Abstract
Purpose
Measures taken to limit the spread of the COVID-19 may have had unintended consequences for the mental and somatic health of children and adolescents.
Methods
A nationwide three-wave survey in a representative sample of 12–16 year olds in Norway, with baseline data collected in January 2019 (n = 9,240; 49% girls) and follow-ups in June 2020 (n = 3,564; 49% girls) and June 2021 (n = 3,540; 47% girls). Linear mixed-effects models were used to estimate change and identify predictors thereof in mental and somatic health complaints.
Results
Following an initial stable trend from before the pandemic to the early phase, both mental health problems (predicted value at T1 .56 [CI .55, .58], T1-T2 change −.04 [CI −.07, −.02], T2-T3 change .12 [CI .09, .14]) and somatic health complaints (predicted value at T1 .59 [95% CI .58, .61], T1-T2 difference −.09 [95% CI −.11, −.65], T2-T3 difference .18 [95% CI .15, .21]) increased significantly 15 months into the pandemic, when controlling for age in the models. When compared to boys, girls had a significantly more pronounced increase in mental health problems and somatic health; loneliness in the early stages of the pandemic significantly predicted health complaints one year later, both mental and somatic complaints.
Discussion
Our findings suggest that the prolonged pandemic situation and the related societal restrictions have had an impact on adolescent health in general and on the health of girls in particular. The rise in mental and somatic health complaints can in part be attributed to an increase in loneliness.
Keywords: COVID-19, Adolescent mental health, Anxiety and depression, Somatic health complaints, Population sample, Prospective study
Implications and Contribution.
Current evidence suggests that with a continued use of persistent measures to combat the spread of COVID-19 virus, we can expect a continued appreciable increase in symptoms of mental and somatic health problems among adolescents. It is critical to continue monitoring adolescents to learn about the persistence of symptoms after the pandemic.
Restrictions aimed at controlling the spread of the COVID-19 have had an impact on the lives of billions of children, adolescents, and their families [1]. Many people have experienced recurring episodes of social isolation and a prolonged fear of contagion. Other pandemic-related factors have been discussed as potential risk factors for psychopathology during the pandemic, such as mandatory school closures, cancellation of all sports and leisure activities, financial hardship, and child and family stress associated with these mitigation measures [2,3]. Norway, a sparsely populated Northern European country known for its social democratic welfare state, was one of the first to implement a nationwide lockdown on March 12, 2020. This included the mandatory closure of all schools at all levels and the cancellation of organized sports. In general, social distancing measures, such as limiting social interactions to household members, were strongly encouraged. While preprimary and primary schools reopened within a few weeks, other educational institutions and organized sports for adolescents remained closed until mid-May 2020. As a result of the dynamic change in contagion, new restrictions have been implemented throughout 2020 and 2021. In Norway, adolescents have been disproportionately affected by restrictions when compared to younger children and adults, as middle and high schools faced the most restrictive measures, including repeated and extended home schooling periods and cancelled sports activities throughout the pandemic years. At the same time, adolescence may be regarded as a vulnerable developmental stage during which mental health issues emerge [4]. Based on previous and current knowledge about adolescent mental health and related risk factors, we are particularly concerned that ongoing efforts to combat the spread of the virus may amplify an already increasing trend in mental health problems among adolescents [5].
Concerns have been raised by the rapid accumulation of research aimed at understanding the impact of the pandemic on multiple domains of adolescent health. As per meta-analytic evidence from the first year of the pandemic, adolescent mental health has deteriorated globally [6]. Despite being less studied, emerging evidence indicates an increase in somatic health complaints [7,8]. Adolescents with pre-existing mental and/or somatic health problems appear to be especially vulnerable to aggravating health problems during the pandemic [8]. However, the evidence from the first year of the pandemic in Norway indicates that most adolescents adapted efficiently to pandemic conditions, as evidenced by no notable changes in depressive symptoms, somatic health, or friendships compared to prepandemic levels [9,10]. The inconclusive results from existing studies may be attributed to factors such as variations in societies' pandemic-related burdens, timing of data collection during the pandemic, and study design [11]. For example, the timing of data collection during the pandemic may have an impact on findings, as symptoms may vary as pandemic measures are implemented [12]. During the pandemic, most studies with adolescent samples published to date have been cross-sectional, relying primarily on convenience and online-based nonprobability sampling [11]. However, studies with adolescents must account for the wide age and gender differences in mental health problems during adolescence [13]. As demonstrated by our first study on changes in Norwegian adolescents' mental health during the pandemic, the observed increase in symptoms appeared to be driven by age rather than pandemic-related factors [9]. Continuous prospective investigation of changes in symptoms is required to understand the long-term changes in symptoms during several waves of infection and subsequent mitigation measures. Preferably, a prepandemic sample would be followed over time.
