Abstract
The coronavirus disease 2019 (COVID-19) pandemic forced many countries into lockdowns to limit the spread of infection. Israel’s containment measures included school closures, mobility restrictions, and workforce reductions. Our study evaluated the effect of COVID-19 on the occurrence and patterns of burn injuries. The study data was obtained via retrospective chart review of burn patients treated between March 15, 2020 and April 30, 2020, namely the period of strict national lockdown. This data was compared against data from paralleling periods between 2017 and 2019. A total of 686 patients were treated for burn injuries in the two study periods. Age group analysis revealed an increased ratio of pediatric patients aged 0–3 years during the lockdown (55.91% vs 40.79%, P = .002). In contrast, there were fewer patients presenting with burn injuries in the 7–16 and 17–29 age groups (9.66% vs 3.15%, P = .017; 16.46% vs 7.09%, P = .007, respectively). During both study periods, scald injuries were the most common burn etiology and burn injuries occurred most often at home. This predominance was further pronounced during the lockdown (71.65% vs 58.68%, P = .007; 90.55% vs 74.60%, P = .0001, respectively). The lockdown period underlined the danger faced by pediatric patients in their household environment. This danger was possibly compounded by an improper level of adult supervision as parents transitioned to remote work. These findings can educate us about factors that render burn injuries more likely not only during lockdowns, but also during regular times, thus shaping the development of burn prevention practices.
In December 2019, an epidemic of viral pneumonia broke out in Wuhan, China, with rapid spread to other parts of the world. On January 30, 2020, the World Health Organization (WHO) declared it a pandemic.1,2 The pandemic was caused by a novel coronavirus, named 2019-nCoV by the WHO. The disease associated with it was subsequently named coronavirus disease 2019 (COVID-19). Some of the symptoms more frequently reported include fever, fatigue, and dry cough. The disease may also be fatal.3 In an effort to minimize social contact and contain the spread of infection, many countries implemented quarantines, lockdowns, and curfews.4 In Israel, the first patient presenting with coronavirus was diagnosed on February 27, 2020, after having traveled from Italy to Israel. On March 14, 2020, with the number of cases increasing to 195, the Israeli government declared a strict national lockdown, which included restrictions on movement, reduction of working capacity to 10%–20%, and educational system shutdown for all ages. This lockdown lasted from March 15, 2020 to April 30, 2020. Meanwhile, no restrictions were made with respect to seeking medical services.5
Burn injuries represent a major public health concern and are among the leading causes of morbidity and mortality in the East Mediterranean region.6 In Israel, burns account for approximately 5% of all trauma admissions.7 The field of burn epidemiology has been thoroughly studied, with multiple publications describing risks and temporal trends that may aid in injury prevention practices and staffing of burn services. And yet, some conclusions remain controversial. Namely, while some studies found correlations between burns and seasonality,8–12 day of the week,13,14 time of the day,15,16 sex,17,18 age groups,7,19,20 among other factors,21,22 others did not.23,24
In the present study, we examined temporal variation in cases of burn injuries treated at Israel’s trauma centers during the COVID-19 outbreak and the subsequent lockdown. This is a unique situation in that not only did the pediatric population stay at home for extended periods of time, but they were not always supervised by an adult, as many parents had to continue working from home. The lockdown may therefore facilitate our understanding of the different circumstances that render burn injuries more likely, and become instrumental in developing educational and preventive strategies.
METHODS
Data was obtained and analyzed for all patient admissions consisting of at least 1-day hospitalization at one of twenty trauma centers (including all six level I trauma centers) in Israel between March 15, 2020 and April 30, 2020. These dates mark the period during which the Israeli government implemented strict lockdown policies. The data collected from this time period was compared to data from paralleling dates between the years 2017 and 2019.
