ABSTRACT
Foot-and-mouth disease (FMD) is an acute contagious disease that affects cloven-hoofed animals and has severe global economic consequences. FMD is most commonly controlled by vaccination. Currently available commercial FMD vaccines contain chemically inactivated whole viruses, which are thought to be slow acting as they are effective only 4 to 7 days following vaccination. Hence, the development of a novel rapid vaccine or alternative measures, such as antiviral agents or the combination of vaccines and antiviral agents for prompt FMD virus (FMDV) outbreak containment, is desirable. Here, we constructed a recombinant baculovirus (BacMam) expressing consensus porcine interferon alpha (IFN-α) that has three additional N-glycosylation sites driven by a cytomegalovirus immediate early (CMV-IE) promoter (Bac-Con3N IFN-α) for protein expression in mammalian cells. Bac-Con3N IFN-α expressing highly glycosylated porcine IFN-α protein increased the duration of antiviral effects. We evaluated the antiviral effects of Bac-Con3N IFN-α in swine cells and mice and observed sustained antiviral effects in pig serum; additionally, Bac-Con3N IFN-α exhibited sustained antiviral effects in vivo as well as adjuvant effects in combination with an inactivated FMD vaccine. Pigs injected with a combination of Bac-Con3N IFN-α and the inactivated FMD vaccine were protected against FMDV at 1, 3, and 7 days postvaccination. Furthermore, we observed that in combination with the inactivated FMD vaccine, Bac-Con3N IFN-α increased neutralizing antibody levels in mice and pigs. Therefore, we suggest that Bac-Con3N IFN-α is a strong potential antiviral and adjuvant candidate for use in combination with inactivated FMD vaccines to protect pigs against FMDV.
IMPORTANCE Early inhibition of foot-and-mouth disease (FMD) virus (FMDV) replication in pigs is highly desirable as FMDV transmission and shedding rates are higher in pigs than in cattle. However, commercial FMD vaccines require at least 4 to 7 days postvaccination (dpv) for protection, and animals are vulnerable to heterologous viruses before acquiring high antibody levels after the second vaccination. Therefore, the development of antiviral agents for use in combination with FMD vaccines is essential. We developed a novel antiviral and immunostimulant, Bac-Con3N IFN-α, which is a modified porcine IFN-α-expressing recombinant baculovirus, to improve IFN stability and allow its direct delivery to animals. We present a promising candidate for use in combination with inactivated FMD vaccines as pigs applied to the strategy had early protection against FMDV at 1 to 7 dpv, and their neutralizing antibody levels were higher than those in pigs administered the vaccine only.
KEYWORDS: BacMam, foot-and-mouth disease virus, interferons, vaccines
INTRODUCTION
Foot-and-mouth disease (FMD), an acute contagious disease affecting cloven-hoofed animals such as cows, pigs, and sheep, induces fever, lameness, and blisters on the mouth, tongue, snout, teats, and feet (1, 2). FMD virus (FMDV), of the Aphthovirus genus of the Picornaviridae family, consists of a single-stranded, positive-sense RNA genome. This virus has seven immunologically distinct serotypes with no cross-immunity: A, O, C, Asia1, South African Territories 1 (SAT1), SAT2, and SAT3. Commercial FMD vaccines are derived from inactivated whole viruses and manufactured as single- or double-emulsion oil-based formulations to be administered to pigs (3). These inactivated vaccines are currently used worldwide, including in Asia, to prevent FMDV transmission. Such vaccines, including the emergency vaccine (>6PD50 [50% protective dose]), are effective against FMDV serotypes A and O only after a minimum of 4 and 7 days, respectively, following vaccination (4–6). Particularly, early inhibition of viral replication in pigs is of great importance as viral shedding in pigs is higher than that in ruminants (7). Therefore, the development of antiviral agents for rapid protection against FMDV is necessary, and several such antiviral agents (interferons [IFNs], chemical compounds, and small interference RNAs [siRNAs]) have been suggested (2, 8–13). A more practical application for early protection against FMDV in pigs using a combination of antiviral agents and FMD vaccines has been demonstrated (14–16).
FMDV is highly sensitive to interferon alpha (IFN-α) (2, 17), which is a promising antiviral candidate for a combination strategy with an inactivated FMD vaccine (15, 18, 19). The protective effects of a vaccine in combination with IFNs against FMDV have been observed by as early as 1 to 2 days postvaccination (dpv). Moraes et al. reported that a combination of a replication-defective human adenovirus type 5 (Ad5) vector-porcine IFN-α (poIFN-α) and an Ad5 A24 vaccine demonstrated protective effects at 1, 3, and 5 dpv (20). We also showed that the combination of an inactivated FMD vaccine and antiviral agents was effective until 4 dpv in previous studies (15, 18). However, this combination strategy did not provide protection in pigs at 7 dpv, possibly owing to the short half-life of IFN in the body. To solve this limitation, modifications of IFN have been suggested. Recently, it was reported that swine injected with pegylated porcine IFN-α protein were protected from FMDV challenge for 5 days posttreatment (21). The addition of N-glycosylation sites to human IFN-α is also known to significantly increase its half-life (22, 23). Glycosylation is a posttranslational modification that increases the half-life of a protein and protects against degradation by proteases. The tripeptide N (Asn)-X-T (Thr) or -S (Ser) is known as the N-glycosylation motif (24, 25). The introduction of N-glycosylation sites by four amino acid mutations (P4N, R23N, K70N, and D77N) or a single amino acid mutation (G104N) was effective in decreasing systemic clearance and increasing antiviral effects in vivo (22, 26). Moreover, the antiviral effect of consensus IFN-α (IFN-α with common amino acid sequences of various subtypes) was significantly higher than that of normal IFN-α (27, 28).
The baculovirus Autographa californica nuclear polyhedrosis virus (AcMNPV) with a cytomegalovirus immediate early 1 (CMV-IE) promoter has been effectively used as a mammalian cell gene delivery vector (BacMam) to produce proteins in various cell lines (29). The baculovirus expression system in insect cells has been classically used for the large-scale production of recombinant proteins (30, 31), and it has proven to be an effective and safe viral vector for gene expression in animals as the baculovirus can transduce genes but cannot replicate in mammalian cells (32–34). The BacMam vector is more suitable for the expression of N-glycosylated proteins in cell lines or animals because the sialylated form of N-glycosylated proteins cannot be produced using the baculovirus-insect cell expression system (35, 36). Furthermore, live AcMNPV is a vaccine adjuvant candidate that induces cellular and humoral immune responses by producing proinflammatory cytokines and type I IFNs (37, 38). The BacMam system has been used to develop an African swine fever (ASF) vaccine; however, only partial protection of vaccinated pigs was observed (34).
Here, we constructed a recombinant baculovirus (BacMam) vector expressing consensus porcine IFN-α with three N-glycosylation sites driven by a CMV-IE promoter. This design was intended to (i) increase the duration and antiviral effect of the interferon protein and (ii) induce a rapid and effective immune response. Therefore, we tested the duration of the antiviral effect of the Con3N IFN-α protein in pig serum and the antiviral effects of Bac-Con3N IFN-α in swine cells and mice. We treated pigs with the inactivated FMD vaccine and Bac-Con3N IFN-α to evaluate protection for 7 days against FMDV. Furthermore, we investigated the adjuvant effects of Bac-Con3N IFN-α in combination with the inactivated FMD vaccine after 7 dpv in mice and pigs.
RESULTS
Bac-Con3N IFN-α protein expression in porcine cells.
Western blotting was performed to evaluate the expression of highly glycosylated porcine IFN-α from Bac-Con3N IFN-α in the mammalian cells. Porcine IFN-α was detected in the supernatants of Bac-Con3N IFN-α-infected porcine kidney (LFBK) cells (Fig. 1B). Highly glycosylated porcine IFN-α was observed as a smeared band with a molecular weight of 13 to 23 kDa; its exact molecular weight was found to be approximately 19 kDa in peptide-N-glycosidase F (PNGase F)-treated Bac-Con3N IFN-α samples.
FIG 1.

Plasmid construction and detection of protein expression in swine cells. (A) Genes of the cytomegalovirus immediate early 1 (CMV-IE) promoter, the signal sequence (ss), and consensus porcine IFN-α with N-glycosylation sites (4th, 23rd, and 78th amino acid positions) were cloned into the pFastBac dual vector by cleaving with the restriction sites SmaI and NheI to construct Bac-Con3N IFN-α. The baculovirus negative control (Bac-Neg con) was constructed by cloning the CMV-IE promoter by cleaving only with the restriction sites SmaI and XhoI. (B) LFBK cells were infected with Bac-Con3N IFN-α or Bac-Neg con at a multiplicity of infection (MOI) of 200. The supernatant was collected and concentrated at 48 h postinfection. Samples were treated with PNGase F or not to detect the presence of nonglycosylated or glycosylated protein and were used for Western blotting. To detect porcine IFN-α, swine IFN-α1 polyclonal antibody and rabbit anti-goat IgG(H+L) (HRP) were used as the primary and secondary antibodies, respectively.
