Abstract
Introduction:
There has been rising concern about e-cigarette usage among teenagers and young adults. As knowledge about the adverse health effects of e-cigarettes accumulates, it is critical to identify factors that may increase risk of vaping initiation and frequency of use. One potential risk factor known to increase risk for other substance use is impulsivity. This study tested the hypothesis that impulsivity prospectively predicts vaping over time.
Methods:
Active e-cigarette users (n=137; 51.8% male; Mean age 20 years at baseline) completed 8 waves of assessment over 21 months (2017–2020). The S-UPPS-P impulse behavior scale was used at baseline to measure impulsivity, and frequency of e-cigarette, cigarette, marijuana and alcohol use was calculated at each wave thereafter.
Results:
Vaping frequency declined over time [Incidence Rate Ratio (IRR) = 0.92]. There were significant, stable, positive associations between e-cigarette use and lack of premeditation (IRR=1.06) and sensation seeking (IRR=1.09). Vaping frequency was inversely associated with negative urgency (IRR=0.95). Positive urgency and lack of perseverance were not associated with frequency of vaping.
Conclusion:
These findings suggest that young adults who have higher impulsivity of certain types may use e-cigarettes more frequently. Thus, vaping interventions for young adults should address these factors to ensure the greatest impact on public health.
Keywords: E-cigarette, Impulsivity, Nicotine, UPPS-P model, Vaping
Introduction
Use of electronic cigarettes (e-cigarettes) has exploded over the past decade in the U.S. young adult population (Dai & Leventhal, 2019). Monitoring the Future data suggest prevalence of past 30-day use increased from 6% of 19–30 year-olds in 2017 to 14% of the same group in 2019 and 2020 (Schulenberg et al., 2021). E-cigarettes are viewed and marketed as a safer, more socially acceptable alternative to combustible cigarettes (Collins et al., 2019). However, evidence of e-cigarette aerosols causing cardiopulmonary disease and increasing health risks has been growing (Masso-Silva et al., 2021; Sharma et al., 2021; Ween et al., 2021; Bozier et al., 2020; Tsai et al., 2020). While key chemicals within e-cigarette solutions (propylene glycol and glycerol) are approved for consumption in food products, little information exists regarding the effects of inhaling these substances chronically. Atomizers from e-cigarettes can release traces of metals such as lead, cadmium, nickel, chromium, or tin into these aerosols (Mikheev et al., 2016). These metals can cause oxidative stress and damage different organs and organ systems (Tegin et al., 2018). Another concern regarding e-cigarette use in youth and young adults is the possibility that it could increase the likelihood of conventional cigarette smoking. E-cigarette use has been be associated with future cigarette use among adolescent never-smokers (Bold et al., 2018; Leventhal et al., 2015), and escalating cigarette use among young adult light smokers (Doran et al., 2017).
Given the risks of e-cigarette use, it is essential to identify factors that may contribute to initiation of vaping. One potential risk factor is impulsivity (Bold et al., 2017; Reff & Baschnagel, 2021), which refers to a tendency toward premature or reckless action. The UPPS-P model conceptualizes impulsivity as comprised of five distinct but related characteristics, each reflecting a tendency toward rash action under specific circumstances. Positive and negative urgency are defined by proneness to impulsive action in response to strong positive and negative moods, respectively; sensation seeking is defined by pursuit of novel, exciting experiences; lack of premeditation is a tendency to act without considering the consequences; and lack of perseverance is difficulty remaining focused on a task (Cyders & Smith, 2007; Lynam et al., 2006).
Impulsivity is increasingly recognized as a multifaceted construct implicated in substance use, especially in adolescents and young adults (Kaiser et al., 2016; Birkley & Smith, 2011; VanderVeen et al., 2016), and has been associated with cigarette smoking and nicotine dependence (Doran et al., 2009; Mitchell 1999; Kale et al., 2018). In terms of the UPPS-P model, positive and negative urgency have been associated with higher nicotine dependence in adult smokers (Pang et al., 2014), and negative urgency appears to be a strong predictor of daily vs. non-daily cigarette smoking in young adults (Lee et al., 2015). Some work has also indicated a link between impulsivity and e-cigarette consumption. In cross-sectional studies, impulsivity has been associated with younger age of e-cigarette initiation and increased e-cigarette susceptibility and use (Bold et al., 2017; Conner et al., 2019; Grant et al., 2019, Reff & Baschnagel, 2021). Preliminary studies suggest young adult e-cigarette users tend to score higher on positive and negative urgency, sensation seeking, and lack of premeditation (Doran & Tully, 2018; Lanza et al., 2020).
