Abstract
Aim
To determine the effectiveness of the progressive muscle relaxation (PMR) technique on anxiety caused by Covid‐19 in pregnant women under the auspices of comprehensive health service centers in the nineteenth district of Tehran University of Medical Sciences.
Method
This study is a randomized clinical trial. A total of 126 pregnant women were randomly allocated to the intervention group (N = 63) and control group (N = 63). All participants completed demographic questionnaires and the Corona Disease Anxiety Scale electronically. The intervention was held in six sessions through Sky Room (three times a week). It consisted of training and practicing the PMR. The intervention group was re‐evaluated with the related questionnaires immediately after the intervention and 2 weeks later, and the control group 2 and 4 weeks after the baseline.
Results
There was a significant difference between the control and intervention groups at the baseline (P = .05). Nevertheless, analysis of variance test results showed that the difference between the intervention and control groups was found to be significantly different statistically; (22.92 ± 6.07) for intervention versus (28.13 ± 6.93) for control, with the second follow up (P = .01).
Conclusions
Progressive muscle relaxation is used as a useful intervention to reduce anxiety in pregnant women during coronavirus pandemics educated and recommended with more emphasis and sensitivity in pregnancy care by healthcare providers.
Keywords: anxiety, Covid‐19, progressive muscle relaxation, pregnancy, relaxation technique
Progressive muscle relaxation is used as a useful intervention to reduce anxiety in pregnant women during coronavirus pandemics and is recommended with more emphasis and sensitivity in pregnancy care by healthcare providers

1. INTRODUCTION
The emerging coronavirus (Covid‐19), which causes respiratory illnesses from the common cold to respiratory distress syndrome and even death, also affects pregnant women as a vulnerable population. 1 , 2 , 3 Limited information is available on the impact of the current outbreak of coronavirus in pregnancy. However, available information on diseases associated with other pathogenic coronaviruses (such as severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS)) may provide useful insight into the effects of the Covid‐19 in pregnancy. 3 , 4 Complications such as acute respiratory distress syndrome, diffuse intravascular coagulation, renal failure, secondary bacterial pneumonia, a threefold need for mechanical ventilation, and 23%‐25% mortality have been observed in studies of pregnant women with SARS and MERS. 3 , 5 Because coronavirus disease may increase the risk of pregnancy complications such as fetal growth retardation, 4 fetal distress, and preterm labor, 3 , 4 , 6 the disease should be managed in a targeted and optimal manner with close monitoring of both mother and fetus. 3 According to existing study data, the principles of coronavirus disease management in pregnancy include premature isolation, infection control processes, oxygen therapy, prevention of fluid overload, and consideration of experimental antibiotics (due to the risk of bacterial infection). Monitoring uterine contractions are the primary mechanical ventilation for progressive respiratory failure, planning for delivery, and adopting a team counseling approach. 3
Epidemics are not just a physical health crisis, but studies show that people who experience a health emergency have varying degrees of stress and anxiety disorders that persist even after the illness is over. 7 , 8 Anxiety is a common symptom in patients with chronic respiratory disorders and can significantly reduce patients' quality of life. 9 The epidemiological studies have reported the following psychological problems in the Covid‐19 epidemic: fear, anxiety, and depression due to fear of illness, fear of death, unknown virus, quarantine, and the influx of news and rumors published on social media, interference in daily activities, and reduced social communication. 4 , 7 , 8 , 10 , 11 The Covid‐19 pandemic has also caused increasing stress and anxiety for pregnant women worldwide, with many pregnant mothers worrying about giving birth in a hospital for fear of contracting the coronavirus and sometimes even refusing to see their doctors. On the other hand, pregnant women's worries about their families' attendance at the hospital, breastfeeding, and neonatal care, such as vaccination and screening during the coronavirus epidemic, also add to the already build up anxiety and stress of these women. Such extreme psychological issues may be associated with side effects such as pre‐eclampsia, preterm labor, low birth weight, and low Apgar score. 10 , 12
