Background
Affective disorders such as major depressive disorder and bipolar disorder are associated with higher infection rates and a more severe course of coronavirus disease (COVID-19). In turn, COVID-19 could trigger mental disease relapse. Vaccinations lead to a reduction of infections and the prevention of severe courses. This work aims to survey the willingness of individuals with affective disorders to get vaccinated and concerns about vaccinations. Methods: An online study (April–May 2021) assessed the current infection and vaccination rate amongst individuals with affective disorder in Austria by surveying attitudes towards the vaccination, the willingness to get vaccinated soon and possible reasons for decision. The analyses included 59 individuals with affective disorders and 59 healthy controls, matched for sex and age. Results: There was an overall high willingness to get vaccinated against COVID-19. Individuals with affective disorders were more skeptical about vaccinations in general but there was no significant difference between the groups in the willingness to get vaccinated against COVID-19. In both groups reasons for waiting were mainly fears of acute and/or long-term side effects and the fast development of the vaccines. Limitations: It was a cross sectional design. Due to the online design, no objective rating of current psychopathological symptoms was assessed. Willingness to get vaccinated in general and against COVID-19 in particular were self-created variables, whereas item statistics and factor analysis were conducted. Discussion: Because of the higher risk for individuals with affective disorders, preventive strategies like vaccinating should be promoted in this group. It is important to help individuals with AD to overcome barriers such as negative beliefs and concerns about acute and/or long-term side effects.
Keywords: Affective disorder, COVID-19, Vaccination, Willingness, Depression, Bipolar disorder
Introduction
Affective disorders (AD) such as major depressive disorder (MDD) and bipolar disorder (BD) are highly prevalent worldwide and frequently have a chronic course. Acute psychopathology, in particular suicidal ideation and suicides present a challenge for the treatment [1]. Furthermore, due to sociopsychological consequences (e.g. low socioeconomic status, cognitive impairment) but also to psychiatric (e.g. substance use disorder, anxiety disorders) and somatic comorbidities (e.g. obesity and associated metabolic and cardiovascular diseases), mortality is higher in individuals with a mental disorder compared to individuals without [2]. In addition to cardiovascular diseases and metabolic alterations, viral diseases such as hepatitis B and C as well as pneumococcal disease rank among the most common somatic comorbidities in mental disorders [3], [4].
Preliminary data also suggest higher infection rates with the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) leading to the coronavirus disease (COVID-19) in psychiatric samples compared to individuals without a mental disorder [5], [6], [7]. Even after adjusting for age, sex, ethnicity, and medical comorbidities, individuals with MDD, BD, schizophrenia and attention-deficit/hyperactivity disorder exhibited a higher infection, hospitalization and mortality risk than individuals without (death rate of 8.5% vs. 4.7%; [6]). Multiple reasons including illness symptomatology, such as depression and psychosis, financial barriers and cognitive deficits are suggested to be responsible for this issue. Additionally, struggling with obtaining health care, stigma, discrimination, reduced communication between patients and physicians as well as inadequacies of health providers in being able to handle emotional problems of individuals with mental disorders increases vulnerability [8], [9].
Recent studies indicate that higher rates of a first manifestation of psychiatric illness were shown after COVID-19 compared to other infectious diseases [5]. In addition, a more severe course of COVID-19 has been found in individuals with a pre-existing mental disorder [6], [10], with overlapping immunological changes and cytokine storm possibly being involved. Chronic low-grade inflammation in acute illness episodes, but also in subclinical episodes, are discussed as one of the most important aetiopathophysiological underpinning of MDD [11] and BD [12], [13], [14]. Moreover, acute infections such as COVID-19 might trigger relapse or exacerbation of mental disorders due to shared immunological alterations and as a psychosocial stressor [15], [16], [17].
Vaccines help to prevent infections or at least prevent a severe course of infectious diseases. Few studies focused on worries, hesitancies and prevalence rates of vaccinations of individuals with mental disorders mostly investigating influenza vaccines showing controversial findings of either higher rates, lower rates or no difference compared to the general population [18]. Results from trials surveying attitudes of parents to have vaccinated their children found some relevant aspects such as knowledge about consequences without vaccinations, communication and media. A general vaccine hesitancy was found in parents receiving their information from mass-media, agreeing with politicians objecting vaccinations as well as believing in economics reasons of pharmaceutical companies [19]. Parents who have heard about HPV and knew about the potential risk reduction for cancer with an HPV vaccine had less concerns about this special vaccine [20].
Vaccines influence the immune system mostly by stimulating the formation of antibodies, but also by evoking a T-cell response In recent literature reviews, conflicting results on vaccine immunogenicity in individuals with MDD, BD, and schizophrenia were found [18], [21]. The interpretation of results was limited by small sample sizes, cross-sectional study designs and heterogeneity of the studies. Overall, due to the higher rates of infection, more severe courses of COVID-19, higher mortality, and the risk of relapse or onset of psychiatric symptomatology, the benefits of vaccines against COVID-19 seem to outweigh any potential risks of vaccination in individuals with mental illness.
Recent studies investigated the willingness to get vaccinated against COVID-19 of the general population in different countries. A large-scale study in the UK found a hesitancy to get vaccinated in 15.4% of the population regardless of an existing depression or anxiety disorder [22]. In France, 28.8% of a representative working-age population reported a refusal of a vaccination. The reluctant attitude positively correlated with age, female gender, lower education level, few vaccinations in the past and a lack of chronic condition except hypertension [23]. In Germany, 64.5% of the respondents would absolutely accept a COVID-19 vaccination and 13.8% would rather accept it [24]. In clinical samples, beside current psychiatric symptomatology (depression, mania, psychosis, anxiety), cognitive deficits, and limited access to health care, an individual’s thoughts and worries (attitudes, assumptions, beliefs, expectations) influence the willingness to get vaccinated. Preliminary data from Maguire et al. [25] show that individuals with schizophrenia had a lower willingness to self-isolate and were more concerned about “catching the flu” from vaccinations than the general population. Additionally, individuals with schizophrenia described concerns about side effects, cost and transport to the clinic [25]. To our knowledge there is no study about the willingness of individuals with AD to get vaccinated against COVID-19 yet.
This survey aimed to investigate (1) the attitude of individuals with AD in comparison to mentally healthy controls (HC) about vaccinations in general, (2) the willingness of individuals with AD compared to HC to get vaccinated against COVID-19 and (3) concerns about the vaccines against COVID-19. We hypothesized that individuals with AD would have lower vaccination rates and a lower willingness to get vaccinated due to fears of side effects than individuals without mental disorders.
Methods
Procedure and participants
The online survey was conducted at the Medical University of Graz, Austria, Department of Psychiatry and Psychotherapeutic Medicine. Individuals with MDD and BD were either former or present inpatients or outpatients and therefore have been diagnosed by a clinician according to the International Statistical Classification of Diseases and Related Health Problems (ICD)-10 before. Inclusion criteria were the diagnosis of a psychiatric disorder, currently with or without illness symptomatology but with the ability to judge or, the absence of any psychiatric history in HC. Exclusion criteria were the lack of ability to judge and make decisions and the presence of dementia or another severe and acute cerebral disease (delirium, brain tumor, traumatic brain injury. HC were recruited from the general population via written invitations and word of mouth (circle of acquaintances, medical students, medical staff). Participants had to be of legal age and had given online informed consent prior to their participation in this study. Participation in the online survey was voluntary, anonymous and without a monetarily or other compensation.
