Abstract
BACKGROUND:
White spot lesions (WSL) are an unsightly and a rather frequent drawback of orthodontic treatment. The complex design of fixed orthodontic appliances (FAs) makes it difficult to perform proper oral hygiene, which amounts to white spot lesions being three times more prevalent in patients wearing orthodontic appliances. As clear thermoplastic aligners (CAs) are removable appliances, it has been speculated that they allow better oral hygiene maintenance and thus less incidence of WSLs.
OBJECTIVES:
This evidence-based scoping review aims to identify the scope and nature of the evidence on white spot lesions during orthodontic clear aligner therapy.
TYPES OF STUDIES REVIEWED:
Strategic and thorough search of the literature for randomized Controlled Trials, Case-Control, Cohort studies, Case reports, full research articles, and review papers on humans published in English in five major databases was undertaken till July 2021 using free text and Medical Subject Headings (MESH) terms, followed by Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) to identify five studies for data extraction.
RESULTS:
Evidence was summarized for study characteristics, diagnostic methods for the detection of white spot lesions, and incidence of white spot lesions during clear aligner therapy. The literature supports that orthodontic treatment with CAs was associated with a low incidence of WSLs when compared with fixed mechanotherapy, with a major role of patient education, motivation, and compliance in maintaining oral hygiene.
PRACTICAL IMPLICATIONS:
The general perception is that clear aligners are more hygienic and show no incidence of white spot lesions. However, our scoping review supports that WSLs can occur with this form of orthodontic treatment also. WSLs in clear aligners could be attributed to the practice of having composite attachments that cover a significant portion of the tooth surface. Thus, regardless of the type of appliance used, a periodic reinforcement by the orthodontist to maintain oral hygiene is necessary for patient motivation, allowing for better oral hygiene practice, and as a result, leads to prevention of WSLs.
Keywords: Clear aligner, clear aligner therapy, white spot lesion
Introduction
Orthodontic treatment helps to establish a balance between functional harmony, structural balance, and improved esthetics, yet, rendering such treatment comes across with potential risks in terms of both hard and soft tissue damage. Such potential risks may include enamel demineralization, periodontal problems, pulp degeneration, root resorption, lacerations, allergic reactions, and temporomandibular joint disorders, apart from the fact that the treatment procedure may fail in itself. All such potential risks should be considered and addressed while making the final decision to render orthodontic treatment on an individual.[1] White spot lesions around orthodontic attachments are unsightly, and one of the common side effects of orthodontic treatment. They are three times more prevalent in patients wearing orthodontic appliances compared to patients not wearing them.[2] Evidence suggests that patients with WSLs, particularly on the anterior teeth, and their parents, perceive the esthetics to be poorer after treatment and report less satisfaction with their smile.[3]
The complex design of fixed orthodontic appliances (FAs) makes it difficult to perform proper oral hygiene, which causes the accumulation of bacterial biofilms on the dental surface, especially around the brackets. A rapid increase in the volume of dental plaque, higher levels of acidogenic bacteria such as Streptococcus mutans and various Lactobacilli, and a persistent low pH for a longer period leads to the demineralization of dental enamel.[4,5] Consequently, patients with fixed appliances should follow a very rigid oral hygiene protocol to prevent these side effects.
Unlike FAs, removable appliances like clear thermoplastic aligners (CAs) can be taken out and thus enable patients to practice oral hygiene procedures under ideal conditions.[6] They have the potential of not deteriorating oral hygiene as patients do not encounter any of the obstructions caused by brackets, bands, or archwires.
In recent years, Clear Aligner Therapy is contemplated as a more comfortable and esthetic alternative to FAs. This has led to an increased demand for this treatment option among young and adult patients.[7] To evaluate their proficiency, all aspects of clear aligner therapy must be scrutinized including their side effects, such as periodontal health integrity, root resorption, discomfort, and demineralization of dental enamel with the subsequent formation of WSLs.
Although the general conjecture is that clear aligners have a hygienic design, and patients treated with clear aligners are expected to show very few WSL formations,[8] this hypothesis still requires high-quality evidence.Nowadays, evidence-based practice in dentistry has gained popularity due to the publication of a large number of systematic and scoping reviews. Scoping review is a relatively new approach for evidence synthesis that provides an overview of the available research evidence in the field of interest.Information regarding enamel decalcification (WSLs) in patients undergoing Clear Aligner therapy has not been promulgated well and is generally deficient in the literature.[9] To unfold this enigma, the current scoping review was aimed to determine the scope and nature of the evidence on white spot lesions during Clear Aligner Orthodontic therapy.
