Abstract
Background:
Antenatal fetal surveillance is a field of increasing importance in modern obstetrics. It is based on fetal heart rate monitoring using nonstress test and contraction stress test, ultrasound biometry and amniotic fluid assessment, Doppler blood flow studies of fetal and uteroplacental circulation, and an evaluation of biophysical fetal parameters. The combination of these methods leads to improvements in fetal morbidity and mortality.
Aim:
The present study aimed to assess the sensitivity, specificity, and positive and negative predictive values of umbilical artery (UA) systolic/diastolic (S/D) ratio, and amniotic fluid index (AFI) in term pregnancies for the prediction of perinatal outcome and their relation with perinatal outcome.
Methods:
This study was conducted at a tertiary care hospital on 100 pregnant women where all the term singleton pregnancies (37–42 weeks) admitted in maternity were subjected to color Doppler for UA S/D ratio assessment and AFI estimation. Further, management of patients was done according to color Doppler findings and their relation with perinatal outcome.
Results:
Out of 100 pregnant women, 68% had AFI >8 (normal), while 32% of women had AFI <8 (abnormal), with the mean AFI being 9.39 ± 2.55 cm, whereas70% had S/D ratio <3 (normal) and 30% of women had S/D ratio >3 (abnormal), with the mean S/D ratio of 2.61 ± 0.450. UA S/D ratio had better performance values (i.e., sensitivity, specificity, and positive and negative predictive value) than AFI in predicting adverse perinatal outcomes.
Conclusion:
AFI and UA S/D ratio are important for predicting low appearance, pulse, grimace, activity, and respiration score, meconium, respiratory complications, and perinatal mortality in high as well as low-risk pregnancy cases. However, UA S/D ratio is a better predictor of perinatal outcome in high-risk pregnancies.
Keywords: Amniotic fluid index, appearance, activity, color doppler, grimace, meconium, negative predictive value, pulse, and respiration, perinatal outcome, positive predictive value, sensitivity, specificity, umbilical artery systolic/diastolic ratio
Introduction
Antepartum fetal surveillance is the cornerstone of management in pregnancy.[1] It is done primarily to reduce the incidence of adverse fetal outcomes. It minimizes morbidity by optimizing the timing of delivery. Fetus genuinely at risk of chronic hypoxia is identified and unnecessary interventions are avoided. However, fetal surveillance acts as a diagnostic modality to detect the influence of maternal, placental, and fetal factors on the fetus. The timely detection of morbid changes in the fetal status followed by adequate interventions to avoid death or disability is one of the most important objectives of prenatal care.[2]
Tests now commonly done for antepartum fetal surveillance are nonstress test (NST), amniotic fluid index (AFI), biophysical profile, Doppler study of umbilical artery (UA), and middle cerebral artery (MCA).[3,4,5,6] However, AFI and UA Doppler velocimetry both form an essential part of the antenatal surveillance in the assessment of fetal well-being. UA Doppler is a powerful tool that allows the obstetrician to follow a sequence of fetal hemodynamic events that happen in response to placental insufficiency.[7] However, several studies have reported higher sensitivities and specificities for UA Doppler ratio for prediction of fetal prognosis.[3,4,5,6]
Amniotic fluid is the product of complex and dynamic fetal and placental physiologic processes. Disruption of the fine balance may result in overproduction or underproduction of fluid. Liquor adequacy often reflects the fetal status. Oligohydramnios is associated with increased perinatal loss. Furthermore, other studies indicate that UA velocimetry is a predictor of adverse outcomes in pregnancies complicated by oligohydramnios.[8,9] Thus, arterial Doppler velocimetry measurement may be useful in predicting adverse pregnancy outcomes adjunct to other antenatal surveillance tests, especially the AFI. Therefore, the present study was done to evaluate the comparative assessment of UA ratio and AFI in predicting adverse perinatal outcomes.
