Highlights
-
•
Shorter time since injury and higher mobility levels as well as poor physical health are associated with higher risk of falls and fall-related injuries, respectively in wheelchair users with spinal cord injury.
-
•
The findings indicate good discriminant ability and clinical utility of the factors presented to identify wheelchair users who are at risk of falls and fall-related injuries.
KEYWORDS: Accidental falls, Rehabilitation, Risk factors, Spinal cord injuries, Wheelchairs
List of abbreviations: ADL, activities of daily living; AIS, American Spinal Injury Association Impairment Scale; AUC, area under the receiver operating characteristic curve; FOF, fear of falling; OR, odds ratio; QOL, quality of life; SCI, spinal cord injury; SCIM III, Spinal Cord Independence Measure III; TAI, Transfer Assessment Instrument; WHOQOL-BREF, World Health Organization Quality of Life-Brief Version; WST, Wheelchair Skill Test
Abstract
Objective
To identify risk factors for falls and fall-related injuries for wheelchair users with spinal cord injury (SCI).
Design
Cross-sectional study.
Setting
Community setting.
Participants
Fifty-nine community dwelling wheelchair users (N=59), 47.5% male, median age of 52.5 years (IQR, 21 years) with chronic SCI, median time since injury of 16.6 years (IQR, 27.3 years).
Interventions
No intervention.
Main Outcome Measures
Outcomes were incidence of falls and fall-related injuries. Participants reported on falls and fall-related injuries experienced in the previous 6 months. Independent variables were self-reported and performance-based measures. Self-reported measures included demographics, characteristics of SCI, fear of falling, psychological measures, functional independence, wheelchair skills, environmental barriers, quality of life, and community participation. Performance-based measures included transfer quality and sitting balance assessments. Logistic regression analyses were conducted to identify factors influencing falls and fall-related injuries.
Results
In total, 152 falls and 30 fall-related injuries were reported from a total of 37 fallers. After logistic regression analysis, the model with the greatest levels of clinical utility and discriminative ability for falls (sensitivity 81%; specificity 55%; area under the receiving operating characteristic curve [AUC] statistics=0.73; 95% CI, 0.60-0.86) included the variables of shorter time since SCI, high mobility level, and having received education on fall prevention. The model for fall-related injuries (sensitivity 79%; specificity 75%; AUC statistics=0.77; 95% CI, 0.59-0.96) included the variables of older male individual, lower physical health score, and having received education on fall prevention.
Conclusions
The regression models presented may be used to identify wheelchair users with SCI at greater risk of falls and fall-related injuries. The findings may help to refer those in need to tailored fall and fall-related injury prevention programs. The findings presented in this study were based on a relatively small sample convenience; therefore, further prospective studies with a larger sample size are warranted.
Falls are common among individuals living with spinal cord injury (SCI). A recent review estimated that approximately 69% of nonambulatory individuals with SCI experience at least 1 fall in a period of 6-12 months.1 Overall, the consequences of falls are far reaching, resulting in individual and societal burdens. Those consequences include physical injuries, fear of falling (FOF), and associated activity curtailment.2, 3, 4 Falls resulting in physical injuries might lead to immobility and bed dependency, which in turn may result in secondary complications, such as pressure ulcers.5 Falls are therefore associated with an increased need for health care utilization contributing to a high socioeconomic cost.2, 3, 4
The effectiveness of fall prevention programs depends on, among other factors, the appropriate identification of the risk predictors for falls. For this purpose, reliable screening tools are essential to allow early identification of individuals with SCI at risk of falls and refer them for appropriate fall preventions programs. Among nonambulatory individuals with SCI, few studies have specifically investigated potential fall risk predictors.6, 7, 8 Those predictors include pain, alcohol abuse, greater motor function, previous falls, number of SCI years, and shorter length of wheelchair, previous recurrent falls, age, and male sex.6, 7, 8
Moreover, pain, greater motor score, previous falls, home entrance inaccessibility, and quality of life (QOL) were identified as predictors of fall-related injuries.6,7 As evidenced above, only 3 studies6, 7, 8 have specifically investigated fall predictors, and only 2 have examined predictors of falls associated with injury in this population.
Consequently, there is a limited understanding of fall risk factors specific for wheelchair users with SCI, ultimately leading to a lack of evidence-based approaches to fall prevention and a reliable fall screening tool to identify individuals at risk of falls in clinical settings. Thus, the purpose of this study is to determine factors associated with falls and fall-related injuries among nonambulatory individuals with SCI. In addition, the study aimed to determine which combination of self-reported and performance-based outcome measures presents with the highest level of discriminant ability to identify individuals at risk of falls and fall-related injuries in this population.
Methods
This is a cross-sectional observational study design. An online survey was conducted between January 2021 and July 2021 in the United States using the Research Electronic Data Capture9 survey platform. In addition to the survey, sitting balance and transfer abilities were assessed remotely. The study was reviewed and approved by the Office for the Protection of Research Subjects at the University of Illinois, Urbana-Champaign (#20718). All participants provided remote informed consent before taking part in the study. The informed consent document was sent to potential participants electronically through Research Electronic Data Capture (REDCap). They were instructed to read and asked any follow-up questions to the research team, if necessary, before signing the informed consent document.
A convenience sample of individuals with SCI were recruited to participate in the study. Participants were recruited from SCI support groups across the United States, Facebook posts, personal communication, and magazine or newsletter advertisements. Participants were invited to take part in the study if they met the following inclusion criteria: (1) 18 years or older with a chronic SCI for at least 12 months after injury, (2) motor complete injury classified as American Spinal Injury Association Impairment Scale (AIS) A or B and motor incomplete injury AIS C who are wheelchair users, (3) level of injury between C5 and above L5, (4) self-report use of a wheelchair for at least 75% of mobility, (5) able to communicate with the research team through smartphone or laptop video conferencing software, and (6) able to understand English. Participants were excluded if they presented with any additional medical conditions that might affect their ability to perform the tests. Individuals with AIS D and E were excluded because they present with motor incomplete injury.