Studies show that reducing anxiety, fear, and stress in epidemics improves mental health. Therefore, effective interventions to reduce fear and anxiety seem necessary. 13 Researchers have found effective ways to reduce anxiety and stress during a coronavirus epidemic. These methods are as follows: staying away from watching, listening, and reading news constantly about the coronavirus,engaging in enjoyable activities (such as reading books, cooking, and practicing playing an instrument); taking care of the body through adequate sleep, a healthy diet; avoiding of drugs and alcohol; performing techniques such as muscle relaxation, deep conscious breathing, and yoga; connecting with friends and trusted people through social media; and talking to them about worries and feelings. 13 , 14 Also, raising awareness about ways of transmitting the coronavirus, risk factors, and providing distance counseling for pregnancy care can reduce the anxiety and worry of pregnant women during the coronavirus epidemic. 2 Among these strategies, progressive muscle relaxation (PMR) is beneficial in relieving muscle stress, reducing stress and anxiety during pregnancy, and making pregnancy a happy and pleasant experience. 12 , 15 , 16 , 17 Studies have also shown the effectiveness of this technique on anxiety. Liu et al 11 in a randomized clinical trial (RCT) study performed on 50 patients with coronavirus, showed that PMR reduces patients' anxiety levels (P <.001). 11 Also, Sharma and Kaur, 18 in her quasi‐experimental study performed on 70 pregnant women and Rajeswari 12 in the form of a RCT study performed on 250 nulliparous pregnant women, have also reported the effectiveness of PMR techniques in reducing anxiety in pregnant women in separate studies (P =.005; P <.001 respectively). 12 , 18
There is also a large information gap in this area due to the limited information on the coronavirus in pregnancy, 2 , 4 and the lack of studies focusing on effective interventions to reduce anxiety caused by Covid‐19 in the pregnant population. Given the adverse effect of anxiety on maternal and fetal outcomes 2 , 12 and the effectiveness of the PMR technique on reducing anxiety 16 , 19 in the general population, and in particular gestational anxiety, 12 , 17 , 18 we studied the effect of PMR on Iranian pregnant women in pandemic time. Therefore, the aim of this study was to determine the effectiveness of PMR techniques on anxiety caused by Covid‐19 in pregnant women under the auspices of comprehensive health service centers in the nineteenth district of Tehran University of Medical Sciences.
2. METHODS
2.1. Setting and participants
The present study is a RCT. Nineteen comprehensive health centers supervised by Tehran University of Medical Sciences in Iran were coordinated. Participants (n = 126) in this experimental trial were recruited from 8 primary healthcare centers and 16 subset healthcare centers of Teheran city between July and August 2020. The inclusion criteria were gestational age under 32 weeks; literacy; access to a smartphone, computer, or laptop on the web; and mothers with a score of mild to moderate levels of anxiety caused by Covid‐19 (based on scores from the Corona Disease Anxiety Scale [CDAS]).
Those with a history of a confirmed psychiatric disorder receiving any psychotherapy in the past 6 months, high‐risk pregnancy, severe anxiety caused by Covid‐19, vision and hearing impairment, migration in the last 6 months, hospitalization in the previous 6 months, loss of a family member in the previous 6 months, suicidal ideation, poor pregnancy outcomes such as preterm delivery, miscarriage, stillbirth, fetal abnormalities in the past year, and unwillingness to participate in the study were excluded.
2.2. Sample size and sampling
The sample size of this study was estimated using an online calculator (https://clincalc.com/stats/samplesize.aspx). The baseline information was retrieved from Apri & wulandari 2019. 20 The reported mean anxiety level was 24.54 ± 7.66 in the intervention group and 32 ± 7.11 in the control group. Using these figures, α = 0.05, a study power of 80%, and a sample size of 52 subjects in each group were estimated. Taking into account the 20% sample loss, this number increased to 63 participants in each group, that is, 126 in total. First, a table of random numbers was used to select primary healthcare centers from the healthcare services in the study area. Next, eligible pregnant women from the selected primary healthcare centers were randomly invited by phone to participate in this study.
The contact information of the eligible subjects who were willing to participate in the study was provided to the project manager. Then, based on the study's inclusion and exclusion criteria, the eligible individuals were identified, after which 228 qualified pregnant women were registered on the list. A table of random numbers was used to invite the study participants. The subjects were then randomly allocated to two groups. The number of envelopes used was 126, 63 of which contained a card marked as the intervention group; the other 63 envelopes each had a card marked as the control group. The envelopes were opaque, and the card inside was not visible, even under intense light. The envelopes were then shuffled several times by someone other than the researcher. Each time a pregnant woman was approached, an envelope was opened by a researcher blinded to the treatment assigned inside each envelope, with mothers being also blinded to the assignment. Before the intervention, the written form of informed consent and other related questionnaires (Demographic Profile Questionnaire, Obstetrical history, and Corona Anxiety Scale) were provided to the individuals electronically and completed by them.
Figure 1 of the flowchart shows the working method in the intervention and control groups.
FIGURE 1.
