Abstract
Rationale & Objective
Children with kidney disease and primary hypertension may be more vulnerable to COVID-19. We examined COVID-19 vaccine hesitancy among parents of children with chronic kidney disease or hypertension.
Study Design
Sequential explanatory mixed-methods design; survey followed by in-depth interviews.
Setting & Participants
Parents of children aged <18 years with kidney disease or primary hypertension within a large pediatric practice.
Exposure
Parental attitudes toward general childhood and influenza vaccines assessed by the Vaccine Hesitancy Scale. Kidney disease classification, demographic and socioeconomic factors, experiences with COVID-19, COVID-19 mitigation activities and self-efficacy, and sources of vaccine information.
Outcome
Willingness to vaccinate child against COVID-19.
Analytical Approach
Analysis of variance (ANOVA) test to compare parental attitudes toward general childhood and influenza vaccination with attitudes toward COVID-19 vaccination. Multinomial logistic regression to assess predictors of willingness to vaccinate against COVID-19. Thematic analysis of interview data to characterize influences on parental attitudes.
Results
Of the participants, 207 parents completed the survey (39% of approached): 75 (36%) were willing, 80 (39%) unsure, and 52 (25%) unwilling to vaccinate their child against COVID-19. Hesitancy toward general childhood and influenza vaccines was highest among the unwilling group (P < 0.001). More highly educated parents more likely to be willing to vaccinate their children, while Black race was associated with being more likely to be unwilling. Rushed COVID-19 vaccine development as well as fear of serious and unknown long-term side effects were themes that differed across the parental groups that were willing, unsure, or unwilling to vaccinate their children. Although doctors and health care teams are trusted sources of vaccine information, perceptions of benefit versus harm and experiences with doctors differed among these 3 groups. The need for additional information on COVID-19 vaccines was greatest among those unwilling or unsure about vaccinating.
Limitations
Generalizability may be limited.
Conclusions
Two-thirds of parents of children with kidney disease or hypertension were unsure or unwilling to vaccinate their child against COVID-19. Higher hesitancy toward routine childhood and influenza vaccination was associated with hesitancy toward COVID-19 vaccines. Enhanced communication of vaccine information relevant to kidney patients in an accessible manner should be examined as a means to reduce vaccine hesitancy.
Plain-Language Summary
Children with kidney disease or hypertension may do worse with COVID-19. As there are now effective vaccines to protect children from COVID-19, we wanted to find out what parents think about COVID-19 vaccines and what influences their attitudes. We surveyed and then interviewed parents of children who had received a kidney transplant, were receiving maintenance dialysis, had chronic kidney disease, or had hypertension. We found that two-thirds of parents were hesitant to vaccinate their children. Their reasons varied, but the key issues included the need for information pertinent to their child and a consistent message from doctors and other health care providers. These findings may inform an effective vaccine campaign to protect children with kidney disease and hypertension.
Index Words: Child, coronavirus disease 2019 (COVID-19), COVID-19 vaccine hesitancy, hypertension, immunization, influenza vaccines, kidney diseases, qualitative research, glomerular diseases, vaccination, vaccination hesitancy
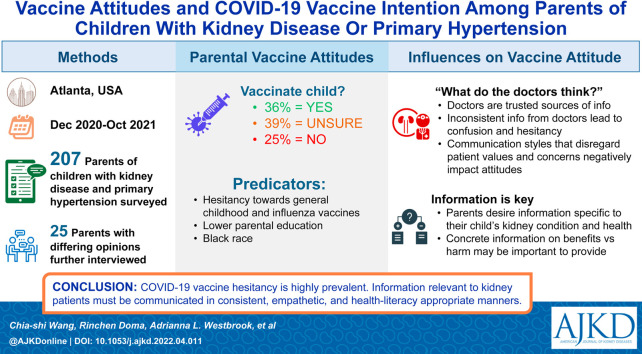
Graphical abstract
Editorial, p. 13
Vaccine hesitancy, defined as “delay in acceptance or refusal of vaccines despite availability of vaccination services,” is a major obstacle in utilizing effective vaccines to mitigate the devastating impact of the global COVID-19 pandemic.1 A COVID-19 vaccine was given Emergency Use Authorization (EUA) by the US Food and Drug Administration (FDA) for children and adolescents ages 12-15 years in May 2021 and for children ages 5-11 years in November 2021. Yet just 52.5% of 12- to 17-year-olds and 11.3% of 5- to 11-year-olds had been fully vaccinated as of December 16, 2021.2 In a national survey conducted in October 2021, 30% of parents with children 5-11 years old said they would “definitely not” vaccinate their child.3 Understanding parental attitudes toward COVID-19 vaccines is critical, particularly for at-risk children.
Approximately 0.5% of children in the United States have chronic kidney disease (CKD).4 Children with CKD, including those with kidney transplants and those receiving maintenance dialysis, have increased infection-related morbidity and mortality.5 The risk of severe COVID-19 complications and death is significantly higher among adult kidney patients.6, 7, 8 Data on COVID-19 in children with CKD are limited, though they may also have increased vulnerability to infection and severe disease due to direct CKD effects, use of immunosuppressive medications among those with kidney transplants and glomerular diseases, comorbid conditions such as hypertension and diabetes, and unavoidable health care facility exposures (eg, hemodialysis).9 , 10 Children with CKD make up 1.7% of pediatric COVID-19 hospitalizations, though CKD prevalence in the United States is much lower.11 A study of 1,000 children with COVID-19 found that kidney disease was among the strongest predictors of hospitalization.12 Hence, an effective COVID-19 vaccine strategy that addresses vaccine hesitancy in this vulnerable population is particularly important.
