Abstract
This clinical trial examined animal-assisted therapy (AAT) as an adjunct to Trauma-Focused Cognitive-Behavioral Therapy (TF-CBT) for abused youth with posttraumatic stress disorder (PTSD). Youth between the ages of 6 and 17 (M = 11.79, SD = 3.08) were randomized to receive standard TF-CBT or TF-CBT with adjunctive AAT (TF-CBT+AAT) employing retired service dogs. Feasibility metrics evaluating the addition of AAT were collected in addition to common clinical outcomes evaluated in TF-CBT trials. The inclusion of AAT increased the number of potential participants who declined participation and there were no noted benefits for treatment retention or satisfaction with services. Analyses showed that the inclusion of AAT did not enhance improvement of PTSD symptom severity (β = .90, t = .94, p = .351) or a number of other outcomes. On the contrary, there were indications from analyses and clinician feedback that AAT may have attenuated improvement in many cases. This study identified a number of important feasibility considerations in the design of studies testing AAT. However, the results examining clinical outcomes suggest that the inclusion of AAT with TF-CBT in the treatment of maltreated youth with PTSD is not warranted at this time.
Keywords: animal-assisted therapy, posttraumatic stress, Trauma-Focused Cognitive-Behavioral Therapy, child abuse, trauma
Current global estimates are that nearly 12.7% of youth experience sexual abuse and 22.6% of youth experience physical abuse before the age of 18 (Stoltenborgh, Bakermans-Kranenburg, Alink, & van IJzendoorn, 2015). Child abuse is linked to various untoward outcomes and one of the most common psychiatric concerns following child abuse is posttraumatic stress disorder (PTSD; Finkelhor, 2008; Saunders, Berliner, & Hanson, 2004). PTSD is a distinct clinical condition that includes intrusive thoughts of the traumatic event, avoidance of stimuli associated with the trauma that could induce distress, alterations in physiological arousal and reactivity, and maladaptive alterations of cognitions and mood (American Psychiatric Association, 2013). The long-term stability of PTSD among youth is thought to be high, with one study showing that 32.7% of abused youth continued to meet full diagnostic criteria two years later (Famularo, Fenton, Augustyn, & Zuckerman, 1996). Given the prevalence and stability of PTSD following child abuse, research examining the identification and implementation of effective treatment options is vital.
Trauma-Focused Cognitive-Behavioral Therapy (TF-CBT; Cohen, Mannarino, & Deblinger, 2017) is a structured protocol commonly utilized for the treatment of psychiatric concerns among youth who experienced various forms of trauma, including child abuse. Multiple randomized controlled trials (RCT) demonstrate that TF-CBT yields greater improvement than rapport-focused treatment for PTSD and a variety of other concerns (Cary & McMillen, 2012; Cohen, Deblinger, Mannarino, & Steer, 2004; Cohen, Mannarino, & Iyengar, 2011). Systematic reviews suggest that TF-CBT is the most well-established intervention for youth experiencing trauma and maltreatment (Gillies, Taylor, Gray, O’Brien, & D’Abrew, 2012; Dorsey et al., 2017). Not surprisingly, TF-CBT is the most recognized and utilized evidence-based treatment among clinicians serving maltreated youth (Allen, Gharagozloo, & Johnson, 2012).
The TF-CBT protocol includes a number of common CBT techniques, such as coping skills training and psychoeducation, as well as imaginal and in vivo exposure exercises meant to desensitize the youth to memories and physical stimuli associated with the trauma. These exposure activities appear particularly effective for youth displaying higher levels of posttraumatic stress avoidance symptoms (Deblinger, Mannarino, Cohen, Runyon, & Steer, 2011). However, qualitative reports indicate that youth report the exposure exercises as being the most difficult portions of the treatment to complete, albeit they recognize them as the most helpful aspect of the intervention afterwards (Dittmann & Jensen, 2014). This may help explain reports that exposure exercises are the component least likely to be implemented by clinicians (Allen & Johnson, 2012) and that some clinicians serving abused youth believe TF-CBT is a poor fit for their patients (Pemberton, Conners-Burrow, Sigel, Sievers, Stokes, & Kramer, 2017).
It is not surprising then that a number of clinicians have sought to integrate interventions they believe may help ease the distress that can result from exposure procedures. Animal-assisted therapy (AAT) is one such technique. AAT is a specific form of animal-assisted intervention where the inclusion of the animal in treatment is done in a structured and goal-directed manner for the purposes of therapeutic benefit (Chandler, 2005) and is specifically promoted by some as a promising intervention for youth who experienced abuse (Parish-Plass, 2008; Reichart, Bermel, & Sori, 2016). The presence of animals is believed to have a calming effect during treatment sessions, allowing youth to better cope with distress and thereby allow for greater discussion and processing of traumatic memories (Reichert et al., 2016; Tedeschi, Sisa, Olmert, Parish-Plass, & Yount, 2015). Indeed, there is some limited evidence suggesting that animals, specifically dogs, can reduce physiological arousal and anxiety for abused youth experiencing other stress-inducing situations, such as participating in forensic interviews (Krause-Parello & Gulick, 2015).
Although nearly one-third of mental health clinicians serving maltreated youth report being at least somewhat likely to implement AAT (Allen & Crosby, 2014), relatively little empirical data examines the effectiveness of AAT. Some non-randomized trials suggest that AAT may improve various clinical outcomes for abused youth (Balluerka, Muela, Amiano, & Caldentey, 2015; Dietz, Davis, & Pennings, 2012); however, reviews of the literature criticize much of the AAT research on methodological grounds, often citing small sample sizes, poor metrics, absent or confounded control groups, and lack of randomization to conditions (e.g., Anestis, Anestis, Zawilinski, Hopkins, & Lilienfeld, 2014; Nimer & Lundahl, 2007; O’Haire, Guerin, & Kirkham, 2015). In addition, data suggests integrating techniques into TF-CBT that are not prescribed by the protocol may serve to weaken the intervention’s effectiveness, making the incorporation of AAT into TF-CBT worrisome (Allen & Hoskowitz, 2017). Nonetheless, if AAT was administered as an adjunct intervention meant to supplement a primary intervention, as is commonly recommended (Lefkowitz, Prout, Bleiberg, Paharia, & Debiak, 2005; Tedeschi et al., 2015), the possibility exists that exposure exercises may be more palatable to youth and thereby improve any number of outcomes, such as treatment retention, clinical symptomatology, and/or the rate of improvement. As such, well-designed RCTs are needed to determine whether incorporating AAT as an adjunct intervention for the child abuse population is feasible and provides incremental efficacy when compared to established trauma treatments such as TF-CBT (Nimer & Lundahl, 2007; Esposito, McCune, Griffin, & Maholmes, 2011).
The current study was developed to provide an initial investigation of whether the integration of AAT into an evidence-based treatment (i.e., TF-CBT) for abused youth with PTSD is feasible and would yield incremental benefit when compared to the standard treatment. The specific goals of the current study were to examine various aspects of feasibility, including whether the inclusion of dogs (a) impacted recruitment or retention efforts within a randomized controlled trial, (b) presented challenges to the implementation of the TF-CBT protocol, and (c) demonstrated sufficient incremental efficacy for the derivation of effect size estimates that might be used for power analyses in the design of a more definitive trial.