To promote adolescent resilience and mitigate the negative effects of current and future pandemics, we must first identify the factors associated with the development of mental and somatic health problems in adolescents during the pandemic. We aimed to determine (1) whether mental health problems, in terms of symptoms of anxiety and depression, and somatic health complaints increased or decreased from before the pandemic to one year into the pandemic, (2) whether certain groups of adolescents were disproportionately affected by the pandemic, as evidenced by a greater increase in symptoms, and (3) what factors predicted higher levels of mental and somatic health complaints one year into the pandemic.
Methods
Design and sample
The study is part of an ongoing nationwide longitudinal survey study of a representative sample of 9,240 Norwegian aged 12–16 years [14]. The first wave of the survey was conducted in January 2019, about a year before the COVID-19 outbreak, with two follow-up assessments in June 2020 and June 2021, respectively, to assess the potential impact of the COVID-19 pandemic on adolescent health and wellbeing. The survey was administered in schools sampled for their geographical representativeness (all regions of Norway were covered), school size, and ethnic minority status. Students participated by filling out an online questionnaire. The survey was only available in Norwegian and students who did not have a sufficient level of Norwegian language skills were unable to participate.
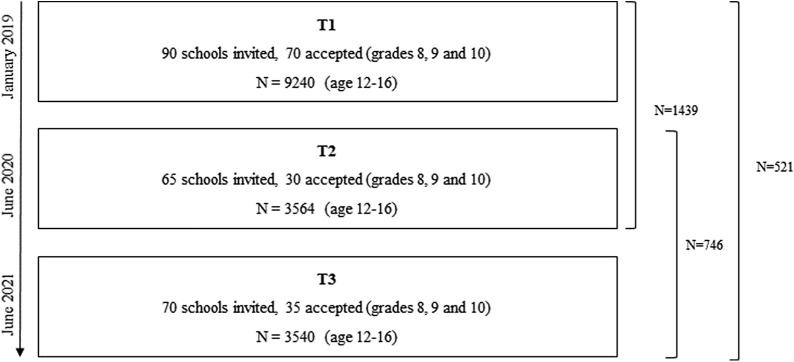
A total of 3,564 (50.1% girls; n = 1,776) took part in the second data collection wave (T2, June 2020), whereas 3,540 (47.3% girls; n = 1,675) took part in the third data collection wave (T3, June 2021). Age range at all three data collection points was 12–16 years. Figure 1 depicts an overview of the study design and data collection points.
Figure 1.
Overview of study design and sample size at the three data collection points.
As the survey was distributed to all participating schools three times, it was possible for students to take part at one, two, or all data collection points. Students who were in the 10th grade at wave 1 and 2 were not eligible at the next wave because they had left school at that point. As such, we lost about one-third of the original sample for each wave and got a new group of eighth graders for each wave. Altogether, 521 adolescents had data at all three time points.
Attrition and representativeness
In terms of all included background variables, samples from T1, T2, and T3 were comparable (Table 1 ). However, further attrition analyses revealed that those who participated at all three time points reported fewer symptoms of mental health problems (mean = .42, SD = .53, possible range 0–3) compared to those who only participated at T1 (mean = .59, SD = 67; P < .001). Similarly, participants who participated at all three time points reported fewer symptoms of somatic health complaints (mean = .49, SD = .53) than those who only participated at T1 (mean = .60, SD = 68; P = .001). This suggests that adolescents with higher levels of mental health problems and somatic health complaints at T1 may have been less likely to participate in follow-up surveys at T2 or T3.
Table 1.
Characteristics of the sample at the three measurement points
| Variables | T1 (2019) N = 9,240 |
T2 (2020) N = 3,564 |
T3 (2021) N = 3,540 |
T1_T2-T3∗ N = 521 |
||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |
| Gender | ||||||||
| Girls | 4,592 | 50.0 | 1,774 | 50.1 | 1,675 | 47.6 | 254 | 51.0 |
| Boys | 4,538 | 49.4 | 1,733 | 49.0 | 1,733 | 49.0 | 241 | 48.4 |
| Non binary | 63 | 0.7 | 33 | 0.9 | 63 | 1.8 | <5 | - |
| Single parent household | ||||||||
| Yes | 2,725 | 29.7 | 1,070 | 30.3 | 1,077 | 30.7 | 138 | 27.8 |
| No | 6,458 | 70.3 | 2,457 | 69.7 | 2,429 | 69.3 | 358 | 72.2 |
| Country of origin | ||||||||
| Non-Nordic | 2,349 | 25.9 | 858 | 24.6 | 904 | 26.1 | 101 | 20.5 |
| Nordic | 6,707 | 74.1 | 2,627 | 75.4 | 2,554 | 73.9 | 391 | 79.5 |
| Family affluence | ||||||||
| Low | 351 | 3.8 | 103 | 3.0 | 131 | 3.8 | 10 | 2.0 |
| High/Normal | 8,773 | 96.2 | 3,369 | 97.0 | 3,337 | 3.8 | 484 | 98.0 |
| Age: mean, SD (12–16) | 14.11 | 0.8 | 14.52 | 0.9 | 14.48 | .96 | 14.53 | .52 |
| HSCL: mean, SD (0–3) | .57 | .66 | .55 | .64 | .72 | .74 | .42 | .53 |
| CSSI: mean, SD (0–3) | .60 | .67 | .53 | .65 | .79 | .83 | .49 | .54 |
Sample with data on all three measurement points–descriptive data reported from the T1 measurement for comparison.