From April 28th to May 20th 2021, the survey was sent out to participants using the software LimeSurvey 3.04 [26]. It was not possible to skip a question, but with some questions (somatic/psychiatric diagnosis; reasons for previous COVID-19 vaccination; reasons for hesitancy) there was a free text option. The sample size was calculated with the statistical programme GPower using a power of 95%, an α of 0.05 and a medium effect size of 0.25 aiming to detect a difference between patients with mental disorders and HC regarding their vaccination willingness. Nevertheless, due to exploratory reasons, we aimed to include as much individuals as possible in this pilot survey.
In total, 165 participants completed the survey and 181 opened it but did not finish it. Of the 165 participants, 76 individuals had a psychiatric diagnosis but groups with psychotic disorders (n = 3), personality disorders (n = 2) and addictive disorders (n = 2) as main diagnosis were too small and therefore excluded. The current investigation included 59 individuals with AD (n = 26 MDD and n = 33 BD) and 59 HC matched according to age and sex. The study has been approved by the local ethics committee (Medical University of Graz, Austria; EK-number: 33-229 ex 20/21) in compliance with the current revision of the Declaration of Helsinki, ICH guideline for Good Clinical Practice and current regulations.
At the time of the start of the survey, 27.92% of the general population in Austria had been at least partially vaccinated against COVID-19 and 10.55% had been fully immunized. At the end of the survey, 41.22% had at least received the first shot and 15.44% were fully immunized [27].
Materials
Sociodemographic questionnaire
Relevant sociodemographic and COVID-19 related data were recorded with a self-constructed questionnaire in German language. Specifically, we collected data on sociodemographic variables (age, sex, education, profession), medical history (psychiatric and somatic diseases, smoking), COVID-19 status (tested positive in the past), and COVID-19 vaccination status (vaccinated yes/no; type of vaccine; resulting side effects).
Willingness to vaccinate questionnaire
We constructed a questionnaire assessing the willingness to vaccinate in general (with 8 items) and the willingness to be vaccinated against COVID-19 (with 9 items) in German language. Items were rated on a five-point Likert scale scale (0 = disagree, 1 = rather disagree, 2 = neutral, 3 = rather agree, 4 = agree) and are described in Table 1. A variable for willingness to vaccinate in general and another variable for the willingness to be vaccinated against COVID-19 was constructed by reversing polarity of certain items as described in Table 1 and consecutively building mean scores for each scale. The newly constructed variables indicated an adequate internal consistency for the items of these scales (Cronbach’s alpha = 0.85 respectively 0.86). Moreover, the survey inquired concerns and reasons for and against the vaccination with a free text.
Table 1.
Items of the constructed variables to assess the “Willingness to vaccinate in general” and the “willingness to be vaccinated against COVID-19”.
| Variable: willingness to vaccinate in general1 | |
| Item 1 | The benefit of vaccinations clearly outweighs the risk |
| Item 2 (recoded) | The risk of immediate side effects from vaccinations clearly outweighs the benefits |
| Item 3 (recoded) | The risk of long-term side effects of vaccinations clearly outweighs the benefits |
| Item 4 | Vaccinations offer good protection for the general population |
| Item 5 (recoded) | I see little benefit for the general population |
| Item 6 (recoded) | I am concerned that vaccinations interact with other medication that I take |
| Item 7 # | I get vaccinated against tick-borne encephalitis regularly |
| Item 8 | I get vaccinated against influenza regularly |
| Variable: willingness to be vaccinated against COVID-192 ## | |
| Item 1 | The benefit of the COVID-19 vaccination clearly outweighs the risk |
| Item 2 (recoded) | The risk of the vaccination clearly outweighs the benefits |
| Item 3 | I want to prevent a personally serious COVID-19 course with a vaccination |
| Item 4 | I might want to help protect others with my own vaccination |
| Item 5 (recoded) | I am concerned that the vaccination will interact with other medication that I take |
| Item 6 | It takes little effort for me to get vaccinated |
| Item 7 | I will mainly get vaccinated because relatives advise me to do so |
| Item 8 | I will mainly get vaccinated because doctors advise me to do so |
| Item 9 (recoded) | I generally do not see any benefit in vaccinations |
Note. 1 Mean of the following eight items on a five-point Likert scale; internal consistency for the items of this scales are given (Cronbach’s alpha = 0.85); 2 Mean of the following eight items on a five-point Likert scale; internal consistency for the items of this scales are given (Cronbach’s alpha = 0.86); # as Austria is an endemic region of tick-borne, regular vaccinations are recommended; ## All questions assess intrinsic willingness to be vaccinated against COVID-19, except for two items which targeted extrinsic motivated willingness to be vaccinated (“I will mainly get vaccinated because relatives advise me to do so”; “I will mainly get vaccinated because doctors advise me to do so”).
Hesitancy to vaccinate questionnaire
To assess hesitancy towards getting vaccinated, participants were asked to answer the following questions on a scale from 0 to 100%: “How likely is it that you will be vaccinated against COVID-19 as soon as you get the chance?”; “How likely is it that you will be vaccinated against COVID-19 within the next year?”; “How likely is it that you will be vaccinated against COVID-19 within five years?”.
If participants answered that they plan to wait for their vaccination, the following questions were presented with a five-point Likert scale option (0 = disagree, 1 = rather disagree, 2 = neutral, 3 = rather agree, 4 = agree): “I am worried about immediate side effects”; “I am worried about long-term side effects”; “I currently see no personal benefit as I have already had COVID-19”; “I do not see personal benefit as I am not expecting a severe COVID-19 course”; “I currently do not see a personal benefit as I generally do not see any benefits in vaccinations”; “I fear that the vaccination will not be effective against infection but only against severe COVID-19 courses and I personally do not expect this”; “It is too difficult to get the vaccination”; “Vaccine development was faster than other vaccine approvals”; “In my opinion the vaccines have not been tested thoroughly”; “other reasons”.
Statistical analyses
All analyses were performed with the IBM Statistical Package for Social Sciences (SPSS), version 25.0, with all hypotheses being tested two-sided at an α-level of 0.05. For the variable willingness to be vaccinated against COVID-19, values of the item analysis (item difficulty and item discrimination values) can be found in Table 2.
Table 2.
Item analysis of the variable willingness to be vaccinated against COVID-19.
| Variable | Item Difficulties | Item Discrimination |
|---|---|---|
| Item 1: Benefit outweighs risk | 84.5 | 0.66 |
| Item 2: Risk outweighs benefit” (recoded) | 66.36 | 0.47 |
| Item 3: Prevention of a serious COVID-19 course | 80.75 | 0.72 |
| Item 4: Help protect others with own vaccination | 84.00 | 0.74 |
| Item 5: Concerned of interaction with other medication (recoded) | 81.97 | 0.38 |
| Item 6: Little effort to get vaccinated | 84.50 | 0.63 |
| Item 7: Mainly because relatives advise | 20.50 | 0.22 |
| Item 8: Mainly because doctors advise | 30.50 | 0.36 |
| Item 9: Generally no benefit in vaccinations (recoded) | 90.59 | 0.65 |
Note. N = 118. Item coding from 0 to 4.
