Abstract
This qualitative study documents and analyzes COVID-19’s impacts on burn care in twelve nations. Burn care saw valuable improvements in surgical techniques, skin grafting, and other acute treatments during the decades before the COVID-19 pandemic which increased severely burned patients’ survival rates and quality of life. Detailed interviews, conducted in the 12 nations reveal that the COVID-19 pandemic greatly affected the delivery of acute and rehabilitation services for burn patients. Resources have been suctioned away from non-COVID healthcare and burn care has not been spared. Acute, post-acute rehabilitation, and mental health services have all suffered. Weak preparation has deeply burdened health care services in most nations, resulting in lower access to care. Access problems have accelerated innovations like telehealth in many nations. The spread of misinformation through social and traditional media has contributed to the varied responses to COVID-19. This compounded problems in health care delivery. Burn care providers delivered services for survivors during extremely difficult circumstances by continuing to furnish acute and long-term services for patients with complex disease. Emphasis on future pandemic preparedness will be vital because they undermine all aspects of burn care and patient outcomes. As the COVID-19 pandemic continues to unfold around the world, it will be important to continue to monitor and analyze the adaptability of nations, health care systems, and burn care providers.
Over the last 30 years, the focus of burn care has shifted to an emphasis on the acute period following traumatic injury and the early period of rehabilitation care and related services.1,2 While these improvements have not been implemented at the same pace globally, these changes have helped to decrease morbidity and mortality.3–5 A previous analysis of acute and rehabilitation burn care in twelve nations—Australia, Canada, Chile, Egypt, Germany, India, Israel, Japan, Mexico, Taiwan, the United Kingdom, and the United States—revealed that most lack the infrastructure needed to deliver appropriate rehabilitation and mental health care after discharge from hospital, especially those in rural areas.6
Since the onset of COVID-19, burn care has been among the many medical services complicated by the evolving global COVID-19 pandemic. Differences in burn patterns, access to acute and post-acute care, and resources pre-dated COVID-19. Acute burn care is resource intensive, requiring highly specialized skills, personnel, supplies, and other resources which many nations lack.6 As resources became scarce with the onset of COVID-19, this disparity grew.7
The pandemic caused reallocation of medical resources in most countries. These changes left acute inpatient burn units (Throughout this paper, we refer to burn units as sites of inpatient, typically acute, burn care; we refer to burn clinics as sites of outpatient burn care.) short on hospital beds, staff, and treatment modalities.8–10 In some nations, government health officials urged hospitals to prepare for COVID-19 surges; but many hospitals were unable to develop effective plans in advance that considered sufficient reserves of caregivers, equipment, or supplies. COVID-19 meant fewer available ICU beds and fewer providers for non-COVID-19 patients. Restructuring of hospital units and reallocation of caregivers across institutions presented new challenges to caring for patients, including burn1* patients.11,12 As numbers of patients critically ill with COVID-19 grew, intensive care units (ICUs) quickly became saturated.13,14 ICUs filled and many hospitals deferred or canceled elective surgeries.15,16
Long-term physical rehabilitation and wound care follow-up are essential to improving quality of life for burn survivors. If they are disrupted, survivors risk durable harm.17,18 Prior to COVID-19, a substantial share of burn rehabilitation patients suffered from care discontinuities and did not receive sufficient follow-up care.6,19 Continuity of post-acute services was further disrupted by COVID-related stay-at-home orders and closures of outpatient facilities.
Compounding this, many patients feared infection and ultimately refused admission to inpatient rehabilitation or visits to outpatient centers that remained open throughout the pandemic.20 Telehealth became a much more important source of post-acute and rehabilitation burn services in some nations.21 Ability to transition to virtual outpatient care successfully and quickly depended on infrastructure and resources available in each country.
COVID-19 has been associated with changes in burn patterns. In the United Kingdom, the reported incidence of adult burns fell in 2020 but burns were substantially more serious. Mean total body surface area (TBSA) burned was 4.3% in 2020 versus 1.8% in 2019.22 In Tokyo, incidence of flame burns, inhalation injuries, and full-thickness burns all rose.23 One study of nine Level I pediatric trauma centers in the United States found that incidence of pediatric burns rose 48.6% in 2020 compared to 2019.24 Researchers cite stay-at-home orders as a possible explanation for this increase. This increase in burns overall during COVID-19, in combination with reduced resources to treat burn patients, resulted in unmet burn care needs in many nations.25,26
Continuity of care for these patients depended in part on the concentration of units and clinics specialized in burn treatment in each area. For example, in the Tokyo metropolitan area, there are approximately fifteen burn units; in Israel, there are five.23,27 In Japan, if a unit or two closes or is reallocated for COVID-19 care, the care infrastructure remains in place for burn patients within that urban setting. On the other hand, in Israel, where there are fewer burn units, if one closes it can severely impact the patients in that catchment area as they may need to travel to other regions of the country for care.
STUDY FRAMEWORK
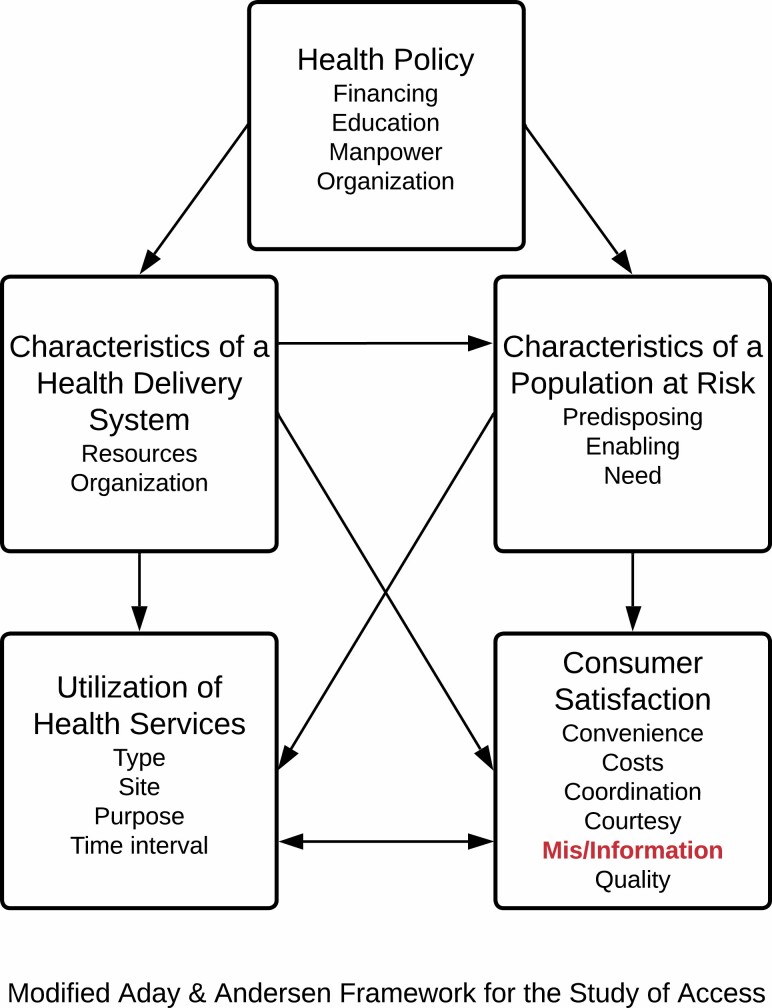
We frame this study with a modified version of the Aday and Andersen model of access to care (Figure 1). This model’s five components are health policy, characteristics of a health delivery system, characteristics of a population at risk, utilization of health services, and patient satisfaction.28,29 We have added “misinformation” to this model because the rapid spread of misinformation has contributed to the global pandemic response and may have heightened patient reluctance to obtain care. In burn treatment specifically, misinformation may have contributed to poor compliance by patients for follow-up care. Other aspects of national health policy, health care delivery, and patient satisfaction with burn care may have been undermined because of distorted information.30–32
Figure 1.