Measures
Background variables
Participants reported their age in years at all three time points. Perceived family affluence was measured using two questions: whether the adolescent perceived the family as having sufficient economic means to purchase necessary goods and whether the adolescent had experienced a decline in participation in after-school activities due to family finances. The two items yielded a Spearman-Brown coefficient of .56. The first question was rated on a four-point scale from 0 (completely agree) to 3 (completely disagree) and the latter was rated on a four-point scale from 0 (never) to 3 (often). A perceived family affluence dichotomized composite score was derived based on responses to these two questions; if two or three were indicated on either of the two questions, a “low perceived family affluence score” was allocated to that individual (1). We also assessed the parents' country of origin, which was coded as Norway, another Nordic country, Europe (outside the Nordic region), or outside of Europe. A history of abuse was evaluated using a series of questions that assessed lifetime exposure to physical, emotional, or sexual abuse and witnessing domestic violence. These experiences were combined into a cumulative scale (possible range 0–7), with a higher score indicating greater exposure.
Anxiety and depression symptoms
We examined anxiety and depression symptoms using the Hopkins Symptom Checklist-10 (HSCL-10) at all three time points. HSCL-10 is a self-report questionnaire used in population surveys to assess psychological distress. Each item is presented on a four-point scale (i.e., 0–3), ranging from ‘Not at all’ and ‘A little’ to ‘Quite a bit’ and ‘Extremely’, and is summarized as a mean score that requires a valid response on at least half of the items to compute a score. Items covered symptoms of worry, anxiety, and lack of interest (e.g., “Feeling tense or keyed up”, “Suddenly scared for no reason”, “Feeling blue”). In Norwegian primary care institutions, the HSCL-10 is used as a valid instrument for screening and identifying depression in adolescents aged 14–16 years [15].
Somatic symptoms
At all three time points, a brief version of the Children's Somatic Symptoms Inventory (CSSI) [16,17] was used to assess self-reported somatic symptoms. Items with adequate statistical properties from the validation study were selected in collaboration with the authors of the CSSI-24 [16]. The scale includes eight items covering stomach pain, headache, back pain, arm or leg pain, faintness or dizziness, rapid heartbeat, nausea, and fatigue. All items are presented on a four-point scale ranging from 0 (not bothered) to 3 (very much bothered). A mean score was calculated when at least 50% of the items had a valid response and internal consistency for the scale was .827.
Pandemic-related worries
With a set of eight questions modified from the Pandemic Anxiety Scale, we inquired about specific concerns about the pandemic and possible consequences at T2 and T3 [18]. Each item was rated on a 5-point Likert scale ranging from 0 (Strongly disagree) to 4 (Strongly agree).
Loneliness
Adolescents' self-reported loneliness over the previous two weeks was mapped using the University of California at Los Angeles loneliness scale short form with three items at T2 and T3 assessments [19,20]. The three-item University of California at Los Angeles version has been shown in large-scale studies to be accurate in measuring loneliness and is related to objective self-isolation [20]. The questions were rated on a three-point scale ranging from 1 (Never) to 3 (Always) and a composite mean score was calculated for the three items.
Procedures
The UEVO study (Norwegian Youth Survey on Child Maltreatment) [14] included 70 schools of which subsamples accepted invitations to participate in T2 and T3. Schools were approached and asked to administer the web-based survey to their entire student body, grades 8 through 10. The survey was administered during school hours by the schools that agreed to participate. The web-based survey took approximately 40 minutes at T1, 15 minutes at T2, and 30 minutes at T3 to complete after watching a short animated video about the study and the ethical principles of voluntary participation, confidentiality, and the right to withdraw at any time during the study without having to give a reason. Students completed the survey in class using a personal computer, tablet, or cell phone.
Ethics
The study protocol was approved by the Regional committee for ethics in medical and health research in the Southeastern region of Norway (Case #2018/522). All participants gave an informed written consent and the adolescents did not need parental permission to participate, in accordance with the Act on Medical and Health Research in Norway, §17 (please see the study cohort profile for a more elaborate description of this regulation which allows for independent consent for adolescents aged more than 12 years [14]).
