Abstract
Introduction
This study aimed to identify the impact of the COVID-19 pandemic upon radiography education across Latin American countries.
Methods
A survey containing 20 questions was circulated to radiography students, across 13 universities in 11 countries of Latin America using Google Forms. The survey contained open and closed questions. Answers were analysed with descriptive statistics and the methodology of interpretative phenomenological analysis for the open answers.
Results
Of the 1310 responses only 23.9% (n = 313) of students reported attending clinical placements and from this cohort only 8.9% (n = 28) became infected with COVID-19. In response to how the pandemic had impacted upon the students’ academic progression, the most common topic in the open answers was “Concerns about the lack of clinical training”, mentioned by 629 students. Students in middle and later years of their radiography education expressed the greatest concern about future clinical placements. Almost all radiography students (95.2%/n = 1247) indicated that their main concerns regarding COVID-19 infection while undertaking clinical placements was in relation to the risk of infecting their families as most students stated they cohabited with relatives (86.6%/n = 1134).
Conclusion
Compared to European findings co-habitation trends increased anxiety related to infection and impacted their mental health. Students expressed concern about the quality of education they were receiving during the pandemic and access to resources to facilitate on-line learning was inadequate. Socio-economic and internet connectivity factors specific to Latin America were identified and these issues need to be addressed if on-line education is required in the future.
Implications for practice
The COVID-19 pandemic has impacted Latin America and this study identifies the implications for radiography students related to their clinical and academic training and highlights factors which require consideration to support radiography students as the pandemic continues.
Keywords: Student radiographers, Radiography education, COVID-19, Clinical placements
Introduction
Coronavirus 2019 (COVID-19), the illness caused by SARS-CoV-2, was declared a pandemic in March 2020 and has provoked important changes in medical education worldwide.1 Universities were forced to cancel in-person classes, close classrooms and laboratories, and suspend clinical rotations in many countries. Some activities were replaced with recorded lectures, webinars or live-streams due to the high probability that students could get infected and the need to conserve personal protective equipment (PPE) in hospitals. In radiography education, though some strategies were implemented, the need for hospital-based clinical placements remained essential. Besides the risk of infection of students, clinical placements were also impacted by the postponement of elective imaging examinations which provide important education and learning opportunities.2 This situation also affected trainees in radiology residency programmes with a reduction in training hours and a direct impact in didactic case-based education due to social distancing diminishing the value of education.3
In a recent study4 involving radiography students from Europe, Asia, Africa, and Australia, the opinions of students on their education and clinical placements due to the COVID-19 pandemic were highlighted. Students were more concerned about the future of their education, and their clinical placements, than with challenges associated with working with patients infected with COVID-19 in hospitals. However, contracting the virus and infecting the people they live were primary concerns.
There are some differences in radiography education between the countries in these mentioned continents and countries from Latin America, e.g. the duration of the programs (ranging from 2 to 5 years), the contents in the syllabus, the balance of hours in lectures and clinical placements. Thus, the current study was implemented to learn more about how COVID-19 is affecting radiography students from Latin America, across 11 countries, with the aim of identifying factors which require addressing to improve the learning environment for Latin American radiography students.
Methods
Survey design
A survey containing 20 questions based on that employed by Rainford et al. (2020),4 with permission, was distributed online via Google Forms (Google LLC, Menlo Park, USA). The questions were developed to investigate the impact of COVID-19 upon clinical placement training and academic provision for student radiographers. The survey took less than 10 min to complete. No incentive was offered to the students for participating in the study. The survey was structured to request demographic information e.g. age, country of study, university, academic year of study, and details about their domestic and health situations. Furthermore, students had to indicate if they had been on clinical placements between March 2020 and April 2021. Students who indicated they had been on clinical placement rotations were asked if these were voluntary or mandatory placements and whether students attended facilities who received and cared for COVID-19 patients. Students were asked to identify the main challenges and concerns about their clinical placements; about concerns about their academic learning; how the pandemic has affected their academic progress; and their perceptions on being a radiography student and their future career following the start of the pandemic.
This research was deemed exempt from full ethical review by the ethics committee of the University of Costa Rica. All responses were anonymous, and participants consented to their data being used in the analysis and any related publications. The responses were collected and exported to spreadsheets for analysis.
Participating institutions
A total of 13 Latin America radiography training universities were invited to participate from 11 countries. The link to the survey was distributed to all radiography students in the selected universities, from first year of education to those in the process of graduation. Each institution used their internal student communication systems to recruit locally. The survey was opened for a 6-week period: May to mid-June 2021 and survey reminders were issued by the participating academic institutions.
Statistical analysis
Data was coded and transcribed to Microsoft Excel (Microsoft Corp., Redmond, USA) sheets for data analysis. Descriptive statistics were employed, and data was analysed in RStudio® software (RStudio, Boston, USA).
Open answer responses were reviewed using interpretative phenomenological analysis, which is a qualitative technique focused on how people give significance to their experiences.5 An initial review of all open-ended responses was undertaken with the aim of identifying trends in the data. Secondly, common topics/themes and finally sub-themes/topic groups were created with the use of NVivo 29.2.0 software (QSR International, Doncaster, Australia).
Results
Demographics
A total of 1310 responses were received from student radiographers from the 13 participating institutions from 11 countries (a total population of 2384 students). An overall response rate of 54.9% was achieved. The mean age of responding students was 23.24 years (SD 4.24). Radiography programme durations in the different institutions varied from: 5 years (n = 303, 23.1%), 4.5 years (n = 233, 17.8%), 4 years (n = 357, 27.2%), 3 years (n = 192, 14.7%), 2.5 years (n = 173, 13.2%), and other (n = 52, 3.9%; ‘varies between 2 and 3 years’). The participants were from varying stages of training, categorised as follows; 3-year programmes: Beginning (Year 1), Middle (Year 2) and Advanced (Year 3); 4-year programmes: Beginning (Year 1), Middle (Years 2 and 3) and Advanced (Year 4); 4.5 and 5-year programmes: Beginning (Years 1 and 2), Middle (Years 3 and 4) and Advanced (Year 5). Finally, due to the impact of the pandemic, some students who had completed all components of their programmes but had outstanding clinical placement which pushed them into a new academic year were categorised as ‘Clinical Placements Outstanding’. This resulted in the categorisation as follows: Beginning (n = 249, 19%), Middle (n = 583, 44.5%), Advanced (n = 349, 26.6%) and Clinical Placements Outstanding (n = 129, 9.8%). Table 1 outlines the demographic of responses by university.
