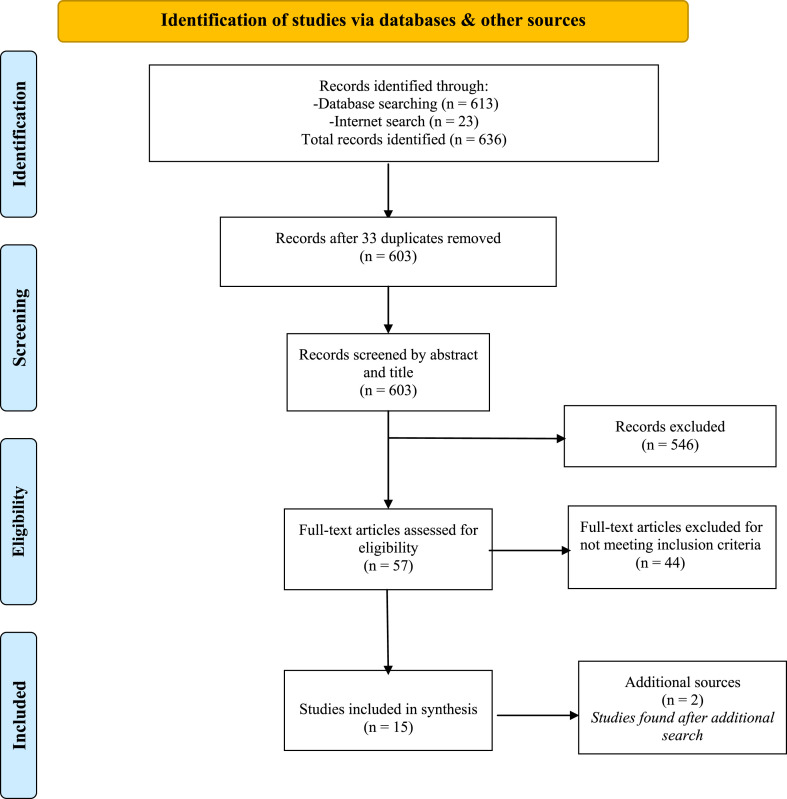
Search results
Overall, 636 records were identified (Fig. 1 ). After the removal of 33 duplicates, 603 abstracts were reviewed against the inclusion criteria. The full texts of 57 articles were reviewed and 44 were excluded. The addition of two articles, identified in a later search, resulted in 15 eligible articles being included.
Fig. 1.
Search process flowchart (PRISMA flow diagram).38
Results
Study characteristics
Table 1 shows that included studies were conducted in the USA,5 Australia and Germany (2 apiece), Iran, Belgium, Israel, the UK and Portugal (1 apiece), while one study was conducted across 11 nations. Studies focused on the allocation of: ventilators,35, 36, 37, 38, 39, 40, 41, 42 ICU beds43, 44, 45 and COVID-19 vaccines.35 , 46 , 47 Various combinations of ethical allocation principles were examined using hypothetical scenarios with ranking,38 , 41 , 46 rating tasks36 , 48 or person trade-off methods.35 , 37 , 39 , 40 , 42 , 43 , 45 , 47, 48, 49, 50, 51 Participant sample size ranged from 306 to 5175. Data were collected between April and December 2021 using cross-sectional online surveys (all) and telephone interviews.46
Table 1.
Characteristics of included studies.
