Abstract
Background and Aim
Falls are common among older adults in India. Several primary studies on its risk factors have been conducted in India. However, no systematic review has been conducted on this topic. Thus, the objective of this systematic review was to synthesize the existing evidence on the risk factors for falls among older adults in India.
Methods
JBI and Preferred Reporting Items for Systematic Reviews and Meta‐Analyse guidelines were followed, and two independent reviewers were involved in the process. This review included observational studies conducted among older adults (aged ≥ 60 years) residing in India, reporting any risk factor for falls as exposure and unintentional fall as the outcome. MEDLINE, EMBASE, PsycInfo, CINAHL, and ProQuest Dissertations and Theses were searched until September 24, 2020. Where possible, data were synthesized using random‐effects meta‐analysis.
Results
The literature search yielded 3445 records. Twenty‐two studies met the inclusion criteria of this systematic review, and 19 studies were included in the meta‐analysis. Out of the 22 included studies in the systematic review, 12 (out of 18) cross‐sectional studies, two case–control studies, and two cohort studies met more than 70% criteria in the respective Joanna Briggs Institute (JBI) checklists. Risk factors for falls among older adults in India included sociodemographic factors, environmental factors, lifestyle factors, physical and/or mental health conditions, and medical interventions.
Conclusions
This systematic review and meta‐analysis provided a holistic picture of the problem in India by considering a range of risk factors such as sociodemographic, environmental, lifestyle, physical and/or mental health conditions and medical intervention. These findings could be used to develop falls prevention interventions for older adults in India.
Systematic Review and Meta‐Analysis Registration
The systematic review and meta‐analysis protocol was registered with PROSPERO (registration number‐CRD42020204818).
Keywords: falls, India, meta‐analysis, older adults, risk factors, systematic review
1. INTRODUCTION
Falls are events that lead to a person coming to rest inadvertently at a lower level. 1 Falls commonly occur in adults aged 60 years or more. 1 , 2 India is the second most populated country, and the number of older adults is estimated to be 137 million in 2021. 3 The number of falls among older adults is increasing with the transition in demographics over time. 4 , 5 The pooled prevalence of falls among older adults in India is estimated to be 31% (95% confidence interval [CI]: 23%–39%). 6
Falls can have a negative long‐term impact on the physical and psychological health and socioeconomic condition of the individual. 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 Impact on health includes morbidity and even mortality in severe cases. 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 Physical health consequences include injuries and fractures and reduced activities of daily living. 2 , 7 , 8 , 11 In India, every year, nearly 1.5–2 million older people suffer injuries due to falls, and 1 million succumb to death due to falls. 16 Psychological health consequences include depression, anxiety, the fear of falling, and the lack of self‐confidence. 9 , 11 , 12 , 13 , 17 Social consequences include the lack of social interaction leading to isolation. 9 Economic consequences include increased health and social care costs. 18 All these can take a toll on the overall quality of life. 9 , 11 Disability‐adjusted life years (DALYs) lost due to falls are also high. 15
Several primary studies have been conducted in India to determine the risk factors for falls among older adults. 5 , 19 , 20 , 21 , 22 , 23 , 24 , 25 However, no systematic review has been conducted on this topic. Thus, the objective of this systematic review was to synthesize the existing evidence on the risk factors for falls among older adults in India. The intention was to provide a holistic picture of the problem in India by considering a range of risk factors such as sociodemographic, environmental, lifestyle, physical and/or mental health conditions, and medical intervention. These findings could be used to develop falls prevention interventions for older adults in India.
2. METHODS
The systematic review process adhered to the Joanna Briggs Institute (JBI) systematic reviews of etiology and risk guidelines 26 and Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA). 27 The review protocol was registered with PROSPERO (registration number: CRD42020204818). Two reviewers were involved in the process and independently screened the titles and abstracts and full texts of studies, assessed the methodological quality of studies, and extracted data from the studies (I. B. and B. A.). Any disagreements that arose between them were resolved through discussion. If consensus was not reached, a third reviewer was involved (K. C.).
3. INCLUSION CRITERIA
3.1. Population
The systematic review included studies conducted among older adults (aged ≥ 60 years) residing in India. A study was also eligible if the mean age of the participants was ≥60 years. Furthermore, if the study findings were stratified by age, required data were extracted from the relevant age group, that is, adults aged ≥60 years. If it was not possible to extract these findings, the study was excluded. Studies conducted in any setting, such as community, residential care, primary care, secondary care, and tertiary care, were eligible.
3.2. Exposure
Studies reporting any risk factors for falls as exposure were included.
3.3. Outcome
Studies reporting unintentional falls as outcomes were included (i.e., the actual occurrence of falls and not the risk or fear of falls). Studies reporting falls due to accidents or intentional actions like self‐harm or domestic violence were excluded.
3.4. Study design
Observational studies (cohort, case–control, and cross‐sectional studies) were included.
4. DATABASES AND SEARCH STRATEGY
We searched for a wide range of sources to find both published and unpublished studies. The following databases were searched for published studies: MEDLINE (Ovid; since 1946), EMBASE (Ovid; since 1974), PsycInfo (Ovid; since 1806), and CINAHL (EBSCOHost; since 1945), and the search for unpublished studies included ProQuest Dissertations and Theses. An initial limited search was carried out on MEDLINE and EMBASE databases using the keywords: “risk factors,” “falls,” and “India.” The titles and abstracts of the studies were screened for keywords, and the index terms used to describe the article were also identified. The search results were inspected to ensure that relevant articles were identified. Based on this, the search strategy for each database was developed in consultation with a senior research librarian and are detailed in the Supporting Information File: Appendix 1. All the databases were searched on September 24, 2020. No date or language restrictions were applied. The reference list of all the identified reviews and studies selected for inclusion in the systematic review were screened for additional studies.
5. STUDY SELECTION
Retrieved studies were collated and uploaded onto EndNote X9 (Clarivate Analytics), a reference management software. 28 After the removal of duplicate studies, the titles, and abstracts of the remaining studies were screened for eligibility using the inclusion criteria. Studies identified as potentially eligible or those without an abstract had their full texts retrieved. Full texts of the studies were assessed for eligibility. Those that did not meet the inclusion criteria were excluded, and the reasons for exclusion are reported in the Supporting Information File: Appendix 2.
6. METHODOLOGICAL QUALITY ASSESSMENT
The included studies were critically assessed using the JBI checklists for observational studies. 26 , 27 , 29 As recommended by JBI, a cut‐off score was not used to include/exclude studies. Hence, all studies irrespective of their methodological quality were included.
7. DATA EXTRACTION
Data were extracted from the included studies using a predeveloped and pretested data extraction, and we used Microsoft Word for this purpose. The following information was extracted: author and year of the study, name of the Indian state, study design, study period, study setting (e.g., community, primary care, secondary care, tertiary care), sample size, population characteristics (mean age [in years], number of females), risk factors explored, the definition of falls and assessment of falls (e.g., self‐reported/using medical notes or reports). Where possible, odds ratios (ORs) were extracted along with 95% CIs. Adjusted ORs were preferred over crude ORs. If only raw data were presented, ORs and 95% CIs were calculated. In case of missing or insufficient data in the paper, the corresponding author was emailed twice and requested to share the same.
