Abstract
Background
Risk factors for poor maternal perinatal mental health include a previous mental health diagnosis, reduced access to perinatal services, economic concerns and decreased levels of social support. Adverse maternal perinatal mental health can negatively influence the psychological wellbeing of infants. The outbreak of the COVID-19 pandemic presented an additional stressor. While literature on the impact of COVID-19 on perinatal mental health exists, no systematic review has focused specifically on maternal perinatal mental health during periods of COVID-19 lockdown.
Aims
This systematic review explores how periods of COVID-19 lockdown impacted women’s perinatal mental health.
Methods
Searches of CINAHL, PsycARTICLES, PsycINFO, PubMed, Scopus and Web of Science were conducted for literature from 1st January 2020–25th May 2021. Quantitative, peer-reviewed, cross-sectional studies published in English with perinatal women as participants, and data collected during a period of lockdown, were included. Data was assessed for quality and narratively synthesized.
Findings
Sixteen articles from nine countries met the inclusion criteria. COVID-19 lockdowns negatively impacted perinatal mental health. Risk factors for negative perinatal mental health noted in previous literature were confirmed. In addition, resilience, educational attainment, trimester, and ethnicity were identified as other variables which may influence mental health during perinatal periods experienced during lockdown. Understanding nuance in experience and harnessing intra and interpersonal support could advance options for intervention.
Conclusion
Developing resources for perinatal women that integrate informal sources of support may aid them when normal routine is challenged, and may mediate potential long-term impacts of poor perinatal maternal health on infants.
Keywords: Systematic review, Perinatal, Mental health, Women, COVID-19, Lockdown
Statement of significance
Problem
Poor mental health during the perinatal period is concerning for mother and infant. Did periods of COVID-19 lockdown exacerbate this experience?
What is already known
A previous mental health diagnosis, reduced access to perinatal services, decreased levels of social support and economic concerns are risk factors for poor perinatal mental health. The COVID-19 pandemic created another stressor. No review exists focusing specifically on the impact of lockdown periods on perinatal mental health.
What this paper adds
This article synthesises research on women’s perinatal mental health during periods of lockdown. It identifies risk and protective factors, and potential areas for intervention, during times of restriction.
1. Introduction
The perinatal period, classified as pregnancy, birth, and the first 12 months post birth, can result in a range of psychological and physiological changes for women [1], [2]. During this time, changes may also be observed in the perinatal woman’s relationship with her partner, her family and her wider social network [3]. Such developments can negatively impact women’s perinatal mental health. While prevalence rates varied globally, it was estimated that up to 20% of women would experience a perinatal mental health problem [4]. This included obsessive-compulsive disorders, post-traumatic stress disorder (PTSD), anxiety, depression or postpartum psychosis [2]. In Ireland and the United Kingdom (UK), the leading cause of death in women during pregnancy, and in the first year following birth, was suicide [4].
Poor perinatal mental health not only affects the woman: it has also been linked with short- and long- term psychological development and wellbeing of infants [4]. Stress and anxiety during pregnancy can lead to infants exhibiting less social and perceptual competencies at birth [5], as well as being less emotionally stable due to reduced levels of emotional self-regulation [6]. Longitudinal studies have suggested an association with antenatal depression and increased emotional problems for children [7], [8], [9], and have been linked with insecure attachment between mother and child [10], [11]. Longitudinal studies indicated that antenatal depression increased the risk of depression during adolescence [12], [13]. They highlighted an association between postnatal depression and children’s externalising behaviours, up to the age of 16, particularly symptoms of attention deficit hyperactivity disorder [14], [15], [16], [17]. Postnatal depression has also been linked with children’s general cognitive and language development, and has impacted the ability to learn and to achieve developmental milestones [17], [18], [19], [20].
In addition to this human cost, financial expenditure has been associated with perinatal mental health difficulties. For example, in the UK, the estimated outlay of perinatal mental health problems was £8.1bn per year [4]. This cost was five times greater than the estimated budget of improving perinatal services [4].
Several risk factors were recognised as contributing to poor perinatal mental health, including a previous mental health diagnosis [21], a tumultuous relationship with life partner [22], social isolation, lack of social support [23], [24], [25], and economic concerns linked to unemployment and low-income [26], [27], [28]. Additionally, coronavirus disease (COVID-19) was, and continues to be, a further stressor with which women in the perinatal period contend.
The first cases of COVID-19, an infectious disease caused by the SARS-CoV-2 virus, were reported in Wuhan, China in December 2019 [29], [30]. The outbreak was declared a Public Health Emergency of International Concern (PHEIC) in January 2020 and later in March 2020 COVID-19 was classed as a pandemic [31]. In an effort to curtail the spread of the virus, many countries imposed movement restrictions and physical distancing measures, commonly referred to as lockdowns [31]. Lockdowns slowed the transmission of the disease, yet restrictions have negatively impacted individual’s social lives [31]. Further, people experienced increased financial pressure [32], [33], social isolation and reduced access to professional services [34], [35].
COVID-19 lockdown restrictions have resulted in some perinatal women having to substitute onsite hospital appointments with online healthcare appointments [36]. Restrictions have also meant less social support from friends and family, increased feelings of isolation, heightened concern regarding finances, remote working, home-schooling and overcrowded homes and increased incidences of domestic violence [36]. All of these variables have the potential to negatively impact perinatal mental health. A particular example of the impact of COVID-19 restrictions on perinatal healthcare was observed in Ireland where restrictions in maternity hospitals led to national protests. Specifically, partners were banned from attending prenatal scans and in some cases, from attending births [37]. These restrictions caused stress and uncertainty for mothers-to-be, partners, family members and hospital staff [37]. The impact of poor perinatal mental health is far reaching and COVID-19 has further complicated a time already fraught with complexities.
1.1. Rationale for current systematic review
Much literature has been published on the impact of COVID-19 on perinatal mental health from the perspective of various stakeholders, including women in the perinatal period, their partners, hospital staff and policymakers. However, to the best of our knowledge, having searched all available global databases using a set of comprehensive Boolean search protocols, no systematic review has been done to date solely focusing on perinatal women’s experiences during periods of COVID-19 lockdown and specifically how lockdown has impacted their perinatal mental health. As there is no end date for the pandemic, it is imperative we understand the effect restrictions have had on women’s perinatal mental health in order to advance understanding of best practice in supporting perinatal women, during and after the pandemic. Additionally, the findings of this review may also be applicable to individuals within society who are regularly cut off from services outside of the pandemic due to socio-demographic factors.
2. Methods
To determine the utility of conducting a systematic review, this study started broadly by completing a scoping review to clarify key concepts and identify gaps in the literature. The subsequent systematic review was reported in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) 2020 guidelines [38].
2.1. Search strategy
A systematic review protocol was registered with PROSPERO. Six electronic databases (CINAHL, PsycARTICLES, PsycINFO, PubMed, Scopus and Web of Science) were searched to identify literature on perinatal mental health during periods of COVID-19 lockdown, published between 1st January 2020 and 25th May 2021. The search strategy combined Boolean operators and truncation with Medical Subject Headings (MeSH), keywords, CINAHL Subject Headings and the APA Thesaurus of Psychological Index Terms. Keywords and their synonyms were combined using the following search string: (Perinatal OR Pregnan* OR Antenatal OR Prenatal OR Postnatal OR Postpartum OR Post-partum OR Maternal OR Breastfeeding OR Intrapartum) AND ("Perinatal mental health" OR "Mental health" OR Mood OR "Mental wellbeing" OR Psychological OR Psycho* OR Psychiatric) AND (COVID-19 OR COVID* OR Coronavirus OR SARS-CoV-2) AND (Lockdown OR restriction* OR limitation* OR “social distancing” OR “physical distancing” OR “cordon sanitaire” OR shutdown OR shut-down OR “shut down” OR shelter-in-place OR “shelter in place” OR safer-at-home OR “safer at home” OR stay-at-home OR “stay at home” OR curfew).
