Abstract
Objective
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) nucleic acid detection “re-positive” phenomenon is encountered clinically. The accuracy of a viral nucleic acid test is crucial to prevent reintroduction of the virus into the community. This study evaluated the effect of virus culturing on increasing the sensitivity and specificity of real-time polymerase chain reaction (RT-PCR) detection and viral genomic sequencing.
Methods
A series of tenfold dilutions of a SARS-CoV-2 viral stock were conducted and cultured for either 24 or 48 hours. The viral load of cultured samples was determined by RT-PCR. The cultured and non-cultured samples of 1x 50% tissue culture infectious dose (TCID50) were sequenced using metagenomic next-generation sequencing. The depth and coverage of SARS-CoV-2 genome were measured.
Results
The lowest viral load detectable in a sample with RT-PCR was 0.01 TCID50. After a 24-h culture, the viral ORF 1ab and N-gene cycle threshold (CT) values were reduced by 4.4 points and 1 point, respectively. One TCID50 viral load of post 24-h culture revealed the sequence depth reached an average of 752 reads, compared with 0.15 in the nonculture; furthermore, the coverage was 99.99% while 6.42% in the nonculture.
Conclusion
These results indicate that virus culturing can significantly increase the viral load, which can increase the certainty of true-positive detection of the viral nucleic acids, and improve the quality of virus genomic sequencing.
Keywords: re-positive, SARS-CoV-2, virus culturing, viral load, diagnosis, sequencing
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID-19), has become a global threat to public health. In the early stages of the COVID-19 pandemic, SARS-CoV-2 was detected in human samples by next-generation sequencing (NGS), electron microscopy, and cell culture.1 The full genome sequence of the virus (29870 bp, excluding the poly [A] tail), was reported on January 10, 2020. Several laboratories began to develop molecular detection tools that targeted open reading frame (ORF) 1ab, the RNA-dependent RNA polymerase N gene, and the E regions of the viral spike genes.2-4 SARS-CoV-2 can be rapidly identified owing to advances in virus detection techniques, including real-time polymerase chain reaction (RT-PCR), reverse transcription loop-mediated isothermal amplification, and RT-PCR. RT-PCR is a widely used technique for diagnosing SARS-CoV-2 infection, and several nucleic acid test kits have been commercialized for clinical use.4
At present, the Omicron variant of SARS-CoV-2, generating BA 1.1, BA 2, and BA 3, have been identified in more than 100 countries and regions worldwide.5,6 The N501Y, H655Y, N679K, and P681H mutations have been shown to have a higher rate of transmission7 than other variants. Given the continuous emergence of new variants, subtype analysis is a critical part of SARS-CoV-2 diagnosis. RT-PCR is used to detect the presence of SARS-CoV-2 viral RNA, and genome sequencing could be meaningful for finding novel mutations and identifying the subtypes.
Several studies have shown that discharged COVID-19 patients can retest positive for SARS-CoV-2 after a period of time. The phenomenon of these “re-positive” SARS-CoV-2 PCR cases has been attributed to various mechanisms. First, the virus might not have been completely eliminated in these recovered patients. In the initial test after discharge, the viral load may have been below the RT-PCR detection threshold, leading to a false negative. The second possibility is that although the live virus was completely killed by the immune system, degraded viral nucleic acid in the airways was still able to be detected, and these viral RNA fragments may have been transported from the lower respiratory tract to the nose/oropharynx region. Third, because the re-positive detection of viral nucleic acid often occurs after discharge, the possibility of re-infection and secondary infection cannot be ignored. Clarifying these 3 possibilities is crucial for COVID-19 pandemic control. In addition, RT-PCR carries some risk of yielding a false-negative result when there is a low viral load in a sample. A low viral load can be related to (1) the source of the collected sample, (2) the conditions of the sample collection and transport, and (3) the sensitivity of the RT-PCR kit.8 To address these problems, the virus culturing technique, a gold standard for the investigation of viruses, was assessed. By culturing virus from recovered patients, it becomes possible to distinguish live virus from noninfectious viral RNA. Furthermore, viral cultures could provide sufficient amounts of viral nucleic acid for RT-PCR to avoid false-negative results and to determine the virus subtypes through genetic sequencing. In this study, we evaluated the effectiveness of virus culturing with Vero E6 cells on the detection limit of RT-PCR and genetic sequencing of SARS-CoV-2.