Method
Participants
Participants (n = 33) were youth between the ages of 6 and 17 (M = 11.79, SD = 3.08) presenting to an outpatient treatment clinic specializing in the treatment of maltreated children and adolescents. The sample was racially diverse with 63.6% Caucasian, 21.2% African-American, and 15.2% reporting multiple racial identities, while 21.2% were of Hispanic/Latino ethnicity. All participants were required to have a primary, non-offending caregiver who agreed to participate in the trial; the majority of the participating caregivers were a biological parent (n = 29, 88%). Complete demographic information is provided in Table 1. Prior to enrollment, all caregivers were administered the UCLA Posttraumatic Stress Disorder Reaction Index for DSM-5 (UCLA; Pynoos & Steinberg, 2014) to report on the trauma history and PTSD symptoms of youth. All youth were required to have experienced at least one incident of physical abuse, sexual abuse, and/or witnessing inter-partner violence and have a qualifying total score of ≥ 32 on the posttraumatic stress symptoms scale of the UCLA. Exclusion criteria included the youth’s estimated IQ being below 80 as assessed on the Kaufman Brief Intelligence Test (2nd ed., Kaufman & Kaufman, 2004), a diagnosed developmental delay or autism spectrum disorder, and significant impairment or safety issue that necessitated a higher level of care for the youth (e.g., active suicidal ideation). Also, given that the trial included interactions with dogs, participants were excluded if they had an uncontrolled allergy to dogs, a significant phobia or dislike of dogs, or a history of aggression toward animals.
Table 1:
Demographic Characteristics
| Demographic | Condition: n (%) | Statistic | p | |
|---|---|---|---|---|
| TF-CBT | TF-CBT+AAT | |||
| Child gender: | ||||
| Male | 5 (31.3) | 6 (35.3) | χ2(1) = .06 | .81 |
| Female | 11 (68.7) | 11 (64.7) | ||
| Child racial identity: | ||||
| White/Caucasian | 9 (56.3) | 12 (70.6) | χ2(2) = .74 | .69 |
| Black/African-American | 4 (25.0) | 3 (17.6) | ||
| Multiple ethnicities | 3 (18.7) | 2 (11.8) | ||
| Child ethnicity: | ||||
| Hispanic/Latino | 4 (25.0) | 3 (17.6) | χ2(1) = −27 | .606 |
| Not Hispanic/Latino | 12 (75.0) | 14 (82.4) | ||
| Index trauma: | ||||
| Sexual abuse | 8 (50.0) | 13 (76.5) | χ2(2) = 3.16 | .206 |
| Physical abuse | 6 (37.5) | 2 (11.8) | ||
| Inter-partner violence | 2 (12.5) | 2 (11.8) | ||
| Caregiver gender: | ||||
| Male | 3 (18.8) | 0 (0.0) | Fisher’s Exact | .103 |
| Female | 13 (81.3) | 17 (100.0) | ||
| Caregiver racial identity: | ||||
| White/Caucasian | 9 (56.3) | 13 (76.5) | χ2(2) = 1.84 | .447 |
| Black/African-American | 4 (25.0) | 3 (17.6) | ||
| Multiple ethnicities | 3 (18.8) | 1 (5.9) | ||
| Caregiver ethnicity: | ||||
| Hispanic/Latino | 4 (25.0) | 1 (5.9) | Fisher’s Exact | .175 |
| Not Hispanic/Latino | 12 (75.0) | 16 (94.1) | ||
| Caregiver highest level of education: | ||||
| Did not complete high school | 6 (37.5) | 2 (11.8) | Fisher’s Exact | .182 |
| Completed high school | 3 (18.8) | 1 (5.9) | ||
| Some college | 5 (31.3) | 7 (41.2) | ||
| Completed bachelor’s degree | 2 (12.5) | 6 (35.3) | ||
| Completed graduate degree | 0 (0.0) | 1 (5.9) | ||
| Caregiver marital status: | ||||
| Single, never married | 2 (12.5) | 5 (29.4) | Fisher’s Exact | .627 |
| Married | 6 (37.5) | 4 (23.5) | ||
| Divorced | 5 (31.3) | 6 (35.3) | ||
| Married, but separated | 2 (12.5) | 1 (5.9) | ||
| Other | 1 (6.3) | 1 (5.9) | ||
| Caregiver relationship to child: | ||||
| Biological parent | 14 (87.5) | 15 (88.2) | Fisher’s Exact | 1.0 |
| Other biological relative | 0 (0.0) | 1 (5.9) | ||
| Adoptive parent | 1 (6.3) | 1 (5.9) | ||
| Other | 1 (6.3) | 0 (0.0) | ||
| Estimated annual family income: | ||||
| Less than $25,000 | 3 (18.8) | 3 (17.6) | Fisher’s Exact | .931 |
| $25,000 - $50,000 | 7 (43.8) | 8 (47.1) | ||
| $50,001 - $75,000 | 5 (31.3) | 3 (17.6) | ||
| $75,001 - $100,000 | 0 (0.0) | 1 (5.9) | ||
| More than $100,000 | 1 (6.3) | 2 (11.8) | ||
Procedure
This study followed a randomized controlled feasibility trial design, conformed to CONSORT guidelines on the reporting of clinical trials, and was pre-registered on www.clinicaltrials.gov (NCT03135119). The following procedures were approved by an applicable Institutional Review Board and procedures related to the use of the participating dogs were approved by an Institutional Animal Care and Use Committee. Participants were recruited through two primary means. First, clinicians working at the treatment site where the trial took place identified potential participants through the course of standard intake procedures and referred qualifying cases to the research staff. Second, caregivers directly contacted study staff after learning of the trial through various forms of public dissemination. As shown in the CONSORT diagram in Figure 1, 54 of the referred potential participants were deemed eligible for inclusion and 33 participants were enrolled.