Antiviral effects of Bac-Con3N IFN-α and sustained effects of highly glycosylated porcine IFN-α against FMDV.
To evaluate the antiviral effects of Bac-Con3N IFN-α against FMDV in swine cells, FMDV replication in LFBK cells treated with either Bac-Con3N IFN-α or the baculovirus negative control (Bac-Neg con) at a multiplicity of infection (MOI) of 50 was analyzed. Viral loads were significantly lower in cells inoculated with Bac-Con3N IFN-α than in cells inoculated with Bac-Neg con (by ~3 log10 units) 24 h following infection (P < 0.05) (Fig. 2). The antiviral effects of Bac-Con3N IFN-α were still observable at 48 h postinfection (hpi). However, inhibition of viral replication was not observed in Bac-Neg con-treated cells. The stability of highly glycosylated porcine IFN-α expressed by Bac-Con3N IFN-α in swine cells (Con3N-poIFN-α) following incubation with pig serum was compared to that of nonengineered porcine IFN-α in mammalian cells (recombinant poIFN-α). The experiment was performed to simulate the antiviral effects of the proteins following their administration to pigs. The units of Con3N-poIFN-α were higher than those of recombinant poIFN-α at 6, 18, 24, and 48 hpi (P < 0.05 and P < 0.01) (Fig. 3). More specifically, the antiviral effects of the recombinant poIFN-α decreased significantly from 450 U/mL to <50 U/mL 18 hpi, whereas Con3N-poIFN-α maintained its antiviral effects at values of >300 U/mL at 48 hpi.
FIG 2.
Antiviral effects of Bac-Con3N IFN-α against FMDV in swine cells. LFBK cells were inoculated with recombinant baculoviruses (Bac-Neg con or Bac-Con3N IFN-α) at an MOI of 50, except for the FMDV control. After 18 h, the recombinant baculoviruses were removed, and cells were washed with DMEM. Thereafter, cells were infected with 100 TCID50 of FMDV; after 1 h of FMDV infection, the inoculum was removed, and DMEM was added. Cells were incubated at 37°C for 24 or 48 h, and the supernatant was collected. To evaluate the effects on FMDV RNA replication, RNA extraction and quantitative real-time PCR were performed using the supernatant.
FIG 3.
Enhanced duration of the antiviral effect of glycosylated porcine IFN-α protein in pig serum. The same units of protein produced from Bac-Con3N IFN-α in LFBK cells and the porcine IFN-α (mammalian) protein (R&D Systems, Minneapolis, MN, USA) expressed in mammalian cells were diluted to a 1:3 (vol/vol) ratio with swine serum. The porcine IFN-α proteins mixed with swine serum were incubated at 37°C for 6, 12, 24, or 48 h and immediately frozen at −80°C. After thawing the samples simultaneously, the biological activities of the IFN-α proteins were measured using the IFN biological assay. Error bars indicate standard deviations (SD) of the means. Unpaired t tests were performed for statistical analysis (*, P < 0.05; **, P < 0.01).
Bac-Con3N IFN-α enhances IFN-stimulated gene mRNA activation.
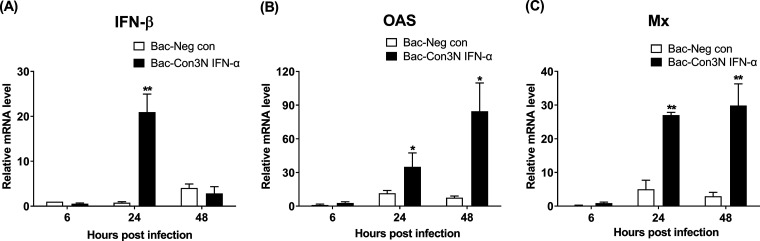
To evaluate the intracellular antiviral effects of Bac-Con3N IFN-α, we measured IFN mRNA levels and Bac-Con3N IFN-α-induced IFN-stimulated gene (ISG) expression in swine cells. The mRNA levels of genes encoding IFN-β, 2′-5′-oligoadenylate synthetase (OAS), and myxovirus resistance (Mx) were significantly higher in Bac-Con3N IFN-α-treated cells than in Bac-Neg con-treated cells (P < 0.05) (Fig. 4). Significant ISG mRNA activation was not observed in Bac-Neg con-treated cells. IFN-β mRNA levels increased by approximately 20-fold from 6 to 24 hpi and decreased again from 24 to 48 hpi following treatment with Bac-Con3N IFN-α (Fig. 4A). OAS and Mx mRNA levels increased from 6 to 48 hpi following treatment with Bac-Con3N IFN-α (Fig. 4B and C).
FIG 4.
Induction of IFN-stimulated genes (ISGs) of Bac-Con3N IFN-α in swine cells. LFBK cells were inoculated with recombinant baculoviruses at an MOI of 50. Cells were collected at 6, 24, and 48 h postinfection, and RNA extraction, DNase I treatment, and quantitative real-time PCR were performed. To analyze ISG expression, quantitative real-time PCR was used to evaluate the levels of interferon beta (IFN-β) (A), 2′-5′-oligoadenylate synthetase (OAS) (B), and myxovirus resistance (Mx) (C) mRNAs. Error bars indicate standard deviations (SD) of the means. Unpaired t tests were performed for statistical analysis (*, P < 0.05).
Inoculation with Bac-Con3N IFN-α improves the survival rates of mice.
Mice were inoculated with 3 × 108 PFU of Bac-Con3N IFN-α or Bac-Neg con and subsequently challenged with FMDV to evaluate the antiviral activity of Bac-Con3N IFN-α in vivo (Fig. 5). Compared with mice in the phosphate-buffered saline (PBS) control group, both groups of mice treated with either Bac-Con3N IFN-α or Bac-Neg con showed improved survival rates. However, 1 or 3 days before the FMDV challenge, the survival rates of the mice inoculated with Bac-Con3N IFN-α (100% or 80%) were higher than those of the mice inoculated with Bac-Neg con (80% or 40%) (Fig. 5A and B).
FIG 5.
Enhanced survival rates in mice injected with Bac-Con3N IFN-α. C57BL/6 mice were inoculated via intraperitoneal injection with 3 × 108 PFU of Bac-Con3N IFN-α or Bac-Neg con and challenged with 200 LD50 (50% lethal doses) of mouse-adapted FMDV O/VIT/2013 at 1 day (A) or 3 days (B) postinoculation. Animals were monitored for 7 days after FMDV infection.
Bac-Con3N IFN-α inoculation induces cytokine activation in mice.
The cytokine levels were measured in mice inoculated with 3 × 108 PFU of Bac-Con3N IFN-α or Bac-Neg con. IFN-α, IFN-γ, interleukin-12 (IL-12), IL-15, and IL-18 levels increased in the mice inoculated with Bac-Con3N IFN-α and Bac-Neg con (P < 0.05) (Fig. 6). IL-6 induction was observed only in those mice inoculated with Bac-Con3N IFN-α (P < 0.01) (Fig. 6E). IFN-α, IFN-γ, IL-12, IL-15, IL-6, and IL-18 levels in the Bac-Con3N IFN-α group were significantly higher than those in the Bac-Neg con group (P < 0.05). The highest IFN-α, IFN-γ, and IL-6 levels in the Bac-Con3N IFN-α group were observed soon after inoculation (6 or 16 h posttreatment), while those of IL-12, IL-15, and IL-18 were observed 16 or 24 h following treatment.
FIG 6.
Measurement of cytokine induction in mice after injection with Bac-Con3N IFN-α. BALB/c mice were inoculated via intraperitoneal injection with 3 × 108 PFU of Bac-Con3N IFN-α or Bac-Neg con. Serum samples were collected at 0, 6, 16, and 24 h postinjection, and protein levels of mouse IFN-α, mouse IFN-γ, mouse IL-12, mouse IL-15, mouse IL-6, and mouse IL-18 were measured using an ELISA. Error bars indicate standard deviations (SD) of the means. An unpaired t test was performed to identify statistically significant differences between the 0-h posttreatment group and the 6-, 16-, or 24-h posttreatment group or between the Bac-Neg con group and the Bac-Con3N IFN-α group (*, P < 0.05; **, P < 0.01).
Bac-Con3N IFN-α and inactivated FMD vaccine coinoculation induces early protective effects against FMDV in pigs.
Pigs coinoculated with 2 × 1010 PFU or 6 × 1010 PFU of Bac-Con3N IFN-α and the inactivated FMD vaccine were challenged with FMDV 1, 3, or 7 days following vaccination. Pigs inoculated with 2 × 1010 PFU of the baculoviruses in the combination group were protected against FMDV at 1 dpv, whereas pigs in the vaccine-PBS group showed higher clinical sign scores and viral copy numbers in their sera and saliva (Table 1). Concerning the challenge at 3 dpv, compared to pigs in the vaccine group, those in the combination group had lower clinical sign scores (1 or 2) and viral copy numbers (by 2 log10 units) in their sera and saliva. All pigs inoculated with the higher baculovirus titer (6 × 1010 PFU) in the combination group were protected against FMDV at 3 or 7 dpv. However, pigs in the vaccine (3 dpv) and PBS groups had the maximum clinical sign scores (9 or 10) and high viral copy numbers in the serum and saliva. Pigs in the vaccine (7 dpv) group exhibited lower clinical sign scores (6 or 7) and serum viral copy numbers (by 3 log10 units) than those in the PBS group.
