Abstract
Objective
The COVID-19 pandemic increased economic, social, and health stressors for families, yet its impacts on families of youth with chronic conditions, such as type 1 diabetes (T1D), are not well understood. Self-regulation (SR)—or the capacities to control emotions, cognition, and behavior in response to challenge—is known to support T1D management and coping in the face of stress. Strong SR may have protected youth with T1D from the impacts of pandemic-related stressors. This study compared youth and parent emotional functioning and T1D management before and after the pandemic’s onset in relation to family pandemic-related stress and youth SR.
Methods
Parents of youth with T1D (N = 88) and a subset of these youth (N = 43; Mean age 15.3 years [SD 2.2]) completed surveys regarding SR, stress, emotional functioning, and T1D-related functioning prior to and after March 2020. Outcomes were compared using mixed effects models adjusting for covariates. Family pandemic-related stress experiences and youth SR were tested as moderators of change.
Results
Parents’ responsibility for T1D management increased across pandemic onset and their diabetes-related distress decreased. Family pandemic-related stress was associated with decreased emotional functioning over time. Youth SR, particularly emotional and behavioral aspects, predicted better emotional and T1D-related functioning.
Discussion
While youth with T1D whose families experienced higher pandemic-related stress had poorer adjustment, strong emotional and behavioral SR appeared to protect against worsening youth mood and adherence across pandemic onset. Both social-contextual and individual factors are important to consider when working with families managing T1D.
Keywords: COVID-19, family, self-regulation (SR), stress, type 1 diabetes (T1D), youth
Introduction
Living with type 1 diabetes (T1D) can be challenging for families, particularly in the pre-adolescent and adolescent years. Developmental changes and transitions in T1D management during this time can make attaining optimal glycemic targets difficult. For example, youth may experience mood disturbances and diabetes-related distress due to additional burdens associated with T1D, and parents may worry about relinquishing control of T1D self-management to their child (Hilliard et al., 2013). Early to late adolescence is a period of rapid development in self-regulation (SR), which includes managing emotional responses to stress, cognitive capacity to set goals and plan, and behavioral control to enact plans (Lansing & Berg, 2014). For youth with T1D, SR skills can allow for increased responsibility in T1D self-management.
The COVID-19 pandemic posed potentially unique challenges and stressors for youth with T1D. First, youth with T1D were at increased risk of serious complications and even death if diagnosed with COVID-19 (Gregory et al., 2021). Second, the pandemic disrupted systems to deliver diabetes supplies and routine medical care (e.g. transition to telemedicine visits; Scott et al., 2020). Youth were also less likely to see auxiliary supportive members of the health care team such as school nurses or pediatric psychologists during the early months of the pandemic (Plevinsky et al., 2020). Third, emotional support systems were affected (Magson et al., 2021) due to physical separation from family and friends during periods with stay at home restrictions. Lifestyle factors related to T1D management changed, such as disruption in grocery shopping, exercise regimens, parental work schedules and availability, and sleep schedules. Finally, changes in daily activities, such as the lack of in-person school or school-based activities may have altered T1D self-management routines (Novak et al., 2020; Plevinsky et al., 2020). Studies of the pandemic’s impact on youth with T1D and their caregivers have found mixed results, with some U.S. youth and caregivers reporting higher stress but also healthier eating habits (Goethals et al., 2021) and global work finding high caregiver stress (Alessi et al., 2021), but decreased diabetes distress in youth during lockdown (Mianowska et al., 2021). A recent study of U.S. teens with T1D found that although youth endorsed high anxiety about COVID-19, they also reported use of coping strategies that helped with their anxiety as well as limited diabetes-specific distress or impacts on diabetes management (O’Donnell et al., 2022).
Although SR was not measured in these studies, it may be relevant given evidence of SR as a driver of youth capacity to manage stress (Buckner et al., 2009). For youth with T1D, associations of stronger SR with higher treatment adherence (Lansing & Berg, 2014), lower family conflict (Vaid et al., 2018), and better glycemic outcomes (Vaid et al., 2018) underscore its potential applicability to managing the challenges of the COVID-19 pandemic. SR is a multi-faceted construct that includes emotional, behavioral, and cognitive components (Nigg, 2017). One study identified various youth-reported strategies that may have helped foster diabetes and general stress resilience during the pandemic; although this study did not measure youth SR, the strategies noted reflect different SR skills, for example perspective-taking, distraction, and stress relieving activities (O’Donnell et al., 2022). Different aspects of youth SR, specifically the capacity to manage emotions effectively in response to stress, cognitive ability to plan and organize, and degree of control over impulsive behavior, may underlie use of such strategies and thus function as a protective factor for both emotional functioning and T1D self-management in the face of the pandemic. Understanding how each aspect of SR may underlie these outcomes may be important in providing clinical guidance for youth and families in coping with stressors.
Furthermore, family diabetes management during adolescence is a dynamic process that has been characterized as interdependent between parent and child, with roles in T1D management changing over time with increasing youth SR capacity (Berg et al., 2017). Given parents’ integral role in family diabetes management, it is reasonable to expect that youth SR may thus not only be protective for youth, but also for parents who are coping with stress and challenges to youth T1D self-management. Indeed, developmental studies suggest that child behavior and parent emotional functioning are mutually influential across childhood, with effects of child behaviors such as externalizing on parent responses becoming stronger over time (Mackler et al., 2015). Therefore, we considered how pandemic-related family stress and youth SR related to changes in both youth and parent emotional functioning and youth T1D self-management across the onset of the pandemic.
Goal of the Current Study
We examined changes in emotional functioning and T1D self-management across the onset of the COVID-19 pandemic and the degree to which families’ pandemic-related stress and youth SR buffered or exacerbated changes. The emphasis on youth SR extends prior research on pandemic impacts on youth with T1D (Goethals et al., 2021; O’Donnell et al., 2022) by studying a dynamic developmental factor with clinical intervention implications. Changes in youth and parent emotional functioning and youth T1D self-management were examined from prior to during the pandemic among two samples of U.S. youth with T1D and their parents. We hypothesized that declines in emotional functioning and T1D self-management would be greater in families reporting more pandemic-related stress and that stronger pre-pandemic youth SR would predict less decline in youth and parent emotional functioning and T1D self-management.
