Abstract
Telehealth is an alternative care delivery model to in-person care. It uses electronic information and telecommunication technologies to provide remote clinical care to patients, especially those living in rural areas that lack sufficient access to health care services. Like other areas of care affected by the COVID-19 pandemic, the prevalence of telehealth has increased in prenatal care. This study reports on telehealth use in prenatal care at a large academic medical center in Middle Tennessee, USA. We examine the electronic health records of over 2500 women to characterize 1) the volume of prenatal visits participating in telehealth, 2) disparities in obstetric patients using telehealth, and 3) the impact of telehealth use on obstetric outcomes, including duration of intrapartum hospital stays, preterm birth, Cesarean rate, and newborn birthweight. Our results show that telehealth mainly was used in the second and third trimesters, especially for consulting services. In addition, we found that certain demographics correlated with lower telehealth utilization, including patients who were under 26 years old, were Black and/or Hispanic, were on a state-sponsored health insurance program, and those who lived in urban areas. Furthermore, no significant differences were found on preterm birth and Cesarean between the patients who used telehealth in their prenatal care and those who did not.
Keywords: Telehealth, obstetrics, prenatal, COVID-19, disparities
Introduction
Telehealth is broadly defined as the delivery and facilitation of health and health-related services using electronic information and telecommunication technologies. [1] It has brought healthcare to patients living in rural areas that lack sufficient access to in-person health care services.[2] Telehealth has further played a role in supporting health care during disasters when travel is limited and in-person care is disrupted. [3;4] The range and use of telehealth services have increased dramatically over the past several decades. A wide variety of services now benefit from telehealth, including long-distance clinical care, patient and professional health-related education, and health administration. [1] In the U.S., the number of patients who used telehealth technology has also grown by 20 times in a five-year span (2013 – 2018), and this number reached an unprecedented 50 million in 2020. [5;6]
The 2019 novel coronavirus (COVID-19) was declared by the World Health Organization (WHO) as a public health emergency of international concern on January 30th, 2020. [7] After the WHO officially classified COVID-19 as a pandemic, [8] the number of infections in the U.S. grew exponentially. [9] Due to rapid viral transmission [10], lack of effective anti-viral treatments, and the potential for long-term sequelae from viral infection [11], the CDC recommended that healthcare providers expand telehealth service to its patient population. [12] The American College of Obstetricians and Gynecologists (ACOG) has published President Task Force on Telehealth. [13] The ACOG encouraged telehealth use in routine prenatal care, consultation services (e.g., psychiatry, endocrinology, and nephrology), and postpartum blood pressure monitoring. [13] Telehealth represents an alternative care model for pregnant women to continue prenatal care while mitigating viral exposure risk.
Various studies [14–18] have shown that telehealth has been incorporated into obstetric care at an accelerated rate. These studies also serve as initial investigations on how telehealth was implemented in the obstetric setting [14–18] and what possible barriers were in its implementation [19–23]. There are several aspects of telehealth in prenatal care that have yet to be addressed in these studies. Therefore, we leverage electronic health records at a large academic medical center to investigate several open issues on telehealth use in prenatal care.
First, what in-person prenatal visits can be replaced with telehealth? Existing studies provide guidance [15–17] about the implementation of telehealth in prenatal care from a theoretical perspective, but this guidance is not validated by the actual telehealth use.
Second, what are the access barriers to telehealth in prenatal care? Even though telehealth increases access to care for obstetric patients, the rapid transition to telehealth can exacerbate health disparities [19], known as a digital divide [24;25]. Potential access barriers to telehealth, including low language proficiency, device unavailability, and non-reimbursement for telehealth in certain types of insurance, have not been systematically investigated in prenatal care.
Third, how does telehealth impact maternal outcomes? Both care providers and patients are concerned about the impact of telehealth on care quality [26;27]; however, few studies provide clear answers.
Methods
We begin this section with a description of the prenatal telehealth dataset investigated in this study. Next, the data is analyzed to characterize: 1) trends of telehealth use during COVID-19 pandemic, 2) the volume of prenatal visits using telehealth, 3) socioeconomic disparities in the patient population using telehealth, and 4) the impact of telehealth on obstetric outcomes.
