Abstract
Background
Cough caused by endotracheal tube (ETT) placement is ubiquitous and correlates with adverse outcomes. Remifentanil administration via target-controlled infusion (TCI) is one of the cough prevention measures used during recovery. In a pilot study, lidocaine administered via the perforated outer cuff of a dual-cuff endotracheal tube was also found to prevent cough due to ETT placement. We therefore compared these two cough prevention approaches during recovery after thyroidectomy in a single-centre, double-blind, randomised study conducted in China during the period from 09/10/2020 to 30/04/2021.
Methods
Ninety-eight female patients aged 18–65 years with American Society of Anaesthesiologists Physical Status scores of I and II were scheduled to undergo thyroidectomy. The ETT contained an internal cuff covered by a perforated outer cuff to allow for lidocaine delivery. Patients were randomised to receive either 4 ml of saline solution (Group R, n = 49) or 4 ml of 2% lidocaine in the outer cuff (Group L, n = 49) at the beginning of skin suturing. Remifentanil (2 ng/ml) was maintained in Group R until extubation, while remifentanil was maintained in Group L until the end of skin suturing. The primary outcome was cough during patient transfer, at 1 min before extubation, and at extubation. The secondary outcomes were haemodynamics and other recovery parameters.
Results
Primary outcomes were compared between remifentanil vs. lidocaine application, namely, the incidence of cough during patient transfer (0% in Group R vs. 0% in Group L), at 1 min before extubation (22.45% in Group R vs. 4.08% in Group L; P = 0.015), and at extubation (61.22% in Group R vs. 20.41% in Group L; P < 0.001). Compared with remifentanil, lidocaine more effectively decreased heart rate elevation and hypoxemia at 5 min after extubation, the spontaneous respiration recovery time, the extubation time, the duration of post-anaesthesia care unit (PACU) stay, Richmond Agitation-Sedation Scale scores in the agitated range and Critical-Care Pain Observation Tool scores.
Conclusion
Lidocaine administered via the perforated outer cuff of the ETT significantly improved recovery from general anaesthesia compared to remifentanil in female patients after thyroidectomy.
Trial registration
Chinese Clinical Trial Registry (No. ChiCTR2000038653), registered on 27/09/2020.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12871-022-01734-1.
Keywords: Anaesthesia, General, Anaesthesia topical, Lidocaine, Endotracheal tube, Modified dual-cuff, Opioid, Remifentanil
Introduction
Cough is ubiquitous (76–80%) during recovery from general anaesthesia and endotracheal tube placement [1, 2], which correlates with hypertension and tachycardia [3, 4], agitation [5] and postoperative haemorrhage [6]. Cough prevention during recovery is recommended for patients with suspected or confirmed coronavirus disease (COVID-19), as it can reduce airborne particles and droplets [7]. Cough prevention is also imperative for reducing the incidence of breathing difficulty associated with haemorrhage after thyroidectomy [8].
Remifentanil administration via target-controlled infusion (TCI) is one of the cough prevention measures used during recovery [9, 10]. In addition, to adequately reduce the stimulation of the tracheal mucosa in contact with the cuff of the EET, we modified a dual-cuff, creating a “disposable reinforced tracheal intubation double balloon dosing-type” endotracheal tube (Supplemental Fig. 1, Xi’an Shen Lan Biomedical Engineering Co., Ltd, China) (Supplemental Video 1), and found that the topical administration of lidocaine via the dual-cuff ETT could effectively prevent cough during recovery. In the pilot study, one patient was intubated with the dual-cuff ETT while sitting up in bed and signing her name (Supplemental Video 2). This dual-cuff ETT (Supplemental Fig. 2B) contains an internal cuff covered by an outer cuff. The small-bore channel is incorporated within the wall of the endotracheal tube and is the channel that delivers lidocaine to the perforated outer cuff through 16 small holes (Supplemental Video 3). The benefit of a modified dual-cuff ETT is that the tracheal mucosa in contact with the outer cuff receives topical anaesthesia by lidocaine via the perforated outer cuff without deflation of the internal cuff, so it is not restricted by the timing of lidocaine administration.
This single-centre, double-blind, randomised study was designed to evaluate the hypothesis that cough prevention with the topical lidocaine approach via the dual-cuff ETT before extubation would be better than that with remifentanil administration during recovery after thyroidectomy. Cough during recovery was chosen as the primary outcome for further study of the potential benefits of a modified dual-cuff ETT, such as the prevention of cough during the recovery of patients with suspected or confirmed COVID-19. The main secondary outcomes included haemodynamics, the time to recovery, hypoxemia, and other recovery parameters.
Materials and methods
Ethics and registration
Ethical approval for this study (Ethical Committee IRB: ZF2020-130.2–01) was provided by the Ethical Committee of Guangdong Provincial Hospital of Chinese Medicine, Guangzhou City, Guangdong Province, People’s Republic of China (Chairperson Prof. Jun Liu) on 28/08/2020. Written informed consent was obtained from each patient before study participation. The full trial protocol was registered before patient enrolment in the Chinese Clinical Trial Registry (ref: ChiCTR2000038653) on 27/09/2020 and adheres to the Consolidated Standards of Reporting Trials guidelines [11] and the Declaration of Helsinki.
In vitro experiments
To achieve an even distribution of lidocaine around the cuff, we modified a dual-cuff endotracheal tube and conducted a dyeing experiment in vitro. We evenly punctured small holes through the outer cuff as a dye liquid delivery channel. As the tracheal diameter ranges from 8.9–17 mm in women [12], a tube with an internal diameter of 14 mm was used to simulate the trachea, and graph paper was placed on the internal surface of the tube to record the outcome of the experiment. The dual-cuff ETT was placed into a 14 mm tube lined with graph paper, and the internal cuff pressure was maintained at 25 cmH2O. To optimise the number of holes and the volume of dye liquid, we assessed the difference between 8 and 16 holes by using 1–4 ml of dye liquid to simulate lidocaine; this experiment was performed in triplicate. The dye liquid was fully transferred from the outer cuff by injecting 20 ml of air into the outer cuff.