Given the prevalence of e-cigarette use, better understanding of the role of predictors such as impulsivity in patterns of vaping is needed to better inform interventions. The goal of the present study was to evaluate impulsivity as a prospective predictor of e-cigarette use in young adult users over time. We predicted that participants with higher baseline positive urgency, negative urgency, sensation seeking, and lack of premeditation would higher levels of e-cigarette use over time.
Methods
Participants
Young adult e-cigarette users (n = 137; Mean age at baseline = 20.0, SD = 1.6, 51.8% male) were recruited for this cohort study. In terms of racial/ethnic background, 73% identified as White, 5.1% as Black, 5.8% as Asian American, 9.5% as Latinx, and 6.6% as having multiple racial or ethnic backgrounds. Inclusion criteria included use of e-cigarettes at least monthly for the past 6 months or longer, and aged 18–24 years at enrollment. Individuals who reported current or past use of conventional cigarettes or other combustible tobacco products at least monthly for any 6-month period in their lifetime were excluded.
Procedure
Participants were recruited from across the US using boosted Facebook posts, and paid $20–40 per wave to complete 8 waves of online assessment administered at 3-month intervals. All subjects underwent informed consent. Each wave consisted of a single assessment. Items utilized in the present study were identical across waves, and the number of items in the full assessment was consistent across waves. Data were collected from July 2017-March 2020. This study was approved by the University of California San Diego Institutional Review Board in accordance with the provisions of the Declaration of Helsinki.
Measures
Demographic characteristics were assessed at baseline, including age, gender, race/ethnicity, student status, work status, education, age at e-cigarette initiation, number of e-cigarette users in the household, and whether the participants’ significant others used e-cigarettes. We estimated years of e-cigarette use at baseline by subtracting age of e-cigarette initiation from age at baseline. Substance use was measured at each wave using an adaptation of the Timeline Followback (Sobell & Sobell, 1992), which has good reliability and validity in online use (Pedersen et al., 2012). At each wave, this approach was used to evaluate whether or not participants had used e-cigarettes, cigarettes, alcohol and marijuana on each of the previous 14 days. The instruction set defined e-cigarettes as products that included only nicotine, and marijuana as including vape products containing THC. These responses were consolidated into count variables reflecting the number of days in the past 2 weeks with any use of each product (i.e., e-cigarette frequency, cigarette frequency, alcohol frequency and marijuana frequency).
Impulsivity was measured at baseline using the S-UPPS-P (Cyders et al., 2014), a 20-item measure that includes 4 items evaluating each of the 5 impulsivity components: lack of perseverance, lack of premeditation, sensation seeking, positive urgency and negative urgency. This short form is psychometrically comparable to the original UPPS scale (Whiteside & Lynam, 2001). Each subscale was coded so that higher values reflected greater impulsivity. Internal consistency for the subscales in this sample ranged from 0.72–0.81.
Analytic Plan
Bivariate analyses evaluated relationships between demographics, other substance use, impulsivity, and outcome variables to identify covariates to be included in hypothesis tests. Years of e-cigarette use was included as a covariate to account for the possibility that more prolonged users would be more likely to be nicotine dependent and thus vape more frequently. Hypotheses were tested using a longitudinal negative binomial regression model after comparisons indicated this distribution fit the data better than alternatives. The model was implemented using the xtnbreg module in Intercooled Stata 15.01 (StataCorp LP, College Station, TX). E-cigarette days in the past 2 weeks at each wave was the time-varying outcome. The model included time and time2 as well as all 5 impulsivity subscale scores as predictors. The initial model also included terms for all possible time*impulsivity and time2*impulsivity interactions, to evaluate whether associations between impulsivity and e-cigarette frequency changed over time. Non-significant interaction terms were removed and the model re-fit. For all analyses, alpha was set to 0.05. Missing data were not imputed; models used all available data from all enrolled participants to calculate parameter estimates.