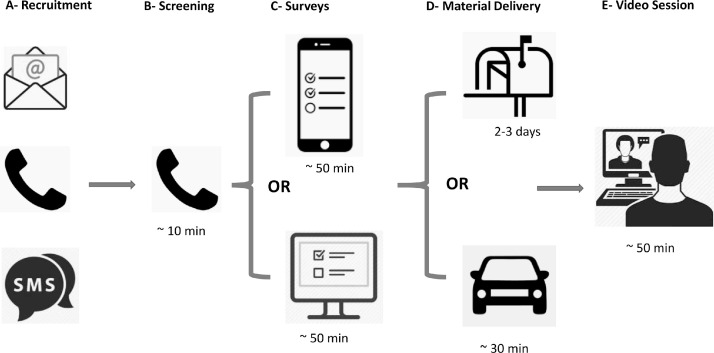
Because of the restrictions placed on human participant research because of the COVID-19 pandemic, all testing procedures were performed remotely. Figure 1 illustrates the steps for the study procedures. After screening for eligibility criteria, participants completed a demographic survey, surveys on falls and fall-related injuries, and questionnaires described in outcome measures. After completion of the online surveys, participants and a researcher met over a video call to perform sitting balance and transfer testing with the assistance of a family member, caregiver, or friend.
Fig 1.
(A) Potential participants contacted the research group and manifested their interest in participating in the study. (B) Potential participants were screened over the phone for eligibility criteria by a researcher. (C) Eligible participants were provided with a link to complete demographics and surveys. (D) A researcher delivered assessment packages to study participants who completed the surveys through drop-off or mail. (E) Participants met with the researcher to perform remote sitting balance and transfer assessments.
Outcome measures
Participants first completed the following self-reported outcome measures:
-
1.
Demographics, characteristics of SCI, and a survey to collect information on the frequency of falls and fall-related injuries experienced by the participants in the previous 6 months. A fall was defined as an unintentional event in which one comes to rest on the ground, floor, or other lower level.10 Participants also responded to a question about whether they ever received education on fall prevention from a health care professional.
-
2.
Fear of falling: Participants responded “yes” or “no” to a question developed to assess FOF11: “Are you worried or concerned that you might fall?” In addition, participants completed the SCI Falls Concern Scale questionnaire.12
-
3.
Psychological measures: The Hospital Anxiety and Depression Scale was used to assess symptoms of depression and anxiety.13
-
4.
Functional independence: The Spinal Cord Independence Measure (SCIM) III was used to evaluate functional independence.14 The SCIM III assesses domains related to self-care, respiration and sphincter control, and mobility.
-
5.
Environmental barriers: The Craig Hospital Inventory of Environmental Factors-Short Form was used to quantify environmental barriers.15
-
6.
Wheelchair skills: The Wheelchair Skills Test 5.0 questionnaire (WST-Q) was used to assess wheelchair skills.16 The Wheelchair Skills Test 5.0 questionnaire evaluates domains such as frequency, confidence, and performance.
-
7.
Quality of life: The World Health Organization Quality of Life-Brief version (WHOQOL-BREF) was used to quantify QOL.17 The WHOQOL-BREF evaluates domains of physical health, psychological health, social relationships, and environment.
-
8.
Community participation: The Community Participation Indicators questionnaire was used to assess participants’ community participation.18 The questionnaire evaluates the following domains: importance of participation and control over participation.
After the completion of the self-reported measures, participants’ sitting balance was evaluated remotely using the Function in Sitting Test,19,20 Trunk Control Test,21,22 T-shirt Test,23,24 and modified Functional Reach Test.22,25 A paper ruler that was sent to the participants was used to estimate reaching distance during the modified Functional Reach Test. The validity and reliability of remote assessment of sitting balance measures have been fully described elsewhere.26 An assessment of transfer quality was performed using the Transfer Assessment Instrument (TAI).27,28 The procedures for the remote TAI assessment are also fully described elsewhere.27,28 A paper goniometer sent to the participants was used during the TAI evaluation. Finally, participants completed a self-assessment of their transfer assessment using the self-TAI.29
Statistical analyses
Data were coded, entered, and analyzed using IBM SPSS Statistics version 25.a Counts and frequencies were used to describe categorical variables, and normality of data was assessed using the Kolmogorov-Smirnov test. Because of the nonnormal distribution, Mann-Whitney U tests were used to examine differences in continuous variables. The associations between fall status and categorical independent variables were tested using chi-square or Fisher exact tests.
Multivariable logistic regression analyses were conducted to examine factors associated with falls and fall-related injuries. Number of falls reported by participants was regarded as the dependent variable of the study, dichotomized as 0 fall (nonfaller) or ≥1 (faller). Fall-related injuries were also used as a dependent variable and dichotomized as 0 injury (no injury) or ≥1 injury (injury). Individual missing data were excluded on a case-by-case basis from the analysis.