2.2. Eligibility criteria
For this review, women in the perinatal period were defined as: women receiving prenatal or antenatal care, women who were pregnant at the time of data collection, women who were intrapartum or who had recently given birth, postpartum women, women in the postnatal period, and women who were breastfeeding within the first year of giving birth. Inclusion criteria were that articles had to be quantitative, peer-reviewed, published in English, and data must have been collected during a period of lockdown. Articles which did not explicitly state that data had been gathered during a period of lockdown, but which provided specific dates that could be verified, were included in the review. Exclusion criteria were articles not published in English, articles linked to other stakeholders such as hospital staff, partners and policymakers, and grey literature (e.g., annual reports, newsletters, theses).
2.3. Data screening and extraction
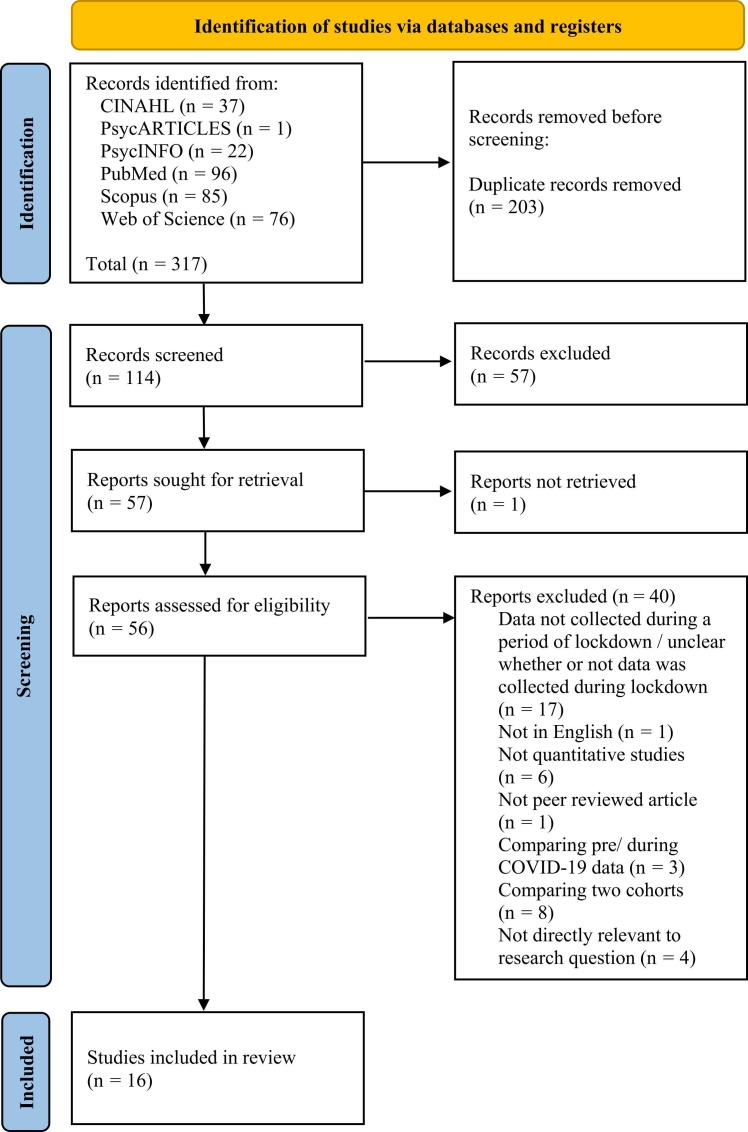
Results from the electronic search were exported to Rayyan - a web application which supported removal of duplicates and streamlined the screening process. The study selection process was summarised in a PRISMA flowchart ( Fig. 1). Following removal of duplicates, the primary researcher (PR) carried out title and abstract screenings on the remaining articles to determine eligibility. Prior to the full text review, reviewers clarified specifics of the inclusion criteria. The PR screened 100% of articles eligible for a full text review while a second reviewer (SR) independently carried out a full text screening on 35% of the articles. There were no disagreements about full text exclusion decisions. Data extracted from eligible studies consisted of: author(s) name, year of publication, study location, sample size, measures and findings ( Table 1).
Fig. 1.
PRISMA flow diagram.
Table 1.
Data extraction table.
| Author (s), year, study location | Sample size | Measures | Findings |
|---|---|---|---|
| Brik et al. (2020), Spain[40]. | PW = 204. | EPDSa STAIb, MOS-SSSc | MHO: Anxiety prevalence rate approx. 60%. 38% of pp reported depressive symptoms. RFs DEP & ANX: Existence of mental health disorders and low levels of social support. TRI: Depression scores higher for women in 1st & 2nd trimester, compared to 3rd trimester. |
| Ceulemans et al. (2020), Belgium[41]. | PW & BFW = 5866. | EPDSa GAD-7d | MHO: Depressive symptoms higher during pregnancy and postpartum compared to pre-COVID-19 estimates. Increased levels of anxiety reported throughout lockdown. |
| Dagklis et al. (2020), Greece[42]. | PW = 269. | STAIb | MHO: Pp anxiety levels negatively impacted during initial stages of lockdown. Anxiety levels decreased after original peak during 1st week. RFs ANX: 1st week following lockdown and being in 3rd trimester. RF DEP: Antenatal depression linked with state anxiety. |
| de Arriba-Garcia et al. (2021), Spain[43]. | PW & PUW = 754. | GHQ-12e | MHO: 58% of pp indicated positive screening for depressive and anxiety symptoms. RFs: Physical health, mental health & economic worries, particularly post week 3 of lockdown. PMHD: Previous diagnosis of depression or anxiety not identified as RF. |
| Dib et al. (2020), UK[44]. | PPW = 1329. | Survey developed for study | MHO: Pp experienced loneliness, irritability, worries and felt down to ‘some’ or ‘high’ extent since lockdown began. Most pp felt they could cope, and felt connected with friends and family. RF: Lower economic status predicted poorer maternal mental health. PFs: Women who received formal and informal support experienced better maternal coping. |
| Fallon et al. (2021), UK[45]. | PPW = 614. | EPDSa STAIb, PSASf PSOCg RQh MSPSSi SAPSj MIBSk | MHO: 43% of pp reported clinically significant depression compared to 11.4% with existing clinical diagnosis of depression. 61% reported clinically significant anxiety compared to 18.4% of pp with existing clinical diagnosis of anxiety. Feelings of depression, anxiety and anxiety about motherhood increased. RFs: Perceived psychological changes during lockdown predicted variance in risk for depression (30%) and anxiety (33%) symptoms. Perceived social changes were not significantly associated with increased risk. |
| Gur et al. (2020), United States of America (Philadelphia)[46]. | PW = 787. | GAD-7d, PHQ-2l, COVID-19 Survey developed for study, Adapted Resilience Questionnaire | MHO: 11.1% of pp met criteria for anxiety. 9.9% met criteria for depression. Black pp more likely to be depressed (16.2%) and anxious (13.9%) than white pp (7.9% and 11%, respectively). RES: Higher levels of resilience through (i) increased self-reliance and emotional regulation and (ii) increased emotional regulation and experiencing less hostile close relationships reduced risk of anxiety and depression, respectively. Findings not moderated by race. |
| Harrison et al. (2020), UK[47]. | PW = 205. | EPDSa MSPSSi PASSm RTQ-10n, De Jong Gierveld Loneliness Scale | MHO: Approx. 50% of pp reported clinically significant scores for perinatal depression and anxiety. 62% of pp experienced loneliness and social isolation. SS: Lower perceived ss was linked with more anxiety and depressive symptoms, loneliness and RNT. Loneliness and RNT mediated effect of perceived ss on anxiety and depression. TRI: Trimester significantly impacted EPDS, PASS and RNT scores, with lower scores reported in 2nd trimester. |
| Harrison et al. (2021), UK[48]. | PNW = 251. | EPDSa MSPSSi PASSm RTQ-10n | MHO: Nearly 50% of pp indicated clinically significant scores for perinatal depression and anxiety, with significant associations between RNT and anxiety and depression. SS: Higher levels of perceived ss from friends moderated negative effects of RNT on anxiety and depression. Family and partner support did not act as a buffer. |
| Ionio et al. (2021), Italy[49]. | PW = 75. | EPDSa IES-Ro CESp RSAq | MHO: Regional differences demonstrated in depressive symptoms. RES: Higher resiliency levels predicted lower depressive symptoms. |
| Lopez et al. (2021), Spain[50]. | PW = 514. | EPDSa STAIb, CD-RISC-10r | MHO: High prevalence rates of clinically significant anxiety and depression during the lockdown. Depression and anxiety were significantly positively correlated. PMHD: State anxiety higher in pp with comorbid psychotic or depressive disorders. Pp with previous psychiatric diagnoses scored higher on the EPDS. EMP: Lower economic status increased pp risk of experiencing depressive symptoms and increased state anxiety. RES: Scores linked with education and income. Practicing coping strategies predicted higher resilience. Scores moderately negatively correlated with depression and anxiety. |
