To the Editor:
In 2020, the University of Washington (UW) removed the race coefficient (Black vs non-Black race) from the 2009 Chronic Kidney Disease Epidemiology Collaboration (2009 CKD-EPIno race) estimated glomerular filtration rate (eGFR) equation in a step toward acknowledging that race is a social and not a biologic construct. Recently, a new eGFR equation, the 2021 Chronic Kidney Disease Epidemiology Collaboration (2021 CKD-EPI) equation, was published, in which the race variable was removed and the coefficients for the other variables (age, sex, and serum creatinine) were recalibrated.1 Subsequently, the National Kidney Foundation and American Society of Nephrology Task Force recommended that the 2021 CKD-EPI equation be implemented for eGFR reporting.2 In these analyses, we examined the effect of the creatinine-based 2021 CKD-EPI and 2009 CKD-EPIno race equations on reclassification of chronic kidney disease stages compared with the 2009 CKD-EPI equation at our institution (UW) and among participants in the National Health and Nutrition Examination Survey (NHANES) to understand the impact of the new eGFR equations in “real-world” populations.
Our study population comprised 2 cohorts: (1) the UW cohort (adults aged ≥18-105 years with serum or plasma creatinine measured in the UW laboratory system between January 1, 2018, and August 15, 2019)3 and (2) the NHANES cohort (adults aged ≥20 years from 3 cycles of NHANES—2013-2014, 2015-2016, and 2017-2018). We first classified individuals into eGFR-based chronic kidney disease stages using the 2009 CKD-EPI equation with eGFR cutoffs ≥90, 60-89, 45-59, 30-44, 15-29, and <15 mL/min/1.73 m2. We then used the 2009 CKD-EPIno race and 2021 CKD-EPI equations and reclassified them into higher or lower eGFR-based chronic kidney disease categories. Full details of methods are available in Item S1.
The analytic population of the UW cohort was 170,941 (Fig S1) and that of the NHANES cohort was 15,392 (Tables S1A and B). For UW patients, the eGFR in Black individuals was lower by a mean (standard deviation) of 13.7 (4.2) and 10.1 (4.9) mL/min/1.73 m2 using the 2009 CKD-EPIno race and 2021 CKD-EPI equations, respectively, than that using the 2009 CKD-EPI equation (Table 1). Similarly, for NHANES participants, the eGFR in non-Hispanic Black individuals was lower by a mean (standard deviation) of 13.9 (4.5) and 10.3 (5.0) mL/min/1.73 m2 using the 2009 CKD-EPIno race and 2021 CKD-EPI equations, respectively, than that using the 2009 CKD-EPI equation (Table 1).
Table 1.
The Difference in Mean and Median eGFR With Different Estimating Equations Among Black and Non-Black Individuals in the UW and NHANES Cohorts
| UW |
NHANES |
|||
|---|---|---|---|---|
| Non-Black Patients | Black Patients | Non-Black Participants | Non-Hispanic Black Participants | |
| eGFR (creatinine-based 2009 CKD-EPI), mL/min/1.73 m2 | ||||
| Mean (SD) | 89.4 (23.4) | 99.8 (30.9) | 92.7 (17.6) | 101.1 (32.7) |
| Median (IQR) | 91.6 (75.9 to 105.3) | 102.6 (81.2 to 121.5) | 97.6 (81.2 to 114.1) | 108.1 (86.9 to 128.2) |
| eGFR (creatinine-based 2009 CKD-EPIno race), mL/min/1.73 m2 | ||||
| Mean (SD) | 89.4 (23.4) | 86.1 (26.7) | 92.7 (17.6) | 87.3 (28.2) |
| Median (IQR) | 91.6 (75.9 to 105.3) | 88.5 (70.1 to 104.8) | 97.6 (81.2 to 114.1) | 93.2 (75.0 to 110.6) |
| eGFR (creatinine-based 2021 CKD-EPI), mL/min/1.73 m2 | ||||
| Mean (SD) | 93.3 (22.9) | 89.7 (26.4) | 96.5 (17.1) | 90.8 (27.9) |
| Median (IQR) | 96.4 (80.7 to 109.1) | 93.1 (74.4 to 108.6) | 101.8 (85.9 to 116.9) | 97.1 (78.8 to 113.9) |
| Difference in eGFR (2009no race–2009), mL/min/1.73 m2 | ||||
| Mean (SD) | 0.0 (0.0) | −13.7 (4.2) | 0 (0) | −13.9 (4.5) |
| Median (IQR) | 0.0 (0.0-0.0) | −14.1 (−16.7 to −11.1) | 0 (0, 0) | −14.8 (−17.6 to −11.9) |
| Difference in eGFR (2021–2009), mL/min/1.73 m2 | ||||
| Mean (SD) | 3.9 (1.5) | −10.1 (4.9) | 3.8 (1.1) | −10.3 (5.0) |
| Median (IQR) | 4.2 (3.2 to 5.0) | −9.4 (−13.0 to −6.8) | 3.7 (2.6 to 4.6) | −10.9 (−14.6 to −7.8) |
Note: UW entries are mean (SD) or median (IQR), as indicated; NHANES entries are weighted mean (SD) or median (IQR), as indicated.