Dataset
The Department of Obstetrics and Gynecology at Vanderbilt University Medical Center (VUMC) provides prenatal care and delivery services to over 4,500 women per year in metropolitan Nashville and surrounding areas. Telehealth for pregnant patients began in the final week of March as the government widely recognized the COVID-19 pandemic. Its continuing use was suggested through the early summer as the outbreak in Tennessee grew. As such, the study period is from March 23rd, 2020 to July 2nd, 2020.
The Epic EHR system at VUMC, which serves as the central source of documentation for patient care, records prenatal encounters and patient information. We collect the information for 2,521 women in this system. The EHR documents patient demographics (age, BMI, race, and ethnicity), residential address, and types of health insurance. We discretize maternal age into four groups: 1) younger than 17, 2) 17 to 25, 3) 26 to 35, and 4) over 35. If a pregnant woman is younger than 17 years old or older than 35 years old, her pregnancy is considered high risk [28].
In addition, we assign each patient to an urbanization level based on their residential county according to the six-level urban-rural classification scheme for U.S. counties and county-equivalent entities developed by the National Center for Health Statistics [29]. The most urban category consists of central counties of large metropolitan areas (denoted as 1), whereas the most rural category consists of nonmetropolitan non-central counties (denoted as 6). Lastly, the insurance type is represented as one of five types: 1) commercial (e.g., Aetna, United Healthcare, or Blue Cross Blue Shield), 2) Medicare, 3) Medicaid, 4) state-level insurance (e.g., TennCare for residents in the State of Tennessee), and 5) some other form of governmental insurance.
All prenatal care encounters were retrieved from the Epic EHR system. Each encounter includes the date of service, visit types (telehealth or non-telehealth), gestational age in weeks, and purpose of visits. In addition, any patient who used telehealth at any point of their prenatal care was assigned to the telehealth group. Lastly, we extract outcome information in the delivery encounter for each patient. The outcomes of interest include duration of intrapartum hospital stays (LOS in days), preterm birth (gestational age < 37 weeks), Cesarean section, and newborn birthweight in kilograms (kg).
Trends of Prenatal Telehealth Use
To study the trend of telehealth use in prenatal care during the study period, we measure the number of telehealth visits per day.
Prenatal Telehealth Visits
We divide prenatal visits into routine prenatal care and consulting. Next, the entire prenatal journey is segmented into three trimesters bases on gestational age, first trimester (1 – 12 weeks), second trimester (13 – 26 weeks), and third trimester (after 26 weeks). Finally, we calculate the number of telehealth visits in routine prenatal care and consulting services in each trimester, respectively.
Sociodemographic Disparities by Telehealth Use
To investigate whether there exist disparities in prenatal telehealth use, we compare socioeconomic factors between telehealth and non-telehealth groups. For each factor, the two proportion Z test is used for the confirmation of the significances in the disparities. We take one of these socioeconomic factors, ethnicity, as an example. Non-Hispanic is chosen as a reference, and we investigate whether patients who were Hispanic and had undecided ethnicity had a different telehealth usage, compared to non-Hispanic patients (reference).
Impact of Telehealth on Obstetric Outcomes
We also examine the impact of telehealth on obstetric outcomes. First, case (telehealth) and control groups (non-telehealth) are matched using propensity score matching on age, race, ethnicity, and prenatal conditions, including hypertensive disorder, gestational diabetes, and infections of genitourinary tract in pregnancy. We then compare the obstetric outcomes between telehealth and non-telehealth groups, including LOS, preterm birth rate, Cesarean rate, birthweight in kg.
Results
Telehealth Use Trend
Figure 1 shows the number of telehealth encounters for prenatal care during the study period. Telehealth visits rapidly escalated in the week of March 23rd, peaked during the week of April 7th, and slowly reduced after the week of June 29th. This reflected the trend of telehealth in the first few months of the COVID-19 pandemic.
Figure 1.