The data included in the study was retrieved from the Israeli National Trauma Registry (INTR), which is coordinated by the National Center for Trauma and Emergency Medicine Research at the Gertner Institute for Epidemiology and Health Policy Research, at Tel Hashomer. The data is comprised of demographic and clinical information, including etiology, prehospital care, depth and size of burn, emergency management, and acute and surgical interventions performed. Of note, the Registry does not account for patients pronounced to be dead at the scene or dead on arrival at the hospital.
Statistical analysis included a preliminary examination of the relationship between variables. The relationship between the dependent variables and independent variables was analyzed. Chi-square tests were used for group comparisons and binomial proportions test was used for proportions. A P-value of <.05 was considered statistically significant. All statistical analysis was performed using the SAS Software version 9.4 (SAS, Cary, NC).
RESULTS
Between March 15, 2020 and April 30, 2020, 127 burn patients were admitted to one of 20 trauma centers within Israel for at least one day of hospitalization (Table 1).
Table 1.
Characteristics of admitted burn patients
| 2017–2019 Parallel Period Mean, N (%) |
2020 Lockdown Period N (%) |
P | |
|---|---|---|---|
| Admissions | |||
| Burn Patients | 186 [Range 172–196] | 127 | |
| Sex | |||
| Male | 121 (64.94) | 77 (60.63) | .36 |
| Female | 65 (35.06) | 50 (39.37) | |
| Ethnicity | |||
| Jewish | 111 (59.93) | 76 (59.84) | .559 |
| Non-Jewish | 75 (40.07) | 51 (40.16) | |
| Age Groups | .0041 | ||
| 0–3 y | 76 (40.79) | 71 (55.91) | .002 |
| 4–6 y | 13 (7.16) | 13 (10.24) | .241 |
| 7–16 y | 18 (9.66) | 4 (3.15) | .0173 |
| 17–29 y | 31 (16.46) | 9 (7.09) | .0071 |
| 30–64 y | 39 (21.11) | 24 (18.9) | .5787 |
| 65+ y | 9 (4.83) | 6 (4.72) | .9599 |
| Geographical Region | .0461 | ||
| Center | 106 (56.89) | 71 (55.91) | .84 |
| North | 64 (34.35) | 36 (28.35) | .195 |
| South | 16 (8.77) | 20 (15.75) | .0182 |
| Location | |||
| Domestic | 139 (74.60) | 115 (90.55) | .0001 |
| Kitchen | 64.66 (46.52) | 51 (44.35) | .678 |
| Other Domestic | 74.33 (53.48) | 64 (55.65) | |
| Occupational | 18 (9.48) | 7 (5.51) | .1529 |
| TBSA*, % | .8859 | ||
| 1 DEG | 9 (5.01) | 8 (6.30) | .5561 |
| 2/3 DEG 1–9% | 134 (71.74) | 91 (71.65) | .9853 |
| 2/3 DEG 10–19% | 30 (16.10) | 18 (14.17) | .5904 |
| 2/3 DEG 20+% | 13 (7.16) | 10 (7.87) | .7786 |
| Injured Area† | |||
| Head and Neck | 70 (37.75) | 55 (43.31) | .246 |
| Torso | 82 (43.83) | 54 (42.52) | .788 |
| Upper Limbs | 65 (34.70) | 50 (39.37) | .3215 |
| Hand | 43 (22.90) | 27 (21.26) | .6903 |
| Lower Limbs, n | 63 (33.99) | 38 (29.92) | .3797 |
| Etiology | .0586 | ||
| Chemical | 13 (7.16) | 10 (7.87%) | .7786 |
| Contact | 12 (6.44) | 5 (3.94) | .2827 |
| Fire | 33.33 (17.89) | 13 (10.24) | .036 |
| Scald | 109 (58.68) | 91 (71.65) | .007 |
| Other | 19 (9.84) | 8 (6.3) | |
| Hospitalization Period | |||
| 0–6 d | 114 (61.18) | 75 (59.06) | .0970 |
| 7+ d | 72 (38.82) | 52 (40.94) | |
| Operation Required | |||
| Yes | 19 (10.20) | 9 (7.09) | .2833 |
| No | 167 (89.80) | 118 (92.91) |
*TBSA – total body surface area.