Vaccine hesitancy is complex and ranges from acceptance of some vaccines, to uncertainty and delays in vaccination, to complete refusal of all vaccines.13 It is context-specific and influenced by wide-ranging factors such as perceived risks of disease; vaccine accessibility; and trust in the effectiveness and safety of vaccines, the health system, and the motivations of the policy-makers.14 The P3 (Practice, Provider, and Patient Level) model provides a comprehensive framework for examining and addressing vaccine hesitancy factors that are specifically relevant to vaccine promotion within health care settings.15 Here, we report vaccine attitudes among parents of children with kidney disease or primary hypertension, clinical and socioeconomic characteristics associated with higher vaccine hesitancy, and an in-depth analysis of influences on COVID-19 vaccine attitudes following the P3 model framework. Our goals are to understand the scope of vaccine hesitancy, identify subgroups who may benefit from targeted interventions, and identify underlying factors influencing attitudes to inform future pragmatic COVID-19 vaccine promotion for pediatric patients with kidney disease.
Methods
Overview of Study
We used a sequential explanatory mixed-method design with (1) a survey on vaccine attitudes of parents (or legal guardians) of children younger than 18 years with kidney disease or primary hypertension (referred to simply as “hypertension” in the remainder of this article), followed by (2) an in-depth interview of select survey participants based on their responses to gain deeper understanding of the influences on vaccine attitudes. The study took place between December 2020 and October 2021, inclusive of key regulatory approval time points for the COVID-19 vaccine for children in the United States: December 2020 for those aged ≥16 years and May 2021 for those aged ≥12 years. The study period preceded the EUA approval in November 2021 for those aged ≥5 years. Ethical approval was received from the Emory University Institutional Review Board (00001594).
Survey
Participants and Sample Size
Parents or legal guardians of children younger than 18 years with kidney transplant, with kidney failure treated by dialysis, or with CKD or hypertension cared for by Children’s Healthcare of Atlanta (CHOA) were included. We excluded adults unable to provide consent and those unable to read or understand the survey in English. The sample size target was 25% of each of the patient subgroups seen during the study period: transplant, dialysis, and CKD, and hypertension. The total target sample size was 200. Only 1 parent/guardian responded per child. Informed consent was obtained.
Survey Design
The survey contained 2 main sections. Section 1 examined parental intent to vaccinate their child for COVID-19. Participants responded to the question, “If a vaccine against COVID-19 were to become available, are you willing to vaccinate your child who has kidney disease?” with response choices of “yes,” “no,” and “unsure.” The same item was repeated for vaccinating oneself and other children (if any) without kidney disease. We examined attitudes toward general childhood and influenza vaccines using the modified Vaccine Hesitancy Scale (VHS).16 Additional descriptions are found in Item S1.
Section 2 of the survey examined potential predictors of vaccine hesitancy, with items created to address constructs outlined by the P3 model that are relevant to vaccine promotion within health care settings: health care delivery, situational, cues to action, preventative activity features, and predisposing and enabling factors (Item S1).15
Survey Administration
Patients with scheduled visits at CHOA were screened for eligibility. Based on research staff availability, eligible participants were approached in person during the clinic appointments across all clinics. Potential participants who verbally consented to participate were emailed links to the informed consent form and the survey to minimize face-to-face exposure between study staff and patient families. To reduce crowding at the dialysis center, parents of children on dialysis were approached via phone. Those who indicated interest were also emailed the consent and survey links.
Survey Analysis
Willingness to receive the COVID-19 vaccine
We described the proportion of survey participants who answered “no,” “unsure,” or “yes” to vaccinate their child with kidney disease against COVID-19. Agreement with responses to receiving a COVID-19 vaccine for self or other children without kidney disease (if any) were assessed using Cohen’s κ statistic and 95% CI.
Parental attitudes toward general childhood and influenza vaccine
The modified VHS scale uses a 4-item Likert scale: (5) strongly disagree, (4) somewhat disagree, (2) somewhat agree, and (1) strongly agree. The answers were averaged to provide a score for parental attitudes toward general childhood and influenza vaccines. A higher score indicates higher vaccine hesitancy.16 Mean and SD VHS scores were calculated for all participants and for participants who answered “no,” “unsure,” or “yes” to the COVID-19 vaccine for their child with kidney disease. Differences among the 3 groups were examined via analysis of variance (ANOVA) tests.
Predictors of willingness to vaccinate child with kidney disease or hypertension against COVID-19
Participant characteristics, inclusive of child’s kidney disease classification and responses to section 2 of the survey, were described by willingness to vaccinate a child. Responses to the self-efficacy scale and the financial and psychological impact scale were averaged for scoring. Information sources for vaccines were summarized into latent classes using latent component analysis for both from whom (primary care doctor, kidney doctor, other doctors, government, scientists, family and friends, celebrities) and where (physicians’ offices, websites, newspaper/magazines, TV, social media) participants received COVID vaccine information. All variables were examined for associations with willingness to vaccinate using χ2 or Fisher test and Kruskal-Wallis rank sum tests. Variables significant at the 0.10 α level in bivariate analysis were examined in multivariable analysis using multinomial logistic regression. Variables with variance inflation factor above 5 were removed until the maximum number of variables could be retained while also retaining the child’s kidney disease classification. Significance level was set to 0.05. Statistical analyses were performed using R Statistical Software (version 2.14.0; R Foundation for Statistical Computing).
Interview
Participants
Among the survey participants who consented to an in-depth interview, we selectively invited participants to reach a target of 5 interviews from each of the transplant, dialysis, and CKD and hypertension subgroups. We also targeted at least 5 participants unwilling and 5 willing to vaccinate their child against COVID-19. We performed additional in-depth interviews until data saturation was reached (ie, no new themes arose).17
Interview Guide and Data Collection
An interview guide based on impacting factors on preventative health behavioral adoption as described by the P3 model was created.15 Three trained qualitative researchers without any prior contacts with the participants conducted the semistructured in-depth interviews via video conferencing. All in-depth interviews were recorded with participant consent.
Interview Analysis
C.-s.W., R.D., and J.J. completed several rounds of close reading of the transcripts to highlight key concepts and developed and refined a codebook containing both deductive codes following the P3 model as well as inductive codes. The transcripts were loaded into the analysis software NVivo (released March 2020; QSR International) and were independently coded by at least 2 coders. A third coder resolved any coding discrepancies. The transcripts were analyzed by C.-s.W., R.D., J.J., and A.K.-F. using thematic analysis with particular focus on concepts that are informative to promote COVID-19 vaccines for pediatric patients with kidney disease in health care settings. Concepts were compared within and across interviews stratified by willingness to vaccinate child with kidney disease against COVID-19.18 C.-s.W. grouped similar concepts into themes, which were discussed among all investigators for interpretation.