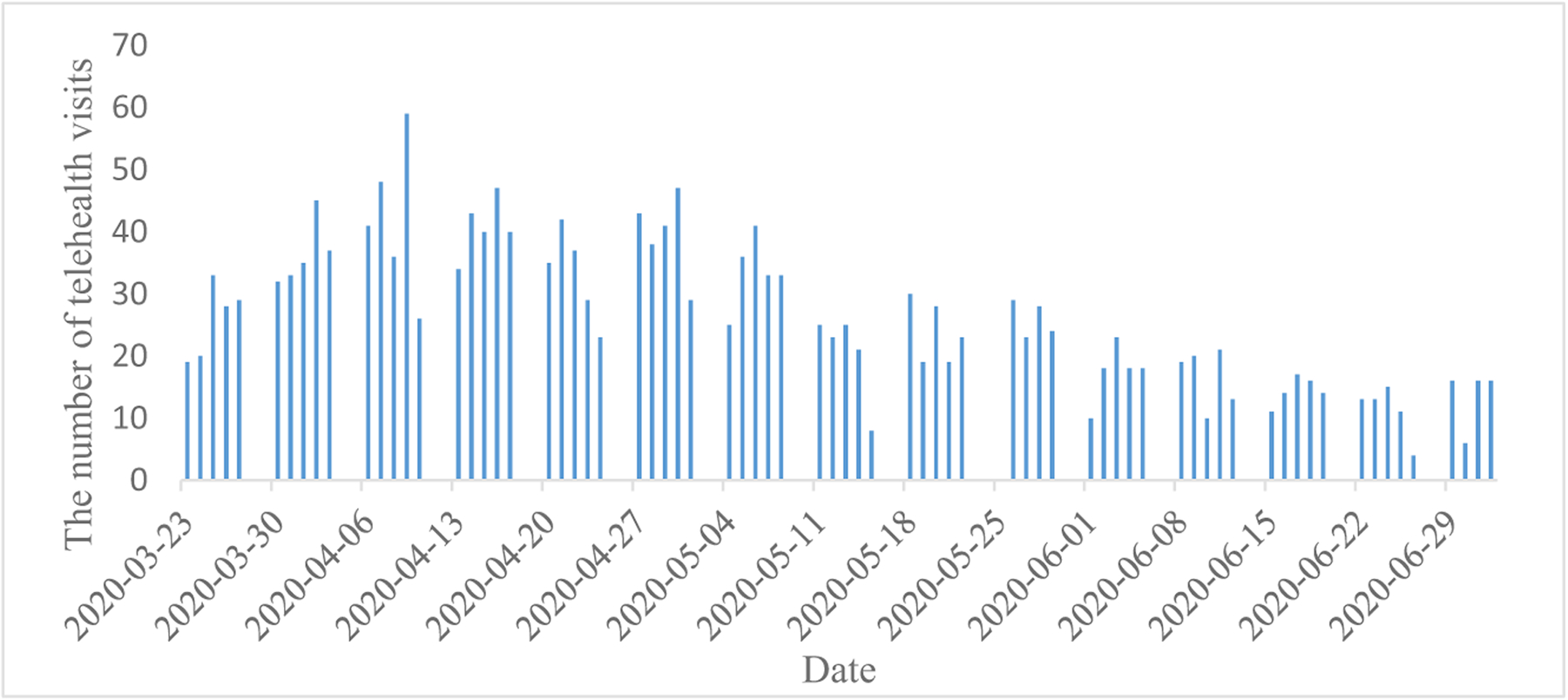
The number of telehealth encounters over the course of the study period
Routine Prenatal Visits and Consulting Services with Telehealth Use
Figure 2 depicts the number of telehealth visits by types in different trimesters. In the first trimester, the number of consulting visits with telehealth was slightly larger than that of routine prenatal care. This trend reversed in the second and third trimesters. We also observe that many more routine visits used telehealth in the second and third trimesters. Furthermore, compared to the first trimester, pregnant patients experienced many more telehealth visits in the second and third trimesters.
Figure 2.
