Summary
Background
Non-optimal temperatures are associated with mortality risk, yet the heterogeneity of temperature-attributable mortality burden across subnational regions in a country was rarely investigated. We estimated the mortality burden related to non-optimal temperatures across all provinces in China in 2019.
Methods
The global daily temperature data were obtained from the ERA5 reanalysis dataset. The daily mortality data and exposure–response curves between daily temperature and mortality for 176 individual causes of death were obtained from the Global Burden of Disease Study 2019 (GBD 2019). We estimated the population attributable fraction (PAF) based on the exposure-response curves, daily gridded temperature, and population. We calculated the cause- and province-specific mortality burden based on PAF and disease burden data from the GBD 2019.
Findings
We estimated that 593·9 (95% UI:498·8, 704·6) thousand deaths were attributable to non-optimal temperatures in China in 2019 (PAF=5·58% [4·93%, 6·28%]), with 580·8 (485·7, 690·1) thousand cold-related deaths and 13·9 (7·7, 23·2) thousand heat-related deaths. The majority of temperature-related deaths were from cardiovascular diseases (399·7 [322·8, 490·4] thousand) and chronic respiratory diseases (177·4 [141·4, 222·3] thousand). The mortality burdens were observed significantly spatial heterogeneity for both high and low temperatures. For instance, the age-standardized death rates (per 100 000) attributable to low temperature were higher in Western China, with the highest in Tibet (113·7 [82·0, 155·5]), while for high temperature, they were greater in Xinjiang (1·8 [0·7, 3·3]) and Central-Southern China such as Hainan (2·5 [0·9, 5·4]). We also observed considerable geographical variation in the temperature-related mortality burden by causes of death at provincial level.
Interpretation
A substantial mortality burden was attributable to non-optimal temperatures across China, and cold effects dominated the total mortality burden in all provinces. Both cold- and heat-related mortality burden showed significantly spatial variations across China.
Funding
National Key Research and Development Program.
Keywords: Non-optimal temperatures, Mortality Burden, China
Research in context.
Evidence before this study
Many studies have estimated the exposure-response associations between ambient temperatures and mortality across the world. However, few studies have quantified the mortality burden attributable to non-optimal temperatures across subnational regions in a country. We searched PubMed, Scopus, Web of Science, and Google Scholar using the combination of key words including “temperature”, “disease burden”, “mortality”, “mortality burden”, “death”, “excess death”, and “attributable” for studies published in English between database inception and November 15, 2021. Most previous studies estimated the temperature-related mortality burden within a single or several cities, or at country level. One study estimated the global, regional, and national mortality burden attributable to non-optimal temperatures from 2000 to 2019. However, no study has estimated the mortality burden attributable to both high and low ambient temperatures at province level in a country.
Added value of this study
This is the first study to estimate the mortality burden attributable to both high and low temperature at province level in China using the comparable Global Burden of Disease Study framework. Our estimations were based on a national dataset and a continuous surface of high-resolution temperature data, and hence covered both urban and rural populations across China. Moreover, this study estimated the temperature-related mortality burden for a diverse set of causes instead of all-cause mortality burden that was estimated in most previous studies. Our findings provided a clear geographical picture in the mortality burden attributable to non-optimal temperatures across China, which could help subnational governments to develop tailored intervention plans.
Implications of all the available evidence
This study provides a comprehensive picture of the mortality burden attributable to non-optimal temperatures at provincial level across China, which could extend our understanding of the health impacts of temperatures and assist adaptation policy making to reduce the mortality burden caused by non-optimal temperatures. The findings of disparate geographical patterns of temperature-related mortality burden suggest geographically specific adaptation actions need to be strengthened to protect human health from non-optimal temperature exposures.
Alt-text: Unlabelled box
Introduction
Many epidemiological studies have estimated the exposure-response associations between ambient temperatures and mortality globally.1, 2, 3, 4, 5, 6, 7 Most studies have found U- or J-shaped associations between temperature and mortality risks from cardiovascular, respiratory, cerebrovascular, and other causes.2,5,6 Both low and high temperatures may increase the risk of mortality, and low temperature has a greater overall effect on mortality than does high temperature. In addition, the magnitude of associations between temperature and mortality is substantially varied between regions and countries.2,5,6
Although temperature-mortality associations have been increasingly assessed, few studies have quantified the mortality burden attributable to non-optimal temperatures at a subnational level in a country.5,8, 9, 10 The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019 reported that non-optimal temperature was one of the ten leading causes of death worldwide.11 Mortality burden attributable to high and low temperatures was estimated for 204 countries/territories from 1990 to 2019.12 A total of 1·69 million deaths were attributable to non-optimal temperature globally in 2019, and temperature-related deaths were about 0·5 million in China.12 Given China's large population and land area, and its wide heterogeneity in climate, socioeconomic development and health, there may be spatial heterogeneity in temperature-attributable mortality across provinces in the country. However, to our knowledge, no previous study has estimated the mortality burden attributable to temperatures at provincial level across China. Therefore, to prioritize region-targeted interventions, it is necessary to comprehensively assess mortality burden of non-optimal temperature for all provinces in China, including subnational variation in deaths from important causes due to both high and low temperatures.
In the current study, we used GBD 2019 data to assess the impact of ambient temperature on mortality burden in China and its provinces in 2019. This was the first study on mortality burden attributable to non-optimal temperatures at provincial level across China. Our findings are informative to make climate adaptation strategies and measures to address both high and low temperature exposures in China and its provinces.