Methods
Participants and Procedures
Two studies of SR and medical regimen adherence in youth with T1D were midway through data collection in mid-March 2020, when the COVID-19 pandemic began in the USA (see Supplementary Figure S1). Study 1, which began data collection in May 2019, was a clinical trial with a SR-focused behavioral intervention enrolling youth and their caregivers (97% parents, thus termed “parents”). Study 2, which began data collection in April 2019, was an observational study of parents of youth with T1D. For both studies, participants were recruited from pediatric endocrinology clinics at the University of Michigan and via online methods (Miller et al., 2020). Study 1 eligibility criteria were: youth (a) 13–17 years old; (b) diagnosed with T1D for at least 6 months; (c) had HbA1c ≥ 7.0%; (d) resided with participating parent/legal guardian at least 50% of the time; (e) had regular access to a smartphone and Wi-Fi; (f) no psychiatric or cognitive conditions that would impede ability to participate; and (g) was sufficiently fluent in English to complete study activities. Study 2 eligibility criteria were: (a) parent had a child 10–17 years of age; (b) child was diagnosed with T1D for at least 6 months; (c) child resided with participating parent/legal guardian at least 50% of the time; and (d) parent sufficiently fluent in English to complete study. Both studies were approved by the University of Michigan Institutional Review Board (IRB-MED). Parents provided informed consent in both studies. Youth provided assent for Study 1. All participants from both studies who had completed assessments prior to mid-March 2020 (N = 121 parents [57 in Study 1, 64 in Study 2]; N = 57 youth, all in Study 1) were contacted via email between May and August, 2020 and invited to participate in an online follow-up to assess functioning during the pandemic. Of these, 73% of parents (N = 88) and 75% of youth (N = 43) participated in the follow-up study and were compensated $25 for survey completion. Mean time elapsed between pre- and during-pandemic assessments was 8.7 months (SD: 3.4). Only pre-intervention data were used from Study 1 for the pre-pandemic assessment (no intervention vs. control differences in demographic or outcome variables at pre-intervention; all p-values <.05). All intervention activities for youth assigned to the intervention (N = 22) had been completed prior to the during-pandemic assessment. Intervention condition was covaried in analyses (see below).
Measures
Measures are described in detail elsewhere (Miller et al., 2020) and reviewed below. All measures were assessed in Study 1, Study 2 (both pre-pandemic), and the during-pandemic assessment except where noted. Cronbach’s alphas ranged from .77 to .95 across all timepoints.
Youth Emotional Functioning (Assessed Pre- and During-Pandemic)
Youth reported on their perceived stress (PSS; Gershon et al., 2013), anxiety symptoms (GAD-7; Spitzer et al., 2006), and diabetes-specific distress (Problem Areas in Diabetes-Teen [PAID-T]; Weissberg-Benchell & Antisdel-Lomaglio, 2011). Parents completed a proxy measure of youths’ perceived stress (PSS; Gershon et al., 2013).
Parent Emotional Functioning (Assessed Pre- and During-Pandemic)
Parents reported on their own emotion regulation difficulties (DERS; Gratz & Roemer, 2004), perceived stress (PSS; Gershon et al., 2013), and diabetes-specific distress (Problem Areas in Diabetes—Parents of Teen version [P-PAID-T]; Shapiro et al., 2018).
Youth T1D Self-Management (Assessed Pre- and During-Pandemic)
Youth completed the self-report version and parents completed the proxy version of the Self-Care Inventory-Revised (SCI-R; Weinger et al., 2005) to assess youth adherence to medical regimen. Parents completed the Diabetes Family Responsibility Questionnaire to assess degree of youth self-management of T1D; higher scores indicate the parent takes more responsibility, and lower scores indicate the youth takes more responsibility (DFRQ; Anderson et al., 1990).
Moderators
Pandemic-Related Family Stress (Assessed During-Pandemic). Parents completed an 11-item COVID-19 Family Stress Screener (Huth-Bocks, 2020), rating if they had experienced increased stress (Strongly Disagree [1] to Strongly Agree [5]) related to job loss, access to medical care and child care, social isolation, and physical health due to the COVID-19 pandemic. Mean scores were created with higher values indicating greater stress (Cronbach’s α = .93).
Youth SR (Assessed Pre- and During-Pandemic). Parents completed the 63-item Behavior Rating Inventory of Executive Function Second Edition (BRIEF-2; Gioia et al., 2015) about youth SR skills. The BRIEF-2 is a clinically-validated tool yielding standardized indices in three distinct domains of SR: emotional SR (attention shift, emotional control), behavioral SR (inhibit, self-monitor), and cognitive SR (initiate, working memory, plan/organize, task-monitor, organize materials). Higher scores on each subscale indicate more difficulty with emotional, behavioral, and cognitive SR, respectively (scores >70 are clinically elevated).
Sociodemographics and T1D Characteristics (Assessed Pre-Pandemic)
Parents reported on their own and their child’s age in years, race/ethnicity (per NIH guidelines), and sex; family income, number of people in the home, and family structure. Income to needs ratio (ITNR) was calculated by dividing income by the poverty threshold that year for a household that size. An ITNR of 1.0 indicates a household is living at the poverty level; higher values indicate greater income (Dearing et al., 2001). Parents reported on youth T1D regimen (i.e. use of continuous glucose monitor; insulin injections/pump) and time since diagnosis. For Study 1 only, HbA1C was collected by blood draw in conjunction with the pre-intervention visit.
Statistical Analysis
We conducted mixed effects models to account for within subject correlation due to having repeated measures on the same participant over time. We included time between assessments as a fixed effect to examine change in emotional functioning and T1D self-management measures from pre- to during-pandemic. Intervention condition was defined as intervention versus control for Study 1 participants; all Study 2 participants were given a value of “control” for the purposes of the current analyses. We next conducted mixed effects models to test whether family pandemic-related stress or youth SR (emotional, behavioral, or cognitive) moderated change in each measure. The interaction term indicated whether the degree of change in each measure from pre- to during-pandemic was associated with family pandemic-related stress or youth SR (moderator). We graphed model-predicted patterns of emotional functioning and T1D self-management over time for participants representing the 10th percentile, the median, and the 90th percentile of the moderator variables to visually explore the corresponding response patterns. Alpha levels for significance were set at p < .05; we conducted follow-up tests to explore interactions with p < .10. Finally, we conducted post-hoc analyses to test for any changes in these models when only control participants from Study 1 and Study 2 participants were included.
