Highlights
-
•
The overall adherence to antiretroviral therapy (ART) was 44.6%.
-
•
Clients who spent less time to reach ART sites were less likely to adhere to ART.
-
•
Those who developed side effects were more likely to adhere to ART.
-
•
Those with a high self-efficacy were more likely to adhere to ART.
-
•
Those who received reminders were more likely to adhere to ART.
Keywords: Antiretroviral therapy, HIV/AIDS, Health Belief Model, Ga West Municipality, Ghana
Abbreviations: HIV, Human Immunodeficiency Virus; AIDS, Acquired Immune Deficiency Syndrome; ART, Antiretroviral Therapy; HBM, Health Belief Model
Abstract
Objectives
Antiretroviral therapy (ART) is used to suppress the HIV viral load but requires optimal adherence to be effective. This study examined the factors influencing ART adherence among HIV-positive clients in the Ga West Municipality, Ghana using the Health Belief Model (HBM).
Methods
A facility-based cross-sectional design was adopted among 397 HIV clients aged 18 years and above. Data were collected using an interviewer-administered questionnaire and analysed using Stata version 16.0. Binary logistic regression was performed at the P < 0.05 level.
Results
Adherence to ART was 44.6%. Clients who took less than 30 minutes to reach ART sites were 59% less likely to adhere to ART (odds ratio (OR) 0.41, 95% confidence interval (CI) 0.20–0.82). Clients who thought they lost income when they went to obtain their ART refill were more likely to adhere to ART (OR 1.71, 95% CI 1.04–2.83), as were those who developed side effects (OR 1.74, 95% CI 1.05–2.89) (perceived barriers). Clients who had confidence in their ability to take their medications (self-efficacy) (OR 1.86, 95% CI 1.05–3.31) and those who received reminders from health workers (cues to action) (OR 1.91, 95% CI 1.04–3.53) were more likely to adhere to ART.
Conclusions
Interventions should focus on increasing client confidence in adhering to ART. Providers should be empowered to provide reminders to patients.
1. Introduction
HIV/AIDS is one of the most destructive epidemics the world has ever faced (Reda & Biadgilign, 2012). Although several interventions have been developed to curb the menace of the disease, such as antiretroviral therapy (ART), the level of adherence remains low (Adjei, 2019). ART is a treatment regimen intended to aid HIV-positive clients to live longer and healthier lives and reduce the risk of HIV transmission. These benefits can be achieved only if HIV-positive patients adhere to their medications (≥95% adherence) (World Health Organization, 2019). However, despite the benefits of adherence to ART, most HIV-positive clients often struggle to maintain adherence owing to diverse determinants (Heestermans et al., 2016).
Globally, an estimated 37.9 million people are living with HIV, of whom 23.3 million are accessing ART; this represents a significant increase in treatment of about 7.7 million since 2010 (World Health Organization, 2019; UNAIDS, 2019a). There has also been a decline in AIDS-related mortality worldwide from 1.7 million in 2004 to 770 000 in 2018. This decline in mortality could be due to extended coverage and adherence to ART. Nevertheless, disparities still exist, with the World Health Organization (WHO) African region recording the largest HIV/AIDS prevalence and mortality (World Health Organization, 2019).
The ambitious “90–90–90” target set by the Joint United Nations Programme on HIV/AIDS (UNAIDS) aimed to ensure that from the year 2020, 90% of all people living with HIV (PLHIV) will know their status, 90% of all people diagnosed will receive sustained ART, and 90% of all people receiving ART will have viral suppression (UNAIDS, 2014).
In Africa, 25.7 million people are living with HIV, with only 16.3 million accessing ART services (World Health Organization, 2019). Also, 470 000 deaths are reported in Africa 2018, (World Health Organization, 2019). An estimated 52% of PLHIV live in sub-Saharan Africa (UNAIDS, 2016). A substantial proportion of PLHIV are still not on ART, and the death rate from HIV/AIDS remains high (Kharsany & Karim, 2016). In Western and Central Africa, out of 2.6 million HIV-positive patients on ART, only 39% have suppressed viral loads, implying non-adherence (UNAIDS, 2019b).
An estimated 334 713 (1.69%) persons were living with HIV at the end of 2018 in Ghana (Ghana AIDS Commission, 2019). Out of these, 35.16% of adults aged ≥15 years and 19.9% of those aged <15 years were receiving ART (Ghana AIDS Commission, 2019). According to UNAIDS (UNAIDS, 2019c), a total of 14 000 people died of AIDS-related causes in Ghana, of whom 11 000 were adults aged ≥15 years,. Cross-sectional studies conducted in various regions of Ghana have shown a varied prevalence of ART adherence among HIV clients. For instance, a study conducted among HIV patients in the Upper West Regional Hospital found that 62.2% of the HIV clients were adherent to their treatment regimen (Obirikorang et al., 2013). Studies conducted in the Sunyani Municipality (Yarney et al., 2016) and the Cape Coast Metropolis (Prah et al., 2018) reported 75.0% and 79.5% ART adherence, respectively.
Several studies conducted among PLHIV have found numerous factors that are likely to influence adherence to ART among HIV-positive patients on this treatment. These factors include side effects of the medications (Legesse & Reta, 2019), distance to the ART centre (Mengistie et al., 2018), stigma and discrimination (Afolabi et al., 2009; Lyimo et al., 2012), alcohol or substance use (Do et al., 2010; Yaya et al., 2014), and non-disclosure of HIV status (Legesse & Reta, 2019; Yaya et al., 2014; Prah et al., 2018). However, due to differences in demographic characteristics, geographical setting, and health system dynamics, it is important that the factors influencing ART adherence among HIV patients are investigated in different regions to aid in improving adherence in those particular areas. This study was performed to investigate the factors influencing ART adherence in Ga West Municipality, using the Health Belief Model (HBM) as the theoretical framework. This municipality was chosen for the study due to the high number of PLHIV who were lost to follow-up in 2019: overall, 640 PLHIV who were on ART were lost to follow-up (Ga West Municipal Health Directorate, 2019). Hence, it was considered necessary to perform this study to ascertain factors that could hinder PLHIV on ART from adhering to the treatment regimen, as well as the facilitators of ART adherence. Findings from the study will provide information to fill the literature gap and assist the Ministry of Health and other major stakeholders in policy-making and reviewing guidelines on HIV management.