Materials and Methods
After obtaining Institutional Ethical Committee approval (Reference No. GU/HREC/EC/2015/1053) and written informed consent from all the patients, this prospective 1-year observational study was conducted on 100 pregnant women who had term singleton pregnancy (37-42 weeks), low- as well as high-risk pregnancies, and were admitted in the department of obstetrics and gynecology of a tertiary care hospital. The sample size was calculated by considering sensitivity (Sn) – 66.6% for appearance, pulse, grimace, activity, and respiration (APGAR) score for AFI criteria as per the reference article,[1] precision [D] – 10%, power – 80%, confidence interval – 95%, and nonresponse rate – 10% by using the formula N = Z2 × Sn (1–Sn)/D2. Calculated N was 89; by adding nonresponse rate of 10%, the final calculated sample size was 97. Considering this, a sample size of 100 was considered for the study. The study was started in January 2015 up till the completion of the sample size. Patients with multiple pregnancies, preterm pregnancies, postterm pregnancies, and pregnancies with congenital malformations were excluded from the study.
A detailed history of patients and demographic data such as age and rural and urban settings were noted. Obstetrical data which included obstetrical history, obstetrical risk factors, date of last menstrual period (LMP), expected date of delivery, and period of gestation (according to LMP and ultrasonographically) were recorded. All women were subjected to color Doppler (UA systolic/diastolic [S/D] ratio) and AFI measurement. On ultrasound examination, fetal and placental positions were recorded. Four-quadrant assessment of amniotic fluid according to guidelines described by Phelan et al.[10] was made. The deepest pocket in each quadrant was measured by calipers contained within the ultrasound unit and recorded. The sum of these measurements yielded AFI.
The women were advised either induction or expectant treatment for the onset of spontaneous labor pains or elective cesarean section depending on the clinical assessment, AFI, color Doppler (S/D Ratio of UA), and any other high-risk factors. Mode of delivery and indications of cesarean delivery were noted. After the delivery, perinatal outcome was assessed by evaluating the gestational age, birth weight, meconium staining of amniotic fluid, APGAR score at 5 min, respiratory distress syndrome, admission to neonatal intensive care unit (NICU), and perinatal mortality. Resuscitative measures were required such as oxygen, bag and mask ventilation, endotracheal intubation, phototherapy, number of days in NICU, and breastfeed initiation (time and duration). Details of obstetrical ultrasonography and fetal color Doppler, i.e., S/D ratio and AFI and relation of these indices with the perinatal outcome, were noted. Assessment of sensitivity, specificity, and positive and negative predictive values was done.
Statistical analysis was performed using Chi-square Test. The significance was graded as P < 0.05–0.01 considered statistically significant, P < 0.01 highly significant, and <0.001 very highly significant.
Results
A total of 100 term singleton pregnant patients were recruited in the study. Maximum number of women belonged to the age group of 25–30 years (66%), urban background (59%), booked (54%), multigravida (58%), and most of the women (64%) underwent cesarean section, as shown in Table 1. The mean age of women was 27.07 ± 3.75 years.
Table 1.
Demographic and obstetric characteristics of women
| Parameters | Number of patients, n (%) |
|---|---|
| Age (years) | |
| <20 | 0 |
| 20–<25 | 23 (23) |
| 25–<30 | 66 (66) |
| >30 | 11 (11) |
| Rural/urban | |
| Rural | 41 (41) |
| Urban | 59 (59) |
| Booked/un-booked | |
| Booked | 54 (54) |
| Un-booked | 46 (46) |
| Gravida status | |
| Primigravida | 42 (42) |
| Multigravida | 58 (58) |
| Mode of delivery | |
| Vaginal delivery | 36 (36) |
| Elective cesarean section | 47 (47) |
| Emergency cesarean section | 17 (17) |
Various high-risk factors were present in pregnant women [Figure 1]. The previous history of cesarean section was the most common indication for cesarean section in the current study, followed by fetal distress.
Figure 1.