Method
Overview
The analyses on the mortality burden related to non-optimal temperature in China and its provinces were a part of GBD 2019. This study included 31 provinces, autonomous regions, and municipalities, and two special administrative regions (Hong Kong and Macao) across China. The detailed information of exposures, outcome metrics, data collection and statistical modelling on GBD 2019 have been reported in previous articles.11, 12, 13
Assessment of exposure-response association between temperature and mortality
The global exposure-response associations between daily temperature and mortality for 176 individual causes of death were obtained from the GBD 2019.11 Briefly, the GBD 2019 study collected daily cause-specific mortality data from eight countries (Brazil, Chile, China, Colombia, Guatemala, Mexico, New Zealand, and the USA), where individual death information on International Classification of Diseases (ICD) code, administrative unit, and day was available. A total of 58·9 million deaths spanning from January 1st 1980 to December 31 2016 were included in the analyses (table S1 in appendix pp 6). Meanwhile, the global daily temperature data between January 1st 1980 and December 31st 2019 were derived from the ERA5 reanalysis, produced by the European Centre for Medium Range Weather Forecasts (ECMWF) with 0·25° × 0·25° (∼30 × 30 km) spatial and hourly temporal resolutions. For each pixel globally, the average of all 24-hour temperature estimates within a day was calculated as the daily mean temperature. Then the annual mean temperatures of all pixels during 1980-2019 were calculated, and it turned out that the annual mean temperatures ranged from 6°C to 28°C. Therefore, all pixels were divided into 23 temperature zones based on the annual mean temperatures. Change of each 1°C represents one temperature zone (e.g., zone 6°C, zone 7°C, zone 8°C, etc.)
For each individual death, we determined the temperature zone and daily temperature corresponding to the date and location of the death. To reduce noise and volatility associated with sparse data at extreme temperatures, temperature zones were truncated to the 1st and 99th percentiles of those in the dataset; and daily mean temperatures were also truncated to the 1st and 99th percentiles within each temperature zone. The cause-specific mortality rates (CSMR) were computed for each cause of death, and for each combination of level 2 location (county or district), temperature zone, and daily temperature. The reference mortality rate for each cause in each county/district was also calculated as the mean CSMR for that cause in that location across all daily mean temperatures. Then, the relative risk (RR) for each cause in each county/district at a given daily mean temperature was calculated as the ratio between cause-specific mortality rate and reference mortality rate. The RR reflects the association of temperature exposure on the same day of death, but does not adjust for lagged effect and seasonality (appendix pp 3).
A robust meta-regression framework (Bayesian, regularized, trimmed tool), MR-BRT, was applied to estimate the exposure-response curves between daily mean temperatures and mortality in each temperature zone.14 This tool could integrate heterogeneous data from different locations into one model to achieve stable estimations of curves. For those J- or U-shaped curves, the curves were constrained to follow a convex shape. For the one-directional curves (e.g., all external causes), monotonicity over the entire temperature range was imposed (appendix pp 3). Finally, the summarized exposure-response curves between daily mean temperatures and mortality for all included causes were obtained for each temperature zone.11 For each temperature zone, the theoretical minimum-risk exposure level (TMREL) across all included causes was estimated. The TMREL was defined as the location-specific daily mean temperature which has the lowest mortality rates for all included causes combined. Temperatures above the TMREL are defined as high temperatures, and temperatures below the TMREL are defined as low temperatures. The sum of high and low temperatures was defined as non-optimal temperatures (appendix pp 3-4).
Cause selection
The causes of mortality were selected based on a list of causes in the GBD cause hierarchy (n=176). We excluded all causes without mortality record in the dataset, with fewer than 100 000 deaths, and causes of death that did not represent a particular entity but rather a summary category. Two more causes, dementia and protein-energy malnutrition, were excluded because of the known inconsistencies in classification practice across countries.11 The remaining causes were selected based on statistical significance. For each cause and each mean temperature zone we determined the widest range of consecutive daily temperatures with statistically significant relative risks, expressed as a percentage of the full range of daily temperatures in that mean temperature zone. We included all causes where at least 30% of zones had a consecutive significance range that spanned at least 5% of the full range of daily temperatures (detailed information in appendix pp 4). Twelve causes met these criteria and were finally included: ischaemic heart disease, stroke, hypertensive heart disease, diabetes, chronic kidney disease, lower respiratory infection, chronic obstructive pulmonary disease, homicide, suicide, mechanical injuries, road injuries, and drowning.11
Estimation of deaths attributable to non-optimal temperatures across China
The estimation of deaths attributable to non-optimal temperatures was based on the comparative risk assessment metric (CRA) framework,15 which includes four inputs: temperature exposures, exposure-response curves between temperature and cause-specific mortality, TMREL, and the total burden estimate for each cause. Daily temperature data across China in 2019 were also obtained from the ERA5, and all pixels were aggregated into temperature zones based on the annual mean temperatures. In each temperature zone, the TMREL and exposure-response associations between temperature and mortality were obtained from the GBD 2019, as described above. The cause-specific burden at provincial level in China was also obtained from the GBD 2019.13
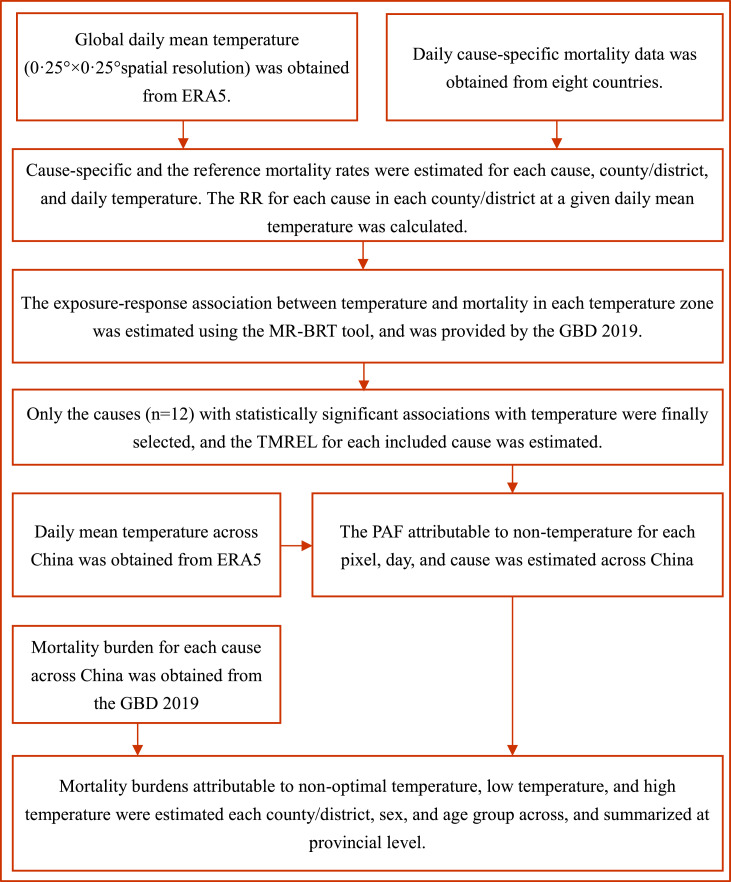
We estimated the population attributable fraction (PAF) for each pixel and day, based on the RRs of daily mean temperatures within a given temperature zone. The PAFs for low and high temperatures below and above the TMREL were estimated, respectively. The PAF for non-optimal temperature was obtained by aggregating the low and high temperature PAFs. Using the cause specific burden in China,13 we calculated the non-optimal temperature related burden for each cause as the product of the cause-specific PAF and the total burden for that cause for each location, sex, and age group (appendix pp 4-5). We also estimated the uncertainty of burden using a posterior simulation. We applied 1000 random draws from the posterior distribution and estimated the 95% uncertainty intervals (95% UI). Finally, based on the PAFs and GBD 2019 burden data, we calculated the number of deaths, death rate, and age-standardized death rate for each cause, province, and nationally. Methods of calculating the GBD 2019 burden data has been described in detail elsewhere,13 and are summarized in Figure 1.