Methodology of the Review
This scoping review was conducted as per the Arksey and O’ Malley framework.[10] The reporting of results was as per the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement extension for Scoping Reviews to increase its relevance for conducting a systematic review in near future.[11]
Eligibility criteria
PICO (participants, intervention, comparator, and outcome) format for articles’ selection was set as follows:
Population- Patients who underwent orthodontic treatment with clear aligners.
Intervention- Clear Aligner Therapy
Comparison- Comparison of treatment with fixed orthodontic appliance therapy
Outcome- Incidence of white spot lesions in clear aligners.
Review question
The question addressed by this review was “Is there a difference in the incidence of white spot lesions between Clear Aligner and Fixed Orthodontic Therapy?”
Information sources
A thorough strategic analysis of the literature was conducted in five databases PubMed/Medline, Cochrane, Scopus, Wiley Online Library, and Google Scholar.Grey and unpublished literature were searched in ClinicalTrials.gov and www. open grey.eu. Furthermore, the references of the included studies and previous reviews were also thoroughly searched. Searches restricted to trials in human participants with the full text published in English were included.
Search
The PRISMA search strategy was planned to use the MESH terms and Boolean terminology (Orthodontic*) AND (Aligner*) OR “Clear Aligner” OR “Invisalign”/“Invisalign” AND “orthodontic appliances” OR “orthodontic” AND “appliances” OR “orthodontic appliances”. The initial search revealed 22 articles in total: 2 in PubMed, 4 in Cochrane, 1 in Wiley Online Scholar, and 15 in Google Scholar. The preferred reporting system of systematic reviews and meta-analysis [Figure 1]criteria left us with five studies for data extraction.
Figure 1.
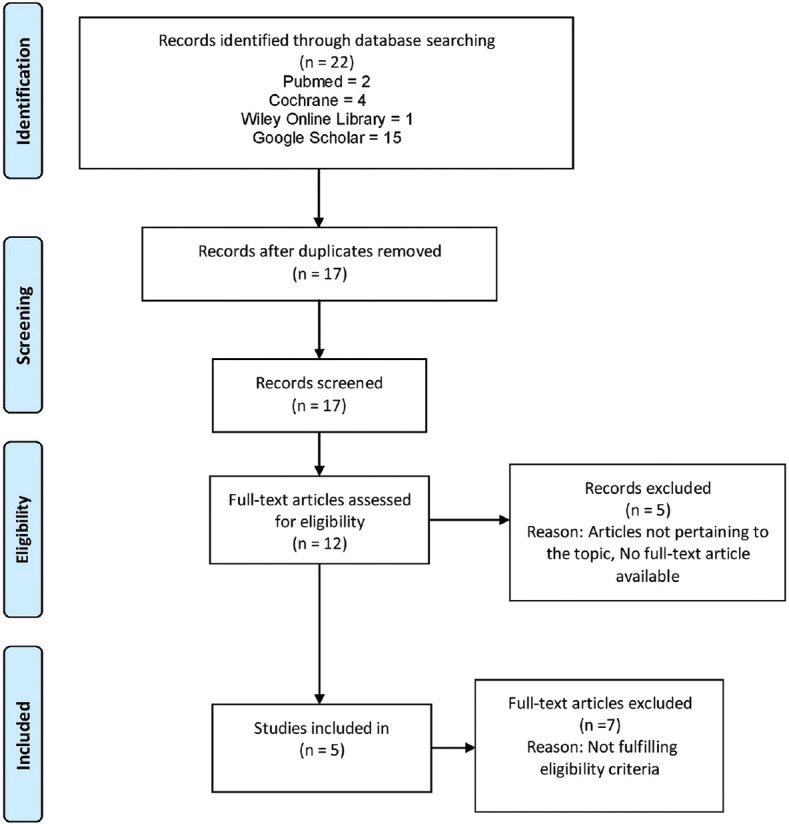
Flow Diagram with a number of records at each stage of scoping review according to PRISMA statement
Selection of sources of evidence
To increase the consistency among the reviewers, all three researchers screened the same 22 studies and performed manual data extraction before beginning screening for this review. Two researchers sequentially evaluated all the identified publications for potentially relevant studies. We resolved the disagreements by consensus, and the third researcher addressed any discordance if needed.The included articles were screened thoroughly, and the level of evidence was ascertained as per Oxford Centre for Evidence-based Medicine (OCEBM).[12]
Data charting process
The data from eligible studies were manually charted in the Microsoft Excel software by two researchers independently. Relevant information on key study characteristics and detailed findings of the included articles were extracted. The third researcher verified the data for accuracy. Any disagreements were resolved through discussion between the two researchers or further adjudication by the third researcher.