TABLE 1.
Clinical responses of pigs treated with the mixture of the vaccine and Bac-Con3N IFN-α and challenged with FMDV depending on the time of challenge and baculovirus titera
| Animal | Treatment(s) | Baculovirus titer (PFU) | Time of challenge (dpv) | Mean max amt of viral RNA detected ± SD (dpc of 1st detection)b in: |
Max clinical score (dpc of 1st detection) | |
|---|---|---|---|---|---|---|
| Serum | Saliva swab | |||||
| 1 | Bac-Con3N IFN-α and vaccine | 2 × 1010 | 1 | Neg | Neg | Neg |
| 2 | Neg | Neg | Neg | |||
| 3 | Neg | Neg | Neg | |||
| 4 | Vaccine | 2.7 × 105 ± 0.2 × 105 (2) | 1.2 × 105 ± 0.2 × 105 (1) | 9 (2) | ||
| 5 | 2.5 × 105 ± 0.6 × 105 (2) | 7.8 × 104 ± 0.1 × 104 (1) | 9 (2) | |||
| 6 | 4.2 × 105 ± 0.3 × 105 (2) | 1.3 × 105 ± 0.2 × 105 (1) | 10 (2) | |||
| 7 | Bac-Con3N IFN-α and vaccine | 3 | 1.4 × 103 ± 0.03 × 103 (4) | 2.4 × 103 ± 0.2 × 103 (2) | 2 (4) | |
| 8 | 9.0 × 102 ± 0.1 × 102 (4) | 1.0 × 103 ± 0.3 × 103 (2) | 1 (5) | |||
| 9 | 1.5 × 103 ± 0.1 × 103 (2) | 6.0 × 103 ± 0.04 × 103 (1) | 2 (4) | |||
| 10 | Vaccine | 1.4 × 105 ± 0.1 × 105 (2) | 1.3 × 105 ± 0.1 × 105 (1) | 8 (2) | ||
| 11 | 9.2 × 104 ± 0.1 × 104 (2) | 6.8 × 104 ± 0.1 × 104 (1) | 8 (2) | |||
| 12 | 1.97 × 105 ± 0.1 × 105 (2) | 3.7 × 104 ± 0.1 × 104 (1) | 8 (2) | |||
| 13 | PBS | 1 | ND | ND | ND | |
| 14 | 3.4 × 105 ± 0.4 × 105 (2) | 1.38 × 105 ± 0.2 × 105 (1) | 9 (3) | |||
| 15 | 3.2 × 105 ± 0.3 × 105 (2) | 4.2 × 104 ± 0.4 × 104 (1) | 10 (3) | |||
| 16 | Bac-Con3N IFN-α and vaccine | 6 × 1010 | 3 | Neg | Neg | Neg |
| 17 | Neg | 2.1 ± 0.6 (5) | Neg | |||
| 18 | Neg | Neg | Neg | |||
| 19 | Vaccine | 4.24 × 104 ± 0.1 × 104 (2) | 4.2 × 104 ± 0.3 × 104 (2) | 10 (3) | ||
| 20 | 5.2 × 104 ± 0.1 × 104 (2) | 9.8 × 104 ± 0.1 × 104 (2) | 9 (3) | |||
| 21 | 3.7 × 104 ± 0.1 × 104 (2) | 3.2 × 105 ± 0.1 × 105 (2) | 9 (3) | |||
| 22 | Bac-Con3N IFN-α and vaccine | 7 | Neg | 1.8 × 101 ± 0.2 × 101 (5) | Neg | |
| 23 | Neg | 6.6 ± 3.6 (8) | Neg | |||
| 24 | Neg | Neg | Neg | |||
| 25 | Vaccine | 4.3 × 103 ± 0.2 × 103 (4) | 6.1 × 104 ± 0.1 × 104 (2) | 6 (3) | ||
| 26 | 4.72 × 103 ± 0.6 × 103 (4) | 9.7 × 103 ± 0.1 × 103 (2) | 6 (3) | |||
| 27 | 4.9 × 103 ± 0.2 × 103 (2) | 5.4 × 104 ± 0.1 × 104 (2) | 7 (3) | |||
| 28 | PBS | 3 | 6.4 × 104 ± 0.5 × 104 (2) | 5.9 × 104 ± 0.2 × 104 (2) | 10 (3) | |
| 29 | 1.7 × 105 ± 0.2 × 105 (2) | 5.7 × 105 ± 0.3 × 105 (2) | 9 (3) | |||
| 30 | 6.6 × 104 ± 0.9 × 104 (2) | 2.1 × 104 ± 0.2 × 104 (2) | 10 (3) | |||
dpv, days postvaccination; dpc, days postchallenge; Neg, no viral RNA and no clinical symptoms were detected; ND, not detected because pig 14 was dead at 1 dpc.
Data (copy numbers of FMDV per milliliter) represent the means ± SD from triplicate RT-qPCR measurements.
Cytokine induction by coinoculation with Bac-Con3N IFN-α and the inactivated FMD vaccine in pigs.
Time-dependent changes in cytokine production levels in pigs were measured following inoculation with Bac-Con3N IFN-α and the inactivated FMD vaccine. IFN-α, IFN-γ, and IL-12 levels increased in pigs inoculated with the combination of Bac-Con3N IFN-α and the vaccine at 3 and 7 dpv (P < 0.05); however, there was no significant increase in the levels of these cytokines in pigs in the vaccine group (P > 0.05) (Fig. 7). Thus, IFN-α, IFN-γ, and IL-12 levels in pigs in the combination group (Bac-Con3N IFN-α plus the vaccine) were significantly higher than those in pigs in the vaccine group at both 3 and 7 dpv (P < 0.05). IFN-α and IFN-γ levels in pigs in the combination group increased at 3 dpv and decreased at 7 dpv (P < 0.01), and their IL-12 levels were unchanged from 3 to 7 dpv.
FIG 7.
Measurement of cytokine induction in pigs after injection with Bac-Con3N IFN-α. Three pigs per group were inoculated via intramuscular injection with the O/SKR/Boeun/2017 vaccine or the O/SKR/Boeun/2017 vaccine in combination with 4 × 1010 TCID50 of Bac-Con3N-poIFN-α, and blood collection was performed at 0, 3, or 7 days postvaccination. The vaccine was formulated with the O/SKR/Boeun/2017 vaccine antigen (15 μg/dose), 10% aluminum hydroxide gel, and Montanide ISA 206. Cytokine assays of serum samples were performed using the porcine IFN-γ ELISA kit, the porcine IFN-α ELISA kit, and the porcine IL-12/IL-23 P40 ELISA kit. Mean values and standard deviations (SD) are indicated with bars. Unpaired t tests were performed to identify statistically significant differences (*, P < 0.05; **, P < 0.01; ***, P < 0.005).
Coinoculation with Bac-Con3N IFN-α and the inactivated FMD vaccine enhances virus-neutralizing antibody levels.
To evaluate the effects of the combination of Bac-Con3N IFN-α and the vaccine on virus-neutralizing antibody titers, mice and pigs were inoculated with the vaccine, the combination of the FMD vaccine and Bac-Neg con (vaccine+Bac-Neg con), or the combination of the FMD vaccine and Bac-Con3N IFN-α (vaccine+Bac-Con3N IFN-α) (Fig. 8). The virus-neutralizing antibody titers in the mice in the vaccine+Bac-Con3N IFN-α and vaccine+Bac-Neg con groups were higher at 1, 2, 3, and 4 weeks postvaccination (wpv) and at 3 and 4 wpv, respectively, than those in the mice in the vaccine group (P < 0.05) (Fig. 8A). Furthermore, neutralizing antibody titers in the mice in the vaccine+Bac-Con3N IFN-α group were higher than those in the mice in the vaccine+Bac-Neg con group at 1, 2, 3, and 4 wpv (P < 0.01). Virus-neutralizing antibody titers were higher at 1, 3, and 5 wpv in pigs in the vaccine+Bac-Con3N IFN-α group than in pigs in the vaccine or vaccine+Bac-Neg con group (P < 0.05) (Fig. 8B). Lowering Bac-Con3N IFN-α titers from 2 × 1010 PFU to 8 × 109 PFU did not negatively affect the virus-neutralizing antibody levels.
FIG 8.