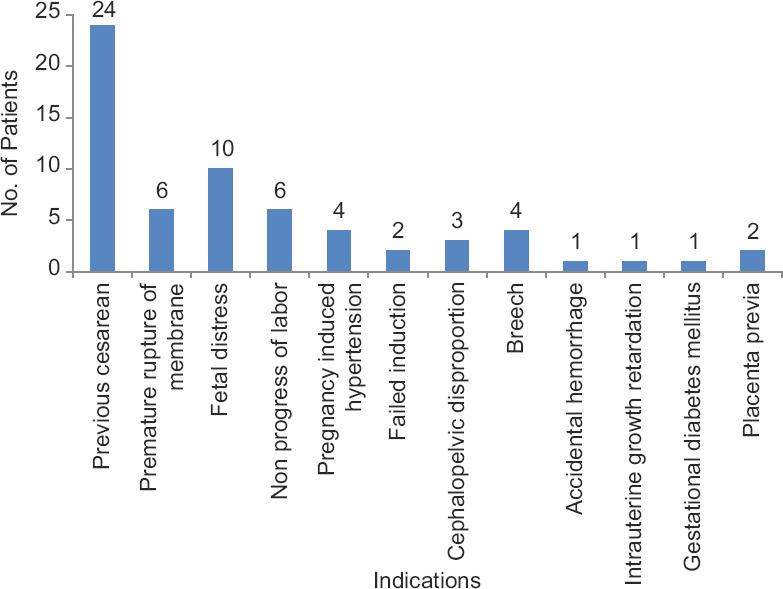
Indications for cesarean section
Out of 100 cases of pregnant women, 68% of women had AFI >8 (normal) (10.53 ± 2.19), while 32% of women had AFI <8 (abnormal) (6.97 ± 1.26). The total mean AFI was computed as 9.39 ± 2.55 cm. The percentage of women having oligohydramnios along with specific indications was 50.01% (32 patients) [Figure 2].
Figure 2.
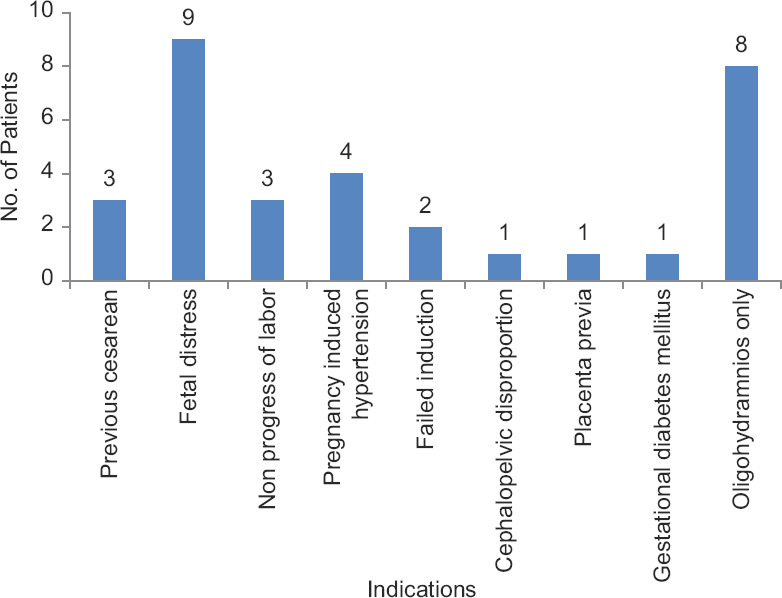
Distribution of cesarean patients having oligohydramnios (amniotic fluid index < 8) along with other high-risk factors
Among 100 pregnant women, 70% had S/D ratio <3 (normal) (2.39 ± 0.34) and 30% of women had S/D ratio >3 (abnormal) (3.14 ± 0.06). The total mean S/D ratio was found to be 2.61 ± 0.45. The ultrasonographic evaluation of UA S/D ratio and AFI was studied and their perinatal outcomes were noted [Tables 2-4].
Table 2.
