Abstract
Background
Prior estimates of the years of life lost (YLLs) in the USA associated with coronavirus disease 2019 (COVID-19) were 1.2 million through 11 July 2020 and 3.9 million through 31 January 2021 (which roughly coincides with the first full year of the pandemic). The aim of this study is to update YLL estimates through the first 2 years of the pandemic.
Methods
We employed data regarding COVID-19 deaths through 5 February 2022 by jurisdiction, gender and age group. We used actuarial life expectancy tables by gender and age to estimate YLLs.
Results
We estimated roughly 9.7 million YLLs due to COVID-19 deaths. The number of YLLs per 10 000 capita was 297.5, with the highest rate in Mississippi (482.7) and the lowest in Vermont (61.4). There was substantial interstate variation in the timing of YLLs and differences in YLLs by gender. YLLs per death increased from 9.2 in the first year of the pandemic to 10.8 through the first 2 years.
Conclusions
Our findings improve our understanding of how the mortality effects of COVID-19 have evolved. This insight can be valuable to public health officials as the disease moves to an endemic phase.
Keywords: COVID-19, infectious disease, mortality
Introduction
Years of life lost (YLLs) is a population-level measure that aggregates across individuals the life expectancy less the age at which they died. It conveys additional information beyond the number of deaths by reflecting the age distribution of decedents. The measure has been used to analyze a range of causes of death1–9 and has recently been applied to deaths due to coronavirus disease 2019 (COVID-19).10–18
This original article follows previous studies by the authors,19,20 which estimated 1.2 million YLLs associated with COVID-19 deaths in the USA through 11 July 2020 and 3.9 million through 31 January 2021. This study updates the prior estimates through the roughly second year of the pandemic and analyzes overall YLLs and YLLs by jurisdiction and gender.
Methods
Data
The data and methods employed follow those used in Quast et al.19 Data regarding COVID-19 deaths were obtained from the dataset ‘Provisional COVID-19 Death Counts by Sex, Age, and State’ published by the National Center for Health Statistics in the US Centers for Disease Control and Prevention (CDC).21 The data reflect the period 1 January 2020 through 5 February 2022 and were obtained on 3 March 2022. We again use the term jurisdiction rather than state to refer the geographic entities as the CDC data included observations for the non-state areas New York City and Washington, D.C. The number of deaths was suppressed in the dataset for a given jurisdiction/gender/age group due to confidentiality concerns if the value ranged from one to nine. Out of 401 533 female deaths, 365 did not include information regarding age. The corresponding values for male deaths was 497 166 and 339. The suppressed deaths were excluded from the analysis.
Life expectancies by age and gender were obtained from actuarial life tables published by the US Social Security Administration.22 The most recent year available was 2019. Appendix Table 1 reports the mapping of age groups used in the COVID-19 deaths data to ages for which the life expectancy was used. The table also reports the approximated life expectancy reported for the specified age.
We again used ‘Annual State Resident Population Estimates’ published by the US Census Bureau as the source of our state-level population data.23 The data were as of 1 July 2019 and were obtained by gender. In order to match the COVID-19 deaths data, we estimated the population of New York City and the remainder of New York state separately. We obtained the population of New York City and the percentage of population by gender as of 1 July 2019 from ‘QuickFacts: New York City, New York’ published by the US Census Bureau.24
Our sample consisted of 52 jurisdictions: 49 states, New York state excluding New York City, New York City and Washington, D.C.
Statistical analysis
As in our previous studies,19,20 we approximated the age of death for each age group based on the single-age values reported in Appendix Table 1. For each death, we assigned a life expectancy for that gender-age cohort. We obtained population-level YLL estimates by summing the life expectancies for the deaths in the relevant population. Per-capita YLLs were calculated per 10 000 residents for the respective jurisdiction-gender population.
We again adjusted our estimates to account for COVID-19 deaths occurring among individuals had significant medical conditions before contracting the disease. A study of deaths in the UK estimated that pre-existing morbidities reduced the estimated YLLs per COVID-19 death from 14 to 13 among men and 12 to 11 among women.14 We followed our earlier methodology and conservatively reduced the expected life expectancy by 25% to reflect the typically greater morbidity of COVID-19 decedents.
Results
Table 1 reports by jurisdiction the number of deaths and YLLs, both the actual values and those measured per 10 000 capita. The jurisdictions are ranked in decreasing order by YLLs per 10 000 capita. Nationally, the roughly 900 000 deaths resulted in nearly 9.7 million YLLs. The YLLs per 10 000 capita were 297.5 and the average YLLs per COVID-19 death was 10.8. Mississippi had the highest YLLs per 10 000 capita at 482.7, which was nearly eight times the lowest state value that was observed in Vermont.
