Highlights
-
•
Only 5 (3.3%) of the postgraduate dissertations were on medical mycology.
-
•
Cryptococcal meningitis (40%, n = 2) was the most researched topic.
-
•
The most common method for studying fungal diseases was culture (60%, n = 3).
-
•
There is limited research on medical mycology at Makerere University, Uganda.
Abstract
Background
As elsewhere worldwide, there is an increasing burden of fungal diseases in Uganda. However, expertise in medical mycology (the study of fungal diseases of medical importance) among clinicians and laboratory personnel remains low.
Objective
This study sought to determine the proportion of dissertations on medical mycology among postgraduate medical microbiology trainees at the College of Health Sciences, Makerere University, Uganda.
Methods
We retrospectively reviewed the topics of dissertations submitted to the Departments of Medical Microbiology and Immunology & Molecular Biology from 2011 through 2018. The proportion of dissertation topics on medical mycology was analysed using descriptive statistics.
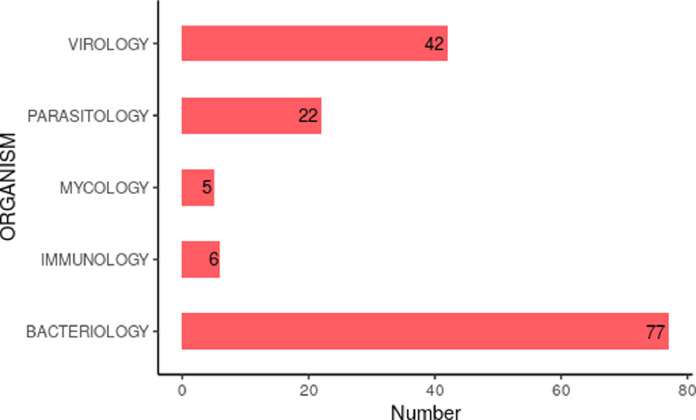
Results
A total of 152 dissertations were retrieved. Of these, only 5 (3.3%) were on medical mycology compared to bacteriology (50.7%, n = 77), virology (27.6%, n = 42), parasitology (14.5%, n = 22) and immunology (4.0%, n = 6). Of the 5 dissertations on fungal diseases, the distribution was as follows: cryptococcal meningitis (40%, n = 2), Candidiasis (20%, n = 1), superficial mycoses (20%, n = 1) and other invasive fungal diseases (20%, n = 1). The most common method that was used for studying the fungal diseases was culture 60%, n = 3.
Conclusion
There is limited research on medical mycology among the postgraduate medical microbiology trainees of Makerere University, Uganda.
Background
Fungal diseases have emerged as important causes of morbidity and mortality worldwide (Bongomin et al., 2017; Brown et al., 2012; Netea & Brown, 2012). The rising incidence of fungal diseases is due to increases in the number of susceptible individuals including people living with human immunodeficiency virus HIV/AIDS (PLWH), cancer patients, immunosuppressive therapy, organ transplant recipients and patients requiring critical care with prolonged hospitalisation (Richardson & Lass-Flörl, 2008; Vallabhaneni et al., 2016).
More than 90% of fungal-related deaths result from species that belong to one of the four genera, Cryptococcus, Candida, Aspergillus and Pneumocystis (Bongomin et al., 2017; Brown et al., 2012; Netea & Brown, 2012). The species of these fungal genera cause a spectrum of diseases which ranges from superficial conditions of the outer keratinised layer of the skin to invasive fungal disease (IFD) of the bloodstream and/or deep seated organs such as the brain, heart, liver, lungs, spleen and the kidneys (Kullberg & Arendrup, 2015). Of particular concern is the high mortality rate associated with invasive fungal infections, which often exceeds 50% despite antifungal therapy (Brown et al., 2012; Ellis et al., 2019).
In Uganda, HIV/AIDS has underscored cryptococcal meningitis as a leading IFD (Parkes-Ratanshi et al., 2015) where the 6-month survival remains ≤ 40 % in routine antiretroviral and antifungal therapy (Longley et al., 2008). One way to contribute to the fight against the burden of fungal diseases is to build capacity through training and research (Brown et al., 2014). Therefore, in this study, we aimed to determine the proportion of research on fungal diseases among postgraduate medical microbiology trainees at the College of Health Sciences, Makerere University, Uganda.
