Abstract
Isolated right ventricular myocardial infarction is an extremely rare condition, and its diagnosis may be challenging. We present the case of a 63-year-old man who arrived at the emergency department with chest pain; electrocardiogram showed ST-segment elevation in precordial leads, for which, the diagnosis of anterior ST-elevation myocardial infarction was initially made. Coronary angiography showed diffuse coronary artery ectasia and total thrombotic occlusion of the right coronary artery that was treated by angioplasty and stenting, resulting in resolution of the chest pain and ST-segment elevation. Echocardiogram showed right ventricular systolic dysfunction and cardiac magnetic resonance confirmed the diagnosis of isolated right ventricular myocardial infarction. We highlight the value of invasive and non-invasive tests to diagnose this rare condition.
<Learning objective: Isolated right ventricular myocardial infarction is a very uncommon, but important differential diagnosis of anterior ST-elevation myocardial infarction. There exist certain electrocardiographic features favoring its diagnosis, although, recognition requires a high index of suspicion and support in different modalities of study including cardiac magnetic resonance and coronary angiography. Proper identification of it, will help to guide treatment and support for possible complications.>
Keywords: Isolated right ventricular myocardial infarction, Electrocardiographic diagnosis, Coronary artery ectasia, Cardiac magnetic resonance
Introduction
Isolated right ventricular myocardial infarction (IRVMI) is an extremely rare condition, and its diagnosis may be challenging. It requires a high index of suspicion and support in different modalities of study. The usual presentation is an electrocardiographic manifestation of ST-segment elevation in the inferior leads, which suggest the right coronary artery (RCA) as the culprit vessel [1], but in limited cases it can be manifested as ST-segment elevation in the anterior leads. Ultimately, it requires complementary imaging studies to confirm the diagnosis and coronary angiography to demonstrate RCA involvement. We present the case of a man who had an IRVMI with an atypical electrocardiographic presentation, emphasizing the usefulness of complementary studies to reach the final diagnosis.
Case report
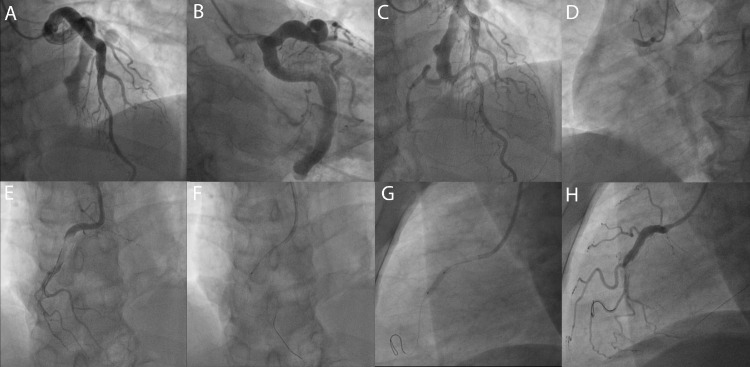
A 63-year-old male without previous cardiovascular history, arrived at the emergency department with acute oppressive chest pain radiating to the left arm, diaphoresis, and dyspnea lasting two hours. He exhibited normal vital signs, physical examination revealed jugular distension, but there was no paradoxical pulse, no murmurs, S3 gallop or other change in heart sounds, and no pulmonary rales were noted, also, there was no lower extremities edema. Electrocardiogram (ECG) showed ST-segment elevation in precordial leads from V1 to V4 and minor ST segment depression (<1 mm) in the inferior leads (Fig. 1A). Diagnosis of anteroseptal ST-elevation myocardial infarction (STEMI) was made, suspecting occlusion of the left anterior descending artery (LAD) as the culprit vessel. The patient was transferred to the catheter laboratory immediately to undergo primary percutaneous coronary intervention. Coronary angiography results showed left side dominant coronary arteries, with diffuse coronary artery ectasia (CAE) in LAD and circumflex artery with thrombolysis in myocardial infarction (TIMI)-2 final flow grade. RCA was also observed with diffuse CAE and total thrombotic occlusion in the proximal segment was treated by angioplasty and stenting. Restoration of TIMI-3 flow to the target vessel was obtained (Fig. 2A-H and Video 1).