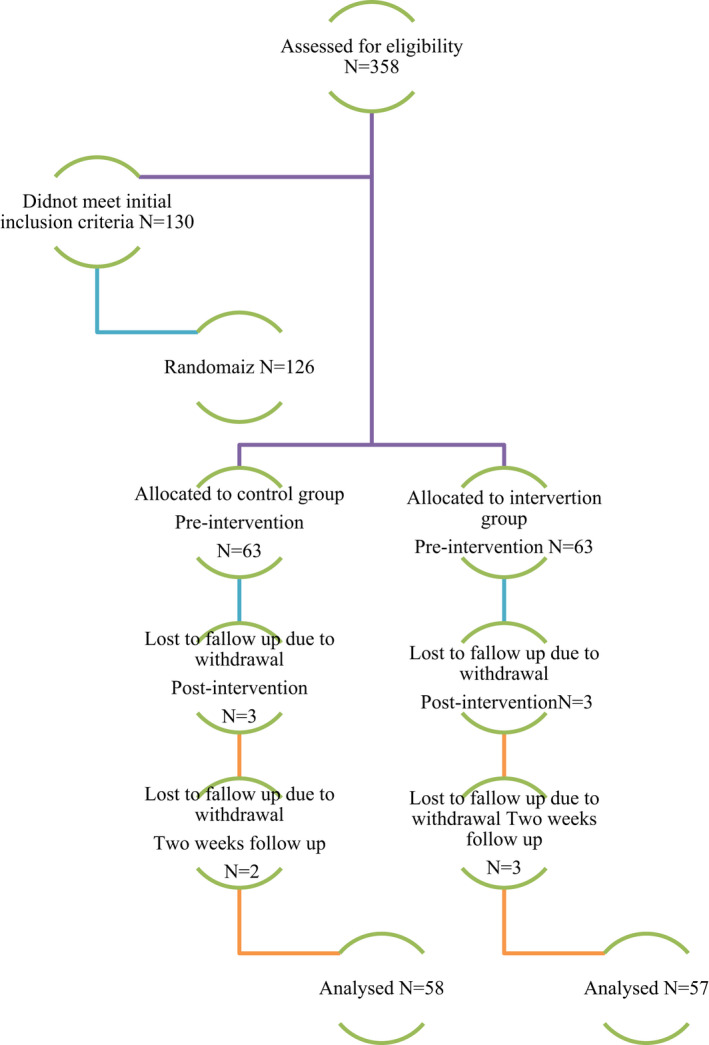
Flowchart of working methods in two groups of intervention and control
2.3. Data tools
Data were collected through a 3‐item demographic (age, education, and employment) and an obstetrical information checklist (gestational age, history of infertility, wanted pregnancy, and the number of children), as well as an 18‐item CDAS.
2.3.1. Corona disease anxiety scale
The questionnaire was developed by Ahmad Alipour et al 21 during the pandemic of coronavirus to measure anxiety caused by the outbreak of coronavirus. The final version of this includes 18 items and two components (factors). Items 1‐9 measure psychological symptoms, and items 10‐18 physical symptoms. The instrument is scored based on a 4‐point Likert scale (never = 0, sometimes = 1, most of the times = 2, and always = 3). Therefore, the possible highest and lowest scores in this questionnaire are between 0 and 54. High scores in this questionnaire indicate a higher level of anxiety in individuals, with scores 0‐16 showing lack of anxiety, 17‐29 moderate anxiety, and 30‐54 severe anxiety caused by Covid‐19. Its reliability is confirmed with Cronbach's alpha value of 0.91 for the whole questionnaire, 0.87 for the first factor, and 0.86 for the second factor. Its validity is also confirmed using exploratory and confirmatory factor analysis. 21
2.4. Progressive muscle relaxation
For the intervention group members, a private Sky Room group was scheduled and also virtual instructions were held in 6 sessions to perform the relaxation techniques (each session lasted 40 min, 3 times a week, for the intervention group). The intervention content detailed in the study protocol (Table 1) included training and practicing the PMR technique, providing information and knowledge about the corona disease, and the possibility of pregnant mothers suffering from anxiety in these conditions. Participants in the intervention group practiced the PMR technique as homework on a daily basis and reported it to the facilitator in the subsequent sessions. Immediately after the intervention (2 weeks after baseline) and 2 weeks after the intervention (4 weeks after baseline), all of the study samples were re‐evaluated with the same Pregnancy Anxiety Questionnaire and SDAS. On the other hand, all members of the control group received their usual prenatal care (pregnancy visits, weight control, blood pressure, etc) in the comprehensive health centers.
TABLE 1.