Results
Table I presents descriptive characteristics for participants who completed questionnaires for the during-pandemic assessment. Participants did not differ on demographic variables from those who did not complete this assessment (Study 1: youth age, sex, and HbA1c; Study 2: youth age and sex, as HbA1c was not collected in Study 2; all p’s > .05).
Table I.
Participant Characteristics (During-Pandemic Assessment)
| Demographic and T1D characteristics | M (SD) or N (%) |
|---|---|
| Youth age (years) (during-pandemic) | 15.3 (2.2); range 10.3–19.1 |
| Youth is female | 46 (52.3%) |
| Youth race/ethnicity | |
| White, Non-Hispanic/Latino(a) | 77 (87.5%) |
| Black, Non-Hispanic/Latino(a) | 4 (4.5%) |
| Other (e.g. Asian/Pacific Islander; Hispanic any race; Biracial) | 6 (6.8%) |
| Do not know/prefer not to answer | 1 (1.1%) |
| Youth pre-pandemic HbA1c (%) | 8.8 (1.3); range 6.8–14.2 |
| Youth uses CGM | 74 (84.1%) |
| Youth uses insulin pump | 69 (78.4%) |
| Time since youth T1D diagnosis (years) | 6.2 (4.0); 1.1–14.9 |
| Parent age (years) (pre-pandemic) | 45.2 (5.4); range 34–59 |
| Parent is female | 78 (88.6%) |
| Parent race/ethnicity | |
| White, Non-Hispanic/Latino(a) | 79 (89.8%) |
| Black, Non-Hispanic/Latino(a) | 5 (5.7%) |
| Other (e.g. Asian/Pacific Islander; Hispanic any race; Biracial) | 3 (3.4%) |
| Do not know/prefer not to answer | 1 (1.1%) |
| Family income-to-needs ratio (pre-pandemic) | 4.3 (2.2); range 0.7–9.4 |
| Single parent (single/never married or separated/divorced) | 9 (10.2%) |
| Moderators | M (SD) |
| COVID-19 pandemic-related family stress | 2.27 (1.01); range 1.00–4.82 |
| Youth BRIEF emotion regulation | 53.5 (9.7); range 40.0–86.0 |
| Youth BRIEF behavior regulation | 49.5 (8.9); range 37.0–82.0 |
| Youth BRIEF cognitive regulation | 53.1 (9.8); range 38.0–81.0 |
Changes from Pre- to During the COVID-19 Pandemic
No change was observed in youth emotional functioning from pre- to during-pandemic. Parents’ diabetes-related distress decreased. Parent-report of youth T1D self-management responsibility (DFRQ) increased, but SCI-R scores did not change (Table II).
Table II.
Emotional Functioning and T1D Self-Management Prior to and During Pandemic
| Pre-pandemic |
During-pandemic |
||||
|---|---|---|---|---|---|
| Construct | M (SD) | N | M (SD) | N | Difference of least squares means (SE); p |
| Youth emotional functioning | |||||
| NIH perceived stress, youth self-report | 2.56 (0.69) | 45 | 2.51 (0.71) | 41 | 0.00 (0.09); .97 |
| NIH perceived stress, parent report on youth | 2.27 (0.60) | 88 | 2.18 (0.67) | 88 | –0.09 (0.06); .13 |
| GAD-7 anxiety, youth self-report | 3.83 (4.38) | 45 | 4.43 (4.63) | 41 | 0.84 (0.69); .23 |