Figure 1:
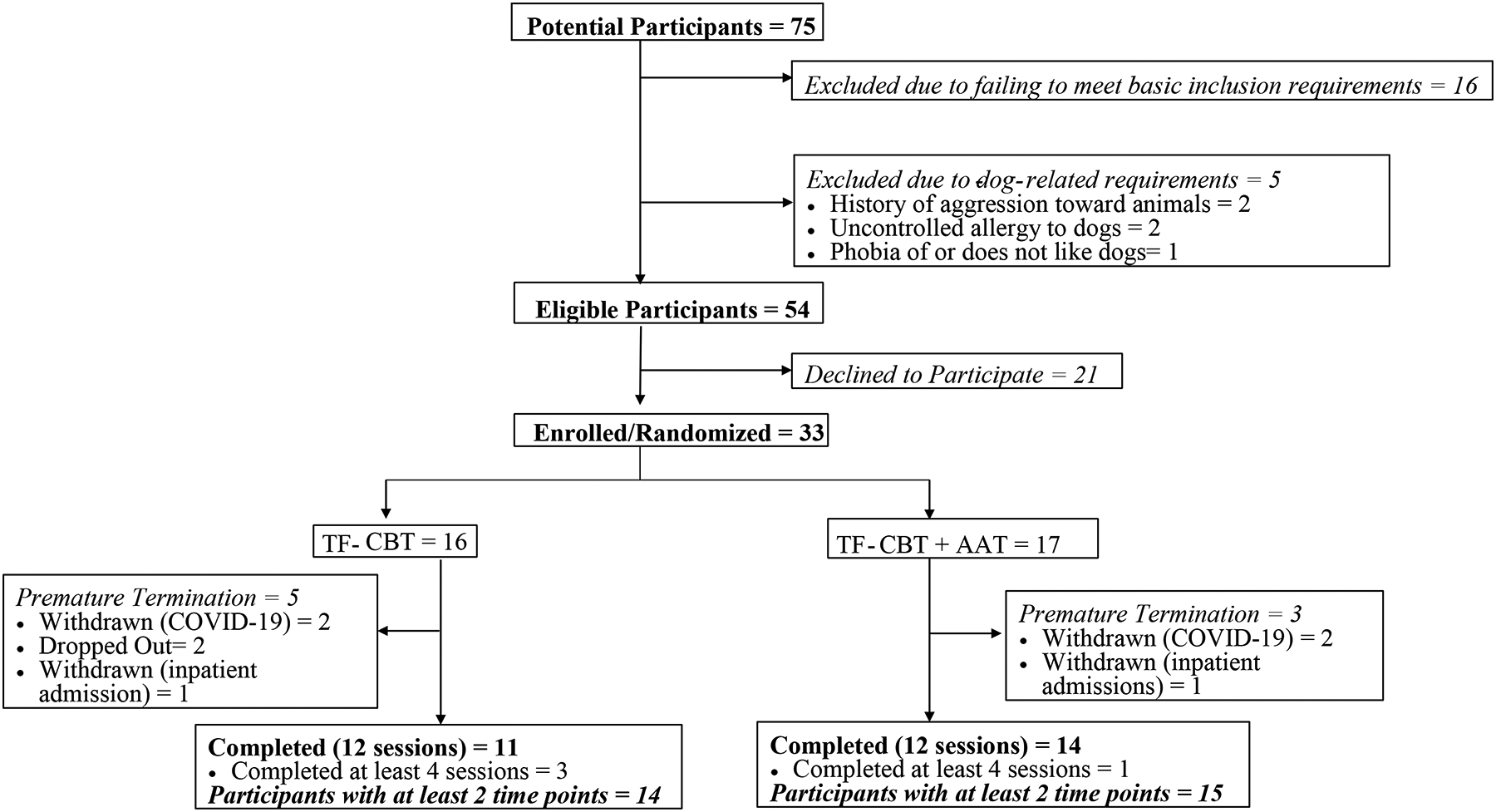
CONSORT Diagram
Enrolled participants were randomized to receive either standard TF-CBT or TF-CBT+AAT. The trial utilized a blocked randomization procedure in an attempt to balance the groups on gender and age (parsed 6–11, 12–17). The randomization sequence was constructed prior to initiation of the trial by the study’s statistician. Two clinicians participated in the trial and each provided care in both conditions. Assignment to clinician was determined randomly. The clinicians were both Master’s-level clinical social workers with 3–5 years experience in the treatment of abused youth. The clinicians were adequately trained in the implementation of both treatment conditions (see below) and there were no observable differences in the proportion of TF-CBT to TF-CBT+AAT cases treated by the two clinicians (χ2(1) = 1.50, p = .221).
Referred youth and their caregivers underwent a pre-treatment assessment to verify eligibility prior to enrollment (Time 1). This assessment included self-report and caregiver-report measures to assess posttraumatic stress symptoms and general internalizing and externalizing concerns. Participants completed the same assessment battery during session 5 (Time 2), at which point foundational skills-building was complete and construction of the trauma narrative began, and session 9 (Time 3), which was the first session following completion of the trauma narrative. In addition, a post-treatment assessment occurred following completion of treatment (Time 4). Caregivers received $50 after completing the pre-treatment and post-treatment assessments and youth received either a toy or gift card valued at $15; caregivers received a $5 gift card to a gas station at the completion of each treatment session. Research assistants were blinded to participant condition at each of the assessment points and remained so throughout the duration of the trial. The study’s coordinator was responsible for coding and managing the collected data and was blinded to participant condition as was the study’s statistician.
TF-CBT
The TF-CBT condition utilized the 12, 90-minute sessions format typical of most TF-CBT trials (Cohen et al., 2017). The first four sessions focused on providing psychoeducation regarding the youth’s specific form of trauma exposure and posttraumatic stress symptoms, and teaching relaxation, affect regulation, and cognitive coping skills. Gradual exposure occurred in each of these sessions by repeatedly discussing the index trauma and how each skill can be used to address its effects. Clinicians met with youth for approximately 45 minutes during each session, after which they met with caregivers for the remaining 45 minutes and provided training in the same skills. Sessions 5 through 9 centered on the development of a factual narrative of the youth’s trauma experience with a particular emphasis on eliciting thoughts, emotions, and physical sensations encountered during and after the event. The trauma narrative is an imaginal exposure exercise designed to extinguish conditioned responses (e.g. physiological, cognitive, avoidance) while reinforcing approach behaviors (e.g. discussing cognitions and affect with others) that facilitate effective coping with the traumatic event. Following construction of the trauma narrative, clinicians employed cognitive restructuring techniques to improve identified maladaptive cognitions. During each session, the clinician shared the youth’s work on the trauma narrative with the caregiver and implemented cognitive change techniques with the caregiver as indicated. The final four sessions of the protocol included the youth discussing the trauma narrative with the caregiver in a conjoint session, developing and implementing an in vivo exposure plan, teaching the youth and caregiver safety skills, and examining how the trauma experience might influence the youth’s life. As this served as the control condition to examine the incremental utility of incorporating a live animal, a stuffed plush animal of the youth’s choosing was required to be present in the room during each session and at the youth’s disposal. Clinicians were trained to TF-CBT certification requirements and met bi-weekly for consultation with the primary author, a certified and experienced TF-CBT clinician and researcher. In addition, clinicians completed fidelity checklists at the completion of each session, which were reviewed by the primary author to insure implementation of required techniques.
TF-CBT+AAT
For implementation of the AAT component, the researchers contracted with a local service dog organization that performs breeding, training, and placement of service dogs. The organization had a team of trained service dogs and their handlers that regularly visit psychiatric care facilities partner with the researchers. All of the dogs were either retired or selected for breeding, and no longer actively working in a service capacity. At the outset of the project, the handlers trained the clinicians in understanding canine body language and providing basic cues to the dog, including how to call the dog over, direct it to move away, and prompt it to sit or place its head on the youth’s lap. A series of pilot sessions with volunteer youth between the ages of 6 and 17 were conducted prior to data collection to allow the clinicians to practice integrating the dog into treatment and to receive feedback from the observing handlers. A participating dog was required to be in the room for all sessions where the youth was engaged in a portion of treatment, including the conjoint session with the caregiver. The manner in which the youth interacted with the dog was not dictated. In some instances the child preferred for the dog to be at his or her feet or sitting next to the chair where it could be easily pet; other youth expressed no significant interest in the dog. The clinician provided cues for the dog to approach or move away in accordance with the youth’s preferences. During situations where the youth appeared stressed, the clinician offered interaction with the dog as a coping skill alongside previously taught skills (e.g., relaxation), but did not otherwise introduce the dog into the activities of the sessions.
The dogs’ handlers visually observed all treatment sessions from behind a one-way mirror in an adjacent room to ensure the safety of the animals. Audio was turned off to protect the confidentiality of participants. Handlers were free to stop sessions at any point by knocking on the treatment room door if they were concerned for the dog’s welfare; only one such instance occurred. Five separate dogs participated in the trial, all of which were Labrador retrievers bred and trained to work as service dogs. When a youth was randomized to the TF-CBT+AAT condition, the assigned clinician scheduled the appointment with the caregiver at a predetermined time that a dog would be available and then notified the lead handler. The lead handler selected the specific dog/handler team that would be assigned for the duration of the youth’s participation in the trial. The assigned dog was considered an extension of the assigned clinician; if for any reason the dog was unable to attend (e.g., sickness) it was considered the same as the clinician being unavailable and the session was re-scheduled. The clinicians’ experiences and any noted challenges of integrating the dogs into the TF-CBT protocol were recorded on specially adapted fidelity checklists and discussed during bi-weekly consultation with the primary author. It should be noted that the primary author was not involved in the collection, management, or analysis of data.