The Aday and Andersen model is comprised of five components: health policy, characteristics of a health delivery system, characteristics of a population at risk, utilization of health services, and patient satisfaction.28,29 We have added “misinformation” to this model because the rapid spread of misinformation has contributed to the global pandemic response and may have heightened patient reluctance to obtain care.
This paper aims to examine the effects of the pandemic on acute burn care and rehabilitation in twelve countries from the vantage point of leading clinicians in these fields.
METHODS
Relying on interviews with burn clinicians in twelve nations, we assess COVID-19’s impacts on acute and post-acute burn care, and on caregivers and patients. We evaluate pandemic preparedness, ability to sustain acute burn care, ability to sustain continuity of post-acute burn care through rehabilitation, mental health of clinicians and patients, changes in access, and perceptions of misinformation’s effects on healthcare and the pandemic.
Qualitative data were collected via semi-structured interviews with burn clinicians and rehabilitation specialists in twelve countries across six continents between July 2020 and January 2021 (Table 2). During these seven months, the pandemic evolved rapidly, and it has continued to do so. When data collection began, much of the world was under stay-at-home orders. In November of 2020, vaccine development was rapidly progressing. By the last interview, in January 2021, several vaccines had been approved and inoculations were beginning. Each interview is a snapshot of each participant’s experience during that time.
Table 2:
Interview questions
| Questions | Probes |
|---|---|
| How has COVID-19 affected healthcare workers (burn surgeons, rehabilitation physicians, etc.) in your hospital/facility? | • Has your hospital/facility started accepting COVID-19patients? • Are burn surgeons treating COVID-19 patients? In addition to their typical patients? • Is your hospital treating any non-COVID-19 patients? • Do healthcare workers in your hospital/facility have access to adequate Personal Protective Equipment? • What measures is your hospital/facility taking to protect healthcare workers? |
| To what extent, if any, has COVID-19 affected the structure of the burn-specific units in your hospital or clinic? |
• Are there fewer beds reserved specifically for burn patients? • What specific concerns do you or your colleagues have regarding burn care in the hospital? • In rehabilitation centers? • At home after patients are discharged? |
| Have you seen any change in the number of burn patients in your hospital/facility since the COVID-19 outbreak in your area? |
• If you have seen a change in the number of burn patients, why do you think that is? |
| Overall, how well do you feel your hospital/facility is caring for patients hospitalized or in rehabilitation for conditions unrelated to COVID-19? |
• ForCOVID-19? |
| How are burn patients who are quarantined in their homes because of COVID-19 able to access care and treatment? |
• How are patients who require critical burn carereceiving treatment? |
| Is there anything else that you would like to share with us regardingCOVID-19? |
The interview guide was informed by literature reviews, reviews of international burn guidelines,33 data on the effects of COVID-19 in twelve countries, discussions with burn clinicians and researchers during visits to each hospital location prior to the pandemic by the third (R.T.) and last author (L.E.K.), and follow-up via e-mail and Zoom conversations with those burn clinicians and researchers. Questions and probes aimed to understand: 1) the depth of the impact of COVID-19 on sustaining hospital operations and treatment of patients; 2) the mental health impact on providers and their patients; 3) continuity of care in the post-acute setting; and 4) rehabilitation services. All interviews were conducted over the Zoom platform.
Verbal informed consent was obtained at the beginning of each interview. Each interview was audio and video recorded via Zoom and transcribed verbatim.
These nations’ responses to the pandemic are modulated by economic, political, and social factors. We describe the pandemic’s effects on burn care by both highlighting the similarities across nations and by identifying salient differences. This sample is heterogeneous; as noted, timing of interviews necessarily varied. Table 1 provides context in this regard,including the country, date of interview, the stage of the pandemic (i.e., first wave, second wave, etc.) and lockdown intensity (i.e., stay-at-home orders, border shutdowns).
Table 1.
Stage of pandemic at time of interview
| Country | Date of Interview | Stage of Pandemic at Time of Interview | Lockdown Restrictions |
|---|---|---|---|
| Australia | Interview 1: July16, 2020 |
Surge | Australian borders closed to all nonresidents; most states and territories under lockdown |
| Interview 2: July21, 2020 |
Surge | Australian borders closed to all nonresidents; most states and territories under lockdown |
|
| Interview 3: August4, 2020 |
Surge | State of Disaster declared in Victoria | |
| Canada | January 13, 2021 | Stable | Under lockdown and border restrictions |
| Chile | September 23, 2020 | Cases decreasing | Easing lockdown restrictions, under nightly curfew |
| Egypt | October 7, 2020 | Cases decreasing | Easing lockdown restrictions |
| Germany | August 12, 2020 | Surge | Lockdown lifted, but large gatherings banned |
| India | October 3, 2020 | Surge | Lockdown imposed |
| Israel | October 22, 2020 | Cases decreasing | Lockdown easing |
| September 22, 2020 | Surge | Lockdown imposed | |
| Japan | October 1, 2020 | Cases decreasing | No lockdown restrictions |
| November 4, 2020 | Cases decreasing | No lockdown restrictions | |
| Mexico | Interview 1: July21, 2020 |
Surge | Lockdown imposed |
| Interview 2: November 4, 2020 |
Surge | Lockdown imposed | |
| Taiwan | October 12, 2020 | Few to no cases | Little restriction |
| UK | December 28, 2020 | Surges in select areas | Lockdown imposed in select areas |
| USA | December 1, 2020 | Surge | Lockdown imposed in certain states |
To analyze interviews, members of the research team began by developing an a
priori codebook, using the semi-structured interview guide as a framework. Team members then analyzed interview transcripts using Grounded Theory based on the Constant Comparative Method in NVivo, a qualitative data software.34,35 Two team members independently reviewed the transcripts and independently generated codes line-by-line. Disagreements in coding were discussed between these two team members, the original code set was refined, and consensus reached.