Enhanced virus-neutralizing antibody (VN Ab) levels caused by the combination of Bac-Con3N IFN-α and an oil-adjuvant-based inactivated FMD vaccine in mice and pigs. (A) C57BL/6 mice were inoculated via intramuscular (i.m.) injection with a mixture of 3 × 108 PFU of Bac-Con3N IFN-α (or Bac-Neg con) and the inactivated FMD vaccine or the FMD vaccine only. The FMD vaccine was formulated using ISA 206, 10% aluminum hydroxide gel, and 1 μg of the O/SKR/Boeun/2017 antigen. (B) Pigs were inoculated via i.m. injection with the mixture of 8 × 109 PFU or 2 × 1010 PFU of Bac-Con3N IFN-α (or 2 × 1010 PFU of Bac-Neg con) and the inactivated FMD vaccine or the FMD vaccine only. The FMD vaccine was formulated using ISA 206 oil adjuvant, 10% aluminum hydroxide gel, and 10 μg of the O/SKR/Boeun/2017 antigen. Serum samples were collected at 1, 2, 3, and 4 weeks postvaccination in mice and at 1, 3, and 5 weeks postvaccination in pigs. The virus-neutralizing antibody test was performed using serum samples. The dotted line indicates the 1:45 (1.65 log10 units) virus-neutralizing titer cutoff level. Error bars indicate standard deviations (SD) of the means. Unpaired t tests were performed to identify statistically significant differences between the vaccine group and others or among the combination groups (*, P < 0.05; **, P < 0.01; ***, P < 0.005).
DISCUSSION
Here, we present a promising drug candidate that exerts antiviral and immunomodulatory effects against FMDV. It was produced using baculoviruses containing a modified porcine IFN-α-expressing mammalian cell transduction (BacMam) delivery system. Interferon glycoengineering has been investigated as a means of improving their biological activity and pharmacokinetic stability (22, 26). We produced porcine IFN-α constructs with amino acid mutations P4N, R23N, and D77N, which were reported previously to effectively induce the production of highly glycosylated human IFN-α2; additionally, the K70N mutation, which was also reported here, was excluded because the 70th amino acid of the consensus porcine IFN-α sequence is different from that of human IFN-α (22). Protein N-glycosylation is a common structural modification that occurs in mammalian cells, and N-glycans are covalently attached to proteins or lipids through the action of glycosyltransferases localized in the Golgi apparatus (39). Glycosylation increases protein stability as glycans prevent contact between the glycoprotein’s surface and protease active sites. Furthermore, glycosylation patterns differ between animal species, and glycosylated proteins produced in nonmammalian cells are significantly different from those produced in mammalian cells (40). Therefore, using delivery vectors for the production of N-glycosylated proteins in target animals could be a promising strategy.
Baculoviruses are attractive vectors for foreign-gene delivery to mammalian cells for their subsequent expression. First, baculoviruses can accommodate large DNA insertions as AcMNPV has a large DNA genome (134 kb) (41). Second, the baculovirus system transiently transduces genes into mammalian cells without DNA integration into the target cell genome, and baculoviruses are replication incompetent in mammalian cells (42). Therefore, the baculovirus vector is safe for use in mammals. Third, baculoviruses are produced in insect cells, but protein expression occurs in mammalian cells. Therefore, compared to viral vectors produced in mammalian cells, they are cost-effective. The baculovirus expression system in insect cells has been widely used for the large-scale production of recombinant proteins (30, 31). Several recombinant-protein vaccines are commercially available, such as a human papillomavirus vaccine (Cervarix; GlaxoSmithKline), a classical swine fever virus vaccine (Porcilis Pesti; MSD Animal Health), and a porcine circovirus type 2 vaccine (Porcilis PCV; MSD Animal Health). Therefore, the scaling-up of baculovirus systems, including BacMam, is no longer a considerable obstacle. Furthermore, unlike proteins produced in insect cells, proteins produced using the BacMam system are N-glycosylated and can be administered directly to animals. The presence of the vesicular stomatitis virus G glycoprotein (VSV-G) on the surface of baculoviruses has been shown to increase their mammalian cell transduction efficacy (43). However, although we did not use this VSV-G-based method here, it can be successfully used for Bac-Con3N IFN-α protein expression in swine cells and animal models. A previous study reported successful BacMam transduction without the use of VSV-G (44). Sodium butyrate is a protein expression enhancer for BacMam (29), and although we did not use it here, its addition could enhance the efficacy of Bac-Con3N IFN-α in vitro and in vivo.
BacMam can be transduced into a wide range of mammalian cells (45). A study on the mechanism of baculovirus entry reported that the baculovirus envelope protein GP64 interacts with phospholipids on the cell surface and mediates its entry into mammalian cells (46–48). In addition, it has been reported that the binding of GP64 with heparan sulfate on the cell surface is essential for baculovirus internalization into mammalian cells (49). Although the receptor responsible for baculovirus entry into mammalian cells has not been identified, it could use ubiquitously distributed molecules for its entry. Therefore, the ability of baculoviruses to be transduced into a wide range of mammalian cells can be a significant advantage for vector delivery in animals. The BacMam delivery system has been used in a recombinant African swine fever (ASF) vaccine (34). Only four out of six pigs immunized using the BacMam vaccine at 107 PFU were protected against ASF virus and had undetectable viremia. However, we used 2 × 1010 and 6 × 1010 PFU Bac-Con3N IFN-α and observed significant antiviral effects in pigs. We speculate that the titers BacMam significantly influence its effects because at a dose of 6 × 1010 PFU, Bac-Con3N IFN-α exerted greater antiviral effects than it did at 2 × 1010 PFU (Table 1). In addition, Bac-Con3N IFN-α is suitable for use alone or in combination with oil-adjuvant-containing inactivated FMD vaccines. We confirmed that Bac-Con3N IFN-α retained its antiviral and adjuvant effects when mixed with ISA 206 and ISA 201 (Seppic, Paris, France), which are commonly used oil adjuvants in inactivated FMD vaccines in mouse experiments (data not shown). We also observed that the antiviral effect of the vaccine formulation with Bac-Con3N IFN-α was significantly superior to that of the vaccine formulation with Bac-Neg con in mice (data not shown). We speculated that the protective effect of the combination of the vaccine and Bac-Con3N IFN-α might be significantly greater than that of the combination of the vaccine and Bac-Neg con in pigs. In addition, the primary motivation of this study was to overcome the limitations of inactivated FMD vaccines. Therefore, we focused on comparing the vaccine group with the combination group (vaccine and Bac-Con3N IFN-α).
The protective effects of the combination of the FMD vaccine and Bac-Con3N IFN-α in vaccinated pigs may be due to the antiviral effects of Bac-Con3N IFN-α and increased virus-neutralizing antibody levels at 7 dpv. We observed early protective effects in pigs injected with the inactivated FMD vaccine and Bac-Con3N IFN-α from 1 to 7 dpv (Table 1), and the neutralizing antibody titers (P < 0.05) increased from 7 dpv in these pigs (Fig. 8). Therefore, we hypothesized that the combination of Bac-Con3N IFN-α and the inactivated FMD vaccine could exert inhibitory effects against FMDV from 1 to a minimum of 35 dpv (5 weeks) without the second vaccination. However, the adjuvant effect of Bac-Con3N IFN-α could be observed after 5 weeks. In addition, further studies are needed on the enhanced neutralizing antibody titers using the combination of a vaccine and Bac-Con3N IFN-α 5 weeks after the second vaccination. Bac-Con3N IFN-α induced various cytokines, including IFN-α, IFN-γ, IL-12, IL-15, IL-6, and IL-18, which are involved in antiviral and immunostimulatory effects in BALB/c mice (Fig. 6). We used BALB/c mice, wherein high cytokine levels can be detected more easily than in C57BL/6 mice (50). IFN-α (type I IFN) and IFN-γ (type II IFN) are effective antiviral agents against FMDV (2). In addition, IL-12 potentiates antiviral effects as it stimulates IFN-γ production and activates natural killer (NK) cells (51–53). Inoculation with Bac-Con3N IFN-α increased the levels of IL-6, IL-12, and IL-15, which are related to B-cell differentiation, and the levels of IL-18 and IL-12, which are related to T-cell immunity (54, 55). In addition, increased IL-12, IL-15, and IL-18 levels were observed in mice inoculated with Bac-Neg con; however, Bac-Con3N IFN-α induced greater cytokine production than Bac-Neg con. Furthermore, IL-12, IL-15, and IL-18 levels increased and remained stable at 6 to 24 h posttreatment in the Bac-Con3N IFN-α and Bac-Neg con groups. These cytokines synergistically induce NK cell activation and IFN-γ production (56). In the Bac-Con3N IFN-α-treated group, IFN-α, IFN-γ, and IL-6 levels increased at 6 h posttreatment and significantly decreased at 24 h posttreatment. Previous studies have reported that live baculoviruses induce B- and T-cell immunity and could act as vaccine adjuvants (37, 57). In addition, IFN-α has been reported to enhance humoral and cell-mediated immunity (58, 59). Increased porcine IFN-α, IFN-γ, and IL-12 levels were also observed in pigs up to 7 dpv (Fig. 7). Therefore, the BacMam system and type I IFN could exert effective synergistic inhibitory effects against FMDV.