Results
Survey Findings
Participants
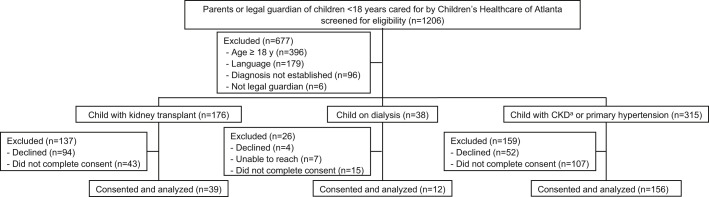
A total of 207 surveys (39% of eligible approached parents) were completed, representing 22% (39 of 176) of approached kidney transplant patients, 32% (12 of 38) of approached dialysis patients, and 50% (156 of 315) of approached CKD (non–kidney failure) or hypertension patients (Fig 1 ). The participant characteristics are given in Table 1 .
Figure 1.
Survey participants on COVID-19 vaccine attitudes for children and adolescents with kidney disease or primary hypertension. aKidney disease due to congenital anomalies of kidney and urinary tract, glomerular disease, cystic/hereditary/congenital disease (C/H/C), or others not include those on dialysis or with a kidney transplant. Abbreviation: CKD, chronic kidney disease.
Table 1.
Characteristics of Survey Participants and Their Child With Kidney Disease or Primary Hypertension, Stratified by Willingness to Vaccinate Child Against COVID-19
| Willingness to Vaccinate Child (N = 207) |
P | |||
|---|---|---|---|---|
| Yes (n = 75) | Unsure (n = 80) | No (n = 52) | ||
| Caregiver Characteristics | ||||
| Race | 0.3 | |||
| White | 42 (56%) | 38 (48%) | 21 (40%) | |
| Black | 22 (29%) | 27 (34%) | 23 (44%) | |
| Other | 11 (15%) | 11 (14%) | 4 (8%) | |
| Declined to respond | 0 | 4 (5%) | 4 (8%) | |
| Ethnicity | 0.6 | |||
| Non-Hispanic | 66 (88%) | 69 (86%) | 45 (87%) | |
| Hispanic | 8 (11%) | 11 (14%) | 4 (8%) | |
| Declined to respond | 1 (1%) | 0 | 3 (6%) | |
| Sex | 0.3 | |||
| Male | 12 (16%) | 9 (11%) | 11 (21%) | |
| Female | 63 (84%) | 69 (86%) | 40 (77%) | |
| Declined to respond | 0 | 2 (3%) | 1 (2%) | |
| Primary language | 0.8 | |||
| English | 68 (91%) | 74 (92%) | 49 (94%) | |
| Other | 7 (9%) | 6 (8%) | 3 (6%) | |
| Insurance type | 0.03 | |||
| Private | 55 (73%) | 43 (54%) | 26 (50%) | |
| Public | 16 (21%) | 23 (29%) | 17 (33%) | |
| No insurance/declined to respond | 4 (5%) | 14 (18%) | 9 (17%) | |
| Education level | 0.01 | |||
| High school or less | 10 (13%) | 21 (26%) | 18 (35%) | |
| Some college | 19 (25%) | 20 (25%) | 17 (33%) | |
| College graduate or higher | 46 (61%) | 38 (48%) | 16 (31%) | |
| Declined to respond | 0 | 1 (1%) | 1 (2%) | |
| Employment | 0.3 | |||
| Unemployed or currently not working | 11 (15%) | 22 (28%) | 10 (19%) | |
| Full-time worker | 45 (60%) | 43 (54%) | 31 (60%) | |
| Part-time worker or full-time housemaker | 18 (24%) | 13 (16%) | 10 (19%) | |
| Declined to respond | 1 (1%) | 2 (3%) | 1 (2%) | |
| Household annual income | 0.1 | |||
| Less than $39,999 | 21 (28%) | 29 (36%) | 15 (29%) | |
| $40,000 to $79,999 | 16 (21%) | 17 (21%) | 15 (29%) | |
| $80,000 to $99,999 | 5 (7%) | 7 (9%) | 4 (8%) | |
| More than $100,000 | 27 (36%) | 17 (21%) | 7 (13%) | |
| Don’t know/declined to respond | 6 (8%) | 10 (13%) | 11 (21%) | |
| No. of children in household | 0.2 | |||
| 1 child | 27 (36%) | 26 (32%) | 25 (48%) | |
| 2 or more children | 48 (64%) | 54 (68%) | 27 (52%) | |
| Age, y | 40.0 [36.0-47.0] | 37.0 [33.0-42.0] | 38.0 [32.0-42.0] | 0.006 |
| Child Characteristics | ||||
| Kidney disease classification | 0.1 | |||
| CAKUT | 11 (15%) | 12 (15%) | 12 (23%) | |
| Transplant recipient | 11 (15%) | 17 (21%) | 11 (21%) | |
| Kidney replacement therapy | 3 (4%) | 9 (11%) | 0 | |
| Glomerular disease | 26 (35%) | 15 (19%) | 7 (13%) | |
| Primary hypertension | 6 (8%) | 7 (9%) | 6 (12%) | |
| Congenital/hereditary/cystic | 9 (12%) | 12 (15%) | 9 (17%) | |
| Other | 9 (12%) | 8 (10%) | 7 (13%) | |
| Sex | 0.01 | |||
| Male | 38 (51%) | 57 (71%) | 27 (52%) | |
| Female | 37 (49%) | 22 (28%) | 24 (46%) | |
| Unknown | 0 | 1 (1%) | 1 (2%) | |
| Child insurance type | 0.002 | |||
| No insurance | 0 | 0 | 0 | |
| Private | 45 (60%) | 27 (34%) | 18 (35%) | |
| Public | 29 (39%) | 52 (65%) | 31 (60%) | |
| Unknown | 1 (1%) | 1 (1%) | 3 (6%) | |
| Child age, y | 11.0 [5.5-15.0] | 8.0 [1.0-14.0] | 11.5 [5.0-14.2] | 0.05 |
| COVID-19 Impact | ||||
| Contracted COVID-19, confirmed or suspected | 26 (35%) | 25 (31%) | 11 (21%) | 0.3 |
| Hospitalized due to COVID-19a | 1 (4%) | 1 (4%) | 0 | 0.9 |
| Significant exposures to COVID-19b | 18 (24%) | 25 (31%) | 15 (29%) | 0.6 |