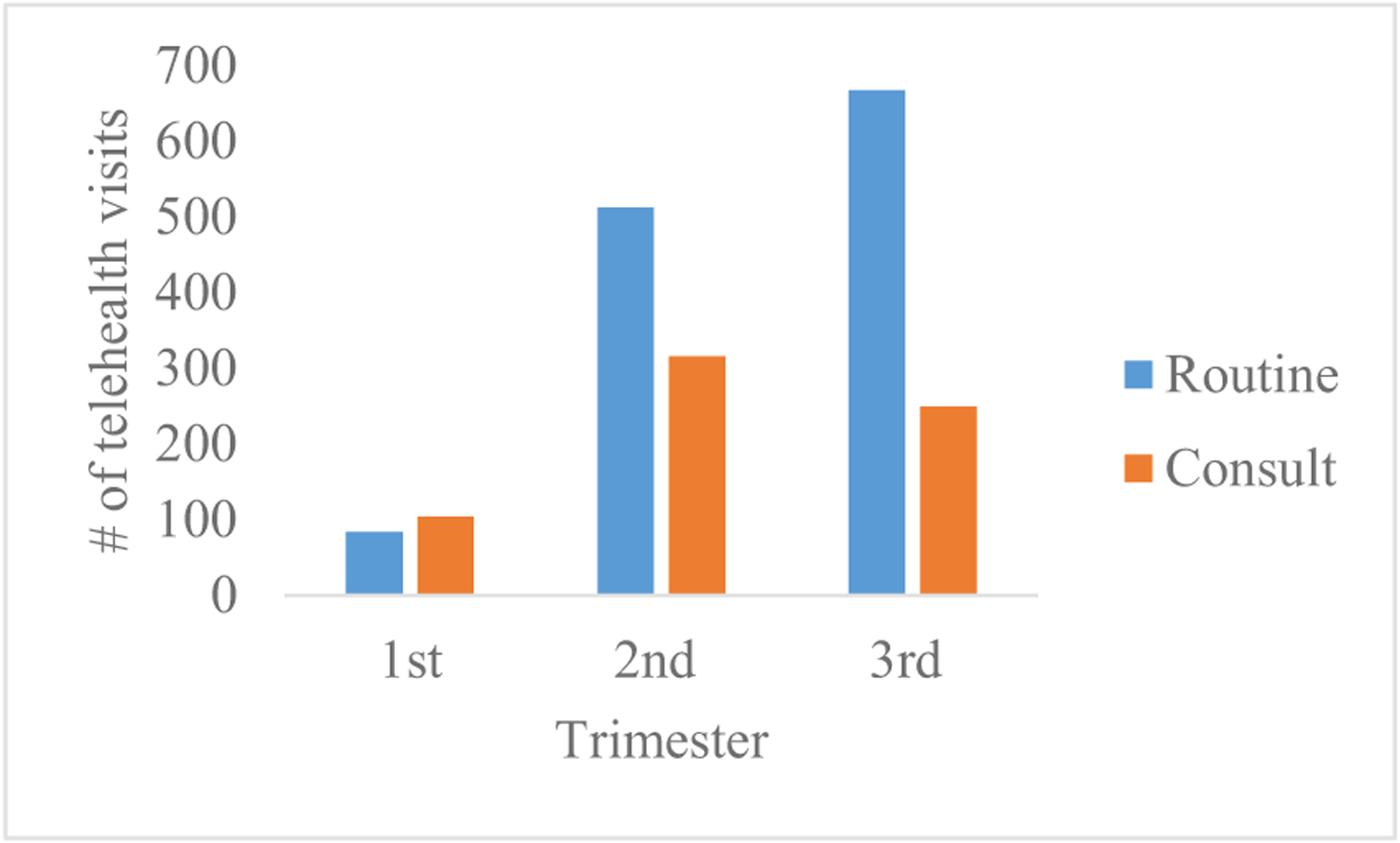
Purpose of telehealth visits by trimester
Sociodemographic Disparities by Telehealth Use
The statistical summary of socioeconomic factors in both telehealth and non-telehealth groups is tabulated in Table 1. P-values in bold indicate that there was a significant difference in telehealth use compared with the reference group.
Table 1.