Chi-square tests (nominal data), were conducted to test for differences between the AD and HC group in descriptive variables. T-tests were used to calculate the differences between the BD and HC group in metric data (willingness to get vaccinated in general and against COVID-19). An exploratory principal axis factor analysis was conducted to assess the underlying structure of the willingness to be vaccinated against COVID-19 items. Two factors were obtained (intrinsic and extrinsic motivated willingness to be vaccinated against COVID-19). Consecutively, t-Tests were used to calculate the differences between the BD and HC group in both factors.
For the exploratory principal axis factor analysis across all items of the willingness to be vaccinated against COVID-19 variable, suitability of data was assessed in advance. The Kaiser-Meyer-Olkin (KMO) criterion verified an adequate sample for carrying out the analysis (KMO = 0.83, and all KMO values for the single items were greater than 0.53, thereby above the acceptable threshold-value of 0.50). Bartlett’s test of sphericity indicated that correlations between all items were adequate for factor analysis (χ2(36) = 514.37, p <.001). An initial analysis was administered to obtain eigenvalues for each factor. Kaiser’s eigenvalue extraction criterion and the scree plot suggested the extraction of two factors (intrinsic and extrinsic motivated willingness to be vaccinated against COVID-19), which explained 56.09% of the total variance. Table 3 shows the unrotated factor loadings. Since normal distribution was not given for the factor of internal and external motivated willingness, the following analyses regarding this factor were calculated with 95%-BCa Bootstrapping confidence intervals.
Table 3.
Unrotated factor loadings for willingness to be vaccinated against COVID-19 items.
| Variable | Factor loading |
|
|---|---|---|
| Factor Internal Motivation |
Factor External Motivation |
|
| Item 1: Benefit outweighs risk Item 2: Risk outweighs benefit” (recoded) Item 3: Prevention of a serious COVID-19 course Item 4: Help protect others with own vaccination Item 5: Concerned of interaction with other medication (recoded) Item 6: Little effort to get vaccinated Item 7: Mainly because relatives advise Item 8: Mainly because doctors advise Item 9: Generally no benefit in vaccinations (recoded) |
0.81 0.58 0.86 0.82 0.50 0.75 0.16 0.33 0.75 |
−0.10 −0.17 −0.01 −0.02 −0.21 −0.06 0.74 0.71 −0.11 |
Note. Extraction method = Principal axis factoring.
Results
Table 4 presents the sociodemographic and clinical data and the differences between the groups.
Table 4.
Sociodemographic and clinical data of participants with AD and HC.
| AD n = 59 |
HC n = 59 |
statistics | p | |
|---|---|---|---|---|
| Sex n (%) Female Male |
41 (69.5) 18 (30.5) |
41 (69.5) 18 (30.5) |
χ 2(1) = 0.00 | 1.000 |
| Age M (SD) | 42.15 (13.41) | 42.66 (13.78) | T (1 1 6) = 0.20 | 0.839 |
| Highest completed education % Compulsory school Apprenticeship Vocational school High school University |
3.4 11.9 8.5 28.8 47.4 |
1.7 5.1 8.5 30.5 54.3 |
χ 2(6) = 6.37 | 0.383 |
| Current occupation % Unemployed Employed Self-employed In training/ education Retirement Rehabilitation measures Grace period |
13.6 32.2 5.1 3.4 28.8 13.6 3.4 |
3.4 62.7 10.2 11.9 8.5 0 3.4 |
χ 2(6) = 27.71 |
< 0.001 |
| Somatic disorder % Hypertension Asthma COPD Acute airway/lung disease Diabetes mellitus Coronary heart disease Immunosuppressive treatment Endocrine disease |
13.6 3.4 0.0 1.7 6.8 3.4 0.0 8.5 |
10.2 3.4 1.7 0.0 1.7 0.0 3.4 0.0 |
χ 2(1) = 0.32 χ 2(1) = 0.00 χ 2(1) = 1.01 χ 2(1) = 1.01 χ 2(1) = 1.88 χ 2(1) = 2.03 χ 2(1) = 2.03 χ 2(1) = 5.22 |
0.569 1.000 0.315 0.315 0.170 0.154 0.154 0.022 |
| Smoking % | 30.5 | 23.7 | χ 2(1) = 0.69 | 0.408 |
| Principal psychiatric diagnosis % MDD BD Psychiatric comorbidity % Anxiety disorder Eating disorder Substance abuse disorder Personality disorder |
44.1 55.9 27.1 8.5 6.8 15.3 |
Note. AD = affective disorders; HC = healthy controls; MDD = major depressive disorder; BD = bipolar disorder; M = mean; SD = standard deviation; COPD = chronic obstructive pulmonary disease; significant differences in bold letters.
There was a difference between individuals with AD and HC in their willingness to get vaccinated in general. HC had a higher willingness than individuals with AD (MAD = 2.71, SD = 0.94 vs MHC = 3.07; SD = 0.85; T(1 1 6) = 2.20; p =.030).
Two individuals of the AD group and five of the HC group had a COVID-19 infection in the past. None of the participants was suffering from COVID-19 at the time of the study. Table 5 shows the knowledge and willingness concerning the vaccination against COVID-19. There was no difference in the self-rated knowledge about the vaccinations. Significantly more HC have been vaccinated at time of testing. Reasons for having been prioritized for the vaccination were risk for a severe illness course (AD 3.4% vs HC 1.7%), working in health care (AD 6.8% vs HC 32.2%), age (AD 1.7% vs HC 3.4%), pedagogical work (AD 5.1% vs HC 3.4%), and no specific reason (AD 10.2% vs HC 3.4%).
Table 5.
Differences between AD and HC in COVID-19 vaccination status and willingness to get vaccinated.
| AD n = 59 |
HC n = 59 |
Statistics | p | |
|---|---|---|---|---|
| Subjective knowledge about COVID-19 vaccination % Very low Rather low Neither high nor low Rather high Very high |
3.4 8.5 20.3 49.2 18.6 |
0 6.8 23.7 45.8 23.7 |
X2(4) = 2.70 | 0.610 |
| Already vaccinated % | 28.3 | 52.0 | X2(1) = 6.03 | 0.014 |
| Option for a vaccination in the past and refusal % | 10.2 | 15.3 | X2(1) = 0.69 | 0.407 |
| Willingness for vaccination against COVID-19 M (SD)a | 2.69 (0.76) | 2.88 (0.76) | T(1 1 6) = 1.41 | 0.161 |
| Internal motivated willingness to get vaccinated M (SD) | −0.12 (0.96) | 0.08 (1.03) | T(1 1 4) = 1.10 | 0.273 |
| External motivated willingness to get vaccinated M (SD) | 0.07 (0.94) | −0.01 (0.86) | T(1 1 4) = −0.48 | 0.635 |
| Either already vaccinated of willing to get vaccinated as soon as possible M (SD) b | 82.14 (33.84) | 86.41 (30.22) | T(1 1 6) = 0.72 | 0.471 |
| Willingness for vaccination of the currently not vaccinated participantsb As soon as possible Within the next year Within the next five years |
n = 38 78.13 (36.87) 80.71 (35.09) 83.66 (34.28) |
n = 23 76.00 (35.80) 79.70 (34.83) 82.91 (30.73) |
T(59) = −0.22 T(59) = −0.11 T(59) = −0.09 |
0.826 0.913 0.932 |
Note. AD = affective disorders; HC = healthy controls; M = mean; SD = standard deviation; a = mean of five-point likert scale: “the benefit of the COVID-19 vaccination clearly outweighs the risk”, “the risk of the vaccination clearly outweighs the benefits” (recoded), “I want to counteract a personally serious COVID-19 course with a vaccination”, I might want to help protect others with my own vaccination”, “I am concerned that the vaccination interact with other medication that I take” (recoded), “It takes little effort for me to get vaccinated”, “I will mainly get vaccinated because relatives advise me to do so”, “I will mainly get vaccinated because doctors advise me to do so”, “I generally do not see any benefit in vaccinations” (recoded); b = response scale 0–100%; significant results in bold letters.