Figure 1.
Process of estimation on mortality burden attributable to non-optimal temperature in China and its provinces, 2019.
GBD 2019: the Global Burden of Disease Study 2019.
MR-BRT: Robust meta-regression framework (Bayesian, regularized, trimmed tool).
TMREL: Theoretical minimum-risk exposure level.
PAF: Population attributable fraction.
In above analyses, RRs were calculated in R and Python, PAFs and TMRELs were calculated in R, and burden of disease was calculated in Python.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
In 2019, the average annual temperature across China was 7·0 (standard deviation [SD]: 8·8) °C (Figure S3 in appendix pp 7), and the daily mean temperatures ranged from -39·8°C to 40·0°C. All studied counties or districts were divided into 23 temperature zones based on the average annual temperatures.
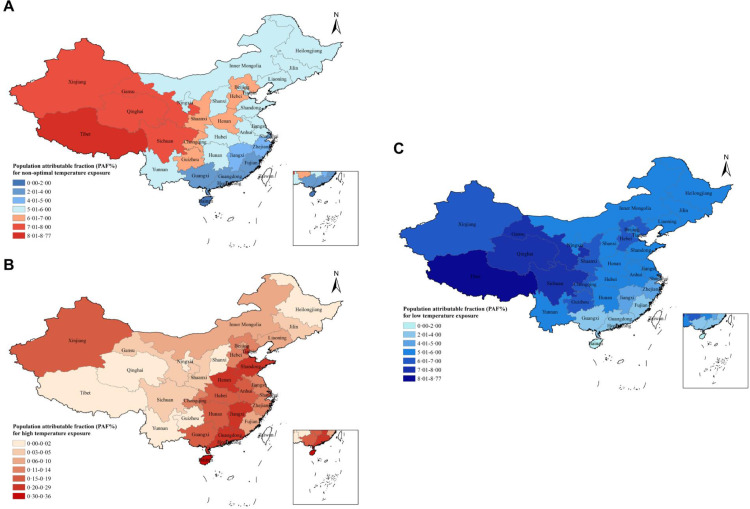
Figure 2 shows the spatial distribution of PAFs for temperatures across China. The national PAFs of non-optimal, low and high temperatures were 5·58% (95% UI: 4·93%, 6·28%), 5·45% (4·80%, 6·18%) and 0·13% (0·07%, 0·21%), respectively. The PAFs of non-optimal temperatures were higher in Western China with the highest in Tibet (8.77% [6.25%, 11.83%]), and lower in Southern China with the lowest in Hainan (1.11% [0.77%, 1.55%]). The distribution of PAF for low temperature was similar to the PAFs of non-optimal temperatures. The PAFs of high temperatures were higher in Central-Southern China and Xinjiang than other regions. The highest PAF for high temperature was found in Hong Kong (0·36%, [0·05%, 1·00%]), and the lowest PAF was found in Tibet (0%) (Table S2 in appendix pp 8). The cause-specific PAFs of temperatures are shown in Table S3 (appendix pp 9). We observed greater PAFs of non-optimal temperatures for chronic obstructive pulmonary disease (COPD) (17·10%, [14·76%, 19·98%]) and lower respiratory infections (12·78%, [8·58%, 16·58%]) than other causes such as drowning (-26·50%, [-30·89%, -22·15%]) and mechanical injuries (-12·94%, [-16·94%, -9·07%]). In particular, the PAFs of low temperature were greater for COPD (16·91%, [14·49%, 19·86%]) and lower respiratory infections (12·04% [7·75%, 15·87%]), while the PAFs of high temperature were larger for drowning (1·46%, [0·95%, 2·59%]).
Figure 2.
PAF of death attributable to non-optimal temperature (A), high-temperature (B), and low-temperature (C) exposures in different provinces in China, 2019.
We estimated that 593·9 (95% UI: 498·8, 704·6) thousand deaths were attributable to non-optimal temperatures in 2019 in China, including 580·8 (485·7, 690·1) thousand cold-related deaths and 13·9 (7·7, 23·2) thousand heat-related deaths. The overall death rates attributable to non-optimal, high and low temperatures at nationwide were 41·8 (35·1, 49·5), 1·0 (0·5, 1·6), and 40·8 (34·1,48·5) per 100 000 population, respectively (Table 1).
Table 1.