8. DATA SYNTHESIS
All the studies were included in the narrative data synthesis. A meta‐analysis was conducted using Review Manager 5.4 (Cochrane Management System) if two or more studies reported the same or similar risk factors. 30 Meta‐analysis was conducted separately for each study design. ORs were pooled together with 95% CIs using random‐effects meta‐analysis models. In the case of multiple categories in a study, two or more categories were combined to form a new category for analysis. For example, in some studies, socioeconomic status was reported as a higher class, middle class, and lower class. In this case, the lower and middle classes were combined to form one category and the higher class was considered as the reference group for the calculation of ORs. The standard errors were calculated using the following formula: standard error = (log upper CI–log lower CI)/3.92, in STATA 16 (Stata Corp.) for the creation of individual forest plots. The I 2 test was used to explore statistical heterogeneity across studies.
9. RESULTS
9.1. Study selection
Figure 1 shows the PRISMA flow diagram of the identification, screening, and eligibility of included articles. Three thousand four hundred and forty‐five studies were identified, and after the removal of duplicates, 3090 studies were left for the title and abstract screening. After title and abstract screening, 44 studies were left for the full‐text screening. After the full‐text screening, 22 studies were included in this systematic review. 5 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 All the included studies were in the English language. Out of these 22 studies, 19 studies were included in the meta‐analysis. 5 , 19 , 23 , 24 , 25 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44
Figure 1.

PRISMA flow diagram of the identification, screening, and eligibility of the included articles.
9.2. Characteristics of included studies
Characteristics of the included studies are presented in Table 1. Six studies were conducted in the northern states of India, 19 , 20 , 24 , 31 , 32 , 41 whereas 13 were conducted in the southern states. 5 , 21 , 22 , 25 , 33 , 34 , 36 , 37 , 39 , 40 , 42 , 43 , 44 Only one study was conducted in an eastern state of India 38 and another in a western state. 23 One study was conducted in both western and southern states (Maharashtra and Karnataka, respectively). 35 Eighteen studies were cross‐sectional, 19 , 20 , 21 , 22 , 23 , 24 , 25 , 31 , 32 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 44 two were case–control 5 , 33 and two were cohort. 42 , 43 The studies were conducted from 2001 onward. Seven studies were conducted in rural India 5 , 22 , 25 , 31 , 34 , 40 , 41 and eight in urban. 21 , 24 , 33 , 37 , 38 , 39 , 43 , 44 Two studies were conducted both in rural and urban India 32 , 42 and five studies did not specify rural‐urban details. 19 , 20 , 23 , 35 , 36 Sixteen studies were conducted in community care settings, 5 , 20 , 23 , 24 , 25 , 31 , 32 , 34 , 35 , 37 , 38 , 39 , 40 , 41 , 42 , 44 two were conducted in tertiary settings, 33 , 43 one in both community and tertiary settings 21 and three in primary settings. 19 , 22 , 36 The sample size ranged from 100 to 2049. The mean age ranged from 63.9 to 75.2 years. The studies included adults of both sexes except one which included only older women. 21 The studies collected self‐reported data on exposures, and physical examinations were also conducted to assess the exposures in nine studies. 19 , 25 , 31 , 32 , 36 , 37 , 38 , 39 , 43 Thirteen studies collected only self‐reported data on falls as reported by the patients/family members, 5 , 20 , 21 , 22 , 23 , 24 , 25 , 33 , 34 , 36 , 38 , 39 , 40 eight studies used both self‐reported data and medical notes 19 , 31 , 32 , 37 , 41 , 42 , 43 , 44 and one study only used medical notes. 35
Table 1.
Characteristics of included studies
| References R | Indian state | Study design | Study period | Study setting | Sample size (n) | Mean age (in years) | Females (n) | Risk factors explored | Definition of falls | Assessment of falls | Critical appraisal score (total % of “yes” to critical appraisal questions) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Johnson 21 | Kerala | Cross‐sectional | 2002 | Community and tertiary care | 145 | 74.00 | 145 | History of falls (S), area of injury in the body (S), location of falls (home/outside) (NS), required medical attention (S) | Not defined | Self‐reported by patients | 38 |
| Patil 37 | Karnataka | Cross‐sectional | 2009–2010 | Community care | 416 | Not reported | 268 | Medicine intake (S), alcohol consumption (S), smoking (S), physical activity (NS), usage of walking aid (S), usage of stairs (S), joint pains (NS), dizziness (S), diabetes (NS), balance (NS), gait (S), vision impairment (S), tremor (S), cataract (S), the urgency of micturition (NS), backache on walking (S), nonsteroidal anti‐inflammatory drugs (S), tricyclic antidepressants (S), usage of loose slippers outside the home (S) | Inadvertently coming to rest on the ground, floor, or other lower level excluding intentional change in position to rest on furniture, wall, or other objects | Self‐reported by patients and medical notes | 100 |
| Suryanarayana et al. 44 | Karnataka | Cross‐sectional | 2010–2011 | Community Care | 416 | 67.00 | 268 | Cluttering in the house (S), lighting inadequate (S), steps at the entrance of the house (S), the uneven floor of the house (S), split levels in the house (S), slippery floors of the house (S), inadequate handholds (NS), thresholds in the house (NS), carpets/loose rugs on the floor (NS), usage of Indian toilet (NS), uneven surfaces in the surroundings (NS) | Inadvertently coming to rest on the ground, floor, or other lower level excluding intentional change in position to rest on furniture, wall, or other objects | Self‐reported by patients and medical notes | 63 |
| Tripathy et al. 32 | Punjab | Cross‐sectional | 2011–2012 | Community Care | 300 | 68.00 | 140 | Age (NS), sex (NS), BMI (NS), balance (S), polypharmacy (S), residence place (urban/rural) (NS) | Not defined | Self‐reported by patients and medical notes | 100 |
| Dhargave and Sendhilkumar | Maharashtra Karnataka | Cross‐sectional | Not reported | Community care | 163 | 74.61 | 87 | Sex (S), vision impairment (S), medicine intake (S), usage of walking aid (S), vertigo (S), balance (S), gait (S), fear of fall (S), history of falls (S), acute medical problem (NS) | Inadvertently coming to rest on the ground, floor, or other lower level excluding intentional change in position to rest on furniture, wall, or other objects | Medical notes | 75 |
| Ravindran and Kutty 33 | Kerala | Case‐control | 2013 | Tertiary care | 482 (includes both cases and controls) | 69.31 | 286 (includes both cases and controls) | Age (S), history of falls (S), vision impairment (S), marital status (S), slippery floors (S) | Injurious falls were defined as falls that resulted in injuries that required hospitalization for at least 24 h | Self‐reported by patients | 70 |
| Saikia 38 | Assam | Cross‐sectional | 2013 | Community Care | 400 | Not reported | 217 | Age (S), gender (S), vision impairment (S), polypharmacy (S), functional status (S), gait (S), dementia (S) | Inadvertently coming to rest on the ground, floor, or other lower level, excluding intentional change in position to rest | Self‐reported by patients | 50 |