Methods
Virus Dilution
A SARS-CoV-2 sample (Genebank accession No. MT123290.1) was obtained from a clinical isolate. Using the Reed–Muench method, the viral titer was determined by the 50% tissue culture infectious dose (TCID50) according to the cytopathic effect. A SARS-CoV-2 virus stock (107 TCID50/mL) was prepared in phosphate-buffered saline (PBS) and diluted to 10, 1, 0.1, 0.01, and 0.001 TCID50/mL in a biosafety III laboratory.
Isolation and Culture
A SARS-CoV-2 dilution series (10, 1, 0.1, 0.01, 0.001 TCID50/mL) was cultured respectively, for 24 and 48 h in African green monkey kidney epithelial (Vero E6) cells in triplicate (n = 3). The cells were cultured at 37°C and 5% CO2 in infection medium, which was Dulbecco’s Modified Eagle Medium (Gibco) supplemented with 2% fetal bovine serum and 100 U/mL mycillin.
To construct the RNA library for metagenomics next-generation sequencing, we cultured the 1 TCID50 titer of the virus in Vero E6 cells for 24 h. Three study groups were established: (1) negative control (NC): only Vero E6 cells; (2) nonculture (VC0, virus titer: 1 TCID50); and (3) 24 h culture (VC24, virus titer: 1 TCID50). Before sequencing, Vero E6 cells were added to the nonculture group to make the sequencing background consistent with that of the cultured group.
RNA Purification and RT-PCR Detection of SARS-CoV-2
In a biosafety III laboratory, total RNA was extracted from 100 µL samples of the 3 groups (NC, VC0, VC24) using the Vazyme FastPure Viral DNA/RNA Mini Kit (Vazyme) following the manufacturer’s instructions. The RT-PCR assay was performed using the 2019-nCoV Nucleic Acid Detection Kit (fluorescence PCR) (Daan Gene), which is commercially available and widely used clinically in China and detected by the 7500 Real-Time PCR System (Fisher Scientific). A positive detection was made when signals for both nucleic acid targets (ORF 1ab and N) were within the valid range (CT ≤ 40).
Library Preparation, Sequencing, and Analysis
For each sample, total RNA was quantified using the Qubit RNA HS Assay Kit (Thermo Fisher Scientific). First-strand complementary deoxyribonucleic acid (cDNA) was synthesized with the HiScriptIII 1st Strand cDNA Synthesis Kit in the presence of specific reagents to ensure that only RNA was used as a template. Double-stranded cDNA was synthesized using DNA Polymerase I Klenow Fragment exo (Vazyme), dNTP mix (Thermo Fisher), and Random Hexamer Primer (Thermo Fisher); the products were purified with Agencourt AMPure XP beads (Beckman). Next, the DNA libraries were prepared using the TruePrep DNA Library Prep Kit V2 for Illumina (Vazyme). The concentration of the DNA libraries was measured by Qubit. Finally, the sequencing was carried out on an Illumina NextSeq 500 system with 75 cycles and using the associated reagent kit.
For each library, low-quality reads, adaptor sequences, noncomplex reads, and duplicated reads were removed using Fastp (v0.22.0). The remaining reads were mapped against the SARS-CoV-2 genome (accession No. NC_045512.2) with Bowtie2 (v2.3.5.1). Samtools (v1.13) was used to extract aligned reads for genome sequence assembly. The abundance level of SARS-CoV-2 was estimated by mapping reads against the corresponding genome and was measured as the read count using Bedtools (v2.3.5.1). A SARS-CoV-2 genome coverage plot of the 3 samples (genome coverage >80% and average depth >100×) was generated by an R script within the Gviz (v1.34.1) package. Aligned reads of the 3 samples were assembled using SPAdes (v3.15.3) to retrieve their full-length individual genome sequence with a single parameter named “isolate.” The NGS data for the nonculture and culture samples were uploaded to the Gene Expression Omnibus (accession No. GSE189731).
Statistical Analysis
Statistical analysis was performed using GraphPad Prism 7.0 software. The mean and standard deviation of the cycle threshold (CT) values of ORF 1ab and N of SARS-CoV-2 were calculated.
