Abstract
A variety of diets have been studied for possible anti-aging effects. In particular, studies of intermittent fasting and time-restricted feeding in laboratory rodents have found evidence of beneficial health outcomes. Companion dogs represent a unique opportunity to study diet in a large mammal that shares human environments. The Dog Aging Project has been collecting data on thousands of companion dogs of all different ages, sizes, and breeds since 2019. We leveraged this diverse cross-sectional dataset to investigate associations between feeding frequency and cognitive function (n = 10,474) as well as nine broad categories of health conditions (n = 24,238). Controlling for sex, age, breed, and other potential confounders, we found that dogs fed once daily rather than more frequently had lower mean scores on a cognitive dysfunction scale, and lower odds of having gastrointestinal, dental, orthopedic, kidney/urinary, and liver/pancreas disorders. Therefore, we find that once-daily feeding is associated with better health in multiple domains. Future research with longitudinal data can provide stronger evidence for a possible causal effect of feeding frequency on health in companion dogs.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11357-022-00575-7.
Keywords: Canine, Canine cognitive dysfunction, Feeding frequency, Healthy aging, Time-restricted feeding
Introduction
For nearly a century, caloric restriction has been known to extend lifespan and delay age-associated pathology in laboratory animals [1–5]. More recently, in both animals and humans, a variety of alternative “anti-aging” diet modalities have been described which are providing new mechanistic insights and potential clinical applications [6]. These diets include intermittent fasting [7, 8], fasting mimicking diets [9, 10], ketogenic diets [11–15], protein or essential amino acid restriction [16, 17], and time-restricted feeding [18–20].
These diets have been most extensively studied in rodents in controlled laboratory settings, due to ease of administering diets on a specific schedule and an enhanced ability to tease apart the mechanisms through which they act. Time-restricted feeding studies in rodents suggest improvements in several metabolic parameters, including glucose and insulin homeostasis, energy expenditure, hepatic pathology, resistance to different obesogenic diets, and improved circadian rhythm maintenance during aging [21–23]. In one study, mice who experienced time-restricted feeding demonstrated an 11% extension in lifespan [18]. Additionally, several studies demonstrate that caloric restriction and intermittent fasting play a protective role in maintaining and enhancing cognitive function, including memory and spatial learning [24–28]. It remains unclear, however, whether these benefits in laboratory animals are generally due to reduced caloric intake or meal frequency or both [6].
Despite mainstream popularization in humans of several of these diets, the beneficial health effects of time-restricted feeding outside of a laboratory setting are less clear. In some human studies, only mild improvements in body composition and cardiovascular risk factors were detected [29], even when subjects also reduced their daily caloric intake [30]. In other studies, detrimental effects on glucose homeostasis were observed with time-restricted feeding [31]. Finally, while some studies have found potential cognitive benefits, especially for memory in older adults [32, 33], other studies have shown no effect of fasting on cognition [34, 35].
Companion dogs provide a potentially powerful animal model to elucidate the relationship between diet and age-related health outcomes [36]. Having co-evolved alongside people for thousands of years [37], companion dogs share human environments, experience similar diseases, and receive similar medical care. Once-daily feeding in dogs serves as a natural model for the intermittent fasting/time-restricted feeding protocols currently being studied both in preclinical rodent models and in human trials [38].
The Dog Aging Project is a large-scale research initiative following thousands of companion dogs over their lifetimes to better understand how biology, lifestyle, and environment impact healthy aging [39, 40]. Participating owners report annually on a variety of aspects related to their dog’s diet, primary and secondary activities, social and physical environments, medications, and health conditions. In the current study, we used cross-sectional data collected in the first year of the Dog Aging Project to ask if feeding frequency is associated with cognitive function and health conditions. Specifically, we hypothesized that dogs fed once-a-day would display lower rates of physical health issues and better cognitive scores compared to dogs fed more frequently.
Methods
Subjects
All dogs had been recruited to join the Dog Aging Project (DAP) via mainstream media, social media, or word of mouth. Their owners then completed the relevant online surveys between December 26, 2019 and December 31, 2020 [41]. Study data were collected and managed using REDCap electronic data capture tools hosted through the DAP [42, 43]. REDCap (Research Electronic Data Capture) is a secure, web-based software platform designed to support data capture for research studies, providing (1) an intuitive interface for validated data capture, (2) audit trails for tracking data manipulation and export procedures, (3) automated export procedures for seamless data downloads to common statistical packages, and (4) procedures for data integration and interoperability with external sources.
Instruments
The first survey that participants completed was the Health and Life Experience Survey (HLES), which collects information regarding dog demographics, physical activity, environment, dog behavior, diet, medications and preventives, health status, and owner demographics. In the current investigation, we were principally interested in feeding frequency and health status, and we identified a priori health conditions that could plausibly be affected by feeding frequency.
After completing HLES, all participants were offered the opportunity to complete the Canine Social and Learned Behavior Survey (CSLB), which measures cognitive function. The CSLB, renamed by the DAP, is the same as the Canine Cognitive Dysfunction Rating Scale (CCDR) [44], with only a handful of minor wording changes. The CCDR has been validated as a clinical instrument to detect cognitive dysfunction over a specific threshold. In this work, we use CSLB as a quantitative score for detecting deterioration towards cognitive dysfunction and acknowledge that it is not yet validated for this purpose. The Canine Cognitive Dysfunction Rating Scale was presented to participants as the Canine Social and Learned Behavior Survey to avoid the negative connotations of the phrase “cognitive dysfunction.” This instrument asks owners to indicate the frequency with which their dogs exhibit behaviors indicative of dementia (i.e., disengagement from social activity; difficulty in navigation, searching, and recognition). Based on owner responses, dogs receive a score that ranges from 16 to 80, where higher scores are indicative of worse cognitive function (i.e., more cognitive dysfunction).
During the study time period, 27,541 DAP participants completed HLES, and 20,096 DAP participants completed CSLB.
Ethical note
The University of Washington IRB deemed that recruitment of dog owners for the Dog Aging Project, and the administration and content of the DAP Health and Life Experience Survey (HLES), is human subjects research that qualifies for Category 2 exempt status (IRB ID no. 5988, effective 10/30/2018). No interactions between researchers and privately owned dogs occurred; therefore, IACUC oversight was not required.