†Each patient may be injured in more than one area.
Male patients were more prone to burn injuries both during the studied and paralleling periods (64.94% vs 60.63%, P = .36).
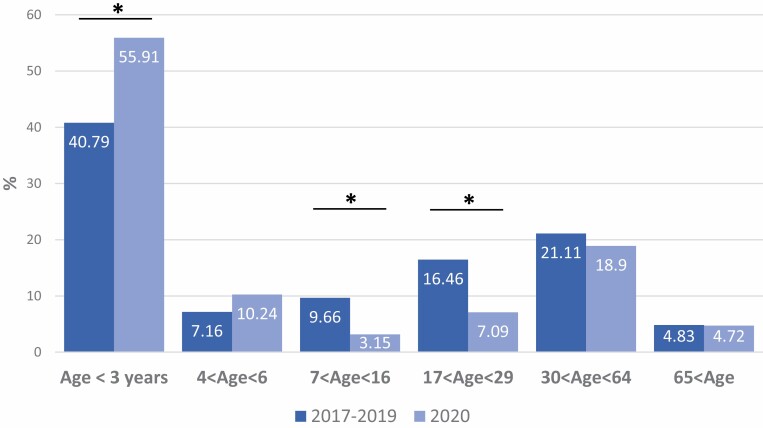
Pediatric patients (ie, under the age of 16) were more susceptible to burn injuries during the lockdown period compared to paralleling periods in 2017–2019 (69.29% vs 57.60%, P = .015). Subgroup analysis revealed that children under 3 years of age were particularly susceptible on comparing the lockdown period to similar dates in 2017–2019 (55.91% vs 40.79%, P = .002). Meanwhile, patients in the age group of 7 to 16 were less susceptible to burn injuries during the lockdown period compared to the 2017–2019 corresponding periods. (9.66% vs 3.15%, P = .017).
Adult patients (ie, aged 17 and above), were less susceptible to burn injuries during the lockdown period compared to paralleling periods in 2017–2019 (30.71% vs 42.40%, P = .015), particularly young adults between 17 and 29 years of age (16.46% vs 7.09%, P = .007) (plotted in Figure 1).
Figure 1.
Distribution of admitted patients with burn injuries by age. *P < .02.
The majority of hospitalized patients were Jewish, both during the lockdown and paralleling periods (59.93% vs 59.84%, P = .56). Based on data from Israel’s Central Bureau of Statistics, at the end of 2019, 6,772,000 (74.1%) of the general population were known to be Jewish.25 Therefore, the ratio of Jews sustaining burn injuries was notably smaller relative to the non-Jewish population. Non-Jewish citizens constituted 40.07% of the burn patients despite constituting only 25.9% of the general population.
In terms of geographic regions, while the total number of patients sustaining burn injuries at the national level decreased, the fraction of injured patients in Southern Israel increased (15.75% vs 8.77%, P = .0182).
During both the lockdown and paralleling dates in 2017–2019, the most common etiology of burn injuries was scald injuries. This predominance increased even further during the lockdown period (71.65% vs 58.68%, P = .007). The increase in burns caused by scalding was even more pronounced among women (84% vs 67.86%, P = .0245). Meanwhile, the fraction of patients hospitalized due to fire injuries decreased (10.24 vs 17.89, P = .036). No statistically significant change was noted as to the cause of burn injuries on subgroup analysis according to age (P > .05).
Furthermore, the severity as well as area injured did not vary between the study periods. Namely, more than 76% of all admissions during both periods were burns of up to 9% of total body surface area (TBSA). The most commonly injured area was the torso during both periods (43.83% vs 42.52, P = .79), and no change was observed with regard to the pattern of injuries during the studied periods, P > .05 (Table 1).