Supplemental Fig. 2A shows the results of the dyeing experiment. There was no interaction between the number of holes (8 and 16 holes) and the dye liquid volume (1, 2, 3, and 4 ml) (P = 0.064). Pairwise comparisons of the area showed significant differences based on the number of holes (796.67 mm2 for 16 holes vs. 584.17 mm2 for 8 holes, P = 0.021) and the volume (937.67 mm2 for 4 ml vs. 477.50 mm2 for 1 ml, P < 0.001; 937.67 mm2 for 4 ml vs. 634.83 mm2 for 2 ml, P = 0.010; and 937.67 mm2 for 4 ml vs. 711.67 mm2 for 3 ml, P = 0.033). Based on these results, 16 holes and 4 ml of dye liquid was determined to be the optimal combination. This combination was subsequently used in vivo.
In vivo experiment
Study design
This single-centre, double-blind, randomised study was conducted at the Department of Anesthesiology, Guangdong Provincial Hospital of Chinese Medicine in Guangzhou, China, from 09/10/2020 to 30/04/2021.
Patients
All 98 females with ASA Physical Status scores of I–II, aged 18–65 years, a height of 140–180 cm and weight of 40–85 kg planned to undergo elective thyroidectomy due to a unilateral thyroid neoplasm (T1/T2 N0 M0 in Tumor-Node-Metastasis System/American Joint Committee on Cancer). The first patient was enrolled on 14/10/2020. The following patients were excluded: patients using a nerve integrity monitor (NIM) standard reinforced electromyography (EMG) endotracheal tube; patients with signs of a difficult airway, perioperative aspiration, or psychosis; patients with an acute respiratory tract infection lasting less than 2 weeks; patients who smoked less than 48 h before the procedure; patients who had an allergic reaction to lidocaine or a beta-adrenergic receptor line; and patients with serious cardiovascular, pulmonary, hepatic, or renal disease.
Randomisation
Patients were randomly allocated at a 1:1 ratio to receive either 4 ml of 2% lidocaine in the outer cuff (Group L) or the predicted effect-site concentration (Ce) of 2.0 ng/ml of TCI remifentanil (Group R), according to a computer-generated centralised random table with no block size and stratification factors. A unique randomisation number was removed from the sequentially numbered containers on the morning of surgery. The first anaesthetist generated the random allocation sequence, performed the randomisation, enrolled the participants, and assigned the participants to interventions, but he was not at all involved in anaesthesia management.
Blind evaluation
Three anaesthetists and 3 anaesthetist nurses participated in this study to conduct a blinded evaluation. The first anaesthetist was the only one with knowledge of the group assignments. The other anaesthetists, anaesthetist nurses, and patients were blinded to the groups. The first anaesthetist completed the following tasks at the beginning of skin suturing: shielding the TCI pump from other anaesthetists, controlling the TCI pump, and providing 4 ml of 2% lidocaine or 4 ml of saline solution to the second anaesthetist, who was blinded to the actual treatments. The second anaesthetist performed anaesthesia management, including intraoperative and postoperative care, except for the control of the TCI pump at the beginning of skin suturing. The third anaesthetist and 3 anaesthetist nurses recorded data for the variables in the post-anaesthesia care unit (PACU).
Intraoperative and postoperative care
Basic monitoring was performed at 3 min intervals. All patients received induction medication, including 1.5 mg/kg propofol, 0.2 mg/kg cisatracurium, the predicted effect-site concentration of TCI remifentanil (Ce 3.5 ng/ml) and 0.4 µg/kg sufentanil to facilitate tracheal intubation. Remifentanil was administered using a TCI pump (targeted effect-site TCI, Minto model and CONCERT-III, Guangxi VERYARK Technology Co., Ltd, China). All patients received a 7.0 mm modified dual-cuff ETT, and the internal cuff pressure was maintained at 20–30 cmH2O with a hand pressure gauge (Hi-Lo™ Hand Pressure Gauge, VBM Medizintechnik GmbH, Germany). Sevoflurane (1.2–2.5%) and TCI remifentanil (Ce 2–5 ng/ml) were used to maintain the mean arterial pressure (MAP) and heart rate (HR) within 20% of baseline (values at one day before surgery). The nasopharyngeal temperature was maintained at 36–37 ℃. The tidal volume and ventilatory frequency were adjusted using end-tidal carbon dioxide (ETCO2) at 34–45 mmHg.
At the beginning of skin suturing, sevoflurane was maintained at 1.4–1.5 times the end-tidal concentration, and remifentanil was maintained at 2 ng/ml. At the same time, 0.5 mg/kg of ketorolac was administered to relieve pain, and 4.48 mg of tropisetron was administered to prevent nausea and vomiting. Neostigmine (50 µg/kg) and atropine (15 µg/kg) were administered to reverse the neuromuscular block to confirm a train-of-four response greater than 90%. Patients with an ETT were randomised to receive either 4 ml of 2% lidocaine in the outer cuff (Group L) or 4 ml of saline solution (placebo) in the outer cuff (Group R), followed by 20 ml of air in the outer cuff at the beginning of skin suturing (each time the internal cuff pressure was less than 30 cmH2O). Remifentanil was maintained at 2 ng/ml in Group R and turned off at the time of tracheal extubation. Remifentanil in Group L and sevoflurane in both groups were turned off at the end of skin suturing (the end of surgery).
Patients with an ETT were transferred to the post-anaesthesia care unit (PACU) after confirmation of stable haemodynamics. During the transfer of patients (the phase from the operating table to the PACU), 2.0 ng/ml remifentanil by TCI was maintained for Group R, whereas remifentanil was stopped for Group L. The phase from the end of surgery to the beginning of transfer took 4 min, and patient transfer took 2 min. All the patients were taken to the PACU with the shielded TCI pump. Recovery profiles were recorded in the PACU by video after obtaining the patients’ consent. Manual ventilation was provided until the patient breathed spontaneously. Mild hypercapnia (end-tidal carbon dioxide, ETCO2 of 45–55 mmHg) was permitted to promote spontaneous respiration. Continuous verbal stimuli were used to prompt the patients to open their eyes without any other stimuli. After opening their eyes, the patients were asked to breathe deeply and nod their head. Extubation was completed when the patients could take an adequate breath on command (ETCO2 < 50 mmHg and ventilatory frequency > 12 beats/min), nod and shake hands on command and achieve spontaneous deglutition.