Table 1.
Demographic data of the participating student radiographers.
| Country | Participating institution | Students (n) | Responses (n) | Response rate (%) | Study category | Mean age (SD, Range) |
|---|---|---|---|---|---|---|
| Argentina | Universidad Nacional de Cuyo | 61 | 43 | 70.5 | Beginning: 6 Middle: 16 Advanced: 12 CPO: 9 |
23.1 (3.0, 19–33) |
| Bolivia | Universidad de San Francisco Xavier | 270 | 182 | 67.4 | Beginning: 118 Middle: 56 Advanced: 1 CPO: 7 |
20.3 (2.8, 17–31) |
| Chile | Universidad Católica del Maule | 30 | 12 | 40.0 | Middle: 10 Advanced: 2 |
22.1 (4.8, 20–37) |
| Chile | Universidad de Chile | 36 | 36 | 100.0 | Beginning: 1 Middle: 27 Advanced: 8 |
22.1 (2.3, 18–30) |
| Colombia | Fundación Universitaria del Área Andina | 532 | 114 | 21.4 | Beginning: 2 Middle: 70 Advanced: 40 CPO: 2 |
25.6 (6.6, 18–54) |
| Costa Rica | Universidad de Costa Rica | 134 | 88 | 65.7 | Beginning: 14 Middle: 47 Advanced: 26 CPO: 1 |
21.8 (2.3, 18–28) |
| Ecuador | Universidad Central del Ecuador | 340 | 323 | 95.0 | Beginning: 39 Middle: 176 Advanced: 69 CPO: 39 |
22.2 (2.6, 18–32) |
| Ecuador | Universidad de Cuenca | 57 | 49 | 86.0 | Beginning: 10 Middle: 27 Advanced: 7 CPO: 5 |
22.9 (2.2, 18–29) |
| Honduras | Universidad Nacional Autónoma de Honduras | 488 | 248 | 50.8 | Beginning: 6 Middle: 91 Advanced: 66 CPO: 85 |
23.3 (4.6, 17–45) |
| Panamá | Universidad Especializada de las Américas | 150 | 69 | 46.0 | Beginning: 2 Middle: 28 Advanced: 28 CPO: 11 |
29.2 (12.2, 19–58) |
| Paraguay | Universidad de Asunción | 106 | 26 | 24.5 | Beginning: Middle: 19 Advanced: 3 CPO: 4 |
24.0 (4.5, 19–40) |
| Perú | Universidad Nacional Mayor de San Marcos | 55 | 23 | 41.8 | Beginning: 1 Middle: 1 Advanced: 5 CPO: 16 |
25.1 (3.7, 20–35) |
| Uruguay | Universidad de la República | 125 | 97 | 77.6 | Beginning: 0 Middle: 90 Advanced: 6 CPO: 1 |
26.4 (6.2, 20–56) |
| Total | 2384 | 1310 | 54.9 | 23.24 (4.24, 17–58) | ||
CPO = Clinical Placements Outstanding across the radiography programme due to COVID-19.
Living situation
Overall, most students cohabited with relatives n = 1134 (86.6%), where n = 587 (44.8%) students live with a family member who has an underlying condition that is compromised due to COVID-19. At least n = 66 (5%) students had one underlying risk factor.
Clinical placements
Only n = 313 (23.9%) students had been in clinical placements from March 2020 to April 2021. Of this cohort, n = 273 (87.2%) students were in centres with COVID-19 patients, n = 98 (31.3%) students identified these as mandatory clinical placements, and n = 215 (68.6%) students stated the rotations were voluntary during the pandemic period. The duration of the clinical placements were: 1–4 weeks (n = 115, 36.7%), 5–8 weeks (n = 60, 19.2%), 9–12 weeks (n = 63, 20.1%), more than 12 weeks (n = 75, 24.0%).
Responses regarding communication with students on placement since the start of COVID-19 pandemic were mixed. The vast majority were “Very Satisfied” n = 129 (36.7%) or “Satisfied” n = 86 (27.5%), n = 77 (24.6%) students were “Neither satisfied nor dissatisfied”, and only n = 19 (6.1%) were “Dissatisfied” or “Very Dissatisfied” n = 16 (5.1%).
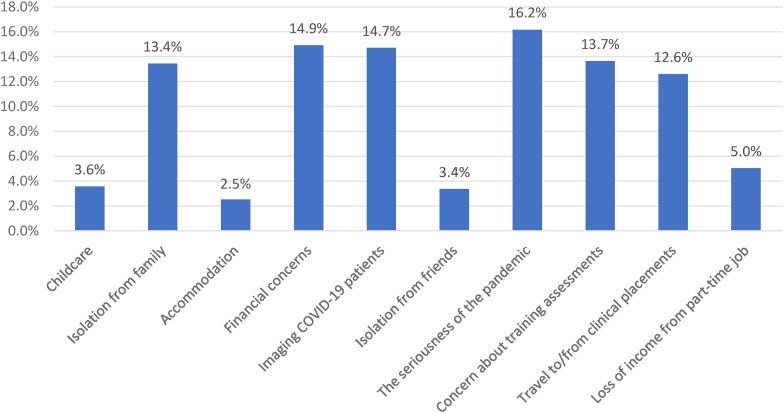
Most students who had been in clinical (213/313 students), said they were “Extremely confident” (n = 87, 27.8%) or “Very confident” (n = 126, 40.3%) in relation to the use of PPE whilst on placements. Of the remaining participants, n = 73 (23.3%) said they were “Somewhat confident”, n = 19 (6.1%) were “Not so confident”, and just n = 8 (2.6%) mentioned they were “Not at all confident”. Fig. 1 summarises the challenges experienced by students during the clinical placements.
Figure 1.
Challenges faced by students who underwent clinical placements during the studied pandemic period.