Outline of sessions for the intensive progressive muscle relaxation technique on anxiety caused by Covid‐19
| Session 1: Introduction to design and introduction, building a rapport with, and obtaining information from the client; discuss Covid‐19 and the causes of anxiety in this condition, training and practicing progressive muscle relaxation technique focusing on the arm and shoulder muscles along with teaching how to breathe deeply. Homework |
| Session 2: Welcome and review the previous session and review homework; practicing progressive muscle relaxation technique on arms and shoulders muscles. In addition, focusing on the head and face muscles with teaching how to breathe deeply. Homework |
| Session 3: Welcome and review the previous session and review homework; practicing progressive muscle relaxation technique on arms, shoulders, head, and face muscles In addition, focusing on muscles of the stomach, abdomen, and buttocks muscles with teaching how to breathe deeply. Homework |
| Session 4: Welcome and review the previous session and review homework, practicing progressive muscle relaxation techniques. In addition to relaxing the various muscles mentioned in the previous sessions, this session is supposed to add leg muscles to the previous parts and thus involve the whole body in this exercise and homework |
| Session 5: Review of progress session 4 |
| Session 6: Review of progress session 4 |
2.5. Statistical analysis
Statistical analyses were performed with SPSS for Windows Version 22 (Statistical package for the social sciences, version 22.0, SPSS Inc). Descriptive statistics were used to determine participants' demographic characteristics and mean anxiety scores. The relationship between variables was evaluated by chi‐squared tests, independent t‐tests, paired t‐tests, and analysis of variance (ANOVA). A P value of .05 or less was considered significant.
2.6. Ethical considerations
The online informed consent had been obtained from all participants. Eligible women were first informed about the study objectives. They were provided with contact details of the research team at Tehran University of Medical Sciences and its deputy research ethics committee (Ethical code: IR.TUMS.MEDICINE.REC.1399.287).
3. RESULTS
3.1. Characteristics of participants
Out of 358 pregnant women, 228 eligible were selected under District 19 health centers' auspices. Of these, 126 were randomly selected for the control and intervention groups. In the control group, three women in the second stage and two women in the third stage withdrew from participating in the study. In the intervention group, three people in the second stage and three in the third stage were excluded from the study. Data were collected from 115 pregnant women, with gestational ages ranging from 6 to 32 weeks (intervention group: n = 57; and control group: n = 58) (Figure 1). The participants' age was 32, and below 67.5%, below 32 years was 32.5% (range 18‐45 years). Differences between participant subgroups were investigated using chi‐squared tests for categorical data (Table 2). As Table 2 shows those in the intervention and control groups did not differ significantly in terms of most demographic characteristics, for example, age, education level, job, pregnancy wanted, and gestational age (pregnancy week).
TABLE 2.
Demographic characteristics of the participants
| Groups | Control N (%) = 58 (50.4%) | Intervention N(%) = 57 (49.6%) | P‐value* |
|---|---|---|---|
| Age | |||
| 32 and below | 39 (67.2) | 38 (66.7) | .15 |
| Above 32 | 19 (32.8) | 19 (33.3) | |
| Education | |||
| Diploma and below | 39 (67.2) | 35 (41.4) | .12 |
| Above diploma | 19 (32.8) | 22 (38.6) | |
| Employed b | |||
| Yes | 9 (15.5) | 3 (5.3) | .06 |
| No | 49 (84.5) | 54 (94.7) | |
| History of infertility b | |||
| Yes | 2 (3.4) | 8 (14) | .04 |
| No | 56 (96.6) | 49 (86) | |
| Pregnancy wanted | |||
| Yes | 29 (50) | 35 (61.4) | .07 |
| No | 29 (50) | 22 (38.6) | |
| Parity | |||
| Nulliparous | 19 (32.8) | 27 (47.4) | .04 |
| Multiparous | 39 (67.2) | 30 (52.6) | |
| Pregnancy week | |||
| 22 week or less | 25 (43.1) | 23 (40/4) | .143 |
| More than 22 week | 33 (56.9) | 34 (59.6) | |
Have expected count less than 5 = Fisher Exact Test.
Have expected count less than 5 = Fisher Exact Test.
*Chi‐squared tests, independent t‐tests, and paired t‐tests.
3.2. Unadjusted analysis
3.2.1. Intervention group
The mean score of anxiety caused by Covid‐19 was 25.26 ± 4.98 before the intervention. The ANOVA test results in Table 3 show that the score declined to 24.98 ± 5.76 after the intervention (P =.057). It was further reduced to 22.92 ± 6.07 by the second follow‐up (P =.028).
TABLE 3.