| Chacko and Thangaraj 34 | Tamil Nadu | Cross‐sectional | 2015–2016 | Community Care | 655 | Not reported | 380 | Age (S), sex (NS), functional disability (NS), formal education (NS), socioeconomic status (NS), arthritis (NS), diabetes (NS), hypertension (NS), vision impairment (NS), medicine intake (NS), alcohol consumption (NS), dizziness (S) | Coming to rest inadvertently on the ground or floor or other lower‐level occurring inside or outside the home | Self‐reported by patients and their family members | 88 |
| Rekha et al. 40 | Kerala | Cross‐sectional | 2012–2013 | Community care | 202 | 69.50 | 110 | Age (NS), sex (NS), formal education (S), marital status (NS), medicine intake (NS), fall history (S), existing morbidity (≥1) (S), multimorbidity (≥2) (NS) | An event that results in a person coming to rest inadvertently on the ground or floor or other levels | Self‐reported by patients | 75 |
| Sirohi et al. 31 | Haryana | Cross‐sectional | 2015 | Community care | 456 | 69.40 | 256 | Age (S), gender (S), socioeconomic status (S), urgency of micturition (S), diabetes (NS), hypertension (S), chronic respiratory morbidity (S), arthritis (S), functional disability (S), BMI (NS), balance (S), gait (S), vision impairment (S), hearing impairment (S), cognitive impairment (S), depression (S) | An event that results in a person coming to rest inadvertently on the ground or floor or other lower level | Self‐reported by patients and medical notes | 100 |
| Sharma et al. 25 | Telangana | Cross‐sectional | 2012 | Community care | 561 | 67.50 | 281 | Depression (S), BMI (S), cardiovascular disease (S) | A person was defined as a faller if s/he answered affirmatively to the following: “Have you fallen in the past 12 months?” and “If so, how many times?” | Self‐reported by patient | 100 |
| Balabaskaran and Dongre 22 | Pondicherry | Cross‐sectional | 2017 | Primary care | 570 | Not reported | Not reported | Type of house (Pucca, Kutcha, semi‐pucca) (NS), the flooring of the house (NS), flooring of the bathroom (S), type of house (NS), lighting in the living area and unstable furniture (NS), type of latrine (NS), flooring of the latrine (S), location of the latrine (NS) | Inadvertently coming to rest on the ground, floor, or other lower level, excluding intentional change in position to rest on furniture, wall, or other objects | Self‐reported by patients | 38 |
| Krishnaiah and Ramanathan 36 | Andhra Pradesh | Cross‐sectional | 2016–2017 | Primary care | 382 | 63.90 | 202 | Age (NS), gender (NS), formal education (NS), socioeconomic status (NS), cataract (S), systemic illness (S) | Unintentionally coming to the ground or some lower level and not as a result of a major intrinsic event (e.g., stroke) or overwhelming hazard | Self‐reported by patients | 100 |
| Pathania et al. 24 | Delhi | Cross‐sectional | 2015 | Community care | 335 | 75.20 | 206 | Age (S), sex (NS), existing morbidity (≥1) (S), formal education (NS), marital status (NS), pension (NS), usage of tobacco (S) | An event that resulted in a person coming to rest inadvertently on the ground or floor or other lower level | Self‐reported by patients | 75 |
| Adila 20 | Delhi | Cross‐sectional | Not reported | Community care | 100 | Not reported | 54 | Age (S), history of falls (S), vision impairment (S), polypharmacy (S), chronic disease (S), balance (S), vertigo (S), usage of walking aid (S) | Not defined | Self‐reported by patients | 50 |
| Peter et al. 5 | Tamil Nadu | Case–control | 2013–2014 | Community care | 280 (includes both cases and controls) | 66.00 | 151 (includes both cases and controls) | Physical activity (NS), vision impairment (NS), fear of falls (S), dizziness (S), diabetes (NS), alcohol consumption (NS), medicine intake (NS) | Inadvertently coming to rest on the ground, floor, or other lower level, excluding intentional change in position to rest in furniture, wall, or other objects | Self‐reported by patients | 90 |
| Jindal et al. 41 | Haryana | Cross‐sectional | 2017 | Community care | 468 | 66.41 | 273 | Gender (S), vertigo (S), hearing impairment (S), polypharmacy (S), slippery floors (S), weakness in any body part (S), joint pain (NS), chronic respiratory disease (S), hypertension (S), diabetes (NS), usage of stairs (S), functional disability (S), cognitive impairment (NS), vision impairment (NS), depression (S), ear discharge (NS), ear pain (NS), dim light (NS), uneven ground (NS), previous disability (S) | Inadvertently coming to rest on the ground, floor, or other lower level, excluding intentional change in position to rest on furniture, wall, or another object (fall within 1 year) | Self‐reported by patients and medical notes | 100 |
| Kumar and Ravindran 39 | Tamil Nadu | Cross‐sectional | 2018 | Community care | 150 | 66.61 | 123 | Age (NS), gender (NS), tremors (NS), multimorbidity (≥2) (NS), hypertension (NS), living alone (NS), diabetes (NS), vision impairment (NS), usage of walking aid (NS), joint pain (NS), physical activity (NS), BMI (NS), cataract (NS), balance (NS), gait (NS), forgetfulness (NS) | Inadvertently coming to rest on the ground, floor, or other lower level, excluding intentional change in position to rest in furniture, wall, or other objects | Self‐reported by patients | 88 |
| Pitchai et al. 23 | Maharashtra | Cross‐sectional | 2016 | Community care | 2049 | 69.69 | 946 | Age (S), gender (NS), formal education (S), marital status (S), living alone (S), socioeconomic status, living arrangement (NS), types of residency (community/institutional) (NS) | Any unintentional change in position where the person ends up on the floor, ground, or other lower level | Self‐reported by patients | 63 |
| Subramanian et al. 19 | Delhi | Cross‐sectional | 2015–2017 | Primary care | 160 | 74.47 | 42 | Fear of fall (S), pension (NS), formal education (NS), socioeconomic status (NS), alcohol consumption (NS), smoking (NS), diabetes (NS), joint pain (NS), the urgency of micturition (NS), chronic respiratory disease (NS), hypertension (NS), vision impairment (NS), functional disability (NS), anti‐anginal medications(S), opioids (S), self‐employment (S) | An event which results in a person coming to rest inadvertently on the ground floor or other lower level | Self‐reported by patients s and medical notes | 100 |
| Sasidharan et al. 42 | Kerala | Cohort | 2015–2017 | Community care | 1000 | 72.70 | 568 | Gender (S), movement disorders/Parkinson's disease (S), arthritis (S), functional disability (S), not the usage of hypertensive medications (S), living alone during daytime (S), history of falls (S), regular exercise or yoga (NS), age group (NS), diabetes (NS), hypertension (NS), asthma or COPD (NS), coronary artery disease (NS), cerebrovascular disease (S), alcohol consumption (NS), smoking (NS), knee pain (NS), numbness and paraesthesia of feet (S), urinary symptoms (S), vision impairment (NS) | Unintentionally coming to the ground or some lower level and other than as a consequence of sustaining a violent blow, loss of consciousness, sudden onset of paralysis as in stroke or an epileptic seizure | Self‐reported by patients and medical notes | 100 |
| Marmamula et al. 43 | Telangana | Cohort | 2017–2019 | Tertiary care | 1074 | 74.40 | 686 | Age (NS), gender (NS), hypertension (NS), diabetes (NS), hearing impairment (NS), depression (S), fear of falling (S), visual impairment (S) | Accidental coming to a halt at the level lower than their normal | Self‐reported by patients and medical notes | 82 |
Abbreviations: NS, nonsignificant; S, significant (as reported by the study authors based on unadjusted/crude measures).