This study was reviewed by the authors’ institution’s Institutional Review Board and was designated exempt (H-39743). The principles outlined in the Declaration of Helsinki were followed and informed consent was obtained from all participants.
RESULTS
Four themes emerged from analysis: adequacy of Covid-19 preparation, access to care, implementation of telehealth, and misinformation regarding the COVID-19 pandemic.
COVID-19 changed aspects of health care and, more specifically, burn care.
Adequacy of COVID-19 Preparation
Since 1918, several viral outbreaks—notably the Spanish Flu, Swine Flu, Severe Acute Respiratory Syndrome (SARS), and the Avian Flu—have spurred interest in emergency preparedness on a trans-national and political scale.36 Two notable attempts to offer guidance on responses to international public health emergencies were released in recent years by the World Health Organization (WHO) and the National Academies of Sciences, Engineering, and Medicine (NASEM). However meaningful this attempt was, the guidelines released were quite
general. Certainly, no organization was prepared for a pandemic on the scale of COVID-19. Additionally, no one could have predicted the level to which misinformation, disbelief, and confusion were spread rapidly and exacerbated the lasting impact of the virus.
Some countries were more prepared to combat the pandemic than others and were able to mobilize more quickly. Taiwan had infectious disease protocols in place after the SARS epidemic in the early 2000s.37 In October 2020, we asked a burn clinician in Taiwan about how well the nation and their hospital were prepared for the COVID-19 pandemic. The clinician, said:
...we had an experience 17 years ago with the SARS epidemic. … During this pandemic, in my opinion, controlling the disease spreading... and good quarantine [was] very important because we controlled the disease in a very early stage to prevent spreading. So, from our experience regarding the 2003 SARS - or this year, COVID 19 - we have a good control of the [suspected COVID-19] victim.
Similarly, Australia had stringent disaster preparedness protocols in place. These stemmed from major burn events, such as the 2002 bombing of a hotel in Bali, where Australian clinicians were amongst first responders.38,39 Even though Australia had prepared carefully over the years, it suffered deficiencies in one area—communication. Three clinicians in Australia spoke about the impact of previous mass casualty training on the country’s response to the COVID-19 pandemic and how miscommunication caused confusion early on. One of them said:
I was involved in disaster management at the national level after the Bali bombing.so,
I understood early, way back in 2002, there was a level of pandemic planning in Australia. … But despite that, there was a lot of anxiety related to communication and the communication was sluggish to begin with because they didn’t know what to communicate because they couldn’t predict.is there enough PPE? What are the plans?
And there were in fact plans in place, but they weren’t communicated well in those early days. Subsequently, that was rectified, and it sort of rolled along and we were able to contain it.
Japan faced three viral outbreaks from 1999 to 2009, Influenza C, Avian Flu, and Swine Flu.40 One Tokyo clinician cites these as a reason Japan was prepared for the COVID-19 pandemic, though maybe not to the degree required. This clinician stated in October of 2020:
At that time, we wore masks, of course, but we did not use eyeglasses. Only a mask. And after that, all hospitals saved many masks, gowns, goggles, and other personal protection equipment. Also, the Japanese government purchased personal protection equipment and many medicine tablets for taking care of influenza patients. … [However] I think it’s not enough for this pandemic. Our experience is not enough for this pandemic.
In the last decade, several countries experienced the Middle East Respiratory Syndrome (MERS), an illness similar to both SARS and COVID-19.41 While Egypt was not as heavily impacted as nearby nations, it did help shape their understanding of a need for disaster preparedness. When asked about Egypt’s preparation for a global pandemic in October of 2020, one clinician compared the current pandemic to the Spanish influenza epidemic of 1918, with infections coming in waves. While they did not speak directly about preemptive measures, this clinician said that the Egyptian government responded quickly in at least one way:
From the very first moment, President Al-Sisi sent the Egyptian Minister of Health to China, and she visited them. She got some input from them and a lot of advice. … Egypt has approached many other countries that are suffering from the problem. There was a lot of discussion about how to manage COVID cases and prevent them and things like that.
In the United Kingdom, one clinician said that the government was behind in its efforts to combat the pandemic and had not obtained sufficient PPE and testing. In December of 2020, this clinician indicated that the government’s policies were about 10 d to 2 wk behind the internal policies their hospital implemented. This specialist also stated that:
There was no PPE when the pandemic hit, there was no PPE at all … apart from the ICU. And there was no testing, as you know. Testing really didn’t start in the UK until maybe August and the lockdown was very well delayed beyond the -- well after the whole of Europe, and even Europe was late.
Access to Care
Prior to COVID-19, access to care was limited by factors including proximity to care, density of services, and cost-related barriers. COVID-19 has shifted the relative importance of these factors. Insurance coverage and out-of-pocket costs had previously been high barriers to care in countries such as the United States.42 In Australia, geographic differences in access were prominent. During the pandemic, hospital resources shifted globally to fighting COVID-19, causing a decrease in resources to treat other conditions.43
Reported access to care in the United States, for example, has worsened during the COVID-19 pandemic. One study found that 38.7% of respondents in June and July of 2020 felt that their access to care deteriorated.44 COVID-19’s effects on access may be less in nations with more primary care physicians or hospital beds per thousand citizens, with more solid financial coverage, or with lower out-of-pocket costs.
With many hospitals serving patients at full inpatient capacity—especially during COVID-19 surges, geographic accessibility of hospital services has suffered with many seeing
increase in travel time. This has been a particular problem in areas with low bed-to-population ratios.45 In September of 2020, one burn clinician in Israel commented that during national lockdowns, they stopped seeing burn patients completely at their hospital:
We did have one case that I actually didn’t even see the patient. When the EMTs radioed that they were on the way we simply told them that if the patient is stable enough -- this was a major burn, 50% burn -- we told him that if the patient was stable enough, they just drive an hour north [to another hospital]...