Results
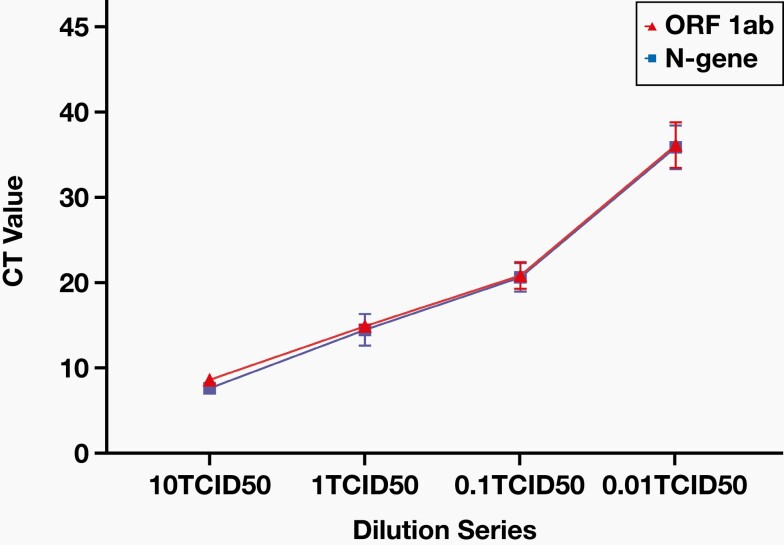
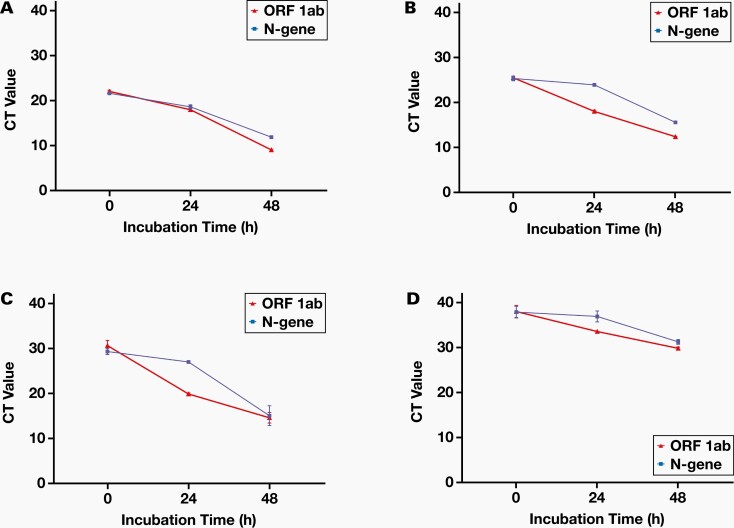
A low viral load in a sample may be the main reason for false-negative viral nucleic acid testing results initially, prior to re-positive detection. To test this hypothesis, we constructed a dilution series (10, 1, 0.1, 0.01, and 0.001 TCID50 titers) of the SAR-CoV-2 culture to determine the lowest viral load detectable by the RT-PCR kit. The lowest viral load that the kit could detect was 0.01 TCID50, which was weakly positive (Figure 1, Table 1). To evaluate the effect of virus culturing on the sensitivity of the RT-PCR method, we cultured the virus with initial concentrations of 10, 1, 0.1, 0.01, and 0.001 TCID50 for 24 h or 48 h, followed by RT-PCR detection. The virus with initial 0.001 TCID50 titer could not be effectively amplified (Figure 2, Table 2). However, when the virus with initial 0.01 TCID50 titer was cultured for 24 h, the virus ORF 1ab CT value decreased by 4.4, and the virus N-gene CT value reduced by 1. After 24 h of culture, the virus titers of 0.1 TCID50 and above showed an average decrease of greater than 9 for the ORF 1ab CT value and an average decrease of 2 for the virus N-gene CT value. These results indicate that if the virus titer of a specimen is as low as 0.01 TCID50, then after culturing the detection sensitivity may be dramatically increased.
Figure 1.
CT) values of the SARS-CoV-2 dilution series.
Table 1.
Average RT-PCR CT Values of SARS-CoV-2 at Serial Dilutions
| Probe | CT Value (Mean ± SD, n = 3) | ||||
|---|---|---|---|---|---|
| 10TCID50 | 1TCID50 | 0.1TCID50 | 0.01TCID50 | 0.001TCID50 | |
| ORF 1ab | 24.34 ± 0.10 | 27.47 ± 0.08 | 30.45 ± 0.78 | 38.1 ± 1.33 | Negative |
| N-gene | 23.84 ± 0.17 | 27.26 ± 0.92 | 30.34 ± 0.84 | 37.95 ± 1.28 | Negative |
CT, cycle threshold; RT-PCR, real-time polymerase chain reaction; TCID50, 50% tissue culture infectious dose.