Table 1.
Number of deaths and YLLs by jurisdiction
| Number of deaths | YLLs | ||||
|---|---|---|---|---|---|
| Jurisdiction | Number | Per 10 000 capita | Number | Per 10 000 capita | YLLs per death |
| USA | 897 995 | 27.7 | 9 655 279 | 297.5 | 10.8 |
| Mississippi | 11 854 | 40.3 | 141 928 | 482.7 | 12.0 |
| New York City | 33 846 | 40.6 | 356 162 | 427.2 | 10.5 |
| Alabama | 17 198 | 35.5 | 204 415 | 421.8 | 11.9 |
| New Mexico | 6760 | 32.6 | 85 771 | 413.6 | 12.7 |
| Arizona | 24 983 | 34.7 | 294 331 | 409.0 | 11.8 |
| Tennessee | 23 129 | 34.3 | 269 971 | 400.0 | 11.7 |
| Oklahoma | 13 745 | 35.2 | 153 894 | 393.7 | 11.2 |
| Nevada | 9811 | 32.2 | 117 462 | 385.8 | 12.0 |
| Arkansas | 9946 | 33.4 | 110 210 | 369.7 | 11.1 |
| Louisiana | 14 393 | 31.4 | 168 527 | 367.1 | 11.7 |
| Texas | 82 757 | 28.9 | 1 046 304 | 365.6 | 12.6 |
| New Jersey | 30 285 | 34.5 | 298 702 | 340.1 | 9.9 |
| Kentucky | 13 885 | 31.5 | 150 119 | 340.1 | 10.8 |
| Georgia | 29 073 | 27.7 | 351 398 | 335.0 | 12.1 |
| West Virginia | 5568 | 31.4 | 59 204 | 333.7 | 10.6 |
| South Carolina | 15 083 | 29.6 | 168 655 | 331.2 | 11.2 |
| Florida | 63 486 | 29.9 | 700 467 | 329.5 | 11.0 |
| Ohio | 38 490 | 33.3 | 378 408 | 327.5 | 9.8 |
| Pennsylvania | 42 761 | 33.8 | 397 122 | 313.5 | 9.3 |
| Indiana | 21 081 | 31.7 | 208 441 | 313.4 | 9.9 |
| Missouri | 18 341 | 30.2 | 189 245 | 312.0 | 10.3 |
| Michigan | 29 380 | 29.7 | 308 090 | 311.9 | 10.5 |
| Montana | 3184 | 30.1 | 32 597 | 308.4 | 10.2 |
| District of Columbia | 1686 | 24.2 | 21 118 | 303.3 | 12.5 |
| North Dakota | 2445 | 32.5 | 22 426 | 298.4 | 9.2 |
| South Dakota | 2768 | 31.7 | 25 690 | 294.4 | 9.3 |
| New York (excl NYC) | 33 824 | 31.1 | 311 109 | 285.6 | 9.2 |
| Kansas | 8078 | 28.1 | 80 910 | 281.1 | 10.0 |
| Wyoming | 1488 | 26.0 | 15 629 | 273.1 | 10.5 |
| Idaho | 4508 | 25.5 | 45 293 | 256.6 | 10.0 |
| Illinois | 31 800 | 25.4 | 319 911 | 255.4 | 10.1 |
| Iowa | 8845 | 28.4 | 79 449 | 254.9 | 9.0 |
| North Carolina | 23 978 | 23.1 | 262 936 | 253.6 | 11.0 |
| Delaware | 2559 | 26.6 | 24 320 | 252.5 | 9.5 |
| California | 85 519 | 21.9 | 979 034 | 250.7 | 11.4 |
| Rhode Island | 3243 | 30.9 | 26 145 | 249.3 | 8.1 |
| Maryland | 14 270 | 23.9 | 147 280 | 246.5 | 10.3 |
| Connecticut | 10 002 | 28.3 | 85 056 | 240.9 | 8.5 |