One clinician in the United Kingdom, interviewed in December of 2020, said waiting time for appointments with general practitioners had “sky-rocketed” during the pandemic, but that people could get help by calling the National Health Service (NHS) hotlines or by going to local pharmacies. For burn care, this clinician stated that during the first wave, they saw an increase in neglected burns because people were afraid to come to the hospital. More recently, telehealth has helped increase access for patients, especially for children:
Once we have the patients, we follow up with the telemedicine. And especially children, the parents send photographs, and we assess them and give them advice on that. … And outpatients used to be run either by video conferencing, which I found not very useful, but mostly by phone consultations in adults and children. That was very, very helpful. But then you can screen and see if you really need to see the patients or not from the phone conversation.
Offering the most positive view, two clinicians in Germany stated that they had suffered little to no disruption of acute burn care, even at the pandemic’s peak, which was extremely beneficial since they faced an increase in pediatric burns. Clinicians largely attributed their
ability to maintain ICU capacity to the technology in their burn ICUs. Non-acute interventions, though, had been disrupted. In August of 2020, one said:
We didn’t admit COVID patients on our ICU… COVID patients were admitted to other ICUs, if necessary, but we didn’t have any burn patient who was COVID positive. We didn’t see any decrease in patient numbers during that period in acute burns. Of course, we had a decrease [in] secondary reconstruction because we were not allowed to admit elective cases for a certain period. But this is since about 5 or 6 weeks ago… For us, in acute burns, [there has been] no difference. In reconstructive burns, yes we are slowly starting again.
Further complicating access to care, hospitals around the world canceled elective surgeries, closed outpatient clinics, and diverted patients to other facilities. In Israel, “all active treatments were stopped,” including elective surgeries as well as physical and occupational therapy. In Mexico and Japan, some hospitals, which previously treated burn survivors, were converted to provide care for COVID-19 patients. Those needing acute burn care were sent to nearby hospitals equipped to care for burns. An American clinician said that during the height of the pandemic at their hospital, there was no outpatient prosthetic services. A physician from India indicated that the entire hospital cared exclusively for COVID-19 patients at the height of the pandemic in 2020; however, by the time we spoke with them, urgent and elective surgeries were starting up again.
Implementation of Telehealth
In order to combat the new strain on healthcare during the pandemic, telehealth became increasingly popular. Telehealth was initially developed in the 1950s to overcome access barriers and provide care when face-to-face doctor-patient interaction was “difficult due to the distance,
cost, or simple unavailability of a suitable transport.” 46–48 In burn care specifically, there have been challenges in implementing and utilizing telehealth as post-acute burn treatment entails frequent rehabilitation, wound care, and follow-up appointments. The quick transition to telehealth to provide these services depended on each country’s pre-existing infrastructure for telehealth, but clinician-patient interactions were limited by the constraints of virtual care.
Furthermore, physical exams, demonstration of rehabilitation exercises, and application of wound dressings proved to be a challenge and were not adequate via telehealth.49
In the United States, transition to telehealth was rapid. This was enabled in part by lowered public policy barriers that had earlier been enacted to protect patient privacy and enhance cybersecurity. Previously, telehealth also had limited economic incentive as there were decreased reimbursement rates, so many physicians did not utilize these platforms. Since COVID-19, regulations changed quickly and the economic incentive was matched by the ease of providing care, leading many physicians to begin to utilize telehealth.50 Interestingly, Japan and Taiwan did not have or see a need to shift to telehealth. In Taiwan, responses to COVID-19 enabled hospitals to remain functional. Access to care was minimally constrained. In Japan, though, COVID-19 initially had widespread effects, with closures of all outpatient clinics including both inpatient and outpatient rehabilitation services, and delays of surgeries for months. One clinician in Tokyo said that the only telehealth used was by telephone. In Australia, the density of healthcare services is much greater in the cities than in expansive rural areas.
Sophisticated telehealth systems had been developed before the pandemic and have continued to enable clinicians to successfully provide burn services across the nation.6 Australian clinicians could expand their use of telehealth to respond to the pandemic with relative ease because they already had the requisite infrastructure and legal permissions.
Similar to the Australian system, telehealth networks in Canada were extensive. This proved to be essential when, during the height of the pandemic, all burn rehabilitation services were “online or nothing,” in the words of one clinician with whom we spoke in January of 2021. Although the system was established, it was not easy to use:
It took forever to organize. … It’s very complex to book [appointments]. And so, there is the idea of telehealth … but it took really some time until Zoom or other media kicked in that you can actually have follow-ups via online platforms.
Mexican clinicians were unable to transition to telehealth even though Mexico saw one of the worst COVID-19 outbreaks during the earlier surges. Legal and health care delivery constraints blocked telehealth. This resulted in severe impacts on continuity of care for burn victims. One clinician opened an e-mail account for her patients, in addition to taking phone calls. The computers in their hospital are not enabled with video calling technology which, coupled with slow internet connectivity, disallowed video telehealth visits with patients. For rural patients or those without reliable electronic connections, one burn clinician in Mexico and their team trained family members to assist in rehabilitating patients. In July 2020, this clinician said:
We’re trying to teach the patients and the family how to take care of the patient and how to do the exercises and everything, but it’s very difficult for us to keep in touch with them and to make them take care of the patient and also to get involved in the rehab. But now it’s very difficult. … If they hurt, if they have any open wounds, for example, they just stop doing the exercise.
The pandemic undermined access to burn care in almost all of the 12 nations. During the height of the pandemic, finding alternate solutions, such as telehealth and family care, were critical. Still, the interview data suggest that most countries examined were able to restore burn
services to their prepandemic levels within several months. Although precautionary procedures are now followed, such as regular use of personal protective equipment (PPE) and limiting patient numbers, most of our interview subjects report that their hospitals have settled into a new normal of burn care. It differs from prepandemic patterns with a new-found emphasis on innovative measures of remote care, such as telehealth. Given the difficulties in establishing follow-up care after acute treatment, telehealth played a significant role in providing for those who are unable to come to outpatient facilities in certain countries.
Misinformation
COVID-19 cases continued to rise globally through the end of 2020. By November, Pfizer, Moderna, and AstraZeneca had announced vaccines against the virus. All the while, misinformation regarding inoculation and the pandemic itself was spread by news networks and social media outlets. In July 2020, a clinician in Mexico stated,
There’s still people that don’t believe that COVID exists. So, actually … they have attacked medical staff.