Abbreviations: CKD-EPI, Chronic Kidney Disease Epidemiology Collaboration; eGFR, estimated glomerular filtration rate; IQR, interquartile range; NHANES, National Health and Nutrition Examination Survey; SD, standard deviation; UW, University of Washington.
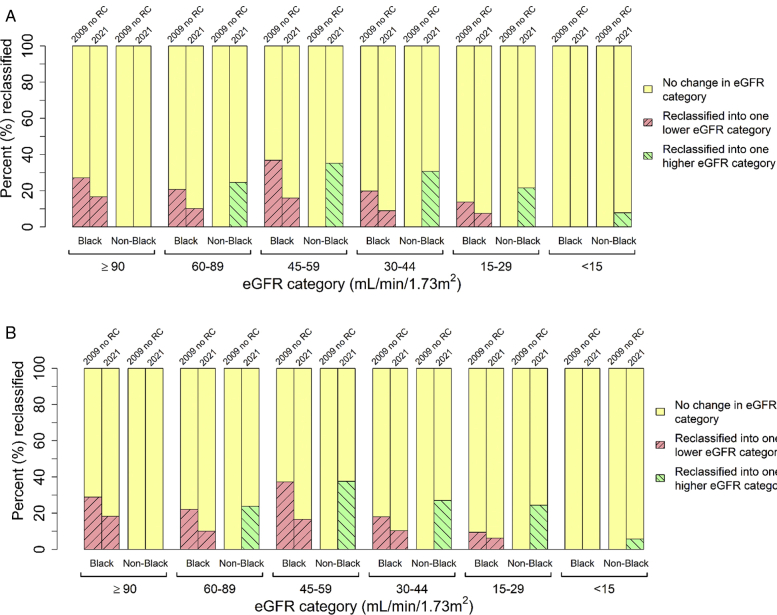
For the UW patients, using the 2009 CKD-EPI no race and 2021 CKD-EPI equations as compared with the 2009 CKD-EPI for eGFR estimation, Black individuals were reclassified into 1 lower eGFR category for every category of eGFR (Fig 1A; Tables S2A and B). In contrast, non-Black individuals moved up in eGFR categories (Fig 1A; Table S2c). Similar reclassification into a lower eGFR category for non-Hispanic Black individuals and a higher eGFR category for non-Black individuals upon using race-free equations was observed for the NHANES cohort (Fig 1B; Tables S3A-C).
Figure 1.