Data analyses
Descriptive statistics for background variables and key outcome variables are presented as percentages, means, and standard deviations. The sample characteristics are presented for all participants who participated at each time point and for participants who participated at all three time points (the longitudinal sample).
To assess the potential impact of the pandemic and lockdown, we ran two mixed-effects models, estimating change and predictors of change in (1) anxiety and depression symptoms and (2) somatic health complaints. Time was treated as a categorical variable with three levels in the mixed-effects models. The models included a number of background variables with an emphasis on their importance for change in the dependent variables, and thus only variables most likely present prior to the first assessment (T1) were included so that the temporal interaction was not hampered. These were gender, low family affluence, family ethnic minority status, and a history of violence exposure. Because mental health problems increase with age throughout adolescence, we controlled for age in the models.
The mixed effects models permitted the use of all observed data regardless of whether individuals had observations at all time points. A positive time coefficient from the mixed-effects model indicates worsening in mental health problems or somatic health complaints associated with the pandemic. To investigate heterogeneity in the effect of the pandemic, interactions between time (before to during the pandemic) and the five risk variables were fitted. In general, missing data in outcome variables were handled by applying the half rule, that is, only participants with valid observations on at least half of the items were included in the scale scores. Under the less restrictive missing at random assumption, mixed-effects models provide valid inference with missing data in the dependent variable.
In the final step, variables predicting levels of mental health problems and somatic health complaints at T3 were analyzed. Two hierarchical multiple regression analyses are presented, investigating variables predicting mental health problems and somatic health complaints, respectively, one year into the pandemic (T3). The dependent variable's distribution was investigated, and to account for non-normality in variables, both regression models were bootstrapped with 1,000 replications, yielding confidence intervals for estimates that did not rely on specific distributional assumptions.
Descriptive statistics and linear regression models were conducted in SPSS version 26 (IBM Corp, released in 2019), while mixed-effects models were run using the lnme (linear and nonlinear mixed effects models) package in R (R Core Team, 2020).
Results
Table 1 provides an overview of sample characteristics. The first three columns describe the samples included at each of the data collection points (T1, T2, and T3), whereas the fourth column describes the sample of adolescents with valid data at all three time points. Gender distribution is similar across all time points, as is the distribution of adolescents living in single-parent households, minority families, and in families with high/low family affluence.
Changes in mental and somatic health complaints over time
We fitted two mixed-effects models, one for anxiety and depression and one for somatic health complaints, one year before the pandemic (2019), three months into the first outbreak (2020), and one year later (2021) to investigate the evolution of mental and somatic health complaints over time. Table 2 shows the parameter estimates for the fixed and random effects. The basic model estimating the change in mental health problems in the total sample showed a nonlinear development over time, reflecting a flat trend from 2019 to 2020, followed by an increase in symptoms from 2020 to 2021 (Predicted value at T1 .56 [95% CI .55,0.58], T1-T2 difference −.04 [95% CI −.07,−.02], T2-T3 difference .12 [95% CI .09,0.14]). As shown in Table 2, Model 1 with covariates assessed at T1 in 2019 (gender, age, family affluence, country of origin, single-parent household, and a history of violence exposure) revealed that, while all covariates were associated with significantly higher levels of anxiety and depression one year prior to the pandemic, girls had a significantly larger increase in mental health symptoms before the pandemic and throughout the period compared to boys.
Table 2.