Measures
Service Satisfaction Scale (SSS)
The SSS is a 5-item measure that assesses one’s satisfaction with services received (Athay & Bickman, 2012). Four of the items ask direct questions designed to quantitatively ascertain one’s perception of the services completed (e.g. “Did you get the kind of services you think you needed?”) and the respondent provides an answer using a 4-point scale ranging from 0 (“No, definitely not”) to 3 (“Yes, definitely”). The four items are summed to yield a total scale score ranging between 0 and 12. The youth self-report and caregiver-report versions of the SSS were administered at the post-treatment assessment. Internal consistency of both versions was not strong (Youth: Cronbach’s α = .63; Caregiver: α = .59).
UCLA PTSD Reaction Index for DSM-5
The UCLA (Pynoos & Steinberg, 2014) is a two-part self-report assessment measure. The first section is a trauma screen that asks whether the youth experienced various potentially traumatic events in a yes/no format. If multiple forms of trauma exposure are endorsed, the most concerning one as currently experienced by the youth is identified for answering questions in the second section. The index trauma identified in the pre-treatment assessment was used as the anchor for answering the second section on posttraumatic stress symptoms throughout the youth’s participation in treatment. In addition, this index trauma (i.e., physical abuse, sexual abuse, or witnessing inter-partner violence) was the focus of the trauma narrative construction during treatment. The second section is a 27-item measure assessing the youth’s experience of posttraumatic stress symptoms over the past month on a frequency scale ranging from 0 (Never) to 4 (Most Days). Responses are summed to compute a total scale score. Although previous research identified an optimal clinical cutoff of 35 for fully diagnostic PTSD cases, a score of 32 was used in the current study to identify sub-threshold cases of significant concern. The caregiver version was used as the primary outcome for the study while the youth self-report version was included as a secondary outcome. The caregiver version of the UCLA was selected as the primary measure because 6-year-old children were included in this trial and the validity of using the UCLA self-report version with children this young is unclear. Youth and caregiver versions were administered at each of the four assessment sessions. Internal consistency across all measure administrations was excellent for both caregiver-report (α = .92) and youth self-report (α = .90).
Strengths and Difficulties Questionnaire (SDQ)
The SDQ (Goodman, 1997) is a measure of youth emotional and behavioral concerns. The 25-item measure asks the caregiver to report whether each item is Not True (0), Somewhat True (1), or Certainly True (2) for the youth. This study utilized the Emotional Problems subscale assessing symptoms of anxiety and depression, and the Conduct Problems subscale assessing externalizing problems. Across each of the four assessment points, internal consistency for the Emotional Problems (α = .76) and Conduct Problems (α = .80) subscales was sufficient.
Moods and Feelings Questionnaire (MFQ)
The short version of the MFQ (Angold, Costello, Messer, Pickles, Winder, & Silver, 1995) is a youth self-report measure assessing the occurrence of depressive symptoms. Youth identify whether each of 13 items is Not True (0), Sometimes True (1), or True (2) for them in the past two weeks. Responses are summed to create a total score. The MFQ was completed at each of the assessments and internal consistency across administrations was acceptable (α = .86).
Screen for Child Anxiety Related Disorders (SCARED)
The SCARED (Birmaher, Brent, Chiappetta, Bridge, Monga, & Baugher, 1999) is a 41-item youth self-report measure assessing various forms of anxiety-related concerns. Youth are asked to report how true each statement is for them over the past 3 months: Not True or Hardly Ever True (0), Somewhat or Sometimes True (1), or Very Often or Very True (2). This trial utilized the total scale score computed by summing each of the individual items. The SCARED was administered at each of the four assessment points. Internal consistency of the total scale across administrations was excellent (α = .94).
Analytic Plan
Initial analyses examined the equivalency of the two treatment groups on demographic variables; Chi-squared tests or Fisher’s exact tests were used to examine categorical variables and independent t-tests were used to examine continuous variables, as appropriate. Evaluation of feasibility outcomes, such as recruitment, retention, dog-related treatment disruptions, and satisfaction with services were analyzed using descriptive, non-parametric statistics, and t-tests, as appropriate. Intent-to-treat analyses were used for all statistical analyses examining change in outcomes over time, making use of all available data. Missing data for longitudinal outcome measures occurred due to attrition. Likelihood-based approaches can be employed for valid inferences under the assumption of missing at random (MAR), which is commonly and reasonably assumed for statistical inference if participants drop out of the study or are lost to follow-up (Groenwold, Donders, Roes, Harrell, & Moons, 2012; Schafer & Graham, 2002). Consequently, maximum likelihood estimation was used when computing all models.
For each longitudinal outcome, multilevel models were employed to evaluate group differences and compare temporal trajectories. Given that none of the demographic variables differed significantly between the groups (see below), no covariates were entered into the models. The tested models can be specified as follows:
where for the ith subject, yij was the outcome measure at time j (j = 1,2,3,4), the primary variables of interest included Groupi for the group indicator (0 = TF-CBT; 1 = TF-CBT+AAT), Timei as the square root of the follow-up measurement time (in weeks), and their interaction terms. The primary effects of interest were quantified by β1 corresponding to the mean outcome difference between the groups in pre-assessment, β2 for the slope estimate of the TF-CBT group, β2+β3 for the slope estimate of the TF-CBT+AAT group, thus β3 for the slope difference between two groups. Furthermore, the random intercept γi was used to capture the correlation among the repeated measures within-subject, which was assumed to follow a normal distribution . The residual term εij also followed a normal distribution . Note that, the random intercept γi was independent with the residual term εij, thus there was an exchangeable correlation for repeated measures from the same subject with the correlation coefficient as . The restricted maximum likelihood approach was used for estimation of the random effect terms, and given the estimate , the parameter estimates of fixed effects were obtained by the generalized least squares approach. Note that the p-values were computed based on t-statistics using Satterthwaite’s method for denominator degrees of freedom (Kuznetsova et al., 2017). All hypothesis tests were two-sided with a significance level of 0.05. Data were analyzed using R software version 3.6.3 (R Core Team, 2019).
Results
Demographic Analyses
Demographic characteristics of the two groups are shown in Table 1. The randomization procedure appeared effective as the two groups did not differ on gender composition (χ2(1) = .061, p = .81) and the groups were comparable on age (TF-CBT: M = 11.56, SD = 3.35; TF-CBT+AAT: M = 12.0, SD = 2.89; t(31) = .40, p =.69). In addition, racial (χ2(2) = .74, p = .69) and ethnic (χ2(1) = .27, p = .61) composition was similar across groups. There were no noted differences between the groups on caregiver demographic factors. The index trauma was sexual abuse for 63.6% of the sample; frequency counts showed some potential differences with 50% of the TF-CBT group and 76% of the TF-CBT+AAT reporting sexual abuse as the index trauma (χ2(1) = 2.50, p = .114). Although this difference was not statistically significant, we nontheless examined whether sexual abuse experience moderated outcome in the analyzed models. None of the models demonstrated significant differences from base models and are not discussed further.
Feasibility Outcomes
Recruitment
As shown in Figure 1, of the 59 potential participants who met standard inclusion criteria for a clinical trial of TF-CBT, 5 (8.5%) were excluded because of the additional criteria related to the inclusion of the dogs. Of the 54 eligible participants, a relatively large percentage (39%) declined to participate. The participating dogs were scheduled in advance and participants were informed up front of when appointments might be scheduled. This did not fit with the schedules of many caregivers and was cited as a factor for declining in the majority of cases.