Data items
Data characteristics (type of study, participants/studies included, control and experimental groups, duration of the study, and quality of evidence as per OCEMB) of selected articles and their findings (diagnostic method of white spot lesion, study selection criteria, outcomes, significant correlations, key interpretations, and limitations.) were summarized in Tables 1 and 2.
Table 1.
Characteristics of included articles
| Author | Type of study | Participants/studies included | Control and experimental group | Duration | Level of evidence* |
|---|---|---|---|---|---|
| Azeem M and Hamid W (2017)[9] | Prospective Study | a. 25 participants b. 13 females, 12 males were recruited c. Mean age±standard deviation16.17±1.76 years |
Experimental Group- CA | 18.11±5.12 months | 3 |
| Alshatti et al. (2017)[13] | Randomized Clinical Trial Block randomization generated by computer software “RandomAllocation Software” Single blinding |
a. 60 participants b. There were more males than females in the three groups. Data not specified c. Mean age±standard deviation Group 1=(21.44±11.62 years) Group 2=(14.82±4.26 years) Group 3=(14.47±3.99 years) |
a. Control Group- None b. Experimental Group- Group 1- CA Group 2- SLB Group 3- FA |
18 months T0=at the beginning of treatment T1=18 months |
2 |
| Buschang et al. (2019)[14] | Retrospective Cohort Study | a. 450 participants, Group 1=244, Group 2=206 b. No data on the sex ratio. c. Mean age±standard deviation Group 1=30.4±14 years Group 2=29.2±11.5 years |
a. Control Group- None b. Experimental Group- Group 1- CA (244) Group 2- FA (206) |
Not mentioned | 3 |
| Karad et al.(2019)[15] | Narrative Review Article | Research articles, systematic reviews, and meta-analyses were used for the preparation of this narrative review corresponding to human subjects | Not applicable | Studies till September 2018 were included | 5 |
| Albhaisi et al (2020)[16] | Randomized clinical trial. Simple randomization (COIN TOSS) Blinding was done only in data assessment |
a. 49 participants were included (42 completed the study) b. 39 females, 10 males were recruited Only 23 subjects (6 male and 17 female) in group 1 and 19 subjects (3 male and 16 female) in group 2 c. Mean age±standard deviation - 21.25±3 years |
a. Control Group- None b. Experimental Group- Group 1- CA (23) Group 2- FA (19) |
3 months T0=before treatment T1=after 3 months |
2 |
Table 2.
Findings of included articles
| Author | Diagnostic method of white spot lesion/study selection criteria | Outcomes | Significant correlations | Interpretation | Limitations | Key findings related to the research question |
|---|---|---|---|---|---|---|
| 1. Azeem M and Hamid W (2017)[9] | Quantitative light-induced fluorescence was taken before and directly after clear aligner treatment | 1. PRIMARY OUTCOME To assess the incidence of WSL formation in the subjects treated with clear aligner therapy | 1. The overall incidence of new WSLs was 2.85% for all the assessed teeth | A total of 1.28% of the patients were affected by at least one new WSL | limited sample size, lack of blinding, lack of control group, and lack of comparison with fixed appliances. | Orthodontic treatment with clear aligner therapy showed a low incidence of newly developed WSLs |
| 2. Alshatti et al.(2017)[13] | Visual evaluation of pre and post-treatment digital photographs, measurement of lesion done only on the maxillary lateral incisor | 1. PRIMARY OUTCOME To measure and compare the incidence of WSLs in the three different groups using a modified version of the “Gorelick White Spot Lesion Index” 2. SECONDARY OUTCOMES a. To measure and compare the severity of WSLs using ImageJ software b. To evaluate correlation between Gingival, Plaque, and Bleeding Indices and WSLs. |
1. For Group 1, 2 and 3, 29%, 44%, 47.4% of the patients developed WSL at T2, respectively. For Group 1, 2, 3, the percentage of patients who change from lesion-free at T0 to having lesion (s) at T2 were 41.18%, 63.64%, and 52.94%, respectively. 2. Surface Area (SA) change from T0 to T2 in Group 1, 2 and 3 was of 0.066±0.092, 0.110±0.095, and 0.093±0.112 respectively with P<0.05. The P value was 0.2763 (> 0.05) for differences in surface area (size) of WSLs among the groups. 3. Lesion size change and the changes in gingival architecture, appearance of plaque, and bleeding pattern were 0.087, 0.167 and 0.0032 with Pvalue of 0.51, 0.21 and 0.98, respectively (all P>0.05). |
1. No significant difference in the incidence of WSL between the types of appliances. 2. WSL size the change were all significant within each group but not significant among the groups. 3. Despite the increase in the gingival index, plaque index, and bleeding on probing index status, there was no correlation between them and the change in the dimension of WSLs. |