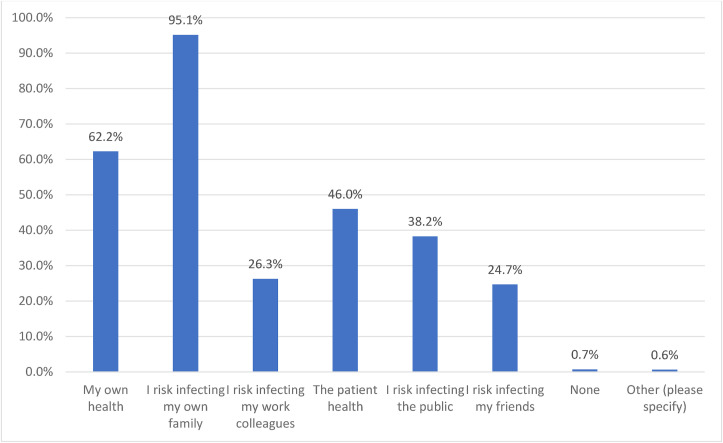
Students were asked if they had any concerns related to starting clinical placements during the pandemic. Only n = 30 (9.6%) students mentioned they were “Not at all worried”. The remainder expressed concern as “Extremely worried” (n = 73, 23.3%), “Very worried” (n = 82, 26.2%), “Somewhat worried” (n = 86, 27.5%), and “Slightly worried” (n = 42, 13.4%). Students were also asked if during these clinical placements they had become infected with the COVID-19; 28 students (8.9%) indicated they had developed COVID-19, the remainder declared that they had not been infected during the clinical placement period (n = 285, 91.0%). Fig. 2 presents the student responses when asked about their concerns related to the risk of infection whilst on clinical placements. An n = 1247 (95.2%) of the respondents indicated “the risk infecting my own family” and secondly “the risk of my own health” (n = 815, 62.2%) as their primary concerns.
Figure 2.
Concerns about infection risk when asked about clinical placement schedules during the pandemic of COVID-19. Percentage represents the total of students that marked that option as a concern, they were able to select three or more.
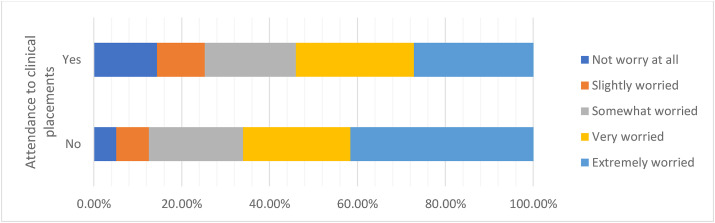
Student responses related to their worries about the impact of COVID-19 on future clinical placements were divided into those who had participated in clinical placements and those who had not (Fig. 3 ). Students who had not attended clinical placements showed a higher percentage in “Extremely worried” n = 415 (41.6%), compared to students with clinical placements experience n = 85 (27.2%)
Figure 3.
Summary of student concerns about the future of clinical placements due to COVID-19 in the cohorts who had attended clinical placements during the pandemic and the cohort who had not.
When asked if the COVID-19 pandemic had caused them to question whether they wished to be a radiographer, n = 294 (21.3%) said they were “Not at all worried”. The vast majority expressed concern as “Extremely worried” (n = 364, 27.8%), “Very worried” (n = 253, 19.3%), “Somewhat worried” (n = 234, 17.9%), and “Slightly worried” (n = 180, 13.7%). Students stated that they had spoken with family members and friends about their COVID-19 concerns, some stating they had discussed with their clinical tutors, lectures, other radiographers, and psychologists or medical doctors. However, n = 135 (10.3%) students indicated they had spoken to no one despite having concerns.
1296 students (98.9%) responded in relation to academic delivery during the pandemic and the main emerging themes identified are summarised in Table 2 . Direct response quotes, translated from Spanish, are provided as participant responses in Table 3 . When students were asked how confident they were that they had an appropriate support network outside the university n = 215 (16.4%) students said they were “Extremely confident” and n = 291 (22.2%) said “Very confident”. Of the remaining participants, n = 399 (30.5%) said they were “Somewhat confident”, n = 237 (18.1%) stated they were “Not so confident”, and n = 168 (12.8%) mentioned they were “Not at all confident”.
Table 2.
Main emerging themes related to concerns in the academic formation and their frequency in the open answers.
| Emerging theme | Number of mentions (% of total of students) |
|---|---|
| Concerns about the lack of clinical training | 626 (47.8%) |
| Issues with online learning | 434 (33.1%) |
| Fear of the virus and caused financial concerns | 161 (12.3%) |
| Delays to progression and graduation | 99 (7.5%) |
| The pandemic and its impact on mental health | 20 (1.5%) |
% represents the percentage of the total of students that mentioned the theme in their open answers. Some students mentioned more than one theme in their answer.
Table 3.
Representative student radiographer responses contained within main themes.
| Emerging theme | Representative responses |
| Concerns about lack of clinical training |
“My main concern is losing the clinical training, because it is so important for our formation as medical technologist.” “Because of the pandemic some institutions are not receiving students for their clinical training, thus we are forced to delay them and advance only with theoretical contents. For that reason, we can't reach the complete learning.” “The main concern is the reduction of practical skills in hospitals. The lack of attendance to clinical placements generates some doubts about my vocational interest with this academic program.” “I'm worried because if we don't have clinical training at the same time with the classes in theoretical contents, we can't deep in that knowledge and when we come back to the clinical training that contents will not be fresh and that can affect the clinical performance during the practice.” |
| Issues with online learning |
“Studying online is so different from doing it face-to-face because we have multiple distractions at home. We need the direct student-teacher interaction to enhance the contents.” “(…) some courses in online modality have less quality if we compare them with the in-face modality.” “It is hard for me to concentrate in the lessons and take it seriously when they are online.” “There is lower academic level in the online modality. The online classes don't reach a high academic standard.” |
| Fear of the virus and financial concerns |
“The online classes are complicated and not always clear, but I prefer the online modality instead of to go in-person to the university and be exposed to the Covid-19.” “[a concern for me is] not been able to pay for the semester in the University because of lack of money and not having a plate of food in the future for the economic impact that the country is having due to the pandemic.” “(…)get infected and bring the virus to my family and my workmates.” “I am afraid to get infected during the clinical rotations and bring the virus to my family.” |
| Delays to progression and graduation |
“[I am having a] delay in the academic plan and uncertainty about the next semesters.” “Not been able to finish my professional formation in the proposed period.” “I am concern that the time to finish the academic plan has been duplicated because of the pandemic.” “The clinical training has been affected because of the Covid-19 and that situation delays the academic plan.” |
| The pandemic and its impact on mental health |
“Other of my bigger concerns is my mental health, because of the online classes and the pandemic. Now I have anxiety attacks and lots of stress.” “I think that the quarantine has affected so much our mental health and motivation to study.” “It is frustrating and boring to be seated in an online class. I have never been so desperate.” |
Comparison of the domestic situation and health concerns with other responses
The respondents’ domestic situations were compared with the responses to the following three items: (1) Worry in advance of starting clinical placements undertaken between March 2020 to April 2021 (during the COVID-19 pandemic), (2) Worry in advance of future clinical placements and (3) Worry about being a radiographer. Student living with relatives were more likely to be “Extremely worried” and if family members had underlying health conditions a greater propensity to be “Extremely worried” about starting clinical placements was recorded (Table 4 ).