Figure 2.
The relationship between real-time polymerase chain reaction cycle threshold (CT) values of ORF1ab/N-gene and different SARS-CoV-2 culturing conditions. A, 10TCID50. B, 1TCID50. C, 0.1TCID50. D, 0.01TCID50. TCID50, 50% tissue culture infectious dose.
Table 2.
Average RT-PCR CT Values of SARS-CoV-2 After Culturing for 24 h and 48 h with Different Initial Viral Concentrations
| Virus titer | Probe | CT Value (Mean ± SD, n = 3) | ||
|---|---|---|---|---|
| 0 h | 24 h | 48 h | ||
| 10TCID50 | ORF 1ab | 22.01 ± 0.29 | 13.25 ± 0.27 | 9.0 ± 0.15 |
| N-gene | 21.59 ± 0.37 | 18.65 ± 0.47 | 11.85 ± 0.13 | |
| 1TCID50 | ORF 1ab | 25.42 ± 0.20 | 17.96 ± 0.27 | 12.32 ± 0.04 |
| N-gene | 25.28 ± 0.52 | 23.85 ± 0.30 | 15.51 ± 0.04 | |
| 0.1TCID50 | ORF 1ab | 30.61 ± 1.15 | 19.87 ± 0.23 | 14.58 ± 1.18 |
| N-gene | 29.29 ± 0.65 | 26.99 ± 0.11 | 15.04 ± 2.21 | |
| 0.01 TCID50 | ORF 1ab | 38.1 ± 1.33 | 33.63 ± 0.25 | 29.9 ± 0.30 |
| N-gene | 37.95 ± 1.28 | 36.99 ± 1.22 | 31.34 ± 0.52 | |
| 0.001 TCID50 | ORF 1ab | Negative | Negative | Negative |
| N-gene | Negative | Negative | Negative |
CT, cycle threshold; RT-PCR, real-time polymerase chain reaction; TCID50, 50% tissue culture infectious dose.
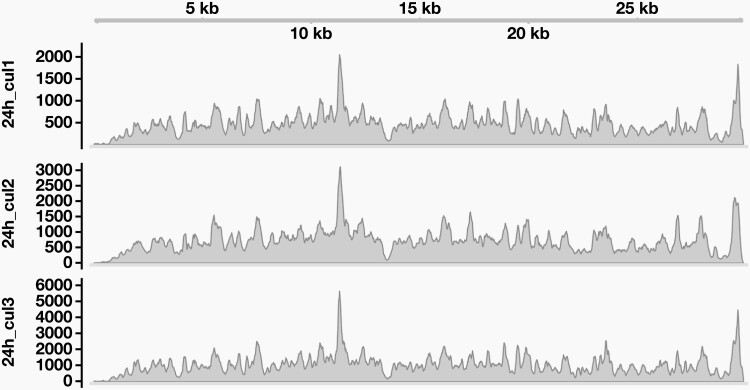
Genome sequencing has been applied to identify SARS-CoV-2 variants in re-positive cases. However, virus genomic sequencing requires a high viral load. Because the noncultured viral loads in a specimen at concentrations of 0.01 or 0.1 TCID50 were extremely low, they could not provide enough material for sequencing. Therefore, our study used the 1 TCID50 noncultured samples and 24 h cultured samples with initial 1TCID50 viral concentration for NGS. The sequencing results of the 24-h culture were significantly improved over those of the noncultured sample, reaching an average of 752 reads, while the nonculture one had only 0.15 reads (Table 3). Furthermore, the coverage of the 24-h culture sample was 99.99%, while that of the nonculture one was only 6.42% (Figure 3). These results indicate that the 24-h culturing, with initial 1 TCID50 viral loading, could render NGS to achieve good results for mutation and subtype analyses.
Table 3.
Coverage and Mean Depth of Sequencing for Cultured and Noncultured Samples
| Sample | Coverage (%) | Mean Depth |
|---|---|---|
| 24 h culture | 99.9911 | 752.031 |
| Nonculture | 6.419637 | 0.147666 |
| Negative control | 0 | 0 |
Figure 3.
Coverage of the SARS-CoV-2 genome. 24 h_cul1–3, 24-h culture of SARS-CoV-2 with 3 replicates.