| PAID-T, youth self-report | 32.46 (14.88) | 39 | 31.88 (14.09) | 40 | 1.30 (2.25); .57 |
| Parent emotional functioning | |||||
| DERS, parent self-report | 63.22 (17.53) | 88 | 65.51 (20.26) | 88 | 2.29 (1.56); .14 |
| NIH perceived stress, parent self-report | 2.41 (0.65) | 88 | 2.35 (0.69) | 88 | –0.06 (0.06); .31 |
| P-PAID-T, parent self-report | 68.44 (25.54) | 88 | 62.98 (26.49) | 87 | –5.02 (2.23); .03* |
| Youth T1D self-management | |||||
| SCI-R, youth self-report | 68.98 (12.83) | 45 | 68.07 (14.20) | 41 | –0.94 (2.21); .67 |
| SCI-R, parent report on youth | 66.74 (14.04) | 88 | 65.38 (14.12) | 88 | 1.36 (1.31); .30 |
| DFRQ, parent report on youth | 32.66 (5.89) | 88 | 33.61 (7.07) | 87 | 0.98 (0.44); .03* |
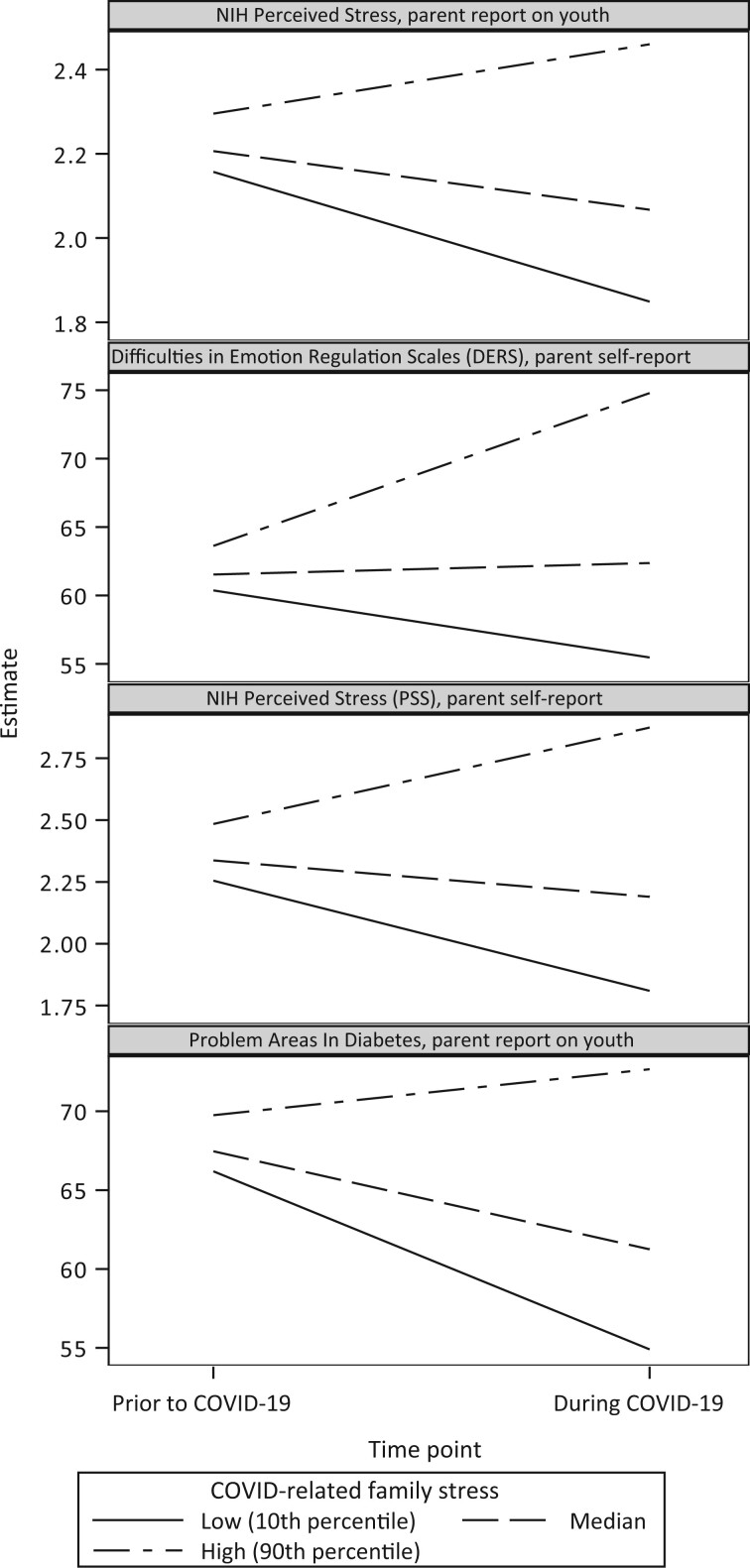
Pandemic-Related Family Stress as Moderator of Change from Pre- to During-Pandemic
Higher pandemic-related family stress was associated with greater declines in emotional functioning from pre- to during-pandemic (Figure 1). Pandemic-related family stress associated with increased parent-reported perceived youth stress (p = .004, pandemic-related family stress × timepoint interaction β = 0.17, 95% CI: 0.06–0.28); and increased parent difficulty with their own emotion regulation (p = .0001, interaction β = 5.74, 95% CI: 2.88–8.60), own perceived stress (p < .0001, interaction β = 0.30, 95% CI: 0.19–0.41), and own diabetes-related distress (p = .02; interaction β = 5.07, 95% CI: 0.79–9.35). Pandemic-related family stress was not a moderator of change in youth-reported constructs. Supplementary Table S1 presents all moderation results.
Figure 1.
Family pandemic-related stress as a moderator of change from pre- to during-pandemic.
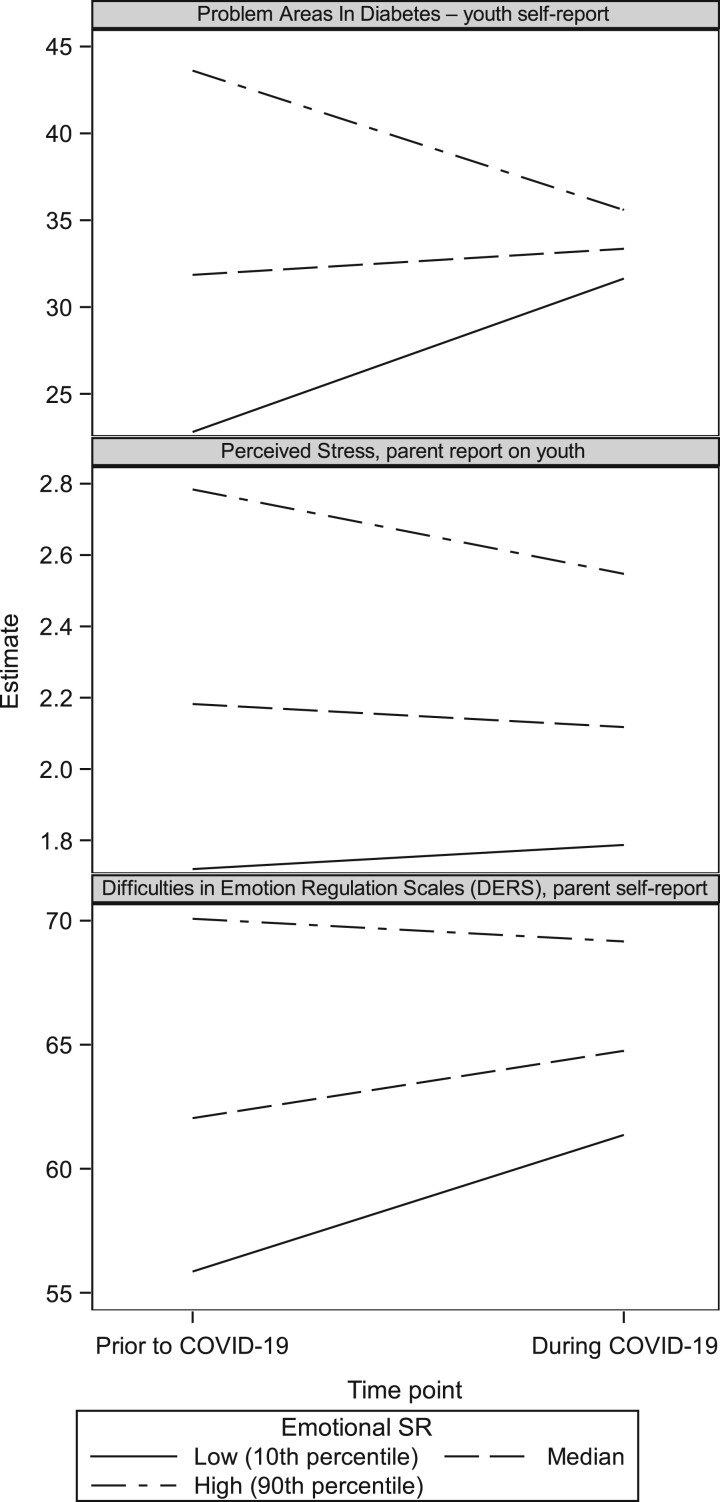
Youth SR as a Moderator of Change from Pre- to During-Pandemic
Emotional SR
Youths’ emotional SR moderated changes in self-reported diabetes-related distress from pre- to during-pandemic (Figure 2). Youth with stronger emotional SR reported decreased diabetes-related distress, whereas those with weaker emotional SR reported increased diabetes-related distress [p = 0.01; SR × timepoint interaction β = –0.73 (95% CI –1.29 to –0.17)]. Youth with stronger emotional SR were reported by parents to show decreased perceived stress, but youth with weaker emotional SR reported to show no change in perceived stress [p < .03; interaction β = –0.01 (95% CI: –0.03 to –0.001)]. Parents of youth with weaker emotional SR reported increased difficulties with their own emotion regulation [DERS; p = .09; interaction β = –0.28 (95% CI: –0.60 to 0.04), whereas parents of youth with stronger emotional SR reported no change.