Results
Demographics and Baseline Data
Baseline demographic and clinical characteristics are shown in Table 1. At baseline, participants reported vaping on an average of 6.96 (SD=4.53) of the past 14 days, compared to 2.74 days (SD=4.58) for marijuana and 0.17 days (SD=0.95) for cigarettes. Bivariate analyses showed that, across all study waves, e-cigarette frequency was positively associated with marijuana (p<0.001) and cigarette frequency (p=0.013), but not alcohol frequency. E-cigarette frequency was higher among male participants (p<0.001) and those who reported having a significant other who vaped (p=0.007). E-cigarette frequency was unrelated to alcohol frequency, race/ethnicity, presence of other e-cigarette users in the household, highest level of education, and student and employment statuses. Consequently, marijuana frequency, cigarette frequency, gender and significant other e-cigarette status were included as covariates in hypothesis tests. Most participants had never used cigarettes at baseline, and of those who had tried cigarettes, the majority had only done so after initial e-cigarette use. In terms of missing data, all participants provided complete data at baseline. At the 7 subsequent waves, data were available for 80–92% of participants. Proportion of missing data was not significantly associated with demographic, impulsivity, or substance use variables.
Table 1.
Baseline demographic and clinical characteristics
| Mean (SD), R or % | |
|---|---|
|
| |
| Age (years) | 20.0 (1.6) |
| Age at first e-cigarette use (years) | 17.4 (1.6) |
| Years of e-cigarette use | 2.6 (1.5), 0.8–9.1 |
| Race/Ethnicity | |
| White | 73.0% |
| Latinx | 9.5% |
| Multiple | 6.6% |
| Asian American | 5.8% |
| Black | 5.1% |
| Gender | |
| Male | 51.8% |
| Female | 46% |
| Student status | |
| Full-time student | 55.5% |
| Part-time student | 14.6% |
| Employment | |
| Full-time position | 16.1% |
| Part-time position | 41.6% |
| Significant other e-cigarette use | |
| Non-user | 32.1% |
| User | 24.8% |
| Currently single | 43.1% |
| Order of nicotine product initial use | |
| Cigarettes before e-cigs | 20.4% |
| E-cigs before cigarettes | 24.8% |
| Never tried cigarettes | 54.7% |
| Impulsivity Subscale Scores | |
| Negative urgency | 9.74 (3.10) |
| Positive urgency | 8.65 (3.28) |
| Lack of perseverance | 8.04 (2.93) |
| Lack of premeditation | 8.03 (3.02) |
| Sensation seeking | 11.32 (3.00) |
Predictors of E-Cigarette Frequency
The final model is shown in Table 2. None of the impulsivity*time terms were significant, indicating that associations between baseline impulsivity scores and e-cigarette use were stable over the 8 waves of the study. E-cigarette frequency was significantly associated with lack of premeditation, such that each 1-point increase in lack of premeditation predicted 6% more e-cigarette days. A 1-standard deviation increase in lack of premeditation was associated with 19% more e-cigarette days. Similarly, e-cigarette frequency was positively associated with sensation seeking, with each 1-point and 1-standard deviation increase in sensation seeking predicting 9% and 25% more e-cigarette days, respectively. Lack of perseverance, positive urgency, and negative urgency were not significant predictors of e-cigarette use.
Table 2.
Longitudinal regression model of e-cigarette frequency over time
| Predictor | Coefficient | Std. Err. | IRR | 95% CI |
|---|---|---|---|---|
|
| ||||
| Intercept | 0.99 | 0.13 | 2.70 | 2.08, 3.50 |
| Time | −0.09 | 0.01 | 0.92 | 0.90, 0.94 |
| Years of e-cigarette use | 0.04 | 1.04 | 0.97, 1.11 | |
| Marijuana frequency | 0.03 | 0.01 | 1.03 | 1.01, 1.04 |
| Cigarette frequency | 0.02 | 0.02 | 1.02 | 0.98, 1.05 |
| Significant other e-cigarette use | ||||
| E-cigarette user | 0.35 | 0.21 | 1.43 | 1.06, 1.92 |
| Currently single | −0.15 | 0.11 | 0.86 | 0.67, 1.11 |
| Gender identity | ||||
| Female | −0.27 | 0.08 | 0.76 | 0.61, 0.94 |
| Impulsivity Traits | ||||
| Lack of premeditation | 0.06 | 0.02 | 1.06 | 1.01, 1.11 |
| Lack of perseverance | −0.03 | 0.02 | 0.96 | 0.93, 1.01 |
| Sensation seeking | 0.08 | 0.02 | 1.09 | 1.04, 1.14 |
| Positive urgency | 0.02 | 0.02 | 1.01 | 0.97, 1.06 |
| Negative urgency | −0.04 | 0.02 | 0.96 | 0.93, 1.00 |
Std. Err. = Standard Error; IRR = incidence rate ratio; CI = confidence interval. For significant others’ e-cigarette use, “non-user” was the reference category. For gender, “male” was the reference category. Impulsivity scores were mean-centered at 0 and coded so that higher scores reflected greater levels of impulsivity.