| Wisconsin | 13 559 | 23.5 | 128 367 | 222.9 | 9.5 |
| Nebraska | 4370 | 22.9 | 42 411 | 222.1 | 9.7 |
| Colorado | 11 917 | 20.9 | 124 648 | 218.9 | 10.5 |
| Virginia | 17 152 | 20.3 | 175 662 | 208.2 | 10.2 |
| Massachusetts | 17 053 | 25.0 | 139 617 | 204.7 | 8.2 |
| Alaska | 1089 | 15.1 | 14 188 | 196.6 | 13.0 |
| Minnesota | 11 780 | 21.1 | 106 228 | 190.7 | 9.0 |
| Utah | 4430 | 14.0 | 53 138 | 168.3 | 12.0 |
| Oregon | 6094 | 14.6 | 64 240 | 153.9 | 10.5 |
| Washington | 10 476 | 13.9 | 112 554 | 149.5 | 10.7 |
| Maine | 2143 | 16.1 | 19 835 | 148.9 | 9.3 |
| New Hampshire | 2250 | 16.7 | 18 607 | 138.1 | 8.3 |
| Hawaii | 1149 | 8.2 | 14 260 | 101.9 | 12.4 |
| Vermont | 481 | 7.8 | 3795 | 61.4 | 7.9 |
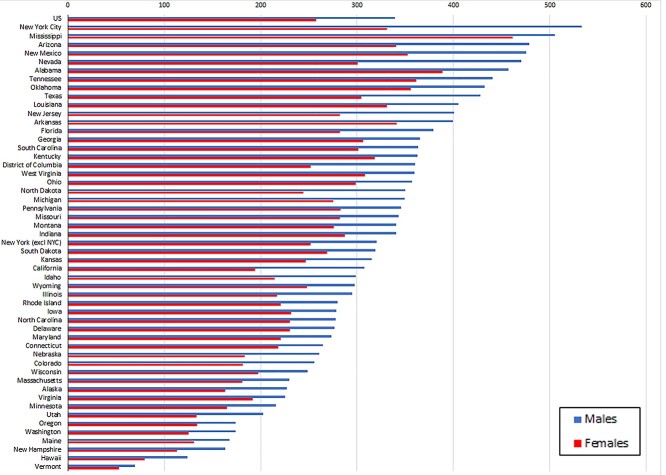
Figure 1 shows that in every jurisdiction the YLLs per 10 000 capita were higher for males than for females. However, the extent of the difference varies substantially. The male value for New York City was approximately 60% greater than the female value, whereas in Mississippi that value was only 9% greater.
Fig. 1.
YLLs per 10 000 capita by jurisdiction and gender.
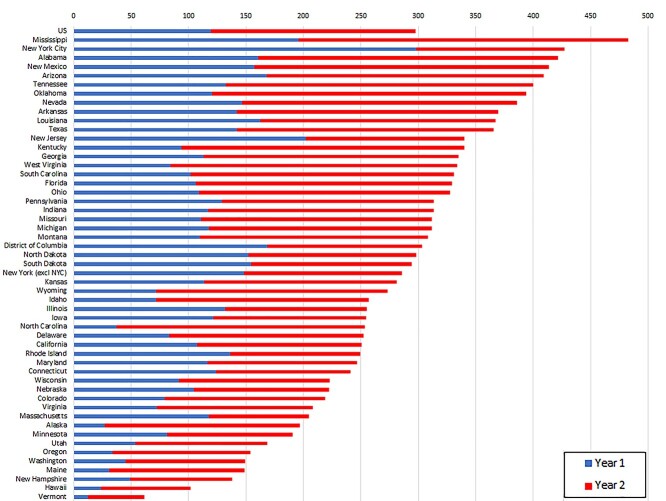
Figure 2 details YLLs per 10 000 capita where the Year 1 value is shaded in blue and the Year 2 value is shaded in red. Nationally, the YLLs per capita in Year 1 were 119.0, whereas the Year 2 amount was 178.5. There was substantial variation across states in the proportion of YLLs by year. For example, Mississippi had a large proportion of YLLs in Year 2, whereas New York City had a much lower proportion. Of North Carolina’s relatively low number of YLLs across the 2 years, a large proportion of them occurred in Year 2.
Fig. 2.
YLLs per 10 000 capita by jurisdiction and year.
Conclusions/Discussion
The main findings
Over the first 2 years of the pandemic, COVID-19 deaths in the USA were associated with approximately 9.7 million YLLs. On average, each death was associated with roughly 10.8 YLLs. There were substantial differences across states both in the number and timing of YLLs. Half of the top 10 states in terms of YLLs were in the southeast USA (Mississippi, Alabama, Tennessee, Arkansas and Louisiana). YLLs per 10 000 capita were higher for males than females, but there was substantial interstate variation in the extent of difference.