While some of the attacks described in Mexico were physical, other countries saw verbal and political attacks against leaders and medical professionals rooted in misinformation. In Chile, misinformation about COVID-19 encouraged citizens to blame the government for the pandemic. One clinician in Chile said that the COVID-19 pandemic has been a difficult time in their country because of the misinformation. In Australia, we spoke to one rehabilitation clinician at a particularly difficult time in the pandemic. Misinformation multiplied confusion.
This clinician told the research team:
So, that is very chaotic. There’s so many conspiracy theorists and antivaxxers that are having an absolute ‘will die on this hill,’ but I just think [vaccines have] to be done. And I think if we do this, hopefully we can resume normality.
The breadth of misinformation is not unique to COVID-19. Bora et al. found higher viewership on YouTube videos containing misinformation during the Zika virus epidemic.51 A study conducted early in the COVID-19 pandemic evaluated the information available in six languages on YouTube. At that time, YouTube was the second most visited website after Google and the top two search results on the site were “coronavirus” and “virus.” The validity of the information in these videos was assessed with a modified DISCERN index and the Medical Information Context Index (MICI). The information provided in these videos was described as “unsatisfactory.” Videos providing misleading content, from unreliable sources, had more views than videos released by government and health agencies.52 Although YouTube is only one source of information, the revelation that people were using it as a significant source of information and receiving mostly misinformation is striking.
Since the onset of the pandemic, reporters, scientific organizations, and governments have attempted to inform the public on the specifics of COVID-19. Misinformation from other sources about the virus, its spread, vaccinations, and other facets of the pandemic has persuaded many people. Additionally, greater use of and access to digital and social media has increased dissemination of misinformation regarding COVID-19. It ranges from conspiracy theories about the source of the virus to vaccine safety and efficacy and to unproven treatments.53,54 This resulting confusion and uncertainty have undermined patient willingness to access care and pursue follow-up treatments. Misinformation has led individuals to refuse to wear masks, ignore
physical distancing recommendations, and reject vaccinations.55 The net result is to overburden hospitals and caregivers.
Widespread misinformation about burn care predated the pandemic. One study found that selected web searches provided inaccurate or incomplete medical information about burn care.56 Investigators used several search engines to look up “first aid for burns” and evaluated the results. They found that both the quality and technical information score of each source was subpar. Of 48 websites evaluated, none provided credible information and 36 provided poor information.
DISCUSSION
Using the Aday and Andersen model, several cross-cutting themes in the treatment of burn patients have emerged that include the impact of misinformation on preparedness and preparedness as it relates to access to care. Furthermore, the use of telehealth as a digital bridge to improving access to care emerged as another theme.
Misinformation and Preparedness
Misinformation has been examined for years. Experts have identified it as a problem requiring a necessary focus of public health interventions.57 Misinformation about the COVID-19 pandemic has made it much harder to treat patients for other conditions, including burn survivors.58 Sound preparation to address pandemics and other disasters—at the national or hospital level—might have countered misinformation or mitigated its effects on patient care.
Sadly, clinicians who were interviewed painted a picture of poor preparedness.
One burn clinician in Mexico stated that their country was not well-prepared to deal with misinformation about the virus. Some patients arrived at hospitals and clinics ill with COVID-19
and did not disclose this. This clinician said that shortages of PPE and misinformed patients combined to infect hospital staff:
Yes, well actually here in Mexico, we have the highest rates of the medical staff infected and dead. We have a lot of medical staff, nurses, doctors that have died because they didn’t have personal protective equipment. And the patients don’t say that they have been infected. That’s already happened, that people don’t say that they are sick, and they look for medical attention. And until they’re in [the hospital], they don’t say that they feel sick.
In the United States, one clinician in a hospital challenged by the pandemic said that preparation was key to combating misinformation. According to this doctor, if a hospital has strong ties with its community, people are more likely to believe the messages coming from the hospital. This burn specialist said:
I think that doing your homework for the months and years, decades ahead of these events -- you have to have that foundation to perform well and to avoid misinformation… to have a flagship facility in the community seen as a resource as opposed to a pathogen. The public health messaging that [my institution] has been a part of for decades has allowed us to not politicize the masking and the distancing and all that stuff because people trust [my institution] and the messages that come from it. … I think that the lesson learned is preparation, not for the pandemic, but for being responsive to your community over a long term.
Failure to combat misinformation and inadequate preparation have been synergistic throughout the pandemic. This interaction deserves attention by governments, public health professionals, and clinicians. Each of the clinicians cited above asserts that messaging from governments and hospitals affects citizens’ and clinicians’ abilities to cope effectively with the pandemic’s enormous demands.
Pandemic Preparedness and Access to Care
Burn clinicians have found ways to adapt to the clinical time, space, and financial resources available. The COVID-19 pandemic resulted in an unprecedented cut in all three types of resources. Weak preparation, cited by almost every clinician interviewed, resulted in a decrease in access to care.
Immediately after the burn injury, access to emergency services is vital for making a full recovery.59,60 While emergency services for burn injuries continued to be available in some large urban regions, some burn units were converted to COVID-19 units, requiring burn patients to travel longer distances. Post-acute treatment is essential to successful burn care. Closure of rehabilitation and outpatient follow-up centers has undermined this treatment. Many patients were afraid to visit rehabilitation centers that remained open due to clusters of COVID-19 outbreaks. Post-acute burn care has suffered, resulting in substantial impacts to patients. Another physician in Mexico commented on this:
Well, we used to see our patients almost every week. So now it’s very difficult to see our patients as often as we would like to. And actually, we don’t – can’t send our patients to their local rehab units now because they’re closed. So, we’re trying to teach the patients and the family, how to take care of the patient and how to make the exercises and everything, but it’s very difficult for us to keep in touch with them and to make them take care of the patient and also to get involved in the rehab.
Lockdowns and economic shutdowns were implemented worldwide and one clinician in India said that they believe this is the reason the pandemic was not as disastrous in their country
as it could have been during the earlier stages of the pandemic. This allowed this clinician and their hospital to stay ahead of cases that they were not prepared for and cases that would have continued to rise if economic activities had continued. This clinician said:
If [the government] had not initiated a lockdown initially, we would have had huge numbers. And we were not prepared for those numbers to get admitted for adequate treatment. Now, at least, even if the numbers are rising, they are not being deprived of the treatment. … I think it was essential. If there was no lockdown, and you had five thousand, ten thousand patients every day, they would [not have had] enough beds....
There is no cry anywhere around that I’m not getting medical attention.