Retention
Two participants in each condition were actively engaged in the study and withdrawn when research activities were suspended due to the COVID-19 pandemic. Of the remaining participants, three failed to complete treatment within the TF-CBT group (21.4%) while only one within the TF-CBT+AAT group failed to complete all sessions (6.7%), a non-significant difference (χ2(1) = 1.33, p = .249). Both groups had one participant withdrawn by the study team due to inpatient hospitalization; this left two participants in the TF-CBT group who voluntarily chose to withdraw from the study while no participants in the TF-CBT+AAT group chose to withdraw, an interesting observation though not statistically significant (Fisher’s Exact = .22).
Treatment disruption
The number of treatment disrupting events that occurred and were attributable to the presence of the dogs were recorded on fidelity checklists (e.g., barking, whining). Of the 157 completed treatment sessions that included a dog, clinicians identified a treatment disrupting event occurring in 10 of them (6.4%). Six of those events were caused by a single dog who often whined and panted after being separated from his handler. These six events all occurred in the context of the treatment of a single participant, as the dog was removed from further involvement after the case was completed. Removing the 12 sessions involving this dog and his six treatment disrupting events left only four of 145 sessions with such disruptions (2.8%).
Satisfaction with Treatment
Caregiver satisfaction with treatment was high among both groups (TF-CBT: M = 11.82, SD = .60; TF-CBT+AAT: M = 11.77, SD = .60) and the difference between them was not significant (t(22) = .20, p = .844). Similarly, youth in both groups generally were pleased with services (TF-CBT: M = 10.82, SD = 1.33; TF-CBT+AAT: M = 10.92, SD = 1.75) and the difference between the groups was not significant (t(22) = −.16, p = .872).
Clinical Outcomes
PTSD Symptom Severity
No significant differences were seen between the groups at the pre-treatment assessment on either caregiver or youth-reported PTSD symptoms (see Table 2). With regards to the temporal trend, both groups exhibited significant improvements in caregiver-reported PTS (TF-CBT: β(SE) = −4.15 (.68), t(82.93) = −6.06, p < .001; TF-CBT+AAT: β(SE) = −3.25 (.68), t(82.17) = −4.81, p < .001). However, the interaction term was not significant (β(SE) = .90 (.96), t(82.56) = .94, p = .351), suggesting the rate of decline did not differ significantly across groups. As a matter of clinical significance, it is noteworthy that the TF-CBT group’s mean score at post-treatment was well below the clinical cut off score, while this was not true for the TF-CBT+AAT group.
Table 2:
Means over time.
| Outcome Measure | Condition | |
|---|---|---|
| TF-CBT M (SD) |
TF-CBT+AAT M (SD) |
|
| UCLA PTSD Index (Caregiver-report): | ||
| Time 1 (Pre-Assessment) | 46.25 (11.34) | 52.29 (12.25) |
| Time 2 (Session 5) | 37.85 (19.14) | 40.4 (14.73) |
| Time 3 (Session 9) | 24.09 (15.67) | 39.64 (11.58) |
| Time 4 (Post-Assessment) | 22.64 (16.43) | 35.85 (14.81) |
| UCLA PTSD Index (Self-report): | ||
| Time 1 | 44.63 (12.38) | 39.5 (18.44) |
| Time 2 | 39.21 (15.9) | 39.6 (18.08) |
| Time 3 | 32.64 (20.18) | 35.21 (18.03) |
| Time 4 | 28.09 (24.09) | 38.38 (12.74) |
| SDQ-Emotional Problems: | ||
| Time 1 | 6.5 (2.58) | 7.65 (2.0) |
| Time 2 | 5.5 (2.59) | 7.13 (2.1) |
| Time 3 | 4.73 (2.53) | 6.14 (2.57) |
| Time 4 | 4.0 (3.0) | 5.08 (1.85) |
| SDQ-Conduct Problems: | ||
| Time 1 | 3.06 (2.91) | 4.12 (2.78) |
| Time 2 | 2.43 (2.5) | 2.87 (2.13) |
| Time 3 | 2.18 (2.04) | 2.93 (2.53) |
| Time 4 | 2.18 (2.04) | 3.15 (2.7) |
| MFQ: | ||
| Time 1 | 9.13 (5.6) | 8.88 (4.69) |
| Time 2 | 9.07 (5.3) | 9.47 (6.57) |
| Time 3 | 8.46 (8.26) | 8.07 (5.43) |
| Time 4 | 5.91 (5.54) | 8.85 (6.12) |
| SCARED: | ||
| Time 1 | 39.64 (18.04) | 35.47 (14.45) |
| Time 2 | 38.57 (18.9) | 37.07 (16.52) |
| Time 3 | 32.0 (20.72) | 29.0 (19.95) |
| Time 4 | 25.45 (19.17) | 31.62 (14.94) |
Note: SDQ = Strengths and Difficulties Questionnaire; MFQ = Moods and Feelings Questionnaire; SCARED = Screen for Child Anxiety-related Disorders.
Youth self-reported PTS outcomes provided interesting results. Children within the TF-CBT group reported significant improvement over time (β(SE) = −3.43 (.73), t(79.57) = −4.72, p < .001) while the children in the TF-CBT+AAT group did not report such improvements (β(SE) = −1.42 (0.74), t(79.61) = −1.93, p = .057). The interaction term (β(SE) = 2.01 (1.03), t(79.59) = 1.94, p = .056) approached the customary level of statistical significance. Given the preliminary nature of this trial, the decision was made to graphically probe this interaction to determine the shape of the data structure. As shown in Figure 2, the TF-CBT group exhibited a decline that appeared to exceed the rate reported by youth in the TF-CBT+AAT group, suggesting the possibility that the inclusion of AAT exerted an suppressing effect on treatment gains.