In conclusion, we developed a novel antiviral agent and immunostimulator, Bac-Con3N IFN-α. This study presents an effective approach to its use, alone or in combination with an inactivated FMD vaccine, as an anti-FMDV strategy in pigs. In the future, the inhibitory effects of Bac-Con3N IFN-α against other viral diseases and its immunostimulatory effects in pigs could be further evaluated. In addition, our results could promote the use of the BacMam system in veterinary disease prevention and treatment.
MATERIALS AND METHODS
Cells and viruses.
Spodoptera frugiperda Sf9 insect cells (Thermo Fisher Scientific, Waltham, MA, USA) were cultured in Sf-900 II serum-free medium (Thermo Fisher Scientific) and grown at 27°C in a shaking incubator (120 rpm). Porcine kidney (LFBK) cells, supplied by the Plum Island Animal Disease Center (Orient, NY, USA), were cultured in Dulbecco’s modified Eagle’s medium (DMEM; Thermo Fisher Scientific) supplemented with 10% fetal bovine serum (pH 7.4) at 37°C in an incubator with 5% CO2. FMDV O/SKR/2002 (GenBank accession no. AH012984.2) and O/Boeun/SKR/2017 (GenBank accession no. MG983730) were isolated in the Republic of Korea by the Animal and Plant Quarantine Agency (APQA). FMDV O/VIT/2013 (GenBank accession no. KY492067) was isolated by the APQA in the Republic of Korea from field samples provided by the National Center for Veterinary Diagnosis in Vietnam and was adapted to mice. Viral titers were calculated using the Spearman-Karber method as 50% tissue culture infective doses (TCID50) (60).
Design and construction of the baculovirus plasmids.
Cytomegalovirus immediate early (CMV-IE) promoter sequences of pcDNA3 vectors (Thermo Fisher Scientific) were used to establish a construct for protein expression in mammalian cells (29). Porcine IFN-α consensus sequences, as reported previously by Huang et al. (28), were codon optimized for use in pigs. The sequences were edited to ensure three predicted N-glycosylation sites (at the 4th, 23rd, and 78th amino acid positions) with a Thr or Ser residue at position +2 (Asn-X-Thr/Ser) (22). The CMV-IE promoter, the signal sequence encoding the MAPTSAFFTALVLLSCNAICSLG peptide, and consensus porcine IFN-α containing the N-glycosylation sites (Fig. 1A) were synthesized by GeneArt (Thermo Fisher Scientific) and cloned into a pFastBac dual vector (Thermo Fisher Scientific) using restriction endonucleases (SmaI and NheI) to create Bac-Con3N IFN-α. The negative-control baculoviruses (Bac-Neg con) were constructed by cloning the CMV-IE promoter and cleaving with only SmaI and XhoI.
Production of recombinant baculoviruses.
Recombinant baculoviruses were generated according to the manufacturer’s instructions for the Bac-to-Bac baculovirus expression system (Thermo Fisher Scientific). Briefly, cloned pFastBac dual vectors were transformed into DH10Bac competent Escherichia coli cells (Thermo Fisher Scientific), and the recombinant bacmids were verified using PCR and nucleotide sequencing. The recombinant bacmids were then transfected into Sf9 cells using Cellfectin II reagent (Thermo Fisher Scientific) to produce recombinant baculoviruses. The recombinant baculoviruses were harvested from the supernatant, concentrated by centrifugation at 80,000 × g for 75 min in a sucrose solution (25% sucrose in 5 mM NaCl and 10 mM EDTA), and then resuspended in Dulbecco’s phosphate buffered saline (D-PBS). The recombinant baculovirus titers were determined using the BacPAK quantitative PCR (qPCR) titration kit (TaKaRa Bio USA Inc., Mountain View, CA, USA).
Bac-Con3N IFN-α protein detection in mammalian cells using Western blotting.
To evaluate protein expression in mammalian cells, LFBK cells in 25-cm2 culture flasks were inoculated with Bac-Con3N IFN-α or Bac-Neg con at an MOI of 200. At 48 h postinfection, the supernatant was collected and concentrated 10-fold using a 10-kDa Amicon Ultra centrifugal filter unit (Merck, Darmstadt, Germany). The concentrated supernatant was mixed with sample buffer, incubated at 95°C for 5 min, and then cooled on ice for 2 min. To determine the exact molecular weight of the protein, partial samples were treated for 1 h at 37°C with PNGase F (New England BioLabs, Ipswich, MA, USA), which catalyzes the cleavage of internal glycosidic bonds. Western blotting was performed as previously described (61). Swine IFN-α1 polyclonal antibodies produced in goats (Kingfisher Biotech, MN, USA) and rabbit anti-goat IgG(H+L) (horseradish peroxidase [HRP]; Abcam, Cambridge, UK) were used as primary and secondary antibodies, respectively. Detection and imaging analyses were performed using the Pierce ECL Western blotting substrate (Thermo Fisher Scientific) and an ImageQuant LAS 4000 system (GE Healthcare Life Sciences, Chicago, IL, USA) according to the manufacturers’ instructions.
Determination of the antiviral effects of Bac-Con3N IFN-α in swine cells.
LFBK cells were inoculated the following day with recombinant baculoviruses, at an MOI of 50, when they reached 90% confluence. After 18 h, the recombinant baculoviruses were removed, and the cells were washed with DMEM. Next, the cells were inoculated with 100 TCID50 FMDV O/Boeun/SKR/2017 for 1 h, after which the inoculum was removed and DMEM was added to the cells. The cells were then incubated at 37°C for 24 or 48 h, and the supernatants were collected. To evaluate the effects of Bac-Con3N IFN-α on FMDV RNA replication, RNA extraction and quantitative real-time PCR (RT-qPCR) were performed using the supernatant. Viral RNA was extracted using the MagNA Pure 96 automation system (Roche, Basel, Switzerland) and the MagNA Pure 96 DNA and viral NA small-volume kit (Roche, Basel, Switzerland). RT-qPCR was conducted as previously described (62).
FMDV-based IFN biological assay.
An FMDV-based IFN biological assay was performed according to a modified version of a previously described method (2). LFBK cells were grown to 90% confluence and exposed to 2-fold dilutions of porcine IFN-α. After 24 h, the supernatants were removed, and the cells were inoculated with 250 TCID50 FMDV O/SKR/2002 for 1 h and incubated at 37°C for 48 h. The antiviral activity (units) was measured at the highest IFN-α dilution that induced 50% inhibition of the cytopathic effect (CPE). The concentrated supernatants of Bac-Con3N IFN-α-exposed LFBK cells and recombinant porcine IFN-α protein expressed in mammalian cells (R&D Systems, Minneapolis, MN, USA) were used for the assay.
In vitro stability of Con3N IFN-α protein in swine serum.
The in vitro stability of the protein produced from Bac-Con3N IFN-α in mammalian cells was evaluated according to a modified version of a previously described method (23). The same units of the protein produced from Bac-Con3N IFN-α in LFBK cells or the recombinant porcine IFN-α protein expressed in mammalian cells (R&D Systems) were diluted with swine serum at a 1:3 (vol/vol) ratio. Porcine IFN-α mixed with swine serum was incubated at 37°C for 2, 6, 12, 24, or 48 h and then immediately frozen at −80°C. After thawing the samples, the biological activity of IFN-α was measured using the IFN biological assay described above.
Analysis of ISGs in porcine cells.
LFBK cells were inoculated with recombinant baculoviruses at an MOI of 50, 24 h after being plated. Cells were collected at the 6-, 24-, and 48-h time points following inoculation, and RNA extraction, DNase I treatment, and RT-qPCR were performed as previously described (62). For ISG expression level analysis, RT-qPCR was performed to determine the levels of IFN-β, myxovirus resistance (Mx), and 2′-5′-oligoadenylate synthetase (OAS) mRNAs. Primers and dually labeled TaqMan probes (5′-FAM [6-carboxyfluorescein]/3′-BHQ-1 [black hole quencher 1]), designed as previously described (2), were synthesized by Bioneer Corp. (Daejeon, Republic of Korea).
Determining the Bac-Con3N IFN-α antiviral effects in mice.
Seven-week-old female C57BL/6 mice were purchased from Cosa-Bio Co. Ltd. (Sungnam, Republic of Korea). This study was approved by the Animal Care and Use Committee of the APQA (approval number AEC 2018-423), and the experiments were conducted in an animal biosafety level 3 facility at the APQA. To evaluate the effects of Bac-Con3N-poIFN-α against FMDV, mice were intraperitoneally injected with 0.1 mL of PBS (nonvaccinated group), Bac-Neg con, or Bac-Con3N-poIFN-α. Recombinant baculoviruses were used at a titer of 3 × 108 PFU, and five mice were selected for each group. At 1 or 3 dpv, the mice were challenged by administering 0.1 mL of mouse-adapted FMDV O/VIT/2013 at 200 LD50 (50% lethal doses) by intraperitoneal injection (63). All mice were observed for 7 days postchallenge (dpc).
Cytokine assay in mice.
