Abstract
Background
COVID-19 vaccines are considered to be a vital tool in controlling the pandemic. Hesitation with COVID-19 immunization has been reported worldwide. The acceptability of the COVID-19 vaccine among health care workers (HCWs) is an important step in determining the success of any new vaccination program. This study aims to estimate the acceptability of COVID-19 vaccines among HCWs in Oman.
Methods
A cross-sectional study using a self- administered questionnaire was conducted among HCWs in December 2020. Data were analyzed using a bivariate level to identify the statistical association with acceptability using the Chi-squared test. At the multivariate level, we determined the socio-demographic and knowledge factors associated with vaccine acceptability.
Results
A total of 608 out of 700 HCWs participated (response rate 87 %), of which 64.8 % were Oman citizens and 53.8 % were aged between 30 and 39 years. The majority of the participants were female (62.8 %) and married (87.0 %), while 48.5 % of the respondents were doctors. Only 43 % of the participants were willing to be vaccinated against COVID-19, while 57 % were either uncertain 35 % or unwilling 22 % to be vaccinated. The main reason for not being willing to receive the vaccine was their perceived adverse events after vaccination. The male participants (OR: 1.96 95 % CI 1.22–3.13) and those with a positive attitude towards the vaccine (OR: 9.17(95 %) CI-1.78–47.07) were more willing to receive the COVID-19 vaccine. Similarly, trust in the government (OR: 2.41 95 % CI 1.57–3.71) and having sound knowledge of the COVID-19 vaccine (OR: 15.91 95 % CI 9.81–25.88) improved the acceptability to vaccinate among the HCWs. In contrast, having a previous experience with SARS-CoV-2 (OR: 1.65, 95 % CI: 1.08–2.54), was associated with a significant decrease in COVID-19 vaccine acceptability.
Conclusion
50 % of HCWs reported being uncertain or unwilling to be vaccinated against the COVID-19 vaccine. Male gender, positive attitude towards the vaccines, trust in government and knowledge of COVID-19 vaccine as key factors that determine improved vaccine acceptability among HCWs. Therefore, to facilitate herd immunity among the population, it is necessary to initiate effective communication strategies among HCWs in order to sensitize them towards the acceptability of the COVID-19 vaccine.
Keywords: COVID-19, COVID-19 vaccine, Acceptability, Oman, Health care workers, HCWs
Introduction
The COVID-19 pandemic, caused by a new Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), has created an extraordinary burden for healthcare systems across the globe [1].
The first two COVID-19 cases in Oman were reported on February 24, 2020, and they were linked to travel to the Islamic Republic of Iran [2]. By April 31, 2022, the total number of laboratory-confirmed COVID-19 patients reported and cured will have reached 389,460, with a mortality rate of 1.1 % [3]. Oman was one of the first countries to respond to COVID-19 control and prevention by implementing social distancing, lockdown, public health awareness, and behavioral change programs, and the implementation was quick and consistent through out.
As vaccines are considered to be the most functional and cost-effective public healthcare interventions for preventing transmissible/communicable diseases [4], COVID-19 vaccine is an integral component of a long-term and effective public health strategy to contain SARS-CoV-2 in addition to non-pharmaceutical interventions (NPIs). To date, more than 267 COVID-19 vaccine candidates are in different phases of pre-clinical and clinical development with 13 vaccines approved and being used under Emergency Use Authorization (EUA) in different countries worldwide [5].
In October 2020, Oman's Ministry of Health announced that the COVID-19 vaccine would be publicly available. Subsequently, the national COVID-19 vaccination campaign was launched in January 2021 first using the Pfizer®/BioNTech vaccine. The original target groups for the vaccination campaign included high-risk groups such as front-line healthcare workers (HCW) and the elderly. HCWs are potential victims of the disease and consequently spreaders due to increased rates of exposure [6]. Protecting HCWs from SARS-CoV-2 infection is beneficial for them, their social contacts and patients and is therefore crucial for the preservation, protection and smooth functioning of the entire healthcare system. Therefore, the acceptance and uptake of the COVID-19 vaccine among HCWs plays a major role in combating this pandemic.
There are many misconceptions and wrong impressions amongst HCWs with respect to the COVID-19 vaccine [7]. The massive amount of online information available on COVID-19 and its vaccines can potentially influence decision-making and recommendation-making behaviors of the HCWs [8]. The World Health Organization (WHO) identified vaccine hesitancy amongst the top ten threats for global health in 2019 [9]. Vaccine hesitancy refers to a delay in acceptance or complete refusal of vaccination despite its availability [8]. There are many misconceptions amongst HCWs with respect to the COVID-19 vaccine [5], [7]. The massive amount of online information available on COVID-19 and its vaccines can potentially influence decision-making and recommendation-making behaviors of HCWs [6], [10]. This study aims to evaluate the opinions of HCWs regarding COVID-19 immunization, specifically whether or not they would accept the vaccine and also recommend the vaccine to others, with a view to provide recommendations to the Ministry of Health in Oman to inform outreach programs.
Methods
Study setting
Oman is located in the south-eastern corner of the Arabian Peninsula with sea coasts that extend 3165 km from the Strait of Hormuz and whose borders include Yemen to the south, and the Kingdom of Saudi Arabia and United Arab Emirates to the west. The country has a population of nearly 5 million out of which 39 % are foreign-born individuals (non-citizens). Out of the total, 2.739.954 (61.3 %) are males and 1.731.194 (38.7 %) are females [11]. Oman is one of 22 countries located within the Eastern Mediterranean Region (EMR) of the World Health Organization (WHO).
Study design and population
This study is an observational cross-sectional questionnaire based study that queried all available and consenting HCWs working at government and private health facilities in Oman.
The sample size was 700, with a margin of error of 3 % and a 95 % confidence interval, based on the conservative assumption that the level of acceptability of 50 %.
The survey will take 10–12 min to complete. The study's participation was purely voluntary. Prior to answering the survey questions, participants were needed to express informed permission.
Data collection and analysis
A questionnaire was developed and distributed using SurveyMonkey™. The questionnaire was organized in four sections: (1) demographic information; (2) general knowledge of COVID-19; (3) awareness, attitudes and behaviors related to the COVID-19 vaccine; and (4) perception or confidence in the government with respect to handling the COVID-19 crisis and the vaccination campaign. The expected outcome variable was willingness to be vaccinated.
Nine questions were used to evaluate awareness of COVID-19 in general, eight related to awareness of the COVID-19 vaccine. Four questions were used to assess attitude towards the vaccine and three questions assessed trust in the government and perceptions towards the government's responses to manage the COVID-19 crisis and provide up-to-date information on COVID-19 vaccine development and its introduction in Oman.
The questionnaire was pilot tested with 11 healthcare workers from Muscat Governorate to assess its coherence and clarity, and no significant modification of the questionnaire was required. The actual study was conducted in the third week of December 2020, using a self-administered anonymous questionnaire in English language. The participants were able to provide consent at the time of participation in the study before answering the questionnaire. The questionnaire was distributed online through a unique link by the Ministry of Health, Oman, and data were collected in the password encrypted SurveyMonkey platform. Data were analyzed using SPSS version 26.
Descriptive analysis
Socio-demographic data is summarized as categorical variables and disaggregated in terms of willingness to take the vaccine (Yes, No, Uncertain (Not sure)) and presented as a frequency table.