Unadjusted mean scores of anxiety caused by Covid‐19 in intervention and control groups
| Intervention group | Control group | P value | |
|---|---|---|---|
| Baseline | 25.26 ± 4.98, n = 57 | 27.98 ± 6.85, n = 58 | .05 |
| After intervention (after 2 weeks) | 24.98 ± 5.76, n = 57 | 28.26 ± 6.77, n = 57 | .057 |
| P value* | .057 | .976 | |
| Second follow up (after 4 weeks) | 22.92 ± 6.07, n = 57 | 28.13 ± 6.93, n = 58 | .01 |
| P value* | .028 | .914 |
*ANOVA test.
3.2.2. Control group
The mean score of anxiety caused by Covid‐19 was 27.98 ± 6.85 before the intervention. ANOVA test results showed that this score changed to 28.26 ± 6.77 after the intervention (P =.976). It further changed to 28.13 ± 6.93 by the second follow‐up (P =.914) (Table 3).
3.2.3. Comparison between anxiety caused by a Covid‐19 score of intervention and control
There was a significant difference between the control and intervention groups at baseline (P =.05). Nevertheless, the difference between the intervention and control groups was found to be significantly different statistically, 22.92 ± 6.07 in the former versus 28.13 ± 6.93 in the latter, by the second follow‐up (P =.01) (Table 3).
3.3. Adjusted analysis
Following the observation of changes in the intervention group in terms of anxiety level, a general linear model was used to identify the adjusted values for both control and intervention groups at three timelines (pre‐intervention, post‐intervention, and 2 weeks follow‐up).
Table 4 shows the result of the general linear model. The findings suggest that none of the confounders (age, education, job, GA, nulliparity, history of infertility, and unwanted pregnancy) had a significant distortion effect on the outcome measured in this study (mean score of anxiety caused by Covid‐19).
TABLE 4.
Adjusted mean scores of anxiety caused by Covid‐19 in intervention and control groups over the trial period
| Baseline | Immediately after intervention (2 weeks after baseline) | P‐value* | 2 weeks after intervention (4 weeks after baseline) | P‐value* | ||||
|---|---|---|---|---|---|---|---|---|
| Intervention N = 57 | Control N = 58 | Intervention N = 57 | Control N = 58 | Intervention N = 57 | Control N = 58 | |||
| Age (Mean year ± SD) | 25.26 ± 1.58 | 27.93 ± 1.62 | 24.98 ± 1.66 | 28.26 ± 1.66 | .701 | 22.93 ± 1.72 | 28.12 ± 1.71 | .938 |
| Education (Mean year ± SD) | 25.26 ± 1.59 | 27.98 ± 1.64 | 24.97 ± 1.66 | 28.26 ± 1.66 | .874 | 22.97 ± 1.71 | 28/07 ± 1.71 | .219 |
| Parity (Mean year ± SD) | 25.20 ± 1.59 | 28.04 ± 1.57 | 24.92 ± 1.66 | 28.32 ± 1.67 | .558 | 22.93 ± 1.73 | 28.11 ± 1.71 | .656 |
| Pregnancy week (Mean year ± SD) | 25.25 ± 1.59 | 27.98 ± 1.57 | 24.98 ± 1.66 | 28.26 ± 1.66 | .995 | 22.91 ± 1.72 | 28.13 ± 1.71 | .952 |
| Employed (Mean year ± SD) | 25.32 ± 1.59 | 27.92 ± 1.57 | 25.09 ± 1.58 | 28.24 ± 1.67 | .914 | 22.92 ± 1.73 | 28.12 ± 1.72 | .810 |
| History of infertility (Mean year ± SD) | 25.43 ± 1.58 | 27.81 ± 1.47 | 25.11 ± 1.66 | 28.13 ± 1.66 | .285 | 23.09 ± 1.72 | 27.96 ± 1.72 | .192 |
| Pregnancy wanted (Mean year ± SD) | 25.25 ± 3.57 | 27.99 ± 1.57 | 24.97 ± 1.66 | 28.27 ± 1.66 | .898 | 22.93 ± 1.72 | 28.11 ± 1.71 | .687 |
The * sign indicates the statistical method used, which is written below the table. The possibility of deleting this mark is completely at the disposal of the Editor in Chief.