Inclusion/exclusion criteria
Given that meal frequency is adjusted as puppies mature, we specified age of inclusion as 1 ≤ age < 18 years for all health outcomes. For the CSLB outcome, we specified age of inclusion as 6 ≤ age < 18 years, as 6 years is the youngest age indicated in the literature where signs of cognitive decline can start to appear in dogs [45–47]. Less than 5% of dogs in the DAP are intact, and these dogs were excluded, as well as dogs (< 1%) whose owners reported that their diet was “not at all consistent.” Thus, in our final sample, all dogs were spayed or neutered due to exclusion criteria, and slightly less than half of dogs were male. About one-fifth of dogs received daily or more frequent omega-3 or other fatty acid supplementation in their diet.
We studied health conditions that were reported in the nine broad categories on HLES that could plausibly be affected by feeding frequency: dental or oral disease, skin disorders, orthopedic disorders, gastrointestinal disorders, cancer or tumors, kidney or urinary disorders, cardiac disorders, neurological disorders, and liver or pancreas disorders. The other broad categories of health conditions reported in HLES were not analyzed because they were either based on temporary situational and/or environmental factors and thus unlikely to be associated with feeding frequency (e.g., trauma, ingesting toxic substances, infectious or parasitic disorders), were infrequently reported and thus had a very small sample size (less than 3.5% of the total sample; e.g., respiratory disorders, endocrine disorders, reproductive system disorders, immune-mediated disorders, and hematopoietic disorders), or there was no compelling rationale as to why feeding frequency would affect them (e.g., ear, nose, and throat disorders, eye disorders).
For the health categories examined in this investigation, all participants were assigned a binary score (affected/unaffected). Dogs were considered “affected” if their owner reported them to have at least one relevant condition within a given category. However, we did not consider any congenital health outcomes as affected: since animals were born with these conditions, their feeding regimen was by definition instituted after onset and could therefore not have affected the development of the condition. Similarly, disorders linked to transient situational factors, including infectious diseases and trauma, were not considered as affected, as the circumstantial nature of these instances made them unlikely to be affected by feeding frequency.
See Supplementary Information 1 for details of all inclusion/exclusion criteria, as well as the specific conditions that qualified a dog as affected within the dental or oral disease, skin disorders, orthopedic disorders, gastrointestinal disorders, cancer or tumors, kidney or urinary disorders, cardiac disorders, neurological disorders, and liver or pancreas disorders categories.
After applying exclusion criteria, the final sample consisted of responses from 24,238 HLES surveys and 10,474 CSLB surveys. The CSLB was always completed at least 1 week after completion of HLES. Most participants in the final sample (88%) completed CSLB within 3 months of completing HLES and always within a year (range: 7 to 352 days, average: 47 days).
Explanatory variables
We analyzed feeding frequency as a binary exposure, comparing dogs fed once-daily to dogs fed more frequently. Specifically, owners were asked “How many times per day is your dog fed?” The dogs of owners who answered “Once” were sorted into the once-daily category, whereas the dogs of owners who answered “Twice”, “Three or more,” or “Free-fed (filling up bowl when empty or always having food available)” were sorted into the fed-more-frequently category. In all analyses, 8% of the total sample was fed once daily (Tables 1 and 2).
Table 1.
Characteristics of 10,474 dogs in CSLB analysis (76 pure breeds included)
| Explanatory variable | n (%) or mean (SD) |
|---|---|
| Age | |
| 6–9.9 years | 4956 (47%) |
| 10–18 (not including 18) years | 5518 (53%) |
| Sex | |
| Male, castrated | 5042 (48%) |
| Female, spayed | 5432 (52%) |
| Body size and weight | |
| Small (< 10 kg) | 2673 (26%) |
| Middle (10–29.9 kg) | 5064 (48%) |
| Large (30–44.9 kg) | 2389 (23%) |
| Giant (≥ 45 kg) | 348 (3%) |
| Breed | |
| Mixed-breed dog | 5885 (56%) |
| Labrador Retriever | 616 (6%) |
| Golden Retriever | 463 (4%) |
| German Shepherd | 192 (2%) |
| Dachshund | 159 (2%) |
| Australian Shepherd | 149 (1%) |
| Poodle (standard) (≥ 13.6 kg) | 130 (1%) |
| Border Collie | 124 (1%) |
| Chihuahua | 107 (1%) |
| Beagle | 105 (1%) |
| Shih Tzu | 93 (1%) |
| Other purebred dogsa | 2451 (23%) |
| Feeding frequency | |
| Fed once per day | 860 (8%) |
| Fed twice per day | 7779 (74%) |
| Fed three or more times per day | 789 (8%) |
| Free fed | 1046 (10%) |
| Fatty acid supplement | |
| Given daily or more often | 2252 (22%) |
| Cognitive activity | |
| Primary or secondary activity requires training | 1759 (17%) |
| CSLB | |
| Score | 36.4 (5.3) |
| Primary diet componentb | |
| Commercial, dry | 8506 (81%) |
| Commercial, canned | 583 (6%) |
| Commercial, freeze-dried | 421 (4%) |
| Commercial, refrigerated/frozen | 357 (3%) |
| Home-prepared, cooked | 151 (1%) |
| Commercial, semi-dry/semi-moist | 128 (1%) |
| Home-prepared, raw | 110 (1%) |
| Other | 218 (2%) |
aSee Supplementary Information 4 for full list and numbers of purebred dogs included in the CSLB analysis
bThis data is included in the table for descriptive purposes only and was not incorporated into our analyses
Table 2.