| Child contracted COVID-19, confirmed or suspected | 15 (20%) | 16 (20%) | 12 (23%) | 0.9 |
| Child hospitalized due to COVID-19a | 1 (7%) | 3 (19%) | 0 | 0.09 |
| Child experienced worsening of kidney disease due to COVID-19a | 0 | 1 (6%) | 0 | 0.9 |
| Child had significant exposures to COVID-19b | 16 (21%) | 16 (20%) | 11 (21%) | 0.9 |
| Child missed more medications during the pandemic | 3 (4%) | 5 (6%) | 4 (8%) | 0.7 |
| Child’s access to care negatively affected by the pandemic | 29 (39%) | 33 (41%) | 19 (37%) | 0.9 |
| No. of mitigation tasks performed | 12.0 [10.0-15.0] | 11.5 [8.8-14.0] | 9.0 [6.8-12.0] | <0.001 |
| Self-efficacy score in mitigating risk of COVID-19 | 3.6 [3.2-4.0] | 3.2 [3.0-3.4] | 3.0 [2.7-3.2] | <0.001 |
| Psychological and financial impact score | 3.5 [2.8-4.6] | 3.6 [2.9-4.6] | 3.5 [2.8-4.8] | 0.8 |
| Information Sources on COVID-19 Vaccines | ||||
| Sources of information | <0.001 | |||
| Physicians | 42 (56%) | 65 (81%) | 46 (88%) | |
| Multiple sourcesc | 33 (44%) | 15 (19%) | 6 (12%) | |
| Venues of information receipt | 0.2 | |||
| Physicians’ offices | 54 (72%) | 59 (74%) | 42 (81%) | |
| Websites | 1 (1%) | 6 (8%) | 1 (2%) | |
| Multiple venuesd | 20 (27%) | 15 (19%) | 9 (17%) | |
Values for continuous variables given as median [IQR]. Abbreviation: CAKUT, congenital anomalies of the kidney and urinary tract.
Proportion among those who contracted COVID-19.
Defined as being in the same room for more than 15 minutes with someone who had COVID-19.
Including physicians, government agencies, scientists, family and friends, and celebrities.
Including physicians’ offices, websites, newspapers/magazines, television, and social media.
Willingness to Receive the COVID-19 Vaccine
In total, 75 (36%) participants indicated they were willing to vaccinate their child with kidney disease or hypertension against COVID-19, while 80 (39%) were “unsure,” and 52 (25%) were unwilling. There was moderate agreement between the parents’ willingness to vaccinate themselves versus their child with kidney disease or hypertension and versus other children without kidney disease (Table 2 ). Parents were less willing to vaccinate their children than themselves. Agreement between willingness to vaccinate the child with kidney disease or hypertension and other children was high although there was lower willingness to vaccinate the child with kidney disease or hypertension (Table 2).
Table 2.
Willingness to Receive the COVID-19 Vaccine for Self, Child With Kidney Disease, and Child Without Kidney Disease (if Any)
| Willingness to Vaccinate Self |
|||
|---|---|---|---|
| Yes | Unsure | No | |
| Willingness to vaccinate child with kidney diseasea | |||
| Yes | 72 (35%) | 1 (1%) | 2 (1%) |
| Unsure | 38 (18%) | 38 (18%) | 4 (2%) |
| No | 2 (1%) | 8 (4%) | 42 (20%) |
| Willingness to vaccinate child without kidney disease | |||
| Yes | 63 (40%) | 1 (1%) | 1 (1%) |
| Unsure | 21 (13%) | 29 (18%) | 3 (2%) |
| No | 0 | 6 (4%) | 35 (22%) |
| Willingness to Vaccinate Child With Kidney Diseasea |
|||
|---|---|---|---|
| Yes | Unsure | No | |
| Willingness to vaccinate child without kidney disease | |||
| Yes | 55 (35%) | 9 (6%) | 1 (1%) |
| Unsure | 2 (1%) | 48 (30%) | 3 (2%) |
| No | 1 (1%) | 2 (1%) | 38 (24%) |
Agreement between COVID-19 vaccine for self versus child with kidney disease: κ, 0.60 (95% CI, 0.51-0.68); agreement between COVID-19 vaccine for self versus child without kidney disease: κ, 0.69 (95% CI, 0.59-0.78); agreement between COVID-19 vaccine for child with kidney disease versus child without kidney disease: κ, 0.83 (95% CI, 0.75-0.90).
Or hypertension.
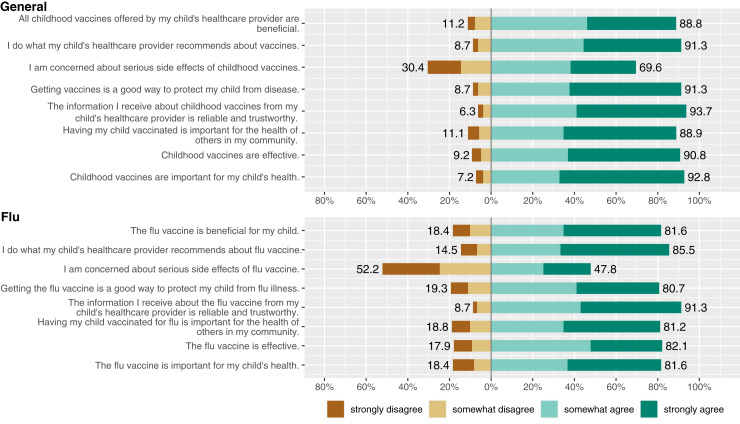
Parental Attitudes Toward General Childhood and Influenza Vaccines
Overall, the mean VHS score for general childhood vaccines was 1.92 ± 0.78 (SD). Nineteen participants (9%) had a score of ≥3, indicating high hesitancy. The VHS scores were higher for influenza vaccines, for which the mean was 2.10 ± 0.99; 37 (18%) participants had score of ≥3 (Fig 2 ). The mean scores for both general childhood and influenza vaccines were highest among those who were unwilling to vaccinate their child with kidney disease or hypertension against COVID-19 (Table 3 ).