Distribution of neonates according to systolic/diastolic ratio and amniotic fluid index and perinatal outcome
| Perinatal outcome | S/D ratio | AFI | ||
|---|---|---|---|---|
|
|
|
|||
| <3 (n=70), n (%) | >3 (n=30), n (%) | <8 (n=32), n (%) | >8 (n=68), n (%) | |
| Meconium | 5 (7.14) | 8 (26.66) | 7 (21.87) | 6 (8.82) |
| APGAR<7/10 at 5 min | 4 (5.71) | 6 (20) | 5 (15.62) | 5 (7.35) |
| RDS within 72 h of delivery | 6 (8.57) | 10 (33.33) | 7 (21.87) | 9 (13.23) |
| Perinatal mortality | 1 (1.42) | 1 (3.33) | 1 (3.12) | 1 (1.47) |
| NICU admissions | 16 (22.85) | 25 (83.33) | 20 (62.5) | 21 (30.88) |
| Normal | 54 (77.14) | 5 (16.66) | 12 (37.5) | 47 (69.11) |
S/D: Systolic/diastolic, AFI: Amniotic fluid index, APGAR: Appearance, pulse, grimace, activity, and respiration, RDS: Respiratory distress syndrome, NICU: Neonatal intensive care unit
Table 4.
Distribution of neonates according to amniotic fluid index and perinatal outcome
| Parameter | AFI | Total | |
|---|---|---|---|
|
| |||
| <8 | >8 | ||
| Meconium | |||
| Present | 7 (true positive) | 6 (false positive) | 13 |
| Absent | 12 (false negative) | 47 (true negative) | 59 |
| Total | 19 | 53 | 72 |
| APGAR score (at 5 min) | |||
| APGAR (<7/10) | 5 (true positive) | 5 (false positive) | 10 |
| APGAR (>7/10) | 12 (false negative) | 47 (true negative) | 59 |
| Total | 17 | 52 | 69 |
| RDS | |||
| Present | 7 (true positive) | 9 (false positive) | 16 |
| Absent | 12 (false negative) | 47 (true negative) | 59 |
| Total | 19 | 56 | 75 |
| Perinatal mortality | |||
| Present | 1 (true positive) | 1 (false positive) | 2 |
| Absent | 12 (false negative) | 47 (true negative) | 59 |
| Total | 13 | 48 | 61 |
AFI: Amniotic fluid index, APGAR: Appearance, pulse, grimace, activity, and respiration, RDS: Respiratory distress syndrome
Table 3.
Distribution of neonates according to systolic/diastolic ratio and perinatal outcome
| Parameter | S/D ratio | Total | |
|---|---|---|---|
|
| |||
| >3 | <3 | ||
| Meconium | |||
| Present | 8 (true positive) | 5 (false positive) | 13 |
| Absent | 5 (false negative) | 54 (true negative) | 59 |
| Total | 13 | 59 | 72 |
| APGAR score (at 5 min) | |||
| APGAR (<7/10) | 6 (true positive) | 4 (false positive) | 10 |
| APGAR (>7/10) | 5 (false negative) | 54 (true negative) | 59 |
| Total | 11 | 58 | 69 |
| RDS | |||
| Present | 10 (true positive) | 6 (false positive) | 16 |
| Absent | 5 (false negative) | 54 (true negative) | 59 |
| Total | 15 | 60 | 75 |
| Perinatal mortality | |||
| Present | 1 (true positive) | 1 (false positive) | 2 |
| Absent | 5 (false negative) | 54 (true negative) | 59 |
| Total | 6 | 55 | 61 |
S/D: Systolic/diastolic, APGAR: Appearance, pulse, grimace, activity, and respiration, RDS: Respiratory distress syndrome
UA S/D ratio had better performance values (i.e., sensitivity, specificity, and positive and negative predictive values) than AFI in predicting perinatal outcome, as shown in Table 5.
Table 5.