A comparison of telehealth and non-telehealth groups on sociodemographic factors
| Variable | Category | Patients | Patients with telehealth visits | Patients lacking telehealth visits | OR (95% CI) | p-value |
|---|---|---|---|---|---|---|
| Age | < 17 | 15 (100%) | 2 (13.33%) | 13 (86.67%) | 0.54 (0.08 – 2.00) | 0.5394 |
| 17 – 25 (reference) | 668 (100%) | 156 (23.35%) | 512 (76.65%) | 1 | N.A. | |
| 26 – 35 | 1452 (100%) | 594 (40.91%) | 858 (59.09%) | 2.27 (1.85 – 2.80) | < 0.0001 | |
| ≥ 36 | 386 (100%) | 186 (48.19%) | 200 (51.81%) | 3.05 (2.33 – 3.99) | < 0.0001 | |
| Ethnicity | Non-Hispanic (reference) | 2098 (100%) | 853 (40.66%) | 1245 (59.34%) | 1 | N.A. |
| Hispanic | 376 (100%) | 71 (18.88%) | 305 (81.12%) | 0.34 (0.26 – 0.44) | < 0.0001 | |
| Undecided | 47 (100%) | 14 (29.79%) | 33 (70.21%) | 0.62 (0.32 – 1.15) | 0.1331 | |
| Race | White (reference) | 1551 (100%) | 683 (44.04%) | 868 (55.96%) | 1 | N.A. |
| Black | 442 (100%) | 132 (29.86%) | 310 (70.14%) | 0.54 (0.43 – 0.68) | < 0.0001 | |
| Asian | 126 (100%) | 44 (34.92%) | 82 (65.08%) | 0.68 (0.46 – 0.99) | 0.0498 | |
| Other | 402 (100%) | 79 (19.65%) | 323 (80.35%) | 0.31 (0.24 – 0.40) | < 0.0001 | |
| Urbanization level | 1 (the urbanist) (reference) | 1313 (100%) | 415 (31.61%) | 898 (68.39%) | 1 | N.A. |
| 2 | 884 (100%) | 337 (38.12%) | 547 (61.88%) | 1.33 (1.11 – 1.59) | 0.0016 | |
| 3 | 201 (100%) | 113 (56.22%) | 88 (43.78%) | 2.78 (2.05 – 3.76) | < 0.0001 | |
| 4 | 18 (100%) | 12 (66.67%) | 6 (33.33%) | 4.27 (1.63 – 12.55) | 0.0016 | |
| 5 | 65 (100%) | 38 (58.46%) | 27 (41.54%) | 3.04 (1.83 – 5.10) | < 0.0001 | |
| 6 (the most rural) | 40 (100%) | 23 (57.5%) | 17 (42.5%) | 2.92 (1.54 – 5.63) | < 0.001 | |
| Insurance type | Commercial (reference) | 1141 (100%) | 552 (48.38%) | 589 (51.62%) | 1 | N.A. |
| TennCare | 890 (100%) | 255 (28.65%) | 635 (71.35%) | 0.43 (0.36 – 0.52) | < 0.0001 | |
| Medicare | 20 (100%) | 12 (60.00%) | 8 (40.00%) | 1.59 (0.65 – 4.14) | 0.3026 | |
| Medicaid | 9 (100%) | 6 (66.67%) | 3 (33.33%) | 2.08 (0.53 – 10.48) | 0.2741 | |
| Other Governmental | 402 (100%) | 89 (22.14%) | 313 (77.86%) | 0.30 (0.23 – 0.39) | < 0.0001 | |
| Other | 59 (100%) | 24 (40.68%) | 35 (59.32%) | 0.73 (0.43 – 1.24) | 0.2483 |
(OR: odds ratio; CI: confidence interval; bold font indicates statistical significance of 0.05 after Bonferroni correction)
There are several findings worth highlighting. First, prenatal visits were more likely to be delivered via telehealth for women aged 26–35 and over 35 (Odds Ratio 95% Confidence interval OR [95% CI]: 2.27 [1.85 – 2.80] and 3.05 [2.33 – 3.99], respectively), comparing to the younger women (17 – 25). Second, Hispanics used telehealth less than non-Hispanics (OR [95% CI]: 0.34 [0.26 – 0.44]). Similarly, telehealth was used by women who were Black or of other race (non-White, non-Asian, non-Black) significantly less than White women (OR [95% CI]: 0.54 [0.43 – 0.68] and 0.31 [0.24 – 0.40]). Third, telehealth services were more likely to be utilized by pregnant women who lived in rural areas (urbanization level (OR [95% CI]): 2 (1.33 [1.11 – 1.59]); 3 (2.78 [2.05 – 3.76]); ; 4 (4.27 [1.63 – 12.55]); 5 (3.04 [1.83 – 5.10]); 6 (2.92 [1.54 – 5.63))) than those who lived in large metropolitan areas. Finally, it was less likely for women with TennCare (state-level Medicaid) and other governmental insurances (OR [95% CI]: 0.43 [0.36 – 0.52] and 0.30 [0.23 – 0.39], respectively) to have prenatal care visits via telehealth than those who were commercially insured.