Responses were categorized as binary (True/False; Yes/No) or as scale (Strongly Agree, Agree, Neutral, Disagree or Strongly Disagree). Participants' responses were disaggregated according to their willingness to be vaccinated and presented in the form of frequency tables.
Analytical statistics
The knowledge and attitude score was calculated by giving a score of one or zero according to the nature of the question. For binary responses, the correct answer was given a score of 1. For binary analysis, the median score served as the cut-off point. For binary analysis, the median score served as the cut-off point of seven for COVID-19 knowledge, whilst 100 % score was used for attitude and perception. For scale variables related to attitude, questions were scored as one or zero depending on the response. For COVID-19 awareness (scoring more than seven versus less than seven), whilst for other variables, the median scores were corresponded to 100 %. Un-adjusted odds ratios were initially calculated. To control for confounding and interactions, only p-value< 0.2 variables were included in the multivariate analysis.
Patient and public involvement statement
-
•
At what stage in the research process were patients/public first involved in the research and how? The questionnaires were sent randomly to the Healthcare workers. The participants were involved during the data collection and questionnaire validation phase of the study.
-
•
How were the research question(s) and outcome measures developed and informed by their priorities, experience, and preferences? The questions and outcome measures were developed after reviewing multiple study literatures on COVID-19 vaccine acceptance globally taking into account the Oman context. In addition, input from the research team was also taken into consideration during the planning and implementation phase of the research study.
-
•
How were patients/public involved in the design of this study? The participants were asked to fill the online questionnaire sent to them randomly.
-
•
How were they involved in the recruitment to and conduct of the study? The questionnaires were sent randomly and participants were asked to provide the consent before answering the questionnaire.
-
•
Were they asked to assess the burden of the intervention and time required to participate in the research? The information on the burden of the intervention as well as estimated time to answer the questionnaire was provided in the consent form which was attached to the questionnaire.
-
•
How were (or will) patients and the public be involved in choosing the methods and agreeing plans for dissemination of the study results to participants and wider relevant communities.The study results will be communicated to the hospitals which were involved in the study and the Ministry of Health Oman is provided with the preliminary results of the study.
Results
Socio-demographic characteristics
A total of 608 out of 700 HCWs participated in the study (response rate 87 %). The majority of participants were Omani nationals (64.8 %; n = 394) and 30 % (n = 183) were from Muscat Governorate. Of the participants, 62.8 % (n = 382) were female, 87 % (n = 539) were married, 89.6 % (n = 545) were under 50 years of age, 71.7 % (n = 436) had a bachelor's or higher degree, 83.9 % (n = 510) were doctors or nurses and 69.6 % (n = 423) were employed in a primary health care facility.
One hundred and eighty two (28.3 %) of the participants were previously infected with SARS-CoV-2, whilst 56 % (n = 342) were actively treating COVID-19 patients ( Table 1).
Table 1.
Socio-demographic characteristics of healthcare workers participating in the study (n = 608).
| Characteristics | Willing to receive COVID-19 vaccine |
Total participants | |||
|---|---|---|---|---|---|
| Yes n (%) | No n (%) | Not sure yet n (%) | n (%) | ||
| Age | |||||
| 20–29 | 17 (6 %) | 13 (10 %) | 22 (10 %) | 52 (9 %) | |
| 30–39 | 137 (52 %) | 69 (53 %) | 121 (57 %) | 327 (54 %) | |
| 40–49 | 78 (30 %) | 40(30 %) | 48 (23 %) | 166 (27 %) | |
| 50–59 | 27 (10 %) | 8 (6 %) | 22 (10 %) | 57 (9 %) | |
| ≥ 60 | 5 (2 %) | 1 (1 %) | 0 | 6 (1 %) | |
| Gender | |||||
| Male | 144 (55 %) | 29 (22 %) | 53 (25 %) | 226 (37 %) | |
| Female | 120 (45 %) | 102 (78 %) | 160 (75 %) | 382 (62.8 %) | |
| Marital status | |||||
| Married | 237 (90 %) | 110 (84 %) | 182 (85 %) | 529 (87 %) | |
| Single | 27 (10 %) | 21 (16 %) | 31 (15 %) | 79 (13 %) | |
| Nationality | |||||
| Omani | 142 (54 %) | 108 (83 %) | 144 (68 %) | 394 (64,8 %) | |
| Non-Omani | 122 (46 %) | 23 (17,6 %) | 69 (32 %) | 214 (35,2 %) | |
| Highest educational level | |||||
| Diploma | 59 (22 %) | 46(35 %) | 67 (31 %) | 172 (28,3 %) | |
| Completed bachelors | 115 (44 %) | 50 (38 %) | 94 (44 %) | 259 (42,6 %) | |
| Completed masters | 56 (21 %) | 20 (15 %) | 33 (15 %) | 109 (17,9 %) | |
| Specialist | 24 (9 %) | 9 (7 %) | 14 (7 %) | 47 (7,7 %) | |
| Doctorate | 10 (4 %) | 6 (5 %) | 5 (2 %) | 21 (3,5 %) | |
| Job Title | |||||
| Doctor | 158 (60 %) | 50 (38 %) | 88 (41 %) | 296 (48 %) | |
| Nurse | 53 (20 %) | 45 (34 %) | 84(39 %) | 214 (35 %) | |
| Pharmaceutical | 11 (4 %) | 11(4 %) | 10(5 %) | 12 (2 %) | |
| Public health staff | 3(1 %) | 0(0 %) | 3(1 %) | 6 (1 %) | |
| Paramedic | 9(3 %) | 11 (8 %) | 12 (6 %) | 32 (5 %) | |
| Midwives | 2 (1 %) | 5 (4 %) | 5 (2 %) | 12 (2 %) | |
| Other | 28(11 %) | 9(7 %) | 11 (5 %) | 48 ( 7 %) | |
| Governorate | |||||
| Muscat | 68(26 %) | 45(34 %) | 70(33 %) | 183 (30 %) | |
| Al-Dhahirah | 7(3 %) | 6(5 %) | 4(2 %) | 17 (2 %) | |
| South Al-Batinah | 51 (19 %) | 20(15 %) | 38(18 %) | 109 (18 %) | |
| Musandam | 5(4 %) | 29(11 %) | 11(5 %) | 45 (7 %) | |
| Al-Buraymi | 3 (2 %) | 3(1 %) | 3(1 %) | 9 (1 %) | |
| North Al-Batinah | 16(6 %) | 8(6 %) | 11 (5 %) | 35 (6 %) | |
| Al-Dakhiliyah | 12 (5 %) | 8(6 %) | 13 (6 % | 33 (5 %) | |
| North Al-Sharqiyah | 15 (6 %) | 10 (8 %) | 5(2 %) | 30 (5 %) | |
| South Al-Sharqiyah | 5(2 %) | 4(3 %) | 14(7 %) | 23 (4 %) | |
| Dhofar | 49(19 %) | 20(15 %) | 39(18 %) | 108 (18 %) | |
| Al Wusta | 9(3 %) | 2(1 %) | 5(2 %) | 30 (4 %) | |
| Type of health facility | |||||
| Primary | 185 (70 %) | 94 (72 %) | 144(68 %) | 423 (70 %) | |
| Secondary | 48(18 %) | 14(11 %) | 37(17 %) | 99 (16 %) | |
| Tertiary | 31 (12 %) | 23(18 %) | 32 (15 %) | 86 (14 %) | |
| Infected with SARS-CoV-2 before | |||||
| No | 198 (75 %) | 95 (72 %) | 143 (67 %) | 436 (72 %) | |
| Yes confirmed | 30(11 %) | 16 (12 %) | 33 (15 %) | 79 (12 %) | |
| Yes suspected | 12 (4 %) | 6 (5 %) | 17 (8 %) | 58 (10 %) | |
| Not sure | 24 (9 %) | 14(11 %) | 20(9 %) | 35 (6 %) | |
| Treating COVID-19 patients | |||||
| Yes | 149 (56 %) | 76 (58 %) | 117 (55 %) | 342 (56 %) | |
| No | 115 (44 %) | 55 (42 %) | 94 (44 %) | 264 (43 %) | |
Willingness to take COVID-19 vaccine
Two hundred and sixty four (43 %) participants state that they were willing to take a COVID-19 vaccine. Of the participants willing to take the vaccine 59 % (n = 134) were below 39 years of age, 55 % (n = 144) were males, 90 % (n = 237) were married, 54 % (n = 142) were Omani nationals, 78 % (n = 205) had completed a bachelors or higher degree, 80 % (n = 211) were either nurses or doctors, 70 % (n = 185) were working at primary healthcare facilities; 56 % (n = 149) were treating COVID-19 patients and 75 % (n = 198) were not previously infected with SARS-CoV-2 (Table 1).