| Mappa et al. (2020), Italy[51]. | PW = 178. | STAIb | MHO: Lockdown led to significant increases in maternal anxiety. PMHD: Increased state anxiety related to pre-existing anxiety. EDU: Pp with lower education level displayed less state anxiety. EMP: Employment status not a significant factor for anxiety. |
| Muhaidat et al. (2020), Jordan[52]. | PW = 944. | Survey developed for study | MHO: Subjective psychological wellbeing affected by periods of lockdown: pp felt sadder (42%); angrier (15%); reported thoughts of self-harm (0.74%) and experienced suicidal thoughts (0.95%). ANC: Approx. 60% of pp did not receive ANC post lockdown, compared to 4% prior to lockdown. |
| Nwafor et al. (2021), Nigeria[53]. | PW = 456. | DASS-21s | MHO: Pp reported: severe/extremely severe depression (14%), severe/extremely severe anxiety (11%) and severe/extremely severe stress (40%). RFs: For anxiety - having a tertiary education; for stress - being in 3rd trimester. TRI: Between 1st & 3rd trimester, stress nearly doubled. |
| Oskovi-Kaplan et al. (2021), Turkey[54]. | PPW = 223. | EPDSa MAIt | MHO: 14.7% of pp at risk for postnatal depression. Pp with depression scored significantly lower maternal attachment scores. |
| Ravaldi et al. (2020), Italy[55]. | PW = 737. | STAIb,COVID- ASSESSu, NSESSS- PTSDv | MHO: Pp demonstrated anxiety (21.7%) and PTSD (10.2%) symptoms. PMHD: Previous psychopathology associated with higher levels of psychological distress. Pp with history of depression or anxiety more worried about COVID-19 and at increased risk of developing anxiety or PTSD symptoms during lockdown. |
ANC = Antenatal care, ANX = Anxiety, BFW = Breast-feeding Women, DEP = Depression, EDU = Education, EMP = Employment, MHO = Mental Health Outcomes, PF = Protective Factor, PMHD = Prior Mental Health Diagnosis, PP= Participants, PNW = Postnatal Women, PPW = Postpartum Women, PUW = Puerperal Women, PW = Pregnant Women, RES = Resilience. RF = Risk Factor, RNT = Repetitive Negative Thinking, SS = Social Support, TRI = Trimester.
Edinburgh Postnatal Depression Scale,
State-Trait Anxiety Inventory,
Medical Outcomes Study Social Support Survey,
Generalized Anxiety Disorder 7-item Scale,
General Health Questionnaire,
Postpartum Specific Anxiety Scale,
Parenting Sense of Competence Scale,
Relationship Questionnaire,
Multidimensional Scale of Perceived Social Support,
The Short Assessment of Patient Satisfaction,
Mother-to-Infant Bonding Scale,
Patient Health Questionnaire 2,
Perinatal Anxiety Screening Scale,
Repetitive Negative Thinking Questionnaire,
Impact of Event Scale- Revised,
Centrality of Event Scale,
Resilience Scale for Adults,
Connor-Davidson Resilience Scale 10-Item,
Depression Anxiety and Stress Scale-21,
Maternal Attachment Inventory,
COVID-19 related Anxiety and StreSs in prEgnancy, posSt-partum and breaStfeeding survey,
National Stressful Events Survey for PTSD-Short Scale.
2.4. Risk of bias assessment
All studies were independently assessed for potential risk of bias using the National Institutes of Health (NIH) Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [39]. This tool provided a checklist which allowed articles to be qualitatively rated as good, fair or poor.
2.5. Quality assessment
Quality appraisal using the NIH Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [39] indicated that the majority of studies were of fair quality, and three were determined to be of good quality i.e., [40], [49], [53]. Due to the parameters of the current review study, four questions on the NIH assessment tool were not applicable (Q8, Q10, Q12 and Q13). No studies were excluded on the basis of the quality assessment. The quality appraisal ratings are presented in supplementary material 1.
2.6. Data synthesis
Due to variability in measures and outcomes of the included studies, the data set was deemed clinically heterogeneous [56]. Where heterogeneity exists, a narrative synthesis is deemed the most appropriate way to synthesise the data [57]. Narrative synthesis employed a textual approach to the way findings were integrated and facilitated exploration of similarities and differences among studies [58]. Quantitative mental health outcome data, as well as additional findings relating to potential risk and protective factors affecting perinatal mental health during lockdown, were reported in a narrative format. The narrative synthesis was guided by Popay et al. [59], specifically in developing a preliminary synthesis through textual descriptions and tabulation, as well as exploration of relationships in the data. To support presenting the data in a narrative format, a thematic approach to analysing the findings was utilised [60].
3. Results
Sixteen articles were included in the review. The initial electronic database search yielded 317 records and 203 duplicates were removed. Following title and abstract screenings, 57 articles were excluded and 57 articles were retained for a full text review. Of these, one article could not be retrieved therefore 56 articles were fully reviewed. Forty articles were excluded. There were seven reasons for exclusion (See Fig. 1). The most common reason linked to study design and included not being a quantitative study and data not being collected during a period of COVID-19 lockdown.
3.1. Study characteristics
Over half of the studies were published during the first year of the pandemic [40], [41], [42], [44], [46], [47], [51], [52], [55]. Sample sizes varied significantly, ranging from 70 to 5866 participants, with data collected from a total of 13401 women across the 16 studies. While more than 60% of the studies focused solely on pregnant women as participants [40], [42], [46], [47], [49], [50], [51], [52], [53], [55], numbers of pregnant and postpartum women recruited were relatively equally distributed (7209 and 6192, respectively). Thirteen studies were conducted within Europe, with the remaining three conducted in North America [46], Asia [52] and Africa [53].
All 16 studies utilised a cross-sectional research design. Twenty-two self-report measures were used. Each study that reported clinical symptoms employed standardised measures. Diagnostic screening tools were not noted and two studies [44], [52] did not use a formal assessment tool.