Mixed effects model predicting change in anxiety depression (Model 1) and somatic health complaints (Model 2) from pre to early and late pandemic
| Model 1. Anxiety and depression |
T2 |
T3 |
||||
|---|---|---|---|---|---|---|
| Interactions with time | Est. | 95% CI | P value | Est. | 95% CI | P value |
| Gender (ref· boy) | −.11 | −.21, 0.01 | <.001 | −.17 | −.25, −.09 | <.001 |
| Family affluence (ref·low) | −.08 | −.49, 0.33 | .69 | .06 | −.20, 0.32 | .66 |
| Living in the capital area of Norway | .01 | −.10, 0.12 | .85 | .04 | −.09, 0.12 | .40 |
| Parents' country of origin (ref·Nordic) | −.00 | −.13, 0.13 | .97 | .00 | −.01, 0.10 | .94 |
| Single-parent household | .09 | −.03, 0.21 | .15 | .09 | −.01, 0.18 | .07 |
| Prior abuse exposure |
−.05 |
−.11, 0.00 |
.06 |
−.59 |
−.10, 0.02 |
.08 |
| Model 2. Somatic health complaints | T2 | T3 | ||||
| Interactions with time | Est. | 95% CI | P value | Est. | 95% CI | P value |
| Gender (ref· boy) | −.16 | −.27, −.04 | <.01 | −.23 | −.32, −.13 | <.001 |
| Family affluence (ref· low) | −.00 | −.45, 0.45 | .99 | −.07 | −.36, 0.22 | .61 |
| Living in the capital area of Norway | −.01 | −.13, 0.11 | .86 | .01 | −.10, 0.08 | .80 |
| Parents' country of origin (ref Nordic) | −.08 | −.07, 0.22 | .28 | .05 | −.07, 0.16 | .41 |
| Single-parent household | .06 | −.07, 0.19 | .36 | .04 | −.06, 0.14 | .43 |
| Prior abuse exposure | −.04 | −.10, 0.02 | .14 | −.05 | −.10, −.00 | .03 |
A strikingly similar trend was observed for somatic health complaints throughout the pandemic. The basic model, which estimated the change in somatic health complaints in the total sample while controlling for an increase in age, also revealed a flat trend from 2019 to 2020, followed by an increasing trajectory of somatic health complaints from 2020 to 2021 (Predicted value at T1 .59 [95% CI .58, .61], T1-T2 slope −.09 [95% CI −.11, −.65], T2-T3 slope .18 [95% CI .15, .21]). As shown in Table 2, Model 2 with covariates assessed at T1 in 2019 revealed that girls experienced a significantly greater increase in somatic health complaints from prior to the pandemic and throughout the period than boys.
Predicting mental and somatic health complaints one year into the pandemic
Tables 3 and 4 show the results of two multiple hierarchical regression models that predict mental and somatic complaints at T3. As per model 3 (Table 4), prepandemic mental health problems, female gender, living in a single-parent household, and abuse exposure significantly predicted higher mental health scores at T3, even when pandemic-related risk factors were controlled for at T2 (model 2) and T3 (model 3). Furthermore, loneliness at T2 was associated with higher mean scores on HSCL at T3. Pandemic-related worries, on the other hand, were inversely related to mean scores on HSCL at T3, indicating that higher pandemic-related worries at T2 predicted lower scores on HSCL at T3. Loneliness at T3 was also significantly related to mean scores on HSCL at T3 when controlling for concurrent and prepandemic risk factors (model 3). As shown in Table 4, we found somewhat similar results for somatic health complaints one year into the pandemic, except that living in a single-parent household and having pandemic-related worries assessed at T2 or T3 did not significantly predict scores on CSSI at T3. The models explained 40% of the variance in anxiety depression at T3 and 33% of the variance in somatic health complaints at T3.
Table 3.
Linear regression model predicting the level of mental health complaints one year into the pandemic
| Variables | Model 1 |
Model 2 |
Model 3 |
|||
|---|---|---|---|---|---|---|
| B (95% CI) | P value | B (95% CI) | P value | B (95% CI) | P value | |
| T1 variables | ||||||
| HSCL | .41 (.29, .53) | <.001 | .29 (.18, .40) | <.001 | .27 (.16, .37) | <.001 |
| Male gender | −.29 (−.40, −.19) | <.001 | −.29 (−.39, −.18) | <.001 | −.24 (−.35, −.14) | <.001 |
| Family affluence | −.35 (−.79, .09) | .121 | −.38 (−.80, .03) | .071 | −.36 (−.75, .03) | .070 |
| Non-Nordic country of origin | .01 (−.12, .15) | .833 | .03 (−.09, .16) | .600 | .03 (−.09, .15) | .638 |
| Single-parent household | .13 (.01, .26) | .032 | .14 (.02, .26) | .020 | .12 (.01, .23) | .039 |
| Abuse exposure (lifetime) | .12 (.05, .18) | .000 | .12 (.06, .18) | <.001 | .09 (.03, .15) | .002 |
| T2 variables | ||||||
| Loneliness | .36 (.26, .47) | <.001 | .18 (.07, .28) | .001 | ||
| Pandemic-related worries | −.09 (−.16, −.02) | .014 | −.08 (−.17, −.00) | .045 | ||
| Parents' pandemic-related job loss | −.05 (−.12, .03) | .216 | −.02 (−.10, −.05) | .496 | ||
| T3 variables | ||||||
| Loneliness | .38 (.28, .48) | <.001 | ||||
| Pandemic-related worries | .02 (−.07, .11) | .689 | ||||
| Parents' pandemic-related job loss | −.04 (−.12, .04) | .306 | ||||
| R2 = .24 | R2 = .33 | R2 = .40 | ||||
Table 4.