10. METHODOLOGICAL QUALITY OF INCLUDED STUDIES
The total critical appraisal scores for each study are presented in Table 1. Tables 2, 3, 4 report the detailed critical appraisal of the included studies.
Table 2.
Critical appraisal results of cohort studies
| Study | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Total % of “yes” to critical appraisal questions |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sasidharan et al. 42 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 100 (11) |
| Marmamula et al. 43 | Y | Y | Y | Y | Y | Y | Y | Y | N | N | Y | 82 (9) |
| Total % of “yes” to each critical appraisal question | 100 (2) | 100 (2) | 100 (2) | 100 (0) | 100 (2) | 100 (2) | 100 (2) | 100 (2) | 50(1) | 50 (1) | 100 (2) |
Abbreviations: N, no; U, unclear; Y, yes.
Were the two groups similar and recruited from the same population?
Were the exposures measured similarly to assign people to both exposed and unexposed groups?
Was the exposure measured in a valid and reliable way?
Were confounding factors identified?
Were strategies to deal with confounding factors stated?
Were the groups/participants free of the outcome at the start of the study (or at the moment of exposure)?
Were the outcomes measured in a valid and reliable way?
Was the follow‐up time reported and sufficient to be long enough for outcomes to occur?
Was follow‐up complete, and if not, were the reasons to loss to follow‐up described and explored?
Were strategies to address incomplete follow‐up utilized?
Was appropriate statistical analysis used?
Table 3.
Critical appraisal results of case–control studies
| Study | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Total % of “yes” to critical appraisal questions |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ravindran and Kutty 33 | U | N | Y | U | Y | Y | Y | Y | Y | Y | 70 (7) |
| Peter et al. 5 | Y | Y | Y | U | Y | Y | Y | Y | Y | Y | 90 (9) |
| Total % of “yes” to each critical appraisal question | 50 (1) | 50 (1) | 100 (2) | 0 (0) | 100 (2) | 100 (2) | 100 (2) | 100 (2) | 100 (2) | 100 (2) |
Abbreviations: N, no; U, unclear; Y, yes.
Were the groups comparable other than the presence of disease in cases or the absence of disease in controls?
Were cases and controls matched appropriately?
Were the same criteria used for the identification of cases and controls?
Was exposure measured in a standard, valid, and reliable way?
Was exposure measured in the same way for cases and controls?
Were confounding factors identified?
Were strategies to deal with confounding factors stated?
Were outcomes assessed in a standard, valid and reliable way for cases and controls?
Was the exposure period of interest long enough to be meaningful?
Was appropriate statistical analysis used?
Table 4.
Critical appraisal results of cross‐sectional studies
| Study | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Total % of “yes” to critical appraisal questions |
|---|---|---|---|---|---|---|---|---|---|
| Johnson 21 | Y | Y | U | N | Y | N | N | N | 38 (3) |
| Patil 37 | Y | Y | Y | Y | Y | Y | Y | Y | 100 (8) |
| Suryanarayana et al. 44 | Y | Y | Y | U | U | N | Y | Y | 63 (5) |
| Tripathy et al. 32 | Y | Y | Y | Y | Y | Y | Y | Y | 100 (8) |
| Dhargave and Sendhilkumar 35 | Y | Y | Y | Y | N | N | Y | Y | 75 (6) |
| Saikia 38 | Y | N | Y | Y | N | N | Y | N | 50 (4) |
| Chacko and Thangaraj 34 | Y | Y | Y | N | Y | Y | Y | Y | 88 (7) |
| Rekha et al. 40 | Y | Y | N | N | Y | Y | Y | Y | 75 (6) |
| Sharma et al. 25 | Y | Y | Y | Y | Y | Y | Y | Y | 100 (8) |
| Sirohi et al. 31 | Y | Y | Y | Y | Y | Y | Y | Y | 100 (8) |
| Balabaskaran and Dongre 22 | N | Y | N | Y | N | N | Y | N | 38 (3) |
| Krishnaiah and Ramanathan 36 | Y | Y | Y | Y | Y | Y | Y | Y | 100 (8) |
| Pathania et al. 24 | Y | Y | N | U | Y | Y | Y | Y | 75 (6) |
| Adila 20 | Y | Y | U | U | N | N | Y | Y | 50 (4) |
| Jindal et al. 41 | Y | Y | Y | Y | Y | Y | Y | Y | 100 (8) |
| Pitchai et al. 23 | Y | Y | Y | Y | N | N | Y | N | 63 (5) |
| Kumar and Ravindran 39 | Y | Y | U | Y | Y | Y | Y | Y | 88 (8) |
| Subramanian et al. 19 | Y | Y | Y | Y | Y | Y | Y | Y | 100 (8) |
| Total % of “yes” to each critical appraisal question | 94 (16) | 94 (16) | 65 (11) | 71 (12) | 71 (12) | 65 (11) | 94 (16) | 76 (13) |
Abbreviations: N, no; U, unclear; Y, yes.
Were the criteria for inclusion in the sample clearly defined?
Were the study subjects and the setting described in detail?
Was the exposure measured in a valid and reliable way?
Were objective, standard criteria used for measurement of the condition?
Were confounding factors identified?
Were strategies to deal with confounding factors stated?
Were the outcomes measured in a valid and reliable way?
Was appropriate statistical analysis used?