Death and death rate attributable to non-optimal temperatures, high temperatures, and low temperatures in China, 2019.
| Non-optimal temperature |
High temperature |
Low temperature |
||||
|---|---|---|---|---|---|---|
| Deaths (thousand, 95%UI) | Death rate (per 100 000, 95%UI) | Deaths (thousand, 95%UI) | Death rate (per 100 000, 95%UI) | Deaths (thousand, 95%UI) | Death rate (per 100 000, 95%UI) | |
| Causes of death | ||||||
| All causes | 593·9(498·8,704·6) | 41·8(35·1,49·5) | 13·9(7·7,23·2) | 1·0(0·5,1·6) | 580·8(485·7,690·1) | 40·8(34·1,48·5) |
| Communicable, maternal, neonatal, and nutritional diseases | 23·7(15·8,32·6) | 1·7(1·1,2·3) | 1·5(0·3,2·7) | 0·1(0·0,0·2) | 22·3(14·1,31·2) | 1·6(1·0,2·2) |
| Lower respiratory infections | 23·7(15·8,32·6) | 1·7(1·1,2·3) | 1·5(0·3,2·7) | 0·1(0·0,0·2) | 22·3(14·1,31·2) | 1·6(1·0,2·2) |
| Non-communicable diseases | 609·8(511·2,721·7) | 42·9(35·9,50·7) | 10·9(5·5,18·8) | 0·8(0·4,1·3) | 599·9(499·8,709·9) | 42·2(35·1,49·9) |
| Cardiovascular diseases | 399·7(322·8,490·4) | 28·1(22·7,34·5) | 7·8(2·7,15·8) | 0·5(0·2,1·1) | 392·4(314·4,484·4) | 27·6(22·1,34·1) |
| Ischemic heart disease | 151·6(107·9,200·5) | 10·7(7·6,14·1) | 4·9(0·9,9·4) | 0·3(0·1,0·7) | 147·0(101·2,197·4) | 10·3(7·1,13·9) |
| Stroke | 218·6(165·5,280·6) | 15·4(11·6,19·7) | 2·4(-2·0,10·3) | 0·2(-0·1,0·7) | 216·3(162·9,280·0) | 15·2(11·4,19·7) |
| Hypertensive heart disease | 29·5(15·6,41·2) | 2·1(1·1,2·9) | 0·4(-0·8,1·7) | 0·0(-0·1,0·1) | 29·1(15·5,40·9) | 2·0(1·1,2·9) |
| Chronic respiratory diseases | 177·4(141·4,222·3) | 12.5(9·9,15·6) | 2·3(-0·6,5·5) | 0·2(0·0,0·4) | 175·4(139·1,220·1) | 12·3(9·8,15·5) |
| Chronic obstructive pulmonary disease | 177·4(141·4,222·3) | 12·5(9·9,15·6) | 2·3(-0·6,5·5) | 0·2(0·0,0·4) | 175·4(139·1,220·1) | 12·3(9·8,15·5) |
| Diabetes mellitus | 16·4(8·8,24·4) | 1·2(0·6,1·7) | 0·6(-0·3,1·4) | 0·0(0·0,0·1) | 15·8(8·2,23·8) | 1·1(0·6,1·7) |
| Chronic kidney disease | 16·5(8·8, 24·3) | 1·2 (0·6, 1·7) | 0·3 (-0·7,1·1) | 0·0 (-0·1,0·1) | 16·2(8·5, 24·3) | 1·1(0·6,1·7) |
| Injuries | -39·6(-50·9,-29·8) | -2·8(-3·6,-2·1) | 1·5(0·9,2·9) | 0·1(0·1,0·2) | -41·4(-53·1,-31·3) | -2·9(-3·7,-2·2) |
| Transport injuries | -12·5(-19·9,-5·5) | -0·9(-1·4,-0·4) | 0·2(0·0,0·7) | 0·0(0·0,0·0) | -12·8(-20·2,-5·6) | -0·9(-1·4,-0·4) |
| Road injuries | -12·5(-19·9,-5·5) | -0·9(-1·4,-0·4) | 0·2(0·0,0·7) | 0·0(0·0,0·0) | -12·8(-20·2,-5·6) | -0·9(-1·4,-0·4) |
| Unintentional injuries | -18·7(-22·9,-14·6) | -1·3(-1·6,-1·0) | 0·9(0·6,1·6) | 0·1(0·0,0·1) | -19·8(-24·1,-15·6) | -1·4(-1·7,-1·1) |
| Drowning | -15·0(-18·2,-11·8) | -1·1(-1·3,-0·8) | 0·8(0·5,1·4) | 0·1(0·0,0·1) | -16·0(-19·3,-12·7) | -1·1(-1·4,-0·9) |
| Mechanical injuries | -3·7(-5·4,-2·1) | -0·3(-0·4,-0·1) | 0·1(0·0,0·2) | 0·0(0·0,0·0) | -3·8(-5·6,-2·1) | -0·3(-0·4,-0·2) |
| Suicide and homicide | -8·4(-12·9,-4·2) | -0·6(-0·9,-0·3) | 0·3(0·1,0·8) | 0·0(0·0,0·1) | -8·8(-13·4,-4·4) | -0·6(-0·9,-0·3) |
| Suicide | -7·7(-12·1,-3·7) | -0·5(-0·8,-0·3) | 0·3(0·1,0·7) | 0·0(0·0,0·0) | -8·0(-12·6,-3·9) | -0·6(-0·9,-0·3) |
| Homicide | -0·7(-1·1,-0·3) | 0·0(-0·1,0·0) | 0·0(0·0,0·1) | 0·0(0·0,0·0) | -0·7(-1·1,-0·3) | -0·1(-0·1,0·0) |
| Sex | ||||||
| Male | 327·6(261·7,397·7) | 45·2(36·1,54·9) | 7·9(4·2,12·8) | 1·1(0·6,1·8) | 320·2(256·0,389·6) | 44·2(35·3,53·7) |
| Female | 266·3(213·2,328·9) | 38·2(30·6,47·2) | 6·1(3·3,9·8) | 0·9(0·5,1·4) | 260·6(208·1,323·1) | 37·4(29·8,46·3) |
| Age (years) | ||||||
| 0-9 | -0·8(-1·9,0·0) | -0·3(-0·6,0·0) | 0·2(0·1,0·4) | 0·1(0·0,0·1) | -1·1(-2·1,-0·3) | -0·3(-0·7,-0·1) |
| 10-24 | -3·5(-4·5,-2·6) | -1·5(-2·0,-1·1) | 0·2(0·1,0·4) | 0·1(0·1,0·2) | -3·8(-4·8,-2·9) | -1·7(-2·1,-1·3) |
| 25-49 | 7·8(3·7,12·5) | 1·4(0·7,2·2) | 0·8(0·5,1·5) | 0·2(0·1,0·3) | 7·0(2·9,11·5) | 1·2(0·5,2·0) |
| 50-74 | 211·0(171·5,256·3) | 26·9(21·8,32·6) | 4·4(2·3,7·6) | 0·6(0·3,1·0) | 206·8(167·5,250·9) | 26·3(21·3,31·9) |
| ≥75 | 379·4(321·4,443·6) | 419·9(355·6,490·9) | 8·2(4·5,13·3) | 9·0(5·0,14·7) | 371·9(314·2,436·1) | 411·5(347·6,482·5) |
Most of the temperature-related deaths occurred in older people, particularly in people aged 75 years or older (379·4 [95% UI: 321·4, 443·6] thousand). Cardiovascular diseases (399·7 [322·8, 490·4] thousand) and chronic respiratory diseases (177·4 [141·4, 222·3] thousand) were the major contributors of temperature-related deaths. Stroke, COPD, ischemic heart disease, hypertensive heart disease, chronic kidney disease, and diabetes mellitus are top six specific causes of deaths attributable to non-optimal temperature, and similar patterns were found for cold- and heat-related deaths. The top three causes for cold-related deaths were stroke (216·3 [162·9, 280·0] thousand), COPD (175·4 [139·1, 220·1] thousand), and ischemic heart disease (147·0 [101·2, 197·4] thousand), while for heat-related deaths, they were ischemic heart disease (4·9 [0·9, 9·4] thousand), stroke (2·4 [-2·0, 10·3] thousand), and COPD (2·3 [-0·6, 5·5] thousand) (Table 1).