Lack of a standardized protocol of image taking technique. | There was no difference in the incidence and the severity of white spot lesions among clear aligners, self-ligating brackets, and conventional brackets. |
| 3. Buschang et al. (2019)[14] | Visual evaluation of pre- and post- treatment photographs by two investigators | 1. PRIMARY OUTCOME To Evaluate the incidence of WSLs among CA and FA groups. 2. SECONDARY OUTCOMES |
1. 1.2% CA and 25.7% FA developed WSLs (P<0.001) 2. Total number of WSLs that developed=3 in CA and 174 in FA (P<0.001) |
1. Patients treated with aligners showed less incidence and risk of developing WSLs than patients treated with traditional braces. 2. Patients with poor pre-treatment OH developed more WSLs than were those with good OH. |
1. Less sensitivity of diagnosing WSLs. 2. Patient withdrawl- 85% of the aligner cases and 48% of the fixed cases |
Patients treated with aligners showed less incidence and risk of developing WSLs than patients treated with traditional braces. |
| a. To Evaluate Risk factors for the development of WSLs. b. To Evaluate the Incidence of WSLs between both arches and all teeth. |
3. Fair (3.4 times) or poor (6.5 times) pre-treatment OH, worsening of OH during treatment (1.6 times more), pre-existing WSLs [8.5 times more likely (P<0.001)], and longer treatment duration (1.6 times more for>2 years) significantly (P<0.05) increased the risk of developing WSLs in FA group. 4. The incidence of WSLs for the maxillary canines, lateral incisors, central incisors, was 7.3%, 6%, 2.9%, respectively. The incidence of WSLs for mandibular canines, laterals incisors, and central incisors, was 7.1%, 2.6%, 2.2% respectively |
3. The low incidence of WSLs in patients with removable aligners can be attributed to the shorter treatment durations and better hygiene. 4. Greater incidence of WSLs for the maxillary than for the mandibular teeth, and it was greater for the canines than for the incisors. |
3. The pre-treatment differences in OH could have been counteracted by the pre-treatment differences in fluorosis. 4. Group differences in pre-treatment complexity and treatment results were not controlled |
|||
| 4. Karad et al. (2019)[15] | Not applicable | Not applicable | Not applicable | 1. Expert opinion- If oral hygiene is adequately maintained, which is possible in the case of aligners, WSL formation can be reduced. 2. Expert opinion- CaSP has been found to be an effective remineralizing agent compared with other agents in a majority of studies; however, these studies were conducted in vitro. |
1. Narrative review with no level of evidence given for the included studies | Orthodontic treatment with CA was associated with a low incidence of newly developed WSLs with a major role in patient education, motivation, and compliance in maintaining oral hygiene. |
| 5. Albhaisi et al (2020)[16] | Quantitative light-induced fluorescence- QLF images were judged visually for signs of decalcificatio. The QLF images were analyzed using customized software (QA2 version 1.18) | 1. PRIMARY OUTCOME To evaluate the mean amount of fluorescence loss (⧍F%) reflecting the mineral loss in percent. |
1. Significant difference between the mean amount of fluorescence loss of 0.4% for the CA group (P=0.283) and 1.2% for the FA group (P=0.013). 2. Significant difference in the number of newly developed lesions between the two groups (P=0.039), the incidence in FA group=8.25 and in CA group=6.21 |
1. Increase in tooth demineralization was seen in both groups, but significantly more in the FA group. 2. More incidence of WSLs was seen in patients with FA than CA. |
1. No long-term evaluation of enamel demineralization due to the short duration of study. 2. No sex-based comparison as most participants were female. |
More incidence of WSLs was seen in FA (8.25) when compared with CA (6.21) |
| 2. SECONDARY OUTCOMES a. To Evaluate the Number of newly developed lesions b. the deepest point in the lesion (⧍Max), c. Lesion area (pixels) d. plaque surface area (⧍R30) |
3. The lesion area was significantly higher (P<0.001) in the CA group at T1. 4. FA group exhibited significantly more plaque at T1 than T0 (P<0.001) and more than the CA group at T1 (P<0.001). |
3. Larger lesion areas with less mineral loss were found in the CA group than in the FA group. 4. More plaque deposition in the FA group at T1 than T0. |
Results
Evidence in this research area was overviewed and mapped and found that adequate number and quality of evidence that would be valuable to knowledge users were unavailable. Hence, this evidence synthesis provides a range of resources for conducting a Systematic Review in near future.