Figure 2.
Responses to the Vaccine Hesitancy Scale,16 including questions on general childhood and influenza vaccines, of parents of children with kidney disease or primary hypertension.
Table 3.
Vaccine Hesitancy Scale Scores Among Parents of Children With Kidney Disease or Hypertension by Willingness to Vaccine Child Against COVID-19
| Willingness to Vaccinate Child Against COVID-19 (N = 207) |
Pa | |||
|---|---|---|---|---|
| No (n = 52) | Unsure (n = 80) | Yes (n = 75) | ||
| Vaccine Hesitancy Scaleb score for | ||||
| General childhood vaccines | 2.6 ± 0.8 | 1.9 ± 0.6 | 1.5 ± 0.5 | <0.001 |
| Influenza vaccines | 2.9 ± 1.0 | 2.1 ± 0.9 | 1.5 ± 0.6 | <0.001 |
Scores given as mean ± SD.
ANOVA test to examine differences in Vaccine Hesitancy Scale scores among the 3 groups (“no,” “unsure,” and “yes”).
Higher scores on Vaccine Hesitancy Scale16 indicate increased hesitancy. A score of ≥3 indicates high hesitancy.
Predictors of Willingness to Vaccinate Child With Kidney Disease or Hypertension Against COVID-19
Table 1 summarizes the findings from the unadjusted analysis. In the adjusted analysis (Table 4 ), having a child with glomerular disease versus congenital anomalies of the kidney and urinary tract (CAKUT) and having a college or higher degree were associated with willingness to vaccinate. The respondents who identified as Black were more likely to be unwilling to vaccinate compared with the White respondents. In analyses contrasting with the group who was unsure, parents with a child of female sex were more likely to be willing to have their child vaccinated, and parents of older age were nominally more likely to be willing to vaccinate, although this result was of borderline statistical significance.
Table 4.
Adjusted Analysis of Predictors of Parental Response to Willingness to Vaccinate Child With Kidney Disease or Hypertension Against COVID-19
| Unsure |
Unwilling |
|||
|---|---|---|---|---|
| OR (95% CI)a | P | OR (95% CI)b | P | |
| Child’s kidney disease classification | ||||
| CAKUT | 1.00 (reference) | 1.00 (reference) | ||
| Transplant recipient | 1.77 (0.51-6.16) | 0.4 | 0.78 (0.21-2.97) | 0.7 |
| Kidney replacement therapyc | — | — | — | — |
| Glomerular disease | 0.84 (0.25-2.82) | 0.8 | 0.21 (0.05-0.80) | 0.02 |
| Hypertension | 1.39 (0.30-6.37) | 0.7 | 0.40 (0.08-2.04) | 0.3 |
| Congenital/hereditary/cystic | 1.95 (0.50-7.53) | 0.3 | 0.53 (0.12-2.24) | 0.4 |
| Other | 1.17 (0.28-4.86) | 0.8 | 0.93 (0.22-3.90) | 0.9 |
| Respondent race | ||||
| White | 1.00 (reference) | 1.00 (reference) | ||
| Black | 1.17 (0.52-2.64) | 0.7 | 2.59 (1.03-6.53) | 0.04 |
| Other | 1.15 (0.37-3.57) | 0.8 | 0.66 (0.15-2.91) | 0.6 |
| Female sex of respondent | 1.43 (0.50-4.12) | 0.5 | 0.38 (0.12-1.18) | 0.1 |
| Respondent insurance type | ||||
| No insurance/declined to respond | 1.00 (reference) | 1.00 (reference) | ||
| Private | 0.32 (0.08-1.25) | 0.1 | 0.42 (0.09-1.88) | 0.3 |
| Public | 0.39 (0.09-1.69) | 0.2 | 0.36 (0.08-1.72) | 0.2 |
| Respondent education level | ||||
| High school or less | 1.00 (reference) | 1.00 (reference) | ||
| Some college | 0.98 (0.32-3.00) | 0.9 | 0.54 (0.17-1.75) | 0.3 |
| College graduate or higher | 0.73 (0.26-2.10) | 0.6 | 0.19 (0.06-0.60) | 0.005 |
| Female sex of child | 0.27 (0.12-0.60) | 0.001 | 1.01 (0.42-2.47) | 0.9 |
| Respondent age, y | 0.96 (0.91-1.00) | 0.05 | 0.95 (0.91-1.00) | 0.08 |
Analysis was by multinomial logistic regression. Variables “number of mitigation tasks performed,” “self-efficacy,” and “sources of information” were not included in multivariate analysis due to multicollinearity. Abbreviations: CAKUT, congenital anomalies of the kidney and urinary tract; OR, odds ratio.
OR for comparison of unsure about vaccinating versus willing to vaccinate.
OR for comparison of unwilling to vaccinate versus willing to vaccinate.
Due to the low number of participants, the OR, CI, and P values were not reliably estimable.
Interview Findings
Participants
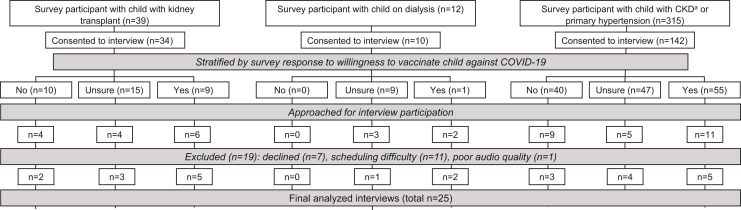
Figure 3 shows the derivation of the cohort of interview participants through targeted sampling. Table S1 shows the number of interview participants by willingness to vaccinate child against COVID-19 and child’s kidney disease classification.