Characteristics of 24,238 dogs in analysis of health outcomes (100 pure breeds included)
| Explanatory variable | n (%) |
|---|---|
| Age | |
| 1–1.9 years | 1672 (7%) |
| 2–5.9 years | 7721 (32%) |
| 6–9.9 years | 7082 (29%) |
| 10–18 (not including 18) years | 7763 (32%) |
| Sex | |
| Male, castrated | 11853 (49%) |
| Female, spayed | 12385 (51%) |
| Body size and weight | |
| Small (< 10 kg) | 5510 (23%) |
| Middle (10–29.9 kg) | 12267 (51%) |
| Large (30–44.9 kg) | 5504 (23%) |
| Giant (≥ 45 kg) | 957 (4%) |
| Breed | |
| Mixed-breed dog | 13308 (55%) |
| Labrador retriever | 1467 (6%) |
| Golden retriever | 1199 (5%) |
| German Shepherd | 502 (2%) |
| Australian Shepherd | 373 (2%) |
| Poodle (standard) (≥ 13.6 kg) | 306 (1%) |
| Dachshund | 305 (1%) |
| Border Collie | 257 (1%) |
| Chihuahua | 205 (1%) |
| Beagle | 187 (1%) |
| Pug | 180 (1%) |
| Other purebred dogsa | 5949 (25%) |
| Feeding frequency | |
| Fed once per day | 1884 (8%) |
| Fed twice per day | 18027 (74%) |
| Fed three times or more per day | 1716 (7%) |
| Free fed | 2611 (11%) |
| Fatty acid supplement | |
| Given daily or more often | 4383 (18%) |
| Health outcomes | |
| Dental/oral | 6414 (26%) |
| Skin | 5619 (23%) |
| Orthopedic | 4270 (18%) |
| Gastrointestinal | 2429 (10%) |
| Cancer | 1906 (8%) |
| Kidney/urinary | 1740 (7%) |
| Cardiac | 1243 (5%) |
| Neurological | 972 (4%) |
| Liver/Pancreas | 673 (3%) |
| Primary diet componentb | |
| Commercial, dry | 20303 (84%) |
| Commercial, canned | 1025 (4%) |
| Commercial, freeze-dried | 934 (4%) |
| Commercial, refrigerated/frozen | 733 (3%) |
| Home-prepared, cooked | 329 (1%) |
| Commercial, semi-dry/semi-moist | 254 (1%) |
| Home-prepared, raw | 235 (1%) |
| Other | 425 (2%) |
aSee Supplementary Information 5 for full list and numbers of purebred dogs included in the analysis of health outcomes
bThis data is included in the table for descriptive purposes only and was not incorporated into our analyses
In our analyses, we adjusted for sex (spayed female or neutered male), age, breed for purebred dogs, and body size (as captured by weight) for mixed breed dogs. We also adjusted for whether the owner reported daily omega-3 (or other fatty acid) diet supplementation for all analyses except for dental/oral disorders and liver/pancreas disorders, as there is evidence in the literature that fatty acids can have beneficial effects on cognitive function, skin, cardiac, gastrointestinal, renal, orthopedic, and neoplastic outcomes [48–56]. For analysis of CSLB, we additionally adjusted for two factors that are thought to affect cognitive function: physical activity level [57] and whether the dog has a history of training (according to the dog’s primary or secondary activity indicated by the owner; e.g., show dogs, service dogs, and dogs trained for field trials vs. pets/companion dogs; see Supplementary Information 2 for full details) [58].
We adjusted for the breed of purebred dogs as a categorical variable. After inspecting the distribution of weight by breed, we subdivided standard poodles into two breeds for the analysis, large poodles (weight ≥ 13.6 kg (30 lb)) and small poodles (weight < 13.6 kg (30 lb)). Although there are over 200 breeds represented in DAP data, for each analysis, we only included breeds that had at least one exposed and one unexposed dog because breeds without variance in the exposure cannot inform the exposure-outcome association. We also restricted our analyses to breeds with at least 10 dogs meeting inclusion criteria. These restrictions reduced the number of breeds to 76 breeds for the CSLB analysis and 100 breeds for the analyses of health outcomes.
Statistical methods
All statistical analyses were carried out in R v.4.0.3 [59]. Age was flexibly modeled using natural splines with interior knots at 7, 10, and 14 years for CSLB analysis and interior knots at 2, 7, and 13 years for health outcomes [60]. Weight was similarly modeled using natural splines with interior knots at 14, 48, and 79 lbs. In each instance, interior knots are at approximately the 10th, 50th, and 90th percentile of each variable. We explored more elaborate adjustment models (e.g., 4 or 5 interior knots), but these were not supported by metrics such as AIC, and examination of some results suggested overfitting.
To adjust for physical activity, we performed principal component analysis on three HLES-reported activity variables: lifestyle activity level (reported as not active, moderately active, or very active over the past year), average activity intensity level (reported as low: walking, medium: jogging, or vigorous: sprinting, such as playing fetch or Frisbee), and average daily time spent physically active (reported in hours and minutes). Parallel analysis recommended retaining one principal component. This principal component captured 52% of the variance, and we used the loadings onto the first principal component as a physical activity score (PA-score). We adjusted for PA-score using natural splines with interior knots at approximately the 10th, 50th, and 90th percentiles.
Mixed breed dogs were included as a separate category of breed, and we adjusted for body size, as measured by weight, for mixed breed dogs only by constructing a variable weight*MB where weight is the dog’s weight and MB = 1 for mixed breed dogs and MB = 0 for purebred dogs. This is analogous to grouping mixed breed dogs by weight and including each group as a breed, except that our approach uses continuous weight information.
We used linear regression for analysis of CSLB and logistic regression for analysis of all health outcomes. For linear regression, the large number of parameters in the model due to 76 breeds does not cause statistical issues. However, large models are problematic for logistic regression when using conventional maximum likelihood model-fitting [61]. Therefore, we fit the logistic models using a conditional likelihood, where the conditioning was on the breed categories. This approach allowed breed to be in the model without necessitating the estimation of 100 breed parameters. Due to the large size of the dataset, maximizing the exact conditional likelihood was not computationally feasible, and we used the Efron approximation (reported in Supplementary Information 3). We used robust standard error estimates for all regression analyses. All hypothesis tests were two-sided and we did not adjust for multiple comparisons.
Secondary analyses
For analysis of CSLB, we performed a sensitivity analysis excluding 2% of dogs with scores < 20 (n = 10,288), as these very low scores are implausible and highly suggestive that the owner did not recognize that some survey questions reflected a bidirectional rather than a unidirectional scale.
For analysis of the nine categories of health conditions, we repeated the analysis using only mixed-breed dogs and dogs from the 10 most common breeds, fitting the model with ordinary logistic regression. The 10 most common breeds were Australian shepherd, beagle, Border collie, Chihuahua, dachshund, German shepherd, golden retriever, Labrador retriever, poodles (large), and pugs (Table 2). We also treated these analyses as secondary analyses to assess the robustness of our findings, including robustness given use of the Efron approximation for the primary analyses.
For all ten outcomes, we repeated our primary analyses but analyzed feeding frequency as a four-level unordered categorical factor.