This scoping review has broadly evaluated the incidence of WSLs duringclear aligner therapy. The results were used to establish whether there was a decrease in the incidence of WSLs with the use of removable CA therapy when compared to fixed mechanotherapy.
Study characteristics
A total of five articles were finally selected and thoroughly studied. Two out of five studies evaluating WSLs included in the present review were randomized controlled trials out of which one was published in a scientific journal,[16] and another one was a thesis.[13] The remaining three studies included one prospective study,[9] one retrospective cohort study,[14] and one review article.[15] The two randomized controlled trials were conducted on 109 participants. The retrospective cohort study and prospective study had 450 and 25 participants, respectively. Table 1 outlines the outcome parameters and the diagnostic methods used to measure the outcomes (WSL). Two of the studies[13,14] used Visual evaluation of pre-and post-treatment photographs, whereas two studies[9,16] used quantitative light-induced fluorescence (QLF) as the diagnostic method for the detection of WSLs. Table 2 outlines the measured outcomes and significant correlations for the incidence of WSLs.
Discussion
The current clinical evidence is still insufficient to prove a substantive clinical result. Amongst the five included studies, three[14,15,16] reported a higher incidence of WSLs in FA therapy when compared with CA, whereas Alshatti et al.[13] reported no difference in the incidence and the severity of WSLs among clear aligners, self ligating brackets (SLBs), and conventional brackets. This might be attributed to the different diagnostic methods used in the studies for the detection and quantification of WSLs. Whereas Albhaisi et al.[16] and Azeem and Hamid[9] used QLF, Buschang et al.[14] and Alshatti et al.[13] used the Visual evaluation of pre-and post-treatment digital photographs as the diagnostic method.
Azeem and Hamid.[9] reported an overall incidence of WSLs at 2.85%. When all the accessed teeth were considered, 28% of the patients presented with at least one new WSL. For tooth groups, 16 to 46, the patient-related incidence was 28%. When the maxillary incisors were considered separately, the incidence was found to be 8%.On the other hand, the incidence of white spot lesions was very high with fixed orthodontic treatment. According to Enaia et al.,[17] the incidence of WSLs in fixed orthodontic therapy was found to be 60.9%. Similarly, Gorelick et al.,[18] Akin et al.,[19] and Tufekci et al.[5] found the incidence to be 50%, 55%, and 46%, respectively. Therefore, the current study states that aligner therapy makes a difference when WSL incidence is concerned.
The three important parameters that should be observed while evaluating white spot lesions are incidence (the number of newly formed lesions), size or surface area of the lesions, and depth of the lesions. The first RCT to compare the incidence of WSL among aligners and traditional braces was done by Alshatti et al.[13] including 60 participants. They reported no significant difference in the incidence of WSL between the types of appliances.They found that for Group 1 (CA), 2 (SLB), and 3 (FA) the percentage of patients who change from lesion-free at the beginning of the treatment (T0) to having lesion(s) after 18 months of treatment (T1) were 41.18%, 63.64%, and 52.94%, respectively, with P = 0.56, rendering the finding statistically insignificant. Also, when they considered the entire sample size, the incidence of WSL, regardless of the appliance type, was about 39%. Moreover, the difference in the WSL Surface Area (SA) was calculated by subtracting the Surface Area at T0 from the size at T2 (i.e., SA Difference = SizeT2-SizeT0). The change in the SA was found to be statistically insignificant between the three groups.