| Author/Year | Study description | Country of origin | Participants (n) | Key findings |
|---|---|---|---|---|
| Ventilator allocation | ||||
| Asghari (2021)40 | Online survey; 11 allocation statements; respondents agreed/disagreed with statements. | Iran | 1262 | Priority based on survival probability, quality of life & social usefulness. Little agreement with prioritization based on first come, first served. |
| Huang (2020)41 | Online survey. Two-stage experimental design (respondents assigned to conditions with/without veil of ignorance applied). | USA | 1276 | Veil of ignorance (VOI) reasoningb favours allocating scarce ventilators to younger patients over older patients, showing that when engaged in VOI reasoning, respondents are more likely to approve of allocation that aims to saving the most lives. |
| Huseynov (2020)42 | Online survey; 1 hypothetical scenario: allocation of 100 ventilators among 1000 COVID-19 patients of varying ages. | USA | 586 | Priority based on survival probability (younger patients). Preference for treating own age group equally. |
| Jin (2021)43 | Online choice based conjoint design; 15 choice sets; 2 hypothetical patients. Recruitment across 11 countries (USA, Brazil, India, UK, Italy, Germany, France, Australia, Spain, China and South Korea) | USA | 5175 | Priority based on survival probability (i.e. allocation to younger patients). |
| Norman (2021)44 | Online DCEa; 12 choice sets. | Australia | 1050 | Priority based on survival probability (i.e. younger, non-smokers), social usefulness & without disability. |
| Werner & Landau (2020)45 | Online survey; 3 hypothetical patients with/without Alzheimer's Disease. Respondents allocated ventilator by order (1st, 2nd and last). | Israel | 309 | Priority based on survival probability & quality of life. Least priority is given to oldest patient with cognitive disorder. |
| Wilkinson (2020)46 | Online survey; 38 choices: 2 hypothetical patients. | UK | 768 | Priority based on survival probability, quality of life & social usefulness. Support for reallocating treatment to save more lives |
| Intensive care bed (ICU) allocation | ||||
| Fallucchi (2020)47 | Online survey; 8 hypothetical triage statements: 2 patients. | USA | 1033 | Priority based on survival probability, social usefulness & those infected with COVID-19. Support for reallocation only when patient has received treatment for 2 months. |
| Street (2021)48 | Online DCEa; 7 choice sets; 14 patient pairs. Respondents prioritise care between two patients requiring ICU bed. | Portugal | 306 | Priority given to patients based on their prognosis (e.g. younger) and social usefulness (i.e. healthcare workers, caregivers). |
| Ventilator and intensive care bed (ICU) allocation | ||||
| Pinho (2021)39 | Online survey; 6 hypothetical allocation statements; 2 patients of different ages, professions, symptom severity, survival. | Australia | 306 | Priority given to patients based on their prognosis, followed by severity of health condition and age. When confronted with survival, youngest first was preferred. Egalitarian allocation least preferred. |
| Sprengholz (2022)49 | Online survey to investigate public's prioritisation preference toward ICU admission for patients who differed in health condition, expected treatment benefits and COVID-19 vaccination status. | Germany | 1014 | Priority given to treating (1) patients who are vaccinated over non-vaccinated; (2) patients with serious health conditions (e.g. heart attack) over patients with COVID-19. The public also more likely to admit a patient to ICU when this meant withholding rather than withdrawing care from another patient. |
| Generic triage policy allocation | ||||
| Buckwalter & Peterson (2020)50 | Three online experiments to investigate public attitude toward hypothetical triage allocation statements. | USA | 1868 | Priority based on survival probability & seriousness of condition, but not when entail reallocation between existing patients, or when they disadvantage at risk groups. |
| COVID-19 vaccine allocation | ||||
| Gollust (2019)49 | Online & telephone survey to assign preference (high-med-low) for delivery of COVID-19 vaccination; 8 hypothetical population groups. | USA | 586 | Priority to people with lower age, higher risk of dying from COVID-19; are pregnant, medical workers or non-medical essential workers. |
| Luyten (2020)51 | Online survey to assign preference (most appropriate-least appropriate) for delivery of COVID-19 vaccination (8 hypothetical population groups). | Belgium | 2060 | Priority to people who are: essential workers, chronically ill and older. Least preferred were egalitarian strategies (e.g. lottery, first come, first served). |
| Sprengholz (2021)51 | Online survey to examine public opinion toward: (1) government COVID-19 allocation policy objectives; and (2) allocating vaccine priority to certain groups (e.g. older vs younger, workers with high exposure risk, nursing home residents). | Germany | 1379 | Public support official COVID-19 vaccination policy objectives. Public support giving vaccine priority to workers with high exposure risk. Least support for assigning priority to older individuals and those living in nursing homes. |
DCE = discrete choice experiment.
Veil of ignorance reasoning = is designed to elicit impartial decision making by denying respondents potentially biasing information about who will benefit the most or least from the available options.
Themes
Five themes emerged from the data that represented the public's preferences for scarce resource allocation under COVID-19 conditions. These are discussed in more detail below.