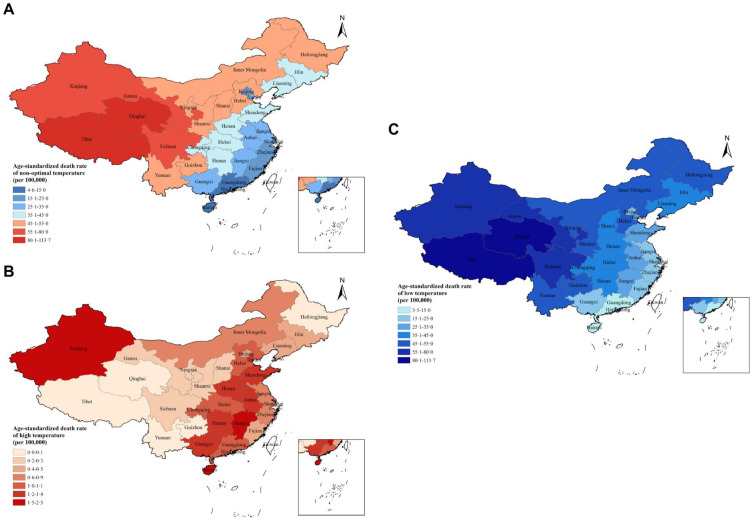
Figure 3 shows the spatial distribution of age-standardized death rate (per 100 000) attributable to temperatures across China. They were 36·0 (95% UI: 30·2, 42·5), 0·9 (0·5, 1·5), and 35·1 (29·4, 41·5) per 100 000 people for non-optimal, high, and low temperatures, respectively. Geographically, the age-standardized death rate attributable to non-optimal temperatures gradually decreased from Western China, with the highest rate in Tibet (113·7 [82·0, 155·5]), to Eastern China, with the lowest rate in Hong Kong (4·6 [2·6, 8·3]). For high temperature, they were higher in Xinjiang (1·8 [0·7, 3·3]) and Central-Southern China such as Hainan (2·5 [0·9, 5·4]) and Jiangxi (1·9 [0·8,3·2]), and lower in Western China and Northeast China, such as Tibet (0·0, [0·0, 0·0]), Qinghai (0·0, [0·0, 0·0]), and Heilongjiang (0·1 [0·0, 0·6]). By contrast, for low temperature, they were greater in Western China, such as Tibet (113·7 [82·0,155·5]) and Qinghai (88·4 [62·2,122·2]), and lower in Southern China, such as Hong Kong (3.5 [0·3, 7·7]), Macao (4·8 [0·4,10·2]), and Hainan (5·3 [2·3, 9·1]) (Table S4 in appendix pp 10).
Figure 3.
Age-standardized death rate (per 100 000) attributable to non-optimal temperature (A), high-temperature (B), and low-temperature (C) exposures in different provinces in China, 2019.
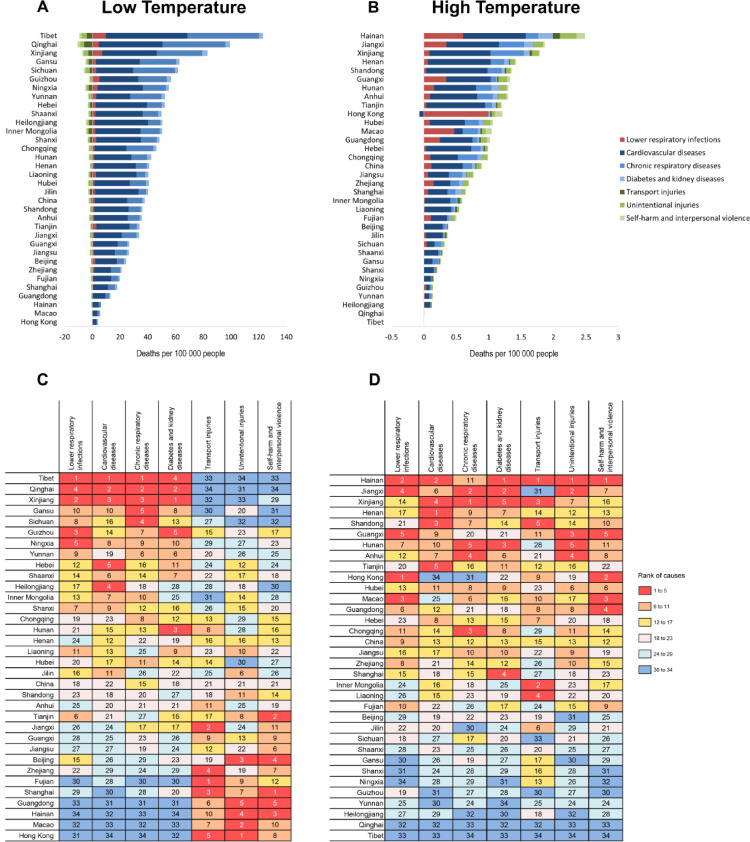
Figure 4 shows the spatial variation in the causes of deaths attributable to temperatures across China. In the age-standardized death rate attributable to low temperature, cardiovascular diseases, chronic respiratory diseases, diabetes and chronic kidney disease, and lower respiratory infections ranked the top in western provinces, and ranked the end in southern provinces, meanwhile injuries ranked the top in southern provinces and ranked the end in western provinces (Panels A and C). In the age-standardized death rate attributable to high temperature, all included causes of death ranked the top in central-southern provinces and in Xinjiang, and ranked the end in western provinces (Panels B and D). The crude death rates by causes attributable to temperatures are shown in Figure S4 (appendix pp 11).