4. DISCUSSION
This study aimed to evaluate the effects of PMR on anxiety caused by Covid‐19 in pregnant women. It showed that PMR was able to reduce the anxiety level caused by Covid‐19 in pregnant women in the intervention group (P =.01), while there was no statistically significant difference in the control group. This is in line with the results of the study by Liu et al 11 on the effectiveness of the PMR technique in reducing anxiety in patients infected by Covid‐19. 11
In the study of Sadeghi et al (2010), muscle relaxation intervention increased pregnant women's general health and decreased anxiety in the intervention group. 22 Urech et al 23 also found that PMR and conscious imaging could significantly reduce anxiety during pregnancy and increase peace and mental health. 23 Sharma and Kaur 18 and Rajeswari and Sanjeevareddy 12 also emphasized the effectiveness of the PMR technique on reducing anxiety in pregnant women. 12 , 18 Therefore, it can be inferred that the training muscle relaxation technique can reduce pregnant women's anxiety. In Chang's study, a rapid improvement in stress score was reported in the intervention group by implementing a muscle relaxation program. No statistically significant difference was observed in pregnancy anxiety scores in the two groups. 24 The discrepancy between the results of the present study and the above‐mentioned findings can be attributed to the difference in the quality of the intervention program.
In the event of social and health crises in which access to the health system is associated with problems and risks, or the presence in the community increases the risk of disease (such as the Covid‐19 disease), e‐services can be a good platform for healthcare implementation. The results of the present study align with Mohammadzadeh's 25 research on the effectiveness of healthcare using cyberspace. 25 Rahmani (2018) showed that after the intervention (training PMR technique using SMS service), the level of overt and covert anxiety in pregnant women in the intervention group was significantly lower than the control group, 26 being consistent with the results of this study.
Although the effectiveness of the PMR technique on the level of anxiety during pregnancy has been confirmed in the studies above, it is the first time this technique has been performed in the context of the coronavirus epidemic with a focus on the population of pregnant women. Like other studies, participants in this study relaxed by learning how to contract and relax their muscles sequentially and identify anxiety symptoms. The reduced anxiety in study participants after PMR training and practice may balance the anterior nucleus and hypothalamus. By reducing the sympathetic activity of the nervous system, the side effects of anxiety can be prevented, and physical and mental relaxation can be promoted. 27 Therefore, muscle relaxation training can reduce risk factors in mental health and improve mental health during pregnancy. 11 This was also proven in the present study.
The present study tried to create a broad perspective on comprehensive pregnancy care in midwifery. It is hoped that the results of this study will enable midwives and midwifery counselors, who have received the necessary training and are considered the first‐line healthcare providers, to consult with pregnant women, and perform simple and easy techniques such as PMR and include it in Routine prenatal care so as to reduce anxiety in pregnant women‐anxiety that may be caused by personal or social reasons and threaten the health of pregnant women. It was also attempted to provide a suitable platform for designing effective interventions to promote the mental health of pregnant women, as important members of society.
4.1. Limitation
The random allocation of the samples and intervention based on a protocol designed by the research team could be mentioned as the strengths of the present study. On the other hand, since this was the first interventional study on the effect of PMR on anxiety caused by Covid‐19 in pregnant women in Iran, more research in this area could be helpful. Despite the efforts made, the study also faced some limitations. In spite of the random selection of the control group, however, the effects of environmental factors such as education, economic conditions, lifestyle, culture, and other elements on the impact of relaxation training should not have been easily ignored. Another limitation of the study was that due to the intervention sessions conducted by the Sky Room internet space, only pregnant mothers who had access to the Internet and smartphones could be included. It is also undeniable that the intervention team received more support and contact with researchers. The study may also be contaminated by bias due to pregnant mothers attending medical centers for routine pregnancy services. However, this probability was very low because pregnant women were randomly selected from different treatment centers (8 primary healthcare centers and 16 subset healthcare centers) and did not communicate with each other during the study; only with the researcher during relaxation sessions in the Sky Room environment. Moreover, the research team's judgment in this study was based on the main variables of the research, such as anxiety, self‐report, and items specified in the questionnaire. In spite of the reliability of self‐report questionnaires, the response bias in interpreting the results should have been considered. Potentially different levels of exposure to Covid‐19 between the control and intervention groups could have been introduced as selection bias.
5. CONCLUSION
According to the results of this study, the PMR technique is effective in reducing the level of anxiety caused by Covid‐19 in pregnant women and helps to improve the quality of their mental health. Therefore, it is recommended that this technique be used as an effective intervention to reduce anxiety in pregnant women during coronavirus pandemic independently or in combination with other adjuvant treatments by healthcare providers.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
MZ and AES participated in study design, psychological intervention, collecting data, and drafting the manuscript. AES participated in revising the manuscript. FE participated in study design, interpreted findings, the professional technical guidance during the intervention, and participated in revising the manuscript. SHJ performed the statistical analysis, interpreted findings, and re‐evaluated the data. All authors read and approved the final manuscript.