Figure 2:
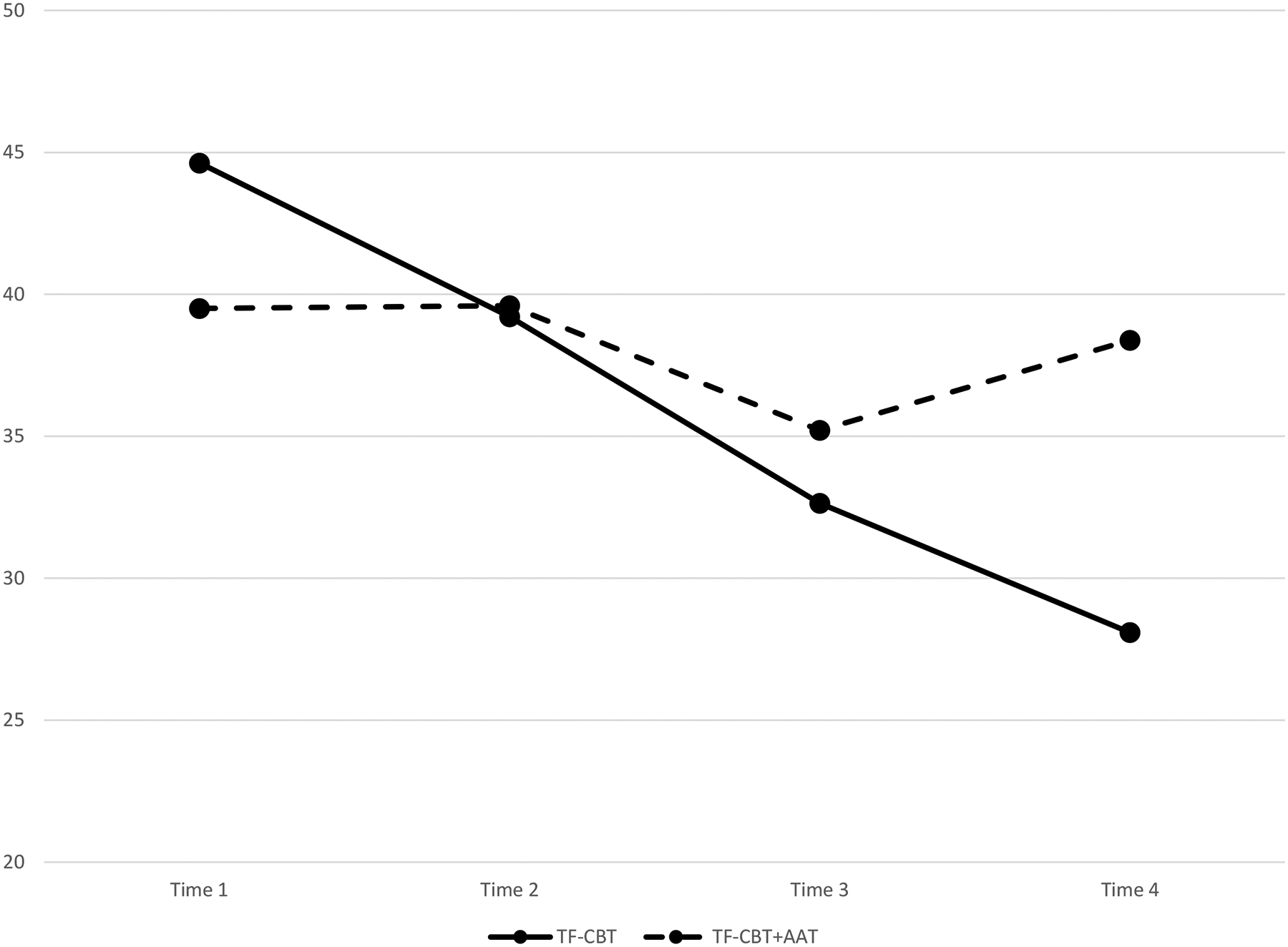
Change in self-reported posttraumatic stress over time
Internalizing Concerns
No significant differences were present at the beginning of treatment for any measurements of internalizing concerns. Over the course of treatment, both groups experienced significant declines in caregiver-reported internalizing concerns on the SDQ-Emotional Problems subscale (TF-CBT: β(SE) = −.37 (0.12), t(86.23) = −2.97, p = .003; TF-CBT+AAT: β(SE) = −.49 (0.12), t(84.68) = −3.93, p < .001), but the rate of improvement did not differ between the groups (β(SE) = −.11 (.18), t(85.47) = −.66, p = .514). On the MFQ, youth in both groups failed to note changes in depressive symptoms (TF-CBT: β(SE) = −.43 (.30), t(86.75) = −1.41, p = .16; TF-CBT+AAT: β(SE) = −.17 (.30), t(85.20) = −.57, p = .57) and no between groups differences were noted (β(SE) = .26 (.43), t(85.99) = .6, p = .55). However, youth in the TF-CBT group did report significant improvements for anxiety on the SCARED (β(SE) = −2.0 (.92), t(83.42) = −2.18, p = .032). The TF-CBT+AAT group did not report significant improvements for anxiety (β(SE) = −1.61 (.85), t(79.97) = −1.89, p = .063), although the interaction term was not significant (β(SE) = .39 (1.25), t(81.82) = .31, p = .758), suggesting that the rate of improvement over time did not differ significantly between the two treatment groups.
Externalizing Concerns
Caregiver-reported externalizing concerns on the SDQ-Conduct Problems scale were similar across groups at the pre-treatment assessment. Over the course of treatment, both groups demonstrated significant behavioral improvements (TF-CBT: β(SE) = −.21 (.10), t(79.69) = −2.15, p = .035; TF-CBT+AAT: β(SE) = −.23 (.10), t(79.34) = −2.37, p = .02). The rate of decline in behavioral problems was not significantly different across the two treatment groups (β(SE) = −.02 (.14), t(79.52) = −.14, p = .892).
Discussion
The current study investigated the feasibility and preliminary effectiveness of integrating AAT into standard TF-CBT for the treatment of abused youth presenting with elevated PTSD symptoms. Results revealed improvements in caregiver-reported PTSD symptoms, internalizing concerns, and externalizing problems among both groups: standard TF-CBT and TF-CBT+AAT. This was expected and is consistent with prior research that has demonstrated TF-CBT to be an effective intervention for reducing psychiatric symptoms in youth who have experienced various forms of trauma, including child abuse (Cary & McMillen, 2012; Cohen, Deblinger, Mannarino, & Steer, 2004; Cohen, Mannarino, & Iyengar, 2011).
Of particular interest are findings based on youth self-report measures, where improvements in posttraumatic stress symptoms appeared contingent on group membership. Statistically significant improvement in symptoms over time was evident for the TF-CBT group, but not the TF-CBT + AAT group. The interaction term approached the traditional benchmark for statistical significance (p = .056), suggesting that the data were trending toward group differences in the rate of improvement, with the standard TF-CBT group outpacing the TF-CBT+AAT group. With a slightly larger sample size, it is likely that this interaction effect would have reached the level of statistical significance. Regardless, it is notable that the youth in the TF-CBT+AAT group did not report significant improvement in posttraumatic stress symptoms despite a robust evidence base that TF-CBT does yield significant declines in these symptoms.
The primary aim of this study was to examine whether integrating AAT into TF-CBT was feasible and might enhance treatment effectiveness for children exposed to maltreatment. This trial identified a number of feasibility challenges related to the incorporation of AAT that may ultimately make this treatment approach a poor choice for implementation and scale in outpatient clinics serving the child maltreatment population. In addition, based on the results of this randomized trial, integrating AAT into TF-CBT does not appear to enhance the effectiveness of TF-CBT, and may in fact impede the effectiveness of TF-CBT for certain outcomes. Prior research suggesting that AAT may yield therapeutic benefit for abused youth (Balluerka et al., 2015; Dietz et al., 2012; Parish-Plass, 2008; Reichart et al., 2016; Tedeschi et al., 2015) has been critiqued on methodological grounds due to small sample sizes, poor metrics, absent or confounded control groups, and lack of randomization to conditions (e.g., Anestis et al., 2014; Nimer & Lundahl, 2007; O’Haire et al., 2015). With the exception of a small sample size, these concerns were directly addressed by the current study through the use of reliable and valid measures of child psychiatric symptoms, and a robust randomized design that included an active control group receiving the same treatment as the group that received adjunctive AAT.
The hallmark of exposure-based treatments, such as TF-CBT, is the inclusion of exposure activities that directly extinguish the avoidance of feared stimuli. Thus, it is not surprising that clinicians would want to identify methods that may help to reduce youth’s distress during exposure exercises and many believe the presence of animals may serve this purpose (Reichert et al., 2016; Tedeschi et al., 2015). Whereas the clinicians in the current study observed some instances where the presence of the animal appeared to assist youth with coping, they more frequently identified concerns that the animal actually served as an additional method of avoidance. Some of the youth would direct their focus to interacting with the dog instead of engaging in exposure activities, particularly during more uncomfortable aspects of constructing the trauma narrative. When this occurred, clinicians found it challenging to re-engage the youth in the exposure exercises. In this sense, including a dog in the therapy room may reinforce avoidance behaviors for certain youth, making therapeutic gains for PTSD symptoms less likely. Such a mechanism would explain the findings of the current study suggesting the potential for AAT to attenuate treatment gains on posttraumatic stress typically observed through TF-CBT.