The majority of the participants 57 % (n = 344;) were either not sure (uncertain) 35 % (n = 213) or unwilling (answering No) 22 % (n = 131) to receive a vaccine. Total number of responses were 608;Yes: 43 % (n = 264); No: 22 % (n = 131); Not sure: 35 % (n = 213).
Of the participants who were hesitant (either not sure (uncertain) or unwilling (answering No)) to receive the vaccine 57 % (n = 344;); 55 % (n = 190) were between the ages of 30 and 39 years, 76 % (n = 262) were female, 85 % (n = 292) were married, 73 % (n = 252) were citizens of Oman, 67 % (n = 237) had an undergraduate degree or higher education, 78 % (n = 267) were physicians and nurses, and 68 % (234) worked in primary care facilities, 69 % (n = 238) had not previously been infected with COVID-19 %, and 56 % (n = 193) were currently treating patients with COVID-19 (Table 1).
There was sufficient awareness about COVID-19 / SARS-CoV-2 among the participants. However, 45 % (n = 271) were unfamiliar with the similarity between SARS-CoV-2 and MERS-CoV, 34 % (n = 206) believed there was a significant stigma associated with the acquisition of COVID-19, 13.5 % (n = 82) were of the view that COVID-19 was not a critical illness for them, 6 % (n = 39) did not consider COVID-19 to be a serious illness for their family and 10 % (n = 59) believed it was not a condition that requires serious attention ( Table 2).
Table 2.
Participants’ knowledge and attitude towards COVID-19 and willingness to receive COVID-19 vaccine (Yes, No, Not sure) (n = 587).
| Variables | Willing to receive COVID 19 vaccine |
Total population |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes |
No |
Unsure |
|||||||
| N | % | N | % | N | % | N | % | ||
| COVID-19 spreads via respiratory droplets of infected population. | |||||||||
| TRUE | 256 | 42 % | 124 | 20 % | 207 | 34 % | 587 | 97 % | |
| FALSE | 7 | 1 % | 8 | 1 % | 4 | 1 % | 19 | 1 % | |
| Person with COVID-19 cannot transmit the virus to others when fever is absent. | |||||||||
| TRUE | 8 | 1 % | 9 | 1 % | 17 | 3 % | 34 | 6 % | |
| FALSE | 256 | 42 % | 122 | 20 % | 194 | 32 % | 572 | 94 % | |
| Corona virus (SARS-C0V-2) is similar to SARS-COV and MERS-CoV | |||||||||
| TRUE | 143 | 24 % | 76 | 13 % | 113 | 19 % | 332 | 55 % | |
| FALSE | 117 | 19 % | 55 | 9 % | 98 | 16 % | 270 | 45 % | |
| There is no effective therapeutic cure for COVID-19 yet. | |||||||||
| TRUE | 232 | 38 % | 109 | 18 % | 182 | 30 % | 523 | 86 % | |
| FALSE | 31 | 5 % | 22 | 4 % | 29 | 5 % | 82 | 14 % | |
| All my activities will be disrupted if I get ill with COVID-19. | |||||||||
| Strongly agree | 122 | 20 % | 26 | 4 % | 75 | 12 % | 233 | 39 % | |
| Agree | 84 | 14 % | 36 | 6 % | 61 | 10 % | 181 | 30 % | |
| Neutral | 25 | 4 % | 25 | 4 % | 33 | 5 % | 83 | 14 % | |
| Disagree | 27 | 4 % | 28 | 5 % | 37 | 6 % | 92 | 15 % | |
| Strongly disagree | 6 | 1 % | 5 | 1 % | 4 | 1 % | 15 | 2 % | |
| I am worried that I might experience stigma if i get ill with COVID-19. | |||||||||
| Strongly agree | 23 | 4 % | 11 | 2 % | 17 | 3 % | 51 | 8 % | |
| Agree | 63 | 10 % | 26 | 4 % | 66 | 11 % | 155 | 26 % | |
| Neutral | 51 | 8 % | 20 | 3 % | 39 | 6 % | 110 | 18 % | |
| Disagree | 56 | 9 % | 28 | 5 % | 47 | 8 % | 131 | 22 % | |
| Strongly disagree | 45 | 7 % | 70 | 12 % | 41 | 7 % | 156 | 26 % | |
| COVID-19 is a serious disease for me. | |||||||||
| Strongly agree | 91 | 15 % | 28 | 5 % | 60 | 10 % | 179 | 30 % | |
| Agree | 101 | 17 % | 32 | 5 % | 92 | 15 % | 225 | 37 % | |
| Neutral | 49 | 8 % | 33 | 5 % | 37 | 6 % | 119 | 20 % | |
| Disagree | 18 | 3 % | 31 | 5 % | 19 | 3 % | 68 | 11 % | |
| Strongly disagree | 4 | 1 % | 7 | 1 % | 3 | 0 % | 14 | 2 % | |
| COVID-19 is a serious disease for my family. | |||||||||
| Strongly agree | 46 | 8 % | 136 | 22 % | 110 | 18 % | 292 | 48 % | |
| Agree | 97 | 16 % | 45 | 7 % | 69 | 11 % | 211 | 35 % | |
| Neutral | 22 | 4 % | 23 | 4 % | 19 | 3 % | 64 | 11 % | |
| Disagree | 7 | 1 % | 12 | 2 % | 11 | 2 % | 30 | 5 % | |
| Strongly disagree | 2 | 0 % | 5 | 1 % | 2 | 0 % | 9 | 1 % | |
| COVID-19 is not a disease that needs serious attention. | |||||||||
| Strongly agree | 11 | 2 % | 2 | 0 % | 4 | 1 % | 17 | 3 % | |
| Agree | 7 | 1 % | 23 | 4 % | 12 | 2 % | 42 | 7 % | |
| Neutral | 14 | 2 % | 19 | 3 % | 15 | 2 % | 48 | 8 % | |
| Disagree | 92 | 15 % | 45 | 7 % | 73 | 12 % | 210 | 35 % | |
| Strongly disagree | 140 | 23 % | 41 | 7 % | 107 | 18 % | 288 | 48 % | |
Eighty-seven percent of participants (n = 526) had received seasonal influenza immunizations in the past five years and 96 % (n = 583) were aware that the Government of Oman was planning to introduce the COVID-19 vaccine in the country. 87 % (n = 531) of the participants believed that they were at risk of contracting COVID-19. Half of the participants (50 % (n = 307)) were of the view that the vaccine could protect them from COVID-19, 57 % (n = 344) believed that the vaccine could protect their families from acquiring COVID-19 %, and 63 % (n = 386) were of the opinion that the vaccine could prevent complications associated with COVID-19 ( Table 3).