Table 4.
Comparison of domestic and health situations versus worry levels, in advance of starting clinical placements undertaken between March 2021 to April 2021 (during the COVID-19 pandemic).
| My situation | Extremely worried | Very worried | Somewhat worried | Slightly worried | Not worried at all | Total no. responses |
|---|---|---|---|---|---|---|
| A. I live alone | 3.8% (12) | 3.2% (10) | 3.2% (10) | 2.6% (8) | 1% (3) | 13.7% (43) |
| B. I live with university/college friends | 0.0% (0) | 1% (3) | 0.3% (1) | 0.6% (2) | 0.3% (1) | 2.2% (7) |
| C. I live with family members, but none have underlying conditions placing them at greater risk with COVID-19 | 7.7% (24) | 8.6% (27) | 12.1% (38) | 4.5% (14) | 5.1% (16) | 38% (119) |
| D. I live with family members who have underlying conditions placing them at greater risk with COVID-19 | 9.9% (31) | 11.5% (36) | 11.2% (35) | 4.8% (15) | 3.2% (10) | 40.6% (127) |
| E. I have an underlying condition placing me at greater risk with COVID-19 | 1.9% (6) | 1.9% (6) | 0.6% (2) | 1% (3) | 0.0% (0) | 5.4% (17) |
| F. I have more than one underlying condition placing me at greater risk COVID-19 | 0.0% (0) | 0.0% (0) | 0.0% (0) | 0.0% (0) | 0.0% (0) | 0.0% (0) |
| Total respondents | 23.3% (73) | 26.2% (82) | 27.5% (86) | 13.4% (42) | 9.6% (30) | 100.0% (313) |
Table 5 shows a similar distribution in terms of future clinical placements with students living with family members with a condition placing them at risk, with the highest number in the category of “Extremely worried” n = 223 (17%). Concerns about being a radiographer were lower than those stated in relation to current clinical placement rotations and were highest in the student cohort living with family members n = 161 (12.3%), despite underlying conditions not being present (Table 6 ).
Table 5.
Comparison of domestic and health situations versus worry levels, in advance of future clinical placements.
| My situation | Extremely worried | Very worried | Somewhat worried | Slightly worried | Not worried at all | Total no. responses |
|---|---|---|---|---|---|---|
| A. I live alone | 2.7% (36) | 1.1% (14) | 1.4% (18) | 0.3% (4) | 1.3% (17) | 6.8% (89) |
| B. I live with university/college friends | 0.9% (12) | 0.4% (5) | 0.0% (0) | 0.0% (0) | 0.3% (4) | 1.6% (21) |
| C. I live with family members, but none have underlying conditions placing them at greater risk with COVID-19 | 14.8% (194) | 10.2% (133) | 9.3% (122) | 3.5% (46) | 4% (52) | 41.8% (547) |
| D. I live with family members who have underlying conditions placing them at greater risk with COVID-19 | 17% (223) | 11.9% (156) | 9.9% (130) | 4.3% (56) | 1.7% (22) | 44.8% (587) |
| E. I have an underlying condition placing me at greater risk with COVID-19 | 2.1% (28) | 1.5% (19) | 0.6% (8) | 0.2% (2) | 0.1% (1) | 4.4% (58) |
| F. I have more than one underlying condition placing me at greater risk with COVID-19 | 0.5% (7) | 0.0% (0) | 0.1% (1) | 0.0% (0) | 0.0% (0) | 0.6% (8) |
| Total respondents | 38.2% (500) | 25% (327) | 21.3% (279) | 8.2% (108) | 7.3% (96) | 100.0% (1310) |
Table 6.
Comparison of domestic and health situations versus worry levels, about being a radiographer.