Discussion
The phenomenon of recovered patients showing a re-positive SARS-CoV-2 nucleic acid detection has been widely reported. Zhang et al9 reported the clinical and laboratory characteristics of 7 patients in Guangdong, China, who were readmitted owing to re-positive PCR detection. Four patients tested positive from rectal swabs, 2 tested positive from throat swabs, and 1 patient tested positive after both throat and rectal swabs positive.9 A 72-year-old woman from South Korea tested re-positive by RT-PCR 6 days after 2 negative results.10 In Switzerland, 2 older women with underlying heart diseases had positive nasopharyngeal swab detection results 18 and 21 days after 2 consecutive negative results.11 If re-positive patients are not isolated, SARS-CoV-2 could potentially spread in the community. Therefore, it is important to identify the nature of the re-positivity, including the infectivity and virus subtype.
The cause of re-positivity needs to be clarified. There are several reasons for a re-positive detection, such as an originally false-negative RT-PCR results, reactivation of the virus, persistent infection, or a new infection with another strain.12
Low viral loads are thought to be the main cause of false-negative results. Additionally, the viral load in a sample is affected by the method and location of sample collection. As found in this study, a 0.01 TCID50 virus titer was the minimum threshold that could be detected by this RT-PCR kit. Thus, a viral load below this level may lead to false-negative results when using this RT-PCR kit. A systematic review found that different RT-PCR kits have different sensitivities, ranging from 71% to 98%.13 Therefore, the minimum virus titer necessary for detection depends on the performance of individual kits. Moreover, RT-PCR cannot distinguish between infectious and noninfectious viral RNA.11 Our results showed that as long as the virus titer was above 0.01 TCID50, an incubation of at least 24 h greatly increased the viral load. Virus culturing not only increases the viral load but also helps to differentiate whether live virus is present in a sample; this process can increase the sensitivity and specificity of viral nucleic acid detection. Regarding virus reactivation, findings have been limited. One study found that some individuals could be virus carriers even after they recovered.14 However, Arevalo-Rodriguez et al13 found that most re-positive cases were asymptomatic and had low viral loads, which suggests that re-positivity is attributed to a low viral load rather than to reactivation. The possibility of persistent infection with the same subtype is also low, and re-positivity is more likely related to prolonged viral shedding.15 As the virus is still evolving, it is possible to become infected with another variant. To identify subsequent infections, the virus could be cultured as in this study to increase the depth and coverage of sequencing, providing the possibility for high-quality NGS results. To prevent community transmission of live virus from re-positive cases, we recommend that samples from these patients should be isolated and cultured before RT-PCR and high-throughput sequencing to increase the detection rate and analyze the virus subtype.
In the future, we will conduct a cohort study of re-positive cases to evaluate the effectiveness of virus culturing for diagnosis.
Conclusion
Virus culturing is beneficial for diagnosing SARS-CoV-2 infection and identifying the subtype in re-positive cases.
Acknowledgments
We thank all the participants in this study.
Glossary
Abbreviations
- SARS-CoV-2
severe acute respiratory syndrome coronavirus 2
- TCID50
50% tissue culture infectious dose
- CT
cycle threshold
- ORF
open reading frame
- RT-PCR
real-time polymerase chain reaction
- Vero E6
African green monkey kidney epithelial cell; cDNA, complementary deoxyribonucleic acid
Contributor Information
Zhiqi Zeng, State Key Laboratory of Respiratory Disease, National Clinical Research Center for Respiratory Disease, Guangzhou Institute of Respiratory Health, the First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China.
Hua Guo, Zhuhai Baso Diagnostics, Zhuhai, China.
Liping Chen, State Key Laboratory of Respiratory Disease, National Clinical Research Center for Respiratory Disease, Guangzhou Institute of Respiratory Health, the First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China.
Zhengshi Lin, State Key Laboratory of Respiratory Disease, National Clinical Research Center for Respiratory Disease, Guangzhou Institute of Respiratory Health, the First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China.
Wenda Guan, State Key Laboratory of Respiratory Disease, National Clinical Research Center for Respiratory Disease, Guangzhou Institute of Respiratory Health, the First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China.
Yutao Wang, State Key Laboratory of Respiratory Disease, National Clinical Research Center for Respiratory Disease, Guangzhou Institute of Respiratory Health, the First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China.
Haiming Jiang, State Key Laboratory of Respiratory Disease, National Clinical Research Center for Respiratory Disease, Guangzhou Institute of Respiratory Health, the First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China.
Xiao Wu, State Key Laboratory of Respiratory Disease, National Clinical Research Center for Respiratory Disease, Guangzhou Institute of Respiratory Health, the First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China.