Linear regression model predicting the level of somatic complaints one year into the pandemic
| Variables | Model 1 |
Model 2 |
Model 3 |
|||
|---|---|---|---|---|---|---|
| B (95% CI) | P value | B (95% CI) | P value | B (95% CI) | P value | |
| T1 variables | ||||||
| CSSI | .55 (.43, .68) | <.001 | .53 (.41, .65) | <.001 | .50 (.38, .62) | <.001 |
| Male gender | −.30 (−.42, −.18) | <.001 | −.30 (−.42, −.18) | <.001 | −.30 (−.42, −.18) | <.001 |
| Family affluence | −.11 (−.60, .37) | .655 | −.13 (−.60, .34) | .587 | −.16 (−.62, .31) | .511 |
| Non-Nordic country of origin | −.00 (−.15, .15) | .994 | .01 (−.13, .16) | .843 | .00 (−.14, .14) | .998 |
| Single-parent household | .11 (−.03, .27) | .121 | .10 (−.03, .24) | .132 | .10 (−.03, .23) | .138 |
| Abuse exposure (lifetime) | .10 (.03, .17) | .005 | .09 (.02, .14) | .008 | .08 (.01, .15) | .018 |
| T2 variables | ||||||
| Loneliness | .23 (.11, .34) | <.001 | .11 (−.01, .23) | .083 | ||
| Pandemic-related worries | −.10 (−.19, −.01) | .021 | −.03 (−.13, .07) | .546 | ||
| Parents' pandemic-related job loss | .04 (−.04, .13) | .325 | .07 (−.02, .15) | .131 | ||
| T3 variables | ||||||
| Loneliness | .25 (.13, .37) | <.001 | ||||
| Pandemic-related worries | −.10 (−.20, .00) | .058 | ||||
| Parents' pandemic-related job loss | −.05 (−.14, .05) | .355 | ||||
| R2 = .26 | R2 = .30 | R2 = .33 | ||||
| Δ R2 = .04 | Δ R2 = .03 | |||||
Discussion
Using a nationwide prospective longitudinal study of Norwegian adolescents from before to during the pandemic, we investigated multiple aspects of adolescent self-reported mental and somatic health complaints. We discovered that one year (15 months) into the pandemic, after an initial stable trend from before the pandemic to the early phase of the pandemic, both mental and somatic health complaints increased. The increase in symptoms from June 2020 to June 2021 was significant both for mental and somatic health complaints. Girls appeared to be disproportionately affected during this time period, as evidenced by a significantly higher increase in both mental and somatic health complaints when compared to boys. Loneliness in the early stages of the pandemic was a significant contributing factor to higher levels of health complaints one year into the pandemic, both for mental and somatic complaints. Prior abuse exposure and living in a single-parent household prior to the pandemic outbreak were also associated with elevated symptoms of mental health problems. A history of abuse was also linked to an increase in somatic health complaints. However, and contrary to expectations, pandemic-related concerns were found to be inversely related to symptoms of mental health problems.
The observed increase in anxiety and depression and in somatic complaints, one year into the pandemic, highlights the concern that prolonged and repeated measures may have had a negative impact on the adolescent population in terms of an increased risk for both mental and somatic health complaints [8]. So far, findings from Norway and other developed countries on changes in symptoms of mental and somatic health have been inconclusive, and few studies have looked at changes in symptoms over a longer period of time. Our findings suggest that if we continue to implement frequent and consistent measures to combat the spread of the COVID-19 virus, we may expect an increase in symptoms of mental and somatic health complaints among adolescents.
In line with previous research on mental and somatic health during the COVID-19 pandemic [13], we discovered that adolescent girls had a relatively greater increase in symptoms of both mental and somatic health complaints than boys. In addition to having more symptoms at the start, girls showed a trend throughout the pandemic that was characterized by a significant worsening of mental and somatic health symptoms when compared to boys. Furthermore, greater changes in loneliness for girls compared to boys during the pandemic may explain a relatively increased risk for internalizing symptoms. As a result, we can speculate that adolescent girls' mental and somatic well-being may be more dependent on social activities that are restricted during lock down than boys. Systematic reviews and meta-analytic findings suggest that adolescent girls may be especially vulnerable to anxiety and depression during the pandemic [6,21]. On an important note, we assessed symptomatology, which is more commonly reported by girls. Boys, on the other hand, may be more prone to externalizing psychopathology, which we did not examine in this study.
As per our findings after the first wave of the pandemic, children in single-parent households experienced an increase in mental health symptoms. Surprisingly, our findings suggest that pandemic-related worries during the first part of the pandemic may have been protective for some in terms of reduced mental health problems one year later. However, other factors such as mandatory closure of schools may also explain why some experienced reduction in symptoms. In line with this, increased anxiety during the pandemic has been found to promote protective behaviors [22].