Independent variables were selected based on the results of previous studies.6,7 Correlation between variables was examined using Spearman rank correlation (ρ). To avoid collinearity in the multivariable logistic regression models and to reduce the number of independent variables, variables with correlation <0.4 were entered in the bivariate analysis. For variables assessing similar constructs even if the correlation was <0.4, only the one with lowest P value was included in the full logistic model. All variables with a P value ≤.15 from the bivariate analysis were considered for inclusion in the logistic regression analysis. This value of ≤.15 was chosen because it is recommended when using regression analysis in smaller cohorts and ensured no relevant variable was left out of the model.30
Two logistic regression models (full and final) were built for each dependent variable. The logistic regression models were analyzed with final independent variables assessed at a P value <.05. Model building was iterative and guided with interpretability, parsimony, and the evaluation of the Wald statistic for each variable at each step. Goodness-of-fit of the final reduced model was assessed using the Hosmer and Lemeshow test and the Nagelkerke R2 value. Odds ratios (ORs) and 95% CIs were reported for factors associated with falls and fall-related injuries. Receiver operating characteristic curve analysis was carried out to select the optimal cutoff point to dichotomize the composite measure of the logistic regression model and the continuous variables. The area under the receiving operating characteristic curve (AUC) statistic value was estimated. AUC statistic values >0.7 were considered appropriate to discriminate between 2 groups.31
Results
A total of 70 eligible individuals agreed to participate in the study. Of the 70 participants, 11 did not provide any data and were excluded from the analysis. Fifty-nine individuals were included in the analyses. The demographics and clinical information of the participants are presented in tables 1 and 2, respectively. No significant differences were observed for demographics and clinical information between fallers and nonfallers.
Table 1.
Characteristics of study participants
| Characteristic | Total Sample (N=59) | Fallers (n=37, 63%) | Nonfallers (n=22, 37%) | P Value |
|---|---|---|---|---|
| Sex, n (%), male; female | 28 (47.5); 31 (52.5) | 21 (56.8); 16 (43.2) | 7 (31.8); 15 (68.2) | .06 |
| Age (y), median (IQR); min-max | 52.5 (21); 19-72 | 51 (22); 19-69 | 53 (17); 26-72 | .23 |
| Race, n (%), Asian; Black; White; Hispanic | 3 (5.1); 6 (10.2); 48 (81.4); 2 (3.4) | 3 (8.1); 4 (10.8); 29 (78.4); 1 (2.7) | 0 (0.0); 2 (9.1); 19 (86.4); 1 (4.5) | .56 |
| Height (cm), mean (SD); min-max | 171.5 (17.1); 137.2-190.5 | 173.0 (19.0); 137.2-190.5 |
170.2 (19.0); 147.3-188.0 |
.77 |
| Weight (kg), median (IQR); min-max | 75 (27); 42-125 | 71.4 (29); 42-120 | 78 (26); 55-125 | .33 |
| Mobility aid, n (%), power WC; manual WC | 17 (28.8); 42 (71.2) | 8 (21.6); 29 (78.4) | 9 (40.9); 13 (59.1) | .11 |
| Cause of SCI, n (%), traumatic; nontraumatic | 43 (72.9); 16 (27.1) | 25 (67.6); 12 (32.4) | 18 (81.8); 4 (18.2) | .23 |
| Time since injury (y), median (IQR); min-max | 16.5 (27.3); 0.5-57 | 11 (27.8); 1-54 | 23.5 (27.3); 0.5-57 | .06 |
| Level of injury, n (%), cervical; high thoracic; low thoracic; lumbar; unknown | 13 (22.0); 15 (25.4); 22 (37.3); 5 (8.5); 4 (6.8) | 5 (13.5); 12 (32.4); 14 (37.8); 3 (8.1); 3 (8.1) | 8 (36.4); 3 (13.6); 8 (36.4); 2 (9.1); 1 (4.5) | .24 |
NOTE. Results are expressed as frequencies and percentages for categorical variables and mean ± SD or median (IQR) for continuous variables.
Abbreviation: WC, wheelchair.
Table 2.
Clinical information of study participants
| Characteristic | Total Sample (N=59) | Fallers (n=37, 63%) | Nonfallers (n=22, 37%) | P Value |
|---|---|---|---|---|
| Education on fall prevention, n (%),* yes; no | 30 (57.7); 22 (42.3) | 16 (53.0); 14 (47.0) | 14 (64.0); 8 (36.0) | .36 |
| FOF, n (%), no; yes | 16 (27.0); 43 (73.0) | 13 (81.0); 24 (56.0) | 3 (19.0); 19 (44.0) | .07 |
| SCI-FCS, n (%) | 28 (14) | 30 (11) | 24 (8) | .18 |
| HADS, median (IQR), Depression; Anxiety | 5 (5); 5 (6) | 3 (4); 4 (7) | 7 (3); 9 (4) | .78; .57 |
| Balance measures,† FIST; TCT; T-shirt Test (s); mFRT (cm); Self-TAI; TAI | 44 (12); 22 (7); 4.8 (2.7); 10.8 (7.8); 6.9 (1.7); 8.2 (1.1) | 44 (12); 23 (7); 5.2 (3.6); 10.8 (7.2); 6.9 (1.8); 8.0 (1.2) | 43 (6); 19 (4); 4.2 (0.1); 7.0 (7.1); 7.3 (0.4); 8.5 (0.3) | .73; .55; .39; .33; .73; .47 |
| Community participation; CPI-Importance; CPI-Control | 50 (15); 55 (8) | 48 (17); 55 (9) | 50 (9); 55 (9) | .28; .96 |
| CHIEF-SF, median (IQR) | 21 (16) | 21 (15) | 21 (16) | .60 |
| SCIM III, median (IQR), self-care; respiration and sphincter control; mobility; total | 18 (3); 28 (13); 16 (6); 62 (16) | 18 (2); 29 (11) 16 (4); 62 (14) |
18 (7); 27 (13) 15 (9); 62 (25) |
.43; .49 .09; .32 |
| WST, median (IQR), capacity; confidence; performance | 83 (22); 82 (21); 65 (31) | 82 (18); 81 (21); 69 (31) | 80 (30); 81 (25); 63 (29) | .51; .61 .68 |
| WHOQOL, median (IQR), physical health; psychological health; social relationships; environment | 65 (11); 69 (12); 65 (31); 88 (25) | 63 (24); 69 (14); 65 (31) 81 (27) |
65 (6); 69 (17) 69 (27); 88 (22) |
.25; .28 .22; .34 |
NOTE. Results are expressed as frequencies and percentages for categorical variables and median (IQR) for continuous variables. N=59 unless otherwise stated.