ETHICS STATEMENT
The present study is part of a research project approved by Tehran University of Medical Sciences with the code IR.TUMS.MEDICINE.REC.1399.287.
INFORMED CONSENT
Written informed consents were obtained from all participants and they were ensured that their identity would be kept anonymous throughout the study.
ACKNOWLEDGEMENTS
It was done with the financial support of the Vice Chancellor for Research of Tehran University of Medical Sciences. We would like to thank all those who helped us in this study. The authors would like to express their gratitude to all the pregnant women in this research.
Zendehdel M, Elyasi F, Jahanfar S, Emami‐Sahebi A. Effectiveness of progressive muscle relaxation technique on anxiety caused by Covid‐19 in pregnant women: A randomized clinical trial. Neuropsychopharmacol Rep. 2022;42:158–165. 10.1002/npr2.12241
This study was approved in Iranian Registry of Clinical Trials (IRCT) at 2020‐08‐21 with code 20200630047962N1.
Funding information
This study was supported by the Tehran University of Medical Sciences. (Grant number =99‐2‐152‐48830). The present study is part of a research project approved by Tehran University of Medical Sciences with the code IR.TUMS.MEDICINE.REC.1399.287
DATA AVAILABILITY STATEMENT
Since our data contain potentially sensitive personal information, it is forbidden to share these data with a third party without obtaining an additional written form of informed consent for information sharing. We did not obtain the additional written consent for information sharing.
REFERENCES
- 1. Dashraath P, Jeslyn WJL, Karen LMX, Min LL, Sarah L, Biswas A, et al. Coronavirus disease 2019 (COVID‐19) pandemic and pregnancy. Am J Obstet Gynecol. 2020;222(6):521–31. 10.1016/j.ajog.2020.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fakari FR, Simbar M. Coronavirus pandemic and worries during pregnancy; a letter to editor. Arch Acad Emerg Med. 2020;8:e21. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7075675/ [PMC free article] [PubMed] [Google Scholar]
- 3. Rasmussen SA, Smulian JC, Lednicky JA, Wen TS, Jamieson DJ. Coronavirus disease 2019 (COVID‐19) and pregnancy: what obstetricians need to know. Am J Obstet Gynecol. 2020;222(5):415–26. 10.1016/j.ajog.2020.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mullins E, Evans D, Viner R, O'Brien P, Morris E. Coronavirus in pregnancy and delivery: rapid review and expert consensus. medRxiv. 10.1101/2020.03.06.20032144 [DOI] [PubMed] [Google Scholar]
- 5. Wong SF, Chow KM, Leung TN, Ng WF, Ng TK, Shek CC, et al. Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome. Am J Obstet Gynecol. 2004;191:292–7. 10.1016/j.ajog.2003.11.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang X, Zhou Z, Zhang J, Zhu F, Tang Y, Shen X. A case of 2019 Novel Coronavirus in a pregnant woman with preterm delivery. Clin Infect Dis. 2020;71(15):844–6. 10.1093/cid/ciaa200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Duan L, Zhu G. Psychological interventions for people affected by the COVID‐19 epidemic. Lancet Psychiatr. 2020;7:300–2. 10.1016/S2215-0366(20)30073-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lima CKT, De Medeiros Carvalho PM, Lima IDAS, De Oliveira Nunes JVA, Saraiva JS, De Souza RI, et al. The emotional impact of Coronavirus 2019‐nCoV (new Coronavirus disease). Psychiatry Res. 2020;287:112915. 10.1016/j.psychres.2020.112915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dong X‐Y, Wang L, Tao Y‐X, Suo X‐L, Li Y‐C, Liu F, et al. Psychometric properties of the anxiety inventory for respiratory disease in patients with COPD in China. Int J Chron Obstruct Pulmon Dis. 2017;12:49–58. 10.2147/COPD.S117626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fard SA, Saffarinia M. The prediction of mental health based on the anxiety and the social cohesion that caused by coronavirus. Social Psychology Research. 2020;9:129–41. http://www.socialpsychology.ir/article_105547_en.html [Google Scholar]