Test performance values of systolic/diastolic ratio and amniotic fluid index according to the perinatal outcome
| Parameters | Test performance | Meconium | APGAR | Respiratory complication | Perinatal mortality |
|---|---|---|---|---|---|
| S/D ratio | Sensitivity (%) | 61.53 | 60 | 62.5 | 50 |
| Specificity (%) | 91.52 | 91.52 | 91.52 | 91.52 | |
| PPV (%) | 61.53 | 54.54 | 66.66 | 16.66 | |
| NPV (%) | 91.52 | 93.10 | 90 | 98.18 | |
| P | 0.0001 | 0.001 | 0.0001 | 0.471 | |
| AFI | Sensitivity (%) | 53.84 | 50 | 43.75 | 50 |
| Specificity (%) | 79.66 | 79.66 | 79.66 | 79.66 | |
| PPV (%) | 36.84 | 29.41 | 36.84 | 7.69 | |
| NPV (%) | 88.67 | 90.38 | 83.92 | 97.91 | |
| P | 0.031 | 0.102 | 0.109 | 0.609 |
APGAR: Appearance, pulse, grimace, activity, and respiration, S/D: Systolic/diastolic, AFI: Amniotic fluid index, NPV: Negative predictive value, PPV: Positive predictive value
Out of 100 women studied, 30 women had an S/D ratio >3. Among, these 27 women (90%) had reduced diastolic flow. Of 27 newborns, 8 (29.61%) had meconium-stained liquor, 3 (11.11%) had APGAR <7/10, 10 (37.03%) respiratory complications within 72 h, 1 (3.70%) neonate expired after NICU admission, and 5 (18.51%) were found normal. A total of 22 (81.48%) newborns got admitted in NICU. However, among 30 women who had an S/D ratio >3, 3 women (10%) had absent diastolic flow. Three newborns (100%) among these women had meconium-stained liquor as well as APGAR <7/10. All these neonates were admitted in NICU.
Discussion
AFI and fetal UA Doppler velocimetry are considered as a newer modality in assessing fetal well-being, thus helped in identifying compromised fetuses. They are important indicators of fetal well-being and both of these indicators help in reducing perinatal morbidity and mortality. In the present study, the mean age of women was 27.07 ± 3.75 years which is comparable with the study conducted by Shivalingaiah et al.[11] and Asgharnia et al.[12] The majority of women were from urban background (59%) and most of them were booked (54%). About 58% of women were multigravida, this is correlated with the study done by Jandial et al.[13] About 64% of women underwent cesarean section, as similar to the study conducted by Bachhav et al.[14] Seventeen percent of the cases presented as breech. Intrauterine fetal death occurred in 5.5% of these pregnancies. As it is a tertiary care referral center and women with various high-risk factors are referred from the periphery, the rates of cesarean section are high. The most common indication for cesarean section was the previous history of cesarean section.
Amniotic fluid volume remains an important component of any obstetric ultrasonographic examination. The AFI was the most commonly used method of measuring amniotic fluid. In the present study, 68% of women had AFI >8 which was considered normal and 32% of women had AFI <8 which was considered to be abnormal. The mean AFI was 9.39 ± 2.55 cm. These findings are correlated with the previous studies.[14,15,16,17] Umbilical arterial Doppler assessment is used in the surveillance of fetal well-being in the third trimester of pregnancy. It is a marker of uteroplacental insufficiency and its assessment has been shown to reduce perinatal mortality and morbidity in high-risk obstetrical situations. The distribution of women according to UA S/D ratio reveals that 70% of women have S/D ratio <3 and 30% of women have S/D ratio >3, which is in accordance with the study conducted by Singh et al.[18] and Carroll et al.[19] and Kwon et al.[20]