| My situation | Extremely worried | Very worried | Somewhat worried | Slightly worried | Not worried at all | Total no. responses |
|---|---|---|---|---|---|---|
| A. I live alone | 2.2% (29) | 1.2% (16) | 0.8% (11) | 0.7% (9) | 1.8% (24) | 6.8% (89) |
| B. I live with university/college friends | 0.5% (6) | 0.2% (3) | 0.3% (4) | 0.4% (5) | 0.2% (3) | 1.6% (21) |
| C. I live with family members, but none have underlying conditions placing them at greater risk with COVID-19 | 12.3% (161) | 7.5% (98) | 6.6% (87) | 6.2% (81) | 9.2% (120) | 41.8% (547) |
| D. I live with family members who have underlying conditions placing them at greater risk with COVID-19 | 11.5% (150) | 8.9% (117) | 8.8% (115) | 6% (79) | 9.6% (126) | 44.8% (587) |
| E. I have an underlying condition placing me at greater risk with COVID-19 | 1.1% (15) | 1.3% (17) | 1.2% (16) | 0.4% (5) | 0.4% (5) | 4.4% (58) |
| F. I have more than one underlying condition placing me at greater risk with COVID-19 | 0.2% (3) | 0.2% (2) | 0.1% (1) | 0.1% (1) | 0.1% (1) | 0.6% (8) |
| Total respondents | 27.8% (364) | 19.3% (253) | 17.9% (234) | 13.7% (180) | 21.3% (279) | 100.0% (1310) |
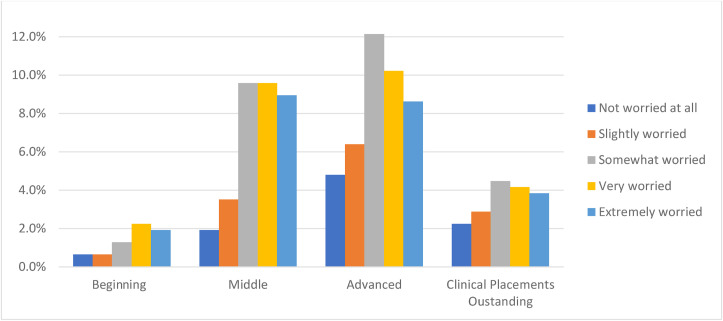
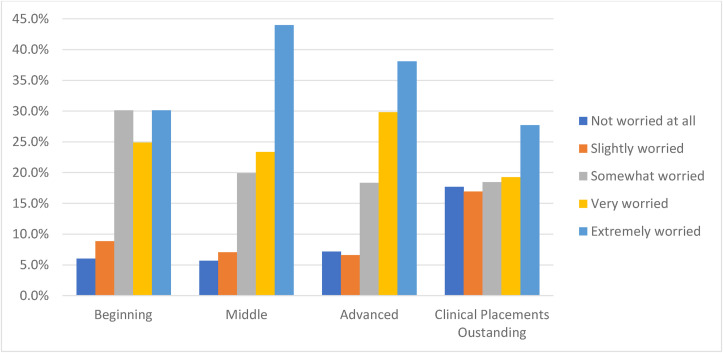
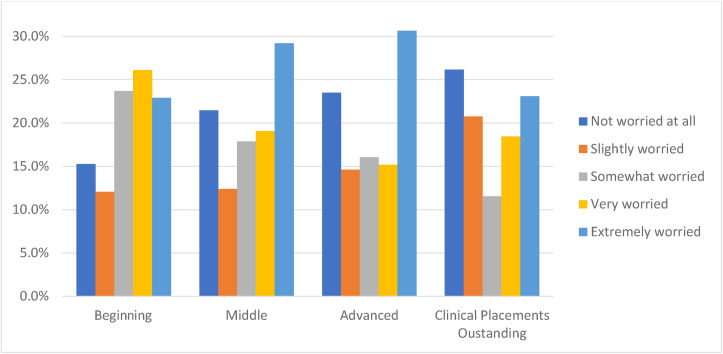
Comparison of respondent year groups with other responses
The responses from students who had attended clinical placements during March 2020 to April 2021 are summarised in Fig. 4 . The ‘Middle’ cohort reported the highest levels of concern due to starting clinical placements in three categories: “Extremely worried” (n = 256, 44%), “Very worried” (n = 136, 23.4%) and “Somewhat worried” (n = 116, 19.9%). The ‘Beginning’ cohort recorded similar levels of concern in top three categories, “Extremely worried” (n = 75, 30.1%), “Very worried” (n = 62, 24.9%) and “Somewhat worried” (n = 75, 30.1%). In ‘Advanced’ cohort, the majority n = 133 (38.1%) reported being “Extremely worried” with regard to resuming clinical placements, whilst students in the ‘Clinical Placement Outstanding’ category stated only n = 36 (27.7%) were “Extremely worried” (Fig. 5 ).
Figure 4.
Responses described by training level categorisations versus concerns related to being on clinical placements at the start of the COVID-19 pandemic. Percentage represents the level of worry of the total of students that were on clinical placements (n = 313) versus their level of training.
Figure 5.
Responses described by training level categorisations versus concerns related to future clinical placements. Percentage represents the level of worry of the total of students versus their level of training.
Fig. 6 depicts worry of becoming a radiographer depending on the stage in their programme and considering the impact on COVID-19 pandemic. For ‘Middle’ (n = 170, 29.2%) and ‘Advanced’ (n = 107, 30.7%) students the category “Extremely worried” received the highest values. Whilst in the second highest response students stated they were “Not worried at all” with ‘Middle’ (n = 125, 21.5%), and ‘Advanced’ (n = 82, 23.5%). In the case of ‘Beginning’ students, the highest was “Very worried” (n = 65, 26.1%) and the lowest “Slightly worried” (n = 30, 12%).
Figure 6.
Responses described by training level categorisations versus concerns about becoming a radiographer. Percentage represents the level of worry of the total of students versus their level of training.
Discussion
The study surveyed 1310 radiography students across thirteen Latin American universities. These universities were included in UNESCO data which reported the pandemic impacted education in more than 100 countries with total or partial closure of academic centres in all the participating countries.6 Across healthcare services internationally decisions were made as to whether healthcare students remained in clinical placements or not during the pandemic. One American paper identified how voluntary participation of medical students was advocated for in direct patient care.7 In Australia a similar response was taken due to the pandemic with the cessation of clinical practice represented concerns about student progression and potential workforce issues.8 These healthcare professional training concerns were replicated globally. Furthermore, the pandemic also impacted the amount of imaging procedures performed internationally, with centres reporting reductions of circa 50% of workflow in radiology services, which also impacted student training.9
Living situation
Our findings identified that n = 1221 (93.2%) participants lived with relatives during the months of study, and the majority n = 587 (44.8%) mentioned having a family member with at least one risk factor (Table 6) which are higher values when compared to 78.4% living with relatives and 25.7% living with a family member with a risk factor in the study by Rainford et al.4 This indicates that Latin American students are more likely to live with their families while attending university which concurs with a Peruvian study that identified that only 20% of the students originated from a different city.10 As stated by Astirbadi et al.,11 universities need to consider concerns about transmitting COVID-19 due to living conditions and our study demonstrates that the potential impact of this varies across countries. In this study 95.1% of students identified infecting family as a main worry, illustrating this impact.
Contracting COVID-19
Principal student concerns identified from the data included the seriousness of the pandemic and imaging COVID-19 patients (Fig. 1). The fear of infection was found to be similar to that reported in a study of American students who expressed their fear of interacting with infected patients, some even mentioned the constant pressure they felt whilst treating them.12 In one further study, 27.9% of 1830 medical students believed they were infected whilst on hospital rotations.13 In the study by Rainford et al.4 most students (87.8%) reported a concern related to the risk of infecting their family, versus 95.1% in the current study, and only 46.4% were worried about their health, versus 62.2% in the current study.