Figure 3.
Interview participants on COVID-19 vaccine attitudes for children and adolescents with kidney disease or primary hypertension. aKidney disease due to congenital anomalies of kidney and urinary tract, glomerular disease, cystic/hereditary/congenital disease (C/H/C), or others not include those on dialysis or with a kidney transplant. Abbreviation: CKD, chronic kidney disease.
Influences on Parental Attitudes Toward COVID-19 Vaccines
Three salient themes described in the following subsections differentiated the participants who were willing, unsure, or unwilling to vaccinate their child with kidney disease or hypertension against COVID-19. Table S2 contains illustrative quotes and numbers of interviewees who expressed each relevant thematic concept by willingness to vaccinate.
Benefits Versus Harm
Most participants (13 of 25) acknowledged that vaccines protect from illnesses, even if they were unsure or unwilling to vaccinate their child against COVID-19. However, attitudes differed in perceptions of benefits versus harm. Those who were unsure or unwilling expressed more often that the COVID-19 vaccines were rushed. Participants were distrustful of the motivations and processes involved in COVID-19 vaccine development and were concerned that side effects, including death, are overlooked in the rush to develop vaccines (ie, they expressed fear of serious side effects). A common linked concept in this group is that long-term side effects are unknown. Another expressed perception was that their child is less vulnerable to COVID-19, with some stating that they had “done well thus far” during the pandemic without issues and that vaccines are really only necessary for those who are more frail, such as seniors. In contrast, those willing to vaccinate more frequently voiced the benefits of the vaccines, including attitudes such as vaccines will allow them to get back to normal and protect others and the community. Participants in the “yes” group also expressed that side effects from the vaccines would be preferable to the actual infection (ie, the benefits of getting vaccinated outweighs the risks of COVID-19).
“What Do the Doctors Think?”
Fourteen of the 25 participants stated a desire to know the doctors’ opinions on the COVID-19 vaccines when asked what information they would like to have. However, the perceptions of providers and experiences with health care differed among the groups. Participants who were unsure or unwilling to vaccinate expressed that “doctors are not on the same page” when it comes to the COVID-19 vaccines and conflicting information was given throughout the pandemic. They also expressed that “doctors just push vaccines” onto patients without listening to their concerns or considering other values that may be more important to patients. By contrast, only those who were willing to vaccinate expressed that “doctors are the most knowledgeable” when it comes to COVID-19 and their child and that doctors and the medical team provide a lot of information on COVID-19. Half of those willing to vaccinate expressed “going along with what the doctors say” to help them reach the decision to vaccinate. By contrast, participants in the “no” and “unsure” groups expressed the importance of “doing one’s own research” when it comes to the COVID-19 vaccines.
Information Still Needed
Regardless of their attitudes toward the COVID-19 vaccines, parents had many questions. Half stated the need to have more information on the effects of the vaccines on their child’s condition (ie, expressed wanting information specific to their unique situation), including effects on children, effects on those who are immunocompromised, and effects on glomerular disease activity and kidney function. Most participants unsure or unwilling to vaccinate (10 of 13) expressed the need for more information on benefits and side effects of the vaccines compared with just 1 out of 12 participants who were willing to vaccinate.
Discussion
In this mixed-methods study of parental attitudes toward vaccines for children with kidney disease or primary hypertension, we found that COVID-19 vaccine hesitancy was highly prevalent (64%) and associated with hesitancy toward general childhood and influenza vaccines. More highly educated parents were more likely to be willing to vaccinate their child against COVID-19, while Black race was associated with being more likely to be unwilling to vaccinate. In interviews, we found that information on COVID-19 vaccine efficacy and side effects, particularly specific to the child’s condition, may be important in influencing parental attitudes. Doctors and the medical team are trusted sources of information, though communication needs to be consistent, appropriate to the level of the parent’s health literacy, and empathetic to the values of the parent.
Our survey findings are similar to other reports. The Centers for Disease Control and Prevention’s National Immunization Survey collected from September 26 to October 30, 2021, found that 26.3% of parents and guardians of children 5-17 years old “definitely will” get their child vaccinated, 25.1% “probably will or are unsure,” and 21% “probably or definitely will not.” Similar to our findings, higher maternal education and insurance other than Medicaid or no insurance were also associated with willingness to vaccinate.19
Pertinent to the pediatric kidney disease community, we found that parents were most hesitant to vaccinate their child with kidney disease compared with themselves and their other children. This highlights the importance of addressing COVID-19 vaccine hesitancy in pediatric kidney practices.
Overall, the proportions of parents in our cohort who had high hesitancy toward general childhood (9%) and influenza (18%) vaccines appear similar to the general US population of 6.1% for childhood and 25.8% for influenza vaccines.16 In our cohort, higher hesitancy toward routine childhood and influenza vaccines correlated with hesitancy toward COVID-19 vaccines. Thus, past vaccination behavior such as refusal or delays in vaccination may be helpful to identify subgroups at risk for low COVID-19 vaccine uptake who may benefit from targeted interventions.
The need for more information on COVID-19 vaccines was a salient theme from our interviews, particularly among those unwilling or unsure about vaccinating their child with kidney disease. Interventions focused on information delivery may be effective. Most parents stated the need for more information on how the COVID-19 vaccines would affect their child’s condition. It may also be helpful to inform parents of concrete benefits of the COVID-19 vaccines. Fear of potential and unknown side effects need to be clearly discussed with the parents.