Abbreviations: CHIEF-SF, Craig Hospital Inventory of Environmental factors-Short Form; CPI, community participation indicator; FIST, Function in Sitting Test; HADS, Hospital Anxiety and Depression Scale; mFRT, Modified Functional Reach Test; SCI-FCS, Spinal Cord Injury-Falls Concern Scale; TCT, Trunk Control Test; WHOQOL, World Health Organization Quality of Life; WST, Wheelchair Skills Test.
n=52.
n=18.
A total of 152 falls were reported in the 6 months prior to data collection: 22 participants (37%) did not experience a fall and were categorized as nonfallers, and 37 (63%) experienced at least 1 fall and were categorized as fallers. Also, from the 37 participants who experienced at least 1 fall, data on the most recent injuries associated with a fall were available for 30 participants. From those 30, a total of 14 (46.7%) reported fall-related injuries and 16 (53.3%) did not report any fall-related injuries after the fall.
After bivariate logistic analysis for fall variable, 8 potential predictor variables presented with a P value ≤.15 and were deemed suitable for further multivariable logistic analysis (appendix 1): sex, time since injury, recurrent fallers (>2 falls), SCIM III self-care, SCIM III mobility, and SCIM III total score. In addition, age was added as a confounder predictor and education on fall prevention was included as a variable of interest. After analysis for multicollinearity, 5 variables (age, time since injury, recurrent falls, SCIM III mobility score, and education on falls) were included in the full multivariable logistic regression analysis (table 3).
Table 3.
Full and final models for multivariate logistic regression analysis (N=59) to identify individuals with SCI at risk of falls
| Variable | Full Model |
Final Model |
|||||
|---|---|---|---|---|---|---|---|
| P Value | β | OR (95% CI) | P Value | β | OR (95% CI) | AUC Value (95% CI) | |
| Constant | - | - | - | .32 | −1.06 | 0.35 | - |
| Time since injury | .08 | −0.04 | 0.96 (0.92-1.01) | .04* | −0.05 | 0.96 (0.92-0.99) | 0.35 (0.21-0.50) |
| SCIM III mobility | .03 | 0.16 | 1.17 (1.01-1.36) | .03* | 0.15 | 1.16 (1.01-1.33) | 0.63 (0.48-0.78) |
| Education on falls: yes | .22 | 0.81 | 2.25 (0.62-8.11) | .15 | 0.92 | 2.52 (0.71-8.88) | 0.44 (0.28-0.59) |
| Age | .65 | −0.01 | 1.00 (0.94-1.04) | - | - | - | - |
| Recurrent fallers: yes | .16 | −0.92 | 0.40 (0.11-1.47) | - | - | - | - |
P < 0.05.
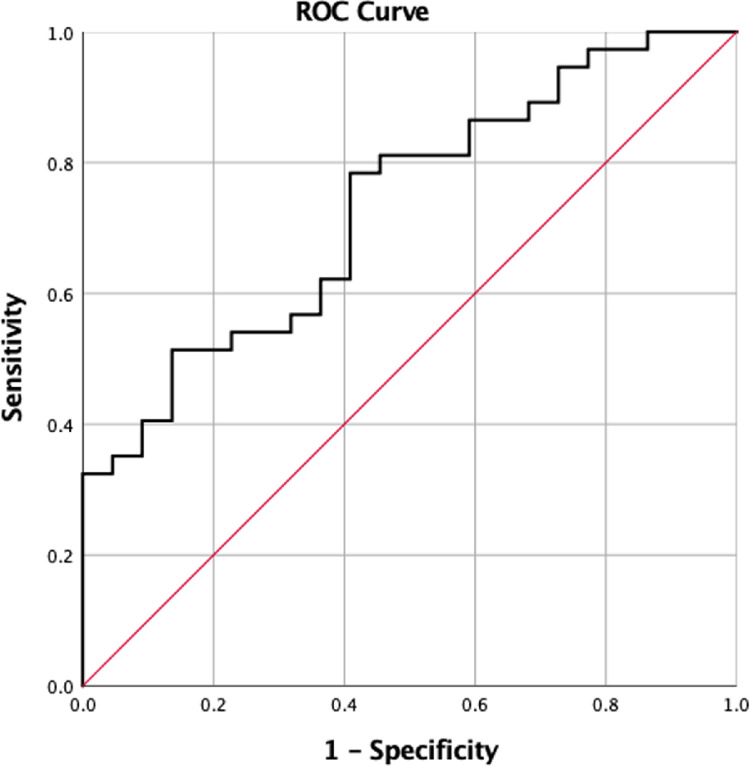
Table 3 also shows the final multivariable logistic regression model with 3 associated factors. The results indicate that participants with shorter time since SCI had approximately 1-time higher odds of being fallers than those with longer time since SCI. Also, participants with greater mobility levels in the SCIM III had 1.16 higher odds of being fallers than those with lower mobility levels in the SCIM III. The AUC statistic (fig 2) of the final model was 0.73 (95% CI, 0.60-0.86, P<.01). This is higher than the AUC values of the included variables in isolation (see table 3). The model's sensitivity and specificity at an optimal cutoff of 0.53 were estimated at 81% and 55%, respectively. The model had a good fit (Hosmer and Lemeshow test, P=.30, Nagelkerke R2=0.22).
Fig 2.
ROC analysis of the final model for risk of falls, AUC=0.73 (95% CI, 0.60-0.86), P<.01. Abbreviation: ROC, receiver operating characteristic.