Seven-week-old female BALB/c mice, purchased from Cosa-Bio Co. Ltd. (Sungnam, Republic of Korea), were intraperitoneally injected with 0.1 mL of Bac-Neg con or Bac-Con3N-poIFN-α at a titer of 3 × 108 PFU. Blood was collected from these mice at 0, 6, 16, and 24 hpi, and their sera were used for an enzyme-linked immunosorbent assay (ELISA) using mouse IFN-α (MyBioSource, San Diego, CA, USA), IFN-γ (MyBioSource), IL-12 (MyBioSource), IL-15 (MyBioSource), IL-6 (Thermo Fisher Scientific), and IL-18 (MyBioSource) ELISA kits. The concentration of each protein evaluated was determined by interpolation from standard curves.
FMDV challenge in pigs injected with the FMD vaccine and Bac-Con3N IFN-α.
Nine-week-old YLD (crossbreed of Yorkshire, Landrace, and Duroc) pigs, confirmed to be negative for FMDV-neutralizing antibodies (virus-neutralizing antibody titer of <1:4), were used for FMDV challenge in pigs injected with the FMD vaccine and Bac-Con3N IFN-α (64). Pigs were intramuscularly (i.m.) injected with the FMDV O/SKR/Boeun/2017 vaccine (2 mL/dose), the combination of the vaccine and Bac-Con3N IFN-α, or PBS (65). The vaccine was formulated using the O/SKR/Boeun/2017 vaccine antigen (15 μg/dose), 10% aluminum hydroxide gel (Rehydragel HPA; General Chemical, Moorestown, NJ, USA), and Montanide ISA 206 (Seppic) in a water-in-oil-in-water (W/O/W) emulsion. Pigs were challenged by intradermally injecting them with 1 × 105 TCID50 of FMDV O/SKR/Boeun/2017 that had been passaged twice through the heel bulb of one foot of the pigs at 1, 3, or 7 dpv. Blood samples were collected once every 2 days, and oral swabs were collected daily from 0 to 8 dpc using the BD universal viral transport kit (BD Biosciences, Franklin Lakes, NJ, USA). FMD viral RNA was identified from viral RNA extracted from serum and oral swab samples for RT-qPCR. The Cador Pathogen 96 QIAcube HT kit (Qiagen, Hilden, Germany) was used for viral RNA extraction, and RT-qPCR was conducted as previously described (62). Clinical signs were monitored daily after the challenge and were scored using the following criteria: (i) lameness (1 point); (ii) vesicles in the hoof and foot (1 or 2 points for each affected hoof and foot, except for the intradermally challenged foot); and (iii) vesicles on the snout, lips, or tongue (1 point for each affected area) (maximum of 10 points) (18).
Cytokine assay in swine.
Nine-week-old YLD pigs, confirmed to be negative for FMDV-neutralizing antibodies (virus-neutralizing antibody titer of <1:4), were used for cytokine assays in swine. Three pigs per group were inoculated with the O/SKR/Boeun/2017 vaccine or the vaccine in combination with 4 × 1010 TCID50 of Bac-Con3N-poIFN-α by intramuscular injection, and blood was collected at 0, 3, or 7 dpv. Cytokine assays were performed on the serum samples using porcine IFN-γ (Abcam), IFN-α (PBL Assay Science, Piscataway, NJ, USA), and IL-12/IL-23 P40 (R&D Systems) ELISA kits. The concentration of each protein evaluated was determined by interpolation from standard curves.
Pig vaccination and virus neutralization tests.
Nine-week-old YLD pigs, confirmed to be negative for FMDV-neutralizing antibodies (neutralizing antibody titer of <1:4), were used for pig vaccination and virus neutralization tests. Four pigs per group were intramuscularly injected with the vaccine composed of the vaccine antigen of O/SKR/Boeun/2017 (10 μg/dose), 10% aluminum hydroxide gel (Rehydragel HPA; General Chemical), and Montanide ISA 206, as described in a previous study, or with a mixture of the vaccine and Bac-Con3N-poIFN-α or Bac-Neg con (66). The mixture of the FMD vaccine and baculovirus was prepared by vortexing. Blood samples were collected at 1, 3, 5, 7, and 9 wpv. Serum was separated from the samples and heat inactivated at 56°C for 30 min. The virus-neutralizing antibody test (VNT) was performed according to the guidelines of the Manual of Diagnostic Tests and Vaccines for Terrestrial Animals (67). FMDV O/SKR/Boeun/2017, passaged four times in LFBK cells, was used for the virus neutralization test. A neutralization reaction was performed between serially diluted sera and 100 TCID50 FMDV at 37°C for 1 h. Next, the neutralized viruses were placed onto 96-well microplates, and LFBK cells were added to them. The microplates were incubated at 37°C for 48 to 72 h to assess the CPE. Neutralizing antibody titers were calculated as the reciprocal of the maximum serum dilution that neutralized 100 TCID50 FMDV.
Statistical analysis.
Unpaired t tests were performed using GraphPad Prism software (version 5.0; GraphPad Software, La Jolla, CA, USA). P values of <0.05 were considered statistically significant.
ACKNOWLEDGMENTS
This work was supported by the Animal and Plant Quarantine Agency, Republic of Korea.
We thank Gyeong Gu Jung and So Hui Park for support with cell culture and animal experiments at the APQA.
Conceptualization was performed by S.-M.K. A.K., J.-H.H., and G.L. performed experiments and analyzed data. S.-M.K. and A.K. wrote the original draft. J.-H.P., M.J.L., and B.K. reviewed the draft. All authors approved the final manuscript.
Contributor Information
Su-Mi Kim, Email: beliefsk@korea.kr.
Bryan R. G. Williams, Hudson Institute of Medical Research
REFERENCES
- 1.Alexandersen S, Zhang Z, Donaldson AI, Garland AJM. 2003. The pathogenesis and diagnosis of foot-and-mouth disease. J Comp Pathol 129:1–36. doi: 10.1016/s0021-9975(03)00041-0. [DOI] [PubMed] [Google Scholar]
- 2.Moraes MP, de Los Santos T, Koster M, Turecek T, Wang H, Andreyev VG, Grubman MJ. 2007. Enhanced antiviral activity against foot-and-mouth disease virus by a combination of type I and II porcine interferons. J Virol 81:7124–7135. doi: 10.1128/JVI.02775-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Doel TR. 2003. FMD vaccines. Virus Res 91:81–99. doi: 10.1016/s0168-1702(02)00261-7. [DOI] [PubMed] [Google Scholar]
- 4.Salt JS, Barnett PV, Dani P, Williams L. 1998. Emergency vaccination of pigs against foot-and-mouth disease: protection against disease and reduction in contact transmission. Vaccine 16:746–754. doi: 10.1016/s0264-410x(97)86180-4. [DOI] [PubMed] [Google Scholar]
- 5.Golde WT, Pacheco JM, Duque H, Doel T, Penfold B, Ferman GS, Gregg DR, Rodriguez LL. 2005. Vaccination against foot-and-mouth disease virus confers complete clinical protection in 7 days and partial protection in 4 days: use in emergency outbreak response. Vaccine 23:5775–5782. doi: 10.1016/j.vaccine.2005.07.043. [DOI] [PubMed] [Google Scholar]
- 6.Nagendrakumar SB, Hong NT, Geoffrey FT, Jacqueline MM, Andrew D, Michelle G, Van Phuc K, Ngon QV, Phuong le TT, Phuc NN, Hanh TX, Van Hung V, Quynhanh le T, Tan TM, Long NT, Wilna V. 2015. A Malaysia 97 monovalent foot-and-mouth disease vaccine (>6PD50/dose) protects pigs against challenge with a variant FMDV A SEA-97 lineage virus, 4 and 7 days post vaccination. Vaccine 33:4513–4519. doi: 10.1016/j.vaccine.2015.07.014. [DOI] [PubMed] [Google Scholar]
- 7.Alexandersen S, Donaldson AI. 2002. Further studies to quantify the dose of natural aerosols of foot-and-mouth disease virus for pigs. Epidemiol Infect 128:313–323. doi: 10.1017/s0950268801006501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chinsangaram J, Moraes MP, Koster M, Grubman MJ. 2003. Novel viral disease control strategy: adenovirus expressing alpha interferon rapidly protects swine from foot-and-mouth disease. J Virol 77:1621–1625. doi: 10.1128/jvi.77.2.1621-1625.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim SM, Lee KN, Park JY, Ko YJ, Joo YS, Kim HS, Park JH. 2008. Therapeutic application of RNA interference against foot-and-mouth disease virus in vitro and in vivo. Antiviral Res 80:178–184. doi: 10.1016/j.antiviral.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Jeong KW, Lee JH, Park SM, Choi JH, Jeong DY, Choi DH, Nam Y, Park JH, Lee KN, Kim SM, Ku JM. 2015. Synthesis and in-vitro evaluation of 2-amino-4-arylthiazole as inhibitor of 3D polymerase against foot-and-mouth disease (FMD). Eur J Med Chem 102:387–397. doi: 10.1016/j.ejmech.2015.08.020. [DOI] [PubMed] [Google Scholar]