Impact of Telehealth on Obstetric Outcomes
As shown in Table 2, there was no significant difference in LOS and baby birthweight between the telehealth group and matched non-telehealth group. In addition, although patients in the telehealth group had a higher rate of preterm births and Cesarean section than those in the matched non-telehealth group, the differences were not significant (p-value: 0.7602 and 0.0998, respectively).
Table 2.
Comparison of obstetric outcomes between telehealth and non-telehealth groups
| Patients with one or more telehealth prenatal visits | Matched patients lacking any telehealth prenatal visits | p-value | |
|---|---|---|---|
| Number of patients | 938 | 938 | - |
|
LOS Mean (IQ) |
3.0 (2.1 – 3.3) | 2.9 (2.1 – 3.2) | 0.4983 |
|
Preterm birth < 37 weeks |
153 (16.3%) | 127 (13.5%) | 0.7602 |
| ≥ 37 weeks | 785 (83.7%) | 811 (86.5%) | |
| Cesarean | 398 (42.4%) | 362 (38.6%) | 0.0998 |
|
Birthweight in kg Mean (IQ) |
3.188 (2.860 – 3.600) | 3.161 (2.842 – 3.620) | 0.3905 |
Discussion
This study examined telehealth use for obstetric patients in their prenatal care at a large academic hospital during the COVID-19 pandemic. There are several findings worth noting. First, the daily number of telehealth visits shows that telehealth was rapidly implemented for prenatal care in the early stage of the pandemic and its use decreased slowly after that. Second, most prenatal telehealth visits exist in routine care and consulting services in the second and third trimesters. Third, our investigation also suggested that certain sociodemographic factors were associated with a lower rate of telehealth use. In particular, we found this to be the case for younger patients, Black, of other race (non-White, non-Black, and non-), Hispanic, with TennCare (state-level Medicaid insurance), or who lived in large metropolitan areas. Lastly, telehealth visits were as effective as in-person visits since there was no significant difference in the four obstetric outcomes between telehealth and non-telehealth groups.
The results have several notable implications for the promotion of telehealth in the post-COVID-19. First, they suggest that there are disparities in the implementation of telehealth. It is important to follow-up on this finding and investigate what, if any, access barriers exist for patients who did not use telehealth. For example, Hispanic patients may be reluctant to use telehealth services due to low English language proficiency or telehealth services without involving clinicians who speak their language. TennCare, the state of Tennessee’s managed Medicaid agency, has covered telehealth services since the beginning of the pandemic, and most TennCare-insured patients are from low-income households; therefore, there are several potential access barriers to telehealth, including Internet and device availability and low technology proficiency. As such, efforts need to be made to ensure that TennCare patients can access telehealth without these barriers.
Second, the findings suggest that there is an opportunity to promote telehealth to obstetric patients who live in metropolitan areas (the city of Nashville in this study). Among the largest population (52.1%) of the studied patients who live in the metropolitan area, only less than one third (31.61%) of them used telehealth in their prenatal care, comparing to a higher adoption rate (55%) for patients who live in more rural areas.