Table 3.
Participants’ knowledge and attitude towards COVID-19 vaccine and vaccination and willingness to receive COVID-19 vaccine (Yes, No and Not sure) (n = 526).
| Variables | Willing to receive COVID 19 vaccine |
Total population |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Yes |
No |
Unsure |
||||||||
| n | % | n | % | n | % | n | % | |||
| Have you receive influenza vaccine during the last five years? | ||||||||||
| Yes | 236 | 39 % | 105 | 17 % | 185 | 30 % | 526 | 87 % | ||
| No | 28 | 5 % | 26 | 4 % | 28 | 5 % | 82 | 13 % | ||
| Are you aware that Oman is planning for the introduction of COVID-19 vaccine once available in coming months? | ||||||||||
| Yes | 259 | 43 % | 124 | 20 % | 200 | 33 % | 583 | 96 % | ||
| No | 5 | 1 % | 7 | 1 % | 11 | 2 % | 23 | 4 % | ||
| COVID-19 vaccination can protect me from getting infected by SARS-CoV-2. | ||||||||||
| Strongly agree | 83 | 14 % | 0 | 0 % | 10 | 2 % | 93 | 15 % | ||
| Agree | 136 | 22 % | 18 | 3 % | 60 | 10 % | 214 | 35 % | ||
| Neutral | 31 | 5 % | 57 | 9 % | 115 | 19 % | 203 | 33 % | ||
| Disagree | 10 | 2 % | 39 | 6 % | 19 | 3 % | 68 | 11 % | ||
| Strongly disagree | 4 | 1 % | 17 | 3 % | 7 | 1 % | 28 | 5 % | ||
| COVID-19 vaccination will protect my family as well if they are also vaccinated. | ||||||||||
| Strongly agree | 96 | 16 % | 1 | 0 % | 15 | 2 % | 112 | 19 % | ||
| Agree | 139 | 23 % | 20 | 3 % | 73 | 12 % | 232 | 38 % | ||
| Neutral | 250 | 41 % | 59 | 10 % | 109 | 18 % | 193 | 32 % | ||
| Disagree | 4 | 1 % | 35 | 6 % | 13 | 2 % | 52 | 9 % | ||
| Strongly disagree | 0 | 0 % | 15 | 2 % | 1 | 0 % | 16 | 3 % | ||
| One of the ways to prevent COVID-19 complication is through COVID-19 vaccination. | ||||||||||
| Strongly agree | 106 | 18 % | 2 | 0 % | 17 | 3 % | 125 | 21 % | ||
| Agree | 141 | 24 % | 23 | 4 % | 94 | 16 % | 258 | 44 % | ||
| Neutral | 45 | 8 % | 10 | 2 % | 84 | 14 % | 123 | 21 % | ||
| Disagree | 7 | 1 % | 39 | 7 % | 12 | 2 % | 58 | 10 % | ||
| Strongly disagree | 0 | 0 % | 21 | 4 % | 4 | 1 % | 25 | 4 % | ||
Perception on COVID-19 vaccine
One hundred and thirty-four participants (22 %) believed that they will not contract COVID-19 after immunization, whilst 35 % (n = 215) of the respondent’s believed that COVID-19 prevention using non pharmaceutical interventions is much better than to be vaccinated and 18 % (n = 106) stated that the COVID-19 vaccine would not yield any benefit to them since they were healthy ( Table 4).
Table 4.
Participants’ attitude towards COVID-19 vaccine and vaccination and trust in the government and willingness to receive COVID-19 vaccine (Yes, No and Not sure).
| Variables | Willing to receive COVID 19 vaccine |
Total population |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Yes |
No |
Unsure |
||||||||
| n | % | n | % | n | % | n | % | |||
| I am worried about the safety of COVID-19 vaccine. | ||||||||||
| Strongly agree | 10 | 2 % | 80 | 13 % | 71 | 12 % | 161 | 27 % | ||
| Agree | 88 | 15 % | 39 | 6 % | 95 | 16 % | 222 | 37 % | ||
| Neutral | 81 | 13 % | 6 | 1 % | 37 | 6 % | 124 | 20 % | ||
| Disagree | 67 | 11 % | 6 | 1 % | 8 | 1 % | 81 | 13 % | ||
| Strongly disagree | 18 | 3 % | 0 | 0 % | 0 | 0 % | 18 | 3 % | ||
| I am worried that there will be side effects after COVID-19 vaccination. | ||||||||||
| Strongly agree | 9 | 1 % | 78 | 13 % | 70 | 12 % | 157 | 26 % | ||
| Agree | 94 | 16 % | 40 | 7 % | 102 | 17 % | 236 | 39 % | ||
| Neutral | 104 | 17 % | 8 | 1 % | 30 | 5 % | 142 | 24 % | ||
| Disagree | 43 | 7 % | 2 | 0 % | 9 | 1 % | 54 | 9 % | ||
| Strongly disagree | 13 | 2 % | 2 | 0 % | 0 | 0 % | 15 | 2 % | ||
| I believe COVID-19 disease prevention method naturally is much better than to be vaccinated (with COVID-19 vaccine). | ||||||||||
| Strongly agree | 6 | 1 % | 57 | 9 % | 20 | 3 % | 83 | 14 % | ||
| Agree | 28 | 5 % | 33 | 5 % | 66 | 11 % | 127 | 21 % | ||
| Neutral | 70 | 12 % | 28 | 5 % | 80 | 13 % | 178 | 29 % | ||
| Disagree | 120 | 20 % | 9 | 1 % | 40 | 7 % | 169 | 28 % | ||
| Strongly disagree | 40 | 7 % | 4 | 1 % | 5 | 1 % | 49 | 8 % | ||
| I value the importance of vaccine and vaccination more now after the onset of COVID-19 pandemic. | ||||||||||
| Strongly agree | 105 | 22 % | 6 | 1 % | 28 | 6 % | 139 | 30 % | ||
| Agree | 104 | 22 % | 19 | 4 % | 75 | 16 % | 198 | 42 % | ||
| Neutral | 11 | 2 % | 43 | 9 % | 46 | 10 % | 100 | 21 % | ||
| Disagree | 3 | 1 % | 16 | 3 % | 4 | 1 % | 23 | 5 % | ||
| Strongly disagree | 1 | 0 % | 6 | 1 % | 1 | 0 % | 8 | 2 % | ||