Materials and Methods
Study Design and Setting
This descriptive retrospective study was conducted between March and October of 2020, inclusive. From 2011 through 2018, lists of postgraduate trainee dissertations of Master of Medicine in Microbiology (M.Med.) and Master of Immunology and Clinical Microbiology (MICM) of Makerere University were used. The study site was the Department of Medical Microbiology, School of Biomedical Sciences, College of Health Sciences, Makerere University.
Data management and analysis
Dissertation data including year, research topic, organism/category of organism and study method used were entered in Microsoft Office Excel 2016 (Microsoft Corp., Redmond, WA, USA). The data were analysed using ggplot2 package in R statistical computing software and analysed for the number of theses, frequency of medical microbiology sub-disciplines of Bacteriology, Virology, Parasitology, Mycology, and Immunology. The research methods used in the theses were further classified as microscopy, culture, molecular biology, antigen detection and serology.
Ethical issues
The authors confirm that the ethical policies of the journal, as noted on the journal's author guidelines page, have been adhered to. No human participants were involved in the study. Secondary data were largely available from Makerere University archive and so no ethical clearance was needed. The student names were anonymised, and only study numbers were used for identification.
Results
A total of 152 dissertations that were submitted to the Departments of MICM from 2011 to 2018 were reviewed (Fig. 1). The least number of dissertations was recorded in 2014 at 5.9% (9/152) while 2018 saw the highest number of submitted dissertations at 21.1% (32/152) (Fig.1) over the eight years. The most popular dissertation sub-discipline was Bacteriology at 50.7% (77/152) while Mycology was the least researched at only 3.3% (5/152) (Fig.2). The rest of the sub-disciplines included: Virology 27.6 % (42/152), Parasitology at 14.5% (22/152), and Immunology of 4.0% (6/152) (Fig.2). The most common methods used for research in the dissertations were immunology 49.3% (75/152), culture 23% (35/152) and molecular biology 22.3% (34/152) while bioinformatics and microscopy were the least used at 4% (6/152) and 1.3% (2/152), respectively (Fig. 3).
Fig. 1.
The number of theses submitted from 2011-2018.
In 2014 and 2018, respectively, the lowest and highest numbers of dissertations were submitted (Fig. 1).
Fig. 2.
Frequency of sub-disciplines of medical microbiology in the dissertations submitted.
Bacteriology dissertations were the most popular among postgraduate microbiology trainees (Fig. 2).
Fig. 3.
Methods for data collection in the dissertations.
Immunological techniques were the most used methods in the dissertations (Fig. 3).
Of the 5 mycology dissertations, 2 of them were on cryptococcal meningitis (40%, n = 2), while the 3 remaining dissertations were each written on superficial mycoses (20%, n = 1), candidiasis (20%, n = 1) and other invasive fungal diseases (20%, n = 1) (Table 1).
Table 1.
Fungal diseases studied by postgraduate trainees who wrote mycology dissertations over the years from 2012 to 2019 and the methods used. The fungal diseases studied, and the methods used are shown.
| Year | Fungal disease | Methods |
|---|---|---|
| 2012 | Superficial mycoses | Culture |
| 2012 | Cryptococcal meningitis | Immunology |
| 2014 | Cryptococcal meningitis | Immunology |
| 2014 | Candidiasis | Culture |
| 2019 | Invasive fungal diseases | Culture |
The study of cryptococcal meningitis by immunological techniques was the most popular dissertation (Table 1).
All the methods used for mycology dissertations were phenotype based; culture (n = 3) and immunology (n = 2) (Table 1).
Discussion
Fungal diseases continue to pose a significant threat to humans, plants and animals globally (Bongomin et al., 2017; Brown et al., 2012; Netea & Brown, 2012). In the present study to determine the proportion of research topics on fungal diseases among postgraduate microbiology trainees in a leading University in a developing country setting of Uganda, only 5/152 (3.3%) dissertations were on fungal diseases. This means that medical mycology was the least researched topic. There are several possible reasons why medical mycology was the least studied field among postgraduate students. As in other developing countries, in Uganda, there is limited epidemiological data and a lack of techniques for rapid diagnosis and management of fungal diseases, and there are few antifungal drugs. Additionally, fungal diseases are prohibitively underfunded with < 3 % of the infectious disease budget from major funding bodies such as the US NIH and UK's Wellcome Trust (Brown et al., 2014). Limited funding could be due to the likely fact that few researchers at Makerere University may be competing for mycology-related funding calls. Collectively, these factors could have affected the choice of dissertation topics among the postgraduate medical microbiology trainees.