Of the already vaccinated individuals with AD, 40.0% got the Pfizer-BioNTech COVID-19 vaccine, 26.7% the COVID-19 Vaccine Moderna, and 33.3% the Oxford/AstraZeneca COVID-19 vaccine. In the HC group, 46.2% were vaccinated with the BioNtech/Pfizer, 3.8% with the Moderna and 50.0% with the AstraZeneca vaccine. There was no difference between the groups between suffering from side effects after the shots (χ 2(6) = 4.87, p =.561). Participants reported no side effects at all (AD 20.0% vs HC 26.9%), very mild symptoms such as fatigue for some hours (AD 6.7% vs HC 15.4%), mild symptoms for one to two days (AD 20.0% vs HC 7.7%), moderate symptoms with restriction in daily routine for one to two days (AD 20.0% vs HC 11.5%), severe symptoms as fever and reduced performance for one to two days (AD 6.7% vs HC 19.2%), moderate symptoms longer than two days (AD 6.7% vs HC 11.5%), and severe symptoms longer than two days (AD 20.0% vs HC 7.7%).
No difference in the constructed variable to test the willingness to be vaccinated against COVID-19 was found between the groups. T-tests showed that there was no difference between individuals with AD and HC regarding their intrinsic as well as their extrinsic motivated willingness to get vaccinated. Furthermore, the desire to get vaccinated as soon as a slot was available in the group of still unvaccinated persons was rather high. No differences were demonstrated in the request of being vaccinated as soon as possible or within one year or within five years.
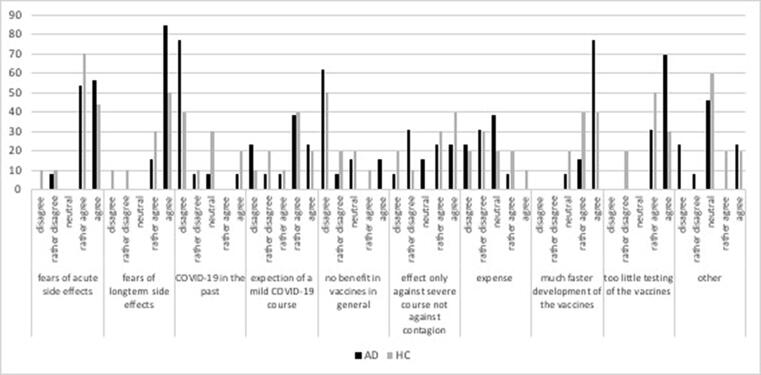
Reasons for waiting to get vaccinated against COVID-19 vaccination are demonstrated in Fig. 1. Many of the HC, but even more individuals with AD, reported fears of acute and/or long-term side effects and the fast development of the vaccines to be the main reasons. Other free text answers of individuals with AD were “Low risk of infection because of little social contact”, “Trust in immune system”, and “Intervention in human genetics”. HC gave the following explanations: “Completely new drug approval in short time”, “Severe COVID-19 courses are rare and expected more in elderly; therefore, no need to risk side effects for the whole population”, “Would like to choose the vaccine”, “Not sufficiently informed about consequences of vaccination in terms of fertility and genetic defects”.
Fig. 1.
Reasons for waiting to get vaccinated against COVID-19 of individuals with AD and HC.
Discussion
This survey found an overall high willingness (about 80%) of individuals with AD and HC to get vaccinated against COVID-19 and found individuals with AD were more skeptical about vaccinations in general, but there was no difference between the groups in the willingness to get vaccinated against COVID-19. This high percentage of willingness was also reported in a Chinese study where 96.2% of 76 of individuals with depression or anxiety disorder and 100% of 134 HC wanted to receive the COVID-19 vaccine [28]. Similar in Denmark high rates of willingness were found in individuals with mental disorders (84.8%) as well as the general population (89.5%) [29]. An UK survey found a pre-pandemic diagnosis of depression or anxiety not to be related to the willingness to get vaccinated against COVID-19 [30]. Reasons for waiting in the present survey were mainly fears of acute and/or long-term side effects and the fast development of the vaccines. The most important finding of our questionnaire study was that the willingness to be vaccinated against COVID-19 was rather high in the study population and did not differ between AD and HC. This is a positive finding, since individuals with AD represent a high-risk group for a COVID-19 infection and are thus more in need of a vaccination than the average population. The rather high willingness indicated in the current study will hopefully then lead to a high vaccination rate not only in the general population, but also in the high-risk group of individuals with AD. Moreover, we found that the vaccination rate of HC at the time of the study was significantly higher than of individuals with AD and that the main reasons for waiting to get vaccinated were fears of acute and/or long-term side effects and the fast development of the vaccines. Last, the willingness to get vaccinated in general was slightly higher among HC than individuals with AD.
In this cohort, HC were significantly more often vaccinated against COVID-19 than individuals with AD. In comparison to the general Austrian population at that time, our HC cohort was vaccinated to a higher percentage while individuals with AD were under the average. The difference between the groups might be explained by the difference in occupational status, as most of the HC were employed while more than half of the individuals with AD were unemployed, retired or in rehabilitation measures. People in active employment, especially in the fields of health care and education were prioritized for vaccination in Austria. In our study, about 82% of the participants with AD and 86% of HC have been vaccinated or reported to be willing to get vaccinated as soon as possible. Although limited to a small number of included trials, some studies found a revealed attenuated immune response to vaccinations in general (mostly influenza investigated) [18], [21], leading to the assumption that this low efficacy might lead to a lower willingness to get vaccinated. Of the not yet vaccinated individuals, the willingness increases from 78.1% as soon as possible to 83.7% within the next five years in individuals with AD and from 76.0% to 82.9% in HC, respectively. At the time of the revision of this manuscript (December 2021), 72.7% of the Austrian population were vaccinated twice and 41.3% already got the recommended third shot [31], [32], although enough vaccines for the whole population are available. Contemporaneously, getting three vaccinations, in particular those based on mRNA, has been found to reduce the risk of infection and severe courses of COVID-19 with no safety concerns [33], [34]. The gap between the study results and current prevalences might be influenced by remaining fear of the vaccines (about effects on fertility [35], adverse side effects [36]), uncertainty with changing regulations and frustration in particular concerning political statutes [37]. In general, a survey of 811 healthcare workers before the possibility to get vaccinated showed that people needing more information about COVID-19 and people believing COVID-19 not to be a severe illness had more concerns about this vaccine [38]. Concluding, specific programs to educate the population about the efficacy and evidence-based recommendations are highly needed.