In the present study, increased loneliness during the first year of the pandemic was strongly related to elevated symptoms of both mental and somatic complaints. The cross-sectional and longitudinal association between loneliness and mental health problems in adolescents is well established in the literature [23] and the relationship between loneliness and mental health problems is most likely bidirectional [24]. However, in line with a recent meta-analysis of 80 studies on loneliness in adolescents, we discovered that loneliness was associated with subsequent anxiety and depression [23]. Our findings add to previous research by demonstrating that initial high levels of loneliness are predictors of correspondingly high levels of internalizing symptoms, both in terms of mental and somatic health complaints.
Strengths and limitations
The sample's representativeness and the prospective design that allows us to compare adolescents' mental and somatic health complaints before and during the COVID-19 pandemic (June 2020 and 2021) are clear strengths of this study.
There is a myriad of factors that could possibly influence the wellbeing of adolescents during a pandemic, and we have only captured some of these in the present study. As we could not reliably assess the degree of restrictive measures in each of the regions in which the participating adolescents live, we cannot conclude firmly about the impact of the restrictions on adolescents' health. It must also be noted that restrictive measures such as mandatory closure of all schools also bring changes in academic pressure, which again, could increase well-being for some students.
School-based surveys, such as this one, frequently fail to include more marginalized groups, such as adolescents with psychosocial problems, adolescents from less affluent or less educated backgrounds, and adolescents who drop out of school. As a result, there is always the risk that findings will underestimate the difficulties faced by the entire population. Attrition analyses revealed that while the sample that participated in all measurements was overall comparable to those who dropped out, participants with higher symptoms of mental health problems and somatic complaints at T1 dropped out at T2 and T3. As a result, we may have underestimated the pandemic's impact on these measures.
Finally, we do acknowledge that there may be regional and cultural differences in how societies have been able to care for their individuals during the pandemic. This could influence the degree to which individuals are impacted by the situation and may compromise the generalizability of the findings. Norway, as most of the countries in the Nordic region, is characterized by a strong public school, health, and welfare system. However, like most other countries, the capacity of these resources was also challenged during the pandemic. During 2021 primary healthcare consultations increased by 38.5% for adolescents aged 13–15 years in Norway, compared to the year before [24]. The increase was highest for anxiety and depression, with a 52% increase in 2021 [24]. Although it is not clear how the social and cultural context impacts the health status of the youth population during such a health-related crisis, knowledge about these contextual factors is pivotal in the findings and comparing these to research from other parts of the world.
Implications and conclusion
Although the trend of increasing mental and somatic health complaints in adolescents is small, it is concerning because it shows a clear acceleration over the last year, and thus suggests that the prolonged situation of the ongoing pandemic and the related restrictions have taken a toll on the adolescent population. Continuous monitoring of symptoms in representative and diverse samples of adolescents must be prioritized to obtain a knowledge-based ground for developing youth mental health interventions. Efforts should be made to reach out to the general youth population with interventions aimed at reducing loneliness and enhancing social relationships in times of crises. Adolescent pandemic mitigation measures must be kept to a bare minimum.
Acknowledgments
We would like to thank Carina Schjem Grimsgaard, Anine Forsberg, and Linn Eirin Aronsen Haugen from our data collection team. The Norwegian Directorate for Children, Adolescents, and Family Matters (Bufdir) funded the research. The funding source played no role in study design, data collection, analysis, and interpretation, manuscript writing, or decision to submit the article for publication.
G.S.H. and E.M.A. designed the study, were responsible for the acquisition of funding, and were in charge of data collection. G.S.H., T.W.L., and S.S.S. carried out all data analyses and produced the tables. S.S.S. conducted and summarized the systematic literature search and conducted the attrition analyses. G.S.H. wrote the first draft of the manuscript and all authors commented on and edited the final version.
Footnotes
Conflicts of interest: The authors have no conflicts of interest to declare.
Data sharing: The dataset is administrated by the Norwegian Centre for Violence and Traumatic Stress Studies. Approval from a Norwegian regional committee for medical and health research ethics (https://helseforskning.etikkom.no) is a prerequirement. Guidelines for access to the data are found at the longitudinal cohort website uevo.nkvts.no.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jadohealth.2022.05.009.