Personal protective equipment
Students that participated in clinical placements indicated being very or extremely confident (n = 213, 68.1% of the total) with the use of PPE. Instructions of use and recommendations given about the correct use of PPE is considered an important factor to make students safe in the clinical placements.11 , 14, 15, 16 The low number of students n = 28 (8.9%) who reported becoming affected by COVID-19 while on placement would indicate the correct use of protective measures. However, be noted that care should be taken when considering this figure outside the context of the prevalence rates, vaccination rates, and stage of the pandemic at the time of the survey or broader socioeconomic factors. The importance of PPE was highlighted in several studies with one stating that hospital staff were mainly worried about protective equipment shortage at the beginning of the pandemic.17 In an Italian study with 300 radiology residents, 66.7% indicated a correct use of PPE, social distancing, and hygienic prevention, and only 4.7% were infected by COVID-19.18
Financial concerns
Financial concerns due to COVID-19 were raised by radiography students in this work (Table 3) and across several published studies, for example, Rainford et al.4 identified the impact of students loosing part-time work on their ability to pay for travel and accommodation costs related to clinical training. Also, the impact of such loss of jobs, on their ability to contribute to support the family economic situation8 and/or financial difficulties to pay for medication19 are all concerns noted by medical students in relation to clinical placements during the pandemic.
Access to clinical placements
Only n = 313 (23.9%) of participants attended clinical placements during March 2020 and April 2021 highlighting the extent to which access to the clinical environment was limited. Many universities concentrated on theoretical activities20 and case simulations to replicate clinical activities in a virtual scenario.2 , 21 Students (n = 626, 47.8%) expressed concern about the lack of clinical training during the pandemic, with many students having their placements postponed. Those who had not attended clinical during the pandemic had expressed greater concern about their future careers in Radiography than those who had experienced clinical practice under COVID-19 conditions. In Costa Rica, an effort was made to provide virtual clinical placements, however, this approach was not effective.22 Also, postponed placements meant delayed graduation which was of concern12 and this remains an issue, despite some initiatives to support the progression of medical education were implemented, it is difficult to provide comparable experiences to pre-pandemic circumstances.23 , 24 ‘Advanced’ students reported increased levels of concern compared to those just starting their training. Our findings are divided regarding radiography as a career, with the majority n = 364 (27.7% of the total of students) indicating they were “Extremely worried” whilst n = 279 (21.3% of the total of students) were “Not worried at all”, substantially higher figures than those reported by Rainford et al.4 where only 4.2% said were “Extremely worried” and 35.4% indicated they were “Not at all worried”.
Academic delivery
The impact of the pandemic on academic delivery also requires consideration as many participants (n = 434, 33.1%) stated concerns in relation to online teaching and considered the provisions as insufficient to reach the expected learning with possible impact upon their graduating competencies. A recent Peruvian study25 identified students displaying an indifferent attitude in relation to online teaching with students feeling uncomfortable in that learning environment. The transition from scheduled, in-person, lessons to flexible home lessons utilising recordings for self-study with no fixed schedule was noted as problematic for some student learners.26 This may be exasperated by an inappropriate environment because distractions at home can impact student engagement and learning.26 Additionally, if staff are not fully trained to teach virtually, they may be unable to optimise teaching and learning under these conditions.27 , 28 A lack of appropriate technological resources to support teacher/student interactions (laptops, computers, tablets and smartphones), and the limited access to a high-speed internet connection could be factors contributing to the anxiety and stress among the students.25 Latin American countries have varied internet connections across and within states. According to the Economic Commission for Latin America and the Caribbean (ECLAC), only the 67% of habitants and 60% of the homes in the Latin American region use the internet with mobile broadband providing the bulk of services and fixed broadband at only 14%. Moreover, there are more than 40 million homes in Latin America with no internet connection, 50% being in the two economically poorest quintiles.29 This is similar for radiography students in Sri Lanka and South Africa, where the unavailability of devices and lack of network coverage put risk the equal access to online education.30 , 31
Student mental health
A further emerging theme is a relationship between the impact of the pandemic and the student's mental health. A mental health crisis among university students was reported before the beginning of the pandemic32 and a recent publication has described a worsening situation with increased levels of uncertainty, fear of death, loneliness, sadness, and irritability.33 Universities have the obligation to ensure student's studies progress using technologies and they also have responsibilities to support students with socio-emotional and/or health issues.
A recent Spanish study34 reported how the pandemic had affected student anxiety levels, cognitive empathy, with particular reference to sex, family circumstances, and their ability to use information technologies and communication methods. It found female students struggled to a greater extent at managing time and dealing with this new reality. The pandemic has limited face-to-face social interaction, increasing the anxiety and lowering empathy levels especially among young people.34 In a study of 107 radiologists, 75.7% of answers demonstrate that the pandemic has had a moderate or extreme negative impact on the morale of trainees with 74.8% reporting feelings of isolation.3 A further study, involving 316 American medical students, reported they felt anxious and vulnerable to COVID-1912 with the main causes of anxiety related to becoming infected or transmitting the virus to their relatives whilst sharing feelings and concerns in addition with being well informed can reduce the levels of stress in students. Graduation delays and insecurities about their learning during the pandemic resulted in perceived reduced competency levels in our study and can be related with the high level of anxiety as reported in previous studies.12 , 34
Student supports
University support mechanisms to minimise the impact of the pandemic on students’ mental health is critical, through psychological support programs, and student wellness departments that generate intervention plans, assistance, or educational advice to develop a healthy student career during these pandemic times.35 , 36 Though health professionals have been reported as showing a high prevalence of depression and anxiety during the pandemic.37 , 38 It has been reported that experienced radiographers seem to cope better than younger radiographers during the pandemic, reporting lowers effects on stress and anxiety.39 Additionally, whilst we need to be cognisant of how well students are adapting to new teaching and learning methods and how they are maintaining their health during the pandemic, these new challenges have potential positives as they develop the new competences and personal skills.33
In our study, only n = 135 (10.3%) of participants had not discussed their concerns with anyone, this is comparable with a higher amount of students (17.9%) reported by Rainford et al.4 Positively, n = 1175 (89.7%) of students considered it important to have someone to share their worries with. In addition, most students n = 399 (30.5%) indicated that they were “somewhat confident” with the support given by the university and indicated that university students were supported by friends and relatives in a greater way than by academic staff or clinically based healthcare professionals. This corresponds to what was reported by Rainford et al.,4 however, effective communication with academics can have a positive impact on students' wellness.21 Organisational communication mechanisms during COVID-19 were reported as difficult but, despite this, n = 115 (36.7%) participants were satisfied with the information and communication provided prior to the commencement of the clinical placements, only n = 16 (5.1%) felt disappointed. This compares with a 50% of satisfied students in the study by Rainford et al.4 and 23.5% “Dissatisfied” or “Very Dissatisfied”.