Results
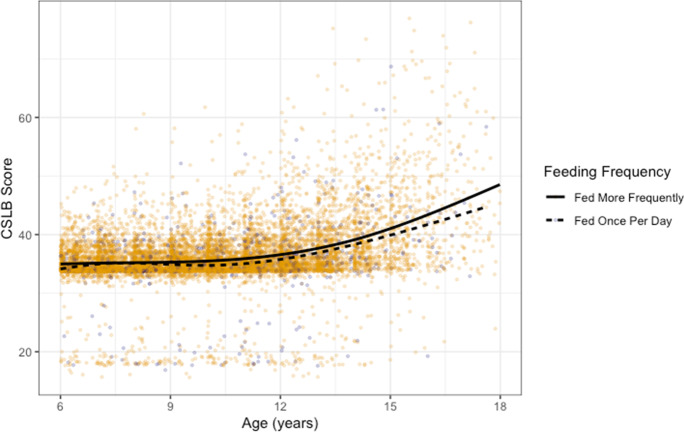
In the CSLB analysis (n = 10,474 dogs), 56% of dogs were mixed breed, and the remaining dogs belonged to 76 breeds (Table 1; Supplementary Information 4). Dogs fed once per day had, on average, a 0.62 point lower CSLB score than dogs fed more than once per day (95%: 0.27, 0.97; p < 0.001), adjusting for age, sex, weight (for mixed breed dogs), breed (for purebred dogs), cognitive activity, physical activity level, and fatty acid supplementation (Fig. 1; see Supplementary Information 3 for the full model). This effect size of 0.62 points is roughly the same difference in mean CSLB score between 11- and 7-year-old dogs. Results were very similar in the sensitivity analysis excluding 2% of dogs with very low CSLB scores (n = 10,288, 0.50 point lower CSLB score (95% CI: 0.20, 0.80), p = 0.0012).
Fig. 1.
Scatterplot of CSLB Scores vs. age with superimposed trend lines. Darker points represent dogs fed once daily and other points represent dogs fed more frequently. Trend lines were constructed separately for the two groups using natural splines. Dogs fed once daily have slightly lower mean CSLB score at all ages (6 ≤ age < 18 years)
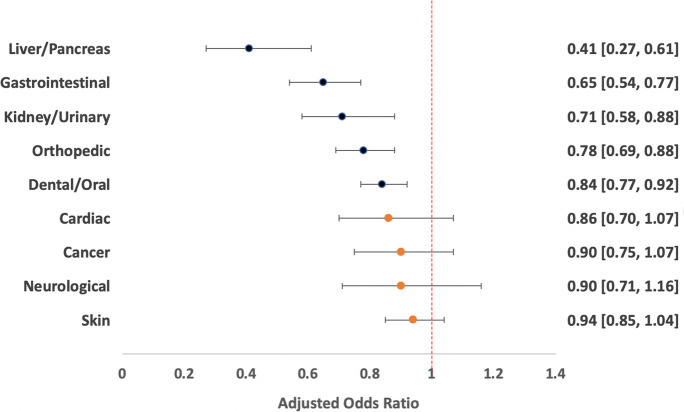
In the analyses of health conditions (n = 24,238 dogs), 55% of dogs were mixed breed, and the remaining dogs belonged to 100 breeds (Table 2; Supplementary Information 5). For five of the nine categories of health conditions analyzed, we found evidence that being fed once per day vs. more often is associated with lower odds of having the health condition (Fig. 2; Table 3). Adjusted odds ratios were less than one and statistically significant for gastrointestinal, dental/oral, orthopedic, kidney/urinary, and liver/pancreas health conditions. Adjusted odds ratios were also less than one for the remaining four categories of health conditions (cardiac, skin, neurological, cancer), but not statistically significant (see Supplementary Information 3 for detailed model results). Results were similar in secondary analyses including only mixed breed dogs and dogs from the ten most common breeds (see Supplementary Information 3 for full report).
Fig. 2.
Summary of results for analysis of health conditions. Circles represent point estimates of adjusted odds ratios, with darker circles indicating statistically significant results. Bars represent 95% confidence intervals. Odds ratios less than 1 indicate lower odds of the outcome among dogs fed once daily; odds ratios greater than 1 indicate higher odds of the outcome among dogs fed once daily
Table 3.
Estimated odds ratios of specific health condition for dogs fed once per day compared to more frequently, adjusted for sex, age, breed for purebred dogs, and body size (as captured by weight) for mixed breed dogs. All analyses except liver/pancreas and dental/oral are also adjusted for omega-3 (or other fatty acid) supplementation
| Health condition | Adjusted odds ratio | 95% CI | p |
|---|---|---|---|
| Liver/pancreas | 0.41 | 0.27–0.61 | < 0.001 |
| Gastrointestinal | 0.65 | 0.54–0.77 | < 0.001 |
| Kidney/urinary | 0.71 | 0.58–0.88 | 0.0012 |
| Orthopedic | 0.78 | 0.69–0.88 | < 0.001 |
| Dental/oral | 0.84 | 0.77–0.92 | < 0.001 |
| Cardiac | 0.86 | 0.70–1.07 | 0.18 |
| Cancer | 0.90 | 0.75–1.07 | 0.24 |
| Neurological | 0.90 | 0.71–1.16 | 0.42 |
| Skin | 0.94 | 0.85–1.04 | 0.22 |
In the secondary analyses treating feeding frequency as a four-level unordered categorical variable, results were very consistent with the primary analysis for dogs fed twice-daily and dogs fed three or more times daily (see Supplementary Information 6). These dogs had higher CSLB scores and higher odds of a health condition compared to dogs fed once daily. Results were somewhat more ambiguous for free-fed dogs. In particular, for dental/oral and kidney/urinary conditions, free-fed dogs in our data were less likely to have a health condition compared to dogs fed once daily, although results were statistically insignificant.
Discussion
Using observational data from the Dog Aging Project, this is the largest study to date of feeding frequency conducted in companion dogs. We found that adult dogs fed once daily have better average cognitive scores and are less likely to have gastrointestinal, dental/oral, orthopedic, kidney/urinary, and liver/pancreas health conditions than dogs fed more frequently. While it is important to note that this study does not demonstrate causality, our observations are consistent with prior work in laboratory mice and observational studies in humans [62] suggesting that diets that restrict the timing of feeding are associated with better cognitive function and physical health.
In addition to being able to observe the animals in a naturalistic versus laboratory setting, one of the major strengths of our investigation is the large sample size of dogs included (CSLB assessment: 10,474 dogs; all other health conditions: 24,238 dogs). Furthermore, our statistical methods used flexible adjustment of continuous covariates (age, weight, and physical activity), reducing the possibility of residual confounding by these factors.