Primary outcome
The primary outcome was the incidence of cough during the recovery period. A cough was defined as any evidence of irritation from the tracheal tube [13]. Cough was recorded during patient transfer (the phase from the operating table to the PACU), at 1 min before extubation and at extubation.
Secondary outcomes
Data from the following five time points were analysed: T0, one day before surgery (baseline); T1, the end of surgery; T2, 1 min before extubation; T3, 5 min after extubation; and T4, 20 min after extubation. The secondary outcomes included the following variables: MAP and HR at the above five time points; elevation of blood pressure and heart rate at T2, T3 and T4 (MAP and HR increase by 30% from their respective values at baseline); eye opening time (time period from the end of surgery to first eye opening on command); consciousness recovery time (time period from the end of surgery to nodding on command); spontaneous respiration recovery time (time period from the end of surgery to an ETCO2 < 55 mmHg and a ventilatory frequency > 10 beats/min); extubation time (time period from the end of surgery to extubation); duration of PACU stay (the time period from the end of surgery to leaving the PACU); the Richmond Agitation-Sedation Scale (RASS) score [14] at T2; and the Critical-Care Pain Observation Tool (CPOT) score [15] at T2.
In addition, the secondary outcomes were a composite of the following variables: hypoxemia at T3 and T4 (less than 95% of Spo2); the sedation grading system (SGS) [16] at T3; postoperative pain at T4 (more than 5 points on the visual analogue scale); residual sedation at T4 (less than a Grade 2 on the SGS); nausea and vomiting at T4 (need for drugs); and pharyngalgia at T4 (swallowing with more than 3 points on the visual analogue scale).
Sample size calculation
PASS11 statistical software (NCSS, LLC) was used to calculate the sample size. The incidence rate of cough during recovery from general anaesthesia was 76% [1]. Based on the assumption that Ce 2.0 ng/ml of TCI remifentanil could suppress cough by 90% [17] and 4 ml of 2% lidocaine used with the dual-cuff endotracheal tube could suppress cough by 50% [16, 18], the proportion of cough suppression was 68.4% in the TCI remifentanil group and 38% in the lidocaine group. Forty-eight patients in each group would be required for 80% power and α = 0.05 with a two-sided Fisher exact test.
Statistical analysis
All values are expressed as the mean ± standard deviation (SD), median (25% – 75%) or number (proportion). Continuous variables with a normal distribution were assessed with a t test or repeated measures analysis of variance with Bonferroni correction. Continuous variables with nonnormal distributions were assessed using the Mann–Whitney U test. Categorical data were assessed using the χ2 test or Fisher’s exact test. SPSS Statistics 20 (SPSS Inc., Chicago, IL, USA) was used to assess the data. Statistical significance was set at P < 0.05.
Results
In vivo experiments
Patients
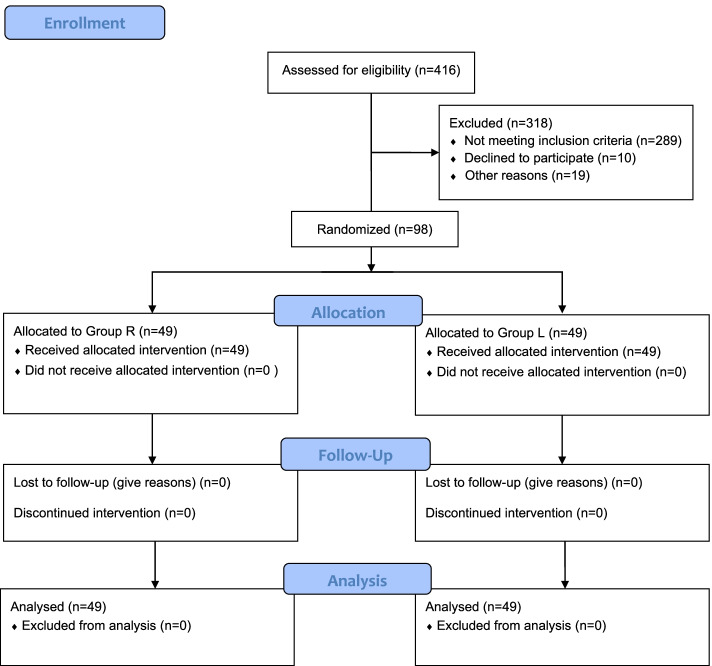
We assessed 416 patients, 98 of whom were enrolled in this study. All 98 patients completed the study [Group L (n = 49); Group R (n = 49)] (Fig. 1). The patient characteristics were similar between the two groups (Table 1).
Fig. 1.
CONSORT diagram of the randomised trial. R, remifentanil; L, topical lidocaine via the perforated outer cuff
Table 1.