E-cigarette use was also inversely associated with time, with each additional wave predicting a 9% decline in frequency. Figure 1 shows the average number of e-cigarette days at each wave, which declined from a high of 7.1 of the past 14 days 3 months after baseline, to a low of 5.1 of the past 14 days at the final wave. For illustrative purposes, figure 1 also shows the proportion of the sample with the reported current use (i.e., any nicotine vaping in the past 14 days) at each wave. Similarly, this declined from 92.0% at baseline to 62.0% at 21 months. E-cigarette frequency was associated with marijuana use, with each additional day of marijuana use predicting a 3% increase in e-cigarette days, but was not associated with combustible cigarette use. Having a significant other who used e-cigarettes was associated with 44% more e-cigarette days compared to a significant other who did not use e-cigarettes. E-cigarette frequency did not differ between those whose significant others were non-users and those who were single, and was unrelated to years of e-cigarette use. Finally, identifying as female predicted 23% fewer e-cigarette days.
Figure 1. Frequency of e-cigarette use over time.
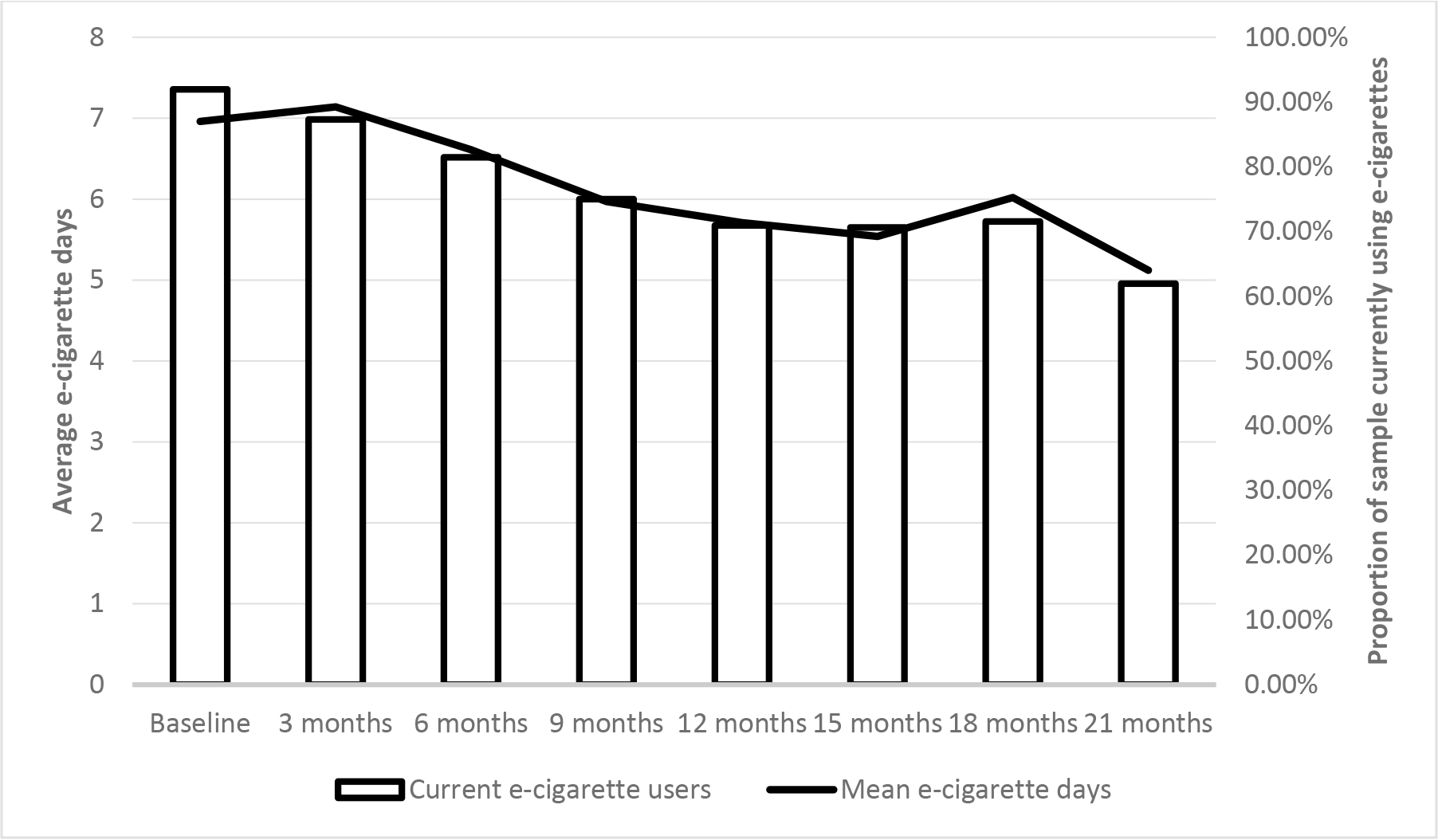
This represents the relationship between the current e-cigarette users (orange bars) with their average number of e-cigarette days of the past 14 days (blue solid line) at each wave of assessment.