Contrary to the above findings, Buschang et al.[14] reported a significantly less incidence of WSL in CA (1.2%) compared with FA (25.7%). Azeem et al.[9] also reported a lower incidence of 2.85% in CA patients. They had used QLF as a diagnostic tool for a younger and smaller sample. The findings also align with the results of Albhaisi et al.[16] who reported an increased incidence of WSLs in the FA group (8.25) compared with the CA group (6.21).
According to Buschang et al.[14] the low incidence of WSLs in patients using removable aligners can be accredited to the shorter treatment durations and better hygiene. As aligners can be removed, lower plaque levels and an improved oral hygiene (OH) were reported in the CA group. This study also reported good maintenance or even an improvement in OH during treatment in 94.3% of CA patients, compared to 84.8% of FA patients. Aligners made it possible for the patients to remove plaque more efficiently and comply with OH instructions.
In contrast to the decreased incidence of WSL in the CA group, Albhaisi et al.[16] reported a significantly larger lesion area in the CA group at T1 (3 months after treatment) than T0 (beginning of treatment) and the FA group. This significant increase in the SA of WSLs during the CA therapy could be attributed to the fact that CA limits the flow of saliva, negating saliva's natural buffering, cleansing, and remineralizing properties. The norm of WSLs as exhibited in the CA group, of having a large coverage area could be attributed to the practice of having attachments that cover a significant portion of the tooth surface.This brings a whole new set of ideas and rules while taking care of their bonding and the kind of patient instructions that are to be given for their proper care and hygiene. Further investigations on the mensuration of these attachments will only able us to understand the functioning and precise nature of these attachments, which if not taken care of shall lead to food entrapment, seen distinctively while comparing angular sharp-edged attachments to smooth circular ones
Although the surface area (SA) of WSLs was found to be more in the CA group, a greater amount of demineralization i.e., depth of the lesion was detected in the FA group with a significantly more mineral loss of 1.2% than 0.4% in the CA group. This finding was consistent with the markedly increased amount of plaque that was present in the FA group and agrees with almost all the studies that illustrated their association.[20] This was because fixed appliances had rough surfaces proven to be the perfect sites for plaque accumulation.
There were differences in WSL formation within and between jaws. Buschang et al.[14] exhibited that WSLs were more likely to develop on maxillary than on mandibular teeth.The canines and maxillary lateral incisors seem to be the teeth most susceptible to WSLs.
This scoping review also included a narrative review where Karad et al.[15] stated that patient education, motivation, and compliance in maintaining oral hygiene plays a major role in the low incidence of WSLs with CA therapy. In this review, experts unanimously agreed that if oral hygiene was adequately maintained, possible in the case of aligners, WSL formation can be reduced notably.
Overall, the present scoping review suggested that patients treated with aligners showed less incidence and risk of developing WSLs and also emphasized the falsehood of the claims that CA therapy is completely safe and does not have any implications on oral health. It is an undeniable fact that patient education and motivation on oral hygiene practice are essential components for the prevention of WSLs.
Limitations of the study
There is a need for more robust studies to validate the results of the incidence of WSLs during orthodontic treatment. Studies tracking long-term effects on the development of WSLs in clear aligner therapy, patient satisfaction, and economic effectiveness are necessary. Thus, interpretation of clinical practice should be made with caution.
Conclusions
The following inferences can be drawn from this scoping review
Increased incidence of WSLs is seen in both Clear aligners and Fixed mechanotherapy.
The majority of the studies included in this review have positively correlated a potential decrease in WSLs with the use of clear aligners when compared with Fixed mechanotherapy.
Clear aligner therapy could be preferred in orthodontic patients at high risk of developing WSLs.