Characteristics of the Patients Randomised between the Two Groups
| Characteristic | Group R (n = 49) | Group L (n = 49) | Z/Mean Difference/OR (95% CI) | P |
|---|---|---|---|---|
| Age (years), median (25% – 75%) | 49 (37–57) | 39 (33–50.5) | -1.94 (0.05–0.06) | 0.052a |
| ASA physical status (I/II), no. (%) | 41(84%)/8(16%) | 40(82%)/9(18%) | 1.153 (0.405–3.286) | 1b |
| Height (cm), mean ± SD | 158.2 ± 5.07 | 158.9 ± 5.23 | -0.70 (-2.72–1.41) | 0.532c |
| Weight (kg), median (25% – 75%) | 55 (50–63.5) | 55 (49.5–60) | -0.63 (0.52–0.54) | 0.531a |
| Duration of surgery (min), median (25% – 75%) | 84 (68–100.5) | 80 (71–99.5) | -0.44 (0.65–0.67) | 0.659a |
| Duration of anaesthesia (min), median (25% – 75%) | 121 (109–141) | 120 (108.5–132.5) | -0.47 (0.64–0.66) | 0.642a |
Abbreviations: ASA American Society of Anesthesiologists, R TCI of remifentanil, L Topical lidocaine via the perforated outer cuff, CI Confidence interval, OR Odds ratio, SD Standard deviation
a Mann–Whitney U test
b Fisher’s exact test
c t test
Primary outcomes
There were no patients with cough during patient transfer. The incidence of cough during T2 was significantly higher in Group R than in Group L (22.45% in Group R vs. 4.08% in Group L; P = 0.015). The incidence of cough during extubation was also significantly higher in Group R than in Group L (61.22% in Group R vs. 20.41% in Group L; P < 0.001) (Table 2).
Table 2.
Primary Outcome and Related Parameters
| Time | Cough | Group R (n = 49) | Group L (n = 49) | OR (95% CI) | P |
|---|---|---|---|---|---|
| Patient transfer | Cough occurrence, no. (%) | 0 (0%) | 0 (0%) | ||
| 1 min before tracheal extubation | Cough occurrence, no. (%) | 11 (22.45%) | 2 (4.08%) | 0.15 (0.03–0.70) | 0.015a |
| Tracheal extubation | Cough occurrence, no. (%) | 30 (61.22%) | 10 (20.41%) | 0.16 (0.07 – 0.40) | < 0.001a |
Abbreviations: R TCI of remifentanil, L Topical lidocaine via the perforated outer cuff, CI Confidence interval, OR Odds ratio. Transferring patients, the phase from the operating table to the post-anaesthesia care unit
a Fisher’s exact test
Secondary outcomes
The secondary outcomes are shown in Table 3. The groups did not differ significantly in terms of MAP or HR (Fig. 2), and the incidence of elevated blood pressure was similar between the groups. The occurrence of heart rate elevation at T2 and T4 was also similar between the groups, but the heart rate elevation at T3 (P = 0.0028) was significantly lower in Group L than in Group R. The time related to recovery from remifentanil vs. lidocaine was as follows: eye opening time, 8.3 min in Group R vs. 7.7 min in Group L (P = 0.460); consciousness recovery time, 9.2 min in Group R vs. 8.1 min in Group L (P = 0.346); spontaneous respiration recovery time, 12.3 min in Group R vs. 8.9 min in Group L (P < 0.001); extubation time, 15.0 min in Group R vs. 11.0 min in Group L (P = 0.009); and duration of PACU stay, 55.4 min in Group R vs. 46.4 min in Group L (P = 0.001). The RASS scores in the agitated range were significantly lower in Group L than in Group R (P = 0.012), but there was no significant difference in scores in terms of the alert, calm, and sedation ranges. CPOT scores were significantly higher in Group R than in Group L (P = 0.003). The occurrence of hypoxemia was significantly lower in Group L than in Group R at T3 (P < 0.001), but there was no significant difference observed at T4. The groups did not differ significantly in grade 2/grade 3 sedation at T3, postoperative moderate pain, nausea and vomiting, or pharyngalgia at T4. No residual sedation was observed at T4 in either group.
Table 3.
Secondary Outcomes and Related Components
| Components | Group R (n = 49) | Group L (n = 49) | Z/Mean Difference/OR (95% CI) | P |
|---|---|---|---|---|
| Elevation of blood pressure at T2, no. (%) | 3 (6.12%) | 3 (6.12%) | 1.00 (0.19–5.22) | 1b |
| Elevation of blood pressure at T3, no. (%) | 2 (4.08%) | 1 (2.04%) | 2.04 (0.18–23.29) | 1b |
| Elevation of blood pressure at T4, no. (%) | 2 (4.08%) | 2 (4.08%) | 1.00 (0.14–7.40) | 1b |
| Elevation of heart rate at T2, no. (%) | 13 (26.53%) | 5 (10.20%) | 3.18 (1.04–9.75) | 0.066b |
| Elevation of heart rate at T3, no. (%) | 16 (32.65%) | 6 (12.25%) | 3.48 (1.23–9.85) | 0.028b |
| Elevation of heart rate at T4, no. (%) | 6 (12.25%) | 7 (14.29%) | 0.84 (0.26–2.70) | 1b |
| Time related to recovery | ||||
| Eye opening time (min), mean ± SD | 8.3 ± 4.22 | 7.7 ± 3.05 | 0.6 (-0.93–2.03) | 0.460c |
| Consciousness recovery time (min), median (25% – 75%) | 9.2 (6.07–11.79) | 8.1 (6.12–10.56) | -0.94 (0.35–0.37) | 0.346a |
| Spontaneous respiration recovery time (min), median (25% – 75%) | 12.3 (9.07–21.00) | 8.9 (7.54–11.25) | -3.72 (0.00–0.0005) | < 0.001a |
| Extubation time (min), median (25% – 75%) | 15.0 (11.00–22.00) | 11.0 (10.00–15.00) | -2.60 (0.007–0.011) | 0.009a |
| Duration of PACU stay (min), mean ± SD | 55.4 ± 15.71 | 46.4 ± 11.05 | 9 (3.55–14.45) | 0.001c |
| RASS score at T2 | ||||
| > 0 agitated range, no. (%) | 8 (16.33%) | 1 (2.04%) | 0.09 (0.01–0.79) | 0.012b |
| 0 alert and calm, no. (%) | 26 (53.06%) | 35 (71.43%) | 2.21 (0.96–5.10) | 0.095b |
| < 0 sedation range, no. (%) | 15 (30.61%) | 13 (26.53%) | 0.64 (0.26–1.58) | 0.367b |
| CPOT score at T2, median (25% – 75%) | 1.04 ± 1.74 | 0.33 ± 1.14 | 0.71(0.12–1.31) | 0.003a |
| Hypoxemia occurrence at T3, no. (%) | 28 (57.14%) | 7(14.29%) | 8 (3.00–21.32) | < 0.001b |
| Hypoxemia occurrence at T4, no. (%) | 6 (12.24%) | 1 (2.04%) | 0.15 (0.02–1.29) | 0.111b |
| Grade of sedation at T3 (Grade 2/Grade 3), no. (%) | 13(27%)/36(73%) | 13(27%)/36(73%) | 1 (0.41–2.45) | 1b |
| Postoperative pain at T4, no. (%) | 1 (2.04%) | 1 (2.04%) | 1 (0.61–16.45) | 1b |
| Residual sedation at T4, no. (%) | 0 (0%) | 0 (0%) | ||