In the current study, perinatal outcome was evaluated on the basis of presence of meconium, Apgar at 5 min, presence of respiratory complications of delivery, NICU admission, and perinatal mortality cases if any. Out of 100 women, 70% of women had an S/D ratio <3, 77.14% had normal perinatal outcome, while 22.85% of women had some perinatal complications, as 7.14% of neonates had meconium, 5.71% of neonates had Apgar <7/10 at 5 min, 8.57% of neonates had respiratory complications within 72 h of delivery, and perinatal deaths were found in 1.42%. Only 22.85% of neonates were admitted in NICU, whereas 30% of women had S/D ratio >3, of them 16.66% of women had normal perinatal outcome and 83.33% of women had some perinatal complications in their neonates. Of them, 26.66% of neonates had meconium, 20% of neonates had APGAR <7/10 at 5 min, 33.33% of neonates had respiratory complications within 72 h of delivery, and perinatal deaths reported were 3.33%. Almost 83.33% of neonates were admitted in NICU. These findings are comparable with earlier studies.[1,18,19,20,21,22]
Moreover, out of 100 women, 68% of women had AFI >8, 69.11% women had normal perinatal outcome, and 30.88% women had some perinatal complications, as 8.82% neonates had meconium, 7.35% neonates had APGAR <7/10 at 5 min, 13.23% neonates had respiratory complications within 72 h of delivery, and perinatal deaths were 1.47%. About 30.88% of neonates were admitted in NICU, whereas out of 100 women, 32% of women had AFI <8, of them 37.5% of women had normal perinatal outcome and 62.5% of women had some perinatal complications in their neonates. Of them, 21.87% of neonates had meconium, 15.62% of neonates had APGAR </10 at 5 min, 21.87% of neonates had respiratory complications within 72 h of delivery, and 3.12% of perinatal deaths were reported among this group. About 62.5% of neonates were admitted in NICU. Similar findings are reported in Goyal et al.[1] study.
Sensitivity, specificity, and positive and negative predictive values were calculated for S/D ratio in accordance with meconium were 61.53%, 91.52%, 61.53%, and 91.52%, respectively (P < 0.0001); in accordance with Apgar at 5 min, they were 60%, 91.52%, 54.54%, and 93.10%, respectively (P < 0.001) as well as in accordance with respiratory complications within 72 h of delivery, they were 62.5%, 91.52%, 66.66%, and 90%, respectively (P < 0.0001); and in accordance with perinatal mortality, they were 50%, 91.52%, 16.66%, and 98.18%, respectively (P < 0.0.471). These results are similar to the study conducted by Goyal et al.[1] and Lakhar et al.[23] Both these studies showed that UA S/D ratio is a good predictor of perinatal outcome in high-risk pregnancy cases. In addition, the sensitivity, specificity, and positive and negative predictive values for AFI in accordance with meconium were 53.84%, 79.66%, 36.84%, and 88.67%, respectively (P < 0.031); in accordance with Apgar score at 5 min, they were 50%, 79.66%, 29.41%, and 90.38%, respectively (P < 0.102); in accordance with respiratory distress syndrome, they were 43.75%, 79.66%, 36.84%, and 83.92%, respectively (P < 0.109); and in accordance with perinatal mortality, they were 50%, 79.66%, 7.69%, and 97.91% (P < 0.609). These results are similar to the previous studies.[1,23,24,25]
Out of 100 women, 30 women had an S/D Ratio >3. Among these women, 27 women (90%) had reduced diastolic flow. Of 27 newborns, 8 (29.61%) had meconium-stained liquor, 3 (11.11%) neonates had APGAR <7/10, 10 (37.03%) neonates had respiratory complications within 72 h, and 1 (3.70%) neonate expired after NICU admission. Of these, 5 (18.51%) newborns were found normal. A total of 22 (81.48%) newborns got admitted in NICU, whereas among 30 women, 3 women (10%) had absent diastolic flow. Three newborns (100%) among these women had meconium-stained liquor as well as APGAR </10. All these neonates were admitted in NICU. There was no case which showed reversal of flow in their color Doppler study. These findings are correlated with the other studies.[1,26] UA S/D ratio had a better performance value than AFI in predicting perinatal outcome.
Some limitations of the study include it did not include fetal MCA Doppler, ductus venosus flow, and uterine arterial Doppler assessment. A larger sample size with a detailed evaluation of these vessels may have proved effective in elucidating any maternal and neonatal side effects related to them. Comparison of AFI with the single deepest pocket for perinatal outcome was not done. Severity of oligohydramnios was also not categorized further in relation to the perinatal outcome.