Figure 2.
Youth emotional self-regulation as a moderator of change from pre- to during-pandemic.
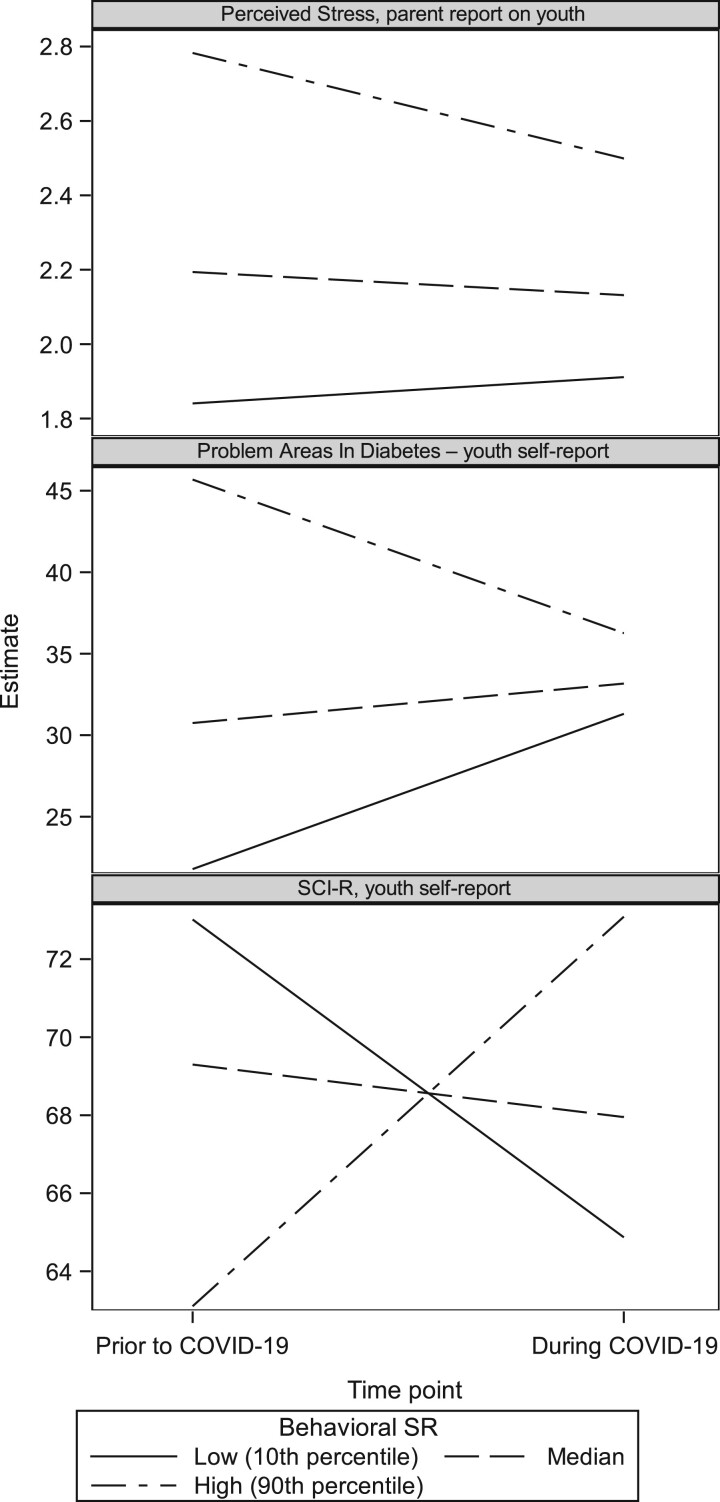
Behavioral SR
Youth with stronger behavioral SR (Figure 3) experienced decreases in parent-reported youth perceived stress from pre- to during-pandemic; perceived stress did not change for youth with weaker behavioral SR [p = .03; SR × timepoint interaction β = –0.01 (95% CI: –0.03 to –0.002). Youth with stronger behavioral SR reported decreased diabetes-related distress, but diabetes distress increased for youth with weaker behavioral SR [p = .007; interaction β = –0.79 (95% CI: –1.34 to –0.23)]. Youth with stronger behavioral SR self-reported increased adherence from pre- to during-pandemic, but adherence decreased for youth with weaker behavioral SR [p = .01; interaction β = 0.76 (95% CI: 0.19–1.32)].
Figure 3.
Youth behavioral self-regulation as a moderator of change from pre- to during-pandemic.
Cognitive SR
No differences were observed based on youth cognitive SR.
Post-Hoc Analyses
In models including only Study 1 control participants and Study 2 participants, we found that emotional SR no longer moderated changes in youth-reported diabetes-related distress. Other moderating relationships remained unchanged after excluding the intervention participants.
Discussion
In this study of emotional functioning and youth T1D self-management across the onset of the COVID-19 pandemic, the level of pandemic-related stress families experienced was associated with decreased emotional functioning, particularly for parents. Critically, youth SR, particularly emotional and behavioral aspects, appeared to protect against worsening youth diabetes distress and regimen adherence across pandemic onset. Findings offer a novel perspective on family and individual factors that may shape emotional functioning and T1D-related outcomes for youth and their parents in the context of a large-scale contextual stressor like the pandemic.