| Nausea and vomiting at T4, no. (%) | 4 (8.16%) | 1 (2.04%) | 0.23 (0.03–2.18) | 0.362b |
| Pharyngalgia at T4, no. (%) | 15 (30.61%) | 7 (14.29%) | 0.38 (0.14–1.03) | 0.89b |
Abbreviations: PACU Post-anaesthesia care unit, RASS Richmond Agitation-Sedation Scale, CPOT Critical-Care Pain Observation Tool, CI Confidence interval, R TCI of remifentanil, L Topical lidocaine via the perforated outer cuff, CI Confidence interval, OR Odds ratio, SD Standard deviation, T0 One day before surgery, T2 1 min before tracheal extubation, T3 5 min after tracheal extubation, T4 20 min after tracheal extubation. Elevation of blood pressure, increase by 30% from the mean arterial pressure at T0; elevation of heart rate, increase by 30% from the heart rate at T0; hypoxemia, Spo2 less than 95%; grade of sedation: Grade 0: deeply sedated and unresponsive; Grade 1: sedated but responsive to light glabellar tap; Grade 2: sedated but responsive to normal voice; Grade 3: awake and responsive. Postoperative pain, more than 5 points on the visual analogue scale (VAS); residual sedation, less than Grade 2; nausea and vomiting, need for drugs; pharyngalgia, swallowing with more than 3 points on the VAS
a Mann–Whitney U test
b Fisher’s exact test
c t test
Fig. 2.
Haemodynamic changes during emergence from general anaesthesia. Data are expressed as the mean (standard deviation). MAP is shown in panel A and heart rate is shown in panel B R, remifentanil; L, topical lidocaine via the perforated outer cuff; MAP, mean arterial pressure; T0, one day before surgery; T1, the end of surgery; T2, 1 min before extubation; T3, 5 min after extubation
Discussion
Compared with remifentanil, lidocaine via the perforated outer cuff more effectively decreased the incidence of cough during recovery, the rate of heart rate elevation, the spontaneous respiration recovery time, the extubation time, the duration of PACU stay, RASS scores in the agitated range, CPOT scores, and hypoxemia at T3. The other recovery parameters did not differ between the two groups.
A meta-analysis comparing treatments for cough suppression during recovery from general anaesthesia revealed that topical lidocaine is the least effective compared to dexmedetomidine, remifentanil, and fentanyl [19]. In addition, the extubation time was delayed after lidocaine administration via the intracuff compared with remifentanil [19]. However, the results of this study were not consistent with the ranking of treatments suppressing cough. Lidocaine administered via a topical route had a better antitussive effect and led to a shortened extubation time compared to remifentanil. The method of topical lidocaine administration in this study was different from the method of tracheal topical lidocaine used at present in the clinic. Topical tracheal lidocaine is currently administered via the tracheal tube or intracuff, by topical administration to the glottis or onto the tracheal mucosa via both upper and lower endotracheal tube cuffs [19]. The reduced efficacy observed for lidocaine administration in the clinic compared to that in this study is possibly due to the following reasons. Lidocaine administered via the tracheal tube before intubation for surgeries lasting < 2 h is undesirable for suppressing cough during recovery [20]. However, the duration of general anaesthesia in this study was > 2 h. The cough-suppressing effect of alkalinised lidocaine intracuff is dependent on the time necessary for the alkalinised lidocaine to permeate across the cuff membrane [21]. A dual-cuff ETT avoids this issue, as the perforations in the outer cuff allow lidocaine to rapidly distribute around the dual-cuff ETT. Lidocaine administered via a laryngotracheal instillation of topical anaesthesia (LITA) tube is distributed onto the glottis or both the upper and lower cuff before extubation [22, 13], resulting in cough suppression in only 75% [13] of patients during recovery, which is a lower rate than that obtained in this study. The tube cuff is a mechanical barrier that hinders the distribution of topical lidocaine anaesthesia to the tracheal mucosa [13]. The outer cuff of the modified dual-cuff ETT can break the mechanical barrier and does not require deflation for the administration of topical lidocaine onto the tracheal mucosa. The tracheal mucosa is under topical anaesthesia with lidocaine via the perforated outer cuff of the ETT, which reduces the stimulation of the tracheal mucosa. These factors could potentially explain the lower RASS and CPOT scores recorded in Group L in this study.
The high efficiency of lidocaine compared with remifentanil in this study was possibly due to the use of topical anaesthesia. The two methods of administration had different antitussive effects because of the primary sites of action. Remifentanil (a μ-opioid receptor activator) indirectly elicits cough-suppressive effects via opioids, which act to suppress sensory nerve activity [23, 24] because μ-opioid receptor activators inhibit calcium currents [25]; however, the stimulation of the tracheal mucosa in contact with the cuff is not reduced. The cough-suppressive effect of lidocaine topical anaesthesia is peripherally mediated, not centrally mediated, because the plasma concentrations (peak serum levels < 1.63 μg/mL) of lidocaine topical anaesthesia do not reach the level needed for cough-suppressive effects (> 3 μg/mL) [13, 20, 26]. The method of lidocaine administration in this study, which used a topical approach, could possibly explain the high efficiency of lidocaine compared with remifentanil. In this study, topical lidocaine adequately and directly reduced the stimulation of the tracheal mucosa in contact with the cuff without restricting the timing of administration or deflating the internal cuff.