Conclusion
We concluded that both the tests AFI and UA S/D ratio form an integral part of antepartum fetal surveillance. In addition, both tests are important for predicting low APGAR, meconium staining, respiratory complications, and perinatal mortality in high- as well as low-risk pregnancy cases. However, UA S/D ratio is a better predictor of perinatal outcome in high-risk pregnancies. The importance of AFI cannot be overlooked; rather, it adds to UA S/D ratio in predicting perinatal outcome, but both are complimentary to each other in decision-making. In future, studies should be designed so as to evaluate fetal MCA Doppler, ductus venosus flow, and uterine arterial Doppler assessment. AFI and single deepest pocket should also be considered in future studies for identifying actual abnormal amniotic fluid (AF) volume estimation.
Ethical clearance
Ethical Clearance was obtained from the Institutional Ethical Committee of Geetanjali Medical College, Udaipur.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Goyal S, Suresh A, Rao AA. Amniotic fluid index versus umbilical artery Doppler velocimetry in prediction of perinatal outcome. Int J Innov Res Dev. 2014;3:91–4. [Google Scholar]
- 2.O'Neill E, Thorp J. Antepartum evaluation of the fetus and fetal well being. Clin Obstet Gynecol. 2012;55:722–30. doi: 10.1097/GRF.0b013e318253b318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arduini D, Rizzo G, Romanini C. Changes of pulsatility index from fetal vessels preceding the onset of late decelerations in growth-retarded fetuses. Obstet Gynecol. 1992;79:605–10. [PubMed] [Google Scholar]
- 4.Sterne G, Shields LE, Dubinsky TJ. Abnormal fetal cerebral and umbilical Doppler measurements in fetuses with intrauterine growth restriction predicts the severity of perinatal morbidity. J Clin Ultrasound. 2001;29:146–51. doi: 10.1002/1097-0096(200103/04)29:3<146::aid-jcu1014>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 5.Arias F. Accuracy of the middle-cerebral-to-umbilical-artery resistance index ratio in the prediction of neonatal outcome in patients at high risk for fetal and neonatal complications. Am J Obstet Gynecol. 1994;171:1541–5. doi: 10.1016/0002-9378(94)90398-0. [DOI] [PubMed] [Google Scholar]
- 6.Makhseed M, Jirous J, Ahmed MA, Viswanathan DL. Middle cerebral artery to umbilical artery resistance index ratio in the prediction of neonatal outcome. Int J Gynaecol Obstet. 2000;71:119–25. doi: 10.1016/s0020-7292(00)00262-9. [DOI] [PubMed] [Google Scholar]
- 7.Arias F, Bhide A, Arulkumaran S, Kaizad Damania, Daftary S, editors. Arias'Practical Guide to High-Risk Pregnancy and Delivery-A South Asian Perspective. 5th ed. New Delhi: Elsevier Publications; 2019. p. 23. [Google Scholar]
- 8.Lombardi SJ, Rosemond R, Ball R, Entman SS, Boehm FH. Umbilical artery velocimetry as a predictor of adverse outcome in pregnancies complicated by oligohydramnios. Obstet Gynecol. 1989;74:338–41. [PubMed] [Google Scholar]
- 9.Carroll BC, Bruner JP. Umbilical artery Doppler velocimetry in pregnancies complicated by oligohydramnios. J Reprod Med. 2000;45:562–6. [PubMed] [Google Scholar]
- 10.Phelan JP, Ahn MO, Smith CV, Rutherford SE, Anderson EJ. Amniotic fluid index measurements during pregnancy. J Reprod Med. 1987;32:601–4. [PubMed] [Google Scholar]