| My government is handling the COVID-19 crisis very well. | ||||||||||
| Strongly agree | 77 | 16 % | 24 | 5 % | 49 | 10 % | 150 | 32 % | ||
| Agree | 100 | 21 % | 36 | 8 % | 75 | 16 % | 211 | 45 % | ||
| Neutral | 35 | 7 % | 17 | 4 % | 27 | 6 % | 79 | 17 % | ||
| Disagree | 9 | 2 % | 8 | 2 % | 4 | 1 % | 21 | 4 % | ||
| Strongly disagree | 3 | 1 % | 5 | 1 % | 1 | 0 % | 9 | 2 % | ||
| I valued the importance of vaccine and vaccination before the COVID-19 pandemic as well. | ||||||||||
| Strongly agree | 105 | 22 % | 6 | 1 % | 28 | 6 % | 139 | 30 % | ||
| Agree | 104 | 22 % | 19 | 4 % | 75 | 16 % | 198 | 42 % | ||
| Neutral | 11 | 2 % | 43 | 9 % | 46 | 10 % | 100 | 21 % | ||
| Disagree | 3 | 1 % | 16 | 3 % | 4 | 1 % | 23 | 5 % | ||
| Strongly disagree | 1 | 0 % | 6 | 1 % | 1 | 0 % | 8 | 2 % | ||
| My government provides transparent and up-to-date information on COVID-19 vaccine development and its introduction in the Sultanate of Oman. | ||||||||||
| Strongly agree | 90 | 19 % | 25 | 5 % | 46 | 10 % | 161 | 34 % | ||
| Agree | 109 | 23 % | 31 | 7 % | 68 | 14 % | 208 | 44 % | ||
| Neutral | 22 | 5 % | 18 | 4 % | 33 | 7 % | 73 | 15 % | ||
| Disagree | 3 | 1 % | 11 | 2 % | 8 | 2 % | 22 | 5 % | ||
| Strongly disagree | 1 | 0 % | 5 | 1 % | 1 | 0 % | 7 | 1 % | ||
| I trust the government on COVID-19 vaccination planning and introduction. | ||||||||||
| Strongly agree | 99 | 21 % | 10 | 2 % | 36 | 8 % | 145 | 31 % | ||
| Agree | 114 | 24 % | 31 | 7 % | 74 | 16 % | 219 | 47 % | ||
| Neutral | 10 | 2 % | 29 | 6 % | 44 | 9 % | 83 | 18 % | ||
| Disagree | 1 | 0 % | 15 | 3 % | 0 | 0 % | 16 | 3 % | ||
| Strongly disagree | 0 | 0 % | 5 | 1 % | 2 | 0 % | 7 | 1 % | ||
In addition, 63 % (n = 385) of participants expressed concern over the safety of COVID-19 vaccines and 65 % (n = 395) of participants were concerned about adverse events following COVID-19 immunization (Table 4).
The majority of participants 77 % (n = 361) had a positive perception towards the government’s strategy on handling the COVID-19 crisis, 78 % (n = 364) were confident in the government's strategic planning and introduction of COVID-19 immunization, and 78 % (n = 369) were satisfied with the seamless and up-to-date information provided by the government on the development of the COVID-19 vaccine and its introduction (Table 4).
Seventy-two percent 72 % (n = 337) of participants appreciated the importance of immunization prior to the COVID-19 pandemic, and this number remained consistent following the COVID-19 crisis as well (Table 4).
Reasons for willingness and not willing to receive COVID-19 vaccine
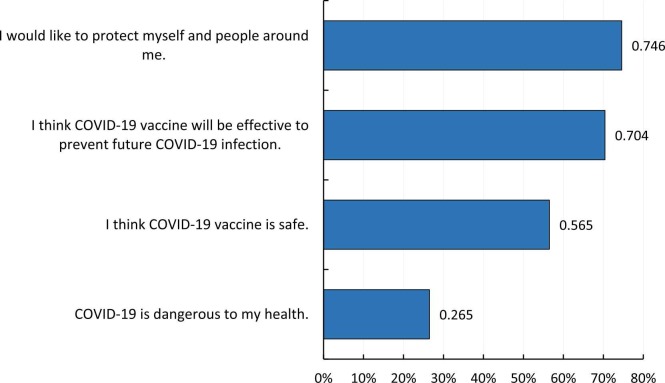
One of the major reasons for the participants’ willingness to accept COVID-19 vaccine was their sense of social responsibility, as stated by almost three-quarter of the participants (74.6 %) that they would like to protect themselves and their families by getting vaccinated against COVID-19. Moreover, 70.4 % of the participants believed that COVID-19 vaccine could be effective in preventing future COVID-19 spread ( Fig. 1).
Fig. 1.
Bar graph showing different reasons for acceptance of COVID-19 vaccine among the study participants (n = 260). Note: The total percentage is not 100 % since this was a multiple response question and was analyzed using multiple response analysis.
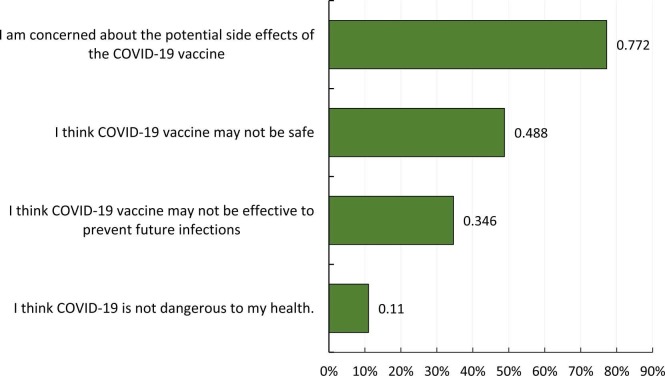
In contrast, concerns about the potential side effects of COVID-19 vaccination was the main reason why participants (77.2 %) did not accept the COVID-19 vaccine, and doubts on vaccine safety were also highlighted by almost half of the participants (48.8 %) ( Fig. 2).
Fig. 2.
Bar graph representing various reasons for not willing and not sure to receive COVID-19 vaccine among the study participants (n = 246). Note: The total percentage is not 100 % since this was a multiple response question and was analyzed using multiple response analysis.
Recommendation of COVID-19 vaccine, vaccine efficacy criteria
Out of 471 participants, 76.6 % (n = 361) stated that they would recommend the COVID-19 vaccine to their patients, whilst 68.6 % (n = 323) would recommend COVID-19 vaccine to their family members (Table 3). Bivariate analysis showed that there was no association between participants’ willingness to receive COVID-19 vaccine and recommending the vaccine to their patients, but participants who were willing to receive COVID-19 vaccine were also likely to recommend the vaccine to their family members (OR: 162.79; 95 % CI: 39.54–670.23) (Table 4).