Third, family members and pregnant women have concerns about the care quality of telehealth visits. [26 – 27] Yet we observed that there were no statistically significant differences in the obstetric outcomes for patients who were managed via telehealth or in person.
Still, there are several limitations to this pilot study. First, this investigation only reflects telehealth usage at the VUMC, an academic medical center that provides prenatal care for high-risk pregnancy patients in middle Tennessee and nearby areas, such that the findings may not generalize for other healthcare systems. Second, we analyzed potential telehealth visits from a space of two types of visits (routine prenatal care and consult) by three trimesters, which were still at a coarse-grained level. An ideal analysis would be conducted at the level of gestational weeks. Additionally, we did not investigate the satisfaction of clinicians and patients regarding telehealth use in prenatal care. Thus, it is challenging for this study to recommend when telehealth should be used in prenatal care.
Third, although our analysis results indicated that certain sub-populations were less likely to use telehealth, we did not adjust patients’ health conditions in these comparisons. In addition, more social determinants of health need to be incorporated in this study, including years of education, lifestyle choices, and poverty levels.
Conclusions
Telehealth was rapidly implemented and played an adequate role in prenatal care, especially in the second and third trimesters. Patients who had telehealth visits in their prenatal care experienced comparable obstetric outcomes as those who did not. However, there were disparities in telehealth use. Further study was suggested to identify access barriers for the underserved patient population.
References
- [1].HHS, Health Resources and Services Administration (HRSA). Telehealth programs. https://www.hrsa.gov/rural-health/telehealth/index.html. Accessed in May 2021.
- [2].Lurie N, Carr BG. The role of telehealth in the medical response to disasters. JAMA internal medicine. 2018. Jun 1, 178(6):745–6. [DOI] [PubMed] [Google Scholar]
- [3].Der-Martirosian C, Chu K, Dobalian A. Use of Telehealth to Improve Access to Care at the U.S. Department of Veterans Affairs during the 2017 Atlantic Hurricane Season. Disaster Med Public Health Prep. 2020:1–5. doi: 10.1017/dmp.2020.88. [DOI] [PubMed] [Google Scholar]
- [4].Der-Martirosian C, Heyworth L, Chu K, Mudoh Y, obalian A. Patient Characteristics of VA Telehealth Users During Hurricane Harvey. J Prim Care Community Heal. 2020;11. doi: 10.1177/2150132720931715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Top 10 benefits of telehealth for patients and doctors, https://www.ortholive.com/blog/top-10-benefits-of-telehealth-for-patients-and-doctors/ accessed in April 2021.
- [6].The benefits of telemedicine in remote patient triage, https://www.beckershospitalreview.com/telehealth/the-benefits-of-telemedicine-in-remote-patient-triage.html, accessed in April 2021.
- [7].Director-General WHO. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). January 30, 2020. Available at: www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-internationalhealth-regulations-(2005)-emergency-committee-regarding-theoutbreak-of-novel-coronavirus-(2019-ncov). Accessed in May 2021.
- [8].WHO Director General’s opening remarks at the media briefing on COVID-19. March 11, 2020. Available at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-themedia-briefing-on-covid-19—11-march-2020. Accessed in May 2021.
- [9].Centers for Disease Control and Prevention. Situation Summary. https://www.cdc.gov/coronavirus/2019-ncov/casesupdates/summary.html. Accessed in May 2021.
- [10].Centers for Disease Control and Prevention. How coronavirus spreads https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html. Accessed in May 2021.
- [11].Centers for Disease Control and Prevention. Long-Term Effects of COVID-19 https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects.html. Accessed in January 2021.
- [12].Centers for Disease Control and Prevention. Telehealth. https://www.cdc.gov/coronavirus/2019-ncov/hcp/telehealth.html. Accessed in January 2021.