Twelve articles provided clinical scores for depressive symptoms [40], [41], [42], [43], [45], [46], [47], [48], [49], [50], [53], [54]. Twelve articles reported clinical scores for anxiety symptoms [40], [41], [42], [43], [45], [46], [47], [48], [50], [51], [53], [55]. One article included clinical stress scores [53] and one reported scores for clinical PTSD symptoms [55]. Two articles reported subjective, non-clinical mental health outcomes [44], [52]. In addition to reporting mental health outcomes, 13 articles provided information on additional risk and protective factors identified which impacted perinatal mental health during periods of lockdown [40], [42], [43], [44], [45], [46], [47], [48], [50], [51], [52], [53], [55].
Two primary themes were identified in the data set: (i) mental health outcomes and (ii) risk and protective factors.
3.2. Mental health outcomes
Clinically significant depression symptoms were reported in all 12 studies which screened for depression, with rates ranging from 9.9% to 49% of participants [40], [41], [42], [43], [45], [46], [47], [48], [49], [50], [53], [54]. Clinically significant anxiety symptoms were experienced by women in 12 studies which screened for anxiety, with rates ranging from 11% to 61% [40], [41], [42], [43], [45], [46], [47], [48], [50], [51], [53], [55]. PTSD symptoms were experienced by 10.2% of participants [55], while significant stress symptoms were reported by 40% of women in a separate study [53]. Social isolation and loneliness were experienced by 62% of participants [47]. More than 50% of participants experienced feeling lonely, irritable and down, and more than 70% of these participants experienced worry to either ‘some extent’ or to a ‘high extent’ since the beginning of lockdown [44]. One study noted 0.95% of participants reported suicidal thoughts and 0.74% of participants experienced thoughts of self-harm [52]. A second study [50] found that 4.2% of respondents reported thoughts of harming themselves.
3.3. Risk and protective factors
3.3.1. Previous mental health diagnosis
Five articles examined the effects of previous mental health diagnoses on current mental health outcomes [40], [43], [50], [51], [55]. Four of these articles indicated that a previous mental health diagnosis appeared to be a significant risk factor for current poor mental health outcomes. State anxiety was related to previous trait anxiety [51], and was higher in women with comorbid psychotic or depressive disorders [50]. The presence of mental health disorders was indicative of increased depressive and anxiety symptoms [40] while previous psychopathology was associated with higher levels of psychological distress [55]. Conversely, being previously diagnosed with depression or anxiety was not indicative of current depressive or anxiety symptoms [43].
3.3.2. Support and social changes
The concept of support was reported in six of the 16 articles [40], [44], [45], [47], [48], [52], with both informal and formal support discussed. Informal support from a partner, family or friends provided social support in terms of affection, positive social interaction and emotional support, peer support in relation to validation and empathy, as well as practical support with household chores. Formal support from healthcare providers offered professional, informational and practical support to women. Women reported that support with their own health, and contacting infant support groups, predicted better mental health. Further, women who were supported with their own health as well as who experienced a more equal splitting up of household chores were associated with better maternal coping [44]. Participants who perceived receiving lower levels of social support displayed increased anxiety and depressive symptoms, were absorbed in more repetitive negative thinking (RNT) and experienced more loneliness [47]. While higher levels of perceived support from friends lessened the negative effects of RNT on anxiety and depression, family member or partner support was not found to act as a buffer [48]. Loneliness and RNT mediate the effect of perceived social support on anxiety and depression [47]. Low levels of social support were indicative of increased depressive and anxiety symptoms [40]. While relationships with partners, feelings towards their baby, level of social support and satisfaction with healthcare provision were negatively affected by lockdown measures, these factors were not significantly correlated with increased risk of depressive or anxiety symptoms [45]. Pregnant women experienced major changes in the provision of antenatal care due to lockdown: antenatal care ceased for almost 60% of women, compared to 4% prior to lockdown [52].
3.3.3. Economic considerations
One quarter of studies included information relating to economic considerations and how these factors impact mental health outcomes [44], [50], [51], [53]. One UK based study found that travelling for work, inability to afford food as a result of lockdown, and having an income less than £30,000 (or equivalent) predicted poorer maternal mental health [44]. Participants with lower incomes, or who were unemployed, were at increased risk of developing depressive symptoms [50]. While low or decreased income predicted increased state anxiety in one study [50], employment status was not found to be a significant factor for state or trait anxiety in an alternative study [51]. Women with an occupation which required physical contact such as a trader, farmer or artisan were at higher risk for depression [53].
3.3.4. Resilience
Resilience, the ability to competently deal with adversity [46], [61], was examined in three studies [46], [49], [50]. Women presenting with higher levels of resilience demonstrated lower depressive symptoms [49]. Resilience varied by geographical location, and was related to sleep disturbances and obsessive or catastrophic thoughts about the pandemic [50]. Women with the lowest incomes demonstrated the most resiliency, followed by those that earned the highest incomes [50]. Women who were used to practicing coping strategies such as painting, cooking, physical exercise or relaxation techniques demonstrated higher resiliency than those who were not used to practicing coping strategies [50]. Greater resilience through increased self-reliance and emotional regulation reduced participant’s risk of anxiety [46], while resilience through increased emotional regulation and experiencing less hostile close relationships reduced participant’s risk of depression [46]. Women with more resilience due to increased emotional regulation and perceptions of neighbourhood safety reduced general worries related to COVID-19, while women with more emotional regulation and who experienced less hostile close relationships had fewer pregnancy specific worries due to COVID-19. Additionally, higher levels of resilience through increased self-reliance were also linked with concerns specific to pregnancy during COVID-19 [46].
3.3.5. Education
Although 62.5% of studies provided information pertaining to participants' level of educational attainment [44], [45], [47], [48], [49], [50], [51], [52], [53], [54], only two studies examined possible relationships between education and mental health outcomes [51], [53]. Women who held a university degree or diploma displayed more state anxiety than women with lower levels of education [51], while having a tertiary education was identified as a predictor of anxiety and stress [53].
3.3.6. Trimester
Seven of the studies included the breakdown of participants by trimester [40], [46], [47], [51], [52], [53], [55], however just four studies provided information about relationships between trimester and mental health outcomes [40], [42], [47], [53]. Being in the third trimester acted as a risk factor for anxiety [42] and stress [53], with stress scores almost doubled for women in the third trimester in comparison to those in their first trimester [53]. Depression scores were found to be higher for women in their first and second trimester, compared to those in their third trimester [40]. Trimester had a significant effect on perinatal depression and anxiety scores, as well as RNT scores, with significantly lower scores found in the second trimester [47].
3.3.7. Ethnicity
Though the ethnic breakdown of participants was provided in seven studies [40], [44], [45], [46], [47], [48], [51], it was not widely used to identify associations with mental health outcomes. One study found that being of Latin-American origin was a predictive factor for anxiety [40], while a separate study focused primarily on racial disparities [46]. Black women were more likely to demonstrate depressive and anxious symptoms than white women, with evident differences in the way financial concerns, access to prenatal care and resources, and resilience were experienced by black and white women [46].
4. Discussion
COVID-19 lockdowns initiated unexpected, unprecedented change for all, across myriad domains of living. It has been a transformative life event. As such, the finding that a significant proportion of women experienced poor perinatal mental health during lockdown is somewhat unsurprising. Our findings are mostly consistent with prior literature in the area. However, this review extends previous findings by further unpacking some of the identified risk factors and highlighting potential areas for intervention.
Risk factors for poor perinatal mental health identified prior to, and during the pandemic, included having a previous mental health diagnosis; social isolation; a lack of social support; economic pressures; and relationship stresses between the perinatal woman and her partner. This review concurred with these findings, albeit for the occasional discrepancy. For example, having a previous mental health diagnosis appeared to be a risk factor for poor perinatal mental health [40], [50], [51], [55] reiterating findings by Johnstone et al. [21]. However, [43] noted that a previous mental health diagnosis was not identified as a significant risk factor for current depressive or anxiety symptoms. This lack of identified association could be due to the low rate of cases: only 166 women, 22% of the sample, indicated having a previous diagnosis.