Reclassification of chronic kidney disease eGFR categories using creatinine-based 2009 CKD-EPIno race and 2021 CKD-EPI equations compared to 2009 CKD-EPI equation. (A) Comparison of creatinine-based 2009 CKD-EPI equation to 2009 CKD-EPIno race and 2021 CKD-EPI in the UW cohort. (B) Comparison of creatinine-based 2009 CKD-EPI equation to 2009 CKD-EPIno race and 2021 CKD-EPI in the NHANES cohort. Percentages represent the percentage of individuals who were reclassified into a higher (green) or lower (red) eGFR category as compared to the 2009 CKD-EPI equation. Comparison of non-Black 2009 CKD-EPI to 2009 CKD-EPIno race is redundant but shown here for completeness. Abbreviations: 2009 no RC, 2009 CKD-EPIno race; 2021, 2021 CKD-EPI; eGFR, estimated glomerular filtration rate.
Among a real-world population at the UW as well as a nationally representative population from NHANES, the use of the race-free 2021 CKD-EPI equation led to the reclassification of Black individuals into a lower, and non-Black individuals into a higher, eGFR category across all eGFR categories in both the cohorts. For both the UW and NHANES cohorts, the greatest proportion of Black individuals was reclassified from the eGFR category 45-59 mL/min/1.73 m2 to the eGFR category 30-44 mL/min/1.73 m2 when changing from the 2009 CKD-EPI equation to the 2009 CKD-EPIno race equation. When changing from the 2009 CKD-EPI equation to the 2021 CKD-EPI equation, for both cohorts, the greatest proportion of Black individuals were reclassified from the eGFR category ≥90 mL/min/1.73 m2 to the eGFR category 60-89 mL/min/1.73 m2. For non-Black individuals, in both cohorts, the greatest proportion of reclassification occurred from the eGFR category 45-59 mL/min/1.73 m2 to the eGFR category 60-89 mL/min/1.73 m2 when changing from the 2009 CKD-EPI equation to the 2021 CKD-EPI equation.
Including race in eGFR calculation risks an overestimation of eGFR in a group of individuals who already have a higher burden of kidney disease arising from health inequities and systemic racism. It is possible that the use of the 2021 CKD-EPI equation will increase the prevalence of chronic kidney disease in Black individuals and have a bearing on medication prescription eligibility, contrast administration for imaging and procedures, clinical trials eligibility, nephrology referral, vascular access referral, and transplant donation and recipient eligibility.4, 5, 6, 7, 8, 9, 10
A strength of our study was the inclusion of a large real-world population, thus providing a closer representation of the general adult population. We acknowledge several limitations, including the possibility of misclassification of race, lack of longitudinal follow-up on clinical outcomes related to the new eGFR equation, and inability to evaluate the impact of the combined creatinine-cystatin C 2021 CKD-EPI equation in our population because cystatin C is not routinely measured.
In conclusion, our study demonstrated that in a real-world clinical population and a nationally representative US population, the 2021 CKD-EPI equation led to the greatest reclassification among Black individuals from eGFR ≥90 mL/min/1.73 m2 to 60-89 mL/min/1.73 m2. Further, the differences between the 2009 CKD-EPIno race and the 2021 CKD-EPI equations were modest. As research laboratories adopt these new eGFR equations, more data will be acquired to determine whether these changes mitigate disparities in health care.
Article Information
Authors’ Contributions
Study design: JKG, JS, LRZ, ANH, RM, and NB; data acquisition: JS and ANH; data analysis: LRZ; data interpretation: JKG, LRZ, and NB. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Support
Funding source: Training grant T32DK007467.
Financial Disclosure
Dr Mehrotra reports being a consultant for Light-line Medical and receiving honoraria from Baxter Healthcare. The remaining authors declare that they have no relevant financial interests.
Peer Review
Received January 17, 2022, as a submission to the expedited consideration track with 2 external peer reviews. Direct editorial input from the Statistical Editor and the Editor-in-Chief. Accepted in revised form February 27, 2022.
Footnotes
Figure S1: Patient demographics of the University of Washington cohort.
Item S1: Supplementary Methods.
Table S1A: Baseline characteristics of the University of Washington (UW) cohort.
Table S1B: Baseline characteristics of the National Health and Nutrition Examination Survey (NHANES) cohort.
Table S2A: Reclassification of estimated glomerular filtration rate (eGFR) category among the University of Washington Black patients when changing from 2009 CKD-EPI to 2009 CKD-EPIno race equation.