Two cohort studies attained more than 70% JBI criteria, that is, answered affirmatively to at least eight questions on the checklist. 42 , 43 The two groups for comparison were similar in characteristics and recruited from the same population in both the studies. 42 , 43 Measurement of exposures was done in a valid and reliable way and clearly described in both the studies. 42 , 43 Both the studies identified confounding factors and used multiple logistic regression analysis to deal with confounding. 42 , 43 The patients were free of the outcome (i.e., no falls) before inclusion in the studies and used standard definitions of falls. 42 , 43 The follow‐up time was at least 1 year which was sufficient to assess falls. 42 , 43 In one study, there was no information on the follow‐up of patients, and the strategies to address incomplete follow‐up were also not described. 43 Appropriate statistical analysis was used as both the studies utilized regression analysis. 42 , 43
Both the case–control studies attained more than 70% JBI criteria, that is, answered affirmatively to at least seven questions on the checklist. 5 , 33 Cases and controls were not matched appropriately in one study. 33 For each of the studies, the same criteria were used for the identification of cases and controls. 5 , 33 It was unclear if the validity of exposure measurement was done in a standard, valid and reliable way. 5 , 33 However, measurement of exposure was done using the same method for cases and controls. 5 , 33 Both the studies identified confounders and used multivariable logistic regression analysis to deal with the potential confounding variables. Standard definitions of falls were used to assess falls in a standard, valid and reliable way for both cases and controls. 5 , 33 The exposure period of interest was at least 6 months in both the studies, which was enough to assess falls. Appropriate statistical analyses were used as multivariable regression analyses were conducted in both the studies. 5 , 33
Twelve out of 18 cross‐sectional studies included in the systematic review attained more than 70% JBI criteria, that is, answered affirmatively to at least six questions on the checklist. 19 , 24 , 25 , 31 , 32 , 34 , 35 , 36 , 37 , 39 , 40 , 41 All the studies reported inclusion criteria except one 22 and study settings and patients except one. 38 The measurement of exposure was unclear in three studies 20 , 21 , 39 and was not described in three studies. 22 , 24 , 40 All the studies defined falls succinctly except three. 21 , 34 , 40 Five studies did not identify the confounders and strategies to deal with the same. 20 , 22 , 23 , 35 , 38 However, studies that mentioned confounders reported age and sex as the most common confounders. In the four studies with insufficient statistical analyses, multivariable logistic regression could have been conducted. 21 , 22 , 23 , 38
11. META‐ANALYSIS
Statistically significant risk factors for falls among older adults in India included sociodemographic factors: increasing age (OR: 2.17, 95% CI: 1.66–2.84), female sex (cohort studies: 1.32, 1.04–1.68; case–control studies: 1.34, 1.13–1.58), no formal education (1.31, 1.01–1.70), and marital status—single/widowed/divorced (1.43, 1.07–1.91); an environmental factor: dim light (1.09, 1.04–1.14); lifestyle factors: physical activity (1.40, 1.03–1.90) and smoking (3.10, 1.52–6.32); physical and/or mental health conditions: poor balance (2.95, 1.65–5.27), abnormal gait (2.70, 1.44–5.06), dizziness (2.24, 1.48–3.39), arthritis/joint pain/knee pain/osteoarthritis (2.05, 1.36–3.08), functional status/previous disability (1.91, 1.34–2.73), coronary artery disease/cardiovascular disease (2.66, 1.55–4.57), diabetes (1.29, 1.02–1.64), hypertension (1.49, 1.20–1.84), difficulty in mobility (2.20, 1.25–3.86), vision impairment/cataract (case–control studies: 2.92, 1.18–7.22; cross‐sectional studies: 2.08, 1.53–2.84), hearing impairment/hearing loss/poor hearing (2.26, 1.68–3.03), history of falls (5.00, 1.01–24.82), urgency of micturition/incontinence of urine/urinary symptoms (3.20, 2.11–4.85), cognitive impairment/dementia/forgetfulness/Parkinsonism (2.53, 1.33–4.82), depression (2.31, 1.51–3.54), fear of falls (3.42, 2.00–5.85), acute medical problem/acute illness of <3 weeks duration (2.55, 1.41–4.64), existing morbidity ≥1 (2.29, 1.36 to 3.86) and multimorbidity ≥2 (1.61, 1.01 to 2.56); medical interventions: medicine intake (1.80, 1.40–2.30), usage of analgesic medications (4.16, 1.09–15.95), usage of medications for the cardiovascular system (2.42, 1.10–5.34), and usage of walking aid/stick (2.11, 1.07–4.17). The summary forest plots for the broad categories of risk factors included in the meta‐analysis are shown in Figures 2, 3, 4, 5, 6. The individual forest plots are represented in the Supporting Information File: Appendix 3 to Figures [Link], [Link], [Link], [Link], [Link]. Supporting Information File: Appendix 4—Figures [Link], [Link], [Link], [Link] show the summary forest plots for the broad categories of risk factors that could not be included in the meta‐analysis.
Figure 2.

Summary forest plot of the association between sociodemographic factors and falls.
Figure 3.

Summary forest plot of the association between environmental factors and falls.
Figure 4.

Summary forest plot of the association between lifestyle factors and falls.
Figure 5.

Summary forest plot of the association between physical and/or mental health conditions and falls.
Figure 6.
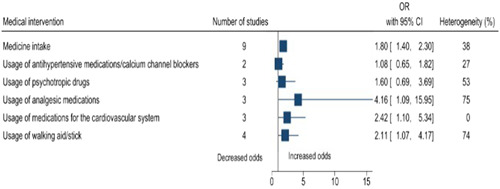
Summary forest plot of the association between medical interventions and falls.
12. DISCUSSION
Risk factors for falls among older adults in India included sociodemographic factors, environmental factors, lifestyle factors, physical and/or mental health conditions, and medical interventions. Some of the review findings were consistent with previous systematic reviews conducted worldwide including increasing age, 45 , 46 , 47 , 48 female sex, 49 dim light, 50 poor balance, 38 , 51 , 52 abnormal gait, 38 , 51 , 52 dizziness, 53 , 54 poor functional status, 45 , 55 , 56 hearing impairment/hearing loss, 57 , 58 cerebrovascular disease/stroke, 58 arthritis/joint pain, 39 , 59 , 60 urgency of micturition/incontinence of urine/urinary symptoms, 58 , 61 , 62 , 63 vision impairment, 56 , 64 , 65 , 66 diabetes, 67 , 68 , 69 hypertension, 70 difficulty in mobility, 58 , 71 history of falls, 38 , 71 depression, 45 , 72 dementia, 56 cognitive impairment, 38 , 45 , 56 , 72 fear of falls, 73 , 74 multimorbidity, 55 , 75 medicine intake, 71 , 76 , 77 , 78 , 79 , 80 , 81 , 82 usage of medications for the cardiovascular system, 76 , 77 , 82 and usage of walking aid/stick. 83 This review also highlighted some additional risk factors for falls among older adults. For example, sociodemographic factors such as being single/widowed/divorced and no formal education, lifestyle factors such as physical activity and smoking, and physical and/or mental health conditions such as acute medical problem/acute illness of <3 weeks duration and existing morbidity (≥1) and medical interventions such as usage of analgesic medications. Globally, age is a well‐known risk factor for falls. 45 , 46 , 47 , 48 In this review, age was found to be a significant risk factor in the meta‐analysis conducted for cross‐sectional studies, however, not for cohort studies. In terms of the hierarchy of study designs, cohort studies are considered better than cross‐sectional studies. However, in this case, there were only two cohort studies, and the statistical heterogeneity was high (84%). On the other hand, there were nine cross‐sectional studies, and the statistical heterogeneity was 43%. It should also be noted that we included only those studies that focused on older adults, and the age range was already narrow. In this review, physical activity was found to be a risk factor. Intuitively, one would expect the opposite, and this issue requires further investigation. The possible reason could be not following the recommended physical activity guidelines, quantity or quality wise. 84
In total, three studies could not be included in the meta‐analysis. In two studies, it was not possible to estimate the ORs due to insufficient raw data, however, other relevant information was extracted. 20 , 21 Another study mentioned unique risk factors which were not reported in any other study. 22 In addition, there were some unique risk factors in the other 19 studies that could not be included in the meta‐analysis. More primary research needs to be conducted on several risk factors for which meta‐analysis could not be performed. The included studies were mostly conducted in the northern and southern states of India, and thus, primary studies need to be conducted in other parts of the country for a more complete picture. The majority of the included studies used the standard definitions of falls. However, the information on falls and risk factors were mostly self‐reported by the patients or their family members. Therefore, future research studies should also incorporate other ways in data collection to minimize the risk of recall bias, such as using medical notes and reports and doing physical examinations. Some of the included studies had poor response rates, and the exact reason should be explored and addressed. For example, the way people are approached to participate in a study. Some of the included studies did not adjust for confounders, and this should be addressed in future research studies.