Above three-quarter of the participants (360/471; 76.4 %) emphasized that they would receive and recommend the COVID-19 vaccine if its efficacy is proven to be ≥ 80 %. Only15 % (n = 71) and 8.5 % (n = 40) of the participants indicated that they would receive the vaccine with 50–80 % efficacy and irrespective of vaccine efficacy respectively. Bivariate analysis revealed that participants who would receive/recommend a 50–80 % effective vaccine were more likely to accept the COVID-19 vaccine (p-value: 0.02; OR: 2.56; 95 % CI: 1.15–5.68) compared to those who would accept/recommend the vaccine irrespective of the efficacy data. However, there was no association between willingness to receive/recommend ≥ 80 % effective vaccine with the acceptance of COVID-19 vaccine (p-value: 0.29; OR: 1.44; 95 % CI: 0.74–2.82).
Source of information on COVID-19, COVID-19 vaccine and vaccination, and communication on COVID-19 vaccination
Social media was the main source of information on COVID-19, COVID-19 vaccine and vaccination for the study participants (Friedman’s test; mean rank: 3.03), followed by scientific journals (mean rank: 3.27). Workplace was the third major source of information among the study participants (mean rank: 3.41). The Ministry of Health’s website (mean rank: 3.79) and fellow colleagues (mean rank: 4.08) were listed as the least frequent source of information on COVID-19 ( Table 5 ).
Table 5.
Sources of information on COVID-19, COVID-19 vaccine and vaccination.
| Source of information | Friedman's test (mean rank) | Rank |
|---|---|---|
| Social Media (Facebook, Twitter, LinkedIn, Instagram) | 3.03 | 1st |
| Scientific Journals | 3.27 | 2nd |
| Workplace | 3.41 | 3rd |
| Radio, Television, Newspaper | 3.42 | 4th |
| Ministry of Health website | 3.79 | 5th |
| Fellow colleagues | 4.08 | 6th |
Note: Least mean rank implies the major information source.
Participants emphasized that direct counseling would be the most suitable way for communication and spreading awareness on COVID-19 vaccination in Oman, followed by Television and social media platforms. Newspapers and posters/leaflets/brochures were categorized as the least appropriate communication channel.
Out of 471 participants, the majority of the participants stated that it is necessary to communicate on COVID-19 vaccine safety (73.9 % (n = 348)), efficacy (75.8 % (n = 357)) and benefits-risk associated with the vaccine (75.2 % (n = 354)). Around 65 % (n = 306) emphasized that the importance of COVID-19 vaccination to mitigate the spread of the disease should also be communicated.
Predictors for COVID-19 vaccine acceptance
In determining the predictors for COVID-19 vaccine our hypothesis was that there would be no difference to willingness to intake the COVID 19 vaccine by gender, age, nationality and Government trust.
Males (OR: 3.82; 95 % CI: 2.66–5.49), participants with completed bachelors or higher education degrees (OR: 1.70; 95 % CI: 1.16–2.51), good knowledge of the COVID-19 vaccine (OR: 1.73; 95 % CI: 1.23–2.43), positive attitudes towards vaccines (OR: 19.31; 95 % CI: 4.76–168.49) and higher trust in the government (OR: 3.05; 95 % CI: 2.16–4.32) were significantly more likely to take the COVID-19 vaccine. However, Omani nationals (OR 0.42; 95 % CI: 0.30–0.66) were less likely than non-Omani nationals to take the vaccine. Males (OR: 1,96 95 % CI (1,22−3,13)), positive attitude towards the vaccine (OR: 9,17(95 %) CI-1,78–47,07), trust in the government (OR: 2,41 95 %CI 1,57–3,71) and sound knowledge of COVID-19 vaccine (OR: 15,91 95 %CI 9,81–25,88))** remained significant positive predictors of the COVID-19 vaccine uptake after multivariate logistic regression analysis ( Table 6).
Table 6.
Multinominal logistic regression and binary logistic regression of willingness to get vaccinated vs different variables.
| Statistical analysis | Bivariate | Multivariate |
|---|---|---|
| Outcomes | Will vaccinate | Will vaccinate |
| Variables | OR (95 % confidence interval) | OR (95 % confidence interval) |
| Age | ||
| ≤ 39 versus ≥ 39 years | 0,74 (0,53–1,05) | 1,04(0,65–1,65) |
| Gender | ||
| Males versus females | 3,82(2,66–5,49)** | 1,96(1,22–3,13)* |
| Marital status | ||
| Married versus single | 1,57(0,93–2,68) | 1,93(0,98–3,03) |
| Nationality | ||
| Omani versus non Omani | 0,42(0,30–0,66)** | 0,68(0,41–1,12) |
| Education | ||
| Completed Bachelors/Masters/Doctorate/Specialist versus Diploma | 1,70(1,16–2,51)** | 0,96(0,56–1,57) |
| Occupation | ||
| Clinician (Doctor; Nurse) versus Allied Health & Others | 1,01(0,66–1,56) | |
| Type of facility | ||
| Primary versus Secondary/Tertiary | 1,05(0,73–1,51) | |
| Infected with SARS previously | ||
| Yes versus No | 0,71(,73–1,51) | 1,00(0,56–1,75) |
| Recommend COVID-19 vaccine to patients | ||
| Yes versus No | ||
| Recommend COVID-19 vaccine to family members | ||
| Yes versus No | 162,79(39,54–670,23)** | 605,29(134,48–2724,37)** |
| Knowledge of COVID-19 | ||
| ≥ 7 versus ≤ 7 | 1,73(1,23–2,43)* | 1,25(0,81–1,93) |
| Knowledge of COVID-19 vaccine | ||
| Score ≥ 8 versus score ≤ 8 | 20,04(12,50–32,54)** | 15,91(9,81–25,88)** |
| Trust on Government | ||
| Score ≥ 3 versus score ≤ 3 | 3,05(2,16–4,32)** | 2,41(1,57–3,71)** |
| Attitude towards COVID-19 vaccine | ||
| Attitude score ≥ 4 versus attitude score ≤ 4 | 19,31(4,76–168,49)* * | 9,17(1,78–47,07)* |
Note: P < 0.05* P < 0.001**.
Participants who were previously infected with COVID-19 were less willing to take the COVID-19 vaccine (OR: 1.59; 95 %CI: 1.02–2.45). In addition participants with a positive attitude towards COVID-19 vaccination (OR: 9.17; 95 % CI: 1.78–47.07) were significantly more likely to accept the COVID-19 vaccine (Table 6).
Discussions
The COVID-19 vaccine is a vital tool in responding to the ongoing pandemic [12]. Current evidence shows that COVID-19 immunization reduces the risk of contracting a serious SARS-CoV-2 infection and its associated hospitalization and mortality [13].
Achieving collective/herd immunity is vital to the impact of the COVID-19 vaccine on the population as well as to control the pandemic. It is therefore essential, at an early stage of vaccine deployment, to determine the potential factors associated with reluctance to receive the COVID-19 vaccine, in such a way that the communication and health promotion strategy can be altered or strengthened.
HCWs who are reluctant to receive the COVID-19 vaccine should undergo counseling to understand the source of the hesitation if we are to mitigate harm in the workplace and obtain collective immunity. The Centre for Disease Control recommended that healthcare workers be amongst the first group in any country to be vaccinated against COVID-19 [14]. These data are based on HCWs who may be exposed to COVID-19 while caring for and treating patients, and HCWs who are likely to transmit the virus to patients during treatment contact [3].
Successful deployment of HCW vaccination may have a positive impact on the general acceptability and uptake of vaccination among the local population. Additionally, a positive attitude from HCWs toward COVID-19 vaccination and a high uptake rate of the COVID-19 vaccine is likely to influence the decision of patients to be vaccinated [6].