Clinically significant depression and anxiety rates were reported in the majority of studies. The findings that participants reported feeling lonely, down, irritable, and worried since the beginning of lockdown [44] echo those of Bauer et al. [4]. They are stark from both short, and long, term perspectives. Specifically, in terms of the former, the social isolation heralded by lockdown dovetailed with added difficulties accessing timely professional support. In terms of the latter, as noted by Oskovi-Kaplan et al. [54], participants who were depressed scored significantly lower maternal attachment scores. Research has suggested antenatal depression is linked with insecure attachments [10], [11]. This is pertinent in terms of ongoing, and longer-term, implications for the wider familial unit. Insecure attachments in early childhood can contribute to psychopathology in later life [62]. As such, poor perinatal maternal health signifies a risk factor for child mental health. In instances where support needs are met by extended family members, ensuring that professional intervention explicitly identifies commonality in parenting values is important. Doing so may diminish the possibility of parenting support becoming contentious or aggravating in terms of mental health. Timely, focused intervention in this area could proactively insulate against ongoing transgenerational mental health issues.
Of 13401 participants included across 16 studies, 1458 were asked whether they experienced thoughts of self-harm and 944 were probed about suicidal ideation. Of these participants, 31 women reported thoughts of self-harm, and nine reported experiencing suicidal thoughts. Initially these numbers may seem low in relation to the overall sample size. However, as suicide was identified as the primary cause of death among perinatal women [4], the dearth of research pertaining to this area is cause for concern. Given that all included studies focused on perinatal mental health, had more studies included questions on self-harm and suicidal ideation these findings may have been significantly higher.
Education, economic concerns and ethnicity were, to varying degrees, noted as risk factors for poor perinatal mental health [26], [28], [36], [40], [46], [51], [53]. In each instance sample sizes were limited. The findings are of interest however in terms of prompting research questions. For example, what could explain the finding that women who have achieved a third level education display more state anxiety than those with a lower level of education [51], [53]? Could this be linked to internal versus external locus of control, or experience in responding to multiple life changes simultaneously, or self-care activities? In terms of employment, notwithstanding the fact that there was ambiguity in the original article regarding meaning of ‘physical contact’ [53], this single study noted that participants whose jobs necessitated physical contact (e.g., trader, farmer) were at a higher risk for depression. This suggests that unpacking the demands of a perinatal woman’s occupation may be an entry point to responding to individualised support needs. How are we to understand differences highlighted by Gur et al. [46] in the way resilience was experienced among black and white women? The link between self-reliance and risk of depression was moderated by race with greater self-reliance predicting lower levels of depression for white, but not for black, women. Could these findings indicate a need to investigate whether ethnicity is really a marker of cultural dislocation, lower socio-economic status or other complex factors? Taken together these findings highlight the need for a deeper delve into how perinatal women from minority groups were affected by lockdown.
During the perinatal period support is crucial. As noted by Dempsey and Peeren [63] and Dunkel Schetter [64], qualitatively different support is needed from various people. Participants experienced a considerable decrease in the availability of formal antenatal care during lockdown [52] and their satisfaction with healthcare provision was negatively impacted [45]. Being unable to draw on formal support resulted in participants worrying about lack of regular antenatal visits [46], [51] and about their birth experience [46]. Through the care they provide, midwives and health professionals are well placed to impact the way perinatal women think and feel about their pregnancy [63], [65]. Harnessing this professional support, through development of audio guided bibliotherapy, could provide a bridge to formal support for perinatal women in instances where in-person access to services is reduced or not feasible and continuity between support sessions. Further, the findings that women who received support for their own health, who contacted infant support groups, and whose partners shared household chores more equally with them, experienced improved perinatal mental health and maternal coping [44], point to potential interventions that may fit within the midwifery services. Specifically, a psychoeducational intervention to support women in prioritising their individual needs (e.g., mental health, social contact, parenting, infant socialisation, managing domestic tasks), could be a relatively low-cost support in promoting positive perinatal mental health. Alternatively, offering perinatal parent-infant art classes based on Bruce and Hackett’s [66] work may aid in promoting perinatal mothers’ mood, self-knowledge, understanding of problems and relational engagement with their babies.
Jonsdottir et al. [3] found that changes in the perinatal woman’s informal support systems e.g. partner, family and friends, were often experienced. Four studies considered relationship status in terms of social support and perinatal mental health outcomes. Negative changes within the perinatal woman’s relationship with her partner were reported but were not a direct risk factor for poor perinatal mental health [45]. This is of particular interest given that COVID-19 lockdowns were linked with increased incidences of domestic violence [67]. Just one article in the current review [47] commented on domestic violence rates during lockdown. As women in the perinatal period are susceptible to experiencing domestic violence [67], [68], and may find it challenging to seek help, routine screening by their midwifery team could scaffold timely intervention and referral for this vulnerable population [68].
Higher levels of perceived social support from friends moderated negative effects of RNT on symptoms of depression and anxiety, though support from family or partners did not act as a buffer [48]. Participants noted that support from their partners was important so why only support from friends served as a buffer is not entirely clear. Harrison et al. [48] postulate that even the most supportive partner cannot fully understand the maternal experience [69]. Another possible explanation draws on Clark and Wells’ [70] and Clarks’ [71] cognitive model of social anxiety whereby people who are socially anxious tend to have a more negative perception of other people’s response to them. Could it be that participants who perceived lower levels of social support were not as fluent as other people in recognising positive responses? Regardless of the reason, there is scope for intervention. One approach may be talk therapy to empower perinatal mothers in identifying what constitutes personal social support for them e.g., being invited to events as normal, adapting activity with friends, being included through online contact. In this way, brief talk therapy can be drawn on to promote social support.
In general, people tend to have an implicit understanding of what is stressful. It makes intuitive sense that enforced lockdown will, for many, have created more challenges and difficulties. Of course, within this there will also be some people who found that lockdown may not have impacted them as negatively as they had predicted, or as other people experienced. Personal resilience can act as a buffer against some of the negative perinatal mental health outcomes associated with lockdown, such as depression. As resilience seems to be influenced by the active practice of coping and relaxation strategies, developing a preventative psychoeducational intervention for perinatal women to promote resilience would seem timely. A potential approach could incorporate the peer-led ‘Wellness Recovery Action Plan’ (WRAP) [72]. This self-management tool, built on the principles of hope, personal responsibility, education, self-advocacy and support, comprises an individualised plan or toolbox of resources and activities identified by the person for themselves. It can be updated regularly in response to needs regarding gaining, or maintaining, control over mental wellbeing. Developing a practical approach is important for wellbeing generally and enhancing quality of life. This is expressly so when routine and normal process is jeopardised.
5. Limitations and strengths
Publication bias may exist as only peer-reviewed articles published in English were included in the review. Additionally, the heterogeneity of studies meant that it was not possible to carry out a meta-analysis. The range of assessment tools used in the studies and national variation in implementation of COVID-19 rules limited comparability of results. In terms of the quality of included articles, due to the cross-sectional nature of the studies it is possible that weaker evidence is provided in comparison with regular cohort studies regarding possible causal relationships between lockdown and perinatal mental health. An example are the findings relating to the role of previous mental health diagnoses on perinatal mental health outcomes during lockdown. While the STAI measures trait anxiety, in the absence of data pertaining to anxiety levels of the same participants prior to the COVID-19 outbreak, it is not possible to comment on the extent that previous mental health diagnoses impacted current mental health outcomes. Similarly, variability on what constitutes a previous mental health diagnosis limits compatibility between studies e.g., one study refers to a diagnosis given by a psychiatrist following clinical interview [40], while other studies ask participants to self-report previous diagnoses [45], [55]. While 11 studies did not provide a sample size justification, this may be explained by the fact observational studies are exploratory in nature and so the focus may not have been on whether the study had a sufficient number of participants to answer the authors research question.