Special vaccination programs might be necessary to reach individuals with mental disorders and provide information and motivation as well as easy access to vaccinations [39]. These programs should be based on scientific actual evidence and transport this knowledge in an appropriate language. A systemic review by Kan and Zhang [40] identified recommendations and advice for vaccinations as a factor for higher willingness in older adults and in individuals with severe mental illness. As a consequence, higher vaccination rates were shown when using special vaccination programs [41]. Therefore, for mentally ill individuals with frequent medical visits, doctors’ recommendations as well as reminders, can be an important tool in increasing the vaccine uptake in this group. All these approaches could potentially help reaching individuals with AD and subsequently increase motivation and willingness to get vaccinated. However, as proposed by Paul and colleagues [42], such campaigns need to be tailored to the specific AD sub-group and contain information about the interaction between COVID-19 and AD, and how the vaccination could help. Examples from other countries with a high vaccination rate such as Israel show that tailoring the measures to a concerned sub-group has helped to increase the population coverage beyond 60% [43]. Further, it was shown that trust in governmental information, the health care system, information regarding vaccine safety in adequate healthy literacy formats and role-modeling by politicians were the key for a successful vaccination program in Israel [44]. An experiment in China in August 2020 showed that people who hesitated to get vaccinated first switched with their attitude when they were prohibited to enter public spaces or public transportation via a mobile based technology [45]. Moreover, telephone or platform-based interactions with clinicians or experts could help raising awareness for the importance of getting vaccinated. For individuals with AD, leaving their house due to symptoms of anxiety or social withdrawal poses a challenge when getting the COVID-19 vaccination. Thus, as proposed by Miles and colleagues [41], mobile vaccination services should be introduced to reach out to this group.
Importantly, regardless of the COVID-19 vaccination, willingness to be vaccinated was generally lower among persons with AD than HC. This could be explained by the fact that these individuals receive less somatic health care in general [8], are thus less familiar with several vaccinations and subsequently less willing to get vaccinated in general. The reasons were considerations of benefits, potential risks, and expected or experienced side effects, and possible medication interaction. In addition, protection for the general population, regular tick-borne and annual influenza vaccinations were asked. Both, individuals with AD and HC, showed quite a good willingness with means in the medium to higher range, however, there was a significant difference between the groups. Studies on prevalence rates of vaccinations in general in cohorts with mental disorders mainly focused on influenza vaccinations and show inconsistent results. While some found higher rates of vaccinations in individuals with depressive symptomatology, mainly against influenza [46], [47], [48] or against influenza and pneumococcus [41], [49], others demonstrated significant lower influenza vaccination rates [50], [51], [52], [53] or influenza and pneumococcal vaccination rates [54]. Other studies found no differences in vaccination prevalence rates in individuals with mental health conditions compared to the general population [55], [56], [57], [58]. Miles and colleagues [41] found higher rates of influenza and pneumococcal vaccinations in individuals with severe and persistent mental illness but lower rates of vaccines against pertussis, hepatitis A and B as well as mumps-measles-rubella.
In this study, no difference in willingness to get vaccinated against COVID-19 was found. Furthermore, no differences in intrinsic or extrinsic motivation were prominent between the groups. Many of the HC, but even more individuals with AD reported fears of acute and/or long-term side effects and the fast development of the vaccines to be the main reasons for waiting to get vaccinated. A recent review showed an increase of psychiatric symptoms e.g. anxiety, depression and stress in individuals with AD during the pandemic [59]. Especially people with a low socioeconomic environment, lack of social support, inadequate information about COVID-19 and a shortage in mental health-services showed a mental-wellbeing impairment. Suicidal ideations could also worsen in psychiatric patients due to the pandemic associated stress, anxiety and depression [60]. To treat these increased symptoms and additionally provide a comprehensive vaccination-education an expansion of the psychosocial and psychiatric infrastructure would be desirable. For the moment, telephone-based or group interventions might be efficient.
In literature, there are hints that sociodemographic parameters like age (being very young or very old were associated with hesitancy), female gender, lower educational level, loss of income during the pandemic, as well as perceiving inconsistent information about vaccines and the pandemic influence the attitudes towards the COVID-19 vaccination [23], [61]. Additionally, distrust in the government of Austria was associated with a hesitancy to get vaccinated [62]. Our results show that a pre-existing AD is not a risk factor for a reluctant attitude. Nevertheless, the survey was completed by individuals with MDD or BD, who were informed about the study in a familiar setting. Maybe, for individuals with more severe depressive or psychotic symptomatology or little insight into their disease, their symptoms or (lack of) knowledge might influence the willingness to get vaccinated. The severity of symptomatology of the severe mentally ill could potentially influence the frequency of access to health care. Anxiety and somatic complaints in depression might lead to an overuse of medical services, while lack of motivation and hopelessness to a decreased use in preventive services [53].
Additionally, the presence of somatic comorbidities might increase the regularity of doctor visits [51]. On the one hand, this might lead to more frequent explanations of and recommendations for preventive vaccinations and therefore contribute higher vaccinations rates [47]. The more health problems the individuals had and the more medication they used, the higher was the vaccination rate [49]. Another study found that mentally ill individuals with physical comorbidities and individuals with antidepressant treatment were more likely to be vaccinated than people without comorbidities and treatment [47]. Individuals taking antidepressants might represent an especially compliant population and are, as a result, more likely to follow doctors’ recommendations to be vaccinated. On the other hand, somatic comorbidities could also lead to lower vaccination rates [51], [53]. Physicians might focus on the mental health problems and neglect somatic health status and as a result focus less on the preventive care in individuals with mental disorders.
Due to higher COVID-19 infection rates and related mortality as well as the elevated risk of psychiatric relapse, vaccinating individuals with AD against COVID-19 is of particular importance. Individuals with AD and HC, who were already vaccinated, reported no difference in the occurrence of side effects. This is contrary to some studies investigating side effects of influenza vaccines which found higher prevalence of mood disturbances [63], [64] and paresthesia [65]. A greater increase in inflammatory markers after vaccination in individuals with depression and anxiety compared to HC was found in one investigation [66]. This increase in proinflammatory cytokines can elicit “sickness behavior” in individuals which is characterized by lethargy, anhedonia, loss of appetite, and social isolation [67] and lead to subjective side effects, like fatigue or headache after vaccination. There were no studies on severe adverse events after vaccinations in individuals with mental disorders. Although our sample was too small to focus on side effects in detail, the results indicate that there is no special need to worry about acute side effects after vaccination against COVID-19 for individuals with AD. Nonetheless, further studies have to investigate long-term effects as well as interactions between psychopharmaceuticals and vaccines against COVID-19.
Limitations and strengths
There are several limitations of this study. Due to the online design, no objective rating of current psychopathological symptoms was assessed. Furthermore, willingness to get vaccinated in general and against COVID-19 in particular were self-created variables without reference values and no standardization. The sample size was too small to conduct analyses investigating the role of side effects. Another limitation is that we cannot generalize from our sample to the population as online surveys are completed only by persons who are literate and who have access to the internet, and by those who are sufficiently biased to be interested in the subject. As the invited persons, who did not complete the questionnaire were not further contacted and asked for their motivations not to participate a selection bias cannot fully be excluded. Furthermore, people might tend to answer in a way they except to be more socially acceptable (social desirability bias).