The key limitation of this work is that it is a cross-sectional analysis. The analysis implicitly assumes that each dog’s feeding frequency has been the same over some meaningful period of the dog’s life. Importantly, we cannot rule out the possibility that dog owners shifted to more frequent feeding in response to health conditions, and observed associations are due in whole or part to reverse causality. This is a particular concern for gastrointestinal conditions and liver conditions, which are the two categories of health conditions with the strongest observed associations. Such a shift would not be captured in the current dataset as owners reported on their dog’s current feeding frequency but did not provide information on feeding frequency history. In the future, we will gather this information through annual “snapshots” since participants complete HLES each year. As the Dog Aging Project accrues longitudinal data over the next several years, investigations can compare dogs with different feeding frequencies who do not have a health condition and prospectively examine incidence of the condition. Such analyses can provide stronger evidence for a causal effect of feeding frequency on health.
It is plausible that once-daily feeding tends to result in lower overall caloric intake compared to more frequent feeding. Since we do not have data on caloric intake, we cannot analyze whether observed associations are mediated by caloric intake or reflect a possible effect of feeding frequency through other pathways. Caloric restriction has been previously reported to extend lifespan and improve health in Labrador retrievers maintained in a laboratory setting [5], although it has not yet been studied in other breeds of dogs or in companion dogs.
This study has other limitations. All data are owner-reported and thus subject to error in recall and interpretation. However, while a given owner’s responses on their dog’s cognitive function, physical activity, and other health conditions might reflect individual differences in interpretation and reporting errors, it is unlikely that these would generate the specific associations we observed. We were also unable to account for dogs reported as fed once-daily but who received snacks and treats throughout the day. Although HLES gathers data on frequency of treats, we did not use these data because the caloric content of treats was unknown. Furthermore, we did not have adequately detailed data to account for the composition of the diets fed, although we do know that the majority of dogs (over 80%) ate a diet consisting primarily of dry, commercial dog food. Finally, due to the rarity of intact dogs in our sample, analyses included only spayed and neutered dogs. While age at spay or neuter might be an important factor for some health outcomes [63, 64], this information was not incorporated into our analyses because data on the timing of gonadectomy were not available with sufficient detail or completeness.
Studies of obesity, including possible associations with feeding frequency [23], will be an important area of future research. This investigation did not consider obesity because information on dogs’ body condition scores was not available. We anticipate that these data will be available in the future when owners share their dogs’ veterinary electronic medical records (VEMR) with the Dog Aging Project.
We view once-daily feeding to be a model of time-restricted feeding and did not expect to see associations between health and feeding frequency among dogs fed more frequently. However, our secondary analyses revealed an intriguing trend for all nine categories of health conditions (not including CSLB). Specifically, we observe higher odds of a health condition from once-daily to twice-daily to three-or-more-times daily feeding. On the other hand, free-fed dogs often did not follow this trend. We speculate that free-fed dogs represent a heterogeneous group that includes dogs with high caloric intake as well as dogs whose owners provide constant access to food because the dog eats very little. We also recognize that free-fed dogs may naturally restrict their period of food consumption each day. While these results are intriguing, we see these analyses as exploratory and hypothesis-generating.
Given the limitations of this cross-sectional, observational study, the results of this investigation should not be used to make decisions about the feeding or clinical care of companion dogs. However, if supported by future studies, it may be prudent to revisit the currently predominant recommendation that adult dogs be fed twice daily. The rationale for twice-daily feeding in dogs is obscure (although see [65]), and our study suggests that more frequent feeding may, in fact, be suboptimal for several age-related health outcomes.
We view these results as an exciting first step of an ongoing exploration of the impact of diet on companion dogs living in human environments. Given the intense interest in, and popularization of, “longevity diets” such as intermittent fasting and time-restricted feeding, these types of studies in dogs are both timely and important. We believe these studies will ultimately offer insights into factors that promote health and longevity for both dogs and humans.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 Supplementary Information 1: Summary of the inclusion and exclusion criteria for subjects across all analyses, including guidelines for how all relevant variables were coded. (PDF 241 KB)
Supplementary file2 Supplementary Information 2: Criteria for determining whether or not a dog had a history of training (coded as a binary variable). (PDF 159 KB)
Supplementary file3 Supplementary Information 3: Regression outputs from the CSLB analysis, as well as the regression outputs from the health outcome analyses (both primary and secondary). (PDF 304 KB)
Supplementary file4 Supplementary Information 4: Complete list of purebred dogs (n = 76) included in the CSLB analysis, with sample sizes. (PDF 144 KB)
Supplementary file5 Supplementary Information 5: Complete list of purebred dogs (n = 100) included in analysis of health conditions, with sample sizes. (PDF 147 KB)
Supplementary file6 Supplementary Information 6: Secondary Analyses of four-level unordered categorical feeding frequency. (PDF 303 KB)
Acknowledgements
The Dog Aging Project thanks study participants, their dogs, and community veterinarians for their important contributions.