A key finding from our study is the importance of doctors and the health care team in providing COVID-19 vaccine information. In unadjusted analysis, the parents who reported receiving their information on COVID-19 vaccines primarily from doctors were more likely to be willing to vaccinate their child with kidney disease. This observation was strengthened by our interview finding that the majority of parents wished to know what their doctors think about the COVID-19 vaccines, regardless of their expressed willingness to vaccinate. Our findings are congruent with prior literature that health care professionals are the most importance sources for vaccine information for parents.20
Our findings further elucidate key issues in patient–provider communication. First, discussions of COVID-19 vaccines need to be tailored to the parent’s level of understanding and may need to be repeated over time to enhance learning20; consistency in messaging among providers and over time also appears to be important. Kidney patients often interact with medical teams consisting of nurses, physicians, advanced practitioners, nutritionists, and social workers. We postulate that implementing regular team training and standardizing patient informational materials to ensure consistent and clear messaging from the multidisciplinary team may be beneficial, though further research is needed.
A final issue is that consideration of parental values and perspectives in vaccine discussions are also important. This requires active listening and engaging parents to express their values and priorities. The literature suggests aligning vaccine messaging with caregiver values is effective in increasing vaccine uptake. In a systematic review by Olson et al,20 message-framing techniques such as emotive anecdotes, emotive imagery, and co-promoted behavioral messaging may be effective ways to promote vaccine uptake. Following the P3 model framework, we summarize our recommendations in Box 1 .
Box 1. Summary of Considerations for COVID-19 Vaccine Promotion for Children With Kidney Disease or Primary Hypertension Following the P3 Model.
Practice Level
-
•
Structure vaccine promotional team with physicians as key members in delivery of vaccine information
-
•
Conduct regular multidisciplinary team training on vaccine communication
-
•
Standardize vaccine informational materials used across the health care setting
-
•
Coordinate staff and clinical encounters to present vaccine information at multiple points of an encounter and in a recurring manner
-
•
Systematically track vaccination history and provide prompts for vaccination
Provider Level
-
•
Active participation in communications with patients and caregivers on vaccination
-
•
Prompts from electronic medical record system to providers for vaccination and alerts regarding missed/delayed vaccination
-
•Communication style training
-
◇Active listening and bidirectional communication
-
◇Message-framing techniques to align messaging with caregiver values
-
◇Delivery appropriate to patient’s/caregiver’s health literacy status
-
◇
Patient Level
-
•Clear informational materials delivered to patients and family in multiple and recurring encounters, covering:
-
◇Targeted information specific to kidney/health condition
-
◇Concrete information on benefits from vaccination
-
◇Clear information on side effects
-
◇
-
•
Prompts to discuss vaccinations with physicians and other members of the team
P3 is the Practice, Provider, and Patient Level model developed by Bednarczyk et al.15
The COVID-19 pandemic continues to evolve. Periodic surges in infections; changes in disease severity and transmissibility associated with different virus variants; updates in vaccine development, rollout, and reports of side effects all could impact caregiver attitudes. These important larger contextual factors were not examined in the current study as we took the approach to evaluate factors relevant and addressable within clinical practice. Parental attitudes and prevalence of COVID-19 vaccine hesitancy are likely to have shifted since our study was conducted. However, our findings that parents have greater hesitancy toward vaccinating their child with kidney disease compared with their other children and that COVID-19 vaccine hesitancy is associated with hesitancy toward general childhood and influenza vaccines among other factors are still relevant to vaccine promotion in health care settings. Our findings on the importance of doctors and the health care team in providing COVID-19 vaccine information and considerations for effective communication remain important regardless of the evolution of the pandemic.
Our study has other limitations. The patient cohort in our study have varied underlying kidney diseases and were cared for by different providers even within a single system, so they experienced different clinical interaction frequencies and possibly communications about the vaccines. These factors were not examined in our survey analysis, and they may have confounded our observation that parents of children with glomerular diseases were more likely to be willing to vaccinate their child. In the design of this study, we recognized the complexity of factors that could influence an individual’s attitude toward vaccines, which would be difficult to fully capture and analyze with clarity via surveys and quantitative analysis. Furthermore, generalizability would be limited across different clinic settings and other institutions and contexts. Thus, we conducted in-depth interviews so that we could gain a more in-depth understanding of the various influences on vaccine attitudes and generate useful knowledge applicable to other centers.
The participants volunteering for the survey and interview may not be representative of most parents. In addition, the response rate differed by the child’s kidney condition and was lowest among the parents of children with a kidney transplant. This may be due to differences in clinic flow. The children in our transplant clinic have many scheduled tasks (eg, blood draws and visits with pharmacists and dieticians), so their parents may not have had as much time to participate in the survey. We did have a sound survey return rate of >20% in each group and 39% overall. We have relatively few children on dialysis, thus issues specific to this vulnerable subgroup may not have been fully captured. Another limitation is our findings may not reflect the attitudes and experiences of non–English-speaking minority groups in the United States.
In summary, we present novel information on the prevalence, predictive factors, and influences on vaccine hesitancy in this vulnerable patient cohort. We combined the strengths of quantitative and qualitative methodology for robust findings to help inform the kidney community on the scope of vaccine hesitancy and develop COVID-19 vaccine promotional campaigns.
Article Information
Authors’ Full Names and Academic Degrees
Chia-shi Wang, MD, MSc, Rinchen Doma, BS, Adrianna L. Westbrook, MPH, Jillian Johnson, BS, Evan J. Anderson, MD, Larry A. Greenbaum, MD, PhD, Shaheen A. Rana, MA, Roshan P. George, MD, Rouba Garro, MD, Anjali Khanna-Farber, MBBS, MPh, Cam Escoffery, PhD, MPH, and Robert A. Bednarczyk, PhD.
Authors’ Contributions
Research idea and study design: C-sW, EJA, LAG, RAB; data acquisition: RD, JJ, AK-F; data analysis/interpretation: C-sW, RD, ALW, JJ, EJA, LAG, SAR, RPG, RG, AK-F, CE, RAB; statistical analysis: C-sW, ALW. Each author contributed important intellectual content during manuscript drafting or revision and agrees to be personally accountable for the individual’s own contributions and to ensure that questions pertaining to the accuracy or integrity of any portion of the work, even one in which the author was not directly involved, are appropriately investigated and resolved, including with documentation in the literature if appropriate.