Additionally, we analysed the frequency of the types of methods that were used for research in the theses (Fig. 3). Most methods that were used were molecular biology techniques. However, molecular techniques are not yet well developed for diagnosis of fungal diseases. Significantly, in resource limited settings, like Uganda, where molecular tests are prohibitively costly, the predominant method for diagnosis of fungal diseases is phenotype-based. In all the medical mycology theses, only phenotypic methods were used. Therefore, it is possible that the available laboratory methods could have affected the limited choice of the students to conduct research in fungal diseases.
This inference is supported by the fact that the most researched fungal disease was cryptococcal meningitis (40 %) which is being studied in many clinical trials in Uganda. The Makerere University, College of Health Sciences through the Infectious Diseases Institute is an internationally recognised research hub for cryptococcal meningitis. However, the index of clinical suspicion for fungal infections is still very low (31%) in Uganda (Kwizera et al., 2020). Supervision, training and research capacity for other fungal diseases is improving. Therefore, the other fungal diseases which were studied included Candidiasis, dermatophytosis and dimorphic fungal mycoses, of which each constituted 20%.
The challenges in medical mycology may be exacerbated by the wide gap in the number of experts in medical mycology and the burden of fungal diseases in Uganda. Additionally, Uganda does not have any national guidelines on fungal diseases, with the exception of cryptococcal disease guidelines. There are also no diagnostic tests for fungal diseases that are paid for by the Ministry of Health, unlike bacterial diseases like TB. Significantly, in the teaching of Mycology in the undergraduate curricula of biomedical sciences and Medicine at Makerere University, there is only limited information on fungal disease and little grant money is spent in this area for research. Therefore, there is a need to establish a stand-alone medical mycology postgraduate program in Uganda.
Following, the Department of Medical Microbiology, Makerere University (Uganda) has developed a program of Master of Science in Medical Mycology (MMY) (in collaboration with Manchester University, UK) that is aimed at producing graduates who are adept at the principles, pathogenesis, diagnosis, treatment, and control of fungal diseases. Graduates of medical and veterinary programs (such as MBChB, B.D. S, B.S. N, B. PHARM, B.RAD., B.V. M) will be eligible for admission to the program. The students will do course work and dissertation writing to meet the requirements for graduation. A recent study from Gulu University in Uganda showed that using freely available online materials on medical mycology can also enhance teaching and learning of medical mycology (Bongomin et al., 2020). Therefore, teaching will be both in person and online. Upon successful completion, graduates of the program can work in hospitals, universities, research institutions and industry to contribute to the fight against fungal diseases.
We also believe that offering scholarships when acquired, for a period of at least 5 years from commencement of the program, will provide strong support to the much-needed program. The findings of our study are in agreement with the report by (Brown et al., 2014) on improving mycology expertise in developing countries through training and funding.
Conclusion
We report a requirement to start a dedicated MSc Medical Mycology program to meet the research needs of postgraduate medical microbiology trainees of Makerere University of Uganda.
Conflict of interest
All authors have no conflict of interest.
Acknowledgments
Authors' contributions
B.A designed the study, collected the data, coordinated the research, performed data analysis wrote and reviewed the manuscript. GM analysed the data and reviewed the manuscript. RK reviewed the manuscript. DPK provided administrative support in archiving the data and reviewed the manuscript. HK provided leadership support and reviewed the manuscript. FB designed the study, coordinated the research, performed data analysis, and reviewed the manuscript. All authors read and approved the final manuscript.
Funding information
This work received no specific grant from any funding agency.
Acknowledgement
We are grateful to Geraldine Nalwadda who retrieved the list of the dissertations submitted to the departments. BA is a NURTURE (NIH/International Fogarty Centre) Fellow under the NIH grant D43TW010132, has EDCTP fellowship (TMA2018CDF-2371) and is MAKRIF faculty grant holder. RK is a PhD fellow supported through the DELTAS Africa Initiative grant # DEL-15-011 to THRiVE-2, from Wellcome Trust grant # 107742/Z/15/Z and the UK government. The funders had no roles in the study design, data collection, analysis, decision to publish or preparation of the manuscript.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ijregi.2022.04.010.