Dog Aging Project Consortium Authors
Joshua M. Akey1, Brooke Benton2, Elhanan Borenstein3,4,5, Marta G. Castelhano6, Amanda E. Coleman7, Kate E. Creevy8, Kyle Crowder9,10, Matthew D. Dunbar10, Virginia R. Fajt11, Annette L. Fitzpatrick12,13,14, Unity Jeffrey15, Erica C. Jonlin2,16, Elinor K. Karlsson17,18, Jonathan M. Levine8, Jing Ma19, Robyn L. McClelland20, Daniel E.L. Promislow2,21, Audrey Ruple22, Stephen M. Schwartz13,23, Sandi Shrager24, Noah Snyder-Mackler25,26,27, Silvan R. Urfer2, Benjamin S. Wilfond28,29
1Lewis-Sigler Institute for Integrative Genomics, Princeton University, Princeton, NJ, USA
2Department of Laboratory Medicine and Pathology, University of Washington School of Medicine, Seattle, WA, USA
3Department of Clinical Microbiology and Immunology, Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel
4Blavatnik School of Computer Science, Tel Aviv University, Tel Aviv, Israel
5Santa Fe Institute, Santa Fe, NM, USA
6Cornell Veterinary Biobank, College of Veterinary Medicine, Cornell University, Ithaca, NY, USA
7Department of Small Animal Medicine and Surgery, College of Veterinary Medicine, University of Georgia, Athens, GA, USA
8Department of Small Animal Clinical Sciences, Texas A&M University College of Veterinary Medicine & Biomedical Sciences, College Station, TX, USA
9Department of Sociology, University of Washington, Seattle, WA, USA
10Center for Studies in Demography and Ecology, University of Washington, Seattle, WA, USA
11Department of Veterinary Physiology and Pharmacology, Texas A&M University College of Veterinary Medicine & Biomedical Sciences, College Station, TX, USA
12Department of Family Medicine, University of Washington, Seattle, WA, USA
13Department of Epidemiology, University of Washington, Seattle, WA, USA
14Department of Global Health, University of Washington, Seattle, WA, USA
15Department of Veterinary Pathobiology, Texas A&M University College of Veterinary Medicine & Biomedical Sciences, College Station, TX, USA
16Institute for Stem Cell and Regenerative Medicine, University of Washington, Seattle, WA, USA
17Bioinformatics and Integrative Biology, University of Massachusetts Chan Medical School, Worcester, MA, USA
18Broad Institute of MIT and Harvard, Cambridge, MA, USA
19Division of Public Health Sciences, Fred Hutchinson Cancer Research Center, Seattle, WA, USA
20Department of Biostatistics, University of Washington, Seattle, WA, USA
21Department of Biology, University of Washington, Seattle, WA, USA
22Department of Population Health Sciences, Virginia-Maryland College of Veterinary Medicine, Virginia Tech, Blacksburg, VA, USA
23Epidemiology Program, Fred Hutchinson Cancer Research Center, Seattle, WA, USA
24Department of Biostatistics, Collaborative Health Studies Coordinating Center, University of Washington, Seattle, WA, USA
25School of Life Sciences, Arizona State University, Tempe, AZ, USA
26Center for Evolution and Medicine, Arizona State University, Tempe, AZ, USA
27School for Human Evolution and Social Change, Arizona State University, Tempe, AZ, USA
28Treuman Katz Center for Pediatric Bioethics, Seattle Children's Research Institute, Seattle, WA, USA
29Department of Pediatrics, Division of Bioethics and Palliative Care, University of Washington School of Medicine, Seattle, WA, USA
Author contribution
All authors contributed to writing — review and editing. E.B.: conceptualization, methodology, data curation, writing — original draft, and project administration. Z.Z.: conceptualization, methodology, formal analysis, and visualization. K.T.: conceptualization and data curation. B.M.: data curation. DAP consortium: resources. M.K.: conceptualization, writing — original draft, and funding acquisition. K.K.: conceptualization, methodology, formal analysis, data curation, writing — original draft, visualization, project administration, and supervision.
Funding
The Dog Aging Project is supported by U19AG057377 and R24AG073137 from the National Institute on Aging, a part of the National Institutes of Health, and by additional grants and private donations. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Data availability
These data are housed on the Terra platform at the Broad Institute of MIT and Harvard.
Code availability
This study did not use custom code or mathematical algorithms.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Emily E. Bray, ebray@email.arizona.edu
Dog Aging Project Consortium:
Joshua M. Akey, Brooke Benton, Elhanan Borenstein, Marta G. Castelhano, Amanda E. Coleman, Kate E. Creevy, Kyle Crowder, Matthew D. Dunbar, Virginia R. Fajt, Annette L. Fitzpatrick, Unity Jeffrey, Erica C. Jonlin, Elinor K. Karlsson, Jonathan M. Levine, Jing Ma, Robyn L. McClelland, Daniel E. L. Promislow, Audrey Ruple, Stephen M. Schwartz, Sandi Shrager, Noah Snyder-Mackler, Silvan R. Urfer, and Benjamin S. Wilfond
References
- 1.Weindruch R, Walford RL. The retardation of aging and disease by dietary restriction. Springfield, IL: Charles C Thomas Pub Limited. 1988.
- 2.Anderson RM, Weindruch R. The caloric restriction paradigm: implications for healthy human aging. Am J Hum Biol. 2012;24:101–106. doi: 10.1002/ajhb.22243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mattison JA, Colman RJ, Beasley TM, et al. Caloric restriction improves health and survival of rhesus monkeys. Nat Commun. 2017;8:14063. doi: 10.1038/ncomms14063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kealy RD, Lawler DF, Ballam JM, et al. Effects of diet restriction on life span and age-related changes in dogs. J Am Vet Med Assoc. 2002;220:1315–1320. doi: 10.2460/javma.2002.220.1315. [DOI] [PubMed] [Google Scholar]
- 5.Lawler DF, Larson BT, Ballam JM, et al. Diet restriction and ageing in the dog: major observations over two decades. Br J Nutr. 2008;99:793–805. doi: 10.1017/S0007114507871686. [DOI] [PubMed] [Google Scholar]
- 6.Lee MB, Hill CM, Bitto A, Kaeberlein M. Antiaging diets: separating fact from fiction. Science. 2021;374:eabe7365. doi: 10.1126/science.abe7365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mattson MP, Longo VD, Harvie M. Impact of intermittent fasting on health and disease processes. Ageing Res Rev. 2017;39:46–58. doi: 10.1016/j.arr.2016.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Cabo R, Mattson MP. Effects of intermittent fasting on health, aging, and disease. N Engl J Med. 2019;381:2541–2551. doi: 10.1056/NEJMra1905136. [DOI] [PubMed] [Google Scholar]
- 9.Brandhorst S, Choi IY, Wei M, et al. A periodic diet that mimics fasting promotes multi-system regeneration, enhanced cognitive performance, and healthspan. Cell Metab. 2015;22:86–99. doi: 10.1016/j.cmet.2015.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wei M, Brandhorst S, Shelehchi M, et al. Fasting-mimicking diet and markers/risk factors for aging, diabetes, cancer, and cardiovascular disease. Sci Transl Med. 2017;9. 10.1126/scitranslmed.aai8700. [DOI] [PMC free article] [PubMed]