Parent and Youth Emotional Functioning Changes Across Pandemic Onset
Pandemic-related family stress moderated parents’ diabetes-related distress, consistent with prior work finding decreases in diabetes-related distress during lockdown among parents reporting no COVID-19-related worries (Mianowska et al., 2021). Unlike parents, youth did not report much change in emotional functioning overall from pre- to during- pandemic or in relation to family pandemic-related stress, also consistent with a prior study (Goethals et al., 2021). Some youth may have experienced these initial months as a break and/or as more boring than stressful (Janssen et al., 2020). Youth with T1D may have felt less diabetes-related distress at home compared to school; other work also found decreased youth diabetes-related distress during lockdown (Mianowska et al., 2021). It may be that the pandemic-related stressors assessed were more salient for parents than youth (e.g. loss of childcare). Data were collected in summer 2020, when uncertainties around COVID-19 transmission and prevention were high and vaccines were not available. It is thus unsurprising that parents reporting more pandemic-related stress had difficulties in emotional functioning, perhaps due to the unpredictable, uncontrollable nature of the pandemic. Parents may also have experienced emotional distress related to implications of the pandemic in a way that youth did not yet process, given the relative egocentrism of their developmental stage and reduced sense of health risks or mortality (Greene et al., 1996).
T1D Self-Management Changes Across Pandemic Onset
Regardless of family pandemic-related stress experiences, parents reported that youth increased their T1D self-management responsibilities across the pandemic onset. With youth and parents sharing the same space due to altered school and work schedules, there may have been more opportunities for parents to transfer T1D self-management responsibilities to youth, and to feel more able to monitor youth T1D management, resulting in less diabetes distress. The finding that T1D self-management did not change much in relation to family pandemic-related stress was surprising considering anticipated challenges of delaying/shifting T1D care visits or loss of daily T1D supports and structure at school (Plevinsky et al., 2020). Our pandemic-related family stress measure assessed job loss, physical health/health care concerns, and loss of social connections, but not factors directly related to T1D management such as loss of access to diabetes routines and supports, changes in physical activity options, noticing changes in blood glucose patterns, difficulties managing blood glucose excursions, or access to supplies, which have been described as pandemic-related T1D concerns (Joensen et al., 2020). Findings are consistent with other work showing that youth did not change many T1D management behaviors and that blood glucose levels either did not change or improved during pandemic onset (Cheng et al., 2021; O’Donnell et al., 2022). Together, findings suggest families’ diabetes-related distress and youth T1D self-management were largely resilient to pandemic-related stressors.
SR Moderators of Emotional Functioning and T1D Self-Management Changes
Findings suggest youth SR may be an important protective factor, in particular in the context of a major, extended stressor like the COVID-19 pandemic. Results differed by SR domain, suggesting some specificity in SR skills that may promote diabetes resilience in the face of challenge. For example, youth with strong emotional SR, who can control their attention and emotions, reported less diabetes distress and were reported by parents to show less perceived stress across time. Emotional SR skills such as the ability to use distraction or calming strategies may have helped these youth feel less distressed and/or deploy effective coping skills to manage stress (both related to diabetes and not). Parents of these youth also regulated their emotions somewhat better compared to parents of youth with poorer emotional SR, highlighting the connected nature of emotions in families, for example through emotion socialization and stress response modeling pathways (Bariola et al., 2011). Youth who were stronger in behavioral SR, reflecting capacities to self-monitor and inhibit behavior, were similarly reported by parents to show less perceived stress, and self-reported lower diabetes distress and better T1D regimen adherence across pandemic onset compared to those who did not demonstrate such skills. As daily activities shifted during the pandemic, behavioral SR may have helped youth prioritize diabetes management routines and reduced feelings of diabetes-related burdens. Findings are consistent with pre-pandemic studies finding that stronger general SR skills associate with better T1D adherence in youth (Perez et al., 2017) and extend this pattern to the context of a major adversity. In contrast to emotional and behavioral SR, youth cognitive SR did not moderate emotional functioning or T1D self-management changes across the pandemic onset.
Implications
Findings contribute to literature on COVID-19 pandemic impacts on youth mental health (Goethals et al., 2021; Magson et al., 2021) and T1D self-management (Mianowska et al., 2021; O’Donnell et al., 2022). In future work, it will be helpful to detail which aspects of SR are most strongly linked to T1D self-management to identify skills to promote adherence in youth T1D populations. Findings highlight SR as a possibly malleable factor that may protect against adverse impacts of stressors on T1D self-management and diabetes-related distress. In our sample, emotional and behavioral SR emerged as key protective factors during significant societal stress, suggesting they may help youth with T1D demonstrate resilience in the face of major stressors, which is important to understand even outside of the pandemic context (Hilliard et al., 2012). Indeed, SR has been proposed as a novel intervention target in efforts to promote T1D outcomes in youth (Miller et al., 2020; Stanger et al., 2021).
Clinically, findings may have implications for pediatric psychologists seeking to support youth and families managing T1D. It may be that using emotional awareness, mindfulness, and/or relaxation strategies to boost emotional SR, or using structured self-management supports and rewards to improve behavioral SR for these youth during periods of intense stress may be more helpful than using memory cues or organizational strategies to support cognitive SR. The finding that youth SR was associated with parents’ own coping may also be clinically relevant as it highlights the interdependent nature of both SR and T1D management between parent and child; if parents can model effective coping strategies that support youth SR development, youth may in turn more easily take on developmentally appropriate T1D management responsibilities (Berg et al., 2017). Identifying how best to support both youth and parent SR, perhaps by connecting parent and child goal-setting and plans for managing stress as well as T1D tasks may be helpful in developing family-level intervention strategies (Bauer et al., 2020). Pediatric psychologists and mental health professionals on diabetes care teams are ideally situated to support youth with T1D and their parents to strengthen SR and apply those skills to adverse situations, including diabetes-specific challenges and other stressors (Kichler et al., 2015).
Strengths and Limitations
We assessed unique constructs—including SR—in youth with T1D and their parents across pandemic onset. However, we did not include task-based SR assessments, and parents reported on constructs that may not have reflected youth viewpoints. It is also possible that pandemic-related stressors may have affected SR. Although we covaried the intervention condition, about half of Study 1 youth had received an intervention, which may have impacted outcomes. The small sample of youth providing self-reports limits interpretation of results, and limited power may explain some null findings. Although new, the COVID-19 measure had good psychometrics in this and other work on family stress (Bates et al., 2021). We controlled for time elapsed but were unable to standardize length of time between assessments, so some families completed the pre-pandemic assessment months prior to pandemic onset, and others completed it just prior. We captured initial adjustment as families were not followed across the duration of the pandemic. Eligibility requirements for youth HbA1C differed between Studies 1 and 2, so these groups may also have differed regarding T1D management or stress. As in many T1D studies, most of the sample was high income and of White, non-Hispanic race/ethnicity. Thus, findings may not represent or generalize to the more diverse populations most impacted by the pandemic (Kantamneni, 2020) and concurrent societal stressors (e.g. racial and political unrest). Including more diverse samples in T1D studies can allow us to examine SR as a possible protective factor for youth who are experiencing structural, environmental, and geopolitical stressors such as poverty, violence, and racism.