Table S2B: Reclassification of estimated glomerular filtration rate (eGFR) category among the University of Washington Black patients when changing from 2009 CKD-EPI to 2021 CKD-EPI equation.
Table S2C: Reclassification of estimated glomerular filtration rate (eGFR) category among the University of Washington non-Black patients when changing from 2009 CKD-EPI to 2021 CKD-EPI equation.
Table S3A: Reclassification of estimated glomerular filtration rate (eGFR) category among the National Health and Nutrition Examination Survey (NHANES) non-Hispanic Black participants when changing from 2009 CKD-EPI to 2009 CKD-EPIno race equation.
Table S3A: Reclassification of estimated glomerular filtration rate (eGFR) category among the National Health and Nutrition Examination Survey (NHANES) non-Hispanic Black participants when changing from 2009 CKD-EPI to 2021 CKD-EPI equation.
Table S3C: Reclassification of estimated glomerular filtration rate (eGFR) category among the National Health and Nutrition Examination Survey (NHANES) non-Black participants when changing from 2009 CKD-EPI to 2021 CKD-EPI equation.
Table S4: CKD-EPI equations for estimating glomerular filtration rate (eGFR).
Supplementary Material
Figure S1; Item S1; Tables S1-S4.
References
- 1.Inker L.A., Eneanya N.D., Coresh J., et al. New creatinine- and cystatin C-based equations to estimate GFR without race. N Engl J Med. 2021;385:1737–1749. doi: 10.1056/NEJMoa2102953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Delgado C., Baweja M., Crews D.C., et al. A unifying approach for GFR estimation: recommendations of the NKF-ASN Task Force on reassessing the inclusion of race in diagnosing kidney disease. Am J Kidney Dis. 2022;79:268–288.e1. doi: 10.1053/j.ajkd.2021.08.003. [DOI] [PubMed] [Google Scholar]
- 3.Shi J., Lindo E.G., Baird G.S., et al. Calculating estimated glomerular filtration rate without the race correction factor: observations at a large academic medical system. Clin Chim Acta. 2021;520:16–22. doi: 10.1016/j.cca.2021.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duggal V., Thomas I.C., Montez-Rath M.E., Chertow G.M., Kurella Tamura M. National estimates of CKD prevalence and potential impact of estimating glomerular filtration rate without race. J Am Soc Nephrol. 2021;32:1454–1463. doi: 10.1681/ASN.2020121780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Diao J.A., Wu G.J., Taylor H.A., et al. Clinical implications of removing race from estimates of kidney function. JAMA. 2021;325:184–186. doi: 10.1001/jama.2020.22124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rangaswami J., Lo K.B., Vaduganathan M., Mathew R.O. Eligibility for SGLT2 inhibitors in heart failure without the race coefficient for kidney function estimation. J Am Coll Cardiol. 2021;78:1669–1670. doi: 10.1016/j.jacc.2021.08.025. [DOI] [PubMed] [Google Scholar]
- 7.Walther C.P., Winkelmayer W.C., Navaneethan S.D. Black race coefficient in GFR estimation and diabetes medications in CKD: national estimates. J Am Soc Nephrol. 2021;32:1319–1321. doi: 10.1681/ASN.2020121724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Casal M.A., Ivy S.P., Beumer J.H., Nolin T.D. Effect of removing race from glomerular filtration rate-estimating equations on anticancer drug dosing and eligibility: a retrospective analysis of National Cancer Institute phase 1 clinical trial participants. Lancet Oncol. 2021;22:1333–1340. doi: 10.1016/S1470-2045(21)00377-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zelnick L.R., Leca N., Young B., Bansal N. Association of the estimated glomerular filtration rate with vs without a coefficient for race with time to eligibility for kidney transplant. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2020.34004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vilson F.L., Schmidt B., White L., et al. Removing race from eGFR calculations: implications for urologic care. Urology. 2022;162:42–48. doi: 10.1016/j.urology.2021.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1; Item S1; Tables S1-S4.