Closings of post-acute burn clinics and society-wide lockdowns required nearly every country to employ new strategies to deliver needed care. One response in places has been to provide more post-acute burn care in the home. In Australia, one clinician noted that home care aided by telehealth and home healthcare nurses had been a standard of care for several years.
Due to the immense size of some Australian states, this has been a service used for years to increase access to care.6 As COVID-19 continues to surge in many nations, planning adequate ways to care for large volumes of COVID-19 patients is crucial to sustain outpatient services generally and rehabilitation services for burn care in particular.
Telehealth and Access to Care
During the pandemic, telehealth became a partial substitute for in-person care.61 While the technology behind telehealth has been around for many years, it was never widely utilized until COVID-19.50 Telehealth enabled clinicians caring for burn patients to sustain continuity of outpatient services. Caregivers could conduct clinic appointments and even view burns through video technology. Many burn rehabilitation practitioners found creative ways to utilize telehealth
to aid in recovery. Throughout the pandemic, increasing use of telehealth has been closely linked with better access to care62 Burn victims who had previously suffered loss of income while traveling to appointments, and who had incurred travel costs, could avoid lost work time and save on travel.63 While telehealth enabled some burn patients to receive outpatient follow-up, patients lacking video-enabled technology, or reliable internet access continued to be at a disadvantage. Telehealth has been a valuable substitute to protect access to care during the COVID-19 pandemic. In burn care, telehealth enabled continuity of care in the post-acute period. Given the difficulties in establishing follow-up care after acute treatment, telehealth played a significant role in providing for those who are unable to come to outpatient facilities in certain countries.
Limitations
This study has several limitations. First, the findings of this study are not generalizable to an entire country’s experience of the COVID-19 pandemic or even the delivery of burn care within that country at the time of the interviews. We interviewed one to four clinical burn specialists in each of the twelve countries. For this reason, some perspectives may be missing.
Still, those interviewed are well-informed clinical leaders in burn care who have wide and rich in-depth understandings of their nation’s health care systems and the COVID-19 pandemic.
Second, cultural differences between and within countries may be associated with differences in expectations about the pandemic, how people responded to COVID-19, and the resulting effects on care. Cultural ideas of collectivism versus individualism may affect adherence to regulations and mandates put in place to protect a nation’s population. Lu et al. found that in collectivist countries, such as Japan or Taiwan, the focus on the group rather than the individual may have resulted in increased mask wearing and adherence to regulations
regarding COVID-19.64 Interestingly, Australia, a country found to be significantly individualistic on Vandello’s and Cohen’s individualism–collectivism index, had a robust response to COVID-19 that was broadly accepted across the nation.65 Variations in response due to cultural differences may have had a significant impact on how the COVID-19 pandemic unfolded in each nation and, ultimately, its impact on the rest of the healthcare system.
A final limitation of this study stems from interviewing participants at varying stages of the pandemic. Interviews began in July of 2020, during the middle of the first wave of the pandemic for several nations. The interviews ended by January of 2021 when vaccine distribution had begun around the world and several participants in this study had already received their first dose. Because of these varying timelines, it is difficult to directly compare all information from interviews between countries and, in some cases, within the same country.
CONCLUSION
The impacts of the COVID-19 pandemic have complicated the delivery of healthcare, generally and in burn care, more specifically across the twelve countries studied. During the first few months of the outbreak, hospitals’ responses were disorganized, owing to lack of preparation for such a virulent disease. With the redirection of healthcare providers and resources throughout the COVID-19 pandemic, the downstream impacts on health care delivery, access to care, and overall utilization of health care services were significant. The broad dissemination of misinformation compounded harm stemming from resource shortages.
Lessons for burn care and rehabilitation can be learned by understanding the course of the COVID-19 pandemic. As healthcare services shifted away from elective procedures and non-urgent in-person care, there were reductions in available outpatient services and strain on rehabilitation for burn care. Continuity of care and mental health services were particularly
impacted by this shift. These components of burn care are important for those returning to the community after a burn injury. As waves of the pandemic surged and waned, access to care was subject to change within days. The disruptions in burn care, as a result, reveal the importance of having robust workflows in place to maintain services that can withstand sudden financial, political, or epidemiological shifts. Some of these processes might include preparing a robust telehealth system, maintaining reserves of PPE, and implementing realistic hospital plans to cope with acute or sustained crises in the future. If nations are able to establish sustainable, replicable preparation plans for future disasters, the global healthcare system may be able to better prepare for and respond to widespread crises.
Conflicts of interest statement: None declared.
Acknowledgements
Dr. Ronald Tompkins passed away while this paper was under preparation. His creativity, insight, dedication, and important contributions to this work leave a lasting legacy to the excellence in burn care that he aspired to provide. Many thanks to the following clinicians who gave of their valuable time to make this work possible (in alphabetical order): Rajeev Ahuja, MBBS, M.CH, DNB, FACS, FICS, FAMS, Dale Edgar, BPhty (Hons), PhD, Mariana Morales Garcia, MD, Joseph Haik, MD, MPH, Bernd Hartmann, Dr. med., Huang Hui-Fu, MD, Marc Jeschke, MD, PhD, FACS, FRCSC, Amr Mabrouk, MD, Naiem Moiemen, MBBCh, MSc, FRCS, Ricardo Roa, MDa, Frank Sander, Dr. med., Yukio Sato, MD, PhD, Yaron Shoham, MD, Yvonne Singer, BS, MPH, Barclay Stewart, MD, PhD, MPH, and Fiona Wood, FRCS, FRACS, AM.
Contributor Information
Ananya Vasudevan, Boston University School of Medicine, Massachusetts, USA.
Hannah M Bailey, Department of Health Law, Policy and Management, Boston University School of Public Health, Massachusetts, USA.
Alan Sager, Department of Health Law, Policy and Management, Boston University School of Public Health, Massachusetts, USA.
Lewis E Kazis, Department of Health Law, Policy and Management, Boston University School of Public Health and Department of Physical Medicine and Rehabilitation, Harvard Medical School, Massachusetts, USA.