Initiating this study by completing a scoping review undoubtedly helped to focus the systematic review, ensuring a comprehensive search of the literature could be carried out. Conducting the systematic review in line with the updated PRISMA guidelines [38] ensures that the study was transparent and complete reporting enhanced the trustworthiness of the findings.
6. Implications
The current study has implications for clinicians, researchers and policymakers. The findings of this study are notable in identifying risk and protective factors which may have contributed to optimum management of perinatal mental health, during and after the COVID-19 lockdown periods. Awareness of risk factors could support increased screening for earlier identification of poor perinatal mental health by healthcare practitioners. With integration of online appointments, health care workers' cognisance that not all service users are computer literate is important. As such, information booklets and bibliotherapy will aid individuals in understanding what supports are available and actions needed to access them. While this review focused specifically on how COVID-19 lockdown restrictions impacted perinatal mental health, there are transferable learnings in terms of people who, regardless of the pandemic, have limited access to services and supports. Findings, and noted interventions, can be drawn on to protect against risk factors in this area and promote positive perinatal mental health.
7. Conclusion
COVID-19 lockdowns amplified the stressors that impact perinatal women’s mental health. When normal routine is disrupted, formal interventions that draw on perinatal women’s intra and interpersonal resources to support changes in their domestic space and facilitate them in developing mental health wellbeing tool kits, may help insulate against the impact of mental health challenges for both mother and child.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.wombi.2022.06.005.
Appendix A. Supplementary material
Supplementary material.
.
References
- 1.Huschke S., Murphy-Tighe S., Barry M. Perinatal mental health in Ireland: a scoping review. Midwifery. 2020;89:1–21. doi: 10.1016/j.midw.2020.102763. [DOI] [PubMed] [Google Scholar]
- 2.Jomeen J. In: Mayes’ Midwifery. MacDonald S., Johnson G., editors. Elsevier; London: 2017. Psychological context of childbirth; pp. 186–199. [Google Scholar]
- 3.Jonsdottir S.S., Thome M., Steingrimsdottir T., Lydsdottir L.B., Sigurdsson J.F., Olafsdottir H., Swahnberg K. Partner relationship, social support and perinatal distress among pregnant Icelandic women. Women Birth. 2017;30(1):e46–e55. doi: 10.1016/j.wombi.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 4.A. Bauer, M. Parsonage, M. Knapp, V. Iemmi, B. Adelaja, 2014. The Costs of Perinatal Mental Health Problems. LSE & Centre for Mental Health; 2014. Available at: 〈https://www.centreformentalhealth.org.uk/sites/default/files/2018-09/costsofperinatal.pdf〉 [Accessed 12 March 2021].
- 5.Figueiredo B., Pacheco A., Costa R., Conde A., Teixeira C. Mother’s anxiety and depression during the third pregnancy trimester and neonate’s mother versus stranger’s face/voice visual preference. Early Hum. Dev. 2010;86:479–485. doi: 10.1016/j.earlhumdev.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 6.Hernandez-Martinez C., Arija V., Balaguer A., Cavalle P., Canals J. Do the emotional states of pregnant women affect neonatal behaviour? Early Hum. Dev. 2008;84:745–750. doi: 10.1016/j.earlhumdev.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 7.Gerardin P., Wendland J., Bodeau N., Galin A., Bialobos S., Tordjman S., Mazet P., Darbois Y., Nizard J., Dommergues M., Cohen D. Depression during pregnancy: is the developmental impact earlier in boys? A prospective case-control study. J. Clin. Psychiatry. 2011;71:378–387. doi: 10.4088/JCP.09m05724blu. [DOI] [PubMed] [Google Scholar]
- 8.Leis J.A., Heron J., Stuart E.A., Mendelson T. Associations between maternal mental health and child emotional and behavioral problems: does prenatal mental health matter? J. Abnorm Child Psychol. 2013;42:161–171. doi: 10.1007/s10802-013-9766-4. [DOI] [PubMed] [Google Scholar]
- 9.Velders F.P., Dieleman G., Henrichs J., Jaddoe V.W.V., Hofman A., Verhulst F.C., Hudziak J.J., Tiemeier H. Prenatal and postnatal psychological symptoms of parents and family functioning: the impact on child emotional and behavioural problems. Eur. Child Adolesc. Psychiatry. 2011;20:341–350. doi: 10.1007/s00787-011-0178-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Atkinson L., Paglia A., Coolbear J., Niccols A., Parker K.C., Guger S. Attachment security: a meta-analysis of maternal mental health correlates. Clin. Psychol. Rev. 2000;20:1019–1040. doi: 10.1016/s0272-7358(99)00023-9. [DOI] [PubMed] [Google Scholar]
- 11.Martins C., Gaffan E.A. Effects of early maternal depression on patterns of infant-mother attachment: a meta-analytic investigation. J. Child Psychol. Psychiatry. 2000;41:737–746. [PubMed] [Google Scholar]
- 12.Pawlby S., Hay D.F., Sharp D., Waters C.S., O’Keane V. Antenatal depression predicts depression in adolescent offspring: prospective longitudinal community-based study. J. Affect Disord. 2009;113:236–243. doi: 10.1016/j.jad.2008.05.018. [DOI] [PubMed] [Google Scholar]
- 13.Pearson R.M., Evans J., Kounali D., Lewis G., Heron J., Ramchandani P.G., O’Connor T., Stein A. Maternal depression during pregnancy and the postnatal period: risks and possible mechanisms for offspring depression at age 18 years. JAMA Psychiatry. 2013;70:1312–1319. doi: 10.1001/jamapsychiatry.2013.2163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Avan B., Richter L.M., Ramchandani P.G., Norris S.A., Stein A. Maternal postnatal depression and children’s growth and behaviour during the early years of life: exploring the interaction between physical and mental health. Arch. Dis. Child. 2010;95:690–695. doi: 10.1136/adc.2009.164848. [DOI] [PubMed] [Google Scholar]