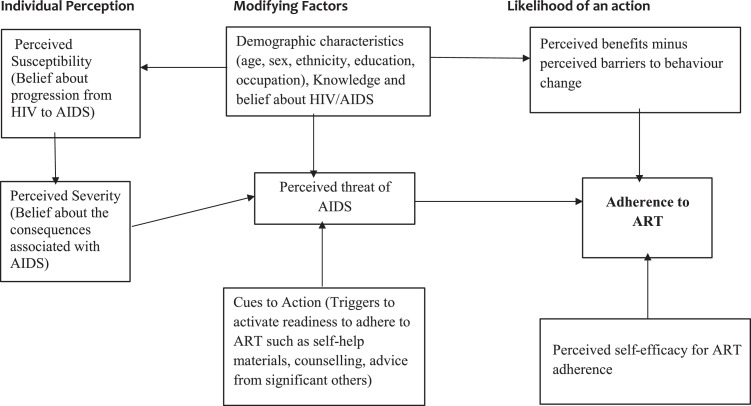
The HBM is one of the most widely used conceptual frameworks in health behaviour research and health behaviour interventions (Champion & Skinner, 2008). The HBM posits that the likelihood of taking the recommended preventive health action is determined by factors that may increase the possibility of practicing the appropriate health behaviour (Hochbaum et al., 1952). These factors include perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, perceived self-efficacy, and modifying factors. The theory has been used to explain HIV and factors influencing adherence to ART in several studies (Vitalis, 2017; Vitalis, 2021; Ssewaya, 2011). The aim of the current study was to determine the factors influencing ART adherence among HIV patients in the Ga West Municipality based on the constructs of the HBM (Figure 1).
Figure 1.
Health Belief Model conceptual framework.
The following hypotheses derived from the HBM were tested in the current study:
Hypothesis 1: Perceived susceptibility will be positively associated with ART adherence.
Hypothesis 2: Perceived severity will be positively associated with ART adherence.
Hypothesis 3: Perceived benefit will be positively associated with ART adherence.
Hypothesis 4: Perceived barriers will be negatively associated with ART adherence.
Hypothesis 5: Cues to action will be positively associated with ART adherence.
Hypothesis 6: Perceived self-efficacy will be positively associated with ART adherence.
2. Materials and methods
2.1. Study site description
The study was conducted in Ga West Municipality, one of the 16 metropolis/municipalities/districts in the Greater Accra region of Ghana. Amasaman is the administrative capital (Ghana Statistical Service, 2014). The Municipality shares boundaries with Ga East and the Accra Metropolis to the east, Akwapim South to the north, Ga South to the south and Ga Central to the north-south. According to the 2010 Population and Housing Census, the Municipality has an estimated population of 219 788, with 51.0% being female (Ghana Statistical Service, 2014). Regarding health facilities that offer ART services, Ga West Municipal Hospital, Mayera Faase Health Centre, Oduman Health Centre, and Pokuase Health Centre have been designated to deliver ART services in the Municipality.
2.2. Study design
The study employed a facility-based cross-sectional design and was conducted in June 2021. This study design was chosen due to its ability to collect data at one point in time and tends to measure outcome and exposure variables within the specified study population.
2.3. Study population
The study included PLHIV aged ≥18 years who were on ART in Ga West Municipality.
2.4. Inclusion and exclusion criteria
The inclusion criteria were as follows: person with HIV, age ≥18 years, on ART for at least 6 months, and consent to participate. The study excluded PLHIV who were critically ill or on admission during the data collection.
2.5. Sample size determination
The sample size for the study was determined using the formula; n = (Snedecor & Cochran, 1989), where n = the required sample size, z = reliability coefficient (z-score) of 1.96 at the 95% confidence level, p = estimated proportion of PLHIV who adhered to ART from a study conducted in the Upper West Regional Hospital, Ghana (62.2%) (Obirikorang et al., 2013), d = margin of error of 5% (0.05), and q = 1 – p, termed the proportion who do not adhere to ART. The estimated sample size was calculated as follows:
Adjusting for a 10% non-response rate (10% of 361.3 = 36.13), the minimum sample size for the study was estimated as 361.3 + 36.13 = 397.4. Therefore, the sample size for the study was set at 397.
2.6. Sampling method
A multistage sampling method was used. The first step involved purposive sampling of all four ART centres in Ga West Municipality. These centres are Ga West Municipal Hospital, Mayera Faase Health Centre, Oduman Health Centre, and Pokuase Health Centre.
A systematic random sampling technique was used to recruit participants into the study from the various ART centres. A list of all HIV-positive patients receiving ART was obtained from the ART centre. Based on the data that were received from the ART centre, a list was created for all of the ART clients who visited the facility for ART services by assigning them serial numbers. The sampling interval (kth) was obtained by dividing the total number of ART clients by the sample size for that ART site. Pieces of papers of equal size were numbered from 1 to kth, placed in a box, and thoroughly shaken to mix.
A piece of paper was blindly selected from the box to determine the start point on the list for selecting participants for the study. The randomly selected number (nth) between 1 and kth was the start point from which every kth client on the list was selected until the required sample size for that site was reached. Any ART client selected was interviewed if they met the inclusion criteria and gave consent. If a person selected to decline to participate, the next person was selected to meet the sample size for that site. This step was repeated at the remaining ART centres to select participants for inclusion in the study.
2.7. Data collection instrument and procedures
Before the data collection began, the ART clients were sensitized on the study for 1 month by the heads of the ART centres where data were collected, for mobilization purposes. The clients were not compensated for participating in the study. Since the ART providers at the various centres assisted with data collection, none of the clients that were approached for the study declined to participate. A structured interviewer-administered questionnaire was used to collect data from the study respondents. The questionnaire was adapted from previous studies (Ssewaya, 2011; Tarkang & Pencille, 2018; Tarkang et al., 2011) and structured into demographic characteristics, ART adherence, and factors that influence ART adherence based on the constructs of the HBM. The questionnaire was pretested among HIV-positive patients who were not part of the study.