Discussion
The aim of this study was to test the hypothesis that facets of impulsivity (positive urgency, negative urgency, sensation seeking, and lack of premeditation) would prospectively predict e-cigarette use over time in a sample of young adult users. Some findings were consistent with our expectations: participants with higher sensation seeking and lack of premeditation at baseline consistently used e-cigarettes more frequently across all 8 waves of assessment. Unexpectedly, e-cigarette use was unrelated to positive and negative urgency. Additionally, there was a modest decline in e-cigarette frequency and prevalence over time.
These longitudinal results further support our previous findings in an independent sample of young adult cigarette smokers. In that study, we found e-cigarette use was positively associated with sensation seeking and lack of premeditation; positive and negative urgency predicted cigarette but not e-cigarette use (Doran & Tully, 2018). Another recent cross-sectional study among European adults suggested urgency measures may be more closely related to use of cigarettes than e-cigarettes (Kale et al., 2020). Overall, the pattern of results suggests that, at least among emerging adults who are not yet daily users, e-cigarette use may be driven by the pursuit of positive reinforcement without concern for consequences, and not in response to acute affective states. This contrasts with evidence regarding combustible cigarette use among emerging adults, which appears to be strongly related to negative urgency in particular (Doran & Tully, 2018; Doran et al., 2013; Spillane et al., 2010), and suggests differences in motivation for use. One potential explanation for these differences is that the greater social acceptability of e-cigarette use (Lee et al., 2017) may yield a broader pool of users, with greater likelihood of being motivated by an interest in experimenting with new, purportedly rewarding behaviors. Another potential explanation is the availability of nontraditional flavors in e-cigarettes making them more appealing and leading to increased frequency of vaping (Landry et al., 2019; Leventhal et al., 2019).
While not a primary focus of this study, the positive association between e-cigarette and marijuana frequency is notable. This is consistent with previous studies of emerging adults (Cohn et al., 2019) and potentially important given trends toward reduced restrictions on marijuana use. For example, Doran et al. (2021) recently reported that the association between e-cigarette and marijuana frequency grew stronger following legalization of recreational marijuana sales in California, perhaps as a result of perceptions that both products are safe (Roditis et al., 2015). This consistent finding suggests that interventions designed to reduce vaping will likely need to address concurrent marijuana use.
Since the participants in our study were young adults, the findings may not be generalized to older population of e-cigarette users. Another limitation of the study is that all participants were current e-cigarette users who did not use combustible cigarettes at the time of enrollment, and most of whom were non-daily e-cigarette users. Thus, we may not be able to extrapolate our findings to daily e-cigarette users, or dual users of e-cigarettes and combustible cigarettes, though frequency of e-cigarette use (35–50% of days) was comparable to other surveys (e.g., Morean et al., 2018; Vogel et al., 2018). Data were provided via online surveys and may be subject to bias, though the same is true of self-report measures collected in controlled settings (Kraut et al., 2004). Data were collected at a time of decreasing restrictions on marijuana use in many jurisdictions, raising the possibility that reported marijuana prevalence reflects a reduction in bias against reporting use. Finally, because there are no validated measures by which to quantify e-cigarette consumption, we focused on frequency of use, potentially obscuring differences in use patterns.
In sum, these findings are helpful in identifying individuals who are vulnerable to e-cigarette use, and potentially paving the way for interventions to help them to stop vaping. Data suggest that emerging adults who are prone to seeking out novel stimuli and who tend to act rashly without considering the consequences may be particularly vulnerable to e-cigarette use over time. These young adults may thus be the highest priority targets for nicotine and tobacco intervention and prevention programs.
Role of Funding Sources:
This work was supported by the National Institutes of Health (grant R01 DA 037217, Doran), which provided financial support but had no other role in this project. Dr. Crotty Alexander’s salary was supported in part by a VA Merit Award (1I01BX004767, PI LCA), NIH NHLBI R01 (R01HL147326, PI LCA), and TRDRP award (T30IP0965, PI LCA).