- 11.Newman JC, Covarrubias AJ, Zhao M, et al. Ketogenic diet reduces midlife mortality and improves memory in aging mice. Cell Metab. 2017;26:547–557.e8. doi: 10.1016/j.cmet.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roberts MN, Wallace MA, Tomilov AA, et al. A ketogenic diet extends longevity and healthspan in adult mice. Cell Metab. 2017;26:539–546.e5. doi: 10.1016/j.cmet.2017.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bostock ECS, Kirkby KC, Taylor BVM. The current status of the ketogenic diet in psychiatry. Front Psychiatry. 2017;8:43. doi: 10.3389/fpsyt.2017.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leung YB, Cave NJ, Heiser A, et al. Metabolic and immunological effects of intermittent fasting on a ketogenic diet containing medium-chain triglycerides in healthy dogs. Front Vet Sci. 2019;6:480. doi: 10.3389/fvets.2019.00480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Packer RMA, Law TH, Davies E, et al. Effects of a ketogenic diet on ADHD-like behavior in dogs with idiopathic epilepsy. Epilepsy Behav. 2016;55:62–68. doi: 10.1016/j.yebeh.2015.11.014. [DOI] [PubMed] [Google Scholar]
- 16.Hill CM, Kaeberlein M. Anti-ageing effects of protein restriction unpacked. Nature. 2021;589:357–358. doi: 10.1038/d41586-020-03662-x. [DOI] [PubMed] [Google Scholar]
- 17.Mirzaei H, Raynes R, Longo VD. The conserved role of protein restriction in aging and disease. Curr Opin Clin Nutr Metab Care. 2016;19:74–79. doi: 10.1097/MCO.0000000000000239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mitchell SJ, Bernier M, Mattison JA, et al. Daily fasting improves health and survival in male mice independent of diet composition and calories. Cell Metab. 2019;29:221–228.e3. doi: 10.1016/j.cmet.2018.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gill S, Le HD, Melkani GC, Panda S. Time-restricted feeding attenuates age-related cardiac decline in Drosophila. Science. 2015;347:1265–1269. doi: 10.1126/science.1256682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Longo VD, Panda S. Fasting, circadian rhythms, and time-restricted feeding in healthy lifespan. Cell Metab. 2016;23:1048–1059. doi: 10.1016/j.cmet.2016.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hatori M, Vollmers C, Zarrinpar A, et al. Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Cell Metab. 2012;15:848–860. doi: 10.1016/j.cmet.2012.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martinez-Lopez N, Tarabra E, Toledo M, et al. System-wide benefits of intermeal fasting by autophagy. Cell Metab. 2017;26:856–871.e5. doi: 10.1016/j.cmet.2017.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chaix A, Zarrinpar A, Miu P, Panda S. Time-restricted feeding is a preventative and therapeutic intervention against diverse nutritional challenges. Cell Metab. 2014;20:991–1005. doi: 10.1016/j.cmet.2014.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang F, Chu X, Yin M, et al. mTOR and autophagy in normal brain aging and caloric restriction ameliorating age-related cognition deficits. Behav Brain Res. 2014;264:82–90. doi: 10.1016/j.bbr.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 25.Shin BK, Kang S, Da Sol K, Park S. Intermittent fasting protects against the deterioration of cognitive function, energy metabolism and dyslipidemia in Alzheimer’s disease-induced estrogen deficient rats. Exp Biol Med. 2018;243:334–343. doi: 10.1177/1535370217751610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vasconcelos AR, Yshii LM, Viel TA, et al. Intermittent fasting attenuates lipopolysaccharide-induced neuroinflammation and memory impairment. J Neuroinflamm. 2014;11:85. doi: 10.1186/1742-2094-11-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li L, Wang Z, Zuo Z. Chronic intermittent fasting improves cognitive functions and brain structures in mice. PLoS ONE. 2013;8:e66069. doi: 10.1371/journal.pone.0066069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Singh R, Lakhanpal D, Kumar S, et al. Late-onset intermittent fasting dietary restriction as a potential intervention to retard age-associated brain function impairments in male rats. Age. 2012;34:917–933. doi: 10.1007/s11357-011-9289-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stote KS, Baer DJ, Spears K, et al. A controlled trial of reduced meal frequency without caloric restriction in healthy, normal-weight, middle-aged adults. Am J Clin Nutr. 2007;85:981–988. doi: 10.1093/ajcn/85.4.981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cienfuegos S, Gabel K, Kalam F, et al. Effects of 4- and 6-h time-restricted feeding on weight and cardiometabolic health: a randomized controlled trial in adults with obesity. Cell Metab. 2020;32:366–378.e3. doi: 10.1016/j.cmet.2020.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carlson O, Martin B, Stote KS, et al. Impact of reduced meal frequency without caloric restriction on glucose regulation in healthy, normal-weight middle-aged men and women. Metabolism. 2007;56:1729–1734. doi: 10.1016/j.metabol.2007.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Witte AV, Fobker M, Gellner R, et al. Caloric restriction improves memory in elderly humans. Proc Natl Acad Sci U S A. 2009;106:1255–1260. doi: 10.1073/pnas.0808587106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leclerc E, Trevizol AP, Grigolon RB, et al. The effect of caloric restriction on working memory in healthy non-obese adults. CNS Spectr. 2020;25:2–8. doi: 10.1017/S1092852918001566. [DOI] [PubMed] [Google Scholar]
- 34.Qasrawi SO, Pandi-Perumal SR, BaHammam AS. The effect of intermittent fasting during Ramadan on sleep, sleepiness, cognitive function, and circadian rhythm. Sleep Breath. 2017;21:577–586. doi: 10.1007/s11325-017-1473-x. [DOI] [PubMed] [Google Scholar]
- 35.Harder-Lauridsen NM, Rosenberg A, Benatti FB, et al. Ramadan model of intermittent fasting for 28 d had no major effect on body composition, glucose metabolism, or cognitive functions in healthy lean men. Nutrition. 2017;37:92–103. doi: 10.1016/j.nut.2016.12.015. [DOI] [PubMed] [Google Scholar]
- 36.Hoffman JM, Creevy KE, Franks A, et al. The companion dog as a model for human aging and mortality. Aging Cell. 2018;17:e12737. doi: 10.1111/acel.12737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Perri AR, Feuerborn TR, Frantz LAF, et al. Dog domestication and the dual dispersal of people and dogs into the Americas. Proc Natl Acad Sci. 2021;118:e2010083118. doi: 10.1073/pnas.2010083118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee JH, Verma N, Thakkar N, et al. Intermittent fasting: physiological implications on outcomes in mice and men. Physiology. 2020;35:185–195. doi: 10.1152/physiol.00030.2019. [DOI] [PubMed] [Google Scholar]
- 39.Kaeberlein M, Creevy KE, Promislow DEL. The dog aging project: translational geroscience in companion animals. Mamm Genome. 2016;27:279–288. doi: 10.1007/s00335-016-9638-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Creevy KE, Akey JM, Kaeberlein M, et al. An open science study of ageing in companion dogs. Nature. 2022;602:51–57. doi: 10.1038/s41586-021-04282-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dog Aging Project. Dog Aging Project - 2020 Curated Data Release, version 1.1 [Data file and codebook]. 2021. https://app.terra.bio/. Terra at the Broad Institute of MIT and Harvard.