Theme 1: Prioritise the youngest
Thirteen studies examined the public's preference for favouring younger patients under pandemic conditions.35, 36, 37, 38, 39, 40, 41, 42, 43 , 45 , 46 , 50 , 51 This theme aligns with the ‘prioritisation’ principle, where the goal is to give preference to younger individuals over older individuals because they have had the least opportunity to live through life's stages.52
Patient age appeared to be a major criterion across studies as when patient age and prognosis were examined together, most respondents gave priority to the youngest patients irrespective of prognosis. Several studies reported that most study participants elected to allocate treatment to a younger patient rather than an older patient in situations where life expectancy and survival chance were said to be the same.38 , 42 , 46 , 48 For example, one study reported that when participants were asked to allocate ventilators to patients with similar prognoses, priority was given to younger patients over older patients.38 Another study identified that the public were more in favour of treating a 10-year-old child with little chance of recovery over a 70-year-old with a high survival probability (30% vs 41%, respectively).35
Theme 2: Save the most lives
Another prominent theme was for saving the most lives during COVID-19 and can be regarded as an application of utilitarianism, which seeks to maximise total population health by saving the most lives or as many years of life as possible.53 This was assessed across 10 studies in terms of a patient's survival probability.35 , 36 , 39 , 40 , 42 , 43 , 45 , 48 , 50 , 51
In most studies, the majority of participants allocated high priority for triage policies that prioritised allocation for patients with higher survival chances.36 , 39 , 40 , 42 , 43 , 45 , 46 , 48 , 50 , 51 For example, Wilkinson and colleagues found that approximately 92% of participants chose to treat a patient with an 80% survival chance, whereas only 5% gave priority to a patient with a 10% probability of survival.42 Several studies found that participants appeared willing to withdraw treatment from a patient in ICU who had a lower survival chance than another patient with a higher survival probability currently presenting with COVID-19.42 , 43
Theme 3: Egalitarian allocation approaches (e.g. waiting lists and random allocation)
This theme relates to giving all patients an equal chance at receiving scarce resources through applying a first-come, first-served basis or random allocation strategy,54 and encompasses the principles of egalitarianism, which aims to give all patients an equal chance at receiving scarce resources.54 Nine studies assessed public support for these allocation strategies.35, 36, 37 , 39 , 40 , 42 , 43 , 45 , 46 , 48 , 50 , 51
Evident across studies that while the public are least supportive of allocation based on order or randomisation, there was heterogeneity in people's moral judgements toward them and this appeared to be influenced by whether or not specific characteristics of competing patients were presented to participants. For example, when asked to consider triage policy statements that contain no information about the patients' age or prognosis, most participants outrightly rejected both randomisation and first-come, first-served principles35, 36, 37 , 39 , 40 , 42 , 43 , 46 , 48 , 50 , 51 or were ambivalent.40 Conversely, when presented with patient clinical information, and age, participants were more likely to default to an ‘equal chance’ position.35, 36, 37 , 39 , 40 , 42 , 43 , 46 , 48 , 50 , 51 For example, one study found that over half of participants (55%) chose a coin toss to decide between two patients with small differences in life expectancy (15 vs 14 years).42
Theme 4: Prioritise healthcare workers
Eight studies35, 36, 37 , 39 , 40 , 42 , 43 , 46 , 48 , 50 , 51 examined public attitude toward prioritization of healthcare workers patients. This appeared to be a popular strategy among participants in seven studies.35, 36, 37 , 39 , 40 , 42 , 43 , 46, 47, 48 , 50 , 51 For example, one study examining COVID-19 vaccine priority found that almost all participants (92%) preferred to give vaccines to frontline healthcare workers before others, including individuals who were at high risk of mortality from COVID-19.46 Another study reported that 63% of the study sample prioritised healthcare workers to receive the remaining ventilator over a non-healthcare professional.42
Theme 5: Bias against particular groups
Nine studies examined the public opinion toward allocation bias.36 , 39, 40, 41, 42 , 45 , 48 , 50 , 55 That is, differences in how participants’ preferences for assigning treatment to specific patient groups, such as those with disabilities and frailty and those with perceived behaviours that may have contributed to their ill-health.
The general public did not appear to favour allocating limited healthcare resources, such as ventilators or ICU beds to patients who were smokers,40 had poor self-rated health,50 had criminal histories,39 or were illicit drug users.48 Patients who were considered likely COVID-19 spreaders or did not comply with COVID-19 rules, such as mask wearing or social distancing were also not given treatment priority by the community.55 The public were also less willing to give lower priority to patients with disabilities40 , 42 , 48 or those with high degrees of frailty.42 For example, one study reported that the majority of respondents (74%) elected to allocate treatment to a non-disabled patient in preference to a patient with a profound learning disability,42 whereas only a minority (∼19%) elected to treat patients with greater disability.42 Another study reported that the public gave priority for COVID-19 vaccinations to staff in medical facilities, outpatient care and nursing homes for the elderly over vulnerable groups (e.g. nursing home residents and people aged 75 years and older).47
Discussion
This study identified several themes related to how the general public preferences the allocation of health care resources during the current COVID-19 pandemic. Our findings show that the public have a clear preference for allocation that aims to save the most lives and give priority to younger patients and health care workers. Participants also demonstrated some degree of allocation bias, deprioritising of those with disabilities and directing resources away from people with behaviours that increased their own risk of becoming diseased. Less support was also found for egalitarian allocation approaches such as first-come, first-served or randomization approaches, particularly when additional information about patient scenarios (e.g. prognosis) were added into scenarios.