In addition, lidocaine resulted in better recovery after respiratory complications and a shorter duration of PACU stay. In contrast, remifentanil increased the occurrence of hypoxemia (57.14%) at T3, the spontaneous respiration recovery time, and the extubation time. This is consistent with Beloeil's study [27], which reported hypoxemia in 61% of the patients treated with remifentanil. Compared with remifentanil, the lower respiratory complications observed in patients treated with lidocaine in this study could be because they were remifentanil-free during recovery from general anaesthesia.
Compared to remifentanil, intravenous (IV) lidocaine increased residual sedation [16]. The lidocaine serum concentration was greater than 3 μg/ml with the administration of 2 mg/kg IV lidocaine [28]. However, a 2 mg/kg dose of 4% lidocaine via topical distribution was used by Diachun [13] before extubation, which resulted in peak serum levels < 1.633 μg/ml. The lidocaine doses in this study were lower than those used in Lee et al.'s study [16], which may explain why the lidocaine used in this study did not increase residual sedation relative to TCI remifentanil.
Limitations and generalisability
This study had several limitations. First, only women were included in the study because women have a higher incidence of thyroid cancer [29], and the incidence of cough shows significant sex differences [30]. Second, an internal cuff carries the risk of air leakage. Thus, the internal cuff must be checked for leakage prior to intubation. Third, the injection of lidocaine, saline solution, or 20 ml of air via the outer cuff could induce cough. A sufficient anaesthesia depth minimises the risk of effect-site TCI remifentanil (2.0 ng/ml) and sevoflurane (1.4–1.5%). Fourth, NIM tubes are fairly standard practice elsewhere, which may make this new modified dual-cuff ETT less useful in clinical practice for certain patients undergoing thyroidectomy. However, cough during recovery was chosen as the primary outcome for further study of the potential benefits of the dual-cuff ETT, such as reducing airborne material and droplets during the recovery of patients with suspected or confirmed COVID-19 [7] or other cough-related adverse events.
Conclusion
In conclusion, lidocaine administered via the perforated outer cuff of the ETT significantly improved recovery from general anaesthesia compared with remifentanil in female patients after thyroidectomy.
Supplementary Information
Additional file 1: Supplemental Figure 1. DISPOSABLE REINFORCED TRACHEAL INTUBATION DOUBLE BALLOON DOSING-TYPE. A dual-cuff ETT contains a white internal cuff covered by a blue outer cuff. Two small-bore channels incorporated within the wall of the endotracheal tube are the channels that deliver air to the cuffs.
Additional file 2: Supplemental Figure 2. Dyed areas (red areas) with different dye liquid volumes and numbers of holes (A). The experiment was performed in triplicate for each combination. Graph paper (25 mm2 per unit) represents the area of the simulative trachea in contact with the perforated outer cuff of the dual-cuff endotracheal tube. The optimal scheme to achieve the even distribution of dye liquid around the endotracheal tube cuff was 16 holes and 4 ml of dye liquid. #P < 0.05 vs. 4 ml of dye liquid volume. &P < 0.05 vs. 8 holes. The structure of a modified dual-cuff endotracheal tube (B). This modified dual-cuff endotracheal tube contains an internal cuff covered by an outer cuff. The function of the internal cuff (black cuff) is the same as that of the single cuff in traditional endotracheal tubes. The small-bore channel incorporated within the wall of the endotracheal tube is the channel that delivers lidocaine to the outer cuff (green area). The outer cuff contains 16 small holes (each hole was 1 mm in diameter), which are evenly arranged in two rows (8 holes per row). The first row of holes (red area) and the second row of holes (blue area) are arranged at one-third and two-thirds of the outer cuff contacted internal cuff (the number represents the distribution of small holes in the outer cuff), respectively. Topical lidocaine is administered via small holes in the perforated outer cuff.
Additional file 3: Supplemental Video 1. The process of the perforated outer cuff.
Additional file 4: Supplemental Video 2. One patient was intubated with the dual-cuff ETT while sitting up in bed and signing her name.
Additional file 5: Supplemental Video 3. Lidocaine pass through the perforated outer cuff.
Acknowledgements
The authors gratefully thank Ai-hua Ou (Department of Big Data of Chinese Medicine research team) for critically reviewing the statistical analysis and Jian-chun Wang and Hong-guo Lin (Department of Vascular Thyroid Surgery) for performing the surgeries. The authors also thank the nurses Zhen-hua Han, Jing-yun Fan, Jing Wang, and Ding Ding (Department of Anesthesiology) for recording data for the variables. All departments were affiliated with Guangdong Provincial Hospital of Chinese Medicine.
Abbreviations
- ETT
Endotracheal tube
- OD
Odds ratio
- CI
Confidence interval
- COVID-19
Coronavirus disease
- TCI
Target-controlled infusion
- ASA
American Society of Anesthesiologists
- R
Remifentanil
- L
Lidocaine
- Ce
Effect-site concentration
- PACU
Post-anaesthesia care unit
- MAP
Mean arterial pressure
- HR
Heart rate
- ETCO2
End-tidal carbon dioxide
- RASS
Richmond Agitation-Sedation Scale
- CPOT
Critical-Care Pain Observation Tool
- SGS
Sedation Grading System
- LITA
Laryngotracheal instillation of topical anaesthesia
- IV
Intravenous
Authors’ contributions
PL and DL helped to design the study, conduct the study, analyse the data and approved the final manuscript. LW helped design and conduct the study. FY, SF, and ZT helped conduct the study. BY, LY, YS, XL and QY helped design the study. GZ helped design the study, analyse the data, write the final manuscript and handle this manuscript. The author(s) read and approved the final manuscript.
Funding
Support was provided solely by the Youth Talent Project of Guangdong Provincial Hospital of Chinese Medicine (Grant Number ZY2022YL13).
Availability of data and materials
The data used and analysed in this study are available from the corresponding author.