Supplementary Data
References
- 1.Brooks S.K., Webster R.K., Smith L.E., et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holmes E.A., O’Connor R.C., Perry V.H., et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hafstad G.S., Augusti E.-M. A lost generation? COVID-19 and adolescent mental health. Lancet Psychiatry. 2021;8:640–641. doi: 10.1016/S2215-0366(21)00179-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Girolamo G., Dagani J., Purcell R., et al. Age of onset of mental disorders and use of mental health services: Needs, opportunities and obstacles. Epidemiol Psychiatr Sci. 2012;21:47. doi: 10.1017/s2045796011000746. [DOI] [PubMed] [Google Scholar]
- 5.Blomqvist I., Henje Blom E., Hägglöf B., et al. Increase of internalized mental health symptoms among adolescents during the last three decades. Eur J Public Health. 2019;29:925–931. doi: 10.1093/eurpub/ckz028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Racine N., McArthur B.A., Cooke J.E., et al. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: A meta-analysis. JAMA Pediatr. 2021;175:1142–1150. doi: 10.1001/jamapediatrics.2021.2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu S., Liu Y., Liu Y. Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: A cross-sectional survey. Psychiatry Res. 2020;289:113070. doi: 10.1016/j.psychres.2020.113070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zijlmans J., Teela L., van Ewijk H., et al. Mental and social health of children and adolescents with pre-existing mental or somatic problems during the COVID-19 pandemic lockdown. Front Psychiatry. 2021;12:692853. doi: 10.3389/fpsyt.2021.692853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hafstad G.S., Sætren S.S., Wentzel-Larsen T., et al. Adolescents’ symptoms of anxiety and depression before and during the Covid-19 outbreak–A prospective population-based study of teenagers in Norway. Lancet Reg Health-Europe. 2021;5:100093. doi: 10.1016/j.lanepe.2021.100093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andreas J.B., Brunborg G.S. Self-reported mental and physical health among Norwegian adolescents before and during the COVID-19 pandemic. JAMA Netw open. 2021;4 doi: 10.1001/jamanetworkopen.2021.21934. e2121934-e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vaillancourt T., Brittain H., Krygsman A., et al. Assessing the quality of research examining change in children’s mental health in the context of COVID-19. UOJM. 2021;11 doi: 10.18192/uojm.v11i1.5950. [DOI] [Google Scholar]
- 12.Creswell C., Shum A., Pearcey S., et al. Young people's mental health during the COVID-19 pandemic. Lancet Child Adolesc Health. 2021;5:535–537. doi: 10.1016/S2352-4642(21)00177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thorisdottir I.E., Asgeirsdottir B.B., Kristjansson A.L., et al. Depressive symptoms, mental well-being and substance abuse among adolescents before andduring the COVID-19 pandemic in Iceland: A longitudinal analysis. Lancet Psychiatry. 2021;8:663–672. doi: 10.1016/S2215-0366(21)00156-5. [DOI] [PubMed] [Google Scholar]
- 14.Hafstad G.S., Sætren S.S., Myhre M.C., et al. Cohort profile: Norwegian youth study on child maltreatment (the UEVO study) BMJ open. 2020;10:e038655. doi: 10.1136/bmjopen-2020-038655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haavet O.R., Sirpal M.K., Haugen W., et al. Diagnosis of depressed young people in primary health care—a validation of HSCL-10. Fam Pract. 2010;28:233–237. doi: 10.1093/fampra/cmq078. [DOI] [PubMed] [Google Scholar]
- 16.Walker L.S., Beck J.E., Garber J., et al. Children's somatization inventory: Psychometric properties of the revised form (CSI-24) J Pediatr Psychol. 2009;34:430–440. doi: 10.1093/jpepsy/jsn093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stone A.L., Walker L.S., Heathcote L.C., et al. Somatic symptoms in pediatric patients with chronic pain: Proposed clinical reference points for the children’s somatic symptoms inventory (formerly the children’s somatization inventory) J Pain. 2019;20:932–940. doi: 10.1016/j.jpain.2019.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McElroy E., Patalay P., Moltrecht B., et al. Demographic and health factors associated with pandemic anxiety in the context of COVID-19. Br J Health Psychol. 2020;25:934–944. doi: 10.1111/bjhp.12470. [DOI] [PubMed] [Google Scholar]
- 19.Hays R.D., DiMatteo M.R. A short-form measure of loneliness. J Personal Assess. 1987;51:69–81. doi: 10.1207/s15327752jpa5101_6. [DOI] [PubMed] [Google Scholar]
- 20.Hughes M.E., Waite L.J., Hawkley L.C., et al. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Res Aging. 2004;26:655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ma L., Mazidi M., Li K., et al. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: A systematic review and meta-analysis. J Affective Disord. 2021;293:78–79. doi: 10.1016/j.jad.2021.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salali G.D., Uysal M.S., Bevan A. Adaptive function and correlates of anxiety during a pandemic. Evol Med Public Health. 2021;9:393–405. doi: 10.1093/emph/eoab037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Loades M.E., Chatburn E., Higson-Sweeney N., et al. Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59:1218–1239.e3. doi: 10.1016/j.jaac.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Evensen M., Hart R.K., Godoy A.A., et al. Impact of the COVID-19 pandemic on mental healthcare consultations among children and adolescents in Norway: A nationwide registry study. Preprint: medRxiv. 2021 doi: 10.1101/2021.10.07.21264549. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.