Footnotes
Disclosure of interest: The authors declare no conflict of interest.
References
- 1.Dai H, & Leventhal AM (2019). Prevalence of e-Cigarette Use Among Adults in the United States, 2014–2018. JAMA, 322(18), 1824–1827. 10.1001/jama.2019.15331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schulenberg JE, Patrick ME, Johnston LD, O’Malley PM, Bachman JG & Miech RA (2021). Monitoring the Future national survey results on drug use, 1975–2020: Volume II, College students and adults ages 19–60. Ann Arbor: Institute for Social Research, University of Michigan. Available at http://monitoringthefuture.org/pubs/monographs/mtf-vol2_2020.pdf. [Google Scholar]
- 3.Collins L, Glasser AM, Abudayyeh H, Pearson JL, & Villanti AC (2019). E-Cigarette Marketing and Communication: How E-Cigarette Companies Market E-Cigarettes and the Public Engages with E-cigarette Information. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco, 21(1), 14–24. 10.1093/ntr/ntx284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Masso-Silva JA, Moshensky A, Shin J, Olay J, Nilaad S, Advani I, Bojanowski CM, Crotty S, Li WT, Ongkeko WM, Singla S, & Crotty Alexander LE (2021). Chronic E-Cigarette Aerosol Inhalation Alters the Immune State of the Lungs and Increases ACE2 Expression, Raising Concern for Altered Response and Susceptibility to SARS-CoV-2. Frontiers in physiology, 12, 649604. 10.3389/fphys.2021.649604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharma A, Lee J, Fonseca AG, Moshensky A, Kothari T, Sayed IM, Ibeawuchi SR, Pranadinata RF, Ear J, Sahoo D, Crotty-Alexander LE, Ghosh P, & Das S (2021). E-cigarettes compromise the gut barrier and trigger inflammation. iScience, 24(2), 102035. 10.1016/j.isci.2021.102035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ween MP, Moshensky A, Thredgold L, Bastian NA, Hamon R, Badiei A, Nguyen PT, Herewane K, Jersmann H, Bojanowski CM, Shin J, Reynolds PN, Crotty Alexander LE, & Hodge SJ (2021). E-cigarettes and health risks: more to the flavor than just the name. American journal of physiology. Lung cellular and molecular physiology, 320(4), L600–L614. 10.1152/ajplung.00370.2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bozier J, Chivers EK, Chapman DG, Larcombe AN, Bastian NA, Masso-Silva JA, Byun MK, McDonald CF, Crotty Alexander LE, & Ween MP (2020). The Evolving Landscape of e-Cigarettes: A Systematic Review of Recent Evidence. Chest, 157(5), 1362–1390. 10.1016/j.chest.2019.12.042 [DOI] [PubMed] [Google Scholar]
- 8.Tsai M, Byun MK, Shin J, & Crotty Alexander LE (2020). Effects of e-cigarettes and vaping devices on cardiac and pulmonary physiology. The Journal of physiology, 598(22), 5039–5062. 10.1113/JP279754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mikheev VB, Brinkman MC, Granville CA, Gordon SM, & Clark PI (2016). Real-Time Measurement of Electronic Cigarette Aerosol Size Distribution and Metals Content Analysis. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco, 18(9), 1895–1902. 10.1093/ntr/ntw128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tegin G, Mekala HM, Sarai SK, & Lippmann S (2018). E-Cigarette Toxicity?. Southern medical journal, 111(1), 35–38. 10.14423/SMJ.0000000000000749 [DOI] [PubMed] [Google Scholar]
- 11.Bold KW, Kong G, Camenga DR, Simon P, Cavallo DA, Morean ME, & Krishnan-Sarin S (2018). Trajectories of E-Cigarette and Conventional Cigarette Use Among Youth. Pediatrics, 141(1), e20171832. 10.1542/peds.2017-1832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leventhal AM, Strong DR, Kirkpatrick MG, Unger JB, Sussman S, Riggs NR, Stone MD, Khoddam R, Samet JM, & Audrain-McGovern J (2015). Association of Electronic Cigarette Use With Initiation of Combustible Tobacco Product Smoking in Early Adolescence. JAMA, 314(7), 700–707. 10.1001/jama.2015.8950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doran N, Brikmanis K, Petersen A, Delucchi K, Al-Delaimy WK, Luczak S, Myers M, & Strong D (2017). Does e-cigarette use predict cigarette escalation? A longitudinal study of young adult non-daily smokers. Preventive medicine, 100, 279–284. 10.1016/j.ypmed.2017.03.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bold KW, Morean ME, Kong G, Simon P, Camenga DR, Cavallo DA, & Krishnan-Sarin S (2017). Early age of e-cigarette use onset mediates the association between impulsivity and e-cigarette use frequency in youth. Drug and alcohol dependence, 181, 146–151. 10.1016/j.drugalcdep.2017.09.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reff J, & Baschnagel JS (2021). The role of affective urgency and emotion regulation in vaping susceptibility. Addictive behaviors reports, 14, 100355. 10.1016/j.abrep.2021.100355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cyders MA & Smith GT (2007). Mood-based rash action and its components: Positive and negative urgency. Pers Ind Dif, 43, 839–50. [Google Scholar]