- [13].American College of Obstetricians and Gynecologists. (2020). Committee Opinion Number 798 implementing telehealth in practice. Obstetrics and Gynecology, 135(2), e73–e79. [DOI] [PubMed] [Google Scholar]
- [14].Madden N, Emeruwa UN, Friedman AM, Aubey JJ, Aziz A, Baptiste CD, Coletta JM, D’Alton ME, Fuchs KM, Goffman D, Gyamfi-Bannerman C. Telehealth uptake into prenatal care and provider attitudes during the COVID-19 pandemic in New York City: a quantitative and qualitative analysis. American journal of perinatology. 2020. Aug;37(10):1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Dosaj A, Thiyagarajan D, Ter Haar C, Cheng J, George J, Wheatley C, Ramanathan A. Rapid implementation of telehealth services during the COVID-19 pandemic. Telemedicine and e-Health. 2021. Feb 1;27(2):116–20. [DOI] [PubMed] [Google Scholar]
- [16].Fryer K, Delgado A, Foti T, Reid CN, Marshall J. Implementation of obstetric telehealth during COVID-19 and beyond. Maternal and child health journal. 2020. Sep;24(9):1104–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Zork NM, Aubey J, Yates H. Conversion and optimization of telehealth in obstetric care during the COVID-19 pandemic. InSeminars in Perinatology 2020. Oct 1 (Vol. 44, No. 6, p. 151300). WB Saunders. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Aziz A, Zork N, Aubey JJ, Baptiste CD, D’alton ME, Emeruwa UN, Fuchs KM, Goffman D, Gyamfi-Bannerman C, Haythe JH, LaSala AP. Telehealth for high-risk pregnancies in the setting of the COVID-19 pandemic. American journal of perinatology. 2020. Jun;37(8):800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Gao C, Osmundson S, Malin B, Chen Y, Prenatal Telehealth During the Pandemic: Sociodemographic and Clinical Associations, accepted for Telehealth and Medicine Today. [Google Scholar]
- [20].Turner-Musa J, Ajayi O, Kemp L. Examining social determinants of health, stigma, and COVID-19 disparities. InHealthcare 2020. Jun (Vol. 8, No. 2, p. 168). Multidisciplinary Digital Publishing Institute. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Abuelgasim E, Saw LJ, Shirke M, Zeinah M, Harky A. COVID-19: Unique public health issues facing Black, Asian and minority ethnic communities. Current problems in cardiology. 2020. May 8:100621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Ferguson JM, Jacobs J, Yefimova M, Greene L, Heyworth L, Zulman DM. Virtual care expansion in the Veterans Health Administration during the COVID-19 pandemic: clinical services and patient characteristics associated with utilization. Journal of the American Medical Informatics Association. 2020. Oct 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].David RA, Rhee M. The impact of language as a barrier to effective health care in an underserved urban Hispanic community. The Mount Sinai Journal of Medicine, New York. 1998. Oct 1;65(5–6):393–7. [PubMed] [Google Scholar]
- [24].Bakhtiar M, Elbuluk N, Lipoff JB. The digital divide: how Covid-19’s telemedicine expansion could exacerbate disparities. J Am Acad Dermatol. 2020. doi: 10.1016/j.jaad.2020.07.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Ramsetty A, Adams C. Impact of the digital divide in the age of COVID-19. J Am Med Inform Assoc. 2020;27(April):1147–1148. doi: 10.1093/jamia/ocaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Rush to Embrace Telehealth Many Physicians still Have Concerns about Quality Care Survey, https://www.fiercehealthcare.com/practices/rush-to-embrace-telehealth-many-physicians-still-have-concerns-about-quality-care-survey, accessed in April 2021.
- [27].Patients’ top 8 telemedicine concerns, benefits, https://www.beckershospitalreview.com/healthcare-information-technology/patients-top-8-telemedicine-concerns-benefits.html, accessed in April 2021.
- [28].Age and Pregnancy, https://www.ssmhealth.com/maternity/high-risk-pregnancy/age-pregnancy, accessed in January 2021.
- [29].National Center for Health Statistics (NCHS) Urban-Rural Classification Scheme for Counties. https://www.cdc.gov/nchs/data_access/urban_rural.htm, accessed in January 2021.
- [30].TennCare. https://www.tn.gov/tenncare/this-is-tenncare.html, accessed in January 2021.
- [31].TennCare telehealth. https://www.tn.gov/partnersforhealth/health-options/telehealth.html, accessed in January 2021.