The current study had several strengths. It is the first known RCT of AAT for the treatment of abused youth that included an active control group, thus allowing for a direct test of its feasibility and incremental utility in a community practice setting. The use of repeated measures and assessments allowed for the construction of slope estimates to examine the rate of change in symptoms over time. Assessments involved a wide range of psychiatric outcomes, including posttraumatic stress symptoms, internalizing concerns, and externalizing problems. Additionally, assessment of symptoms included both child- and parent-report, which improved the validity of findings and revealed important differences in perceived symptomatology, and those collecting and analyzing the data were blinded to participant condition. The sample was racially and ethnically diverse and caregivers varied on a number of demographic factors (e.g., marital status, level of education, and estimated family annual income), which helps to improve generalizability of the findings. Furthermore, the randomization to condition appeared successful, as the two treatment groups did not differ on any of the sociodemographic characteristics examined or baseline level of symptomatology.
The current study is not without limitations, however. Most notably, a randomized feasibility trial design was adopted, which necessitated a small sample to demonstrate preliminary effects. While feasibility metrics were successfully obtained, the small sample size decreased statistical power to detect potential interaction effects that may have limited the detection of differences between groups. However, the use of repeated measures over multiple time points helped to increase statistical power and partially alleviate this concern. Part of the reason for a smaller than expected sample size was that the rate of eligible participants who declined involvement in the study was unexpectedly high (39%). This was largely due to limitations in scheduling to accommodate the presence of the animals, which was not anticipated to present such a barrier. Due to child abuse reporting laws in the state of Pennsylvania, our study also included a disproportionately large sample of participants who had an index trauma of sexual abuse when compared to national prevalence rates for different child abuse subtypes. Although sexual abuse is the trauma most often identified in studies of TF-CBT, generalizability of study findings to the experience of other forms of maltreatment may be limited. However, preliminary analyses revealed that sexual abuse did not moderate any of our study outcomes. It should also be noted that much of the AAT literature discusses the active and deliberate integration of animals into techniques throughout treatment delivery. That was not the case here and it is unclear whether a more animal-focused approach would have yielded greater benefits. In addition, many practicing clinicians utilizing AAT own and train their own animals and, therefore, the clinician is also the animal’s handler. Although there were no significant concerns noted by either the clinicians or handlers with the dogs’ responses to clinicians’ cues, the current study cannot definitively state whether this factor impacted outcome.
Given the limitations of the extant research on integrating AAT into treatment with abused youth, there are a number of possibilities for future research. A meta-analysis of 49 studies investigating the use of AAT for a broad range of presenting problems noted there are enough quantitative and qualitative studies in this area that research should move toward rigorous study designs as opposed to anecdotal reports and case studies (Nimer & Lundahl, 2007). A systematic review of ten studies examining the use of animals in treatment for trauma noted that, although there was support for reduced depression, PTSD, and anxiety symptoms, half of the studies did not include a comparison condition, only one used random assignment, and none used fidelity checklists or treatment manuals (O’Haire et al., 2015), which hinders conclusions regarding whether AAT can be beneficial for those needing treatment. Indeed, our study addressed a number of these shortcomings and results showed that AAT did not demonstrate evidence of added benefit beyond standard TF-CBT. Further research and replication is necessary to draw definitive conclusions regarding the incremental effectiveness of AAT being added to an established treatment. Similar to the current investigation, designs that utilize an active control group and isolate the inclusion of the AAT component as the manipulated variable are imperative.
Future RCTs could directly address issues of feasibility that were present in the current study. For example, scheduling was limited due to the need to collaborate with a local organization that provided the dogs and, consequently, a number of potential participants declined to enroll in the tiral. Institutions or organizations that have therapy animals onsite may be able to achieve a lower decline rate. Another option is to conduct a clinical trial with participants who are partnered with their own service dogs, however, this would introduce greater variability and potentially reduce methodological rigor.
As suggested by prior reviews (Nimer & Lundahl, 2007; O’Haire et al., 2015), future research should examine the conditions under which the inclusion of a service animal may be most helpful. One meta-analysis examined potential moderators of AAT response and did not find evidence that characteristics of participants produced differential outcomes (Nimer & Lundahl, 2007). However, young children appeared to benefit consistently from AAT, as evidenced by improvement across a range of outcome variables, compared to older age groups (e.g., adolescents and adults). In the current study, clinicians noted that the presence of the dogs appeared to be helpful for some and a larger sample would allow for a more in-depth investigation that distinguishes the profiles of individuals most likely to benefit. However, given the lack of evidence for enhanced treatment effectiveness based on the current study’s findings, and serious limitations among prior studies, it does not appear that a large-scale clinical trial of AAT as an adjunct for TF-CBT is warranted at this time.
Given the observation that a meta-analytic review was unable to offer specific recommendations regarding the conditions for which AAT may be most beneficial (Nimer & Lundahl, 2007) and the lack of evidence for feasibility and incremental effectiveness observed in this trial, we cannot recommend the inclusion of service animals into TF-CBT for the treatment of abused youth with PTSD. Instead, we recommend the administration of TF-CBT alone given its wealth of prior evidence (Dorsey et al., 2017) and performance in the current trial. Moreover, exposure is and has been used throughout decades of clinical trial research on TF-CBT (Cohen et al., 2000), suggesting that exposure can be delivered safely and effectively with the child abuse population (e.g. Deblinger et al., 2011). Although we do understand the interest of some clinicians in utilizing AAT to alleviate potential stress related to exposure-based techniques, we find it more advisable that clinicians with concerns about exposure seek out additional evidence and training on the ways to effectively deliver this widely used technique (Dorsey et al., 2017). If one does choose to implement AAT, it should not be implemented as a standalone treatment and certainly not as an alternative to an established evidence-based treatment, such as TF-CBT. Furthermore, if clinicians do opt to use AAT as an adjunctive treatment, it is important to be aware that the presence of an animal could potentially hinder treatment progress.
Acknowledgments
The project described in this paper was funded by the Eunice Kennedy Shriver National Institute for Child Health and Human Development (NICHD) grant R21HD091887 to the primary author (BA). In addition, Drs. Allen and Shenk were supported by NICHD grant P50HD089922. The views expressed in this paper are solely those of the authors and do not necessarily reflect the views of NICHD or the National Institutes of Health (NIH). The authors wish to thank the trial’s clinicians, Amy Slenker, LCSW, and Ryan Hagarman, LCSW, as well as all the youth and families that participated in this trial.