Declarations
Ethics approval and consent to participate
Ethical approval for this study (Ethical Committee IRB: ZF2020-130.2–01) was provided by the Ethical Committee of Guangdong Provincial Hospital of Chinese Medicine, Guangzhou City, Guangdong Province, People’s Republic of China (Chairperson Prof. Jun Liu) on 28/08/2020. Written informed consent was obtained from each patient before study participation. The full trial protocol was registered before patient enrolment in the Chinese Clinical Trial Registry (ref: ChiCTR2000038653) on 27/09/2020 and adheres to the Consolidated Standards of Reporting Trials guidelines [11] and the Declaration of Helsinki.
Consent for publication
Written informed consent was obtained from the participants for publication of the videos.
Competing interests
The authors declare no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kim ES, Bishop MJ. Cough during emergence from isoflurane anesthesia. Anesth Analg. 1998;87(5):1170–1174. doi: 10.1213/00000539-199811000-00036. [DOI] [PubMed] [Google Scholar]
- 2.Aouad MT, Al-Alami AA, Nasr VG, Souki FG, Zbeidy RA, Siddik-Sayyid SM. The effect of low-dose remifentanil on responses to the endotracheal tube during emergence from general anesthesia. Anesth Analg. 2009;108(4):1157–1160. doi: 10.1213/ane.0b013e31819b03d8. [DOI] [PubMed] [Google Scholar]
- 3.Leech P, Barker J, Fitch W. Proceedings: Changes in intracranial pressure and systemic arterial pressure during the termination of anaesthesia. Br J Anaesth. 1974;46(4):315–316. doi: 10.1093/bja/46.4.315-a. [DOI] [PubMed] [Google Scholar]
- 4.Bidwai AV, Bidwai VA, Rogers CR, Stanley TH. Blood-pressure and pulse-rate responses to endotracheal extubation with and without prior injection of lidocaine. Anesthesiology. 1979;51(2):171–173. doi: 10.1097/00000542-197908000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Fields A, Huang J, Schroeder D, Sprung J, Weingarten T. Agitation in adults in the post-anaesthesia care unit after general anaesthesia. Br J Anaesth. 2018;121(5):1052–1058. doi: 10.1016/j.bja.2018.07.017. [DOI] [PubMed] [Google Scholar]
- 6.Irwin RS. Complications of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 Suppl):54s–58s. doi: 10.1378/chest.129.1_suppl.54S. [DOI] [PubMed] [Google Scholar]
- 7.Chen X, Liu Y, Gong Y, Guo X, Zuo M, Li J, Shi W, Li H, Xu X, Mi W, et al. Perioperative management of patients infected with the novel coronavirus: recommendation from the joint task force of the chinese society of anesthesiology and the chinese association of anesthesiologists. Anesthesiology. 2020;132(6):1307–1316. doi: 10.1097/ALN.0000000000003301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosenbaum MA, Haridas M, McHenry CR. Life-threatening neck hematoma complicating thyroid and parathyroid surgery. Am J Surg. 2008;195(3):339–343. doi: 10.1016/j.amjsurg.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 9.Leone M, Rousseau S, Avidan M, Delmas A, Viviand X, Guyot L, Martin C. Target concentrations of remifentanil with propofol to blunt coughing during intubation, cuff inflation, and tracheal suctioning. Br J Anaesth. 2004;93(5):660–663. doi: 10.1093/bja/aeh250. [DOI] [PubMed] [Google Scholar]
- 10.Nho JS, Lee SY, Kang JM, Kim MC, Choi YK, Shin OY, Kim DS, Kwon MI. Effects of maintaining a remifentanil infusion on the recovery profiles during emergence from anaesthesia and tracheal extubation. Br J Anaesth. 2009;103(6):817–821. doi: 10.1093/bja/aep307. [DOI] [PubMed] [Google Scholar]
- 11.Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8:18. doi: 10.1186/1741-7015-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karmali S, Rose P. Tracheal tube size in adults undergoing elective surgery - a narrative review. Anaesthesia. 2020;75(11):1529–1539. doi: 10.1111/anae.15041. [DOI] [PubMed] [Google Scholar]
- 13.Diachun CA, Tunink BP, Brock-Utne JG. Suppression of cough during emergence from general anesthesia: laryngotracheal lidocaine through a modified endotracheal tube. J Clin Anesth. 2001;13(6):447–451. doi: 10.1016/S0952-8180(01)00299-9. [DOI] [PubMed] [Google Scholar]
- 14.Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O'Neal PV, Keane KA, Tesoro EP, Elswick RK. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166(10):1338–1344. doi: 10.1164/rccm.2107138. [DOI] [PubMed] [Google Scholar]
- 15.Gélinas C, Arbour C, Michaud C, Vaillant F, Desjardins S. Implementation of the critical-care pain observation tool on pain assessment/management nursing practices in an intensive care unit with nonverbal critically ill adults: a before and after study. Int J Nurs Stud. 2011;48(12):1495–1504. doi: 10.1016/j.ijnurstu.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 16.Lee JH, Koo BN, Jeong JJ, Kim HS, Lee JR. Differential effects of lidocaine and remifentanil on response to the tracheal tube during emergence from general anaesthesia. Br J Anaesth. 2011;106(3):410–415. doi: 10.1093/bja/aeq396. [DOI] [PubMed] [Google Scholar]
- 17.Lee B, Lee JR, Na S. Targeting smooth emergence: the effect site concentration of remifentanil for preventing cough during emergence during propofol-remifentanil anaesthesia for thyroid surgery. Br J Anaesth. 2009;102(6):775–778. doi: 10.1093/bja/aep090. [DOI] [PubMed] [Google Scholar]
- 18.Minogue SC, Ralph J, Lampa MJ. Laryngotracheal topicalization with lidocaine before intubation decreases the incidence of coughing on emergence from general anesthesia. Anesth Analg. 2004;99(4):1253–1257. doi: 10.1213/01.ANE.0000132779.27085.52. [DOI] [PubMed] [Google Scholar]