The most common location where burn injuries were sustained was at home, a finding that was even more pronounced during the lockdown period (90.55% vs 74.60%, P = .0001). The kitchen area was a common location of injury during both investigated periods (44.35% vs 46.52%, P = .67). Meanwhile, there was no evidence of a statistically significant decline in the number of patients sustaining occupational burn injuries (5.51% vs 9.48%, P = .15) (Table 1).
Additionally, the length of hospital stays did not significantly change between the two periods investigated, and most patients were hospitalized for up to 6 days (61.18% vs 59.06%, P = .097). Only a minority of patients were admitted to the ICU in both periods (10.02% vs 10.24%, P = .94), and most admitted patients did not require surgical interventions (89.8% vs 92.91%, P = .28) (Table 1).
DISCUSSION
Burn injuries are among the most common and devastating yet preventable injuries, placing patients at high risk for morbidity and mortality. Furthermore, these accidents have a large impact on caregivers and healthcare services.6,7 Enhancing our understanding of and predicting the relationship between specific conditions and their susceptibility to burn injuries are essential to developing burn prevention practices and configuring burn units.
With the onset of the pandemic in December 2019, many countries went into lockdown with the aim of halting the spread of infection. The Israeli government issued strict lockdown measures on March 15, 2020, which included restrictions on mobility, school closures, and reduction in workforce to 10%–20% capacity. This nationwide lockdown, which lasted until April 30, 2020, allowed us to study burn etiologies in real-world settings, especially in a period that found many families unprepared both physically and emotionally. During that time frame, many parents had to adjust to working remotely while their children were at home due to schools being shut down.26 It is therefore possible that parental supervision was reduced during the lockdown, leading to a rise in burn cases.27 Perhaps, parents were distracted by the multitude of tasks at hand and struggled to keep track of their children’s activities and supervise them at all times. Moreover, some families could not afford to hire a babysitter or count on their children’s extracurricular activities since all in-person classes were shut down. Other solutions for childcare that families used to rely on, such as the support of older relatives became irrelevant, given their age group’s high-risk profile for contracting COVID-19. The abovementioned situation was made even more complicated for parents who were classified as essential workers, as they continued going in to work daily, sometimes without having the means for arranging proper supervision for their children. In some cases, children were left to be supervised by older, yet minor siblings.
During the lockdown period (March 15, 2020–April 30, 2020), 127 burn patients were admitted to one of Israel’s 20 trauma centers for at least one day of hospitalization. Evaluation of age group susceptibility to burn injuries between 2017 and 2019 revealed a relatively higher incidence in younger children, especially among patients aged 0 to 3 years (40.79%), as supported by prior studies.7,19,20,28 Throughout the lockdown, the occurrence of burn injuries in this same age group increased even further, a finding that was statistically significant (55.91% vs 40.79%, P = .002). On one hand, this increase may be explained by the higher occurrence of cooking and dining activities during the lockdown period. In most cases, the household kitchen environment is not as well-suited for the prevention of burn injuries as supervised kindergartens, whose layout includes a kitchen area with restricted access as well as safe water temperatures at the basin.
While an increase in activities around the kitchen may represent one component of the increase in burn injuries in children between the ages of 0 and 3 years, an additional component is the developing curiosity that is typical of children in these ages. More importantly, there is an imbalance between the level of curiosity and the level of mental preparedness required for preventing and responding to accidents around the kitchen.29 As previously reported in the literature, pediatric patients often sustain burn injuries from hot liquids when reaching up to an elevated surface such as the kitchen countertop or stovetop, or coming in contact with hot tap water when using a sink or showering.30–33 Impetuous behavior or underdeveloped motor skills may render children more susceptible to kitchen-related accidents. All of these factors were further complicated by the need for supervision of children in these age groups, which may have been interrupted during the lockdown as parents were now juggling multiple tasks, including working from home and looking after their children.