References
- Allen B, & Crosby JW (2014). Treatment beliefs and techniques of clinicians serving child maltreatment survivors. Child Maltreatment, 19, 49–60. [DOI] [PubMed] [Google Scholar]
- Allen B, Gharagozloo L, & Johnson JC (2012). Clinician knowledge and utilization of empirically-supported treatments for maltreated children. Child Maltreatment, 17, 11–21. [DOI] [PubMed] [Google Scholar]
- Allen B, & Hoskowitz NA (2017). Structured trauma-focused CBT and unstructured play/experiential techniques in the treatment of sexually abused children: A field study with practicing clinicians. Child Maltreatment, 22, 112–120. [DOI] [PubMed] [Google Scholar]
- Allen B, & Johnson JC (2012). Utilization and implementation of Trauma-Focused Cognitive-Behavioral Therapy for the treatment of maltreated children. Child Maltreatment, 17, 80–85. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Anestis MD, Anestis JC, Zawilinski LL, Hopkins TA, & Lilienfeld SO (2014). Equine-related treatments for mental disorders lack empirical support: A systematic review of empirical investigations. Journal of Clinical Psychology, 70, 1115–1132. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Messer SC, Pickles A, Winder F, & Silver D (1995). The development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research, 5, 237–249. [Google Scholar]
- Athay MM, & Bickman L (2012). Development and psychometric evaluation of the youth and caregiver Service Satisfaction Scale. Administration and Policy in Mental Health and Mental Health Services Research, 39, 71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balluerka N, Muela A, Amiano N, & Caldentey MA (2015). Promoting psychosocial adaptation of youths in residential care through animal-assisted psychotherapy. Child Abuse and Neglect, 50, 193–205. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, & Baugher M (1999). Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 1230–1236. [DOI] [PubMed] [Google Scholar]
- Cary CE, & McMillen JC (2012). The data behind the dissemination: A systematic review of trauma-focused cognitive-behavioral therapy for use with children and youth. Children and Youth Services Review, 34, 748–757. [Google Scholar]
- Chandler CK (2005). Animal-assisted therapy in counseling. New York: Routledge. [Google Scholar]
- Cohen JA, Deblinger E, Mannarino AP, & Steer RA (2004). A multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms. Journal of the American Academy of Child & Adolescent Psychiatry, 43, 393–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP, Berliner L, & Deblinger E (2000). Trauma-focused cognitive behavioral therapy for children and adolescents: An empirical update. Journal of Interpersonal Violence, 15, 1202–1223. [Google Scholar]
- Cohen JA, Mannarino AP, & Deblinger E (2017). Treating trauma and traumatic grief in children and adolescents (2nd ed.). New York: Guilford Press. [Google Scholar]
- Cohen JA, Mannarino AP, & Iyengar S (2011). Community treatment of posttraumatic stress disorder for children exposed to intimate partner violence: A randomized controlled trial. Archives of Pediatrics and Adolescent Medicine, 165, 16–21 [DOI] [PubMed] [Google Scholar]
- Deblinger E, Mannarino AP, Cohen JA, Runyon MK, & Steer RA (2011). Trauma-focused cognitive-behavioral therapy for children: Impact of the trauma narrative and treatment length. Depression and Anxiety, 28, 67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietz TJ, Davis D, & Pennings J (2012). Evaluating animal-assisted therapy in group treatment for child sexual abuse. Journal of Child Sexual Abuse, 21, 665–683. [DOI] [PubMed] [Google Scholar]
- Dittmann I, & Jensen TK (2014). Giving a voice to traumatized youth-Experiences with trauma-focused cognitive-behavioral therapy. Child Abuse & Neglect, 38, 1221–1230. [DOI] [PubMed] [Google Scholar]
- Dorsey S, McLaughlin KA, Kerns SEU, Harrison JP, Lambert HK, Briggs EC, & Amaya-Jackson L (2017). Evidence base update for psychosocial treatments for children and adolescents exposed to traumatic events. Journal of Clinical Child and Adolescent Psychology, 46, 303–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito L, McCune S, Griffin JA, & Maholmes V (2011). Directions in human-animal interaction research: Child development, health, and therapeutic interventions. Child Development Perspectives, 5, 205–211. [Google Scholar]
- Famularo R, Fenton T, Augustyn M, & Zuckerman B (1996). Persistence of pediatric posttraumatic stress disorder after 2 years. Child Abuse & Neglect, 20, 1245–1248. [DOI] [PubMed] [Google Scholar]
- Finkelhor D (2008). Childhood victimization: Violence, crime, and abuse in the lives of young people. New York: Oxford University Press. [Google Scholar]
- Gillies D, Taylor F, Gray C, O’Brien L, & D’Abrew N (2012). Psychological therapies for the treatment of post-traumatic stress disorder in children and adolescents. Cochrane Database of Systematic Reviews, 2012 (12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman R (1997). The Strengths and Difficulties Questionnaire: A research note. Journal of Child Psychology and Psychiatry, 38, 581–586. [DOI] [PubMed] [Google Scholar]
- Groenwold RHH, Donders ART, Roes KCB, Harrell FE, & Moons KGM (2012). Dealing with missing outcome data in randomized trials and observational studies. American Journal of Epidemiology, 175, 210–217 [DOI] [PubMed] [Google Scholar]
- Kaufman AS, & Kaufman NL (2004). Kaufman Brief Intelligence Test (2nd ed.). Bloomington, MN: Pearson. [Google Scholar]
- Krause-Parello CA, & Gulick EE (2015). Forensic interviews for child sexual abuse allegations: An investigation into the effects of animal-assisted intervention on stress biomarkers. Journal of Child Sexual Abuse, 24, 873–886. [DOI] [PubMed] [Google Scholar]
- Kuznetsova A, Brockhoff PB, & Christensen RHB (2017) lmerTest Package: Tests in linear mixed effects models. Journal of Statistical Software, 82, 1–26. [Google Scholar]
- Lefkowitz C, Prout M, Bleiberg J, Paharia I, & Debiak D (2005). Animal-assisted prolonged exposure: A treatment for survivors of sexual assault suffering posttraumatic stress disorder. Society & Animals, 13, 275–296. [Google Scholar]
- Nimer J, & Lundahl B (2007). Animal-assisted therapy: A meta-analysis. Anthrozoös, 20, 225–238. [Google Scholar]
- O’Haire ME, Guerin, & Kirkham AC (2015). Animal assisted interventions for trauma: A systematic literature review. Frontiers in Psychology, 6, 1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parish-Plass N (2008). Animal-assisted therapy with children suffering from insecure attachment due to abuse and neglect: A method to lower the risk of intergenerational transmission of abuse? Clinical Child Psychology and Psychiatry, 13, 7–30. [DOI] [PubMed] [Google Scholar]
- Pemberton JR, Conners-Burrow NA, Sigel BA, Sievers CM, Stokes LD, & Kramer TL (2017). Factors associated with clinician participation in TF-CBT post-workshop training components. Administration and Policy in Mental Health and Mental Health Services Research, 44, 524–533. [DOI] [PubMed] [Google Scholar]
- Pynoos RS, & Steinberg AM (2014). The UCLA PTSD Reaction Index for the DSM-5. Los Angeles: Behavioral Health Innovations. [Google Scholar]
- R Core Team. (2019). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. [Google Scholar]
- Reichert E, Bermel L, & Sori CF (2016). Animal-assisted therapy for sexually abused children. In Sori CF, Hecker LL, & Bachenberg ME (Eds.), The therapist’s notebook for children and adolescents: Homework, handouts, and activities for use in psychotherapy (2nd ed.; pp. 125–130). New York: Routledge. [Google Scholar]
- Saunders BE, Berliner L, & Hanson R (2004). Child physical and sexual abuse: Guidelines for treatment (final report: January 15, 2004). Charleston, SC: National Crime Victims Research and Treatment Center. [Google Scholar]
- Schaefer JL, & Graham JW (2002). Missing data: Our view of the state of the art. Psychological Methods, 7, 147–177. [PubMed] [Google Scholar]
- Stoltenborgh M, Bakermans-Kranenburg MJ, Alink LRA, & van IJzendoorn MH (2015). The prevalence of child maltreatment across the globe: Review of a series of meta-analyses. Child Abuse Review, 24, 37–50. [Google Scholar]
- Tedeschi P, Sisa ML, Olmert MD, Parish-Plass N, & Yount R (2015). Treating human trauma with the help of animals: Trauma informed intervention for child maltreatment and adult posttraumatic stress. In Fine AH (Ed.), Handbook on animal-assisted therapy: Foundations and guidelines for animal-assisted interventions (4th ed.; pp. 305–319). San Diego, CA: Elsevier Academic Press. [Google Scholar]