- 15.Fihrer I., McMahon C.A., Taylor A.J. The impact of postnatal and concurrent maternal depression on child behaviour during the early school years. J. Affect Disord. 2009;119:116–123. doi: 10.1016/j.jad.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 16.Hanington L., Heron J., Stein A., Ramchandani P. Parental depression and child outcomes-is marital conflict the missing link? Child Care Health Dev. 2012;38:520–529. doi: 10.1111/j.1365-2214.2011.01270.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Letourneau N.L., Tramonte L., Willms J.D. Maternal depression, family functioning and children’s longitudinal development. J. Pediatr. Nurs. 2013;28:223–234. doi: 10.1016/j.pedn.2012.07.014. [DOI] [PubMed] [Google Scholar]
- 18.Conroy S., Pariante C.M., Marks M.N., Davies H.A., Farrelly S., Schacht R., Moran P. Maternal psychopathology and infant development at 18 months: the impact of maternal personality disorder and depression. J. Am. Acad. Child Adolesc. Psychiatry. 2012;51:51–61. doi: 10.1016/j.jaac.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 19.Kaplan P.S., Danko C.M., Diaz A., Kalinka C.J. An associative learning deficit in 1-year-old infants of depressed mothers: role of depression duration. Infant. Behav. Dev. 2011;34:35–44. doi: 10.1016/j.infbeh.2010.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sutter-Dallay A.L., Murray L., Dequae-Merchadou L., Glatigny-Dallay E., Bourgeois M.L., Verdoux H. A prospective longitudinal study of the impact of early postnatal vs chronic maternal depressive symptoms on child development. Eur. Psychiatry. 2011;26:484–489. doi: 10.1016/j.eurpsy.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 21.Johnstone S.J., Boyce P.M., Hickey A.R., Morris-Yatees A.D., Harris M.G. Obstetric risk factors for postnatal depression in urban and rural community samples. Aust. N. Z. J. Psychiatry. 2001;35(1):69–74. doi: 10.1046/j.1440-1614.2001.00862.x. [DOI] [PubMed] [Google Scholar]
- 22.Khajehei M., Doherty M. Exploring postnatal depression, sexual dysfunction and relationship dissatisfaction in Australian women. Br. J. Midwifery. 2017;25(3):162–172. [Google Scholar]
- 23.Aktan N.M. Social support and anxiety in pregnant and postpartum women: a secondary analysis. Clin. Nurs. Res. 2012;21(2):183–194. doi: 10.1177/1054773811426350. [DOI] [PubMed] [Google Scholar]
- 24.Corrigan C.P., Kwasky A.N., Groh C.J. Social support, postpartum depression, and professional assistance: a survey of mothers in the Midwestern United States. J. Perinat. Educ. 2015;24(1):48–60. doi: 10.1891/1058-1243.24.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Negron R., Martin A., Almog M., Balbierz A., Howell E.A. Social support during the postpartum period: mothers’ views on needs, expectations, and mobilization of support. Matern. Child Health J. 2013;17(4):616–623. doi: 10.1007/s10995-012-1037-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mezey G., Bacchus L., Bewley S., White S. Domestic violence, lifetime trauma and psychological health of childbearing women. BJOG. 2005;112:197–204. doi: 10.1111/j.1471-0528.2004.00307.x. [DOI] [PubMed] [Google Scholar]
- 27.Tuten M., Jones H.E., Svikis D.S. Comparing homeless and domiciled pregnant substance dependent women on psychosocial characteristics and treatment outcomes. Drug Alcohol Depend. 2003;69(1):95–99. doi: 10.1016/s0376-8716(02)00229-6. [DOI] [PubMed] [Google Scholar]
- 28.Yamamoto N., Abe Y., Arima K., Nishimura T., Akahoshi E., Oishi K., Aoyagi K. Mental health problems and influencing factors in Japanese women 4 months after delivery. J. Physiol. Anthr. 2014;33(32):1–6. doi: 10.1186/1880-6805-33-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.World Health Organization, 2021. Coronavirus: Overview. World Health Organization; 2021. Available at: 〈https://www.who.int/health-topics/coronavirus#tab=tab_1〉 [Accessed 12 June 2021].
- 30.World Health Organization, 2020. Archived: WHO Timeline - COVID-19. World Health Organization; 2020. Available at: 〈https://www.who.int/news/item/27–04-2020-who-timeline---covid-19〉 [Accessed 30 April 2021].
- 31.World Health Organization, 2020. Coronavirus disease (COVID-19): Herd immunity, lockdowns and COVID-19. World Health Organization; 2020. Available at: 〈https://www.who.int/news-room/questions-and-answers/item/herd-immunity-lockdowns-and-covid-19〉 [Accessed 10 April 2021].
- 32.Coronini‐Cronberg S., John Maile E., Majeed A. Health inequalities: The hidden cost of COVID‐19 in NHS hospital trusts? J. R. Soc. Med. 2020;113:179–184. doi: 10.1177/0141076820925230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Knight M., Bunch K., Vousden N., Morris E., Simpson N., Gale C., O’Brien P., Quigley M., Brocklehurst P., Kurinczuk J.J. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population based cohort study. BMJ. 2020;369(m2107):1–7. doi: 10.1136/bmj.m2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., Kontopantelis E., Webb R., Wessely S., McManus S., Abel K.M. Mental health before and during the COVID‐19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7(10):883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.A. Andrew, S. Cattan, M.C. Dias, C. Farquharson, L. Kraftman, S. Krutikova, A. Phimister, A. Sevilla, 2020. How are mothers and fathers balancing work and family under lockdown? Institute for Fiscal Studies; 2020. Available at: 〈https://ifs.org.uk/uploads/BN290-Mothers-and-fathers-balancing-work-and-life-under-lockdown.pdf〉 [Accessed 16th April 2021].
- 36.Caparros-Gonzalez R.A., Alderdice F. The COVID-19 pandemic and perinatal mental health. J. Reprod. Infant Psychol. 2020;38(3):223–225. doi: 10.1080/02646838.2020.1786910. [DOI] [PubMed] [Google Scholar]
- 37.K. Matvienko-Sikar, 2021. How the pandemic increased prenatal distress for pregnant women. Raidió Teilifís Éireann; 2021. Available at: 〈https://www.rte.ie/brainstorm/2021/0526/1223963-pregnancy-pandemic-prenatal-distress/〉 [Accessed 10 June 2021].
- 38.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., Chou R., Glanville J., Grimshaw J.M., Hróbjartsson A., Lalu M.M., Li T., Loder E.W., Mayo-Wilson E., McDonald S., McGuinness L., Stewart L., Thomas J., Tricco A., Welch V., Whiting P., Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372(n71):1–9. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.National Institutes of Health, 2014. Quality assessment tool for observational and cross-sectional studies. National Heart, Lung, and Blood Institute; 2014. Available at: 〈https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools〉 [Accessed 7 August 2021].