- 17.Lynam DR, Smith GT, Whiteside SP, Cyders MA (2006). The UPPS-P: Assessing five personality pathways to impulsive behavior (Technical Report). West Lafayette, IN: Purdue University. [Google Scholar]
- 18.Kaiser A, Bonsu JA, Charnigo RJ, Milich R, & Lynam DR (2016). Impulsive Personality and Alcohol Use: Bidirectional Relations Over One Year. Journal of studies on alcohol and drugs, 77(3), 473–482. 10.15288/jsad.2016.77.473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Birkley EL, & Smith GT (2011). Recent advances in understanding the personality underpinnings of impulsive behavior and their role in risk for addictive behaviors. Current drug abuse reviews, 4(4), 215–227. 10.2174/1874473711104040215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.VanderVeen JD, Hershberger AR, & Cyders MA (2016). UPPS-P model impulsivity and marijuana use behaviors in adolescents: A meta-analysis. Drug and alcohol dependence, 168, 181–190. 10.1016/j.drugalcdep.2016.09.016 [DOI] [PubMed] [Google Scholar]
- 21.Doran N, Cook J, McChargue D, & Spring B (2009). Impulsivity and cigarette craving: differences across subtypes. Psychopharmacology, 207(3), 365–373. 10.1007/s00213-009-1661-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mitchell SH (1999). Measures of impulsivity in cigarette smokers and non-smokers. Psychopharmacology, 146(4), 455–464. 10.1007/pl00005491 [DOI] [PubMed] [Google Scholar]
- 23.Kale D, Stautz K, & Cooper A (2018). Impulsivity related personality traits and cigarette smoking in adults: A meta-analysis using the UPPS-P model of impulsivity and reward sensitivity. Drug and alcohol dependence, 185, 149–167. 10.1016/j.drugalcdep.2018.01.003 [DOI] [PubMed] [Google Scholar]
- 24.Pang RD, Hom MS, Geary BA, Doran N, Spillane NS, Guillot CR, & Leventhal AM (2014). Relationships between trait urgency, smoking reinforcement expectancies, and nicotine dependence. Journal of addictive diseases, 33(2), 83–93. 10.1080/10550887.2014.909695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee DC, Peters JR, Adams ZW, Milich R, & Lynam DR (2015). Specific dimensions of impulsivity are differentially associated with daily and non-daily cigarette smoking in young adults. Addictive behaviors, 46, 82–85. 10.1016/j.addbeh.2015.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Conner M, Grogan S, Simms-Ellis R, Scholtens K, Sykes-Muskett B, Cowap L, Lawton R, Armitage CJ, Meads D, Schmitt L, Torgerson C, West R, & Siddiqi K (2019). Patterns and predictors of e-cigarette, cigarette and dual use uptake in UK adolescents: evidence from a 24-month prospective study. Addiction (Abingdon, England), 114(11), 2048–2055. 10.1111/add.14723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grant JE, Lust K, Fridberg DJ, King AC, & Chamberlain SR (2019). E-cigarette use (vaping) is associated with illicit drug use, mental health problems, and impulsivity in university students. Annals of clinical psychiatry : official journal of the American Academy of Clinical Psychiatrists, 31(1), 27–35. [PMC free article] [PubMed] [Google Scholar]
- 28.Doran N, & Tully L (2018). Impulsivity and tobacco product use over time. Addictive behaviors, 85, 153–157. 10.1016/j.addbeh.2018.06.007 [DOI] [PubMed] [Google Scholar]
- 29.Lanza HI, Motlagh G, & Orozco M (2020). E-cigarette use among young adults: A latent class analysis examining co-use and correlates of nicotine vaping. Addictive behaviors, 110, 106528. 10.1016/j.addbeh.2020.106528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sobell L & Sobell M (1992). Timeline follow-back. In Measuring Alcohol Consumption: Psychological and Biological Methods, Allen J & Litten R (Eds). Humana Press, Totowa, NJ. doi: 10.1007/978-1-4612-0357-5_3. [DOI] [Google Scholar]