After bivariate logistic analysis for fall-related injuries variable, there were 5 potential predictor variables with a P value ≤.15 that were deemed suitable for further full multivariable logistic regression analysis (appendix 2). These factors included age, sex, WHOQOL physical health, Craig Hospital Inventory of Environmental Factors-Short Form, and education on fall prevention (table 4). Sex was included because it was regarded as a confounder. Also, education on fall prevention was included.
Table 4.
Full and final models for multivariate logistic regression analysis (N=59) to identify individuals with SCI at risk of fall-related injury
| Variable | Full Model |
Final Model |
|||||
|---|---|---|---|---|---|---|---|
| P Value | β | OR (95% CI) | P Value | β | OR (95% CI) | AUC Value (95% CI) | |
| Constant | - | - | - | .60 | −1.06 | 0.92 | - |
| WHOQOL-PH | .09 | −0.07 | 0.93 (0.86-1.01) | .04* | −0.05 | 0.92 (0.85-0.99) | 0.34 (0.14-0.54) |
| Age | .08 | 0.09 | 1.09 (0.99-1.21) | .07 | 0.15 | 1.08 (0.99-1.18) | 0.64 (0.43-0.85) |
| Sex: Female | .05 | −2.21 | 0.11 (0.01-1.02) | .12 | 0.92 | 0.20 (0.03-1.49) | 0.60 (0.40-0.81) |
| Education on falls: Yes | .91 | −1.08 | 0.34 (0.13-6.03) | .92 | −0.10 | 0.91 (0.14-5.91) | 0.54 (0.33-0.75) |
| CHIEF-SF | .10 | −0.08 | 0.92 (0.85-1.01) | - | - | - | - |
Abbreviation: WHOQOL-PH: World Health Organization Quality of Life-physical health.
P < 0.05.
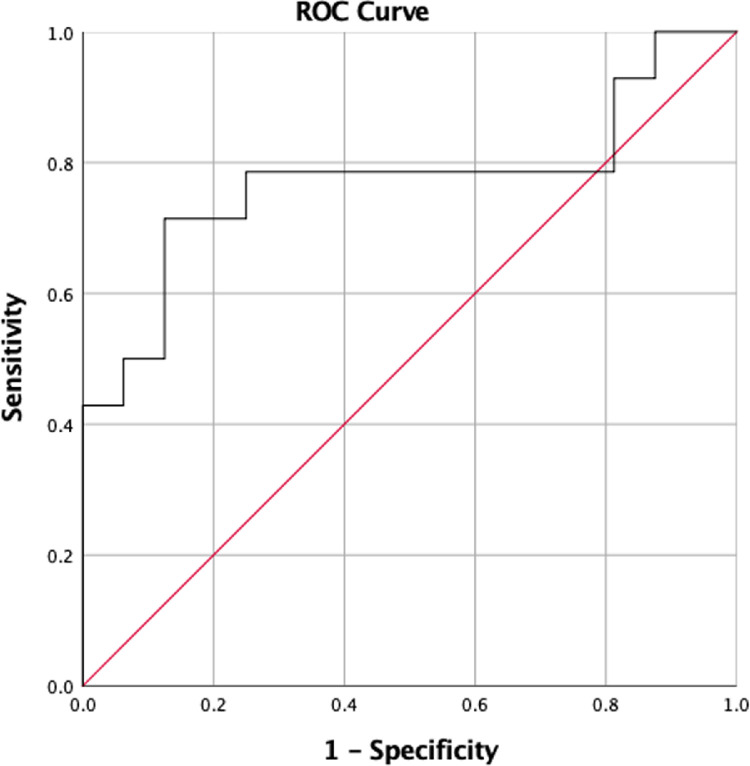
Table 4 also shows the final multivariable logistic regression model with 4 predictor-associated factors. The results indicate that for each unit increase in WHOQOL physical health (higher score on physical health domain of quality of life), the OR of experiencing a fall-related injury decreases by 8% (OR, 0.92; P=.04). The AUC statistic (fig 3) of the final model was 0.77 (95% CI, 0.59-0.96, P=.01). This is higher than the AUC values of the included variables in isolation (see table 4). The model's sensitivity and specificity at an optimal cutoff of 0.37 were estimated at 79% and 75%, respectively. The model had an adequate fit (Hosmer and Lemeshow test, P=.05, Nagelkerke R2=0.39).
Fig 3.
ROC analysis of the final model for fall-related injury, AUC=0.77 (95% CI, 0.59-0.96), P=.01. Abbreviation: ROC, receiver operating characteristic.
Discussion
This research investigated factors associated with falls and fall-related injuries among nonambulatory individuals with SCI. After analyzing a broader range of variables compared with previous studies,6, 7, 8 time since injury and SCIM III mobility score were found to be significant risk indicators for falls in this population. The model containing these indicators presented with a sensitivity of 81%, specificity of 55%, and AUC statistic value of 0.73 (95% CI, 0.60-0.86). In addition, the physical health domain of WHOQOL was found to be the only significant risk indicator for fall-related injuries. The model containing the WHOQOL-physical health presented with a sensitivity of 79%, specificity of 71%, and AUC statistic value of 0.77 (95% CI, 0.59-0.96). These findings provide further, insight on factors associated with falls and fall-related injuries in this population. This information is useful to improve the ability of clinicians to identify individuals at risk for falling and develop fall risk screening tools for this population. In addition, the identification of factors associated with falls may be used to inform the development of effective fall prevention programs.