- 40.Brik M., Sandonis M.A., Fernandez S., Suy A., Parramon- Puig G., Maiz N., Dip M.E., Ramos- Quiroga J.A., Carreras E. Psychological impact and social support in pregnant women during lockdown due to SARS- CoV2 pandemic: a cohort study. Acta Obstet. Gynecol. Scand. 2020;100(6):1026–1033. doi: 10.1111/aogs.14073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ceulemans M., Hompes T., Foulon V. Mental health status of pregnant and breastfeeding women during the COVID‐19 pandemic: a call for action. Int. J. Gynaecol. Obstet. 2020;151(1):146–147. doi: 10.1002/ijgo.13295. [DOI] [PubMed] [Google Scholar]
- 42.Dagklis T., Tsakiridis I., Mamopoulos A., Athanasiadis A., Pearson R., Papazisis G. The impact of the COVID‐19 lockdown on antenatal mental health in Greece. Psychiatry Clin. Neurosci. 2020;74:616–617. doi: 10.1111/pcn.13135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.de Arriba-Garcia M., Diaz-Martinez A., Monfort-Ortiz R., Roca-Prats A., Monfort-Beltran S., Ivanez-Munoz M., Alberola-Rubio J., Perales-Marin A. GESTACOVID project: psychological and perinatal effects in Spanish pregnant women subjected to confinement due to the COVID-19 pandemic. J. Matern. Fetal Neonatal Med. 2021:1–7. doi: 10.1080/14767058.2021.1888922. [DOI] [PubMed] [Google Scholar]
- 44.Dib S., Rougeaux E., Vazquez‐Vazquez A., Wells J.C.K., Fewtrell M. Maternal mental health and coping during the COVID‐19 lockdown in the UK: data from the COVID‐19 New Mum Study. Int. J. Gynaecol. Obstet. 2020;151(3):407–414. doi: 10.1002/ijgo.13397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fallon V., Davies S.M., Silverio S.A., Jackson L., De Pascalis L., Harrold J.A. Psychosocial experiences of postnatal women during the COVID-19 pandemic. A UK-wide study of prevalence rates and risk factors for clinically relevant depression and anxiety. J. Psychiatr. Res. 2021;136:157–166. doi: 10.1016/j.jpsychires.2021.01.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gur R.E., White L.K., Waller R., Barzilay R., Moore T.M., Kornfield S., Njoroge W., Duncan A.F., Chaiyachati B.H., Parish-Morris J., Maayan L., Himes M., Laney N., Simonette K., Riis V., Elovitz M.A. The disproportionate burden of the COVID-19 pandemic among pregnant black women. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Harrison V., Moulds M.L., Jones K. Perceived social support and prenatal wellbeing; The mediating effects of loneliness and repetitive negative thinking on anxiety and depression during the COVID-19 pandemic. Women Birth. 2020 doi: 10.1016/j.wombi.2020.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Harrison V., Moulds M.L., Jones K. Support from friends moderates the relationship between repetitive negative thinking and postnatal wellbeing during COVID-19. J. Reprod. Infant Psychol. 2021 doi: 10.1080/02646838.2021.1886260. [DOI] [PubMed] [Google Scholar]
- 49.Ionio C., Gallese M., Fenaroli V., Smorti M., Greco A., Testa I., Zilioli A., Bonassi L. COVID-19: what about pregnant women during first lockdown in Italy? J. Reprod. Infant Psychol. 2021 doi: 10.1080/02646838.2021.1928614. [DOI] [PubMed] [Google Scholar]
- 50.Lopez D., Hinojo C., Bernal J., Laiz M., Santiago J.A., Vilches V., Fernandez M., Moral A., Perdigones A., Rodriguez B., Palomino A., Lorite J., Martín P., Sanchez-Prieto M., Sanchez-Borrego R., Gonzalez-Mesa E. Resilience and psychological distress in pregnant women during quarantine due to the COVID-19 outbreak in Spain: a multicentre cross-sectional online survey. J. Psychosom. Obstet. Gynaecol. 2021;42(2):115–122. doi: 10.1080/0167482X.2021.1896491. [DOI] [PubMed] [Google Scholar]
- 51.Mappa I., Adalgisa Distefano F., Rizzo G. Effects of coronavirus 19 pandemic on maternal anxiety during pregnancy: a prospectic observational study. J. Perinat. Med. 2020;48(6):545–550. doi: 10.1515/jpm-2020-0182. [DOI] [PubMed] [Google Scholar]
- 52.Muhaidat N., Fram K., Thekrallah F., Qatawneh A., Al-Btoushet A. Pregnancy during COVID-19 outbreak: the impact of lockdown in a middle-income country on antenatal healthcare and wellbeing. Int. J. Women’s Health. 2020;12:1065–1073. doi: 10.2147/IJWH.S280342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nwafor J.I., Okedo-Alex I.N., Ikeotuonyeet A.C. Prevalence and predictors of depression, anxiety, and stress symptoms among pregnant women during COVID-19-related lockdown in Abakaliki, Nigeria. Malawi Med. J. 2021;33(1):54–58. doi: 10.4314/mmj.v33i1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Oskovi-Kaplan Z.A., Buyuk G.N., Ozgu-Erdinc A.S., Keskin H.L., Ozbas A., Tekin O.M. The effect of COVID-19 pandemic and social restrictions on depression rates and maternal attachment in immediate postpartum women: a preliminary study. Psychiatr. Q. 2021;92(2):675–682. doi: 10.1007/s11126-020-09843-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ravaldi C., Ricca V., Wilson A., Homer C., Vannacc A. Previous psychopathology predicted severe COVID-19 concern, anxiety, and PTSD symptoms in pregnant women during “lockdown” in Italy. Arch. Women’s Ment. Health. 2020;23:783–786. doi: 10.1007/s00737-020-01086-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Boland A., Cherry M.G., Dickson R. SAGE Publications; London: 2017. Doing a systematic review: a student’s guide. [Google Scholar]
- 57.Baumeister R.F. In: The portable mentor: expert guide to a successful career in psychology. Prinstein M.J., Patterson M.D., editors. New York: Spring; 2013. Writing a Literature Review; pp. 119–132. [Google Scholar]
- 58.Lisy K., Porritt K. Narrative synthesis: considerations and challenges. Int. J. Evid. Based Health. 2016;14(4):201. [Google Scholar]
- 59.Popay J., Roberts H., Sowden A., Petticrew M., Arai L., Rodgers M., Britten N., Roen K., Duffy S., 2006. Guidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC Methods Programme. Lancaster University; 2006. Available at: 〈https://www.lancaster.ac.uk/media/lancaster-university/content-assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1-April2006.pdf〉 [Accessed 10 August 2021].
- 60.Braun V., Clarke V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006;3:77–101. [Google Scholar]
- 61.Ungar M., Theron L. Resilience and mental health: how multisystemic processes contribute to positive outcomes. Lancet Psychiatry. 2019;7:441–448. doi: 10.1016/S2215-0366(19)30434-1. [DOI] [PubMed] [Google Scholar]
- 62.Mikulincer M., Shaver P.R. An attachment perspective on psychopathology. World Psychiatry. 2012;11(1):11–15. doi: 10.1016/j.wpsyc.2012.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dempsey M., Peeren S. Keeping things under control: exploring migrant Eastern European womens’ experiences of pregnancy in Ireland. J. Reprod. Infant Psychol. 2016;34(4):370–382. [Google Scholar]
- 64.Dunkel Schetter C. Psychological science on pregnancy: stress processes, biopsychosocial models, and emerging research issues. Annu. Rev. Psychol. 2011;62(1):531–558. doi: 10.1146/annurev.psych.031809.130727. [DOI] [PubMed] [Google Scholar]
- 65.Leventhal H., Brissette I., Leventhal E.A. In: The self-regulation of health and illness behaviour. Cameron L.D., Leventhal H., editors. Routledge; London: 2003. The Common-sense Model of Self-regulation of Health and Illness; pp. 42–65. [Google Scholar]
- 66.Bruce D., Hackett S.S. Developing art therapy practice within perinatal parent-infant mental health. Int. J. Art. Ther. 2021;26(3):111–122. [Google Scholar]
- 67.Kotlar B., Gerson E., Petrillo S., Langer A., Tiemeier H. The impact of the COVID-19 pandemic on maternal and perinatal health: a scoping review. Reprod. Health. 2021;18(10):1–39. doi: 10.1186/s12978-021-01070-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.O’Reilly R., Peters K. Opportunistic domestic violence screening for pregnant and post-partum women by community based health care providers. BMC Women's Health. 2018;18(128):1–8. doi: 10.1186/s12905-018-0620-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Coates R., Ayers S., de Visser R. Women’s experiences of postnatal distress: a qualitative study. BMC Pregnancy Childbirth. 2014;14(359):1–14. doi: 10.1186/1471-2393-14-359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Clark D.M., Wells A. In: Social phobia: Diagnosis, assessment, and treatment. Heimberg R.G., Liebowitz M.R., Hope D.A., Schneier F.R., editors. The Guilford Press; New York: 1995. A Cognitive Model of Social Phobia; pp. 69–91. [Google Scholar]
- 71.Clark D.M. In: International handbook of social anxiety. Crozier W.R., Alden L.E., editors. Wiley; Chichester: 2001. A Cognitive Perspective on Social Phobia; pp. 405–430. [Google Scholar]
- 72.Cook J.A., Copeland M.E., Corey L., Buffington E., Jonikas J.A., Curtis L.C., Grey D.D., Nichols W.H. Developing the evidence base for peer-led services: changes among participants following Wellness Recovery Action Planning (WRAP) education in two statewide initiatives. Psychiatr. Rehabil. J. 2010;34(2):113–120. doi: 10.2975/34.2.2010.113.120. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material.