Support
This study was funded by the Children’s Healthcare of Atlanta Clinical Outcomes Research and Public Health Center. Statistical consultation was provided by Emory Pediatric Institute Biostatistical Core. Qualitative research consultation was supported in part by the Intervention Development, Dissemination and Implementation (IDDI) Shared Resource of Winship Cancer Institute of Emory University and National Institute of Health/National Cancer Institute under award number P30CA138292. Dr Wang is supported by the NIH-NIDDK under Award Number K23DK118189. The funders had no rule in study design; collection, analysis, and interpretation of data; writing the report; and the decision to submit the report for publication.
Financial Disclosure
Dr Anderson has consulted for Pfizer, Sanofi-Pasteur, Janssen, and Medscape, and his institution receives funds to conduct clinical research unrelated to this article from MedImmune, Regeneron, PaxVax, Pfizer, GSK, Merck, Sanofi-Pasteur, Janssen, and Micron. He also serves on a safety monitoring board for Kentucky BioProcessing, Inc, and Sanofi-Pasteur. His institution has also received funding from the NIH to conduct clinical trials of Moderna and Janssen COVID-19 vaccines. The remaining authors declare that they have no relevant financial interests.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Peer Review
Received December 22, 2021. Evaluated by 2 external peer reviewers, with direct editorial input from a Statistics/Methods Editor, an Associate Editor, and the Editor-in-Chief. Accepted in revised form April 25, 2022.
Footnotes
Complete author and article information provided before references.
Item S1: Survey design.
Table S1: Number of interview participants by response to willingness to vaccinate child with kidney disease or hypertension against COVID-19 and child’s kidney disease classification.
Table S2: Salient themes in interviews with parents on attitudes toward COVID-19 vaccines for their child with kidney disease or hypertension, with illustrative quotes.
Supplementary Material
Item S1. Tables S1-S2.
References
- 1.World Health Organization Strategic Advisory Group of Expert on Immunication (SAGE) Report of the SAGE Working Group on Vaccine Hesitancy. https://web.archive.org/web/20211025133401/https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdfhttps://cdn.who.int/media/docs/default-source/immunization/sage/2014/october/2-sage-appendicies-background-final.pdf?sfvrsn=2259f1bf_4
- 2.Centers for Disease Control and Prevention COVID data tracker: demographic trends of people receiving COVID-19 vaccinations in the United States. COVID-NET. https://covid.cdc.gov/covid-data-tracker/#vaccination-demographics-trends
- 3.Hamel L., Lopes L., Sparks G., et al. KFF COVID-19 vaccine monitor. KFF, October 8, 2021. KFF. 2021. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-october-2021/
- 4.Johansen K.L., Chertow G.M., Foley R.N., et al. US Renal Data System 2020 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2021;77(4 Suppl 1):A7–a8. doi: 10.1053/j.ajkd.2021.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harambat J., van Stralen K.J., Kim J.J., Tizard E.J. Epidemiology of chronic kidney disease in children. Pediatr Nephrol. 2012;27(3):363–373. doi: 10.1007/s00467-011-1939-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Banerjee D., Popoola J., Shah S., Ster I.C., Quan V., Phanish M. COVID-19 infection in kidney transplant recipients. Kidney Int. 2020;97(6):1076–1082. doi: 10.1016/j.kint.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Henry B.M., Lippi G. Chronic kidney disease is associated with severe coronavirus disease 2019 (COVID-19) infection. Int Urol Nephrol. 2020;52(6):1193–1194. doi: 10.1007/s11255-020-02451-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gibertoni D., Reno C., Rucci P., et al. COVID-19 incidence and mortality in non-dialysis chronic kidney disease patients. PLoS One. 2021;16(7) doi: 10.1371/journal.pone.0254525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ikizler T.A. COVID-19 and dialysis units: what do we know now and what should we do? Am J Kidney Dis. 2020;76(1):1–3. doi: 10.1053/j.ajkd.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shen Q., Wang M., Che R., et al. Consensus recommendations for the care of children receiving chronic dialysis in association with the COVID-19 epidemic. Pediatr Nephrol. 2020;35(7):1351–1357. doi: 10.1007/s00467-020-04555-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention Laboratory-confirmed COVID-19-associated hospitalizations. https://gis.cdc.gov/grasp/COVIDNet/COVID19_5.html
- 12.Howard L.M., Garguilo K., Gillon J., et al. The first 1000 symptomatic pediatric SARS-CoV-2 infections in an integrated health care system: a prospective cohort study. BMC Pediatr. 2021;21(1):403. doi: 10.1186/s12887-021-02863-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization Ten threats to global health in 2019. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019
- 14.MacDonald N.E., Hesitancy SWGoV. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 15.Bednarczyk R.A., Chamberlain A., Mathewson K., Salmon D.A., Omer S.B. Practice-, provider-, and patient-level interventions to improve preventive care: development of the P3 Model. Prev Med Rep. 2018;11:131–138. doi: 10.1016/j.pmedr.2018.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kempe A., Saville A.W., Albertin C., et al. Parental hesitancy about routine childhood and influenza vaccinations: a national survey. Pediatrics. 2020;146(1) doi: 10.1542/peds.2019-3852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hennink M.M., Kaiser B.N., Marconi V.C. Code saturation versus meaning saturation: how many interviews are enough? Qual Health Res. 2017;27(4):591–608. doi: 10.1177/1049732316665344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hennink M., Hutter I., Bailey A. Sage; 2011. Qualitative Research Methods. [Google Scholar]
- 19.Centers for Disease Control and Prevention COVID-19 vaccination coverage and vaccine confidence among children. CovidVaxView. https://www.cdc.gov/vaccines/imz-managers/coverage/covidvaxview/interactive/children.html
- 20.Olson O., Berry C., Kumar N. Addressing parental vaccine hesitancy towards childhood vaccines in the United States: a systematic literature review of communication interventions and strategies. Vaccines (Basel) 2020;8(4):590. doi: 10.3390/vaccines8040590. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Item S1. Tables S1-S2.