Conclusions
Understanding how individual and family factors shaped responses is instructive as we enter new phases of pandemic coping and prepare for future societal disruptions (e.g. climate disasters, public health crises). Pediatric psychologists can help diabetes providers consider youth strengths—like SR—and exposures to family and societal stressors in their diabetes care.
Supplementary Data
Supplementary data can be found at: https://academic.oup.com/jpepsy.
Funding
This research was funded by the National Institutes of Health (NIH) / Office of Behavioral and Social Sciences Research (OBSSR) / Common Fund UH3HD087979 and UH3HD087979-04S1. Data available on request.
Conflicts of interest: None declared.
Supplementary Material
References
- Alessi J., de Oliveira G. B., Feiden G., Schaan B. D., Telo G. H. (2021). Caring for caregivers: The impact of the COVID-19 pandemic on those responsible for children and adolescents with type 1 diabetes. Scientific Reports, 11(1), 6812. 10.1038/s41598-021-85874-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson B. J., Auslander W. F., Jung K. C., Miller J. P., Santiago J. V. (1990). Assessing family sharing of diabetes responsibilities. Journal of Pediatric Psychology, 15(4), 477–492. 10.1093/jpepsy/15.4.477 [DOI] [PubMed] [Google Scholar]
- Bariola E., Gullone E., Hughes E. K. (2011). Child and adolescent emotion regulation: The role of parental emotion regulation and expression. Clinical Child and Family Psychology Review, 14(2), 198–212. 10.1007/s10567-011-0092-5 [DOI] [PubMed] [Google Scholar]
- Bates C. R., Nicholson L. M., Rea E. M., Hagy H. A., Bohnert A. M. (2021). Life interrupted: Family routines buffer stress during the COVID-19 pandemic. Journal of Child and Family Studies, 30(11), 2641–2651. 10.1007/s10826-021-02063-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer K. W., Hilliard M. E., Albright D., Lo S. L., Fredericks E. M., Miller A. L. (2020). The role of parent self-regulation in youth type 1 diabetes management. Current Diabetes Reports, 20(8), 37–37. 10.1007/s11892-020-01321-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg C. A., Butner J., Wiebe D. J., Lansing A. H., Osborn P., King P. S., Palmer D. L., Butler J. M. (2017). Developmental model of parent-child coordination for self-regulation across childhood and into emerging adulthood: Type 1 diabetes management as an example. Developmental Review: DR, 46, 1–26. 10.1016/j.dr.2017.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner J. C., Mezzacappa E., Beardslee W. R. (2009). Self-regulation and its relations to adaptive functioning in low income youths. The American Journal of Orthopsychiatry, 79(1), 19–30. 10.1037/a0014796 [DOI] [PubMed] [Google Scholar]
- Cheng H. P., Wong J. S. L., Selveindran N. M., Hong J. Y. H. (2021). Impact of COVID-19 lockdown on glycaemic control and lifestyle changes in children and adolescents with type 1 and type 2 diabetes mellitus. Endocrine, 73(3), 499–506. 10.1007/s12020-021-02810-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dearing E., McCartney K., Taylor B. A. (2001). Change in family income-to-needs matters more for children with less. Child Development, 72(6), 1779–1793. 10.1111/1467-8624.00378 [DOI] [PubMed] [Google Scholar]
- Gershon R. C., Wagster M. V., Hendrie H. C., Fox N. A., Cook K. F., Nowinski C. J. (2013). NIH toolbox for assessment of neurological and behavioral function. Neurology, 80(11 Suppl 3), S2–S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gioia G. A., Isquith P. K., Guy S. C., Kenworth L. (2015). Behavior rating inventory of executive function®–Second edition (BRIEF® 2). PAR Publishing. [Google Scholar]
- Goethals E. R., Bergner E. M., Mayberry L. S., Novak L. L., Erfe F., Jaser S. S. (2021). Distressed families demonstrate resilience in the context of COVID-19: Perspectives of adolescents with type 1 diabetes and their mothers. Diabetes Spectrum. Advance online publication. https://doi.org/10.2337/ds21-0026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz K. L., Roemer L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. 10.1023/B:JOBA.0000007455.08539.94 [DOI] [Google Scholar]
- Greene K., Rubin D. L., Hale J. L., Walters L. H. (1996). The utility of understanding adolescent egocentrism in designing health promotion messages. Health Communication, 8(2), 131–152. 10.1207/s15327027hc0802_2 [DOI] [Google Scholar]
- Gregory J. M., Slaughter J. C., Duffus S. H., Smith T. J., LeStourgeon L. M., Jaser S. S., McCoy A. B., Luther J. M., Giovannetti E. R., Boeder S., Pettus J. H., Moore D. J. (2021). COVID-19 severity is tripled in the diabetes community: A prospective analysis of the pandemic’s impact in type 1 and type 2 diabetes. Diabetes Care, 44(2), 526–532. 10.2337/dc20-2260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilliard M. E., Harris M. A., Weissberg-Benchell J. (2012). Diabetes resilience: A model of risk and protection in type 1 diabetes. Current Diabetes Reports, 12(6), 739–748. 10.1007/s11892-012-0314-3 [DOI] [PubMed] [Google Scholar]
- Hilliard M. E., Holmes C. S., Chen R., Maher K., Robinson E., Streisand R. (2013). Disentangling the roles of parental monitoring and family conflict in adolescents’ management of type 1 diabetes. Health Psychology, 32(4), 388–396. 10.1037/a0027811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huth-Bocks A. (2020). COVID-19 family stress screener. University Hospitals Cleveland Medical Center/Society for Research on Child Development. https://commons.srcd.org/HigherLogic/System/DownloadDocumentFile.ashx?DocumentFileKey=4d647e65-0459-4c72-a051-c671d42eb9ab [Google Scholar]