Limitations
Participating university response rates varied resulting in differences in student representation in each institution. Additionally constraining a time limit of twelve months may not represent the total experience of radiographer students in Latin America. Aspects like a previous participation in clinical placements at the beginning of the pandemic were not taken in consideration. A poor level of written expression among the students was noted exclusive of participants from Chile, Costa Rica and Uruguay which rendered review of open-ended questions difficult.
Conclusion
The full impact of COVID-19 on radiography education will not be known until the pandemic is declared to be at an end. Even then the impact of COVID-19 will likely be something that radiography students who graduate will carry throughout their careers. This study aimed to evidence the current impact of the pandemic on radiography students in Latin America. Student concerns with respect to becoming infected and/or risk to their family were found to be higher than international student cohorts mainly due to differences in living conditions in Latin America. Concerns about the quality of their learning during the pandemic, specifically related to the use of online teaching and learning were noted, with students perceiving online learning and the lack of guaranteed internet connectivity and computer equipment as problematic and requiring attention. Students were identified as being more open to discuss their concerns with third parties compared to student cohorts in similar studies which is important as higher anxiety levels were noted in related to across several matters including financial stability, accessing clinical placements and achieving acceptable competency levels when compared to other radiography cohorts.
Funding declaration
The corresponding author of this work has been supported in undertaking the research by the Universidad de Costa Rica (Grant number: 424-C1-186).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.radi.2022.06.003.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Ferrel M.N., Ryan J.J. The impact of COVID-19 on medical education. Cureus. 2020;12(3):10–12. doi: 10.7759/cureus.7492. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Virarkar M., Jensen C., Javadi S., Saleh M., Bhosale P.R. Radiology education amid COVID-19 pandemic and possible solutions. J Comput Assist Tomogr. 2020;44(4):472–478. doi: 10.1097/RCT.0000000000001061. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Robbins J.B., England E., Patel M.D., DeBenedectis C.M., Sarkany D.S., Heitkamp D.E., et al. COVID-19 impact on well-being and education in radiology residencies: a survey of the association of program directors in radiology. Acad Radiol. 2020;27(8):1162–1172. doi: 10.1016/j.acra.2020.06.002. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rainford L.A., Zanardo M., Buissink C., Decoster R., Hennessy W., Knapp K., et al. The impact of COVID-19 upon student radiographers and clinical training. Radiography. 2021;27(2):464–474. doi: 10.1016/j.radi.2020.10.015. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duque H., Aristizábal Díaz-Granados E.T. Análisis fenomenológico interpretativo : Una guía metodológica para su uso en la investigación cualitativa en psicología. Pensando Psicol. 2019;15(25):1–24. doi: 10.16925/2382-3984.2019.01.03. Available from: [DOI] [Google Scholar]
- 6.United Nations Educational . Education: From disruption to recovery. UNESCO; 2021. Scientific and cultural organization (UNESCO)https://enunescoorg/covid19/educationresponse#schoolclosures [cited 2021 November 27]. Available from: [Google Scholar]
- 7.Whelan A., Prescott J., Young G., Catanese V., McKinney R. AMMC; 2020. Guidance on medical students' participation in direct in-person patient contact activities.https://www.aamc.org/news-insights/press-releases/important-guidance-medical-students-clinical-rotations-during-coronavirus-covid-19-outbreak [cited 2021 November 27] Available from: [Google Scholar]
- 8.Sharma D., Bhaskar S. Addressing the covid-19 burden on medical education and training: the role of telemedicine and tele-education during and beyond the pandemic. Front Public Health. 2020;8(November;1–14 doi: 10.3389/fpubh.2020.589669. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cavallo J.J., Forman H.P. The economic impact of the COVID-19 pandemic on radiology practices. Radiology. 2020;296(3):E141–E144. doi: 10.1148/radiol.2020201495. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Angulo-Giraldo M., Quispe-Díaz A., Requena-Calderón M. Migración, autoidentificación y religión: los estudiantes de la Facultad de Letras y ciencias humanas (Universidad Nacional mayor de San Marcos) Praxis (Bern 1994) 2019;15(2):207–221. doi: 10.21676/23897856.3250. Available from: [DOI] [Google Scholar]
- 11.Astirbadi D., Lockwood P. COVID-19: a literature review of the impact on diagnostic radiography students. Radiography. 2021;28(2):553–559. doi: 10.1016/j.radi.2021.09.009. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gallagher T., Schleyer A.M. We signed up for this!” - student and trainee responses to the covid-19 pandemic. N Engl J Med. 2020;96(1):1969–1973. doi: 10.1056/NEJMp2005234. Available from. [DOI] [PubMed] [Google Scholar]
- 13.Bani Hani A., Alaridah N., Abu Abeeleh M., Shatarat A., Rayyan R., Kamal A., et al. Medical students and risk of COVID-19 infection: a descriptive cross-sectional study from the University of Jordan. Ann Med Surg [Internet] 2021;70 doi: 10.1016/j.amsu.2021.102775. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alvin M.D., George E., Deng F., Warhadpande S., Lee S.I. The impact of COVID-19 on radiology trainees. Radiology. 2020;296(2):246–248. doi: 10.1148/radiol.2020201222. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mossa-Basha M., Medverd J., Linnau K.F., Lynch J.B., Wener M.H., Kicska G., et al. Policies and guidelines for COVID-19 preparedness: experiences from the university of Washington. Radiology. 2020;296(2):E26–E31. doi: 10.1148/radiol.2020201326. Available from: [DOI] [PubMed] [Google Scholar]