Figure 4.
The age-standardized death rates (per 100 000 population) attributable to both low-temperature and high-temperature and their ranks by causes of death and province, 2019.
Panel A: Age-standardized death rates attributable to low-temperature.
Panel B: Age-standardized death rates attributable to high-temperature.
Panel C: The ranks of cause-specific age-standardized death rates attributable to low-temperature.
Panel D: The ranks of cause-specific age-standardized death rates attributable to high-temperature.
In Panels C and D, the number in each grid indicates the ranks of age-standardized death rates among provinces, and smaller number means the toper position in the ranks.
Discussion
Based on a comparative framework and a national dataset, this study assessed the mortality burden of non-optimal temperatures in China and its provinces. The results showed that there were 593·9 thousand deaths attributable to non-optimal temperatures across China in 2019. The majority of the burden was caused by low temperatures and cardiorespiratory diseases. Cold related mortality dominated in Western China while heat related mortality was prominent in Xinjiang and Central-Southern China.
Although numerous studies have estimated the exposure-response associations between non-optimal temperature and human health,2,5,8, 9, 10 few have translated the associations into the estimates of mortality burden. Zhao et al.8 applied a three-stage modeling to estimate the global mortality attributable to non-optimal temperatures, and reported that the excess death ratio attributable to non-optimal temperatures in Eastern Asia was 10·96% (80 excess deaths per 100 000 population). Gasparrini et al. reported in a multicounty study that the PAF attributable to non-optimal temperature was 11·00% in China.2 Those findings were higher than the present study (5·58% for non-optimal temperature), and this inconsistency may be due to several reasons. First, previous studies have applied all-cause mortality to estimate the burden of non-optimal temperatures.5,8 However, we only included causes which had statistically significant association with temperature. Some other causes which did not met our inclusion criteria, but potentially have significant associations with temperatures were excluded in our study. Second, our study applied a methodological approach which did not consider lagged effects and adjust for seasonality. We did not adjust for seasonality because of the strong correlation between ambient temperature and seasonality which may lead to potential collinearity and incomplete disentangling of these two factors.16 Additionally, although previous studies have found several weeks’ lag effects of low temperatures,5,9 we postulated that the long-time delayed effects might indeed be seasonal rather than a temperature effect.16 As a result, the burden of low temperatures estimated on the same day exposure may be underestimated in this study. Third, previous studies applied the data mainly from individual cities, whereas we relied on data with continuous spatial coverage including rural populations. One previous study has reported that people in more urbanized areas and higher population densities were more vulnerable to non-optimal temperatures.17
Our study found that most of mortality burden attributable to non-optimal temperatures was driven by low temperatures, which is consistent with previous studies.2,5,6,8,18,19 Chen et al. reported in a study including 272 main Chinese cities that the PAFs attributable to low and high temperatures were 11·62% and 2·71%, respectively. A multi-country study observed more mortality caused by low temperature (7·29%) than by high temperature (0·42%).2 National studies from India and Spain also reported higher attributable risks on mortality burden for low temperature than high temperature.6,19 The results suggest that the national and provincial governments need to develop better cold adaptation plans to reduce the mortality burden of low temperatures even in the context of global warming.
We observed a strong spatial variation in the temperature-related burden across China. The age-standardized death rate attributable to non-optimal temperatures was higher in Western China than in other regions in China, and so does for low temperature. For example, the age-standardized death rate attributable to non-optimal temperature in Tibet (113·7 per 100 000) was near 25 times that in Hong Kong (4·6 per 100 000). This geographical heterogeneity may be related to temperature exposures and disease prevalence in different provinces. Western China particularly the Qinghai-Tibet Plateau has much lower daily temperatures (appendix pp 7),20 and the temperature variation between day and night, indoor and outdoor was also larger than other regions,21,22 which could lead to more pronounced mortality risk. In addition, the disease prevalence was usually higher in western provinces.23,24 For example, the GBD 2017 study showed that the age standardized YLL rates of lower respiratory infection, ischemic heart disease, stroke, hypertensive heart disease, and COPD in Tibet, Xinjiang, and Qinghai were substantially higher than most other provinces in China.23 By contrast, the age-standardized death rate attributable to high temperature was higher in Central-Southern China and Xinjiang. The larger death rate in Central-Southern China may be mainly related to their higher daily temperatures (appendix pp 7). For example, the climate in Hainan is tropical, which has the highest annual mean temperature among all provinces in China. The higher death rate in Xinjiang may be related to both high temperature and disease burden.
Our findings have important implications for the national and provincial governments to identify major health problems related to ambient temperatures and help to tailor province-specific policy and intervention programs to protect populations from non-optimal temperatures. All provinces particularly for western provinces need to develop better cold weather plans (CWP) which was currently overlooked in most provinces across China. The CWP should be included in the national and regional strategies of climate change adaptation. Different levels of adaptation actions needed to be integrated into the CWP, including year-round planning, winter preparedness and action, cold spell forecast (alert and readiness), and emergency response.25 Local organizations and departments such as health and social care, weather, communities, and individuals, should be included in the CWP. For example, community- and individual-level cold vulnerability assessment could be implemented to identify the location of most vulnerable people, and specific interventions can be designed to protect them more efficiently and effectively.