What is already known on this topic
Prior multi-national analyses have generally found that YLLs in the USA were generally higher than in other countries. Per-capita YLLs in the USA were found to be 13% higher than in Italy and more than six times as large as those in Germany.10 An analysis of 81 countries through 2020 found that the ratio of YLLs associated with COVID-19 relative to other major causes in the USA was second only to Italy.18 Another study of thirty countries through the summer of 2020 estimated that the YLLs per capita in the USA were the eighth highest.12 In contrast, a study that employed the standardized mortality ratio found that the YLLs per capita in the UK and the USA were similar.11
Our earlier studies of the USA estimated YLLs associated with COVID-19 to have been roughly 1.2 m through 11 July 2020 and 4 million through January 2021.19,20 A microsimulation analysis of the USA estimated roughly 9 million YLLs through March 2021.15 However, this estimate was based on all excess deaths and not solely on COVID-19 deaths. Several analyses of the USA have observed disproportionate YLLs among Hispanics and Blacks, both at the national13,15 and regional17 levels.
What this study adds
The use of consistent data and methodology implies that our two prior studies and the current study provide insight into the evolution of YLLs associated with COVID-19 in the USA. For instance, although the number of COVID-19 deaths increased by roughly 13% from Year 1 to Year 2 of the pandemic, YLLs increased by 49%. YLLs per death increased from 9.2 in the first year of the pandemic to 10.8 through the first 2 years. Taken together, these results suggest a shift to a younger age distribution in COVID-19 deaths. Our findings also highlight geographic variation in the timing of COVID deaths as well as the persistence of male YLLs exceeding female YLLs. As COVID-19 enters an endemic phase, these results will be important to monitor to best shape public health efforts.
Limitations
This study shares several limitations with our previous analyis.15 We were unable to investigate YLLs by race and ethnicity. The COVID-19 deaths data were provisional in that there can be delays in the reporting of deaths, but the impact of these delays were likely negligible given the 2-year analytic period. Data regarding 713 deaths were suppressed due to confidentiality concerns, but the effect of these missing data were likely minimal given the nearly 900 000 total COVID-19 deaths.
We relied on national (rather than jurisdiction-level) life expectancy estimates and the estimates are conditional upon an individual reaching the specified age. We had to employ a rough approximation for the pre-existing reduced expected life expectancy of those who died from COVID-19. Although our use of a 25% reduction is conservative, especially in light of earlier estimates,15 a more precise estimate based on US data would provide greater clarity.
Conclusions
Our estimates illustrate the continuing toll of COVID-19 and the extent to which the disease is cutting lives short. Taken together with our earlier analyses, this study demonstrates the persistent variation in the mortality effects across geographies and genders and suggests the effectiveness of nuanced public health responses.
Supplementary Material
Troy Quast, Professor
Ross Andel, Professor
Sean Gregory, Research Affiliate
Eric A. Storch, Professor
Contributor Information
Troy Quast, University of South Florida, College of Public Health, Tampa, FL 33612, USA.
Ross Andel, University of South Florida, College of Behavioral and Community Sciences, School of Aging Studies, Tampa, FL 33620, USA; Charles University and Motol University Hospital, Department of Neurology, Prague, Czechia; International Clinical Research Center, St. Anne’s University Hospital, Brno, Czechia.
Sean Gregory, Department of Psychiatry & Behavioral Sciences, Baylor College of Medicine, Houston, TX 77030, USA.
Eric A Storch, Department of Psychiatry & Behavioral Sciences, Baylor College of Medicine, Houston, TX 77030, USA.