These findings can be contrasted with previous research and published opinions that have examined how to allocate resources in the context of resource scarcity (see Appendix 1). Donor organ allocation is one area that faces ongoing scarcity and ethical debate and therefore makes a useful and relevant comparison to our study.17 , 56 It is evident that, irrespective of context, the public view reducing mortality as an important achievement when considering scarce healthcare allocation. When selecting organ transplant recipients, the public regard the capacity to survive and benefit as one of the most important criteria,17 , 56 which aligns with our finding of prioritised allocation for patients with higher survival chances under COVID-19 conditions. This is also consistent with prior research examining community preferences under pandemic conditions.57, 58, 59, 60, 61, 62 It is also apparent that across contexts the public make judgements based on a patient's lifestyle decisions under conditions of scarcity in that the public are willing to assign less priority to individuals with perceived behaviours that may have contributed to their illness for both donor organ recipients17 , 56 and COVID-19 patients.36 , 39, 40, 41, 42 , 45 , 50 , 55 Prior studies also suggest that the public tend to negatively sanction those who are deemed responsible for their predicament.63, 64, 65, 66, 67 These overall findings suggest that while the community are willing to endorse allocation policies that maximise the number of lives saved during conditions of healthcare scarcity, they also believe the patient's deservingness to receive scarce treatment should be taken into consideration. Our findings may have particular importance in the current COVID-19 context as individuals with substance abuse disorders, for example, are a high-risk group for contracting COVID-19 and its transmission and casualties because they usually suffer from poorer health, weaker immune function, chronic infections, as well as various issues with physical and psychiatric comorbidities.68 , 69
Some of our findings appear less consistent with the preferences expressed among community members for the allocation of donor organs17 , 56 (see also Appendix 1). When considering donor organ allocation, the public are not in favour of prioritising patients based on their occupation,17 , 56 whereas we found strong community support for giving preferences to healthcare workers during COVID-19. Rather, community opinion is that patients in need of a donor organ should be placed on a wait list unless they are children, patients with dependents or have spent long periods on a wait list.17 , 56 Under COVID-19 conditions, we observed little community support for treating patients on a first-come, first-served basis. When comparing our findings with prior studies of allocation during pandemics, we also find mixed support for these principles.59 , 70 Studies examining public attitudes toward limited healthcare distribution during an influenza pandemic, for example, have reported inconsistent results.59 , 61 For example, one study found community support for prioritising healthcare workers for treatments,62 whereas another study reported public support for wait lists but not instrumental value.61 However, it should be noted that these studies were not conducted under ‘real-life’ global pandemic conditions, so it is plausible that our findings may be more of an accurate reflection of community sentiment during a public health crisis.
Expert opinions related to this field have also been published. For example, in 2020, the New England Journal of Medicine published an opinion paper written by medical ethicists discussing recommendations for the allocation of scarce medical resources during the COVID-19 pandemic.71 Overall, there was high agreement between our findings and the opinions of these authors for allocation strategies under COVID-19 conditions (see Appendix 1). For example, the overarching view among both groups is that one of the most important goals of pandemic preparations is mortality reduction or ‘saving the most lives’, especially to individuals who may be at ‘risk of dying young and not having a full life’.71 In addition, members of the community and ethicists agree that treatment preference should be given to frontline COVID-19 healthcare workers because of their instrumental value in keeping critical infrastructure operating.71 However, the public disagree with these authors' recommendation that treatment priority should be given to people involved in COVID-19 therapeutics research and development (e.g. vaccines).71 Further agreement was also reached on allocation strategies where patients had small differences in treatment outcomes. That is, when presented with patients with small differences in survival probability, the public appears to agree with the authors' position that randomization should be applied rather than wait lists.71
Conclusion
Under COVID-19 conditions, the public appear to agree that saving the most lives, especially the youngest, is the most important principle for scarce resource allocation. In addition, the public support giving treatment priority to frontline healthcare workers and are willing to deprioritise particular patient groups, such as those with disabilities or those who are considered to having contributed to their own ill health in some way (e.g. drug takers, smokers). Allocation involving egalitarian approaches received the least support among community members. The values expressed by the public under pandemic conditions were found to both converge and diverge from expert guidance as well as with community attitudes toward donor organ allocation. Awareness of these differences highlights the importance of involving the public in discussions around the efficient allocation of scarce resources and here qualitative research would be helpful in understanding an individual's motivation for their allocation preferences.
Author statements
Ethical approval
None sought.
Funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interests
All authors declare that they have no financial, personal, or potential conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2022.06.004.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.COVID Live . 2022. Coronavirus statistics - worldometer. Cases and deaths from covid-19.https://www.worldometers.info/coronavirus/ (Viewed 20 April 2022) [Google Scholar]
- 2.Supady A., Curtis J., Abrams D., Lorusso R., Bein T., Boldt J., et al. Allocating scarce intensive care resources during the COVID-19 pandemic: practical challenges to theoretical frameworks. Lancet Respir Med. 2021;9(4):430–434. doi: 10.1016/S2213-2600(20)30580-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Emanuel E., Persad G., Upshur R., Thome B., Parker M., Glickman A., et al. Fair allocation of scarce medical resources in the time of covid-19. N Engl J Med. 2020;382(21):2049. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 4.Rosenbaum L. Facing covid-19 in Italy - ethics, logistics, and therapeutics on the epidemic's front line.(perspective) N Engl J Med. 2020;382(20):1873. doi: 10.1056/NEJMp2005492. [DOI] [PubMed] [Google Scholar]
- 5.White D., Lo B. A framework for rationing ventilators and critical care beds during the COVID-19 pandemic. JAMA. 2020;323(18):1773. doi: 10.1001/jama.2020.5046. [DOI] [PubMed] [Google Scholar]
- 6.Arya A., Buchman S., Gagnon B., Downar J. Pandemic palliative care: beyond ventilators and saving lives. CMAJ (Can Med Assoc J) 2020;192(15):E400–E404. doi: 10.1503/cmaj.200465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ehmann M., Zink E., Levin A., et al. Operational recommendations for scarce resource allocation in a public health crisis. Chest. 2021;159(3):1076–1083. doi: 10.1016/j.chest.2020.09.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smorto G. The right to health and resource allocation. Who gets what and why in the COVID-19 pandemic. Glob Jurist. 2020;21(1):59–72. [Google Scholar]
- 9.Jerry R. COVID-19: responsibility and accountability in a world of rationing. J law Biosci. 2020;7(1) [Google Scholar]
- 10.Robert R., Kentish-Barnes N., Boyer A., Laurent A., Azoulay E., Reignier J. Ethical dilemmas due to the Covid-19 pandemic. Ann Intensive Care. 2020;10(1):84. doi: 10.1186/s13613-020-00702-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abubakar I., Aldridge R.W., Devakumar D., Orcutt M., Burns R., Barreto M.L., et al. The UCL–lancet commission on migration and health: the health of a world on the move. Lancet. 2018;392(10164):2606–2654. doi: 10.1016/S0140-6736(18)32114-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abouna G. Ethical issues in organ transplantation. Med Princ Pract. 2003;12(1):54–69. doi: 10.1159/000068158. [DOI] [PubMed] [Google Scholar]
- 13.Freeman R., Bernat J. Ethical issues in organ transplantation. Prog Cardiovasc Dis. 2012;55(3):282–289. doi: 10.1016/j.pcad.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 14.Modra L., Hilton A. Ethical issues in organ transplantation. Anaesth Intensive Care Med. 2021;22(8):467–470. [Google Scholar]
- 15.Pratt B., Hyder A. Fair resource allocation to health research: priority topics for bioethics scholarship. Bioethics. 2017;31(6):454–466. doi: 10.1111/bioe.12350. [DOI] [PubMed] [Google Scholar]
- 16.Tong A., Chapman J., Wong G., Craig J. Perspectives of transplant physicians and surgeons on reimbursement, compensation, and incentives for living kidney donors. Am J Kidney Dis. 2014;64(4):622–632. doi: 10.1053/j.ajkd.2014.02.019. [DOI] [PubMed] [Google Scholar]
- 17.Tong A., Howard K., Jan S., Cass A., Rose J., Chadban S., et al. Community preferences for the allocation of solid organs for transplantation: a systematic review. Transplantation. 2010;89(7):796–805. doi: 10.1097/TP.0b013e3181cf1ee1. [DOI] [PubMed] [Google Scholar]
- 18.Howard K., Jan S., Rose J., Chadban S., Allen R., Irving M., et al. Community preferences for the allocation & donation of organs-the PAraDOx study. BMC Publ Health. 2011;11(1):386. doi: 10.1186/1471-2458-11-386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Broumand M., Parsapoor A., Asghari F. Public opinion of organ donation: a survey in Iran. Clin Transplant. 2012;26(5):E500–E504. doi: 10.1111/ctr.12001. [DOI] [PubMed] [Google Scholar]
- 20.Chandler J., Burkell J., Shemie S. Priority in organ allocation to previously registered donors: public perceptions of the fairness and effectiveness of priority systems. Prog Transplant. 2012;22(4):413–422. doi: 10.7182/pit2012324. [DOI] [PubMed] [Google Scholar]
- 21.ANZICS . 2021. ANZICS COVID-19 guidelines. Version 4, 23 September 2021. [Google Scholar]
- 22.Persaud N., Woods H., Workentin A., Adekoya I., Dunn J., Hwang S., et al. Recommendations for equitable COVID-19 pandemic recovery in Canada. Can Med Assoc J. 2021;193(49):E1878–E1888. doi: 10.1503/cmaj.210904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hurford J. The BMA COVID-19 ethical guidance: a legal analysis. N Bioeth. 2020;26(2):176–189. doi: 10.1080/20502877.2020.1762027. [DOI] [PubMed] [Google Scholar]
- 24.Società Italiana di Anestesia Analgesia Rianimazione e Terapia Intensiva (SIAARTI 2020) Airway research group and the European airway management society (EAMS 2020) https://reference.medscape.com/viewarticle/928166 (Viewed 12 Dec 2020).