Notably, shorter time since SCI and greater mobility function reported in our study as factors associated with falls align with the predictors previously highlighted by Nelson et al7 in this population. Individuals with more recent onset of SCI are often adults who are highly active, engaging in both basic and instrumental activities of daily living (ADL). Engaging in ADL with few experiences using a wheelchair might lead to an increase exposure to falls. Also, individuals with greater mobility function are generally more independent and more engaged in their ADL, which might lead to falls. Other studies have also highlighted greater mobility function,8 higher level of ability,32 and higher levels of physical activity33 as predictors of falls in individuals with SCI. Other fall predictors, such as pain in the previous 2 months, alcohol abuse, and a shorter length of wheelchair reported by Nelson et al,7 were not examined in our study. However, the model presented in our study, with 2 factors, achieved a sensitivity of 81% and an AUC of 0.73. While our model presented with good discriminant ability and sensitivity, the moderate specificity (55%) indicates that some nonfallers may be incorrectly identified as fallers using our model. These individuals might be unnecessarily referred to fall prevention programs. This unnecessary referral to fall prevention programs will only benefit these individuals to improve their knowledge about fall prevention.34,35 Nonetheless, our model will allow clinicians to identify most individuals at risk of falls, communicate the probability of falling to these individuals, and refer them to appropriate fall prevention programs.
The subanalysis of those who experienced at least 1 fall indicates that WHOQOL-physical health was the only factor associated with fall-related injuries among nonambulatory individuals with SCI. This finding suggests that increased scores on the physical health domain of the WHOQOL questionnaire was associated with decreasing odds of having a fall-related injury. The physical health domain of the WHOQOL questionnaire evaluates components related to energy and fatigue, mobility, physical pain and discomfort, sleep and rest, work capacity, performance of ADL, and medication.17 For example, pain and discomfort may lead to a dysfunctional seated posture in a wheelchair, resulting in decreased efficiency in movements during transfers or reaching for an object, which could contribute to an increased risk of sustaining an injury after a fall. Considering the components evaluated by the physical health domain of the WHOQOL during fall risk screenings is important to appropriately identify individuals at risk of fall-related injuries.
Our results align with the report by Forslund et al,6 who indicated general QOL as the only predictor of fall-related injury in this population. Because QOL is broad, our results add to knowledge about the specific domain (physical health) associated with fall-related injuries. Moreover, our findings presented with a sensitivity and specificity of 79% and 75%, respectively, and an AUC of 0.77, indicating good discriminant ability of the model. The alignment between our results and the findings by Forslund et al6 indicates that clinicians might use the physical health domain of WHOQOL-BREF to identify nonambulatory individuals at risk of falls and refer them to appropriate fall prevention programs.
Surprisingly, having received education on fall prevention was not found as a factor associated with fall related outcomes. Although, this is the first study to analyze this variable as a potential risk factor, the findings suggest that the current education on fall prevention for individuals with SCI may not be affecting fall-related outcomes. The interpretation of this finding was somewhat limited because the specific components, length of the educational programs, and which professional provided the education received by the participants was not investigated and details on those programs were lacking. However, further examination of the influence of fall prevention programs on fall-related outcomes is needed to inform clinicians whether improvement of those programs is necessary.
Compared with ambulatory individuals with SCI among whom performance-based measures have shown ability to differentiate between fallers and nonfallers,36,37 performance-based measures such as balance measures including the Function in Sitting Test, Trunk Control Test, or TAI were not found to be associated with falls and fall-related injuries among nonambulatory individuals with SCI. This might be because of the lack of sensitivity of clinical performance-based measures used for nonambulatory individuals.38 Efforts should be made by clinicians and researchers to improve the sensitivity of those outcome measures to facilitate their inclusion in research and clinical settings. Also, the complexity of falls from a wheelchair might explain the absence of associations between clinical performance-based measures and falls among nonambulatory individuals. Although the performance-based measures evaluated in this study were not significant to identify individuals at risk of falls, findings from qualitative research highlight the importance of these measures. Participants often report poor balance, transfers, and reaching for items to be associated with falls.6,39,40 Accurate prediction of falls from a wheelchair likely requires the integration of the factors associated with falls described in this study and the integration of findings from qualitative research described in previous studies.6, 7, 8
Study limitations
There are several limitations that should be considered in this study. First, we included a relatively small sample size in our study. Specifically, the subanalysis of fall-related injuries was performed with a small number of fallers. When comparing the literature on fall predictors among nonambulatory individuals with SCI to the existing literature on ambulatory individuals36,37 or individuals with other neurologic diseases,41,42 it becomes evident that further research with a bigger sample size is required to provide more robust findings. Another limitation is that our analyses were based on self-reported and retrospective fall data. Compared with prospective fall tracking, retrospective fall data may be influenced by recall bias, therefore limiting the interpretation of our results. Also, the sample of convenience might be affected by the respondent bias, which may hinder the evaluation of the representativeness of our sample. Lastly, we suspect that most participants underreported minor fall-related injuries. Future studies using emerging fall detection devices that will automatically and accurately detect and provide an objective report of falls might help to provide more robust findings.43,44
Conclusions
In summary, our findings confirm the need to increase awareness about falls and fall-related injuries in this population. During fall risk screenings, clinicians should consider time since injury and level of mobility, as well as components included in the physical health domain of the quality of life questionnaire, such as level of energy and reports of fatigue and physical pain. Carefully considering these findings and reports are important because they have been found to be associated with falls and fall-related injury, respectively. Identifying nonambulatory individuals with SCI at risk of falls will improve referrals to rehabilitation professionals for enrollment in fall prevention programs in a timely manner. Education on wheelchair-related falls should be incorporated in early stages of SCI rehabilitation process.
Supplier
a. SPSS Version 25.0 for Windows; SPSS Inc, Chicago, IL.
Footnotes
Supported by the Illinois Physical Therapy Association (IPTF 098442).
Disclosures: none.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.arrct.2022.100195.