- 42.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Salvin HE, McGreevy PD, Sachdev PS, Valenzuela MJ. The canine cognitive dysfunction rating scale (CCDR): a data-driven and ecologically relevant assessment tool. Vet J. 2011;188:331–336. doi: 10.1016/j.tvjl.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 45.Studzinski C, Christie L, Araujo J, et al. Visuospatial function in the beagle dog: an early marker of cognitive decline in a model of human aging and dementia. Neurobiol Learn Mem. 2006;86:197–204. doi: 10.1016/j.nlm.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 46.Harvey ND. How Old Is My Dog? Identification of rational age groupings in pet dogs based upon normative age-linked processes. Front Vet Sci. 2021;8:643085. doi: 10.3389/fvets.2021.643085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Packer RMA, McGreevy PD, Salvin HE, et al. Cognitive dysfunction in naturally occurring canine idiopathic epilepsy. PLoS ONE. 2018;13:e0192182. doi: 10.1371/journal.pone.0192182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ogilvie GK, Fettman MJ, Mallinckrodt CH, et al. Effect of fish oil, arginine, and doxorubicin chemotherapy on remission and survival time for dogs with lymphoma. Cancer. 2000;88:1916–1928. [PubMed] [Google Scholar]
- 49.Zicker SC, Jewell DE, Yamka RM, Milgram NW. Evaluation of cognitive learning, memory, psychomotor, immunologic, and retinal functions in healthy puppies fed foods fortified with docosahexaenoic acid–rich fish oil from 8 to 52 weeks of age. J Am Vet Med Assoc. 2012;241:583–594. doi: 10.2460/javma.241.5.583. [DOI] [PubMed] [Google Scholar]
- 50.Brown SA, Brown CA, Crowell WA, et al. Beneficial effects of chronic administration of dietary ω-3 polyunsaturated fatty acids in dogs with renal insufficiency. J Lab Clin Med. 1998;131:447–455. doi: 10.1016/s0022-2143(98)90146-9. [DOI] [PubMed] [Google Scholar]
- 51.Freeman LM, Rush JE, Markwell PJ. Effects of dietary modification in dogs with early chronic valvular disease. J Vet Intern Med. 2006;20:1116–1126. doi: 10.1892/0891-6640(2006)20[1116:eodmid]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 52.Mueller RS, Fettman MJ, Richardson K, et al. Plasma and skin concentrations of polyunsaturated fatty acids before and after supplementation with n-3 fatty acids in dogs with atopic dermatitis. Am J Vet Res. 2005;66:868–873. doi: 10.2460/ajvr.2005.66.868. [DOI] [PubMed] [Google Scholar]
- 53.Hickman MA, Anne Hickman M. Interventional nutrition for gastrointestinal disease. Clin Tech Small Anim Pract. 1998;13:211–216. doi: 10.1016/S1096-2867(98)80005-4. [DOI] [PubMed] [Google Scholar]
- 54.Fritsch D, Allen TA, Dodd CE, et al. Dose-titration effects of fish oil in osteoarthritic dogs. J Vet Intern Med. 2010;24:1020–1026. doi: 10.1111/j.1939-1676.2010.0572.x. [DOI] [PubMed] [Google Scholar]
- 55.Comblain F, Serisier S, Barthelemy N, et al. Review of dietary supplements for the management of osteoarthritis in dogs in studies from 2004 to 2014. J Vet Pharmacol Ther. 2016;39:1–15. doi: 10.1111/jvp.12251. [DOI] [PubMed] [Google Scholar]
- 56.Hadley KB, Bauer J, Milgram NW. The oil-rich alga Schizochytrium sp. as a dietary source of docosahexaenoic acid improves shape discrimination learning associated with visual processing in a canine model of senescence. Prostaglandins Leukot Essent Fat Acids. 2017;118:10–18. doi: 10.1016/j.plefa.2017.01.011. [DOI] [PubMed] [Google Scholar]
- 57.Cotman CW, Berchtold NC. Physical activity and the maintenance of cognition: learning from animal models. Alzheimers Dement. 2007;3:S30–S37. doi: 10.1016/j.jalz.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 58.Milgram NW, Siwak-Tapp CT, Araujo J, Head E. Neuroprotective effects of cognitive enrichment. Ageing Res Rev. 2006;5:354–369. doi: 10.1016/j.arr.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 59.R Development Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. 2016. Retrieved from http://www.R-project.org.
- 60.Harrell FE. Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. Springer. 2001;20–24.
- 61.Peduzzi P, Concato J, Kemper E, et al. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49:1373–1379. doi: 10.1016/s0895-4356(96)00236-3. [DOI] [PubMed] [Google Scholar]
- 62.Regmi P, Heilbronn LK. Time-restricted eating: benefits, mechanisms, and challenges in translation. iScience. 2020;23:101161. doi: 10.1016/j.isci.2020.101161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zlotnick M, Corrigan V, Griffin E, et al. Incidence of health and behavior problems in service dog candidates neutered at various ages. Front Vet Sci. 2019;6:334. doi: 10.3389/fvets.2019.00334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Simpson M, Albright S, Wolfe B, et al. Age at gonadectomy and risk of overweight/obesity and orthopedic injury in a cohort of Golden Retrievers. PLoS ONE. 2019;14:e0209131. doi: 10.1371/journal.pone.0209131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Raghavan M, Glickman N, McCabe G, et al. Diet-related risk factors for gastric dilatation-volvulus in dogs of high-risk breeds. J Am Anim Hosp Assoc. 2004;40:192–203. doi: 10.5326/0400192. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary file1 Supplementary Information 1: Summary of the inclusion and exclusion criteria for subjects across all analyses, including guidelines for how all relevant variables were coded. (PDF 241 KB)
Supplementary file2 Supplementary Information 2: Criteria for determining whether or not a dog had a history of training (coded as a binary variable). (PDF 159 KB)
Supplementary file3 Supplementary Information 3: Regression outputs from the CSLB analysis, as well as the regression outputs from the health outcome analyses (both primary and secondary). (PDF 304 KB)
Supplementary file4 Supplementary Information 4: Complete list of purebred dogs (n = 76) included in the CSLB analysis, with sample sizes. (PDF 144 KB)
Supplementary file5 Supplementary Information 5: Complete list of purebred dogs (n = 100) included in analysis of health conditions, with sample sizes. (PDF 147 KB)
Supplementary file6 Supplementary Information 6: Secondary Analyses of four-level unordered categorical feeding frequency. (PDF 303 KB)
Data Availability Statement
These data are housed on the Terra platform at the Broad Institute of MIT and Harvard.
This study did not use custom code or mathematical algorithms.