- 25.National Bioethics Committee, Pakistan . Center of Biomedical Ethics & Culture National Bioethics Committee, Pakistan Ministry of National Health Services Regulations & Coordination; 2020. COVID-19 pandemic: guidelines for ethical healthcare decision-making in Pakistan.https://storage.covid.gov.pk/new_guidelines/01June2020_Guidelines_for_Ethical_Healthcare_Decision-Making_in_Pakistan.pdf Published May 6, 2020. (Viewed 12 Dec 2020) [Google Scholar]
- 26.Critical Care Society of Southern Africa (CCSSA) 5 May 2020. Allocation of scarce critical care resources during the COVID-19 public health emergency in South Africa - version 3. Critical care society of Southern Africa.https://criticalcare.org.za/wp-content/uploads/2020/06/V3-2020-May-05-Allocation-of-Scarce-Critical-Care-Resources-During-the-COVID-19-Public-Health-Emergency-in-South-Africa-FINAL-.pdf [PubMed] [Google Scholar]
- 27.The National Institute for Health and Care Excellence (NICE) National Institute for Health and Care Excellence; 2020. COVID-19 rapid guideline: managing COVID-19.https://www.nice.org.uk/guidance/ng191/resources/covid19-rapid-guideline-managing-covid19-pdf-51035553326 [Google Scholar]
- 28.The National Institute for Health and Care Excellence (NICE) National Institute for Health and Care Excellence; 2020. NICE updates rapid COVID-19 guideline on critical care - 25 March 2020.https://www.nice.org.uk/news/article/nice-updates-rapid-covid-19-guideline-on-critical-care [Google Scholar]
- 29.Silva D., Gibson J., Robertson A., Bensimon C., Sahni S., Maunula L., et al. Priority setting of ICU resources in an influenza pandemic: a qualitative study of the Canadian public's perspectives. BMC Publ Health. 2012;12(1):241. doi: 10.1186/1471-2458-12-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gu Y., Lancsar E., Ghijben P., Butler J., Donaldson C. Attributes and weights in health care priority setting: a systematic review of what counts and to what extent. Soc Sci Med. 2015;146:41–52. doi: 10.1016/j.socscimed.2015.10.005. (1982) [DOI] [PubMed] [Google Scholar]
- 31.Ahlert M., Pfarr C. Attitudes of Germans towards distributive issues in the German health system. Eur J Health Econ. 2016;17(4):471–496. doi: 10.1007/s10198-015-0693-x. [DOI] [PubMed] [Google Scholar]
- 32.Krutli P., Rosemann T., Tornblom K., Smieszek T. How to fairly allocate scarce medical resources: ethical argumentation under scrutiny by health professionals and lay people.(report) PLoS One. 2016;11(7):e0159086. doi: 10.1371/journal.pone.0159086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Krütli P., Rosemann T., Törnblom K.Y., Smieszek T. How to fairly allocate scarce medical resources: ethical argumentation under scrutiny by health professionals and lay people. PLoS One. 2016;11(7):e0159086. doi: 10.1371/journal.pone.0159086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Page M., McKenzie J., Bossuyt P., Boutron I., Hoffman T., Mulrow C., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;(71):372. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pinho M. Public preferences for allocating absolute scarce critical healthcare resources during the COVID-19 pandemic. J Health Organisat Manag. 2021;35(8):964–986. doi: 10.1108/JHOM-12-2020-0494. [DOI] [PubMed] [Google Scholar]
- 36.Asghari F., Parsapour A., Shamsi Gooshki E. Priority setting of ventilators in the COVID-19 pandemic from the public's perspective. AJOB empirical bioethics. 2021;12(3):155–163. doi: 10.1080/23294515.2021.1907474. [DOI] [PubMed] [Google Scholar]
- 37.Huang K., Bernhard R., Barak-Corren N., Bazerman M., Greene J. Veil-of-Ignorance reasoning favors allocating resources to younger patients during the COVID-19 crisis. Judgement and Decision Making. 2021;16(1):1–19. [Google Scholar]
- 38.Huseynov S., Palma M., Nayga R. 2020. General public preferences for allocating scarce medical resources during covid-19. (Online article) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jin L., Huang Y., Liang Y., Zhang Q. Who gets the ventilator? Moral decision making regarding medical resource allocation in a pandemic. J Asso Consum Res. 2021;6(1):159–167. [Google Scholar]