To the best of our knowledge, this was the first systematic review to synthesize the existing evidence on the risk factors for falls among older adults in India. A robust process was followed using JBI and PRISMA guidelines. The probability of missing relevant articles was minimal as we searched for both published and unpublished studies, without any date or language restrictions, and a large number of studies were included. Although the definition of each risk factor was not provided in the articles, in the meta‐analysis, the reviewers tried their best to pool together risk factors having the same or similar meaning. The sample size of the included studies ranged from 100 to 2049, and one might question how reliable would the pooled estimates be when dealing with such a diverse set of samples. To explain this, a sensitivity analysis could have been done by excluding smaller studies, but the problem was to determine how small was small and where to draw the line. Also, the diverse sampling techniques could affect the reliability of the findings.
The systematic review findings could be valid in neighboring South Asian nations because of similarities in population characteristics, sociocultural setups, and healthcare systems. For example, similar to the findings of our review, a primary study conducted in Pakistan reported the association between diabetes and falls among older adults, 85 and research shows that South Asians are more likely to have diabetes. 86 Hence, the findings could be used by a range of stakeholders (including policymakers) in the South Asian region to develop falls prevention targeted interventions, depending on the exact risk factor. If there is more than one risk factor, a multifactorial intervention is recommended to prevent falls. 87 , 88 It should be noted that the “one‐size‐fits‐all” concept should not be applied, and “need‐sensitive” interventions are required. One such example could be yoga‐based interventions. 89
13. CONCLUSION
This systematic review and meta‐analysis reported a wide range of risk factors for falls among older adults in India such as sociodemographic, environmental, lifestyle, physical and/or mental health condition, and medical intervention. These findings could be used to develop fall prevention interventions for older adults in India.
AUTHOR CONTRIBUTIONS
Isha Biswas: Conceptualization; data curation; formal analysis; investigation; methodology; resources; software; validation; visualization; writing—original draft; writing—review and editing. Busola Adebusoye: Data curation; formal analysis; investigation; methodology; software; validation; writing—review and editing. Kaushik Chattopadhyay: Conceptualization; funding acquisition; investigation; methodology; resources; software; supervision; validation; visualization; writing—original draft; writing—review and editing.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
TRANSPARENCY STATEMENT
The manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Supporting information
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
ACKNOWLEDGMENT
The authors thank Alison Ashmore, Senior Research Librarian at the University of Nottingham (UK), for her contribution in developing the search strategies. I. B. was a Master's student funded by the University of Nottingham Developing Solutions Masters Scholarship (award number: RFDX42DB2). B. A. is a PhD student funded by the University of Nottingham Vice‐Chancellor Scholarship for Research Excellence (award number: PN8ZcDcE).
Biswas I, Adebusoye B, Chattopadhyay K. Risk factors for falls among older adults in India: A systematic review and meta‐analysis. Health Sci Rep. 2022;5:e637. 10.1002/hsr2.637
DATA AVAILABILITY STATEMENT
The authors confirm that the data supporting the findings of this study are available within the article [and/or] its supplementary materials.
REFERENCES
- 1. World Health Organization . Falls. Accessed August 15, 2020. https://www.who.int/news-room/fact-sheets/detail/falls
- 2. Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(2):37‐41. [DOI] [PubMed] [Google Scholar]
- 3. Prakash IJ. Ageing in India. World Health Organization; 1999:1‐22. Accessed September 27, 2020. http://www.popbook.com/en/in/pdf/ageinginindia.pdf [Google Scholar]
- 4. Central Statistical Organisation . Elderly in India—profile and programmes. Ministry of Statistics and Programme Implementation; 2004. [Google Scholar]
- 5. Peter RM, Joseph A, John KR, Logaraj M. A community‐based case‐control study on the risk of fall among the elderly in rural Kattankulathur block, Tamil Nadu. Indian J Commun Med. 2019;44(3):277‐280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kaur R, Kalaivani M, Goel AD. Burden of falls among elderly persons in India: a systematic review and meta‐analysis. Natl Med J India. 2020;33:195‐200. [DOI] [PubMed] [Google Scholar]
- 7. Masud T, Morris RO. Epidemiology of falls. Age Ageing. 2001;30(4):3‐7. [DOI] [PubMed] [Google Scholar]
- 8. Tripathy JP. Fall injury prevention‐a neglected public health issue: challenges and way forward in the Indian scenario. Iran J Publ Health. 2013;42(8):923‐924. [PMC free article] [PubMed] [Google Scholar]
- 9. Joseph A, Kumar D, Bagavandas M. A review of epidemiology of fall among elderly in India. Indian J Commun Med. 2019;44(2):166‐168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Baker SP, Harvey AH. Fall injuries in the elderly. Clin Geriatr Med. 1985;1:501‐512. [PubMed] [Google Scholar]
- 11. Cumming RG, Salkeld G, Thomas M, Szonyi G. Prospective study of the impact of fear of falling on activities of daily living, SF‐36 scores and nursing home admissions. J Gerontol. 2000;55(5):299‐305. [DOI] [PubMed] [Google Scholar]
- 12. Parry SW, Steen N, Galloway SR. Falls and confidence related quality of life outcome measures in an older British cohort. Postgrad Med J. 2001;77(904):103‐108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kumar S, Vendhan G, Awasthi S, et al. Relationship between fear of falling, balance impairment and functional mobility in community dwelling elderly. Indian J Phys Med Rehabil. 2008;19:48‐52. [Google Scholar]
- 14. Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical costs of fatal and nonfatal falls in older adults. J Am Geriatr Soc. 2018;66:693‐698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. James SL, Lucchesi LR, Bisignano C, et al. The global burden of falls: global, regional and national estimates of morbidity and mortality from the Global Burden of Disease Study 2017. Inj Prev. 2020;26(1):3‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Krishnaswamy B, Gnanasambandam U. Falls in older people. National/Regional Review, India. Accessed September 27, 2020. http://www.who.int/ageing/projects/SEARO.pdf
- 17. Choi NG, Marti CN, DiNitto DM, Kunik ME. Longitudinal associations of falls and depressive symptoms in older adults. Gerontologist. 2019;59(6):1141‐1151. [DOI] [PubMed] [Google Scholar]
- 18. Craig J, Murray A, Mitchell S, Clark S, Saunders L, Burleigh L. The high cost to health and social care of managing falls in older adults living in the community in Scotland. Scott Med J. 2013;58(4):198‐203. [DOI] [PubMed] [Google Scholar]