- 11. Liu K, Chen Y, Wu D, Lin R, Wang Z, Pan L. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID‐19. Complement Ther Clin Pract. 2020;39:101132. 10.1016/j.ctcp.2020.101132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rajeswari S, Sanjeevareddy N. Efficacy of progressive muscle relaxation on pregnancy outcome among anxious indian primi mothers. Iran J Nurs Midwifery Res. 2020;25:23. 10.4103/ijnmr.IJNMR_207_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Huang PH. Lessening anxiety, panic, and complacency in pandemics. SSRN Electronic Journal. 2020;20(14):1–36. 10.2139/ssrn.3575101 [DOI] [Google Scholar]
- 14. Allahtavakoli M. Coping with the stress of COVID_19 epidemic. JUMS Journal. 2020;7:253–4. http://journal.jmu.ac.ir/article‐1‐371‐fa.html [Google Scholar]
- 15. Emami‐Sahebi A, Elyasi F, Yazdani‐Charati J, Shahhosseini Z. Psychological interventions for nausea and vomiting of pregnancy: a systematic review. Taiwan J Obstetr Gynecol. 2018;57:644–9. 10.1016/j.tjog.2018.08.005 [DOI] [PubMed] [Google Scholar]
- 16. Gawande S, Vaidya M, Tadke R, Kirpekar V, Bhave S. Progressive muscle relaxation in hyperemesis gravidarum. JSAFOG. 2011;3:28–32. 10.5005/jp-journals-10006-1118 [DOI] [Google Scholar]
- 17. Alder J, Urech C, Fink N, Bitzer J, Hoesli I. Response to induced relaxation during pregnancy: comparison of women with high versus low levels of anxiety. J Clin Psychol Med Settings. 2011;18:13–21. 10.1007/s10880-010-9218-z [DOI] [PubMed] [Google Scholar]
- 18. Sharma S, Kaur B. Effect of progressive muscle relaxation on anxiety among antenatal mothers attending antenatal OPD of GGSMC & Hospital, Faridkot, Panjab. Int J Nurs Edu. 2020;12:79. 10.5958/0974-9357.2020.00017.3 [DOI] [Google Scholar]
- 19. Apóstolo JLA, Kolcaba K. The effects of guided imagery on comfort, depression, anxiety, and stress of psychiatric inpatients with depressive disorders. Arch Psychiatr Nurs. 2009;23:403–11. 10.1016/j.apnu.2008.12.003 [DOI] [PubMed] [Google Scholar]
- 20. Wulandari AN, Susanti BAD. The effect of mindfulness therapy on the pregnant women's anxiety level in facing childbirth. Int J Commun Med Public Health. 2019;6:3754–9. 10.18203/2394-6040.ijcmph20193965 [DOI] [Google Scholar]
- 21. Ahmad Alipour AG, Alipour Z, Abdollahzadeh H. Preliminary validation of the Corona Disease Anxiety Scale (CDAS) in the Iranian sample. Journal of Health Psychology. 2020;8(32):163–75. 10.30473/hpj.2020.52023.4756 [DOI] [Google Scholar]
- 22. Sadeghi A, Sirati‐Nir M, Ebadi A, Aliasgari M, Hajiamini Z. The effect of progressive muscle relaxation on pregnant women's general health. Iran J Nurs Midwifery Res. 2015;20:655. 10.4103/1735-9066.170005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Urech C, Fink NS, Hoesli I, Wilhelm FH, Bitzer J, Alder J. Effects of relaxation on psychobiological wellbeing during pregnancy: a randomized controlled trial. Psychoneuroendocrinology. 2010;35:1348–55. 10.1016/j.psyneuen.2010.03.008 [DOI] [PubMed] [Google Scholar]
- 24. Chuang L‐L, Lin L‐C, Cheng P‐J, Chen C‐H, Wu S‐C, Chang C‐L. Effects of a relaxation training programme on immediate and prolonged stress responses in women with preterm labour. J Adv Nurs. 2012;68:170–80. 10.1111/j.1365-2648.2011.05765.x [DOI] [PubMed] [Google Scholar]
- 25. Mohammadzadeh A. Effectiveness of electronic health care and drug monitoring program to prevent COVID‐19 and adherence to therapeutic regimen in patients with ischemic heart disease‐a pilot study. JMM. 2020;22:139–46. 10.30491/JMM.22.2.139 [DOI] [Google Scholar]
- 26. Rahmanibilondi R, Najafi S, Banafsheh E, Abdolazimi Z, Tavafi M, Rahmanibilondi M. The effect of relaxation training using short message service on pregnant women's anxiety. Iran J Nurs Res. 2019;14:42–9. http://ijnr.ir/article‐1‐2163‐en.html [Google Scholar]
- 27. Ferendiuk E, Biegańska JM, Kazana P, Pihut M. Progressive muscle relaxation according to Jacobson in treatment of the patients with temporomandibular joint disorders. Folia Med Cracov. 2019;113–22. 10.24425/fmc.2019.131140 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Since our data contain potentially sensitive personal information, it is forbidden to share these data with a third party without obtaining an additional written form of informed consent for information sharing. We did not obtain the additional written consent for information sharing.