References
- 1. Vienonen MA, Jousilahti PJ, Mackiewicz K et al. Preventable premature deaths (PYLL) in Northern Dimension partnership countries 2003–13. Eur J Public Health 2019;29(4):626–30. 10.1093/eurpub/cky278. [DOI] [PubMed] [Google Scholar]
- 2. Shavelle RM, Paculdo DR, Kush SJ et al. Life expectancy and years of life lost in chronic obstructive pulmonary disease: findings from the NHANES III Follow-up Study. Int J Chron Obstruct Pulmon Dis 2009;4:137–48. 10.2147/copd.s5237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Martinez R, Soliz P, Caixeta R, Ordunez P. Reflection on modern methods: years of life lost due to premature mortality—a versatile and comprehensive measure for monitoring non-communicable disease mortality. Int J Epidemiol 2019;48(4):1367–76. 10.1093/ije/dyy254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vries E de, Meneses MX, Piñeros M. Years of life lost as a measure of cancer burden in Colombia, 1997-2012. Biomedica 2016;36(4):547–555. 10.7705/biomedica.v36i4.3207. [DOI] [PubMed] [Google Scholar]
- 5. Alva ML, Hoerger TJ, Zhang P, Cheng YJ. State-level diabetes-attributable mortality and years of life lost in the United States. Ann Epidemiol 2018;28(11):790–5. 10.1016/j.annepidem.2018.08.015. [DOI] [PubMed] [Google Scholar]
- 6. Imtiaz S, Shield KD, Roerecke M et al. The burden of disease attributable to cannabis use in Canada in 2012. Addiction 2016;111(4):653–62. 10.1111/add.13237. [DOI] [PubMed] [Google Scholar]
- 7. Salazar A, Moreno S, Sola HD et al. The evolution of opioid-related mortality and potential years of life lost in Spain from 2008 to 2017: differences between Spain and the United States. Curr Med Res Opin 2020;36(2):285–91. 10.1080/03007995.2019.1684251. [DOI] [PubMed] [Google Scholar]
- 8. Jung Y-S, Kim K-B, Yoon S-J. Factors associated with regional years of life lost (YLLs) due to suicide in South Korea. IJERPH 2020;17(14):4961. 10.3390/ijerph17144961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Izadi N, Mirtorabi SD, Najafi F et al. Trend of years of life lost due to suicide in Iran (2006–2015). Int J Public Health 2018;63(8):993–1000. 10.1007/s00038-018-1151-1. [DOI] [PubMed] [Google Scholar]
- 10. Mitra AK, Payton M, Kabir N et al. Potential years of life lost due to COVID-19 in the United States, Italy, and Germany: an old formula with newer ideas. IJERPH 2020;17(12):4392. 10.3390/ijerph17124392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Briggs AH, Goldstein DA, Kirwin E, et al. Estimating (quality-adjusted) life-year losses associated with deaths: with application to COVID-19. Health Econ 2021;30(3):699–707. 10.1002/hec.4208. [DOI] [PubMed] [Google Scholar]
- 12. Oh I-H, Ock M, Jang SY et al. Years of life lost attributable to COVID-19 in high-incidence countries. J Korean Med Sci 2020;35(32):e300–e310. 10.3346/jkms.2020.35.e300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bassett MT, Chen JT, Krieger N. Variation in racial/ethnic disparities in COVID-19 mortality by age in the United States: a cross-sectional study. Tsai AC, editor. PLoS Med 2020;17(10):e1003402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hanlon P, Chadwick F, Shah A et al. COVID-19 – exploring the implications of long-term condition type and extent of multimorbidity on years of life lost: a modelling study. Wellcome Open Res 2020;5:75. 10.12688/wellcomeopenres.15849.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Reif J, Heun-Johnson H, Tysinger B, Lakdawalla D. Measuring the COVID-19 mortality burden in the United States: a microsimulation study. Ann Intern Med 2021;174(12):1700–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Vieira A, Ricoca VP, Aguiar P et al. Years of life lost by COVID-19 in Portugal and comparison with other European countries in 2020. BMC Public Health 2021;21(1):1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lilly D, Akintorin S, Unruh LH et al. Years of potential life lost secondary to COVID-19: Cook County. Illinois Ann Epidemiol 2021;58:124–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pifarré i Arolas H, Acosta E, López-Casasnovas G et al. Years of life lost to COVID-19 in 81 countries. Sci Rep Nat Publishing Group 2021;11(1):3504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Quast T, Andel R, Gregory S, Storch EA. Years of life lost associated with COVID-19 deaths in the United States. J Public Health (Oxf). 10.1093/pubmed/fdaa159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Quast T, Andel R, Gregory S, Storch EA. Years of life lost associated with COVID-19 deaths in the USA during the first year of the pandemic. J Public Health 2021:e20–e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. U.S. Centers for Disease Control and Prevention . Provisional COVID-19 Death Counts by Sex, Age, and State. 2020. Jul 22. https://data.cdc.gov/NCHS/Provisional-COVID-19-Death-Counts-by-Sex-Age-and-S/9bhg-hcku
- 22. U.S. Social Security Administration . Actuarial Life Table. [undated] https://www.ssa.gov/oact/STATS/table4c6.html (3 March 2022, date last accessed).
- 23. U.S. Census Bureau . State Population by Characteristics: 2010–2019. https://www.census.gov/data/tables/time-series/demo/popest/2010s-state-detail.html#par_textimage_673542126 (13 February 2022, date last accessed).
- 24. U.S. Census Bureau . QuickFacts: New York City, New York. https://www.census.gov/quickfacts/newyorkcitynewyork (1 March 2022, date last accessed).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.