The principal investigator trained three research assistants to help in the data collection. The data collection took place at the selected ART centres in a private room to help ensure confidentiality. The questionnaire took 15–30 minutes to complete. At the end of every data collection session, all of the questionnaires were reviewed for accuracy and completeness. This process was continued until the sample size for the study was attained.
2.8. Study variables
ART adherence was the dependent variable in the study. Adherence was defined as taking all prescribed antiretroviral medications following the initiation of highly active antiretroviral therapy (HAART) at the correct doses, at the prescribed time intervals, and in the correct manner, observing any dietary restrictions, and at least 95% of the time. The independent variables consisted of the modifying factors (sociodemographic characteristics) and the constructs of the HBM. The items under each construct of the HBM were measured on a 4-point Likert scale (strongly agree, agree, disagree, and strongly disagree). During the analysis, strongly agree and agree were classified as agree, and strongly disagree and disagree were classified as disagree.
The reliability of the data collection instrument was tested using Cronbach's alpha and by pretesting. With regard to the analyses conducted to test the hypotheses, all calculations were accompanied by reliability coefficients, as shown in Table 3.
Table 3.
Association between individual perceptions and ART adherence level
| Model component | LR Chi-square | df | P-value | Pseudo R-square | Explanatory power of the model | Reliability analysis (alpha) |
|---|---|---|---|---|---|---|
| Perceived threat | 0.72 | 1 | 0.400 | 0.13 | 13.0% | 0.8798 |
| Perceived benefit | 0.00 | 1 | 0.965 | 0.00 | 0% | 0.8437 |
| Perceived barrier | 0.44 | 1 | 0.510 | 0.10 | 10% | 0.6176 |
| Cues to action | 2.28 | 1 | 0.134 | 0.42 | 42.0% | 0.5460 |
| Perceived self-efficacy | 0.19 | 1 | 0.666 | 0.30 | 30% | 0.6350 |
| Modifying factors | 92.65 | 3 | 0.012* | 0.357 | 35.7% | 0.6637 |
| Integrated value mapping (IVM) (combination of all models excluding modifying factors) | 3.46 | 5 | 0.119 | 0.64 | 64.0% | 0.6637 |
ART, antiretroviral therapy; df, degrees of freedom; LR, likelihood ratio. *P < 0.05.
Cronbach's alpha coefficients were calculated using the best combination of items under each construct of the HBM and most of the scores were adequate (0.64–0.85). However, it is important to note that according to Polit and Beck (2004), the following characteristics of the measurement situation can affect the value of Cronbach's alpha obtained:
-
•
The coefficient alpha does not provide a very good estimate when the items making up the measurement scale are heterogeneous in their relationship to each other or when their number is small. The more items the instrument contains the more accurate the alpha coefficient.
-
•
Cronbach's alpha increases with the spread of variance of scores. A low reliability coefficient may also be due to the homogeneity of the sample. The more homogeneous the sample is, the lower is Cronbach's alpha coefficient.
-
•
The alpha coefficient is a function of test length. The longer the test, the higher the level of alpha. Cronbach's alpha is lower when a response with two possible answers is used. The coefficient is improved when a Likert scale response option is used.
The lower reliability coefficients observed for the modifying factors and cues to action could be due to these characteristics. Therefore, Cronbach's alpha showed that the combination of the questions and items for measuring the constructs of the HBM had adequate reliability based on Taber's interpretation (Taber, 2018).
2.9. Statistical analyses
The data analysis was performed using Stata software version 16.0. Binomial logistic regression and likelihood ratio tests were performed to examine the association between ART adherence and the HBM constructs. The regression analysis results were presented in a tabular format using log-likelihood ratios, Chi-square, and pseudo-R-square. A P-value of 0.05 or less was considered statistically significant. The results of the regression analysis were presented using the odds ratio (OR) with the respective 95% confidence interval (CI).
3. Results
3.1. Sociodemographic characteristics of respondents
Table 1 presents the sociodemographic characteristics of the respondents. The majority (41.3%) were under 30 years of age. Furthermore, the majority of the respondents were married (n = 175, 44.1%), and Christian by religion (n = 331, 83.4%). By ethnic group, most respondents were Ewe/Guan (n = 150, 37.8%). Thirty-seven percent (n = 147) had attained a secondary level of education. Most of the respondents received a monthly income of GH₵ 1000 or less (n = 206, 51.9%), were female (n = 204, 51.4%), resided in urban areas (n = 298, 75.1%), and had children (n = 246, 62.0%). The means of transport was dominantly a vehicle (n = 351, 88.4%), and it took the majority of the respondents at most 30 minutes to reach the facility (n = 140, 35.3%).
Table 1.
Sociodemographic characteristics (N = 397)
| Variable | Frequency (n) | Percentage (%) |
|---|---|---|
| Age (years) | ||
| <30 | 164 | 41.3 |
| 30–39 | 123 | 40.0 |
| >40 | 110 | 27.7 |
| Sex | ||
| Female | 204 | 51.4 |
| Male | 193 | 48.6 |
| Marital status | ||
| Never married | 142 | 35.8 |
| Married | 175 | 44.1 |
| Divorced | 21 | 5.3 |
| Widow | 16 | 4.0 |
| Cohabiting | 43 | 10.8 |
| Religion | ||
| Christianity | 331 | 83.4 |
| Islam | 44 | 11.1 |
| African traditional | 22 | 5.5 |
| Ethnicity | ||
| Ewe/Guan | 150 | 37.8 |
| Ga/Dangbe | 100 | 25.2 |
| Akan | 126 | 31.7 |
| Mole-Dagbani | 21 | 5.3 |
| Educational level | ||
| No formal education | 108 | 27.2 |
| Primary education | 73 | 18.4 |
| Secondary education | 147 | 37.0 |
| Tertiary | 69 | 17.4 |
| Income (GH₵) | ||
| ≤300 | 133 | 33.5 |
| ≤1000 | 206 | 51.9 |
| ≥2000 | 58 | 14.6 |
| Occupation | ||
| Unemployed | 56 | 14.1 |
| Government | 65 | 16.4 |
| Self-employed | 204 | 51.4 |
| Private employee | 72 | 18.1 |
| Children | ||
| Yes | 246 | 62.0 |
| No | 151 | 38.0 |
| Settlement type | ||
| Urban | 298 | 75.0 |
| Rural | 15 | 3.8 |
| Sub-rural | 84 | 21.2 |
| Distance (meters) | ||
| <186 | 11 | 2.8 |
| 186 | 386 | 97.2 |
| Transport means | ||
| Vehicle | 351 | 88.4 |
| Walking | 46 | 11.6 |
| Time to reach ART site (minutes) | ||
| <30 | 43 | 10.8 |
| 30 | 140 | 35.3 |
| 30–50 | 113 | 28.5 |
| 60 | 101 | 25.4 |
ART, antiretroviral therapy.