Low levels of COVID-19 vaccine acceptance in HCWs can have a negative impact on the general population, since HCWs who are willing to receive the vaccine are more likely to recommend vaccination to patients and their families [15]. This is also a worrisome situation given the front line position of healthcare workers in the fight against the spread of the COVID-19 pandemic, serving those most at risk of serious complications related to COVID-19 [16].
Previous research has shown that HCWs intending to be vaccinated plan to recommend the vaccine to family and friends which aligns with the findings in our study [15].
The willingness of HCWs to be vaccinated against COVID-19 was 43 % in Oman. Findings from this study contradict findings from other studies conducted through self-administered surveys in 6 countries: China, India, Indonesia, Singapore, Vietnam and Bhutan on willingness to vaccinate, which showed that over 95 % of HCWs surveyed in those countries were willing to receive the COVID-19 vaccine. [13] A survey of HCWs in France, French-speaking Belgium and Quebec, Canada, demonstrated 72.4 % acceptance for COVID-19 vaccination among healthcare workers [17].
In addition, the willingness to be vaccinated is lower in our study as compared to a survey conducted at the State University of New York (SUNY), New York, amongst HCWs where a 57.5 % willingness to take the COVID-19 vaccine was observed. This result is similar to a survey conducted amongst HCWs, comprising physicians and administrative health care assistants in Poland showing a 54.3 % willingness to be vaccinated against COVID-19 [18].
The willingness to be vaccinated is lower in our study as compared to studies conducted among HCWs in Saudi Arabia where 50.5 % and 65 % were willing to receive the COVID-19 vaccine [19], [20]. Furthermore, an online survey conducted across Middle Eastern Region via social marketing indicated that 62.4 % (n = 543) of the participants would accept COVID-19 vaccine if it became available free of charge [21]. In contrast our findings are higher than the 25 % willing to receive a vaccine and 33 % being hesitant as reported via a self-administered questionnaire was distributed through social media applications in four Arab countries (Jordan, Saudi Arabia, Lebanon, and Iraq) [22]. The willingness to be vaccinated is higher in our study than in an analytical cross-sectional study among 23 congolese referral hospitals, including three university hospitals, located in three towns indicating that only 27.7 % of HCWs were willing to accept the COVID-19 vaccination [23].
Males were more willing to accept COVID-19 vaccination and this has been consistently shown in other studies [23], [24], [25]. The increased willingness for COVID-19 vaccine uptake amongst males could be due to their positive perception of the underlying risks, as a number of reports have shown higher risks for COVID-19 complications, infectivity and death among males than females [26].
In our study HCWs with good knowledge of COVID-19 (OR: 1.73; 95 % CI: 1.23–2.43) and the vaccine (OR 15,91(9.81–25.88)) were more willing to be vaccinated against COVID-19. Knowledge of both COVID-19 and the vaccination is important in influencing a decision to take the COVID-19 vaccine. This was also found in a study in Vietnam in two general hospitals that indicated HCWs with good knowledge had a 3.37 more likely odds to accept COVID-19 vaccines [27].
Similar to other studies our study found that HCWs with positive perception towards the COVID-19 vaccination and trust in the government’s strategies were more willing to receive the COVID-19 vaccination. A six nation study in Asia showed that those willing to be vaccinated were more likely to “have trust in the country’s public healthcare system/government competency” (p-value < 0.001); 2) belief that the “country’s public healthcare system/government has responded effectively to the COVID-19 pandemic”, and participants willing to vaccinate were more likely to believe that the “country’s public healthcare system/government has provided honest information/been transparent about the COVID-19 pandemic to the public” (p-value = 0.014) [28].
The above findings highlight the importance of appropriate communication by the relevant authorities to build trust and confidence towards the vaccination program. In the current era of easy access to social media, a comprehensive and transparent strategy that encompasses explanations of how vaccines work, how they are developed, importance of vaccines in controlling the pandemic, the time needed to reach an effective level (requirement of multiple doses), contingency management plans in situations of unexpected health adverse effects, and the importance of herd immunity is essential firstly for healthcare workers and then to the general population. Moreover, additional training and awareness programs and supportive supervision on COVID-19 vaccine and vaccination programs can be implemented to boost the confidence of healthcare workers.
Limitations
The is a cross-sectional study, which does not allow the assessment of causality. Second, the questionnaires were self-administered due to the strict infection control measures in all participating institutions. Therefore, the information obtained is subject to self reporting bias. Furthermore, the mode of communication was through WhatsApp® and email and it is assumed that most healthcare workers in Oman have access to this platform. The findings are not generalizable to the general public given that the healthcare workers’ perception and risk profile of the pandemic differ. In addition, the COVID-19 vaccine acceptance among Oman's HCWs is predicted to have altered between data collection and publication of the findings. The existing research shows that vaccination acceptance changes between subgroups of the community and over time, possibly due to a shift in vaccine perceptions, increased or decreased faith in COVID-19 vaccine, or increased or decreased trust in health authorities/government.
Conclusions
To the best of our knowledge, this is the first study of its kind focusing on HCWs in Oman regarding COVID-19 vaccination. Despite many prevailing concerns regarding the COVID-19 vaccine, 43 % of HCWs in Oman are willing to receive the COVID-19 vaccine. Participants outlined the social responsibility of protecting themselves and people around them as the main reason to accept the COVID-19 vaccine, whereas the major reason for not willing to receive the vaccine was the concern about the potential side-effects of COVID-19 vaccination. Males HCWs, having a good knowledge of the COVID-19 disease, COVID-19 vaccination, positive attitude and good government perception of handling the COVID-19 pandemic were positive predictors of willingness to take the vaccine. The above determinants demonstrate the need for a comprehensive, clear, fact-based and transparent communication to the HCWs to increase the uptake as well as to improve the recommendation behavior of HCWs towards COVID-19 vaccine.
Previous Presentations Statement
None.
Patient consent for publication
Not required.
Funding
No funding was received for this study.
Ethics approval
Ethical approval for this study was granted from the National Oman Ethical Committee (#MoH/CSR/20/24135). This study does not contravene the internal institutional review board and follows the Declaration of Helsinki.
CRediT authorship contribution statement
All authors were involved during the planning of this study. STA, HA, MK, AA, SA and CD conceptualized the project and conducted initial background research, STA, HA, AA, SA and OM planned and conducted the formal analysis and validation, STA, OM, HA, AA and SA interpreted the results, STA led the writing (original draft and editing) of the manuscript, STA, HA, MK, AA, SA and OM write the manuscript STA, CD, HA and MK supervised the project. All authors approved the final article.
DMG was registered in the EMJMD LIVE (Erasmus+ Mundus Joint Master Degree Leading International Vaccinology Education), co-funded by Universitat de Barcelona, Universitat Autónoma de Barcelona, Universiteit Antwerpen, Université Jean Monnet de Saint-Etienne, Université Claude Bernard Lyon 1 (Coordinator), European commission (EACEA-2018-1484), Sanofi Pasteur, Institut Mérieux, IDEXLYON of Université de Lyon in the frame of “Investissements d′avenir” (ANR-16-IDEX-0005 Project, and received a scholarship from the EACEA.