- 11.Goris N, De Palma A, Toussaint JF, Musch I, Neyts J, De Clercq K. 2007. 2′-C-methylcytidine as a potent and selective inhibitor of the replication of foot-and-mouth disease virus. Antiviral Res 73:161–168. doi: 10.1016/j.antiviral.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 12.Perales C, Agudo R, Tejero H, Manrubia SC, Domingo E. 2009. Potential benefits of sequential inhibitor-mutagen treatments of RNA virus infections. PLoS Pathog 5:e1000658. doi: 10.1371/journal.ppat.1000658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen W, Yan W, Du Q, Fei L, Liu M, Ni Z, Sheng Z, Zheng Z. 2004. RNA interference targeting VP1 inhibits foot-and-mouth disease virus replication in BHK-21 cells and suckling mice. J Virol 78:6900–6907. doi: 10.1128/JVI.78.13.6900-6907.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Choi JH, Jeong K, Kim SM, Ko MK, You SH, Lyoo YS, Kim B, Ku JM, Park JH. 2018. Synergistic effect of ribavirin and vaccine for protection during early infection stage of foot-and-mouth disease. J Vet Sci 19:788–797. doi: 10.4142/jvs.2018.19.6.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.You SH, Kim T, Choi JH, Park G, Lee KN, Kim B, Lee MH, Kim HS, Kim SM, Park JH. 2017. Coinjection of a vaccine and anti-viral agents can provide fast-acting protection from foot-and-mouth disease. Antiviral Res 143:195–204. doi: 10.1016/j.antiviral.2017.04.009. [DOI] [PubMed] [Google Scholar]
- 16.Dias CC, Moraes MP, Weiss M, Diaz-San Segundo F, Perez-Martin E, Salazar AM, de los Santos T, Grubman MJ. 2012. Novel antiviral therapeutics to control foot-and-mouth disease. J Interferon Cytokine Res 32:462–473. doi: 10.1089/jir.2012.0012. [DOI] [PubMed] [Google Scholar]
- 17.Chinsangaram J, Koster M, Grubman MJ. 2001. Inhibition of L-deleted foot-and-mouth disease virus replication by alpha/beta interferon involves double-stranded RNA-dependent protein kinase. J Virol 75:5498–5503. doi: 10.1128/JVI.75.12.5498-5503.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim SM, Park JH, Lee KN, Kim SK, You SH, Kim T, Tark D, Lee HS, Seo MG, Kim B. 2015. Robust protection against highly virulent foot-and-mouth disease virus in swine by combination treatment with recombinant adenoviruses expressing porcine alpha and gamma interferons and multiple small interfering RNAs. J Virol 89:8267–8279. doi: 10.1128/JVI.00766-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Diaz-San Segundo F, Montiel NA, Sturza DF, Perez-Martin E, Hickman D, Ramirez-Medina E, Grubman MJ, de Los Santos T. 2016. Combination of Adt-O1Manisa and Ad5-boIFNλ3 induces early protective immunity against foot-and-mouth disease in cattle. Virology 499:340–349. doi: 10.1016/j.virol.2016.09.027. [DOI] [PubMed] [Google Scholar]
- 20.Moraes MP, Chinsangaram J, Brum MCS, Grubman MJ. 2003. Immediate protection of swine from foot-and-mouth disease: a combination of adenoviruses expressing interferon alpha and a foot-and-mouth disease virus subunit vaccine. Vaccine 22:268–279. doi: 10.1016/S0264-410X(03)00560-7. [DOI] [PubMed] [Google Scholar]
- 21.Diaz-San Segundo F, Medina GN, Azzinaro P, Gutkoska J, Mogulothu A, Attreed SE, Lombardi KR, Shields J, Hudock TA, de Los Santos T. 2021. Use of protein pegylation to prolong the antiviral effect of IFN against FMDV. Front Microbiol 12:668890. doi: 10.3389/fmicb.2021.668890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ceaglio N, Etcheverrigaray M, Kratje R, Oggero M. 2008. Novel long-lasting interferon alpha derivatives designed by glycoengineering. Biochimie 90:437–449. doi: 10.1016/j.biochi.2007.10.013. [DOI] [PubMed] [Google Scholar]
- 23.Ceaglio N, Etcheverrigaray M, Conradt HS, Grammel N, Kratje R, Oggero M. 2010. Highly glycosylated human alpha interferon: an insight into a new therapeutic candidate. J Biotechnol 146:74–83. doi: 10.1016/j.jbiotec.2009.12.020. [DOI] [PubMed] [Google Scholar]
- 24.Varki A. 1993. Biological roles of oligosaccharides: all of the theories are correct. Glycobiology 3:97–130. doi: 10.1093/glycob/3.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goochee CF, Gramer MJ, Andersen DC, Bahr JB, Rasmussen JR. 1991. The oligosaccharides of glycoproteins: bioprocess factors affecting oligosaccharide structure and their effect on glycoprotein properties. Biotechnology (N Y) 9:1347–1355. doi: 10.1038/nbt1291-1347. [DOI] [PubMed] [Google Scholar]
- 26.Katla S, Yoganand KNR, Hingane S, Ranjith Kumar CT, Anand B, Sivaprakasam S. 2019. Novel glycosylated human interferon alpha 2b expressed in glycoengineered Pichia pastoris and its biological activity: N-linked glycoengineering approach. Enzyme Microb Technol 128:49–58. doi: 10.1016/j.enzmictec.2019.05.007. [DOI] [PubMed] [Google Scholar]
- 27.Gowen BB, Ennis J, Russell A, Sefing EJ, Wong MH, Turner J. 2011. Use of recombinant adenovirus vectored consensus IFN-α to avert severe arenavirus infection. PLoS One 6:e26072. doi: 10.1371/journal.pone.0026072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huang L, Cao RB, Wang N, Liu K, Wei JC, Isahg H, Song LJ, Zuo WY, Zhou B, Wang WW, Mao X, Chen PY. 2012. The design and recombinant protein expression of a consensus porcine interferon: coPoIFN-α. Cytokine 57:37–45. doi: 10.1016/j.cyto.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 29.Condreay JP, Witherspoon SM, Clay WC, Kost TA. 1999. Transient and stable gene expression in mammalian cells transduced with a recombinant baculovirus vector. Proc Natl Acad Sci USA 96:127–132. doi: 10.1073/pnas.96.1.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kost TA, Condreay JP. 1999. Recombinant baculoviruses as expression vectors for insect and mammalian cells. Curr Opin Biotechnol 10:428–433. doi: 10.1016/s0958-1669(99)00005-1. [DOI] [PubMed] [Google Scholar]
- 31.Steele KH, Stone BJ, Franklin KM, Fath-Goodin A, Zhang X, Jiang H, Webb BA, Geisler C. 2017. Improving the baculovirus expression vector system with vankyrin-enhanced technology. Biotechnol Prog 33:1496–1507. doi: 10.1002/btpr.2516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hefferon KL, Oomens AG, Monsma SA, Finnerty CM, Blissard GW. 1999. Host cell receptor binding by baculovirus GP64 and kinetics of virion entry. Virology 258:455–468. doi: 10.1006/viro.1999.9758. [DOI] [PubMed] [Google Scholar]
- 33.Ono C, Okamoto T, Abe T, Matsuura Y. 2018. Baculovirus as a tool for gene delivery and gene therapy. Viruses 10:510. doi: 10.3390/v10090510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Argilaguet JM, Pérez-Martín E, López S, Goethe M, Escribano JM, Giesow K, Keil GM, Rodríguez F. 2013. BacMam immunization partially protects pigs against sublethal challenge with African swine fever virus. Antiviral Res 98:61–65. doi: 10.1016/j.antiviral.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 35.Marchal I, Jarvis DL, Cacan R, Verbert A. 2001. Glycoproteins from insect cells: sialylated or not? Biol Chem 382:151–159. doi: 10.1515/BC.2001.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jenkins N, Curling EM. 1994. Glycosylation of recombinant proteins: problems and prospects. Enzyme Microb Technol 16:354–364. doi: 10.1016/0141-0229(94)90149-x. [DOI] [PubMed] [Google Scholar]
- 37.Heinimäki S, Tamminen K, Malm M, Vesikari T, Blazevic V. 2017. Live baculovirus acts as a strong B and T cell adjuvant for monomeric and oligomeric protein antigens. Virology 511:114–122. doi: 10.1016/j.virol.2017.08.023. [DOI] [PubMed] [Google Scholar]
- 38.Hervas-Stubbs S, Rueda P, Lopez L, Leclerc C. 2007. Insect baculoviruses strongly potentiate adaptive immune responses by inducing type I IFN. J Immunol 178:2361–2369. doi: 10.4049/jimmunol.178.4.2361. [DOI] [PubMed] [Google Scholar]