Meanwhile, adults above the age of 17 sustained less burn injuries during the lockdown period when compared to paralleling dates in 2017–2019 (30.71% vs 42.40%, P = .015). Within the adult subgroups, young adults between 17 and 29 years of age were particularly less susceptible to burn injuries during the mandatory curfew relative to paralleling periods in 2017–2019 (16.46% vs 7.09%, P = .007). As part of the lockdown, many of these individuals, who presumably used to work at places such as restaurants, pubs, stores, or factories, now had to stay home as these places had to close.
Further analysis of the adult and pediatric patient populations according to sex revealed a higher incidence of burn injuries among males during both the lockdown and the paralleling dates between 2017 and 2019 (64.94% vs 60.63%, P = .36), a finding that has also been described in previous studies.17,31,34 Male predominance when it comes to burn injuries is likely influenced by environmental, psychosocial, and socioeconomic factors.20
With regard to injury location, the fraction of burns occurring in the domestic environment significantly increased during the lockdown period (90.55% vs 74.60%, P = .0001). This finding is consistent with prior studies, which showed that most burns, particularly among the pediatric population, occurred at a domestic environment.16,30,32 This increase can be attributed to the stay home mandate for most of the population, the school shutdowns, and the workforce reduction during the COVID-19 lockdown.
When examining the different etiologies of burn injuries, we found scalds to represent the most common cause in both the lockdown period and paralleling periods. The fraction of scald injuries was significantly larger during the COVID-19 lockdown compared to the paralleling dates in 2017–2019 (58.68% vs 71.65%, P = .007). This, along with the finding that burn injuries were more prevalent at the domestic environment, may underline the trend toward more in-home cooking and dining activities as a result of the stay-home mandate. This is in contrast to regular times, when many meals take place at school, work, or restaurant. Meanwhile, burn injuries caused by fire decreased during the lockdown period as compared to paralleling periods (17.89% vs 10.24%, P = .036). The larger diversity in etiologies of burn injuries identified for the 2017–2019 dates is consistent with previous studies.17
Analysis of the data according to geographical location revealed an increase in the fraction of burn patients in southern Israel (15.75% vs 8.77%, P = .0182). This finding may be explained by the region’s high prevalence of the Bedouin population, some of whom continue to live as semi-nomads to this day. As described in a previous study, this population constitutes approximately half of the burns in southern Israel.35 The Bedouin population’s socio-economic status is limited by their level of education and poor living conditions, which consequently places them at an increased risk for burn injuries. Specifically, their increased predisposition may be explained by the overcrowding that is characteristic of the Bedouin families, as well as the poor organization as it relates to cooking and heating. Of note, most of the daily life happens on the floor, and both hot beverages and cooking over an open fire are mainstays of the Bedouin cuisine, thus exposing children who play near the cooking space to scald injuries or burns caused by fire.36–38 During the lockdown, this trend has likely been exacerbated since children spent an even larger amount of their time at an environment with numerous hazards for burn injuries.
Despite the difference in etiologies of burn injuries, there was no significant difference in the TBSA burned between the COVID-19 lockdown period and the paralleling periods in 2017–2019 (P = .89). Similarly, the ratio of patients who required hospitalization for longer than 7 days (40.94% vs 38.82%, P = .0970) and the fraction of patients requiring surgical intervention (7.09% vs 10.2%, P = .2833) did not differ between the studied periods.
STRENGTHS AND LIMITATIONS
This was a retrospective study of data collected from the INTR. Logic tests are built in the data entry software and therefore ensure standardization and uniformity of the data used. Furthermore, quality assurance was independently performed by the Gertner institute. However, data collected in the present study only accounts for hospitalized burns and does not take into consideration non-hospitalized burns. Despite this limitation, we believe that the trends observed in our study provide an important account of the studies phenomenon, as the TBSA burned and the severity of injury were not significantly different between the two study periods.
Despite the evident limitations, this study does provide an overview of burn admissions in Israel during a unique time period. Additionally, it may be used to further elaborate on the epidemiology of burn injuries within this geographical area.