Appendix. Supplementary materials
References
- 1.Khan A, Pujol C, Laylor M, et al. Falls after spinal cord injury: a systematic review and meta-analysis of incidence proportion and contributing factors. Spinal Cord. 2019;57:526–539. doi: 10.1038/s41393-019-0274-4. [DOI] [PubMed] [Google Scholar]
- 2.Peterson EW, Cho CC, Finlayson ML. Fear of falling and associated activity curtailment among middle aged and older adults with multiple sclerosis. Mult Scler. 2007;13:1168–1175. doi: 10.1177/1352458507079260. [DOI] [PubMed] [Google Scholar]
- 3.Sung J, Shen S, Peterson EW, et al. Fear of falling, community participation, and quality of life among community-dwelling people who use wheelchairs full time. Arch Phys Med Rehabil. 2021;102:1140–1146. doi: 10.1016/j.apmr.2020.11.013. [DOI] [PubMed] [Google Scholar]
- 4.Abou L, Alluri A, Fliflet A, et al. Effectiveness of physical therapy interventions in reducing fear of falling among individuals with neurologic diseases: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2021;102:132–154. doi: 10.1016/j.apmr.2020.06.025. [DOI] [PubMed] [Google Scholar]
- 5.McKinley WO, Jackson AB, Cardenas DD, et al. Long-term medical complications after traumatic spinal cord injury: a regional model systems analysis. Arch Phys Med Rehabil. 1999;80:1402–1410. doi: 10.1016/s0003-9993(99)90251-4. [DOI] [PubMed] [Google Scholar]
- 6.Forslund EB, Jørgensen V, Franzén E, et al. High incidence of falls and fall-related injuries in wheelchair users with spinal cord injury: a prospective study of risk indicators. J Rehabil Med. 2017;49:144–151. doi: 10.2340/16501977-2177. [DOI] [PubMed] [Google Scholar]
- 7.Nelson AL, Groer S, Palacios P, et al. Wheelchair-related falls in veterans with spinal cord injury residing in the community: a prospective cohort study. Arch Phys Med Rehabil. 2010;91:1166–1173. doi: 10.1016/j.apmr.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 8.Jørgensen V, Butler Forslund E, Franzén E, et al. Factors associated with recurrent falls in individuals with traumatic spinal cord injury: a multicenter study. Arch Phys Med Rehabil. 2016;97:1908–1916. doi: 10.1016/j.apmr.2016.04.024. [DOI] [PubMed] [Google Scholar]
- 9.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95 doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lamb SE, Jørstad-Stein EC, Hauer K, et al. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 2005;53:1618–1622. doi: 10.1111/j.1532-5415.2005.53455.x. [DOI] [PubMed] [Google Scholar]
- 11.Tennstedt S, Howland J, Lachman M, et al. A randomized, controlled trial of a group intervention to reduce fear of falling and associated activity restriction in older adults. J Gerontol B Psychol Sci Soc Sci. 1998;53:P384–P392. doi: 10.1093/geronb/53b.6.p384. [DOI] [PubMed] [Google Scholar]
- 12.Boswell-Ruys CL, Harvey LA, Delbaere K, et al. A falls concern scale for people with spinal cord injury (SCI-FCS) Spinal Cord. 2010;48:704–709. doi: 10.1038/sc.2010.1. [DOI] [PubMed] [Google Scholar]
- 13.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 14.Itzkovich M, Gelernter I, Biering-Sorensen F, et al. The Spinal Cord Independence Measure (SCIM) version III: reliability and validity in a multi-center international study. Disabil Rehabil. 2007;29:1926–1933. doi: 10.1080/09638280601046302. [DOI] [PubMed] [Google Scholar]
- 15.Whiteneck GG, Harrison-Felix CL, Mellick DC, et al. Quantifying environmental factors: a measure of physical, attitudinal, service, productivity, and policy barriers. Arch Phys Med Rehabil. 2004;85:1324–1335. doi: 10.1016/j.apmr.2003.09.027. [DOI] [PubMed] [Google Scholar]
- 16.Kirby RL, Dupuis DJ, Macphee AH, et al. The Wheelchair Skills Test (version 2.4): measurement properties. Arch Phys Med Rehabil. 2004;85:794–804. doi: 10.1016/j.apmr.2003.07.007. [DOI] [PubMed] [Google Scholar]
- 17.Skevington SM, Lotfy M, O'Connell KA, et al. The World Health Organization's WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004;13:299–310. doi: 10.1023/B:QURE.0000018486.91360.00. [DOI] [PubMed] [Google Scholar]
- 18.Heinemann AW, Magasi S, Bode RK, et al. Measuring enfranchisement: importance of and control over participation by people with disabilities. Arch Phys Med Rehabil. 2013;94:2157–2165. doi: 10.1016/j.apmr.2013.05.017. [DOI] [PubMed] [Google Scholar]
- 19.Abou L, Sung J, Sosnoff JJ, et al. Reliability and validity of the function in sitting test among non-ambulatory individuals with spinal cord injury. J Spinal Cord Med. 2020;43:846–853. doi: 10.1080/10790268.2019.1605749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Palermo AE, Cahalin LP, Garcia KL, et al. Psychometric testing and clinical utility of a modified version of the Function in Sitting Test for individuals with chronic SCI. Archives of Physical Medicine and Rehabil. 2020;101:1961–1972. doi: 10.1016/j.apmr.2020.06.014. [DOI] [PubMed] [Google Scholar]
- 21.Quinzaños J, Villa AR, Flores AA, et al. Proposal and validation of a clinical trunk control test in individuals with spinal cord injury. Spinal Cord. 2014;52:449–454. doi: 10.1038/sc.2014.34. [DOI] [PubMed] [Google Scholar]
- 22.Abou L, de Freitas GR, Palandi J, et al. Clinical instruments for measuring unsupported sitting balance in subjects with spinal cord injury: a systematic review. Top Spinal Cord Inj Rehabil. 2018;24:177–193. doi: 10.1310/sci17-00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen CL, Yeung KT, Bih LI, et al. The relationship between sitting stability and functional performance in patients with paraplegia. Arch Phys Med Rehabil. 2003;84:1276–1281. doi: 10.1016/s0003-9993(03)00200-4. [DOI] [PubMed] [Google Scholar]