Contributor Information
Beatrice Achan, Email: beatriceachan@yahoo.co.uk.
Gerald Mboowa, Email: gmboowa@gmail.com.
Richard Kwizera, Email: kwizerarichard@ymail.com.
David P. Kateete, Email: davidkateete@gmail.com.
Henry Kajumbula, Email: henrykajumbula427@gmail.com.
Felix Bongomin, Email: drbongomin@gmail.com.
Appendix. Supplementary materials
References
- Bongomin F., Erima B., Kwizera R., Odongo-Aginya E.I. Online Learning Resources Enhanced Teaching and Learning of Medical Mycology among Medical Students in Gulu University, Uganda. Education Research International. 2020;2020:1–5. doi: 10.1155/2020/9468241. [DOI] [Google Scholar]
- Bongomin F., Gago S., Oladele R., Denning D. Global and Multi-National Prevalence of Fungal Diseases—Estimate Precision. Journal of Fungi. 2017;3(4):57. doi: 10.3390/jof3040057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown G.D., Denning D.W., Gow N.A.R., Levitz S.M., Netea M.G., White T.C. Hidden killers: Human fungal infections. Science Translational Medicine. 2012;4(165):1–9. doi: 10.1126/scitranslmed.3004404. [DOI] [PubMed] [Google Scholar]
- Brown G.D., Meintjes G., Kolls J.K., Gray C., Horsnell W., Working Group from the EMBO-AIDS Related Mycoses Workshop. Achan B., Alber G., Aloisi M., Armstrong-James D., Beale M., Bicanic T., Black J., Bohjanen P., Botes A., Boulware D.R., Brown G., Bunjun R., Carr W.…Yang Y. AIDS-related mycoses: The way forward. Trends in Microbiology. 2014;22(3):107–109. doi: 10.1016/j.tim.2013.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis J., Bangdiwala A.S., Cresswell F.V, Rhein J., Nuwagira E., Ssebambulidde K., Tugume L., Rajasingham R., Bridge S.C., Muzoora C., Meya D.B., Boulware D.R. The Changing Epidemiology of HIV-Associated Adult Meningitis, Uganda 2015-2017. Open Forum Infectious Diseases. 2019;6(10):ofz419. doi: 10.1093/ofid/ofz419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kullberg B.J., Arendrup M.C. Invasive Candidiasis. N Engl J Med. 2015;373(15):1445–1456. doi: 10.1056/NEJMra1315399. [DOI] [PubMed] [Google Scholar]
- Kwizera R., Bongomin F., Lukande R. Deep fungal infections diagnosed by histology in Uganda: A 70-year retrospective study. Medical Mycology. 2020:1–9. doi: 10.1093/mmy/myaa018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longley N., Muzoora C., Taseera K., Mwesigye J., Rwebembera J., Chakera A., Wall E., Andia I., Jaffar S., Harrison T.S. Dose response effect of high-dose fluconazole for HIV-associated cryptococcal meningitis in southwestern Uganda. Clinical Infectious Diseases : An Official Publication of the Infectious Diseases Society of America. 2008;47(12):1556–1561. doi: 10.1086/593194. [DOI] [PubMed] [Google Scholar]
- Netea M.G., Brown G.D. Fungal infections: The next challenge. Current Opinion in Microbiology. 2012;15(4):403–405. doi: 10.1016/j.mib.2012.07.002. [DOI] [PubMed] [Google Scholar]
- Parkes-Ratanshi R., Achan B., Kwizera R., Kambugu A., Meya D., Denning D.W. Cryptococcal disease and the burden of other fungal diseases in Uganda; Where are the knowledge gaps and how can we fill them? Mycoses. 2015;58:85–93. doi: 10.1111/myc.12387. [DOI] [PubMed] [Google Scholar]
- Richardson M., Lass-Flörl C. Changing epidemiology of systemic fungal infections. Clinical Microbiology and Infection. 2008;14(SUPPL. 4):5–24. doi: 10.1111/j.1469-0691.2008.01978.x. [DOI] [PubMed] [Google Scholar]
- Vallabhaneni S., Mody R.K., Walker T., Chiller T. The Global Burden of Fungal Diseases. Infectious Disease Clinics of North America. 2016;30(1):1–11. doi: 10.1016/j.idc.2015.10.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.