- 19.Tung A, Fergusson NA, Ng N, Hu V, Dormuth C, Griesdale DEG. Medications to reduce emergence coughing after general anaesthesia with tracheal intubation: a systematic review and network meta-analysis. British J Anaesthesia. 2020;124(4):480–495. doi: 10.1016/j.bja.2019.12.041. [DOI] [PubMed] [Google Scholar]
- 20.Minogue SC, Ralph J, Lampa MJ. Laryngotracheal topicalization with lidocaine before intubation decreases the incidence of coughing on emergence from general anesthesia. Anesthesia and analgesia. 2004;99(4):1253–1257. doi: 10.1213/01.ANE.0000132779.27085.52. [DOI] [PubMed] [Google Scholar]
- 21.Nath P, Williams S, Herrera Méndez LF, Massicotte N, Girard F, Ruel M. Alkalinized lidocaine preloaded endotracheal tube cuffs reduce emergence cough after brief surgery: a prospective randomized trial. Anesth Analg. 2018;126(2):615–620. doi: 10.1213/ANE.0000000000002647. [DOI] [PubMed] [Google Scholar]
- 22.Gonzalez RM, Bjerke RJ, Drobycki T, Stapelfeldt WH, Green JM, Janowitz MJ, Clark M. Prevention of endotracheal tube-induced coughing during emergence from general anesthesia. Anesth Analg. 1994;79(4):792–795. doi: 10.1213/00000539-199410000-00030. [DOI] [PubMed] [Google Scholar]
- 23.Mazzone SB, Undem BJ. Cough sensors. V. Pharmacological modulation of cough sensors. Handbook of Experiment Pharmacol. 2009;187:99–127. doi: 10.1007/978-3-540-79842-2_6. [DOI] [PubMed] [Google Scholar]
- 24.Takahama K, Shirasaki T. Central and peripheral mechanisms of narcotic antitussives: codeine-sensitive and -resistant coughs. Cough (London, England) 2007;3:8. doi: 10.1186/1745-9974-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hamra M, McNeil RS, Runciman M, Kunze DL. Opioid modulation of calcium current in cultured sensory neurons: mu-modulation of baroreceptor input. Am J Physiol. 1999;277(2):H705–713. doi: 10.1152/ajpheart.1999.277.2.H705. [DOI] [PubMed] [Google Scholar]
- 26.Nishino T, Hiraga K, Sugimori K. Effects of i.v. lignocaine on airway reflexes elicited by irritation of the tracheal mucosa in humans anaesthetized with enflurane. British journal of anaesthesia. 1990;64(6):682–687. doi: 10.1093/bja/64.6.682. [DOI] [PubMed] [Google Scholar]
- 27.Beloeil H, Garot M, Lebuffe G, Gerbaud A, Bila J, Cuvillon P, Dubout E, Oger S, Nadaud J, Becret A, et al. Balanced opioid-free anesthesia with dexmedetomidine versus balanced anesthesia with remifentanil for major or intermediate noncardiac surgery. Anesthesiology. 2021;134(4):541–551. doi: 10.1097/ALN.0000000000003725. [DOI] [PubMed] [Google Scholar]
- 28.Yukioka H, Yoshimoto N, Nishimura K, Fujimori M. Intravenous lidocaine as a suppressant of coughing during tracheal intubation. Anesth Analg. 1985;64(12):1189–1192. doi: 10.1213/00000539-198512000-00010. [DOI] [PubMed] [Google Scholar]
- 29.Cook MB, Dawsey SM, Freedman ND, Inskip PD, Wichner SM, Quraishi SM, Devesa SS, McGlynn KA. Sex disparities in cancer incidence by period and age. Cancer Epidemiology, Biomarkers & Prevention. 2009;18(4):1174–1182. doi: 10.1158/1055-9965.EPI-08-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tercan E, Kotanoglu MS, Yildiz K, Dogru K, Boyaci A. Comparison of recovery properties of desflurane and sevoflurane according to gender differences. Acta Anaesthesiol Scand. 2005;49(2):243–247. doi: 10.1111/j.1399-6576.2004.00559.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplemental Figure 1. DISPOSABLE REINFORCED TRACHEAL INTUBATION DOUBLE BALLOON DOSING-TYPE. A dual-cuff ETT contains a white internal cuff covered by a blue outer cuff. Two small-bore channels incorporated within the wall of the endotracheal tube are the channels that deliver air to the cuffs.
Additional file 2: Supplemental Figure 2. Dyed areas (red areas) with different dye liquid volumes and numbers of holes (A). The experiment was performed in triplicate for each combination. Graph paper (25 mm2 per unit) represents the area of the simulative trachea in contact with the perforated outer cuff of the dual-cuff endotracheal tube. The optimal scheme to achieve the even distribution of dye liquid around the endotracheal tube cuff was 16 holes and 4 ml of dye liquid. #P < 0.05 vs. 4 ml of dye liquid volume. &P < 0.05 vs. 8 holes. The structure of a modified dual-cuff endotracheal tube (B). This modified dual-cuff endotracheal tube contains an internal cuff covered by an outer cuff. The function of the internal cuff (black cuff) is the same as that of the single cuff in traditional endotracheal tubes. The small-bore channel incorporated within the wall of the endotracheal tube is the channel that delivers lidocaine to the outer cuff (green area). The outer cuff contains 16 small holes (each hole was 1 mm in diameter), which are evenly arranged in two rows (8 holes per row). The first row of holes (red area) and the second row of holes (blue area) are arranged at one-third and two-thirds of the outer cuff contacted internal cuff (the number represents the distribution of small holes in the outer cuff), respectively. Topical lidocaine is administered via small holes in the perforated outer cuff.
Additional file 3: Supplemental Video 1. The process of the perforated outer cuff.
Additional file 4: Supplemental Video 2. One patient was intubated with the dual-cuff ETT while sitting up in bed and signing her name.
Additional file 5: Supplemental Video 3. Lidocaine pass through the perforated outer cuff.
Data Availability Statement
The data used and analysed in this study are available from the corresponding author.