3.2. Antiretroviral therapy adherence
The results showed that 44.6% of the respondents were ART adherent.
3.3. Individual perceptions influencing ART adherence based on the HBM
The results of the items under the various constructs of the HBM (perceived threat, perceived benefit, perceived barrier, perceived self-efficacy, and cues to action) are presented in Table 2. In all, the majority (n = 346, 87.2%) had a high perceived threat, the majority (n = 334, 84.1%) had a high perceived benefit, most (n = 282, 71.0%) had a high perceived barrier, the majority (n = 308, 77.6%) had a high perceived self-efficacy, and the majority (n = 306, 77.1%) had a high cue to action (Table 2).
Table 2.
Individual perceptions influencing ART adherence based on the Health Belief Model (N = 397)
| Variable | Frequency (n) | Percentage (%) |
|---|---|---|
| Perceived threat | ||
| Refusal to attend ART is a serious risk | ||
| Disagree | 33 | 8.3 |
| Agree | 364 | 91.7 |
| Refusal to adhere leads to getting AIDS faster | ||
| Disagree | 39 | 9.8 |
| Agree | 358 | 90.2 |
| Severe consequences due to non-adherence | ||
| Disagree | 48 | 12.1 |
| Agree | 349 | 87.9 |
| Irregular intake of drugs can lead to death | ||
| Disagree | 33 | 8.3 |
| Agree | 364 | 91.7 |
| Non-adherence is life-threatening | ||
| Disagree | 38 | 9.6 |
| Agree | 359 | 90.4 |
| Perceived threat | ||
| No perceived threat | 51 | 12.8 |
| Perceived threat | 346 | 87.2 |
| Perceived benefits | ||
| Following a treatment plan can make me healthy | ||
| Disagree | 34 | 8.6 |
| Agree | 363 | 91.4 |
| Following a treatment plan can reduce viral load | ||
| Disagree | 37 | 9.3 |
| Agree | 360 | 90.7 |
| Adhering to ART improves the condition | ||
| Disagree | 35 | 8.2 |
| Agree | 362 | 91.2 |
| Strict adherence to a treatment plan is crucial | ||
| Disagree | 58 | 14.6 |
| Agree | 339 | 85.4 |
| Perceived benefit | ||
| No perceived benefit | 63 | 15.9 |
| Perceived benefit | 334 | 84.1 |
| Perceived barriers | ||
| I develop side effects | ||
| Disagree | 82 | 20.6 |
| Agree | 315 | 79.4 |
| Lots of time spent for a refill | ||
| Disagree | 103 | 25.9 |
| Agree | 294 | 74.1 |
| Expensive transportation cost | ||
| Disagree | 105 | 26.4 |
| Agree | 292 | 73.6 |
| ART still effective without regular use | ||
| Disagree | 107 | 26.9 |
| Agree | 290 | 73.1 |
| Lose income | ||
| Disagree | 84 | 21.2 |
| Agree | 313 | 78.8 |
| Perceived barrier | ||
| No perceived barrier | 115 | 29.0 |
| Perceived barrier | 282 | 71.0 |
| Self-efficacy | ||
| Recommended ART plan not difficult | ||
| Disagree | 51 | 12.8 |
| Agree | 346 | 87.2 |
| Confident to take all my ART | ||
| Disagree | 149 | 37.5 |
| Agree | 248 | 62.5 |
| Self-discipline to adhere to ART | ||
| Disagree | 85 | 21.4 |
| Agree | 312 | 78.6 |
| ART adherence despite side effects | ||
| Disagree | 62 | 15.6 |
| Agree | 335 | 84.4 |
| Self -efficacy | ||
| Low self-efficacy | 89 | 22.4 |
| High self-efficacy | 308 | 77.6 |
| Cues to action | ||
| Know friend or family who died of HIV | ||
| Disagree | 80 | 20.2 |
| Agree | 317 | 79.9 |
| Know friend or family who died of HIV due to non-adherence | ||
| Disagree | 52 | 13.1 |
| Agree | 345 | 86.9 |
| Reminders from health workers for a refill | ||
| Disagree | 54 | 13.6 |
| Agree | 343 | 86.4 |
| Cues to action | ||
| No perceived cues | 91 | 22.9 |
| Perceived cues | 306 | 77.1 |
ART, antiretroviral therapy.
3.4. Logistic regression analysis of the outcome variable: ART adherence
Model estimation focused on mapping the significant drivers of a patient's adherence to ART from a vector of consistently significant components suggested by the HBM. The binomial logistic model proposed by Agresti (2007) was used. The dependent variable (ART adherence) remained the same for all of the modelling alternatives (the various constructs of the HBM and the integrated value mapping (IVM)). For specific values of the independent variables (the various constructs of the HBM), the corresponding estimated P-value was the probability of the event that respondents adhered to ART. So the alternative values of the regressors could be used in the estimated component to predict the probability of adhering to ART (Table 3).
All of the constructs of the HBM including the IVM had a Cronbach alpha above 0.5. The highest explanatory power of the model was recorded in the IVM (combination of all models) (64.0%), followed by cues to action (42%), then modifying factors (35.7%), self-efficacy (30.0%), perceived threat (13.0%), and perceived barriers (10.0%). The results of the Chi-square statistics showed significance only for the modifying factors (P = 0.012) (Table 3).