In contrast, this study shows a good picture of the overview of a high-risk group to this present and highly relevant topic. Other strengths are the well-defined and diagnosed investigation group and the aged and sex-matched control group. Our self-constructed questionnaire indicated good internal consistency and differentiated excellently between intrinsic and extrinsic motivations for vaccination and could thus be further developed in future studies examining attitudes towards COVID-19 vaccinations. Last, this study represents the current view on the pandemic and the related vaccination attitudes of people in Austria, thus giving the opportunity for politics, scientists and healthcare providers to consider these attitudes in further vaccination campaigns. Reaching all population groups is of utmost importance since a sufficiently high vaccination rate is necessary to save human lives, relieve the healthcare system and find a way out of the pandemic, especially for those in need of a stable healthcare such as high-risk patients like individuals with AD.
Conclusion
The results of this survey indicate a high acceptance of vaccination against COVID-19. No difference in the willingness to get vaccinated between individuals with AD and HC was observed. As individuals with AD suffer more prominently from infectious diseases than the general population and COVID-19 is more serious with higher mortality in psychiatric patients resulting often in psychiatric relapse, preventive strategies like vaccinating should be promoted in this group. It is important to help individuals with AD to overcome barriers such as negative beliefs and concerns about acute and/or long-term side effects. For this purpose, telephone-based interventions or in-person education by reference clinicians might be a promising approach to explain the mechanism of action of the vaccines and to negate wrong information these individuals might have about the COVID-19 vaccines. This could help raise the willingness to get vaccinated and as a result the vaccination rate in this group.
Author contributions
FF has designed the study, written the first and last draft, was responsible for the study conception, coordination, and publication of data. NB and ER were involved in study conceptualization and writing. MR was responsible for data collection. ES and ND were involved in statistical analyses. All authors were responsible for proofreading and revising the manuscript.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We especially thank all study participants for their kind participation.
References
- 1.De Berardis D., Fornaro M., Valchera A., Cavuto M., Perna G., Di Nicola M., et al. Eradicating Suicide at Its Roots: Preclinical Bases and Clinical Evidence of the Efficacy of Ketamine in the Treatment of Suicidal Behaviors. Int J Mol Sci. 2018;19(10):2888. doi: 10.3390/ijms19102888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Hert M., Dekker J.M., Wood D., Kahl K.G., Holt R.I., Möller H.J. Cardiovascular disease and diabetes in people with severe mental illness position statement from the European Psychiatric Association (EPA), supported by the European Association for the Study of Diabetes (EASD) and the European Society of Cardiology (ESC) Eur Psychiatry. 2009;24(6):412–424. doi: 10.1016/j.eurpsy.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 3.De hert M., Correll C.U., Bobes J., Cetkovich-bakmas M., Cohen D., Asai I., et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10(1):52–77. doi: 10.1002/j.2051-5545.2011.tb00014.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seminog O.O., Goldacre M.J. Risk of pneumonia and pneumococcal disease in people with severe mental illness: English record linkage studies. Thorax. 2013;68(2):171–176. doi: 10.1136/thoraxjnl-2012-202480. [DOI] [PubMed] [Google Scholar]
- 5.Taquet M., Luciano S., Geddes J.R., Harrison P.J. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8(2):130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang Q., Xu R., Volkow N.D. Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatry. 2021;20(1):124–130. doi: 10.1002/wps.20806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang H., Chen W., Hu Y., Chen Y., Zeng Y.u., Sun Y., et al. Pre-pandemic psychiatric disorders and risk of COVID-19: a UK Biobank cohort analysis. Lancet Healthy Longev. 2020;1(2):e69–e79. doi: 10.1016/S2666-7568(20)30013-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bradford D.W., Kim M.M., Braxton L.E., Marx C.E., Butterfield M., Elbogen E.B. Access to medical care among persons with psychotic and major affective disorders. Psychiatr Serv. 2008;59(8):847–852. doi: 10.1176/ps.2008.59.8.847. [DOI] [PubMed] [Google Scholar]
- 9.De Hert M., Cohen D., Bobes J., Cetkovich-Bakmas M., Leucht S., Ndetei D.M., Newcomer J.W., Uwakwe R., Asai I., Möller H.J., Gautam S., Detraux J., Correll C.U. Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry. 2011;10(2):138–151. doi: 10.1002/j.2051-5545.2011.tb00036.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee S.W., Yang J.M., Moon S.Y., Yoo I.K., Ha E.K., Kim S.Y., et al. Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: a nationwide cohort study. Lancet Psychiatry. 2020;7(12):1025–1031. doi: 10.1016/S2215-0366(20)30421-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Howren M.B., Lamkin D.M., Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: a meta-analysis. Psychosom Med. 2009;71(2):171–186. doi: 10.1097/PSY.0b013e3181907c1b. [DOI] [PubMed] [Google Scholar]
- 12.Anderson G., Maes M. Bipolar disorder: role of immune-inflammatory cytokines, oxidative and nitrosative stress and tryptophan catabolites. Curr Psychiatry Rep. 2015;17(2):8. doi: 10.1007/s11920-014-0541-1. [DOI] [PubMed] [Google Scholar]
- 13.Bai Y.-M., Su T.-P., Li C.-T., Tsai S.-J., Chen M.-H., Tu P.-C., et al. Comparison of pro-inflammatory cytokines among patients with bipolar disorder and unipolar depression and normal controls. Bipolar Disord. 2015;17(3):269–277. doi: 10.1111/bdi.12259. [DOI] [PubMed] [Google Scholar]
- 14.Leboyer M., Soreca I., Scott J., Frye M., Henry C., Tamouza R., et al. Can bipolar disorder be viewed as a multi-system inflammatory disease? J Affect Disord. 2012;141(1):1–10. doi: 10.1016/j.jad.2011.12.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marangoni C., Hernandez M., Faedda G.L. The role of environmental exposures as risk factors for bipolar disorder: A systematic review of longitudinal studies. J Affect Disord. 2016;15(193):165–174. doi: 10.1016/j.jad.2015.12.055. [DOI] [PubMed] [Google Scholar]
- 16.Miller B.J., Graham K.L., Bodenheimer C.M., Culpepper N.H., Waller J.L., Buckley P.F. A prevalence study of urinary tract infections in acute relapse of schizophrenia. J Clin Psychiatry. 2013;74(3):271–277. doi: 10.4088/JCP.12m08050. [DOI] [PubMed] [Google Scholar]
- 17.Page L.A., Seetharaman S., Suhail I., Wessely S., Pereira J., Rubin G.J. Using electronic patient records to assess the impact of swine flu (influenza H1N1) on mental health patients. J Ment Health. 2011;20(1):60–69. doi: 10.3109/09638237.2010.542787. [DOI] [PubMed] [Google Scholar]
- 18.Bonkat N, Fellendorf FT, Dalkner N, Reininghaus EZ. Severe mental disorders and vaccinations – a systemic review. World J Biol Psychiatry. 10.1080/15622975.2021.2013095. [DOI] [PubMed]
- 19.Bianco A., Mascaro V., Zucco R., Pavia M. Parent perspectives on childhood vaccination: How to deal with vaccine hesitancy and refusal? Vaccine. 2019;37(7):984–990. doi: 10.1016/j.vaccine.2018.12.062. [DOI] [PubMed] [Google Scholar]
- 20.Della Polla G., Pelullo C.P., Napolitano F., Angelillo I.F. HPV vaccine hesitancy among parents in Italy: a cross-sectional study. Hum Vaccin Immunother. 2020;16(11):2744–2751. doi: 10.1080/21645515.2020.1744367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xiao K., Gillissie E.S., Lui L.M.W., Ceban F., Teopiz K.M., Gill H., et al. Immune response to vaccination in adults with mental disorders: A systematic review. J Affect Disord. 2022;304:66–77. doi: 10.1016/j.jad.2022.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Batty GD, Deary IJ, Altschul D. Pre-pandemic mental and physical health as predictors of COVID-19 vaccine hesitancy: evidence from a UK-wide cohort study. medRxiv [Preprint]’ 2021 Apr 30:2021.04.27.21256185. 10.1101/2021.04.27.21256185. [DOI] [PMC free article] [PubMed]
- 23.Schwarzinger M., Watson V., Arwidson P., Alla F., Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021;6(4):e210–e221. doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bendau A., Plag J., Petzold M.B., Ströhle A. COVID-19 vaccine hesitancy and related fears and anxiety. Int Immunopharmacol. 2021;27(97) doi: 10.1016/j.intimp.2021.107724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maguire P.A., Reay R.E., Looi J.C. Nothing to sneeze at - uptake of protective measures against an influenza pandemic by people with schizophrenia: willingness and perceived barriers. Australas Psychiatry. 2019;27(2):171–178. doi: 10.1177/1039856218815748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Limesurvey GmbH. LimeSurvey: An Open Source survey tool/LimeSurvey GmbH, Hamburg, Germany. URL http://www.limesurvey.org.