CONCLUSION
The COVID-19 outbreak and the subsequent lockdown allowed us to investigate the different causes and conditions that predispose to burn injuries during such unique and unforeseeable circumstances. The present study demonstrated an increase in the ratio of burn injuries among infants and toddlers up to 3 years of age. In contrast, this ratio decreased among children between 7 to 16 years of age and young adults aged 17 to 29. Since younger children are already at an increased risk for burns in the domestic environment during regular times, the COVID-19 lockdown only aggravated this trend.
Furthermore, the study results pointed to a decrease in occupational injuries, which coincided with Israel’s mandated workforce reduction. This finding is supported by the observation that adult burns are mostly workplace-related. Among children, particularly toddlers in the age group of 0 to 3, the lockdown period taught us that the domestic environment is not necessarily safe or well-suited for prolonged homestay when parental supervision may be lacking. Overall, the main etiology of burns in both studied periods was scald injuries. This incidence of scald injuries was even more pronounced during the lockdown period, possibly due to cooking and dining activities occurring more frequently. These results may improve our understanding of the inherent susceptibility of various circumstances to burn injuries, and likewise, assist us in developing burn preventive strategies, such as campaigns or guides that will instruct parents in the event of additional lockdowns or similar circumstances in the future.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest statement. None.
Contributor Information
Dani Kruchevsky, Plastic & Reconstructive Surgery Department, Rambam Health Care Campus, Haifa, Israel.
Shir Levanon, Rappaport Faculty of Medicine, Technion Institute, Haifa, Israel.
Adi Givon, Israel National Center for Trauma and Emergency Medicine Research, Gertner Institute for Epidemiology and Health Policy Research, Tel Hashomer, Israel.
Moran Bodas, Israel National Center for Trauma and Emergency Medicine Research, Gertner Institute for Epidemiology and Health Policy Research, Tel Hashomer, Israel; School of Public Health, Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel.
Yitzchak Ramon, Plastic & Reconstructive Surgery Department, Rambam Health Care Campus, Haifa, Israel.
Yehuda Ullmann, Plastic & Reconstructive Surgery Department, Rambam Health Care Campus, Haifa, Israel.
Assaf A Zeltzer, Plastic & Reconstructive Surgery Department, Rambam Health Care Campus, Haifa, Israel; Rappaport Faculty of Medicine, Technion Institute, Haifa, Israel.
Israeli Trauma Group:
Asaf Acker, Nimrod Aviran, Hany Bahouth, Alon Bar, Alexander Becker, Alexander Braslavsky, Dmitry Fadeev, Adam Lee Goldstein, Ilia Grevtsev, Igor Jeroukhimov, Asaf Kedar, Alexander Korin, Milad Qarawany, Alon Schwarz, Wael Shomar, Dror Soffer, Michael Stein, Moris Venturero, Michael Weiss, Ori Yaslowitz, and Itay Zoarets
REFERENCES
- 1. Li Q, Guan X, Wu Pet al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 2020;382:1199–207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Statement on the Second Meeting of the International Health Regulations. Emergency committee regarding the outbreak of novel coronavirus (2019-nCoV). 2005, accessed 9 June 2020; available from https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov); Internet.
- 3. Gorbalenya AE, Baker SC, Baric RSet al. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol 2020;5:536–44. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med 2020;27:1–4. doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Israel coronavirus: 18,180 cases and 299 deaths. Worldometer, accessed 9 June 2020; available from https://www.worldometers.info/coronavirus/country/israel/; Internet.