Even though, generally, perceived barriers, perceived self-efficacy, and cues to action were not significantly associated with ART adherence (Table 3), some items under these constructs were significantly associated with ART adherence (Table 4). The log-likelihood ratio test indicated that people who thought they lost income when going to obtain their ART refill were more likely to adhere to ART (OR 1.71, 95% CI 1.04–2.83; P = 0.036), as were those who developed side effects (OR 1.74, 95% CI 1.05–2.89; P = 0.032) (perceived barriers). Also, those who had the confidence to take their medications (perceived self-efficacy) (OR 1.86, 95% CI 1.05–3.31; P = 0.034) and those who received reminders from service providers (cues to action) (OR 1.91, 95% CI 1.04–3.53; P = 0.038) were more likely to adhere to ART.
Table 4.
Likelihood ratio test of the items under each construct of the Health Belief Model to ART adherence
| Variables | −2 Log likelihood of reduced model | Chi-square (P-value) | COR (95% CI) (P-value) | df |
|---|---|---|---|---|
| Perceived threat | ||||
| Refusal to attend ART is a serious risk | 271.741 | 1.01 (0.315) | 1 | |
| Refusal to adhere leads to getting AIDS faster | 271.567 | 1.36 (0.244) | 1 | |
| Severe consequences due to non-adherence | 272.153 | 0.20 (0.652) | 1 | |
| Irregular intake of drugs can lead to death | 271.741 | 1.01 (0.315) | 1 | |
| Non-adherence is life-threatening | 272.198 | 0.11 (0.735) | 1 | |
| Perceived benefits | ||||
| Following treatment plan can make me healthy | 271.578 | 1.33 (0.249) | 1 | |
| Following treatment plan can reduce viral load | 271.862 | 0.78 (0.378) | 1 | |
| Adhering to ART improves condition | 271.395 | 1.68 (0.194) | 1 | |
| Strict adherence to treatment plan is crucial | 272.2.7 | 0.09 (0.758) | 1 | |
| Perceived barriers | ||||
| I develop side effects | 269.885 | 4.66 (0.031) | 1.74 (1.05–2.89) (0.032*) | 1 |
| Lots of time spent for refill | 272.075 | 0.36 (0.549) | 1 | |
| Expensive transportation cost | 272.197 | 0.12 (0.733) | 1 | |
| ART still effective without regular use | 272.205 | 0.10 (0.753) | 1 | |
| Lose income | 263.985 | 1.46 (0.035) | 1.71 (1.04–2.83) (0.036*) | 1 |
| Self-efficacy | ||||
| Recommended ART plan not difficult | 272.170 | 0.17 (0.682) | 1 | |
| Confident to take all my ART | 272.170 | 0.84 (0.358) | 1 | |
| Self-discipline to adhere to ART | 271.834 | 0.54 (0.461) | 1 | |
| ART adherence despite side effects | 269.898 | 4.60 (0.032) | 1.86 (1.04–3.31) (0.034*) | 1 |
| Cues to action | ||||
| Know friend or family who died of HIV | 272.656 | 0.19 (0.276) | 1 | |
| Know friend or family who died of HIV due to non-adherence | 272.000 |
2.46 (0.117) | 1 | |
| Reminders from health workers for a refill | 269.985 | 4.42 (0.036) | 1.91 (1.04– 3.53) (0.038*) | 1 |
ART, antiretroviral therapy; CI, confidence interval; COR, crude odds ratio; df, degrees of freedom. *P < 0.05.
3.5. Association between modifying factors and ART adherence
The results of the likelihood ratio test showed that people who took less than 30 minutes to reach their ART site were 59% less likely to adhere to ART (OR 0.41, 95% CI 0.20–0.82; P = 0.012) (Table 5).
Table 5.
Modifying factors (demographic factors): likelihood ratio test
| Variables | −2 Log likelihood of reduced model | OR (95% CI) (P-value) | Chi-square | df | P-value |
|---|---|---|---|---|---|
| Age | 271.13 | 2.25 | 2 | 0.324 | |
| Sex | 270.53 | 3.45 | 1 | 0.063 | |
| Marital status | 271.63 | 1.25 | 4 | 0.870 | |
| Religion | 272.00 | 0.51 | 2 | 0.775 | |
| Ethnicity | 271.70 | 1.11 | 3 | 0.775 | |
| Educational level | 271.92 | 0.67 | 3 | 0.881 | |
| Income | 272.17 | 0.18 | 2 | 0.915 | |
| Occupation | 271.99 | 0.54 | 3 | 0.911 | |
| Children | 271.82 | 0.88 | 1 | 0.348 | |
| Settlement type | 270.73 | 3.05 | 2 | 0.218 | |
| Distance | 271.61 | 0.92 | 4 | 0.921 | |
| Transport means | 271.62 | 1.26 | 1 | 0.261 | |
| Time to reach ART site <30 min |
262.55 | 0.41 (0.20–0.82) (0.012*) | 19.00 | 3 | <0.001** |
| Duration on ART | 272.23 | 0.05 | 2 | 0.977 |
ART, antiretroviral therapy; CI, confidence interval; df, degrees of freedom; OR, odds ratio. *P < 0.05; **P < 0.001.
4. Discussion
4.1. Adherence to ART
The current study found the level of ART adherence to be 44.6%. This finding is similar to those of studies conducted in Ghana, with a reported 47.5% level of ART adherence (Nichols et al., 2019), and Nigeria, with a reported 42.0% adherence (Afe et al., 2017). In contrast, other studies conducted both within Ghana and other countries have reported a higher ART adherence. For instance, a study conducted in Southwest Ethiopia found the level of adherence to be 63.8% (Azagew et al., 2020). Another study conducted in Nigeria found the level of ART adherence to be 79.2% (Onyekwere, 2013). Among the studies conducted in Ghana, the level of ART adherence among HIV-positive clients was 79.5% in Cape Coast (Prah et al., 2018), 75% in Brong-Ahafo Region (Yarney et al., 2016), and 62.2% in Kumasi (Obirikorang, et al., 2013).