- 27.Bundesministerium Österreich. Coronaschutzimpfung in Österreich. Retrieved July 10th 2021 from https://info.gesundheitsministerium.at.
- 28.Hao F., Wang B., Tan W., Husain S.F., McIntyre R.S., Tang X., et al. Attitudes toward COVID-19 vaccination and willingness to pay: comparison of people with and without mental disorders in China. BJPsych Open. 2021;7(5) doi: 10.1192/bjo.2021.979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jefsen O.H., Kølbæk P., Gil Y., Speed M., Dinesen P.T., Sønderskov K.M., et al. COVID-19 vaccine willingness amongst patients with mental illness compared with the general population. Acta Neuropsychiatr. 2021;33(5):273–276. doi: 10.1017/neu.2021.15. [DOI] [PubMed] [Google Scholar]
- 30.Batty GD, Deary IJ, Altschul D. Pre-pandemic mental and physical health as predictors of COVID-19 vaccine hesitancy: evidence from a UK-wide cohort study. medRxiv [Preprint]; 2021 Apr 30:2021.04.27.21256185. 10.1101/2021.04.27.21256185. Update in: Ann Med. 2022 Dec;54(1):274–282. [DOI] [PMC free article] [PubMed]
- 31.Our World in Data. Coronavirus (COVID-19) Vaccinations. Retrieved January 1st 2022 from https://ourworldindata.org/covid-vaccinations?country=AUT.
- 32.Bundesministerium. Nationales Impfgremium. Retrieved January 1st 2022 from https://www.sozialministerium.at/Themen/Gesundheit/Impfen/Nationales-Impfgremium.html.
- 33.Haas E.J., McLaughlin J.M., Khan F., Angulo F.J., Anis E., Lipsitch M., et al. Infections, hospitalisations, and deaths averted via a nationwide vaccination campaign using the Pfizer-BioNTech BNT162b2 mRNA COVID-19 vaccine in Israel: a retrospective surveillance study. Lancet Infect Dis. 2022;22(3):357–366. doi: 10.1016/S1473-3099(21)00566-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Munro A.P.S., Janani L., Cornelius V., Aley P.K., Babbage G., Baxter D., et al. COV-BOOST study group. Safety and immunogenicity of seven COVID-19 vaccines as a third dose (booster) following two doses of ChAdOx1 nCov-19 or BNT162b2 in the UK (COV-BOOST): a blinded, multicentre, randomised, controlled, phase 2 trial. Lancet. 2021;398(10318):2258–2276. doi: 10.1016/S0140-6736(21)02717-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Diaz P., Zizzo J., Balaji N.C., Reddy R., Khodamoradi K., Ory J., et al. Fear about adverse effect on fertility is a major cause of COVID‐19 vaccine hesitancy in the United States. Andrologia. 2022;54(4) doi: 10.1111/and.v54.410.1111/and.14361. [DOI] [PubMed] [Google Scholar]
- 36.Bono S.A., Faria de Moura Villela E., Siau C.S., Chen W.S., Pengpid S., Hasan M.T., et al. Factors Affecting COVID-19 Vaccine Acceptance: An International Survey among Low- and Middle-Income Countries. Vaccines. 2021;9(5):515. doi: 10.3390/vaccines9050515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Desson Z., Kauer L., Otten T., Peters J.W., Paolucci F. Finding the way forward: COVID-19 vaccination progress in Germany, Austria and Switzerland. Health Policy Technol. 2022;11(2):100584. doi: 10.1016/j.hlpt.2021.100584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Di Giuseppe G., Pelullo C.P., Della Polla G., Montemurro M.V., Napolitano F., Pavia M., et al. Surveying willingness toward SARS-CoV-2 vaccination of healthcare workers in Italy. Expert Rev Vaccines. 2021;20(7):881–889. doi: 10.1080/14760584.2021.1922081. [DOI] [PubMed] [Google Scholar]
- 39.Ndiaye S.M., Hopkins D.P., Shefer A.M., Hinman A.R., Briss P.A., Rodewald L., et al. Task Force on Community Preventive Services. Interventions to improve influenza, pneumococcal polysaccharide, and hepatitis B vaccination coverage among high-risk adults: a systematic review. Am J Prev Med. 2005;28(5):248–279. doi: 10.1016/j.amepre.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 40.Kan T., Zhang J. Factors influencing seasonal influenza vaccination behaviour among elderly people: a systematic review. Public Health. 2018;156:67–78. doi: 10.1016/j.puhe.2017.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Miles L.W., Williams N., Luthy K.E., Eden L. Adult Vaccination Rates in the Mentally Ill Population: An Outpatient Improvement Project. J Am Psychiatr Nurses Assoc. 2020;26(2):172–180. doi: 10.1177/1078390319831763. [DOI] [PubMed] [Google Scholar]
- 42.Paul E., Steptoe A., Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. Lancet Reg Health Eur. 2021;1:100012. doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rosen B., Waitzberg R., Israeli A., Hartal M., Davidovitch N. Addressing vaccine hesitancy and access barriers to achieve persistent progress in Israel's COVID-19 vaccination program. Isr J Health Policy Res. 2021;10(1):43. doi: 10.1186/s13584-021-00481-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Levin-Zamir D. Communication, Health Literacy and a Systems Approach for Mitigating the COVID-19 Pandemic: The Case for Massive Vaccine Roll-out in Israel. J Health Commun. 2020;25(10):816–818. doi: 10.1080/10810730.2021.1884773. [DOI] [PubMed] [Google Scholar]
- 45.Wang J., Wagner A.L., Chen Y., Jaime E., Hu X., Wu S., et al. Would COVID-19 vaccination willingness increase if mobile technologies prohibit unvaccinated individuals from public spaces? A nationwide discrete choice experiment from China. Vaccine. 2021 doi: 10.1016/j.vaccine.2021.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Davis R.E., Geneus C.J. Impact of Health-Related Quality of Life and Social Determinants on Yearly Influenza Immunization in the United States. Value in Health. 2016;19(3):A221. doi: 10.1016/j.jval.2016.03.1866. [DOI] [Google Scholar]
- 47.Lawrence T., Zubatsky M., Meyer D. The association between mental health diagnoses and influenza vaccine receipt among older primary care patients. Psychol Health Med. 2020;25(9):1083–1093. doi: 10.1080/13548506.2020.1717557. [DOI] [PubMed] [Google Scholar]