Central-southern provinces should focus on reducing heat-related mortality burden. Although heat-health action plans (HAP) have been integrated into the national and regional strategies of climate change adaptation, intensified adaptation measures are needed in Central-southern provinces. First, the HAP should be developed and implemented among the most related agencies and the public. Second, different actions such as public advisories, risk information communication, intensified surveillance, and air-conditioned shelter opening should be taken depending on different alert levels of high temperature. Third, a sound and concrete risk communication and public education program are necessary to increase the awareness of high temperature, and transform the knowledge to behavior adaptation. Fourth, urban planning such as optimizing building design, building parks, and green spaces, could also assist in reducing vulnerability, establishing resilience and promoting health.26
We further found that the types and ranks of main health risks caused by non-optimal temperature largely varied among provinces, and each province should pay attention to their specific health risk. For example, western provinces like Tibet and Qinghai may take more actions to prevent deaths from cardiopulmonary diseases, diabetes, and kidney diseases in cold days. Meanwhile central-southern provinces like Hainan and Jiangxi need to take more intensified comprehensive measures to prevent deaths from cardiopulmonary diseases, diabetes, kidney diseases, and injuries in hot days. In particular, the mortality burden attributable to both high and low temperatures in Xinjiang ranked the top among all provinces in China. Therefore, comprehensive adaptation measures are needed to reduce both heat- and cold-related mortality burden in Xinjiang.
This study has several strengths. First, we applied a comparative framework to estimate the burden attributable to non-optimal temperatures in China based on a national dataset and a high-resolution (0·25° × 0·25°) of temperature data. The representativeness of data ensured the high quality of our findings at national level. Moreover, the national dataset with continuous spatial coverage included both urban and rural areas, which could provide more precise estimation of the mortality burden attributable to non-optimal temperatures at both national and provincial levels. Second, we applied a novel meta-regression tool, MR-BRT, to estimate the exposure-response associations between temperature and mortality by temperature zone. This tool was specifically developed for application within the GBD, ensuring internal consistency and comparability across risk factors. Third, this is the first study to estimate the mortality burden attributable to non-optimal temperatures at provincial levels in China. The study could help subnational governments to develop tailored intervention plans.
Several limitations should be acknowledged. First, due to the unavailability of data, our dataset did not include morbidity data, and therefore we did not estimate years lived with disability (YLDs) caused by non-temperature. We hope to extend our estimation to include non-fatal outcomes in future studies. Second, the methodological approach in this study did not consider the lagged and cumulative effects of temperatures, and did not adjust for long-term trend, day of week, air pollutants, and other meteorological factors such as humidity, which may limit the comparability and consistency of findings with other studies beyond the GBD framework. Third, the exposure-response associations between non-optimal temperatures and mortality were estimated based on a global mortality dataset from eight countries (including China), but was not specifically based on the province-specific mortality dataset or subpopulation dataset (e.g., urban-rural areas, sex or age groups) across China. The GBD 2019 framework assumed that the exposure-response associations were consistent across all pixels within the same temperature zone.12 Therefore, the heterogeneity of mortality burden between provinces cannot be accounted for by socioeconomic status, demographics, air conditioning usage, and development levels of infrastructure and public health services, which have been shown to impact the temperature-mortality associations even within similar climates.27, 28, 29 The temperature-related mortality burden in some provinces with greater temperature susceptibility might be underestimated, and in some provinces with less temperature susceptibility might be overestimated. However, we estimated the cause-specific temperature-mortality curve across 23 temperature zones. These exposure-response curves were applied to the underlying location and population specific burden to derive the temperature-attributable burden. While our exposure-response curves do not account for effect modifiers such as sex, age, rural-urban areas, the burden estimates to which we apply our exposure-response functions do. Fourth, only one-year mortality data were included from China. However, the number of death (6·1 million) was larger than many other countries such as New Zealand (0·76 million), Colombia (0·95 million), and Guatemala (0·49 million), and the global mortality dataset had 58·9 million deaths spanning from 1980 to 2016, which provided a robust global association between temperature and mortality. Fifth, the temperature exposure was assessed using the ambient temperature, but not based on the individual-level exposure, which may lead to misclassification bias of exposure because people usually spend more time indoors.30 These limitations suggest the need for continued focus on estimating the temperature related mortality burden in future GBD works.
In conclusion, a substantial mortality burden for a diverse set of causes of death is attributable to non-optimal temperatures in China. The mortality burden was dominated by low temperature and cardiorespiratory diseases at the national level or provincial level. Cold-related mortality dominated in Western China while heat-related mortality was prominent in Xinjiang and Central-Southern China. Our results provided valuable information for the public and policy makers to understand the mortality burden of non-optimal temperature. In the context of unequivocal climate change globally, we call for more decisive and coordinated actions to protect human health from non-optimal temperatures.
Contributors
J Liu and T Liu conducted the data analysis and wrote the first draft of the manuscript. K G Burkart participated in the data analyses and interpretation. M Zhou and W Ma conceived the original idea and provided input with data analyses and interpretation. All authors were involved in drafting and revising the manuscript.
Data sharing statement
To download GBD data used in the analyses in this article please visit the Global Health Data Exchange GBD 2019 website.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
Jeffrey D Stanaway reports grants from the Bill and Melinda Gates Foundation, during the conduct of the study. All other authors declare no competing interests.
Acknowledgments
This work was supported by the China National Key Research and Development Program (2018YFC1315300 and 2018YFA0606200), and National Natural Science Foundation of China (42075173 and 42175181).
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanwpc.2022.100493.
Contributor Information
Wenjun Ma, Email: mawj@gdiph.org.cn.
Maigeng Zhou, Email: zhoumaigeng@ncncd.chinacdc.cn.