- 31.Pedersen ER, Grow J, Duncan S, Neighbors C, & Larimer ME (2012). Concurrent validity of an online version of the Timeline Followback assessment. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors, 26(3), 672–677. 10.1037/a0027945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cyders MA, Littlefield AK, Coffey S, & Karyadi KA (2014). Examination of a short English version of the UPPS-P Impulsive Behavior Scale. Addictive behaviors, 39(9), 1372–1376. 10.1016/j.addbeh.2014.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Whiteside Stephen & Lynam Donald. (2001). The Five Factor Model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences. 30. 669–689. 10.1016/S0191-8869(00)00064-7. [DOI] [Google Scholar]
- 34.Kale D, Pickering A, & Cooper A (2020). Examining the relationship between impulsivity-related personality traits and e-cigarette use in adults. Addictive behaviors, 106, 106348. 10.1016/j.addbeh.2020.106348 [DOI] [PubMed] [Google Scholar]
- 35.Doran N, Khoddam R, Sanders PE, Schweizer CA, Trim RS, & Myers MG (2013). A prospective study of the Acquired Preparedness Model: the effects of impulsivity and expectancies on smoking initiation in college students. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors, 27(3), 714–722. 10.1037/a0028988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Spillane NS, Smith GT, & Kahler CW (2010). Impulsivity-like traits and smoking behavior in college students. Addictive behaviors, 35(7), 700–705. 10.1016/j.addbeh.2010.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee HY, Lin HC, Seo DC, & Lohrmann DK (2017). Determinants associated with E-cigarette adoption and use intention among college students. Addictive behaviors, 65, 102–110. 10.1016/j.addbeh.2016.10.023 [DOI] [PubMed] [Google Scholar]
- 38.Leventhal AM, Goldenson NI, Cho J, Kirkpatrick MG, McConnell RS, Stone MD, Pang RD, Audrain-McGovern J, & Barrington-Trimis JL (2019). Flavored E-cigarette Use and Progression of Vaping in Adolescents. Pediatrics, 144(5), e20190789. 10.1542/peds.2019-0789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Landry RL, Groom AL, Vu TT, Stokes AC, Berry KM, Kesh A, Hart JL, Walker KL, Giachello AL, Sears CG, McGlasson KL, Tompkins LK, Mattingly DT, Robertson RM, & Payne TJ (2019). The role of flavors in vaping initiation and satisfaction among U.S. adults. Addictive behaviors, 99, 106077. 10.1016/j.addbeh.2019.106077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cohn AM, Abudayyeh H, Perreras L, & Peters EN (2019). Patterns and correlates of the co-use of marijuana with any tobacco and individual tobacco products in young adults from Wave 2 of the PATH Study. Addictive behaviors, 92, 122–127. 10.1016/j.addbeh.2018.12.025 [DOI] [PubMed] [Google Scholar]
- 41.Doran N, Strong D, Myers MG, Correa JB, & Tully L (2021). Post-legalization changes in marijuana use in a sample of young California adults. Addictive behaviors, 115, 106782. 10.1016/j.addbeh.2020.106782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Roditis ML, & Halpern-Felsher B (2015). Adolescents’ Perceptions of Risks and Benefits of Conventional Cigarettes, E-cigarettes, and Marijuana: A Qualitative Analysis. The Journal of adolescent health : official publication of the Society for Adolescent Medicine, 57(2), 179–185. 10.1016/j.jadohealth.2015.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Morean ME, Butler ER, Bold KW, Kong G, Camenga DR, Cavallo DA, Simon P, O’Malley SS, & Krishnan-Sarin S (2018). Preferring more e-cigarette flavors is associated with e-cigarette use frequency among adolescents but not adults. PloS one, 13(1), e0189015. 10.1371/journal.pone.0189015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vogel EA, Ramo DE, & Rubinstein ML (2018). Prevalence and correlates of adolescents’ e-cigarette use frequency and dependence. Drug and alcohol dependence, 188, 109–112. 10.1016/j.drugalcdep.2018.03.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kraut R, Olson J, Banaji M, Bruckman A, Cohen J, & Couper M (2004). Psychological research online: report of Board of Scientific Affairs’ Advisory Group on the Conduct of Research on the Internet. The American psychologist, 59(2), 105–117. 10.1037/0003-066X.59.2.105 [DOI] [PubMed] [Google Scholar]