- 11.Shivalingaiah N, Varadarajan R, Mamatha MS. A clinical study of amniotic fluid index and umbilical artery Doppler study at or beyond 34 weeks gestation and its relation to perinatal outcome. J Evol Med Dent Sci. 2015;4:3040–6. [Google Scholar]
- 12.Asgharnia M, Faraji R, Salamat F, Naimian S. Perinatal outcomes of pregnancy with borderline versus normal amniotic fluid index. Iran J Reprod Med. 2013;11:705–10. [PMC free article] [PubMed] [Google Scholar]
- 13.Jandial C, Gupta S, Sharma S, Gupta M. Perinatal outcome after antepartum diagnosis of oligohydramnios at or beyond 34 weeks of Gestation. JK Sci. 2007;9:213–4. [Google Scholar]
- 14.Bachhav AA, Waikar M. Low amniotic fluid index at term as a predictor of adverse perinatal outcome. J Obstet Gynaecol India. 2014;64:120–3. doi: 10.1007/s13224-013-0489-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Iqbal S, Noreen A. Low amniotic fluid index as a predictor of perinatal outcome in low risk pregnancies at term. Services Institute of Medical Sciences, Lahore. PJMHS. 2010;4:270–1. [Google Scholar]
- 16.Jagatia K, Singh N, Patel S. Maternal and fetal outcome in oligohydramnios. A study of 100 cases. Int J Med Sci Public Health. 2013;2:724–7. [Google Scholar]
- 17.Kaur P, Desai DA, Taraiya A. A study on the perinatal outcome in cases of oligohydramnios. Int J Reprod Contracept ObstetGynaecol. 2016;5:98–109. [Google Scholar]
- 18.Singh BB, Ara S, Birla N, Jyothi D, Chodhary S. Umbilical artery Doppler indices better predictor for perinatal and obstetrics outcome in oligohydromnios at or beyond 34 weeks of gestation, paripex. Indian J Res. 2015;4:6–7. [Google Scholar]
- 19.Carroll BC, Brunner JP. Umbilical artery Doppler as a predictor of perinatal outcome in pregnancies complicated by oligohydramnios. Am J ObstetGynaecol. 1998;178:86. [Google Scholar]
- 20.Kwon JY, Kwon HS, Kim YH, Park YW. Abnormal Doppler velocimetry is related to adverse perinatal outcome for borderline amniotic fluid index during third trimester. J ObsGynaecol Res. 2006;32:545–9. doi: 10.1111/j.1447-0756.2006.00459.x. [DOI] [PubMed] [Google Scholar]
- 21.Sriya R, Singhai S, Rajan M, Sharman M, Nagel P. Perinatal outcome in patients with amniotic fluid index<=5cm. J ObstetGynaecol India. 2001;51:98–100. [Google Scholar]
- 22.Arora D, Desai SK, Sheth PN, Prema K. Significance of umbilical velocimetry in perinatal outcome of growth retarded fetuses. J ObstetGynaecol India. 2005;55:138–43. [Google Scholar]
- 23.Lakhkar BN, Rajagopal KV, Gourisankar PT. Doppler prediction of adverse perinatal outcome in PIH and IUGR. Indian J Radiol Imaging. 2006;16:109–16. [Google Scholar]
- 24.Dubinsky T, Lau M, Powell F, Garcia J, Mastobattista J, Parvey HR, et al. Predicting poor neonatal outcome:A comparative study of noninvasive antenatal testing methods. AJR Am J Roentgenol. 1997;168:827–31. doi: 10.2214/ajr.168.3.9057543. [DOI] [PubMed] [Google Scholar]
- 25.Sultana S, Akbar Khan MN, Khanum Akhtar KA, Aslam M. Low amniotic fluid index in high-risk pregnancy and poor apgar score at birth. J Coll Physicians Surg Pak. 2008;18:630–4. doi: 10.2008/JCPSP.630634. [DOI] [PubMed] [Google Scholar]
- 26.Jang DG, Jo YS, Lee SJ, Kim N, Lee GS. Perinatal outcomes and maternal clinical characteristics in IUGR with absent or reversed end-diastolic flow velocity in the umbilical artery. Arch Gynecol Obstet. 2011;284:73–8. doi: 10.1007/s00404-010-1597-8. [DOI] [PubMed] [Google Scholar]