Provenance and peer review
Not commissioned; nor externally peer reviewed conducted.
Competing interests
None declared.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.jiph.2022.06.005.
Appendix A. Supplementary material
Supplementary material
Data availability statement
The data are available from the correspondence author upon reasonable on request.
References
- 1.World Health Organization. Coronavirus disease (COVID-19): looking back at a year that changed the world: WHO’s response to COVID-19. 〈https://www.who.int/emergencies/diseases/novel-coronavirus-2019/strategies-and-plans〉, [Accessed 20 April 2021].
- 2.Khamis Faryal, Al Rashidi Badria, Al-Zakwani Ibrahim, et al. Epidemiology of COVID-19 infection in Oman: analysis of the first 1304 cases. Oman Med J. 2020;35(3) doi: 10.5001/omj.2020.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coronavirus WHO, EMR. (COVID-19) Dashboard. 〈https://app.powerbi.com/view?r=eyJrIjoiN2ExNWI3ZGQtZDk3My00YzE2LWFjYmQtNGMwZjk0OWQ1MjFhIiwidCI6ImY2MTBjMGI3LWJkMjQtNGIzOS04MTBiLTNkYzI4MGFmYjU5MCIsImMiOjh9〉, [Accessed 30 April 2022].
- 4.World Health Organization. Vaccines and immunization. 〈https://www.who.int/health-topics/vaccines-and-immunization?adgroupsurvey={adgroupsurvey}&gclid=Cj0KCQjw9_mDBhCGARIsAN3PaFPrgJ5A4kzR9_G4ouHcOuDXaohIL_NbsHG3–34B9zqWjdF6Wo7_CvMaAiW1EALw_wcB#tab=tab_1〉, [Accessed 13 April 2021].
- 5.World Health Organization. Draft landscape and tracker of COVID-19 candidate vaccines. 〈https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines〉, [Accessed 14 April 2021].
- 6.World Health Organization. Health workers exposure risk assessment and management in the context of COVID-19 virus. 〈https://apps.who.int/iris/bitstream/handle/10665/331340/WHO-2019-nCov-HCW_risk_assessment-2020.1-eng.pdf〉, [Accessed 15 April 2021].
- 7.Loomba S., de Figueiredo A., Piatek S.J., et al. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat Hum Behav. 2021;5:337–348. doi: 10.1038/s41562-021-01056-1. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. Coronavirus disease (COVID-19): Vaccines [Internet]. Who.int.; 2020. 〈https://www.who.int/news-room/q-a-detail/coronavirus-disease-(covid-19)-vaccines?adgroupsurvey={adgroupsurvey}&gclid=Cj0KCQjwseDBhC7ARIsAI8YcWIyh4HOQI3v0PkLxLk2XabPccSD2i8UruzrrtgqtaE9MdleoSn_PY0aAsnVEALw_wcB〉, [Accessed 18 April 2021].
- 9.World Health Organization. Ten health issues WHO will tackle this year [Internet]. Who.int.; 2019. 〈https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019〉, [Accessed 18 April 2021].
- 10.Report of the SAGE working group on vaccine hesitency; 2004. 〈https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf〉, [Accessed 19 April 2021].
- 11.National Center for Statistics & Information. 〈https://data.gov.om/OMPOP2016/population?indicator=1000140®ion=1000020-muscat&nationality=1000020-expatriate-non-omani〉, [Accessed 2 May 2021].
- 12.WHO, COVID-19 vaccines. 〈https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines〉, [Accessed 22 May 2021].
- 13.Doshi P. Will covid-19 vaccines save lives? Current trials aren’t designed to tell us. BMJ. 2020;371:m4037. doi: 10.1136/bmj.m4037. [DOI] [PubMed] [Google Scholar]
- 14.CDC’s COVID-19 Vaccine Rollout Recommendations. 〈https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations.html〉, [Accessed 13 July 2021].
- 15.Shekhar R., Sheikh A.B., Upadhyay S., et al. COVID-19 vaccine acceptance among healthcare workers in the United States. Vaccines. 2021;9(2) doi: 10.3390/vaccines9020119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nguyen, LH, Drew, DA, Joshi, AD, et al. Risk of COVID-19 among frontline healthcare workers and the general community: a prospective cohort study. medRxiv: the preprint server for health sciences; 2020, 2020.04.29.20084111. 〈 10.1101/2020.04.29.20084111〉. [DOI]
- 17.Shaw J, Stewart T, Anderson KB, et al. Assessment of US healthcare personnel attitudes towards coronavirus disease 2019 (COVID-19) vaccination in a large university healthcare system. Clin Infect Dis; 2021. [Accessed 12 March 2021]. [DOI] [PMC free article] [PubMed]
- 18.Szmyd B., Karuga F.F., Bartoszek A., et al. Attitude and behaviors towards SARS-CoV-2 vaccination among healthcare workers: a cross-sectional study from Poland. Vaccines. 2021;9(3) doi: 10.3390/vaccines9030218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Qattan A.M.N., Alshareef N., Alsharqi O., et al. Acceptability of a COVID-19 vaccine among healthcare workers in the Kingdom of Saudi Arabia. Front Med. 2021;8(83) doi: 10.3389/fmed.2021.644300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Noushad M., Nassani M.Z., Alsalhani A.B., et al. COVID-19 vaccine intention among healthcare workers in Saudi Arabia: a cross-sectional survey. Vaccines. 2021;9:835. doi: 10.3390/vaccines9080835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaadan M.I., Abdulkarim J., Chaar M., et al. Determinants of COVID-19 vaccine acceptance in the Arab world: a cross-sectional study. Glob Health Res Policy. 2021;6:23. doi: 10.1186/s41256-021-00202-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rana Abu-Farha, Mukattash Tareq, Itani Rania, Karout Samar, Khojah Hani M.J., Al-Mahmood Asia Abed, et al. Willingness of Middle Eastern public to receive COVID-19 vaccines, Saudi. Pharmaceut J. 2021;29(7) doi: 10.1016/j.jsps.2021.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shekhar R., Sheikh A.B., Upadhyay S., et al. COVID-19 vaccine acceptance among healthcare workers in the United States. Vaccines. 2021;9 doi: 10.3390/vaccines9020119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dror A.A., Eisenbach N., Taiber S., et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Agyekum M.W., Afrifa-Anane G.F., Kyei-Arthur F., et al. Acceptability of COVID-19 vaccination among healthcare workers in Ghana. Adv Public Health. 2021;2021 [Google Scholar]
- 26.Galbadage T., Peterson B.M., Awada J., et al. Systematic review and meta-analysis of sex-specific COVID-19 clinical outcomes. Front Med. 2020;7:348. doi: 10.3389/fmed.2020.00348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huynh G., Tran T., Nguyen H., et al. COVID-19 vaccination intention among healthcare workers in Vietnam. Asian Pac J Trop Med. 2021;14(4):159–164. [Google Scholar]
- 28.Chew N.W.S., Cheong C., Kong G., et al. An Asia-Pacific study on healthcare workers’ perceptions of, and willingness to receive, the COVID-19 vaccination. Int J Infect Dis. 2021;106:52–60. doi: 10.1016/j.ijid.2021.03.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
The data are available from the correspondence author upon reasonable on request.