- 19. Subramanian MS, Singh V, Chatterjee P, Dwivedi SN, Dey AB. Prevalence and predictors of falls in a health‐seeking older population: an outpatient‐based study. Aging Med. 2020;3(1):25‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Adila BR. To find out the prevalence and various risk factors for falls in older adults (60‐75 years) community NCR Delhi. Indian J Physiother Occup Ther. 2019;13(1):1‐5. [Google Scholar]
- 21. Johnson SJ. Frequency and nature of falls among older women in India. Pac J Public Health. 2006;18(1):56‐61. [DOI] [PubMed] [Google Scholar]
- 22. Balabaskaran S, Dongre AR. Household environmental risk factors for fall in older people (= 65 years) in rural Pondicherry. Online J Health Allied Sci. 2018;17(2):1‐3. [Google Scholar]
- 23. Pitchai P, Dedhia HB, Bhandari N, Krishnan D, D'Souza N, Bellara JM. Prevalence, risk factors, circumstances for falls and level of functional independence among the geriatric population—a descriptive study. Indian J Public Health. 2019;63(1):21‐26. [DOI] [PubMed] [Google Scholar]
- 24. Pathania A, Haldar P, Kant S, Gupta SK, Pandav CS, Bachani D. Prevalence of fall, and determinants of repeat incidents of fall in older persons living in old age homes in the National Capital Territory of Delhi, India. Natl Med J India. 2018;31(6):329‐333. [DOI] [PubMed] [Google Scholar]
- 25. Sharma PK, Bunker CH, Singh T, et al. Burden and correlates of falls among rural elders of south India: mobility and independent living in elders' study. Curr Gerontol Geriatr Res. 2017;2017:1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Moola S, Munn Z, Tufanaru C, et al. Chapter 7: Systematic reviews of etiology and risk. In: Aromataris E, Munn Z, eds. Joanna Briggs Institute Reviewer's Manual. The Joanna Briggs Institute; 2017. Accessed September 28, 2020. https://reviewersmanual.joannabriggs.org/ [Google Scholar]
- 27. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA G, The PRISMA Group . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Endnote. Endnote X9.3 Clarivate Analytics, PA, USA [Internet]. Accessed September 30, 2020. http://endnote.com/
- 29. Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. 2015;13(3):147‐153. [DOI] [PubMed] [Google Scholar]
- 30. The Cochrane Collaboration. Review manager (RevMan) Version 5.4 [Computer program]; 2020
- 31. Sirohi A, Kaur R, Goswami AK, Mani K, Nongkynrih B, Gupta SK. A study of falls among elderly persons in a rural area of Haryana. Indian J Public Health. 2017;61(2):99‐104. [DOI] [PubMed] [Google Scholar]
- 32. Tripathy NK, Jagnoor J, Patro BK, Dhillon MS, Kumar R. Epidemiology of falls among older adults: a cross‐sectional study from Chandigarh, India. Injury. 2015;46(9):1801‐1805. [DOI] [PubMed] [Google Scholar]
- 33. Ravindran RM, Kutty VR. Risk Factors for fall‐related injuries leading to hospitalization among community‐dwelling older persons: a hospital‐based case‐control study in Thiruvananthapuram, Kerala, India. Asia Pac J Public Health. 2016;28(1):70‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chacko T, Thangaraj PM. Epidemiology of fall and its risk factors among elders in a rural area of Coimbatore, India. Int J Community Med Public Health. 2017;4:3864. [Google Scholar]
- 35. Dhargave P, Sendhilkumar R. Prevalence of risk factors for falls among elderly people living in long‐term care homes. J Clin Gerontol Geriatr. 2016;7(3):99‐103. [Google Scholar]
- 36. Krishnaiah S, Ramanathan RV. Impact of blindness due to cataract in elderly fallers: findings from a cross‐sectional study in Andhra Pradesh, South India. BMC Res Notes. 2018;11(1):773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kural M, Noor NN, Pandit D, Joshi T, Patil A. Risk factors for fall among elderly: a community‐based study. Int J Health Allied Sci. 2015;4(3):135‐140. [Google Scholar]
- 38. Saikia A. Prevalence and correlates of falls among community‐dwelling elderly of Guwahati city, Assam . Indian J Basic Appl Med Res. 2016;5(2):185‐190. [Google Scholar]
- 39. Kumar SR, Ravindran K. A cross‐sectional study on the prevalence and risk factors of fall among the elderly in an urban slum in Chennai. Int J Commun Med Public Health. 2019;6:1102. [Google Scholar]
- 40. Rekha MR, Mini GK, Kutty VR. Falls among older adults: a community‐based study in rural Kerala, India. Glob J Health Sci. 2017;9:165. [Google Scholar]
- 41. Jindal HA, Duggal M, Jamir L, et al. Mental health and environmental factors associated with falls in the elderly in north India: a naturalistic community study. Asian J Psychiatr. 2019;39:17‐21. [DOI] [PubMed] [Google Scholar]
- 42. Sasidharan DK, Vijayakumar P, Raj M, et al. Incidence and risk factors for falls among community‐dwelling elderly subjects on a 1‐year follow‐up: a prospective cohort study from Ernakulam, Kerala, India. BMJ Open. 2020;10(7):e033691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Marmamula S, Barrenkala NR, Challa R, et al. Falls and visual impairment among elderly residents in ‘homes for the aged' in India. Sci Rep. 2020;10(1):13389. 10.1038/s41598-020-70066-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Suryanarayana SP, Patil SS, Rajaram D, et al. Circumstances and consequences of falls in community‐living elderly in north Bangalore, Karnataka. J Krishna Inst Medical Sci Univ. 2015;4(4):27‐35. [Google Scholar]
- 45. Feng Z, Lugtenberg M, Franse C, et al. Risk factors and protective factors associated with incident or increase of frailty among community‐dwelling older adults: a systematic review of longitudinal studies. PLoS One. 2017;12(6):e0178383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Cheng MH, Chang SF. Frailty as a risk factor for falls among community dwelling people: evidence from a meta‐analysis. J Nurs Scholarsh. 2017;49(5):529‐536. [DOI] [PubMed] [Google Scholar]
- 47. Gama ZA, Gómez‐Conesa A. Risk factors for falls in the elderly: systematic review. Rev Saude Publica. 2008;42(5):946‐956. [DOI] [PubMed] [Google Scholar]
- 48. Vieira ER, Freund‐Heritage R, da Costa BR. Risk factors for geriatric patient falls in rehabilitation hospital settings: a systematic review. Clin Rehabil. 2011;25(9):788‐799. [DOI] [PubMed] [Google Scholar]
- 49. Bloch F, Thibaud M, Dugué B, Brèque C, Rigaud AS, Kemoun G. Episodes of falling among elderly people: a systematic review and meta‐analysis of social and demographic pre‐disposing characteristics. Clinics. 2010;65(9):895‐903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Valipoor S, Pati D, Kazem‐Zadeh M, Mihandoust S, Mohammadigorji S. Falls in older adults: a systematic review of literature on interior‐scale elements of the built environment. J Aging Environ. 2020;34(3):1‐24. [Google Scholar]
- 51. Thomas E, Battaglia G, Patti A, et al. Physical activity programs for balance and fall prevention in elderly: a systematic review. Medicine. 2019;98(27):16218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. McCrum C, Gerards MHG, Karamanidis K, Zijlstra W, Meijer K. A systematic review of gait perturbation paradigms for improving reactive stepping responses and falls risk among healthy older adults. Eur Rev Aging Phys Act. 2017;14:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Fernández L, Breinbauer HA, Delano PH. Vertigo and dizziness in the elderly. Front Neurol. 2015;6:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Walther LE, Rogowski M, Schaaf H, Hörmann K, Löhler J. Falls and dizziness in the elderly. Otolaryngol Pol. 2010;64(6):354‐357. [DOI] [PubMed] [Google Scholar]