Appendix. Supplementary materials
References
- 1.Watts N, Adger WN, Ayebkarlsson S, et al. The Lancet Countdown: tracking progress on health and climate change. Lancet. 2017;389:1151–1164. doi: 10.1016/S0140-6736(16)32124-9. [DOI] [PubMed] [Google Scholar]
- 2.Gasparrini A, Guo Y, Hashizume M, et al. Mortality risk attributable to high and low ambient temperature: A multicountry observational study. Lancet. 2015;386:369–375. doi: 10.1016/S0140-6736(14)62114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Medina-Ramón M, Schwartz J. Temperature, temperature extremes, and mortality: a study of acclimatisation and effect modification in 50 US cities. Occup Environ Med. 2007;64:827–833. doi: 10.1136/oem.2007.033175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ye X, Wolff R, Yu W, Vaneckova P, Pan X, Tong S. Ambient temperature and morbidity: a review of epidemiological evidence. Environ Health Perspect. 2012;120:19–28. doi: 10.1289/ehp.1003198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen R, Yin P, Wang L, et al. Association between ambient temperature and mortality risk and burden: time series study in 272 main Chinese cities. BMJ. 2018;363:k4306. doi: 10.1136/bmj.k4306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Achebak H, Devolder D, Ballester J. Trends in temperature-related age-specific and sex-specific mortality from cardiovascular diseases in Spain: a national time-series analysis. Lancet Planet Health. 2019;3:e297–e306. doi: 10.1016/S2542-5196(19)30090-7. [DOI] [PubMed] [Google Scholar]
- 7.Ma W, Wang L, Lin H, et al. The temperature–mortality relationship in China: An analysis from 66 Chinese communities. Environ Res. 2015;137:72–77. doi: 10.1016/j.envres.2014.11.016. [DOI] [PubMed] [Google Scholar]
- 8.Zhao Q, Guo Y, Ye T, et al. Global, regional, and national burden of mortality associated with non-optimal ambient temperatures from 2000 to 2019: a three-stage modelling study. Lancet Planet Health. 2021;5:e415–ee25. doi: 10.1016/S2542-5196(21)00081-4. [DOI] [PubMed] [Google Scholar]
- 9.Liu T, Zhou C, Zhang H, et al. Ambient Temperature and Years of Life Lost: A National Study in China. Innovation (N Y) 2021;2 doi: 10.1016/j.xinn.2020.100072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang C, Barnett AG, Wang X, Tong S. The impact of temperature on years of life lost in Brisbane, Australia. Nat Clim Chang. 2012;2:265–270. [Google Scholar]
- 11.GBD 2019 Risk Factors Collaborators Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burkart KG, Brauer M, Aravkin AY, et al. Estimating the cause-specific relative risks of non-optimal temperature on daily mortality: a two-part modelling approach applied to the Global Burden of Disease Study. Lancet. 2021;398:685–697. doi: 10.1016/S0140-6736(21)01700-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.GBD 2019 Diseases and Injuries Collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zheng P, Barber R, Sorensen RJD, Murray CJL, Aravkin AY. Trimmed constrained mixed effects models: formulations and algorithms. J Comput Graph Stat. 2021;30:544–556. [Google Scholar]
- 15.Murray CJ, Lopez AD. On the comparable quantification of health risks: lessons from the Global Burden of Disease Study. Epidemiology. 1999;10:594–605. [PubMed] [Google Scholar]
- 16.Burkart K, Kinney PL. What drives cold-related excess mortality in a south Asian tropical monsoon climate–season vs. temperatures and diurnal temperature changes. Int J Biometeorol. 2017;61:1073–1080. doi: 10.1007/s00484-016-1287-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang Y, Xiang Q, Yu Y, Zhan Z, Hu K, Ding Z. Socio-geographic disparity in cardiorespiratory mortality burden attributable to ambient temperature in the United States. Environ Sci Pollut Res Int. 2019;26:694–705. doi: 10.1007/s11356-018-3653-z. [DOI] [PubMed] [Google Scholar]
- 18.Chen S, Xiao Y, Zhou M, et al. Comparison of life loss per death attributable to ambient temperature among various development regions: a nationwide study in 364 locations in China. Environ Health. 2020;19:98. doi: 10.1186/s12940-020-00653-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fu SH, Gasparrini A, Rodriguez PS, Jha P. Mortality attributable to hot and cold ambient temperatures in India: a nationally representative case-crossover study. PLoS Med. 2018;15 doi: 10.1371/journal.pmed.1002619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yu Y, Duan SB, Li ZL, et al. Interannual spatiotemporal variations of land surface temperature in China from 2003 to 2018. IEEE J Sel Top Appl Earth Obs Remote Sens. 2021;14:1783–1795. [Google Scholar]
- 21.Deng C, Ding Z, Li L, et al. Burden of non-accidental mortality attributable to ambient temperatures: a time series study in a high plateau area of southwest China. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-024708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cai M, Hu J, Zhou C, et al. Mortality burden caused by diurnal temperature range: a nationwide time-series study in 364 Chinese locations. Stoch Environ Res Risk Assess. 2021;35:1605–1614. [Google Scholar]
- 23.Zhou M, Wang H, Zeng X, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394:1145–1158. doi: 10.1016/S0140-6736(19)30427-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhou M, Wang H, Zhu J, et al. Cause-specific mortality for 240 causes in China during 1990-2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387:251–272. doi: 10.1016/S0140-6736(15)00551-6. [DOI] [PubMed] [Google Scholar]
- 25.Public Health England. The cold weather plan for England: Protecting health and reducing harm from cold weather. London, 2018. https://www.gov.uk/government/publications/cold-weather-plan-cwp-for-england. Accessed 29 January 2022
- 26.Lin H, Ma W, Liu Q. Springer; Singapore: 2019. Ambient temperature and health in China. [Google Scholar]
- 27.Sera F, Hashizume M, Honda Y, et al. Air conditioning and heat-related mortality: A multi-country longitudinal study. Epidemiology. 2020;31(6):779–787. doi: 10.1097/EDE.0000000000001241. [DOI] [PubMed] [Google Scholar]
- 28.Son J-Y, Liu JC, Bell ML. Temperature-related mortality: a systematic review and investigation of effect modifiers. Environ Res Lett. 2019;14 [Google Scholar]
- 29.Huang Z, Lin H, Liu Y, et al. Individual-level and community-level effect modifiers of the temperature–mortality relationship in 66 Chinese communities. BMJ Open. 2015;5 doi: 10.1136/bmjopen-2015-009172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Duan X. China Environment Press; Beijing: 2013. Exposure factors handbook of Chinese Population (Adults) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.