- Janssen L. H. C., Kullberg M.-L. J., Verkuil B., van Zwieten N., Wever M. C. M., van Houtum L. A. E. M., Wentholt W. G. M., Elzinga B. M. (2020). Does the COVID-19 pandemic impact parents’ and adolescents’ well-being? An EMA-study on daily affect and parenting. PLoS One, 15(10), e0240962. 10.1371/journal.pone.0240962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joensen L. E., Madsen K. P., Holm L., Nielsen K. A., Rod M. H., Petersen A. A., Rod N. H., Willaing I. (2020). Diabetes and COVID-19: Psychosocial consequences of the COVID-19 pandemic in people with diabetes in Denmark-what characterizes people with high levels of COVID-19-related worries? Diabetic Medicine: A Journal of the British Diabetic Association, 37(7), 1146–1154. 10.1111/dme.14319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kantamneni N. (2020). The impact of the COVID-19 pandemic on marginalized populations in the United States: A research agenda. Journal of Vocational Behavior, 119(01), 103439. 10.1016/j.jvb.2020.103439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kichler C. J., Harris A. M., Weissberg-Benchell J. (2015). Contemporary roles of the pediatric psychologist in diabetes care. Current Diabetes Reviews, 11(4), 210–221. https://doi.org/http://dx.doi.org/10.2174/1573399811666150421104449 [DOI] [PubMed] [Google Scholar]
- Lansing A. H., Berg C. A. (2014). Topical review: Adolescent self-regulation as a foundation for chronic illness self-management. Journal of Pediatric Psychology, 39(10), 1091–1096. 10.1093/jpepsy/jsu067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackler J. S., Kelleher R. T., Shanahan L., Calkins S. D., Keane S. P., O’Brien M. (2015). Parenting stress, parental reactions, and externalizing behavior from ages 4 to 10. Journal of Marriage and the Family, 77(2), 388–406. 10.1111/jomf.12163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magson N. R., Freeman J. Y. A., Rapee R. M., Richardson C. E., Oar E. L., Fardouly J. (2021). Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. Journal of Youth and Adolescence, 50(1), 44–57. 10.1007/s10964-020-01332-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mianowska B., Fedorczak A., Michalak A., Pokora W., Barańska-Nowicka I., Wilczyńska M., Szadkowska A. (2021). Diabetes related distress in children with type 1 diabetes before and during the COVID-19 lockdown in Spring 2020. International Journal of Environmental Research and Public Health, 18(16), 8527. 10.3390/ijerph18168527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller A. L., Lo S. L., Albright D., Lee J. M., Hunter C. M., Bauer K. W., King R., Clark K. M., Chaudhry K., Kaciroti N., Katz B., Fredericks E. M. (2020). Adolescent interventions to manage self-regulation in type 1 diabetes (AIMS-T1D): Randomized control trial study protocol. BMC Pediatrics, 20(1), 112. 10.1186/s12887-020-2012-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg J. T. (2017). Annual Research Review: On the relations among self-regulation, self-control, executive functioning, effortful control, cognitive control, impulsivity, risk-taking, and inhibition for developmental psychopathology. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 58(4), 361–383. 10.1111/jcpp.12675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novak L. L., Baum H. B. A., Gray M. H., Unertl K. M., Tippey K. G., Simpson C. L., Uskavitch J. R., Anders S. H. (2020). Everyday objects and spaces: How they afford resilience in diabetes routines. Applied Ergonomics, 88, 103185. 10.1016/j.apergo.2020.103185 [DOI] [PubMed] [Google Scholar]
- O’Donnell M. B., Hilliard M. E., Cao V. T., Bradford M. C., Barton K. S., Hurtado S., Duran B., Perez S. G., Rahman K. S., Scott S., Malik F. S., DeSalvo D. J., Pihoker C., Zhou C., Rosenberg A. R., Yi-Frazier J. P. (2022). “It Just Kind of Feels Like a Different World Now”: Stress and resilience for adolescents with type 1 diabetes in the era of COVID-19. Frontiers in Clinical Diabetes and Healthcare, 3, 49–50. 10.3389/fcdhc.2022.835739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez K. M., Patel N. J., Lord J. H., Savin K. L., Monzon A. D., Whittemore R., Jaser S. S. (2017). Executive function in adolescents with type 1 diabetes: Relationship to adherence, glycemic control, and psychosocial outcomes. Journal of Pediatric Psychology, 42(6), 636–646. 10.1093/jpepsy/jsw093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plevinsky J. M., Young M. A., Carmody J. K., Durkin L. K., Gamwell K. L., Klages K. L., Ghosh S., Hommel K. A. (2020). The impact of COVID-19 on pediatric adherence and self-management. Journal of Pediatric Psychology, 45(9), 977–982. 10.1093/jpepsy/jsaa079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott E. S., Jenkins A. J., Fulcher G. R. (2020). Challenges of diabetes management during the COVID-19 pandemic. The Medical Journal of Australia, 213(2), 56–57.e51. 10.5694/mja2.50665 [DOI] [PubMed] [Google Scholar]
- Shapiro J. B., Vesco A. T., Weil L. E. G., Evans M. A., Hood K. K., Weissberg-Benchell J. (2018). Psychometric properties of the problem areas in diabetes: Teen and parent of teen versions. Journal of Pediatric Psychology, 43(5), 561–571. 10.1093/jpepsy/jsx146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R. L., Kroenke K., Williams J. B. W., Löwe B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Stanger C., Kowatsch T., Xie H., Nahum-Shani I., Lim-Liberty F., Anderson M., Santhanam P., Kaden S., Rosenberg B. (2021). A digital health intervention (SweetGoals) for young adults with type 1 diabetes: Protocol for a factorial randomized trial. JMIR Research Protocols, 10(2), e27109. 10.2196/27109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaid E., Lansing A. H., Stanger C. (2018). Problems with self-regulation, family conflict, and glycemic control in adolescents experiencing challenges with managing type 1 diabetes. Journal of Pediatric Psychology, 43(5), 525–533. 10.1093/jpepsy/jsx134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinger K., Butler H. A., Welch G. W. L., Greca A. M. (2005). Measuring diabetes self-care: A psychometric analysis of the Self-Care Inventory-Revised with adults. Diabetes Care, 28(6), 1346–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissberg-Benchell J., Antisdel-Lomaglio J. (2011). Diabetes-specific emotional distress among adolescents: Feasibility, reliability, and validity of the problem areas in diabetes-teen version. Pediatric Diabetes, 12(4 Pt 1), 341–344. 10.1111/j.1399-5448.2010.00720.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.