- 40.Norman R., Robinson S., Dickinson H., Williams L., Meshcheriakova E., Manipis K., et al. The Patient-Patient-Centered Outcomes Research; 2021. Public preferences for allocating ventilators in an intensive care unit: a discrete choice experiment. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Werner P., Landau R. Laypersons' priority-setting preferences for allocating a COVID-19 patient to a ventilator: does a diagnosis of alzheimer's disease matter? Clin Interv Aging. 2020;15:2407–2414. doi: 10.2147/CIA.S283015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wilkinson D., Zohny H., Kappes A., Sinnott-Armstrong W., Savulescu J. Which factors should be included in triage? An online survey of the attitudes of the UK general public to pandemic triage dilemmas. BMJ Open. 2020;10(12) doi: 10.1136/bmjopen-2020-045593. e045593-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fallucchi F., Faravelli M., Quercia S. Fair allocation of scarce medical resources in the time of COVID-19: what do people think? J Med Ethics. 2020;382:2049–2055. doi: 10.1136/medethics-2020-106524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ashcraft A.S., Owen D.C. From nursing home to acute care: signs, symptoms, and strategies used to prevent transfer. Geriatr Nurs. 2014;35(4):316–320. doi: 10.1016/j.gerinurse.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 45.Sprengholz P., Korn L., Felgendreff L., Eitze S., Betsch C. Medical Letter on the CDC & FDA; 2022. A lay perspective on prioritization for intensive care in pandemic times: vaccination status matters; p. 31. (Updated May 6, 2022) [Google Scholar]
- 46.Gollust S., Saloner B., Hest R., L B. US adults' preferences for public allocation of a vaccine for coronavirus disease 2019. JAMA Netw Open. 2019;3(9) doi: 10.1001/jamanetworkopen.2020.23020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sprengholz P., Korn L., Eitze S., Betsch C. Allocation of COVID-19 vaccination: when public prioritisation preferences differ from official regulations. J Med Ethics. 2021;47(7):452–455. doi: 10.1136/medethics-2021-107339. [DOI] [PubMed] [Google Scholar]
- 48.Buckwalter W., Peterson A. Public attitudes toward allocating scarce resources in the COVID-19 pandemic. PLoS One. 2020;15(11) doi: 10.1371/journal.pone.0240651. e0240651-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.McLeod C., Norman R., Schultz A., Mascaro S., Webb S., Snelling T. Discrete choice experiment to evaluate preferences of patients with cystic fibrosis among alternative treatment-related health outcomes: a protocol. BMJ Open. 2019;9(8) doi: 10.1136/bmjopen-2019-030348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Street A., Street D., Flynn G. Who gets the last bed? A discrete-choice experiment examining general population preferences for intensive care bed prioritization in a pandemic. Med Decis Making. 2021;41(4):408–418. doi: 10.1177/0272989X21996615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Luyten J., Kessels R., Tubeuf S. Who should get it first? Public preferences for prioritising a covid-19 vaccine. Covid Eco Vetted Real Time Papers. 2020;57:1–19. [Google Scholar]
- 52.White D., Katz M., Luce J., Lo B. Who should receive life support during a public health emergency? Using ethical principles to improve allocation decisions. Ann Intern Med. 2009;150(2):132–138. doi: 10.7326/0003-4819-150-2-200901200-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Scheunemann L., White D. The ethics and reality of rationing in medicine. Chest. 2011;140(6):1625. doi: 10.1378/chest.11-0622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Persad G., Wertheimer A., Emanuel E. Principles for allocation of scarce medical interventions. Lancet. 2009;373(9661):423–431. doi: 10.1016/S0140-6736(09)60137-9. [DOI] [PubMed] [Google Scholar]
- 55.Luyten J., Kessels R., Goos P., Beutels P. Public preferences for prioritizing preventive and curative health care interventions: a discrete choice experiment. Value Health. 2015;18(2):224–233. doi: 10.1016/j.jval.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 56.Oedingen C., Bartling T., Mühlbacher A., Schrem H., Krauth C. Systematic review of public preferences for the allocation of donor organs for transplantation: principles of distributive justice. Patient. 2019;12(5):475–489. doi: 10.1007/s40271-019-00363-0. [DOI] [PubMed] [Google Scholar]