- 39.Solá RJ, Griebenow K. 2009. Effects of glycosylation on the stability of protein pharmaceuticals. J Pharm Sci 98:1223–1245. doi: 10.1002/jps.21504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yehuda S, Padler-Karavani V. 2020. Glycosylated biotherapeutics: immunological effects of N-glycolylneuraminic acid. Front Immunol 11:21. doi: 10.3389/fimmu.2020.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kost TA, Condreay JP, Jarvis DL. 2005. Baculovirus as versatile vectors for protein expression in insect and mammalian cells. Nat Biotechnol 23:567–575. doi: 10.1038/nbt1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kost TA, Condreay JP, Ames RS. 2010. Baculovirus gene delivery: a flexible assay development tool. Curr Gene Ther 10:168–173. doi: 10.2174/156652310791321224. [DOI] [PubMed] [Google Scholar]
- 43.Barsoum J, Brown R, McKee M, Boyce FM. 1997. Efficient transduction of mammalian cells by a recombinant baculovirus having the vesicular stomatitis virus G glycoprotein. Hum Gene Ther 8:2011–2018. doi: 10.1089/hum.1997.8.17-2011. [DOI] [PubMed] [Google Scholar]
- 44.Mansouri M, Bellon-Echeverria I, Rizk A, Ehsaei Z, Cianciolo Cosentino C, Silva CS, Xie Y, Boyce FM, Davis MW, Neuhauss SC, Taylor V, Ballmer-Hofer K, Berger I, Berger P. 2016. Highly efficient baculovirus-mediated multigene delivery in primary cells. Nat Commun 7:11529. doi: 10.1038/ncomms11529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mansouri M, Berger P. 2018. Baculovirus for gene delivery to mammalian cells: past, present and future. Plasmid 98:1–7. doi: 10.1016/j.plasmid.2018.05.002. [DOI] [PubMed] [Google Scholar]
- 46.Salminen M, Airenne KJ, Rinnankoski R, Reimari J, Välilehto O, Rinne J, Suikkanen S, Kukkonen S, Ylä-Herttuala S, Kulomaa MS, Vihinen-Ranta M. 2005. Improvement in nuclear entry and transgene expression of baculoviruses by disintegration of microtubules in human hepatocytes. J Virol 79:2720–2728. doi: 10.1128/JVI.79.5.2720-2728.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kaname Y, Tani H, Kataoka C, Shiokawa M, Taguwa S, Abe T, Moriishi K, Kinoshita T, Matsuura Y. 2010. Acquisition of complement resistance through incorporation of CD55/decay-accelerating factor into viral particles bearing baculovirus GP64. J Virol 84:3210–3219. doi: 10.1128/JVI.02519-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kataoka C, Kaname Y, Taguwa S, Abe T, Fukuhara T, Tani H, Moriishi K, Matsuura Y. 2012. Baculovirus GP64-mediated entry into mammalian cells. J Virol 86:2610–2620. doi: 10.1128/JVI.06704-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wu C, Wang S. 2012. A pH-sensitive heparin-binding sequence from baculovirus gp64 protein is important for binding to mammalian cells but not to Sf9 insect cells. J Virol 86:484–491. doi: 10.1128/JVI.06357-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Koo GC, Gan Y-H. 2006. The innate interferon gamma response of BALB/c and C57BL/6 mice to in vitro Burkholderia pseudomallei infection. BMC Immunol 7:19. doi: 10.1186/1471-2172-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Xu M, Mizoguchi I, Morishima N, Chiba Y, Mizuguchi J, Yoshimoto T. 2010. Regulation of antitumor immune responses by the IL-12 family cytokines, IL-12, IL-23, and IL-27. Clin Dev Immunol 2010:832454. doi: 10.1155/2010/832454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.de Groen RA, Boltjes A, Hou J, Liu BS, McPhee F, Friborg J, Janssen HL, Boonstra A. 2015. IFN-λ-mediated IL-12 production in macrophages induces IFN-γ production in human NK cells. Eur J Immunol 45:250–259. doi: 10.1002/eji.201444903. [DOI] [PubMed] [Google Scholar]
- 53.Konjević GM, Vuletić AM, Mirjačić Martinović KM, Larsen AK, Jurišić VB. 2019. The role of cytokines in the regulation of NK cells in the tumor environment. Cytokine 117:30–40. doi: 10.1016/j.cyto.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 54.Moens L, Tangye SG. 2014. Cytokine-mediated regulation of plasma cell generation: IL-21 takes center stage. Front Immunol 5:65. doi: 10.3389/fimmu.2014.00065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yoshimoto T, Takeda K, Tanaka T, Ohkusu K, Kashiwamura S, Okamura H, Akira S, Nakanishi K. 1998. IL-12 up-regulates IL-18 receptor expression on T cells, Th1 cells, and B cells: synergism with IL-18 for IFN-gamma production. J Immunol 161:3400–3407. [PubMed] [Google Scholar]
- 56.Lusty E, Poznanski SM, Kwofie K, Mandur TS, Lee DA, Richards CD, Ashkar AA. 2017. IL-18/IL-15/IL-12 synergy induces elevated and prolonged IFN-γ production by ex vivo expanded NK cells which is not due to enhanced STAT4 activation. Mol Immunol 88:138–147. doi: 10.1016/j.molimm.2017.06.025. [DOI] [PubMed] [Google Scholar]
- 57.Quattrocchi V, Molinari P, Langellotti C, Gnazzo V, Taboga O, Zamorano P. 2013. Co-inoculation of baculovirus and FMDV vaccine in mice, elicits very early protection against foot and mouth disease virus without interfering with long lasting immunity. Vaccine 31:2713–2718. doi: 10.1016/j.vaccine.2013.03.067. [DOI] [PubMed] [Google Scholar]
- 58.Le Bon A, Schiavoni G, D’Agostino G, Gresser I, Belardelli F, Tough DF. 2001. Type I interferons potently enhance humoral immunity and can promote isotype switching by stimulating dendritic cells in vivo. Immunity 14:461–470. doi: 10.1016/S1074-7613(01)00126-1. [DOI] [PubMed] [Google Scholar]
- 59.Gujer C, Sandgren KJ, Douagi I, Adams WC, Sundling C, Smed-Sörensen A, Seder RA, Karlsson Hedestam GB, Loré K. 2011. IFN-α produced by human plasmacytoid dendritic cells enhances T cell-dependent naïve B cell differentiation. J Leukoc Biol 89:811–821. doi: 10.1189/jlb.0810460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ramakrishnan MA. 2016. Determination of 50% endpoint titer using a simple formula. World J Virol 5:85–86. doi: 10.5501/wjv.v5.i2.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kim SM, Kim SK, Park JH, Lee KN, Ko YJ, Lee HS, Seo MG, Shin YK, Kim B. 2014. A recombinant adenovirus bicistronically expressing porcine interferon-α and interferon-γ enhances antiviral effects against foot-and-mouth disease virus. Antiviral Res 104:52–58. doi: 10.1016/j.antiviral.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 62.Kim SM, Lee KN, Lee SJ, Ko YJ, Lee HS, Kweon CH, Kim HS, Park JH. 2010. Multiple shRNAs driven by U6 and CMV promoter enhances efficiency of antiviral effects against foot-and-mouth disease virus. Antiviral Res 87:307–317. doi: 10.1016/j.antiviral.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 63.Ko MK, Jo HE, Choi JH, You SH, Shin SH, Jo H, Lee MJ, Kim SM, Kim B, Park JH. 2019. Chimeric vaccine strain of type O foot-and-mouth disease elicits a strong immune response in pigs against ME-SA and SEA topotypes. Vet Microbiol 229:124–129. doi: 10.1016/j.vetmic.2018.12.023. [DOI] [PubMed] [Google Scholar]
- 64.Jo HE, Ko MK, Choi JH, Shin SH, Jo H, You SH, Lee MJ, Kim SM, Kim B, Park JH. 2019. New foot-and-mouth disease vaccine, O JC-R, induce complete protection to pigs against SEA topotype viruses occurred in South Korea, 2014-2015. J Vet Sci 20:e42. doi: 10.4142/jvs.2019.20.e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lee G, Hwang JH, Park JH, Lee MJ, Kim B, Kim SM. 2020. Vaccine strain of O/ME-SA/Ind-2001e of foot-and-mouth disease virus provides high immunogenicity and broad antigenic coverage. Antiviral Res 182:104920. doi: 10.1016/j.antiviral.2020.104920. [DOI] [PubMed] [Google Scholar]
- 66.Hwang JH, Lee G, Kim A, Park JH, Lee MJ, Kim B, Kim SM. 2021. A vaccine strain of the A/ASIA/Sea-97 lineage of foot-and-mouth disease virus with a single amino acid substitution in the P1 region that is adapted to suspension culture provides high immunogenicity. Vaccines (Basel) 9:308. doi: 10.3390/vaccines9040308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.OIE. 2018. Chapter 3.1.8: Foot-and-mouth disease (infection with foot and mouth disease virus). In Manual of diagnostic tests and vaccines for terrestrial animals. OIE, Paris, France. http://www.oie.int/fileadmin/Home/eng/Health_standards/tahm/3.01.08_FMD.pdf. [Google Scholar]