- 55. Pfortmueller C, Lindner G, Exadaktylos AK. Reducing fall risk in the elderly: risk factors and fall prevention, a systematic review. Minerva Med. 2014;105(4):275‐281. [PubMed] [Google Scholar]
- 56. Härlein J, Dassen T, Halfens RJ, Heinze C. Fall risk factors in older people with dementia or cognitive impairment: a systematic review. J Adv Nurs. 2009;65(5):922‐933. [DOI] [PubMed] [Google Scholar]
- 57. Jiam NTL, Li C, Agrawal Y. Hearing loss and falls: a systematic review and meta‐analysis. Laryngoscope. 2016;126(11):2587‐2596. [DOI] [PubMed] [Google Scholar]
- 58. Lukaszyk C, Harvey L, Sherrington C, et al. Risk factors, incidence, consequences and prevention strategies for falls and fall‐injury within older indigenous populations: a systematic review. Aust N Z J Public Health. 2016;40(6):564‐568. [DOI] [PubMed] [Google Scholar]
- 59. Brenton‐Rule A, Dalbeth N, Bassett S, Menz HB, Rome K. The incidence and risk factors for falls in adults with rheumatoid arthritis: a systematic review. Semin Arthritis Rheum. 2015;44(4):389‐398. [DOI] [PubMed] [Google Scholar]
- 60. Welsh VK, Clarson LE, Mallen CD, McBeth J. Multisite pain and self‐reported falls in older people: systematic review and meta‐analysis. Arthritis Res Ther. 2019;21(1):67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Noguchi N, Chan L, Cumming RG, Blyth FM, Naganathan V. A systematic review of the association between lower urinary tract symptoms and falls, injuries, and fractures in community‐dwelling older men. Aging Male. 2016;19(3):168‐174. [DOI] [PubMed] [Google Scholar]
- 62. Szabo SM, Gooch KL, Walker DR, Johnston KM, Wagg AS. The association between overactive bladder and falls and fractures: a systematic review. Adv Ther. 2018;35(11):1831‐1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Chiarelli PE, Mackenzie LA, Osmotherly PG. Urinary incontinence is associated with an increase in falls: a systematic review. Aust J Physiother. 2009;55(2):89‐95. [DOI] [PubMed] [Google Scholar]
- 64. Dillon L, Clemson L, Ramulu P, Sherrington C, Keay L. A systematic review and meta‐analysis of exercise‐based falls prevention strategies in adults aged 50+ years with visual impairment. Ophthalmic Physiol Opt. 2018;38(4):456‐467. [DOI] [PubMed] [Google Scholar]
- 65. Zhang XY, Shuai J, Li LP. Vision and relevant risk factor interventions for preventing falls among older people: a network meta‐analysis. Sci Rep. 2015;5:10559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Salonen L, Kivelä SL. Eye diseases and impaired vision as possible risk factors for recurrent falls in the aged: a systematic review. Curr Gerontol Geriatr Res. 2012;26:271481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Yang Y, Hu X, Zhang Q, Zou R. Diabetes mellitus and risk of falls in older adults: a systematic review and meta‐analysis. Age Ageing. 2016;45(6):761‐767. [DOI] [PubMed] [Google Scholar]
- 68. Gravesande J, Richardson J. Identifying non‐pharmacological risk factors for falling in older adults with type 2 diabetes mellitus: a systematic review. Disabil Rehabil. 2017;39(15):1459‐1465. [DOI] [PubMed] [Google Scholar]
- 69. Lee AK, Juraschek SP, Windham BG, et al. Severe hypoglycemia and risk of falls in type 2 diabetes: the atherosclerosis risk in communities (ARIC) study. Diabetes Care. 2020;43(9):2060‐2065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Klein D, Nagel G, Kleiner A, et al. Blood pressure and falls in community‐dwelling people aged 60 years and older in the VHM&PP cohort. BMC Geriatr. 2013;13(1):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Evans D, Hodgkinson B, Lambert L, Wood J. Falls risk factors in the hospital setting: a systematic review. Int J Nurs Pract. 2001;7(1):38‐45. [DOI] [PubMed] [Google Scholar]
- 72. Bunn F, Dickinson A, Simpson C, et al. Preventing falls among older people with mental health problems: a systematic review. BMC Nurs. 2014;13(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Barbosa PS, Passos GHCQC, Lima LJ, et al. Fear of falling and risk of falling: a systematic review and meta‐analysis. ACTA Paul Enferm. 2019;32(4):456‐463. [Google Scholar]
- 74. Denkinger MD, Lukas A, Nikolaus T, Hauer K. Factors associated with fear of falling and associated activity restriction in community‐dwelling older adults: a systematic review. Am J Geriatr Psychiatry. 2015;23(1):72‐86. [DOI] [PubMed] [Google Scholar]
- 75. Vetrano DL, Palmer K, Marengoni A, et al. Frailty and multimorbidity: a systematic review and meta‐analysis. J Gerontol. 2019;74(5):659‐666. [DOI] [PubMed] [Google Scholar]
- 76. Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta‐analysis: II. cardiac and analgesic drugs. J Am Geriatr Soc. 1999;47(1):40‐50. [DOI] [PubMed] [Google Scholar]
- 77. De Vries M, Seppala LJ, Daams JG, et al. Fall‐risk‐increasing drugs: a systematic review and meta‐analysis: I. cardiovascular drugs. J Am Med Dir Assoc. 2018;19(4):1‐9. [DOI] [PubMed] [Google Scholar]
- 78. Davies LE, Spiers G, Kingston A, Todd A, Adamson J, Hanratty B. Adverse outcomes of polypharmacy in older people: systematic review of reviews. J Am Med Dir Assoc. 2020;21(2):181‐187. [DOI] [PubMed] [Google Scholar]
- 79. Hartikainen S, Lönnroos E, Louhivuori K. Medication as a risk factor for falls: critical systematic review. J Gerontol. 2007;62(10):1172‐1181. [DOI] [PubMed] [Google Scholar]
- 80. Berlie HD, Garwood CL. Diabetes medications related to an increased risk of falls and fall‐related morbidity in the elderly. Ann Pharmacother. 2010;44(4):712‐717. [DOI] [PubMed] [Google Scholar]
- 81. de Vries M, Seppala LJ, Daams JG, et al. Fall‐risk‐increasing drugs: a systematic review and meta‐analysis. J Am Med Dir Assoc. 2018;19(4):1‐8. [DOI] [PubMed] [Google Scholar]
- 82. Darowski A, Whiting R. Cardiovascular medication and falls. Rev Clin Gerontol. 2011;21(2):170‐179. [Google Scholar]
- 83. Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community‐dwelling older people: a systematic review and meta‐analysis. Epidemiology. 2010;21(5):658‐668. [DOI] [PubMed] [Google Scholar]
- 84. Pereira CLN, Baptista F, Infante P. Role of physical activity in the occurrence of falls and fall‐related injuries in community‐dwelling adults over 50 years old. Disabil Rehabil. 2014;36(2):117‐124. [DOI] [PubMed] [Google Scholar]
- 85. Ghazal J, Malik AN, Amjad I. Task oriented training improves the balance outcome & reducing fall risk in diabetic population. Pak J Med Sci. 2016;32(4):983‐987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. International Diabetes Federation (IDF). IDF diabetes atlas. 9th ed. IDF; 2019. [Google Scholar]
- 87. Tricco AC, Thomas SM, Veroniki AA, et al. Comparisons of interventions for preventing falls in older adults: a systematic review and meta‐analysis. JAMA. 2017;318(17):1687‐1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. NICE . Falls in older people: assessing risk and prevention of falls. NICE clinical guideline 161 [CG161]. National Institute for Health and Care Excellence. 2013. Accessed September 30, 2020. https://www.nice.org.uk/Guidance/CG161 [PubMed]
- 89. National Health Service . A guide to yoga. Accessed October 29, 2021. https://www.nhs.uk/live-well/exercise/guide-to-yoga/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article [and/or] its supplementary materials.