The finding of this study implies that most PLHIV are not regularly going for their ART medications or do not take them regularly as scheduled. Hence the viral load of these individuals may remain relatively high. Therefore, adherence to ART should be emphasized, especially during counselling sessions, as it is required for an optimal clinical response and complete viral suppression (Oku et al., 2013). It should be noted that the collection of the data during the COVID-19 pandemic era could have impacted the outcome of the study, since the pandemic negatively affected the management of chronic diseases in diverse settings due to the burden on the health systems, as well as the risk of persons with compromised immune systems contracting the coronavirus (Fernandes et al., 2021).
4.2. Factors associated with ART adherence based on the constructs of the HBM
In the current study, four constructs of the HBM were significantly associated with ART adherence: modifying factors, perceived barriers, cues to action, and perceived self-efficacy.
In contrast to earlier findings that the shorter the distance to the ART site, the higher the adherence level (Shigdel et al., 2014; Wasti et al., 2012), the current study found an inverse association. This finding may be due to the issue of procrastination as a result of the proximity of the clients to the ART centres, which could eventually lead to forgetfulness. Also, if the clients did not feel ill after missing an appointment, they could begin to relapse from adhering to the medication. People who spend less than 30 minutes reaching the ART site are assumed to be those who live or stay close to the ART clinic. These people, due to stigmatization, might avoid going for their medications at the nearby ART centres, leading to a lower likelihood of ART adherence. Further studies, possibly qualitative studies, should be conducted to explore the plausible reasons behind this current finding.
Regarding perceived barriers, clients who experienced side effects of the medications failed to adhere to the treatment regimen, as reported in several studies (Legesse & Reta, 2019; Mengistie et al., 2018; Zhang et al., 2016; Wasti et al., 2012). Contrary to these findings, PLHIV in the current study adhered to ART despite the side effects and this could be attributed to the confidence they have in the suppression of their viral load when they adhere to ART. This finding of the current study implies that in the presence of medication side effects, quality client education and counselling could be a pivotal means of instigating client confidence in adhering to ART.
Additionally, PLHIV were more likely to adhere to their treatment regimen despite the loss of income, as found in the current study. This finding is contrary to those of previous studies, which have reported that a scarcity of resources and income were negatively associated with ART adherence (Dorcélus et al., 2021; Becker et al., 2020). Although ART is given free of charge, financial and other resources are lost in attempts to obtain or access the medications. Yet, PLHIV receiving ART in Ga West Municipality adhered to ART despite the income loss incurred daily, and this could be linked to the perceived efficacy of adhering to the medications to reduce their viral load, enabling them to live a normal life and prolong their lifespan when compared to not taking the medications. According to the assumptions of the HBM, clients who perceive or experience barriers to ART adherence will adhere to their treatment only if the confidence in their ability to adhere to the treatment (self-efficacy) is enhanced (Champoin & Skinner, 2008). This can be done by giving reassurance, skills, and incentives, and correcting misperceptions. The promotion of self-efficacy is thus an important task in achieving ART adherence among clients in the current study.
Clients who received reminder messages (cues to action) from service providers were more likely to adhere to ART. Similar findings were reported in Ghana (Shigdel et al., 2014; Prah et al., 2018). This result further supports the assertion that regular follow-up from clinicians is associated with ART adherence (Negesa et al., 2017). A plausible explanation for this finding might be that the reminder messages prompt the client's assertiveness to take their medications (Prah et al., 2018). This finding highlights the use of reminder tools in ensuring ART adherence and should be encouraged in chronic disease management. Based on the assumptions of the HBM, if clients in the current study are not motivated by the threat of AIDS to adhere to their medication, an intense stimulus (reminder messages) is needed as a cue to action to prompt them to adhere to their medication.
The confidence to take medication despite the side effects (perceived self-efficacy) was positively associated with ART adherence in the current study. This finding supports those of other studies (Zhang et al., 2016). Self-efficacy is an important motivator that enhances people's task performances (Themanson & Rosen, 2015; Bandura, 1989). Clients with strong self-efficacy may be more active and persistent in making efforts to follow their medical provider's instructions (Buchmann, 1997). Although medication side effects may influence ART non-adherence, adherence self-efficacy, which includes the ability to overcome side effects, appears to supress the influence of side effects and enhance patient willingness to follow the instructions and thus remain adherent to ART. Awareness and education on the means to practically overcome the side effects of ART should be the focus in raising the level of adherence among the PLHIV in Ga West Municipality. The results of the current study are in line with the assumptions of the HBM. Therefore, the hypotheses that perceived self-efficacy and cues to action will be positively associated with ART adherence are accepted at the 0.05 level of significance.
4.3. Limitations of the study
First, the cross-sectional nature of the study does not allow a causal relationship between ART adherence and the constructs of the HBM to be established. Second, respondents possibly withheld information from the data collectors and hence the true reflection of their ART adherence and the possible hindrances might not be established. Due to the sensitive nature of the study, social desirability bias might have prevailed. Another possible limitation of the current study is the Hawthorne effect; simply because the participants knew that they were subjects in a study, they may have answered questions or performed differently. However, the assurance of confidentiality might have mitigated these limitations.
4.4. Conclusions
ART adherence in Ga West Municipality was found to be low. Factors influencing ART adherence were the time to the ART centre (sociodemographic variable), side effects of the medications, income (perceived barriers), reminder messages from health workers (cues to action), and confidence in medication adherence despite the side effects (self-efficacy). Health promotion interventions to enhance ART adherence in Ga West Municipality should focus on providing cues to action and increasing the self-efficacy for ART adherence.
Author contributions
Mavis Kessewa Addo and Elvis Enowbeyang Tarkang conceived and designed the study. Richard Aboagye and Elvis Tarkang analysed the data. Mavis Addo collected the data. Mavis Addo, Richard Aboagye, and Elvis Tarkang led the writing of the manuscript and critically reviewed the manuscript. All authors read and approved the final manuscript.
Declarations
Funding: This study was funded by the authors.