- 6. Othman N, Kendrick D. Epidemiology of burn injuries in the East Mediterranean Region: a systematic review. BMC Public Health 2010;10:83. doi: 10.1186/1471-2458-10-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Haik J, Liran A, Tessone Aet al. Burns in Israel: demographic, etiologic and clinical trends, 1997-2003. Isr Med Assoc J 2007;9:659–62. [PubMed] [Google Scholar]
- 8. Hultman CS, Tong WT, Surrusco Met al. To everything there is a season: impact of seasonal change on admissions, acuity of injury, length of stay, throughput, and charges at an accredited, regional burn center. Ann Plast Surg 2012;69:30–4. doi: 10.1097/SAP.0b013e31823f3df0. [DOI] [PubMed] [Google Scholar]
- 9. Ruckart P, Orr M. Temporal trends of acute chemical incidents and injuries—Hazardous Substances Emergency Events Surveillance, nine states, 1999–2008. MMWR Suppl. 2015;64:10–7. [PubMed] [Google Scholar]
- 10. Chen XJ, Sun WJ, Wang Jet al. Epidemiology of bedside stove burns in a retrospective cohort of 5089 pediatric patients. Burns 2014;40:1761–9. doi: 10.1016/j.burns.2014.03.018. [DOI] [PubMed] [Google Scholar]
- 11. Yao Y, Liu Y, Zhou Jet al. The epidemiology of civilian inpatients’ burns in Chinese military hospitals, 2001-2007. Burns 2011;37:1023–32. doi: 10.1016/j.burns.2011.03.021. [DOI] [PubMed] [Google Scholar]
- 12. Rainey S, Cruse CW, Smith JSet al. The occurrence and seasonal variation of accelerant-related burn injuries in central Florida. J Burn Care Res 2007;28:675–80. doi: 10.1097/BCR.0b013E318148C86E. [DOI] [PubMed] [Google Scholar]
- 13. Castner J, Yin Y, Loomis Det al. Medical Mondays: ED utilization for medicaid recipients depends on the day of the week, season, and holidays. J Emerg Nurs 2016;42:317–24. doi: 10.1016/j.jen.2015.12.010. [DOI] [PubMed] [Google Scholar]
- 14. Trehan K, Healy J, Gregg SCet al. Are burn unit admissions increased during weekends and certain holidays? J Emerg Trauma Care 2017;2:6; available from https://www.imedpub.com/archive/ipjetc-volume-2-issue-2-year-2017.html; Internet; accessed 30 May 2020. [Google Scholar]
- 15. Kai-Yang L, Zhao-Fan X, Luo-Man Zet al. Epidemiology of pediatric burns requiring hospitalization in China: a literature review of retrospective studies. Pediatrics 2008;122:132–42. doi: 10.1542/peds.2007-1567. [DOI] [PubMed] [Google Scholar]
- 16. Verey F, Lyttle MD, Lawson Zet al. When do children get burnt? Burns 2014;40:1322–8. doi: 10.1016/j.burns.2014.01.010. [DOI] [PubMed] [Google Scholar]
- 17. Forjuoh SN. Burns in low- and middle-income countries: a review of available literature on descriptive epidemiology, risk factors, treatment, and prevention. Burns 2006;32:529–37. doi: 10.1016/j.burns.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 18. Blom L, Klingberg A, Laflamme Let al. Gender differences in burns: a study from emergency centres in the Western Cape, South Africa. Burns 2016;42:1600–8. doi: 10.1016/j.burns.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 19. Goldman S, Aharonson-Daniel L, Peleg K. Childhood burns in Israel: a 7-year epidemiological review. Burns 2006;32:467–72. doi: 10.1016/j.burns.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 20. Lee CJ, Mahendraraj K, Houng Aet al. Pediatric burns: a single institution retrospective review of incidence, etiology, and outcomes in 2273 burn patients (1995-2013). J Burn Care Res 2016;37:e579–85. doi: 10.1097/BCR.0000000000000362. [DOI] [PubMed] [Google Scholar]
- 21. Rimmer RB, Weigand S, Foster KNet al. Scald burns in young children- a review of arizona burn center pediatric patients and a proposal for prevention in the hispanic community. J Burn Care Res 2008;29:595–605. doi: 10.1097/BCR.0b013e31817db8a4. [DOI] [PubMed] [Google Scholar]
- 22. Moore JX, McGwin G, Griffin RL. The epidemiology of firework-related injuries in the United States: 2000-2010. Injury. 2014;45:1704–9. doi: 10.1016/j.injury.2014.06.024. [DOI] [PubMed] [Google Scholar]
- 23. Abeyasundara SL, Rajan V, Lam Let al. The changing pattern of pediatric burns. J Burn Care Res 2011;32:178–84. doi: 10.1097/BCR.0b013e31820aada8. [DOI] [PubMed] [Google Scholar]
- 24. Teo AIC, Van As AB, Cooper J. A comparison of the epidemiology of paediatric burns in Scotland and South Africa. Burns 2012;38:802–6. doi: 10.1016/j.burns.2012.04.010. [DOI] [PubMed] [Google Scholar]
- 25. Population of Israel on the Eve of 2020, accessed 29 Mar. 2021; available from https://www.cbs.gov.il/en/mediarelease/Pages/2019/Population-of-Israel-on-the-Eve-of-2020.aspx.; Internet.