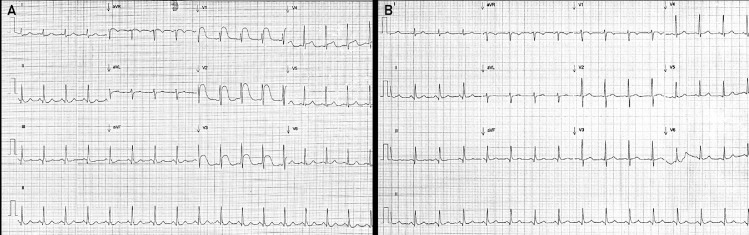
Fig. 1.
Electrocardiographic findings. (A) Initial electrocardiogram (ECG) showing convex ST-segment elevation in the anterior precordial leads V1 to V4, with peak elevation in V2 and progressive reduction in ST-segment elevation across the precordial leads, minor ST-segment depression in the inferior leads and clockwise rotation of the heart is also observed. (B) Post-coronary angioplasty ECG showing normal sinus rhythm with resolution of ST-segment elevation and no anterior Q waves.
Fig. 2.
Coronary angiography. (A, B, C) Diffuse coronary ectasia was observed in left anterior descending artery and circumflex artery, both vessels with thrombolysis in myocardial infarction (TIMI) flow grade 2. (D) Right coronary artery with total thrombotic occlusion in the proximal segment. (E, F, G, H) Right coronary artery angioplasty and stenting with final TIMI flow grade 3.
After the procedure, he was admitted to the coronary care unit, and a control ECG showed normalization of the ST-segment (Fig. 1B). A central venous catheter was inserted, initially registering a central venous pressure of 11 mmHg. The chest radiography did not show pulmonary congestion. Initial laboratory results revealed elevated levels of high-sensitivity cardiac troponin T (3096 pg/mL), creatine kinase-MB (178 ng/mL), and N-terminal pro-brain natriuretic peptide (371 pg/mL).
Routine echocardiogram showed hypokinetic right ventricular free wall, dilated right ventricle (RV), tricuspid annular plane systolic excursion of 16 mm, and S wave tissue Doppler velocity of 9 cm/seg. Left ventricle (LV) was of average size, without partial or segmental mobility alteration, and left ventricular ejection fraction was 59%.
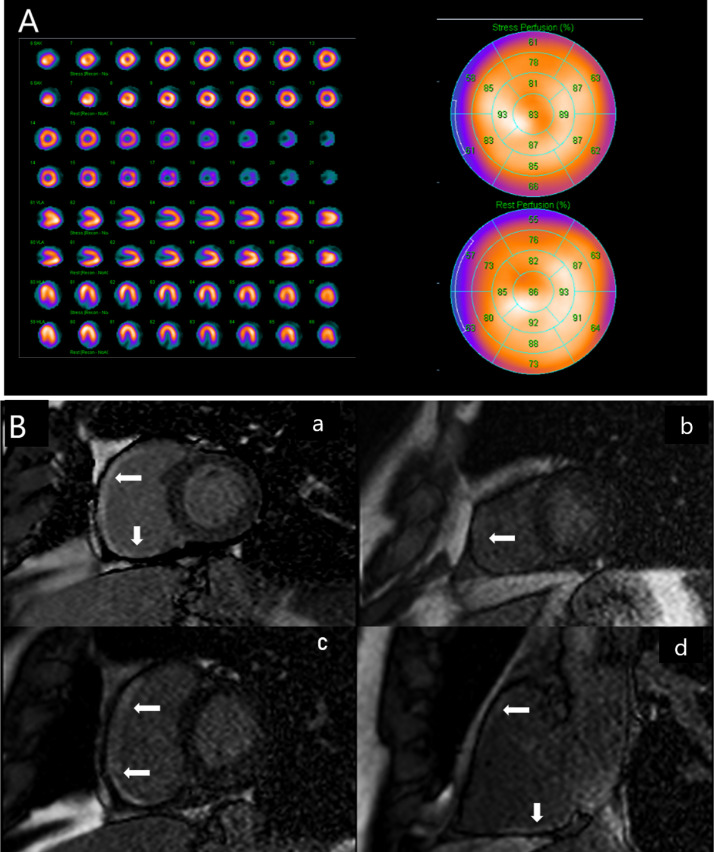
Before discharge, it was decided to perform a rest-stress myocardial perfusion scintigraphy with single photon emission computed tomography/computed tomography (SPECT/CT) without evidence of myocardial perfusion disturbances that suggest post-myocardial infarction scarring or stress ischemia in the LV (Fig. 3A). Also, cardiac magnetic resonance imaging (CMR) was performed, showing transmural late enhancement of the inferior and free wall of the RV with no late enhancement in LV (Fig. 3B).