References
- 1. Sheridan RL, Schulz JT, Ryan CM, McGinnis PJ. Case 6-2004: A 35 year-old woman with extensive, deep burns from a nightclub fire. N Engl J Med 2004;350. [DOI] [PubMed] [Google Scholar]
- 2. Tompkins RG. . Survival from burns in the new millennium: 70 years’ experience from a single institution. Ann Surg 2015;261:263–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rowan MP, Cancio LC, Elster EA, et al. Burn wound healing and treatment: Review and advancements. Crit Care 2015;19:243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Harshman J, Roy M, Cartotto R. Emergency care of the burn patient before the burn center: A systematic review and meta-analysis. J Burn Care Res 2019;40(Pt 2): 166 - 188. [DOI] [PubMed] [Google Scholar]
- 5. Zuo KJ, Medina A, Tredget EE. Important developments in burn care. Plast Reconstr Surg 2017;139:120e–38e. [DOI] [PubMed] [Google Scholar]
- 6. Kazis LE, Sager A, Bailey HM, Vasudevan A, Garrity B, Tompkins RG. Physical rehabilitation and mental health care after burn injury: A multinational study. Burn Care Res 2021;43:868–79. doi: 10.1093/jbcr/irab214 [DOI] [PubMed] [Google Scholar]
- 7. Sen-Crowe B, Sutherland M, McKenney M, Elkbuli A. A closer look into global hospital beds capacity and resource shortages during the COVID-19 pandemic. J Surg Res 2021;260:56–63. doi: 10.1016/j.jss.2020.11.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Farrell NM, Hayes BD, Linden JA. Critical medication shortages further dwindling hospital resources during COVID-19. Am J Emerg Med 2020;40:202–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Badreldin HA, Atallah B . Global drug shortages due to COVID-19: Impact on patient care and mitigation strategies. Res Social Adm Pharm 2021;17:1946–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Abbasi J. “Abandoned” nursing homes continue to face critical supply and staff shortages as COVID-19 toll has mounted. JAMA 2020;324:123–5. [DOI] [PubMed] [Google Scholar]
- 11. Leng C, Challoner T, Hausien O, Filobbos G, Baden J. From chaos to a new norm: The Birmingham experience of restructuring the largest plastics department in the UK in response to the COVID-19 pandemic. J Plast Reconstr Aesthet Surg 2020;73:2136–41. doi: 10.1016/j.bjps.2020.08.127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ilenghoven D, Hisham A, Ibrahim S, Mohd Yussof SJ. Restructuring burns management during the COVID-19 pandemic: A Malaysian experience. Burns 2020;46:1236–9. doi: 10.1016/j.burns.2020.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Grimm CA. Hospital Experiences Responding to the COVID-19 Pandemic: Results of a National Pulse Survey March 23–27, 2020. 2020. [Google Scholar]
- 14. Powder J. Too Many COVID-19 Patients, Too Few Ventilators: An Ethical Framework to Guide Hospitals. . Johns Hopkins Bloomberg School of Public Health. https://publichealth.jhu.edu/2020/too-many-covid-19-patients-too-few-ventilators-an-ethical-framework-to-guide-hospitals. [Google Scholar]
- 15. COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. British J Surg. 2020;107:1440–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tran LD, Rose L, Urech T, Dalton A, Wu S, Vashi AA. Short-term effects of canceled elective procedures due to COVID-19: Evidence from the veterans affairs healthcare system. Ann Surg 2021;274:45–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kazis LE, Marino M, Ni P, et al. Development of the life impact burn recovery evaluation (LIBRE) profile: Assessing burn survivors’ social participation. Qual Life Res 2017;26:2851–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gauglitz GG, Williams FN.. Overview of the management of the severely burned patient. uptodate.com2021. [Google Scholar]
- 19. Rencken CA, Harrison AD, Aluisio AR, Allorto N. A qualitative analysis of burn injury patient and caregiver experiences in Kwazulu-Natal, South Africa: Enduring the transition to a post-burn life. European Burn J 2021;2:75–87. doi: 10.3390/ebj2030007 [DOI] [Google Scholar]
- 20. Kleinitz P, Mills JA, Connolly B, Skelton B, Smith G, Clift Z. Rehabilitation Considerations during the COVID-19 outbreak. 2020. https://iris.paho.org/bitstream/handle/10665.2/52035/NMHMHCOVID19200010_eng.pdf?sequence=6
- 21. Koonin LM, Hoots B, Tsang CA, et al. Trends in the use of telehealth during the emergence of the COVID-19 pandemic — United States, January–March 2020. Morb Mortal Wkly Rep 2020;69:1595–9. https://www.cdc.gov/mmwr/volumes/69/wr/mm6943a3.htm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Varma P, Kazzazi D, Anwar MU, Muthayya P. The impact of COVID-19 on adult burn management in the United Kingdom: A regional center experience. J Burn Care Res 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yamamoto R, Sato Y, Matsumura K, Sasaki J. Characteristics of burn injury during COVID-19 pandemic in Tokyo: A descriptive study. Burns Open 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Black, L. Accidental Burns Increased for Children at Home During Pandemic. 2021. https://www.aap.org/en/news-room/news-releases/aap/2021/accidental-burns-increased-for-children-at-home-during-pandemic/
- 25. Saha S, Kumar A, Dash S, Singhal M. . Managing burns during COVID-19 outbreak. J of Burn Care Res 2020;41:1033–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Won P, Celie K-B, Perez V, Gillenwater TJ, Yenikomshian HA. The Patient’s Perspective: Burn Reconstructive Surgery During the COVID-19 Pandemic. J Burn Care Res 2021;42:76–7. [DOI] [PubMed] [Google Scholar]
- 27. Krieger Y, Shoham Y, Levi A, Bogdanov-Beresovsky A, Silberstien E, Sagi A. Burn treatment framework in Israel. Ann Burns Fire Disasters 2011;24:199–202. [PMC free article] [PubMed] [Google Scholar]
- 28. Aday LA, Andersen R. A Framework for the Study of Access to Medical Care. Health Services Res 1974;20:8–220. [PMC free article] [PubMed] [Google Scholar]
- 29. Andersen R. . Revisiting the Behavioral Model and Access to Medical Care: Does it Matter? J Health Soc Behav 1995;36:1–10. [PubMed] [Google Scholar]
- 30. Earnshaw VA, Katz IT. . Educate, Amplify, and Focus to Address COVID-19 Misinformation. JAMA Health Forum. 2020;1:e200460–e200460. doi: 10.1001/jamahealthforum.2020.0460 [DOI] [PubMed] [Google Scholar]
- 31. Abbasi J. COVID-19 Conspiracies and Beyond: How Physicians Can Deal With Patients’ Misinformation. JAMA. 2021;325:208–10. doi: 10.1001/jama.2020.22018 [DOI] [PubMed] [Google Scholar]