- 26. Viner RM, Russell SJ, Croker H.et al. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Heal. 2020;4:397–404. doi: 10.1016/S2352-4642(20)30095-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sethuraman U, Stankovic C, Singer Aet al. Burn visits to a pediatric burn center during the COVID-19 pandemic and “Stay at home” period. Burns 2021;47:491–2. doi: 10.1016/J.BURNS.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Othman N, Kendrick D, Al-Windi A. Childhood burns in Sulaimaniyah province, Iraqi Kurdistan: a prospective study of admissions and outpatients. Burns 2015;41:394–400. doi: 10.1016/j.burns.2014.07.008. [DOI] [PubMed] [Google Scholar]
- 29. Peck MD. Epidemiology of burns throughout the world. Part I: distribution and risk factors. Burns 2011;37:1087–100. doi: 10.1016/j.burns.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 30. Riedlinger DI, Jennings PA, Edgar DWet al. Scald burns in children aged 14 and younger in Australia and New Zealand - an analysis based on the Burn Registry of Australia and New Zealand (BRANZ). Burns 2015;41:462–8. doi: 10.1016/j.burns.2014.07.027. [DOI] [PubMed] [Google Scholar]
- 31. Johnson DM, White LJ, Gilstrap Jet al. Fireworks and seafood boils: the epidemiology of burns in Louisiana. J Burn Care Res 2020;41:280–8. doi: 10.1093/JBCR/IRZ159. [DOI] [PubMed] [Google Scholar]
- 32. Drago DA. Kitchen scalds and thermal burns in children five years and younger. Pediatrics 2005;115:10–6. doi: 10.1542/peds.2004-0249. [DOI] [PubMed] [Google Scholar]
- 33. Delgado J, Ramírez-Cardich ME, Gilman RHet al. Risk factors for burns in children: crowding, poverty, and poor maternal education. Inj Prev 2002;8:38–41. doi: 10.1136/ip.8.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Williams FN, Sljivic S, Chrisco Let al. Acuity is seasonal in a tertiary care burn center. J Burn Care Res 2020;41:359–62. doi: 10.1093/JBCR/IRZ172. [DOI] [PubMed] [Google Scholar]
- 35. Cohen AD, Gurfinkel R, Glezinger Ret al. Pediatric burns in the Bedouin population in southern Israel. Sci World J. 2007;7:1842–7. doi: 10.1100/tsw.2007.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mohammed M, Michal H-L, Isack Ket al. Burn injuries and adolescents in Israel. Int J Adolesc Med Health 2004;16:201–6. doi: 10.1515/IJAMH.2004.16.3.201. [DOI] [PubMed] [Google Scholar]
- 37. Broides A, Assaf M. Home accidents in Arab Bedouin Children in Southern Israel. 2016;7:207–14. doi: 10.1177/13674935030073006. [DOI] [PubMed] [Google Scholar]
- 38. Gurfinkel R, Cohen AD, Glezinger Ret al. Burns at the soroka university medical center - a two-year experience. Ann Burns Fire Disasters 2007;20:3–6; available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3188045/; Internet; accessed 25 Oct. 2021. [PMC free article] [PubMed] [Google Scholar]