Fig. 3.
Single photon emission computed tomography/computed tomography imaging (A) and cardiac magnetic resonance imaging (B). (A) A normal polar map of left ventricular perfusion, with no change in the images between rest and stress. (B) Short axis (a, b, c) and right two-chamber axis (d) showing transmural late enhancement (arrows) of the free and inferior wall of the right ventricle. No late enhancement was observed in left ventricle.
The results of these studies helped to conclude the diagnosis of IRVMI. The patient was discharged with standard treatment plus oral anticoagulation.
Discussion
ST-segment elevation in the anterior precordial leads in patients with acute coronary syndromes usually indicates LAD occlusion. However, anterior ST-segment elevation has also been described in RCA occlusion and is thought to signify RVMI [2]. RVMI may occur in isolation or combination with LV involvement. The association of RVMI with infarction of the inferior wall of the LV has been found in 10-50% of patients [3] and is attributed to occlusion of the proximal RCA [4], usually manifests with ST-segment elevations in leads II, III, and aVF as well as in V3R and V4R.
Isolated RVMI occurs seldom; approximately only 2% of cases are reported on autopsy and are associated with higher in-hospital morbidity as well as mortality related to hemodynamic and electrophysiological complications [5]. Isolated RVMI occurs during the following anatomic situations: occlusion of a non-dominant RCA artery [6], proximal occlusion of the RCA (proximal to the acute marginal branches) with the brisk left to RCA collateral blood flow [7], isolated occlusion of an acute marginal branch [8], and heart rotation [9].
Isolated ST-segment elevation in precordial leads due to RVMI is uncommon in clinical practice. In this case, there was observed ST-segment elevation in the precordial leads associated with a minor ST-segment depression in the inferior leads. This finding has been described previously [1], and usually suggests an occlusion of the distal LAD. This is the reason why taking right precordial leads in this scenario is not performed routinely. Certain electrocardiographic features have been suggested, which may help differentiate ST-segment elevation secondary to isolated RVMI from LAD territory infarction. However, these features are not pathognomonic, and it may be impossible to make this distinction based on electrocardiography alone. The absence of Q-wave development, convex ST elevation, peak ST elevation in V2, and progressive reduction in ST-segment elevation across the precordial leads have been reported as favoring the diagnosis of RVMI [5]; all these features were observed in our clinical case.
RV dilation has been identified as a predisposing factor for cardiac clockwise rotation because of right ventricular dilatation and the increase of right ventricular diastolic pressure, which also may be associated with ST-segment elevation in precordial leads in patients with acute occlusion of RCA [9]. In our case this could be another possible explanation of the ST- segment elevation in the precordial leads.
Recognition of isolated RVMI requires a high index of suspiciousness and appropriate imaging of both ventricles with either echocardiography or CMR to detect dilation and hypokinesia of the RV and preserved left ventricle function.
Echocardiogram in patients with extensive RV infarction usually shows dilatation of the cavity and disturbances in the mobility of its walls [3]. In our patient, an apparent right ventricular dysfunction was found by this method.