Ethical approval: Ethical approval was obtained from the University of Health and Allied Sciences Research Ethics Committee (UHAS-REC A.9[181]2021), Ho before the start of the study. Institutional permission was sought from the Ga West Municipal Health Directorate, the Municipal Hospital, and all of the ART centres before the data collection. The principal investigator ensured that no names, phone numbers, addresses, or any identifiable information that could be traced to any participant were captured on the questionnaires. Unique codes were assigned to each participant and were used for the analysis. Confidentiality was ensured by not disclosing information about participants to anybody. All of the study procedures were clearly explained to the participants in a language they could easily understand in the informed consent. Participation and withdrawal were voluntary. There were no risks associated with participating in this study. All COVID-19 protocols were adhered to during the data collection.
Conflict of interest: The authors declare that they have no conflict of interest.
References
- Adjei B. 2019. Knowledge of People Living with HIV and Its Effect on Adherence to Antiretroviral Therapy in the New Juabeng Municipality (Doctoral dissertation University of Ghana) [Google Scholar]
- Afe J.A., Motunrayo O., Gbadebo O.O. Explaining Adherence to HAART among Patients Living with HIV/AIDS in Nigeria. Behavioral Theory Analysis. Clin Immunol Res. 2017;1(1):1–8. [Google Scholar]
- Afolabi M.O., Ijadunola K.T., Fatusi A.O., Olasode O.A. Determinants of adherence to antiretroviral drugs among people living with HIV/AIDS in the Ife-Ijesa zone of Osun state, Nigeria. African Journal of Primary Health Care & Family Medicine. 2009;1(1) [Google Scholar]
- Agresti A. Wiley; New York: 2007. An introduction to categorical data analysis. [Google Scholar]
- Azagew, A. W., Mekonnen, C. K., Ferede, A. J., Yazew, K. G., & Tezera, Z. B. (2020). Adherence to Highly Active Antiretroviral Therapy and Its Association with Serostatus Disclosure among People Living with HIV in Ethiopia: A Systematic Review and Meta-Analysis.
- Bandura A. Human agency in social cognitive theory. American psychologist. 1989;44(9):1175. doi: 10.1037/0003-066x.44.9.1175. [DOI] [PubMed] [Google Scholar]
- Becker N., Cordeiro L.S., Poudel K.C., Sibiya T.E., Sayer A.G., Sibeko L.N. Individual, household, and community-level barriers to ART adherence among women in rural Eswatini. PloS one. 2020;15(4) doi: 10.1371/journal.pone.0231952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchmann W.F. Adherence: a matter of self-efficacy and power. Journal of advanced nursing. 1997;26(1):132–137. doi: 10.1046/j.1365-2648.1997.1997026132.x. [DOI] [PubMed] [Google Scholar]
- Champion V.L., Skinner C.S. The health belief model. Health behavior and health education: Theory, research, and practice. 2008;4:45–65. [Google Scholar]
- Do N.T., Phiri K., Bussmann H., Gaolathe T., Marlink R.G., Wester C.W. Psychosocial factors affecting medication adherence among HIV-1 infected adults receiving combination antiretroviral therapy (cART) in Botswana. AIDS research and human retroviruses. 2010;26(6):685–691. doi: 10.1089/aid.2009.0222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorcélus L., Bernard J., Georgery C., Vanessa C. Factors associated with antiretroviral therapy adherence among people living with HIV in Haiti: a cross-sectional study. AIDS research and therapy. 2021;18(1):1–9. doi: 10.1186/s12981-021-00405-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandes A., Brito A.M., Mendes T., Alcobia A. Effect of COVID-19 pandemic on antiretroviral therapy adherence. 4CPS-392. 2021 [Google Scholar]
- Ga West Municipal Health Directorate. (2019). Annual Report. Unpublished.
- Ghana AIDS Commission. (2019). National HIV and AIDS Policy. Retrieved on April 02, 2020 from https://www.ghanaids.gov.gh/mcadmin/Uploads/nationalHIVandAIDSPolicy.pdf
- Ghana Statistical Service. (2014). District Analytical Report-Ga West Municipal http://www2.statsghana.gov.gh/docfiles/2010_District_Report/Greater%20Accra/GA%20WEST.pdf
- Heestermans T., Browne J.L., Aitken S.C., Vervoort S.C., Klipstein-Grobusch K. Determinants of adherence to antiretroviral therapy among HIV-positive adults in sub-Saharan Africa: a systematic review. BMJ global health. 2016;1(4) doi: 10.1136/bmjgh-2016-000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hochbaum G., Rosenstock I., Kegels S. Health belief model. United states public health service, W432W8784. 1952 [Google Scholar]
- Kharsany A.B., Karim Q.A. HIV infection and AIDS in sub-Saharan Africa: current status, challenges and opportunities. The open AIDS journal. 2016;10:34. doi: 10.2174/1874613601610010034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legesse T.A., Reta M.A. Adherence to Antiretroviral Therapy and Associated Factors among People Living with HIV/AIDS in Hara Town and Its Surroundings, North-Eastern Ethiopia: A Cross-Sectional Study. Ethiopian journal of health sciences. 2019;29(3) doi: 10.4314/ejhs.v29i3.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyimo R.A., de Bruin M., van den Boogaard J., Hospers H.J., van der Ven A., Mushi D. Determinants of antiretroviral therapy adherence in northern Tanzania: a comprehensive picture from the patient perspective. BMC public health. 2012;12(1):716. doi: 10.1186/1471-2458-12-716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mengistie A., Birhane A., Tesfahun E. Assessment of Adherence to Antiretroviral Therapy Among Adult People Living with HIV/AIDS in North East, Ethiopia. BioRxiv. 2018 [Google Scholar]
- Negesa L., Demeke E., Mekonnin W. Adherence to antiretroviral therapy and factors affecting people living with HIV/AIDS and taking antiretroviral therapy, Dire Dawa Town, Eastern Ethiopia. J Infect Dis Treat. 2017;3(1):5. [Google Scholar]
- Nichols J.S., Kyriakides T.C., Antwi S., Renner L., Lartey M., Seaneke O.A., et al. High prevalence of non-adherence to antiretroviral therapy among undisclosed HIV-infected children in Ghana. AIDS care. 2019;31(1):25–34. doi: 10.1080/09540121.2018.1524113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obirikorang C., Selleh P.K., Abledu J.K., Fofie C.O. Predictors of adherence to antiretroviral therapy among HIV/AIDS patients in the upper west region of Ghana. Isrn Aids. 2013;2013 doi: 10.1155/2013/873939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oku A.O., Owoaje E.T., Ige O.K., Oyo-Ita A. Prevalence and determinants of adherence to HAART amongst PLHIV in a tertiary health facility in south-south Nigeria. BMC infectious diseases. 2013;13(1):1–9. doi: 10.1186/1471-2334-13-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onyekwere LI. Factors Affecting Compliance with the use of Anti-Retroviral Drugs Among Persons Living With HIV/AIDS at the University of Nigeria Teaching Hospital Enugu, Nigeria 2013 (Masters Dissertation), University of Ibadan, Nigeria.