- 32. Ugarte DA, Cumberland WG, Flores L, Young SD. . Public Attitudes About COVID-19 in Response to President Trump’s Social Media Posts. JAMA Network Open. 2021;4:e210101–e210101. doi: 10.1001/jamanetworkopen.2021.0101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. ISBI Practice Guidelines Committee. ISBI Practice Guidelines for Burn Care. Burns 2016;42:953:1021. [DOI] [PubMed] [Google Scholar]
- 34. Glaser BG, Strauss AL.. The Discovery of Grounded Theory: Strategies for Qualitative Research. Hawthorne, NY: Aldine de Gruyter; 1967. [Google Scholar]
- 35. Leech NL, Onwuegbuzie AJ. Beyond constant comparison qualitative data analysis: Using NVivo. School Psychology Quarterly. 2011;26:70–84. doi: 10.1037/a0022711 [DOI] [Google Scholar]
- 36. Harrington WN, Kackos CM, Webby RJ. The evolution and future of influenza pandemic preparedness. Experimental & Molecular Medicine 2021;53:737–49. doi: 10.1038/s12276-021-00603-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. World Health Organization. Severe Acute Respiratory Syndrome (SARS). 2021. https://www.who.int/health-topics/severe-acute-respiratory-syndrome#tab=tab_2 [Google Scholar]
- 38. Chim H, Yew WS, Son g C. Managing burn victims of suicide bombing attacks: outcomes, lessons learnt, and changes made from three attacks in Indonesia. Critical Care. 2007;11:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. BBC Staff. Bali bombing: Survivors mark 10 year anniversary. BBC News. https://www.bbc.com/news/uk-19712683 [Google Scholar]
- 40. Matsumoto K. History of pandemic influenza in Japan. J Japan Surg Asso. 2010;68:1595–601. [PubMed] [Google Scholar]
- 41. World Health Organization. Middle East respiratory syndrome coronavirus (MERS-CoV). 2019. https://www.who.int/news-room/fact-sheets/detail/middle-east-respiratory-syndrome-coronavirus-(mers-cov) [Google Scholar]
- 42. Wray CM, Khare M, Keyhani S. Access to Care, Cost of Care, and Satisfaction With Care Among Adults With Private and Public Health Insurance in the US.. JAMA Network Open Health Policy 2021;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Emanuel EJ, Persad G, Upshur R et al. Fair Allocation of Scarce Medical Resources in the Time of Covid-19. N Engl J Med 2020;382:2049–55. doi: 10.1056/NEJMsb2005114 [DOI] [PubMed] [Google Scholar]
- 44. Centers for Disease Control and Prevention Staff. Reduced Access to Care. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/covid19/rands/reduced-access-to-care.htm
- 45. Weiss DJ, Nelson A, Vargas-Ruiz CA et al. Global maps of travel time to healthcare facilities. Nat Med 2020;26:1835–8. doi: 10.1038/s41591-020-1059-1 [DOI] [PubMed] [Google Scholar]
- 46. Gogia S. Chapter 2 - Rationale, history, and basics of telehealth. In: Gogia S, Novaes Ma, Basu Ar, Gogia Kr, Gogia Sp, eds. Fund Telemedicine Telehealth 2020;30:11–34. [Google Scholar]
- 47. Nickelson DW. Telehealth and the Evolving Health Care System: Strategic Opportunities for Professional Psychology. Professional Psychology: R Practice. 1998;29:527–35. [Google Scholar]
- 48. Nesbitt ThS. The Evolution of Telehealth: Where Have We Been and Where Are We Going? Washington DC: National Academies Press (US); 2012. [Google Scholar]
- 49. Gajarawala SN, Pelkowski JN. Telehealth Benefits and Barriers. J Nurse Pract 2021;17:218–21. doi: 10.1016/j.nurpra.2020.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hoffman DA. Increasing access to care: telehealth during COVID-19. J Law Biosci 2020;7:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Bora K, Das D, Barman B, Borah P. Are internet videos useful sources of information during global public health emergencies? A case study of YouTube videos during the 2015–16 Zika virus pandemic. Pathogens Global Health 2018;112:320–8. doi: 10.1080/20477724.2018.1507784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Dutta A, Beriwal N, Van Breugel LM, et al. YouTube as a source of medical and epidemiological information during COVID-19 pandemic: A cross-sectional study of content across six languages around the globe. Cureus 2020;12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Roozenbeek J, Schneider CR, Dryhurst S, et al. Susceptibility to misinformation about COVID-19 around the world. R Soc Open Sci 2020;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Brennen JS, Simon F, Howard PN, Nielsen RK. Types, sources, and claims of COVID-19 misinformation. Reuters Institute. https://reutersinstitute.politics.ox.ac.uk/types-sources-and-claims-covid-19-misinformation
- 55. Wardle C, Singerman E. Too little, too late: social media companies’ failure to tackle vaccine misinformation poses a real threat. Br Med J 2021;372:6. [DOI] [PubMed] [Google Scholar]
- 56. Tiller G, Rea S, Silla R, Wood F. Burns first aid information on the Internet. Burns 2006;32:897–901. [DOI] [PubMed] [Google Scholar]
- 57. Southwell BG, Niederdeppe J, Cappella JN, et al. Misinformation as a misunderstood challenge to public health. Am J Prev Med 2019;57:282–5. doi: 10.1016/j.amepre.2019.03.009 [DOI] [PubMed] [Google Scholar]
- 58. Barua Z, Barua S, Aktar S, Kabir N, Li M. Effects of misinformation on COVID-19 individual responses and recommendations for resilience of disastrous consequences of misinformation. Progress in Disaster Science 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Rice J, Phillip L, Orgill DP. Emergency care of moderate and severe thermal burns in adults. Accessed October 11, 2021, https://www.uptodate.com/contents/emergency-care-of-moderate-and-severe-thermal-burns-in-a dults#H32
- 60. Wallis LA, Fleming J, Hasselberg M, Laflamme L, Lundin J. A Smartphone App and Cloud-based consultation system for burn injury emergency care. PLoS One 2016;11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health 2020;20:1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Centers for Disease Control and Prevention Staff. Telemedicine Access and Use. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/covid19/rands/telemedicine.htm [Google Scholar]
- 63. Head WT, Garcia DI, Kahn S, Lesher A. 61 real-time burn outpatient virtual visits in the home during the era of COVID-19. J Burn Care Res 2021;42:3410–24. [Google Scholar]
- 64. Lu JG, Jin P, English AS. Collectivism predicts mask use during COVID-19. Proc Natl Acad Sci USA 2021;118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Vandello JA, Cohen D. . Patterns of individualism and collectivism across the United States. J Pers Soc Psychol 1999;77:279–92. [Google Scholar]