- 57.Grover S., McClelland A., Furnham A. Preferences for scarce medical resource allocation: differences between experts and the general public and implications for the COVID-19 pandemic. Br J Health Psychol. 2020 doi: 10.1111/bjhp.12439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Daugherty Biddison E., Gwon H., Schoch-Spana M., Cavalier R., White D., Dawson T., et al. The community speaks: understanding ethical values in allocation of scarce lifesaving resources during disasters. Ann Am Thorac Soc. 2014;11(5):777–783. doi: 10.1513/AnnalsATS.201310-379OC. [DOI] [PubMed] [Google Scholar]
- 59.Li-Vollmer M. Society for Participatory Medicine; 2010. Health care decisions in disasters: engaging the public on medical service prioritization during a severe influenza pandemic.https://participatorymedicine.org/journal/evidence/case-studies/2010/12/14/health-care-decisions-in-disasters-engaging-the-public-on-medical-service-prioritization-during-a-severe-influenza-pandemic/ (Viewed 12 Dec 2021) [Google Scholar]
- 60.Ritvo P., Wilson K., Gibson J., Guglietti C., Tracy C., Nie J.X., et al. Canadian survey on pandemic flu preparations. BMC Publ Health. 2010;10(1):125. doi: 10.1186/1471-2458-10-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vawter D., Garrett J., Gervais K., Witt Prehen A., DeBruin D., Tauer C., et al. Minnesota Pandemic Ethics Project Report; 2010. For the good of us all:ethically rationing health resources in Minnesota a severe influenza pandemic.https://www.health.state.mn.us/communities/ep/surge/crisis/ethics.pdf Minnesota Dept of Health. [Google Scholar]
- 62.Krütli P., Rosemann T., Törnblom K., Smieszek T. How to fairly allocate scarce medical resources: ethical argumentation under scrutiny by health professionals and lay people. PLoS One. 2016;11(7) doi: 10.1371/journal.pone.0159086. e0159086-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ghamari S.H., Abbasi-Kangevari M., Zamani N., Hassanian-Moghaddam H., Kolahi A.A. Priorities towards fair allocation of ventilators during COVID-19 pandemic: a delphi study. Front Med. 2021;8 doi: 10.3389/fmed.2021.769508. 769508-769508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Abbasi-Kangevari M., Arshi S., Hassanian-Moghaddam H., Kolahi A.-A. Public opinion on priorities toward fair allocation of ventilators during COVID-19 pandemic: a nationwide survey. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.753048. 753048-753048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Skitka L., Tetlock P. Allocating scarce resources: a contingency model of distributive justice. J Exp Soc Psychol. 1992;28(6):491–522. doi: 10.1016/0022-1031(92)90043-J. [DOI] [Google Scholar]
- 66.Furnham A., Thomson K., McClelland A. The allocation of scarce medical resources across medical conditions. Psychol Psychother. 2002;75(2):189–203. doi: 10.1348/147608302169643. [DOI] [PubMed] [Google Scholar]
- 67.Fortes P., Zoboli E. A study on the ethics of microallocation of scarce resources in health care. J Med Ethics. 2002;28(4):266–269. doi: 10.1136/jme.28.4.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Farhoudian A., Baldacchino A., Clark N., Gerra G., Ekhtiari H., Dom G., et al. COVID-19 and substance use disorders: recommendations to a comprehensive healthcare response. An international society of addiction medicine (ISAM) practice and policy interest group position paper. Basic Clin Neurosci. 2020;11(2):133–150. doi: 10.32598/bcn.11.covid19.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wang Q., Kaelber D., Xu R., Volkow N. COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol Psychiatr. 2021;26(1):30–39. doi: 10.1038/s41380-020-00880-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Norisue Y., Deshpande G., Kamada M., Nabeshima T., Tokuda Y., Goto T., et al. Allocation of mechanical ventilators during a pandemic: a mixed-methods study of perceptions among Japanese health care workers and the general public. Chest. 2021;159(6):2494–2502. doi: 10.1016/j.chest.2021.01.015. [DOI] [PubMed] [Google Scholar]
- 71.Lenton A., Blair I., Hastie R. The influence of social categories and patient responsibility on health care allocation decisions: bias or fairness? Basic Appl Soc Psychol. 2006;28(1):27–36. doi: 10.1207/s15324834basp2801_3. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.