Recommendations
Based upon the limited available scientific data, the results should be evaluated with caution, and more clinical trials in this area are welcome to have a better conclusion in terms of which appliance therapy would provide optimal dental health during and after orthodontic therapy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Reddy V, Vasudevan V, Sankar G, Arun AV, Mahendra S, Khalid MK. Orthodontic scars. J Indian Aca Oral Med Radiol. 2012;24:217–22. [Google Scholar]
- 2.Khera A, Bisht S, Raghav P. White spot lesions: An iatrogenic effect of fixed orthodontic therapy. Int J Dent Oral Care. 2021;1:14. [Google Scholar]
- 3.Maxfield BJ, Hamdan AM, Tüfekçi E, Shroff B, Best AM, Lindauer SJ. Development of white spot lesions during orthodontic treatment: Perceptions of patients, parents, orthodontists, and general dentists. Am J Orthod Dentofacial Orthop. 2012;141:337–44. doi: 10.1016/j.ajodo.2011.08.024. [DOI] [PubMed] [Google Scholar]
- 4.Julien KC, Buschang PH, Campbell PM. Prevalence of white spot lesion formation during orthodontic treatment. Angle Orthod. 2013;83:641–7. doi: 10.2319/071712-584.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tufekci E, Dixon JS, Gunsolley JC, Lindauer SJ. Prevalence of white spot lesions during orthodontic treatment with fixed appliances. Angle Orthod. 2011;81:206–10. doi: 10.2319/051710-262.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taylor MG, McGorray SP, Durrett S, Pavlow S, Downey N, Lenk M, et al. Effect of invisalignaligners on periodontal tissues. J Dent Res. 2003;82:1483–9. [Google Scholar]
- 7.Rossini G, Parrini S, Castroflorio T, Deregibus A, Debernardi CL. Efficacy of clear aligners in controlling orthodontic tooth movement: A systematic review. Angle Orthod. 2015;85:881–9. doi: 10.2319/061614-436.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moshiri M, Eckhart JE, McShane P, German DS. Consequences of poor oral hygiene during aligner therapy. J Clin Orthod. 2013;47:494–8. [PubMed] [Google Scholar]
- 9.Azeem M, Hamid WU. Incidence of white spot lesions during orthodontic clear aligner therapy. J World Fed Orthod. 2017;6:127–30. [Google Scholar]
- 10.Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. [Google Scholar]
- 11.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist andexplanation. Ann Intern Med. 2018;169:467–73. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 12.Incidence of white spot lesions during orthodontic clear aligner therapy. J World Fed Orthod. 2017;6:127–30. [Google Scholar]
- 13.Alshatti H. Doctoral dissertation. Connecticut: University of Connecticut; 2017. Comparison of White Spot Lesions among Clear Aligners, Self-Ligating Brackets and Conventional Brackets-A Randomized Controlled Clinical Trial. [Google Scholar]
- 14.Buschang PH, Chastain D, Keylor CL, Crosby D, Julien KC. Incidence of white spot lesions among patients treated with clear aligners and traditional braces. Angle Orthod. 2019;89:359–64. doi: 10.2319/073118-553.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karad A, Dhole P, Juvvadi SR, Joshi S, Gupta A. White spot lesions in orthodontic patients: An expert opinion. J Int Oral Health. 2019;11:172–7. [Google Scholar]
- 16.Albhaisi Z, Al-Khateeb SN, Alhaija ES. Enamel demineralization during clear aligner orthodontic treatment compared with fixed appliance therapy, evaluated with quantitative light-induced fluorescence: A randomized clinical trial. Am J Orthod Dentofacial Orthop. 2020;157:594–601. doi: 10.1016/j.ajodo.2020.01.004. [DOI] [PubMed] [Google Scholar]
- 17.Enaia M, Bock N, Ruf S. White-spot lesions during multibracket appliance treatment: Achallenge for clinical excellence. Am J Orthod Dentofacial Orthop. 2011;140:e17–24. doi: 10.1016/j.ajodo.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 18.Gorelick L, Geiger AM, Gwinnett AJ. Incidence of white spot formation after bonding and banding. Am J Orthod. 1982;81:93–8. doi: 10.1016/0002-9416(82)90032-x. [DOI] [PubMed] [Google Scholar]
- 19.Akin M, Tazcan M, Ileri Z, Ayhan F. Incidence of white spot lesion during fixed orthodontic treatment. Turkish J Orthod. 2013;26:98–102. [Google Scholar]
- 20.Chhibber A, Agarwal S, Yadav S, Kuo CL, Upadhyay M. Which orthodontic appliance is best for oral hygiene.A randomized clinical trial? Am J Orthod Dentofacial Orthop. 2018;153:175–83. doi: 10.1016/j.ajodo.2017.10.009. [DOI] [PubMed] [Google Scholar]