- 24.Boswell-Ruys CL, Sturnieks DL, Harvey LA, et al. Validity and reliability of assessment tools for measuring unsupported sitting in people with a spinal cord injury. Arch Phys Med Rehabil. 2009;90:1571–1577. doi: 10.1016/j.apmr.2009.02.016. [DOI] [PubMed] [Google Scholar]
- 25.Lynch SM, Leahy P, Barker SP. Reliability of measurements obtained with a modified functional reach test in subjects with spinal cord injury. Phys Ther. 1998;78:128–133. doi: 10.1093/ptj/78.2.128. [DOI] [PubMed] [Google Scholar]
- 26.Abou L, Rice LA, Frechette ML, et al. Feasibility and preliminary reliability and validity of remote sitting balance assessments among wheelchair users. Int J Rehabil Res. 2021;44:177–180. doi: 10.1097/MRR.0000000000000458. [DOI] [PubMed] [Google Scholar]
- 27.Worobey LA, Zigler CK, Huzinec R, et al. Reliability and validity of the revised Transfer Assessment Instrument. Top Spinal Cord Inj Rehabil. 2018;24:217–226. doi: 10.1310/sci2403-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Worobey LA, Hibbs R, Rigot SK, et al. Intra- and interrater reliability of remote assessment of transfers by wheelchair users using the Transfer Assessment Instrument (version 4.0) Arch Phys Med Rehabil. 2022;103:816–821. doi: 10.1016/j.apmr.2020.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Worobey LA, Rigot SK, Boninger ML, et al. Concurrent validity and reliability of the Transfer Assessment Instrument Questionnaire as a self-assessment measure. Arch Rehabil Res Clin Transl. 2020;2 doi: 10.1016/j.arrct.2020.100088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Steyerberg EW, Eijkemans MJ, Harrell FE, Jr, et al. Prognostic modelling with logistic regression analysis: a comparison of selection and estimation methods in small data sets. Stat Med. 2000;19:1059–1079. doi: 10.1002/(sici)1097-0258(20000430)19:8<1059::aid-sim412>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 31.Hajian-Tilaki K. Receiver operating characteristic (ROC) curve analysis for medical diagnostic test evaluation. Caspian J Intern Med. 2013;4:627–635. [PMC free article] [PubMed] [Google Scholar]
- 32.Wannapakhe J, Arrayawichanon P, Saengsuwan J, et al. Medical complications and falls in patients with spinal cord injury during the immediate phase after completing a rehabilitation program. J Spinal Cord Med. 2015;38:84–90. doi: 10.1179/2045772313Y.0000000173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Matsuda PN, Verrall AM, Finlayson ML, et al. Falls among adults aging with disability. Arch Phys Med Rehabil. 2015;96:464–471. doi: 10.1016/j.apmr.2014.09.034. [DOI] [PubMed] [Google Scholar]
- 34.Rice LA, Sung JH, Keane K, et al. A brief fall prevention intervention for manual wheelchair users with spinal cord injuries: a pilot study. J Spinal Cord Med. 2020;43:607–615. doi: 10.1080/10790268.2019.1643070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abou L, Qin K, Alluri A, et al. The effectiveness of physical therapy interventions in reducing falls among people with multiple sclerosis: a systematic review and meta-analysis. J Bodyw Mov Ther. 2022;29:74–85. doi: 10.1016/j.jbmt.2021.09.015. [DOI] [PubMed] [Google Scholar]
- 36.Abou L, Ilha J, Romanini F, et al. Do clinical balance measures have the ability to predict falls among ambulatory individuals with spinal cord injury? A systematic review and meta-analysis. Spinal Cord. 2019;57:1001–1013. doi: 10.1038/s41393-019-0346-5. [DOI] [PubMed] [Google Scholar]
- 37.Musselman KE, Arora T, Chan K, et al. Evaluating intrinsic fall risk factors after incomplete spinal cord injury: distinguishing fallers from nonfallers. Arch Rehabil Res Clin Transl. 2021;3 doi: 10.1016/j.arrct.2020.100096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nguyen US, Kiel DP, Li W, et al. Correlations of clinical and laboratory measures of balance in older men and women. Arthritis Care Res (Hoboken) 2012;64:1895–1902. doi: 10.1002/acr.21783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sung J, Trace Y, Peterson EW, et al. Falls among full-time wheelchair users with spinal cord injury and multiple sclerosis: a comparison of characteristics of fallers and circumstances of falls. Disabil Rehabil. 2019;41:389–395. doi: 10.1080/09638288.2017.1393111. [DOI] [PubMed] [Google Scholar]
- 40.Singh H, Scovil CY, Bostick G, et al. Perspectives of wheelchair users with spinal cord injury on fall circumstances and fall prevention: a mixed methods approach using photovoice. PLoS One. 2020;15 doi: 10.1371/journal.pone.0238116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rice LA, Abou L, Denend TV, et al. Falls among wheelchair and scooter users with multiple sclerosis—a review. US Neurol. 2018;14:82–87. [Google Scholar]
- 42.Coote S, Comber L, Quinn G, et al. Falls in people with multiple sclerosis: risk identification, intervention, and future directions. Int J MS Care. 2020;22:247–255. doi: 10.7224/1537-2073.2020-014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Abou L, Fliflet A, Hawari L, et al. Sensitivity of Apple Watch fall detection feature among wheelchair users. Assistive Technol. 2021 May 25. [Epub ahead of print]. [DOI] [PubMed]
- 44.Frechette ML, Abou L, Rice LA, et al. The validity, reliability, and sensitivity of a smartphone-based seated postural control assessment in wheelchair users: a pilot study. Front Sports Act Living. 2020;2 doi: 10.3389/fspor.2020.540930. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.