- 16.Has-Heger T., Pook C., Kirkman M., Simmonds S. Healthcare students' experience of personal protective equipment shortages during COVID-19. J Clin Nurs. 2021:1–2. doi: 10.1111/jocn.16108. 00. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen Q., Liang M., Li Y., Guo J., Fei D., Wang L., et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet. 2020;7:e15–e16. doi: 10.1016/S2215-0366(20)30078-X. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cavalieri S., Spinetta M., Zagaria D., Franchi M., Lavazza G., Nardelli F., et al. The impact of COVID-19 pandemic on radiology residents in Northern Italy. Eur Radiol. 2021;31(9):7077–7087. doi: 10.1007/s00330-021-07740-0. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nguyen H.T., Do B.N., Pham K.M., Kim G.B., Dam H.T.B., Nguyen T.T., et al. Fear of COVID-19 scale—associations of its scores with health literacy and health-related behaviors among medical students. Int J Environ Res Publ Health. 2020;17(11):1–14. doi: 10.3390/ijerph17114164. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abreu L., León R., García J. Pandemia de COVID-19 y educación médica en Latinoamérica. FEM. 2020;23(5):237–242. doi: 10.33588/fem.235.1088. Available from: [DOI] [Google Scholar]
- 21.Velazque L., Valenzuela C., Murillo F. Pandemia COVID-19 : repercusiones en la educación universitaria. Odontología Sanmarquina. 2020;23(2):203–205. doi: 10.15381/os.v23i2.17766. 2020;23(2):203–206. Available from: [DOI] [Google Scholar]
- 22.Guevara S. Semanario Universidad.; 2021. Estudiantes de carreras de salud piden un regreso paulatino a sus campos clínicos y prácticas.https://semanariouniversidad.com/universitarias/estudiantes-de-carreras-de-salud-piden-un-regreso-paulatino-a-sus-campos-clinicos-y-practicas-presenciales/ [cited 2021 November 28]. Available from: [Google Scholar]
- 23.Ahmed H., Allaf M., Elghazaly H. COVID-19 and medical education. Lancet Infect Dis. 2020;20:777–778. doi: 10.1016/S1473-3099(20)30226-7. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rose S. Medical student education in the time of COVID-19. JAMA, J Am Med Assoc. 2020;323(21):2131–2132. doi: 10.1001/jama.2020.5227. Available from: [DOI] [PubMed] [Google Scholar]
- 25.Estrada Araoz E.G., Gallegos Ramos N.A., Mamani Uchasara H.J., Huaypar Loayza K.H. vols. 1–19. 2020. (Actitud de los estudiantes universitarios frente a la educación virtual en tiempos de la pandemia de COVID-19. Rev Bras Educ do Campo). Available from: [DOI] [Google Scholar]
- 26.Teo L., Pang T., Ong Y., Lai C. Coping with COVID-19: perspective of student radiographers. J Med Imag Radiat Sci. 2020:358–360. doi: 10.1016/j.jmir.2020.05.004. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Appolloni A., Colasanti N., Fantauzzi C., Fiorani G., Frondizi R. Distance learning as a resilience strategy during covid-19: an analysis of the Italian context. Sustainability. 2021;13:1388. doi: 10.3390/su13031388. Available from: [DOI] [Google Scholar]
- 28.Humphrey E., Wiles J. Lessons learned through listening to biology students during a transition to online learning in the wake of the COVID-19 pandemic. Ecol Evol. 2021;11:3450–3458. doi: 10.1002/ece3.7303. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Economic Commission for Latin American and the Caribbean (ECLAC) 2020. Universalizar el acceso a las tecnologías digitales para enfrentar los impactos del COVID-19. Observatorio COVID-10 en América Latina y el Caribe. Impacto Económico y Social.https://www.cepal.org/sites/default/files/presentation/files/final_final_covid19_digital_26_agosto.pdf CEPAL. [cited 2021 Novembre 30]. Available from: [Google Scholar]
- 30.Chandrasiri N., Weerakoon B. Online learning during the COVID-19 pandemic: perceptions of allied health sciences undergraduates. Radiography. 2022;28(2):545–549. doi: 10.1016/j.radi.2021.11.008. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gumede L., Badriparsad N. Online teaching and learning through the students' eyes- Uncertainty through the COVID-19 lockdown: a qualitative case study in Gauteng province, South Africa. Radiography. 2022;28:193–198. doi: 10.1016/j.radi.2021.10.018. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alarcón R. La salud mental de los estudiantes universitarios. Editorial Rev Med Hered. 2019;30:219–221. doi: 10.20453/rmh.v30i4.3655. Available from: [DOI] [Google Scholar]
- 33.Cobo-Rendón R., Vega-Valenzuela A., García-Álvarez D. Consideraciones institucionales sobre la Salud Mental en estudiantes universitarios durante la pandemia de Covid-19. CienciAmérica. 2020;9(2):277. doi: 10.33210/ca.v9i2.322. Available from: [DOI] [Google Scholar]
- 34.Íñiguez-Berrozpe T., Lozano-Blasco R., Quílez-Robres A., Cortés Pascual A. Universitarios y Confinamiento. Factores Socio-personales que Influyen en sus Niveles de Ansiedad y Empatía. Rev Int Educ para la Justicia Soc. 2020;9(3):301–316. doi: 10.15366/riejs2020.9.3.016. Available from: [DOI] [Google Scholar]
- 35.Martínez D., Navarrete J., Montero J. Feasibility, effectiveness, and mechanisms of a brief mindfulness- and compassion-based program to reduce stress in university students: a pilot randomized controlled trial. Int J Environ Res Publ Health. 2022;19 doi: 10.3390/ijerph19010154. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Modrego M., López Y., García J., Pérez A., Navarro M., Beltrán M., et al. Efficacy of a mindfulness-based programme with and without virtual reality support to reduce stress in university students: a randomized controlled trial. Behav Res Ther. 2021;142 doi: 10.1016/j.brat.2021.103866. [DOI] [PubMed] [Google Scholar]
- 37.Da Silva R., Rodrigues C., De Medeiros P., Rolim M. Psychological effects caused by the COVID-19 pandemic in health professionals: a systematic review with meta-analysis. Prog Neuro-Psychopharmacol Biol Psychiatry. 2021:104. doi: 10.1016/j.pnpbp.2020.110062. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sahebi A., Nejati B., Moayedi S., Yousefi K., Torres M., Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Prog Neuro-Psychopharmacol Biol Psychiatry. 2021;107 doi: 10.1016/j.pnpbp.2021.110247. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yasin B., Barlow N., Milner R. The impact of the Covid-19 pandemic on the mental health and work morale of radiographers within a conventional X-ray department. Radiography. 2021;27:1064–1072. doi: 10.1016/j.radi.2021.04.008. Available from: [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.