- 48.LaVela S., Goldstein B., Etingen B., Miskevics S., Weaver F. Factors Associated With H1N1 Influenza Vaccine Receipt in a High-Risk Population During the 2009–2010 H1N1 Influenza Pandemic. Top Spinal Cord Inj Rehabil. 2012;18(4):306–314. doi: 10.1310/sci1804-306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Buchwald D., Sheffield J., Furman R., Hartman S., Dudden M., Manson S. Influenza and pneumococcal vaccination among Native American elders in a primary care practice. Arch Intern Med. 2000;160(10):1443–1448. doi: 10.1001/archinte.160.10.1443. [DOI] [PubMed] [Google Scholar]
- 50.Bazargan M., Wisseh C., Adinkrah E., Ameli H., Santana D., Cobb S., et al. Influenza Vaccination among Underserved African-American Older Adults. Biomed Res Int. 2020;2020:1–9. doi: 10.1155/2020/2160894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Druss B.G., Rask K., Katon W.J. Major depression, depression treatment and quality of primary medical care. Gen Hosp Psychiatry. 2008;30(1):20–25. doi: 10.1016/j.genhosppsych.2007.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lorenz R.A., Norris M.M., Norton L.C., Westrick S.C. Factors associated with influenza vaccination decisions among patients with mental illness. Int J Psychiatry Med. 2013;46(1):1–13. doi: 10.2190/PM.46.1.a. [DOI] [PubMed] [Google Scholar]
- 53.Thorpe J.M., Kalinowski C.T., Patterson M.E., Sleath B.L. Psychological distress as a barrier to preventive care in community-dwelling elderly in the United States. Med Care. 2006;44(2):187–191. doi: 10.1097/01.mlr.0000196965.54871.d5. [DOI] [PubMed] [Google Scholar]
- 54.Druss B.G., Rosenheck R.A., Desai M.M., Perlin J.B. Quality of preventive medical care for patients with mental disorders. Med Care. 2002;40(2):129–136. doi: 10.1097/00005650-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 55.Fischer B.C., Schulz K.-T., Wiemann M., Lücke E., Schreiber J. Untersuchungen zu Einflussfaktoren auf die Influenza-Impfraten bei Patienten mit chronisch obstruktiver Lungenerkrankung [Studies on Factors Influencing Influenza Vaccination Rates in Patients with Chronic Obstructive Pulmonary Disease] Pneumologie. 2021:499–506. doi: 10.1055/a-1180-0111. [DOI] [PubMed] [Google Scholar]
- 56.Green C.A., Pope C.R. Depressive symptoms, health promotion, and health risk behaviors. Am J Health Promot. 2000;15(1):29–34. doi: 10.4278/0890-1171-15.1.29. [DOI] [PubMed] [Google Scholar]
- 57.Kwon D.S., Kim K., Park S.M. Factors associated with influenza vaccination coverage among the elderly in South Korea: the Fourth Korean National Health and Nutrition Examination Survey (KNHANES IV) BMJ Open. 2016;6(12):e012618. doi: 10.1136/bmjopen-2016-012618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Peytremann-Bridevaux I., Voellinger R., Santos-Eggimann B. Healthcare and preventive services utilization of elderly Europeans with depressive symptoms. J Affect Disord. 2008 Jan;105(1–3):247–252. doi: 10.1016/j.jad.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 59.Fleischmann E., Dalkner N., Fellendorf F.T., Reininghaus E.Z. Psychological impact of the COVID-19 pandemic on individuals with serious mental disorders: A systematic review of the literature. World J Psychiatr. 2021;11(12):1387–1406. doi: 10.5498/wjp.v11.i12.1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fountoulakis K.N., Karakatsoulis G., Abraham S., Adorjan K., Ahmed H.U., Alarcón R.D., et al. Results of the COVID-19 mental health international for the general population (COMET-G) study. Eur Neuropsychopharmacol. 2022;54:21–40. doi: 10.1016/j.euroneuro.2021.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Soares P., Rocha J.V., Moniz M., Gama A., Laires P.A., Pedro A.R., et al. Factors Associated with COVID-19 Vaccine Hesitancy. Vaccines (Basel) 2021;9(3):300. doi: 10.3390/vaccines9030300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Schernhammer E., Weitzer J., Laubichler M.D., Birmann B.M., Bertau M., Zenk L., et al. Correlates of COVID-19 vaccine hesitancy in Austria: trust and the government. J Public Health (Oxf) 2022;44(1):e106–e116. doi: 10.1093/pubmed/fdab122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Harper J.A., South C., Trivedi M.H., Toups M.S. Pilot investigation into the sickness response to influenza vaccination in adults: Effect of depression and anxiety. Gen Hosp Psychiatry. 2017;48:56–61. doi: 10.1016/j.genhosppsych.2017.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Niemegeers P., De Boer P., Dumont G.J.H., Van Den Eede F., Fransen E., Claes S.J., et al. Differential Effects of Inflammatory and Psychosocial Stress on Mood, Hypothalamic-Pituitary-Adrenal Axis, and Inflammation in Remitted Depression. Neuropsychobiology. 2016;74(3):150–158. doi: 10.1159/000466698. [DOI] [PubMed] [Google Scholar]
- 65.De Serres G., Rouleau I., Skowronski D.M., Ouakki M., Lacroix K., Bédard F., et al. Paresthesia and sensory disturbances associated with 2009 pandemic vaccine receipt: Clinical features and risk factors. Vaccine. 2015;33(36):4464–4471. doi: 10.1016/j.vaccine.2015.07.028. [DOI] [PubMed] [Google Scholar]
- 66.Sharpley A.L., Cooper C.M., Williams C., Godlewska B.R., Cowen P.J. Effects of typhoid vaccine on inflammation and sleep in healthy participants: a double-blind, placebo-controlled, crossover study. Psychopharmacology. 2016;233(18):3429–3435. doi: 10.1007/s00213-016-4381-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dantzer R. Cytokine-induced sickness behaviour: a neuroimmune response to activation of innate immunity. Eur J Pharmacol. 2004;500(1–3):399–411. doi: 10.1016/j.ejphar.2004.07.040. [DOI] [PubMed] [Google Scholar]