Yong Yin, Zhuhai Baso Diagnostics, Zhuhai, China.
Zelong Gao, Zhuhai Baso Diagnostics, Zhuhai, China.
Canxiong Chen, State Key Laboratory of Respiratory Disease, National Clinical Research Center for Respiratory Disease, Guangzhou Institute of Respiratory Health, the First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China.
Zifeng Yang, State Key Laboratory of Respiratory Disease, National Clinical Research Center for Respiratory Disease, Guangzhou Institute of Respiratory Health, the First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China; Guangzhou Key Laboratory for Clinical Rapid Diagnosis and Early Warning of Infectious Diseases, Guangzhou, China.
Disclosure
Hua Guo was employed by Baso Diagnostics.
Funding
This work was supported by the National Key Research and Development Program of China (Grant No. 2020YFA0708002), Zhongnanshan Medical Foundation of Guangdong Province (Grant No. ZNSA-2020012), Science and Technology Program of Foshan (Grant No. 2020001000206), Science and Technology Program of Guangzhou (Grant No. 202102100003), China Evergrande (Grant No. 2020GIRHHMS23, 2020GIRHHMS01, 2020GIRHHMS18), National Natural Science Foundation of Guangdong (Grant No. 2020B1515120045), National Natural Science Foundation of Guizhou (Grant No. [2020]4Y219), Science and Technology Bureau Project of Dongguan (Grant No. 202071715001114), Science and Technology Program of Guangzhou (Grant No. 202206010025), Key Research and Development Program of Guangdong Province (Grant No. 2021A1111120009).
Data Availability
The datasets generated and analyzed during the current study are available in the Gene Expression Omnibus (accession No. GSE189731).
References
- 1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Corman VM, Landt O, Kaiser M, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25(3):2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chen L, Liu W, Zhang Q, et al. RNA based mNGS approach identifies a novel human coronavirus from two individual pneumonia cases in 2019 Wuhan outbreak. Emerging Microbes Infect. 2020;9(1):313–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chu D, Pan Y, Cheng S, et al. Molecular diagnosis of a novel coronavirus (2019-nCoV) causing an outbreak of pneumonia. Clin Chem. 2020;66(4):549–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Meo SA, Meo AS, Al-Jassir FF, Klonoff DC. Omicron SARS-CoV-2 new variant: global prevalence and biological and clinical characteristics. Eur Rev Med Pharmacol Sci. 2021;25(24):8012–8018. [DOI] [PubMed] [Google Scholar]
- 6. Thakur V, Ratho RK. OMICRON (B.1.1.529): a new SARS-CoV-2 variant of concern mounting worldwide fear. J Med Virol. 2022;94(5):1821–1824. [DOI] [PubMed] [Google Scholar]
- 7. Kimura I, Kosugi Y, Wu J, et al. The SARS-CoV-2 Lambda variant exhibits enhanced infectivity and immune resistance. Cell Reports. 2022;38(2):110218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Xu K, Cai H, Shen Y, et al. Management of COVID-19: the Zhejiang experience [in Chinese]. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2020;49(2):147–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhang B, Liu S, Dong Y, et al. Positive rectal swabs in young patients recovered from coronavirus disease 2019 (COVID-19). J Infect. 2020;81(2):e49–e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chae KJ, Jin GY, Lee CS, Lee HB, Lee JH, Kwon KS. Positive conversion of COVID-19 after two consecutive negative RT-PCR results: a role of low-dose CT. Eur J Radiol. 2020;129:109122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ravioli S, Ochsner H, Lindner G. Reactivation of COVID-19 pneumonia: a report of two cases. J Infect. 2020;81(2):e72–e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Osman AA, Al Daajani MM, Alsahafi AJ. Re-positive coronavirus disease 2019 PCR test: could it be a reinfection? New Microbes New Infect. 2020;37:100748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Arevalo-Rodriguez I, Buitrago-Garcia D, Simancas-Racines D, et al. False-negative results of initial RT-PCR assays for COVID-19: a systematic review. PLoS One. 2020;15(12):e0242958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lan L, Xu D, Ye G, et al. Positive RT-PCR test results in patients recovered from COVID-19. JAMA. 2020;323(15):1502–1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Xu K, Chen Y, Yuan J, et al. Factors associated with prolonged viral RNA shedding in patients with COVID-19. Clin Infect Dis. 2020;71(15):799–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed during the current study are available in the Gene Expression Omnibus (accession No. GSE189731).