- Polit D.F., Beck C.T. Lippincott Williams & Wilkins; 2004. Nursing research: Principles and methods. [Google Scholar]
- Prah J., Hayfron-Benjamin A., Abdulai M., Lasim O., Nartey Y. Factors affecting adherence to antiretroviral therapy among HIV/AIDS patients in cape coast metropolis. Ghana J HIV AIDS. 2018;4(1) [Google Scholar]
- Reda A.A., Biadgilign S. Determinants of adherence to antiretroviral therapy among HIV-infected patients in Africa. AIDS Research and treatment. 2012:2012. doi: 10.1155/2012/574656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shigdel R., Klouman E., Bhandari A., Ahmed L.A. Factors associated with adherence to antiretroviral therapy in HIV-infected patients in Kathmandu District, Nepal. Hiv/aids (Auckland, NZ) 2014;6:109. doi: 10.2147/HIV.S55816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snedecor G.W., Cochran W.G. 8th Ed. Ames: Iowa State University Press; Iowa: 1989. Statistical methods. [Google Scholar]
- Ssewaya A. Universiteit van Amsterdam; 2011. Sustaining adherence to antiretroviral therapy among HIV/AIDS patients in Uganda (Doctoral Dissertation. ) [Google Scholar]
- Taber K.S. The use of Cronbach's alpha when developing and reporting research instruments in science education. Research in Science Education. 2018;48(6):1273–1296. [Google Scholar]
- Tarkang E.E., van der Wal D.M., Ehlers V.J. The explanatory power of factors associated with the perception of risk contracting HIV among senior secondary school learners in Kumba Cameroon. Africa Journal of Nursing and Midwifery, 1682-5055. 2011;13(2):77–91. 2011; [Google Scholar]
- Tarkang E.E., Pencille L.B. Psychosocial predictors of consistent condom use among migrant road construction workers in the Southwest Region of Cameroon using the Health Belief Model. Pan African Medical Journal. 2018;29:215. doi: 10.11604/pamj.2018.29.215.15130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Themanson J.R., Rosen P.J. Examining the relationships between self-efficacy, task-relevant attentional control, and task performance: Evidence from event-related brain potentials. British Journal of Psychology. 2015;106(2):253–271. doi: 10.1111/bjop.12091. [DOI] [PubMed] [Google Scholar]
- UNAIDS . UNAIDS; Geneva: 2014. 90-90-90: An ambitious treatment target to help end the AIDS epidemic.https://www.unaids.org/en/resources/909090 Retrieved from. on 20th November 2019. [Google Scholar]
- UNAIDS . 2016. Global Aids Update 2016.https://www.unaids.org/sites/default/files/media_asset/global-AIDS-update-2016_en.pdf Retrieved on April 03, 2020 from. [Google Scholar]
- UNAIDS . 2019. Fact Sheet.http://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf Retrieved on April 03, 2020 from. [Google Scholar]
- UNAIDS . 2019. Regional Factsheets-Central and West Africa.https://aidsinfo.unaids.org/ Retrieved on April 24, 2020 from. [Google Scholar]
- UNAIDS . 2019. Country Factsheets-Ghana.https://aidsinfo.unaids.org/ Retrieved on April 24, 2020 from. [Google Scholar]
- Vitalis D. Predicting adherence to antiretroviral therapy among pregnant women in Guyana: Utility of the Health Belief Model. International journal of STD & AIDS. 2017;28(8):756–765. doi: 10.1177/0956462416665989. [DOI] [PubMed] [Google Scholar]
- Vitalis D. Adherence to Antiretroviral Therapy among Perinatal Women in Guyana. Palgrave Macmillan; Singapore: 2021. Utility of the Health Belief Model to Predict Adherence; pp. 201–217. [Google Scholar]
- Wasti S.P., Simkhada P., Randall J., Freeman J.V., Van Teijlingen E. Factors influencing adherence to antiretroviral treatment in Nepal: a mixed-methods study. PloS one. 2012;7(5):e35547. doi: 10.1371/journal.pone.0035547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2019. HIV/AIDS.https://www.who.int/news-room/fact-sheets/detail/hiv-aids Retrieved on March 27, 2020 from. [Google Scholar]
- Yarney L., Amankwah A.K., Mba C.J., Asamoah K., Bawole J.N. Facilitators and barriers to antiretroviral therapy adherence among Ghanaian patients: A multi-case study. African Population Studies. 2016;30(2):2341–2355. [Google Scholar]
- Yaya I., Landoh D.E., Saka B., Wasswa P., Aboubakari A.S., N'Dri M.K.…Pitche P. Predictors of adherence to antiretroviral therapy among people living with HIV and AIDS at the regional hospital of Sokodé, Togo. BMC public health. 2014;14(1):1308. doi: 10.1186/1471-2458-14-1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L., Li X., Lin Z., Jacques-Tiura A.J., Xu J., Zhou Y.…Stanton B. Side effects, adherence self-efficacy, and adherence to antiretroviral treatment: a mediation analysis in a Chinese sample. AIDS care. 2016;28(7):919–926. doi: 10.1080/09540121.2015.1124984. [DOI] [PMC free article] [PubMed] [Google Scholar]