CMR emerged as a powerful tool in visualizing myocardial injury after STEMI. In our case, SPECT-CT imaging was useful in the identification of isolated RVMI, which was then confirmed by finding late gadolinium enhancement in the RV in the CMR, with no late enhancement in the LV.
In this particular case, not only the unusual diagnosis of isolated RVMI, but also diffuse CAE was found. Patients with CAE can suffer infarction by various mechanisms, from obstructive lesions to decreased intracoronary flow [10]. In our clinical case, CAE could have been a factor associated with acute myocardial infarction.
To our knowledge, this is the first case of isolated RVMI with electrocardiographic expression in precordial leads confirmed by CMR and associated with CAE.
Conclusion
Isolated RVMI is an uncommon but essential differential diagnosis of anterior STEMI, although it requires a high index of suspicion and invasive and non-invasive tests to confirm.
Declaration of Competing Interest
The authors declare that there is no conflict of interest.
Acknowledgments
No acknowledgments
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jccase.2022.01.012.
Appendix. Supplementary materials
References
- 1.Zimetbaum P.J., Josephson M.E. Use of the electrocardiogram in acute myocardial infarction. N Engl J Med. 2003;348:933–940. doi: 10.1056/NEJMra022700. [DOI] [PubMed] [Google Scholar]
- 2.Nabais S., Martin-Yuste V., Masotti M., Sabaté M. Isolated right ventricular infarction presenting with anterior ST-segment elevation: a case for careful assessment of right ventricular branch occlusion. Rev Port Cardiol. 2012;31:301–304. doi: 10.1016/j.repc.2011.09.022. [DOI] [PubMed] [Google Scholar]
- 3.Vargas-Barrón J., Romero-Cárdenas A., Roldán F.J., Vázquez-Antona CA. Acute right atrial and ventricular infarction. Rev Esp Cardiol. 2007;60:51–66. [PubMed] [Google Scholar]
- 4.Jim M.H., On-On Chan A., Wong C.P., Yiu K.H., Miu R., Wai-Luen Lee S., Lau C.P. Clinical implications of precordial ST-segment elevation in acute inferoposterior myocardial infarction caused by proximal right coronary artery occlusion. Clin Cardiol. 2007;30:331–335. doi: 10.1002/clc.20096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Namana V., Gupta S.S., Abbasi A.A., Raheja H., Shani J., Hollander G. Right ventricular infarction. Cardiovasc Revasc Med. 2018;19(1 Pt A):43–50. doi: 10.1016/j.carrev.2017.07.009. [DOI] [PubMed] [Google Scholar]
- 6.Kircher T., Moothart R. Isolated right ventricular infarction with massive dilation: acquired Uhl's disease? Arch Pathol Lab Med. 1982;106:385–387. [PubMed] [Google Scholar]
- 7.Cafri C., Orlov G., Weinstein J.M., Kobal S., Ilia R. ST elevation in the anterior precordial leads during right ventricular infarction: lessons learned during primary coronary angioplasty–a case report. Angiology. 2001;52:417–420. doi: 10.1177/000331970105200607. [DOI] [PubMed] [Google Scholar]
- 8.Koh T.W., Coghlan J.G., Lipkin D.P. Anterior ST segment elevation due to isolated right ventricular infarction during right coronary angioplasty. Int J Cardiol. 1996;54:201–206. doi: 10.1016/0167-5273(96)02610-1. [DOI] [PubMed] [Google Scholar]
- 9.Zheng J., Lin J., Shen N., Qu B. Proximal complete occlusion of right coronary artery presenting with precordial ST-segment elevation: a case report. Medicine (Baltimore) 2016;95:e5113. doi: 10.1097/MD.0000000000005113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Plata-Corona J.C., Carvajal-Juarez I., Espinola-Zavaleta N., Damas-De Los Santos F., Rivera-Bravo B., Alexanderson-Rosas E. (13)N-Ammonia myocardial blood flow quantitation in patient with aneurismal coronary artery disease. J Nucl Cardiol. 2021 doi: 10.1007/s12350-021-02642-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.