Abstract
Objective
Psychological trauma (e.g., abuse, neglect) and posttraumatic stress symptoms (PTSS) commonly occur in pediatric pain populations and may be related to various maladaptive coping strategies, which may in turn affect short- and long-term pain-related outcomes in youth. Accordingly, the current scoping review and conceptual framework seeks to identify important gaps in the field’s current understanding of how coping impacts outcomes in youth who have experienced trauma/PTSS and pediatric chronic pain and explores avenues for future investigation.
Methods
A scoping review of the literature was performed in Medline, Embase, Cochrane Library, PsycInfo, and Sociological Abstracts. Eligibility criteria included pediatric populations experiencing chronic pain, trauma, adverse childhood events, and/or PTSS and associated coping mechanisms. Nine research papers were selected and used to support the conceptual framework. The framework builds upon the work of Compas et al.’s’ model of control-based coping (Compas et al., 2006; Compas & Harding Thomsen, 1999) and outlines the potential effects of trauma and/or PTSS and pain on coping and pain-related outcomes (e.g., pain chronicity, functional outcomes) in pediatric chronic pain populations.
Results
A history of chronic pain and psychological trauma and/or PTSS in youth may contribute to increased risk for maladaptive coping and in turn, poorer pain-related and psychosocial outcomes long-term.
Conclusions
Findings from the current scoping review and proposed conceptual framework will guide future research and treatment efforts for youths experiencing pain and trauma and/or PTSS and thereby enhance long-term outcomes.
Keywords: chronic and recurrent pain, coping skills and adjustment, posttraumatic stress and trauma, psychosocial functioning
Introduction
Coping is a multifactorial construct that encompasses an individual’s efforts to manage internal or external demands or stressors (Lazarus & Folkman, 1984). In youth with chronic pain, certain coping styles have been found to be significantly predictive of poor physical (e.g., functional disability) and psychosocial (e.g., anxiety, depression) outcomes (Claar et al., 2008; Cunningham et al., 2014; Kashikar-Zuck et al., 2002; Lami et al., 2018; Wojtowicz & Banez, 2015). Previous research indicates that the experience of stressful events or psychological trauma (herein referred to as “trauma”: i.e., “actual or threatened death, serious injury, or sexual violence”; American Psychiatric Association, 2013) in childhood or adolescence may predispose pediatric and adult populations to the development and maintenance of chronic pain conditions (Bonilla & Saps, 2013; Edwards et al., 2016; Nelson et al., 2016). There is likely a compounding effect of maladaptive coping on pain-related outcomes in traumatized youth with chronic pain.
In youth with chronic pain, a history of trauma and/or posttraumatic stress symptoms (PTSS; e.g., intrusion symptoms, avoidance of trauma reminders, negative alterations in cognitions and mood, etc.; American Psychiatric Association, 2013) may limit coping resources and contribute to poor outcomes. Irrespective of pain, youth with a history of trauma and PTSS experience maladaptive coping manifested as cognitive distortions surrounding the traumatic event (e.g., “It was my fault”, etc.) or behavioral avoidance of trauma reminders (Hamblen & Barnett, 2016). Maladaptive coping in this context is notable given the high incidence of stressful or traumatic life-events (over 80%) and PTSS (up to 32%) in pediatric pain populations compared to healthy youth (Nelson et al., 2018; Nelson & Cunningham, 2020; Noel et al., 2016) and the high rate of somatic symptoms in traumatized pediatric populations (Rimsza et al., 1988). Youth with a history of trauma and/or PTSS may not be as responsive to traditional pain-focused cognitive behavioral therapy (Nelson & Cunningham, 2020), which could put them at greater risk for poorer outcomes long-term. Subjective (i.e., coping) versus objective (i.e., physiological response) adaptation to trauma has also been more significantly associated with PTSS chronicity (Olff et al., 2005), and PTSS chronicity has been proposed to be a maintenance factor for chronic pain (Holley et al., 2016) and related symptoms (e.g., pain-related disability; Maujean et al., 2017) in pediatric and adult populations. In summary, a history of trauma and/or PTSS is linked to poorer outcomes in children with chronic pain.
A prior nonsystematic review conducted more than 5 years ago suggests a multitude of factors impact pain outcomes in youth with trauma and comorbid pain. Within the broader conceptual model proposed by Holley et al. (2016), the presence of PTSS following a trauma was proposed to affect aspects of coping in pediatric pain populations through avoidance and cognitive coping (e.g., changed view of oneself and/or the world, etc.; Holley et al., 2016). However, coping was only briefly addressed in this model given the extremely limited literature available at that time. The goal of our current review was to build upon the growing literature base in pediatric chronic pain to establish a systematic and reproducible review process with exclusive focus on coping mechanisms in pediatric chronic pain populations who have experienced trauma.
Within the adult literature, few existing coping models have highlighted aspects of the relationship between coping and outcomes in traumatized and/or pain populations. For example, one model examines the relationship between psychosocial and coping processes in the transition from acute to chronic pain in adults (Casey et al., 2008). As this model does not account for developmental considerations, it may not be translatable to pediatric populations. A comprehensive examination of coping and its role in potentially magnifying risk for poorer functional and psychosocial outcomes in youth with chronic pain who also have a history of trauma and/or PTSS is warranted, particularly during vulnerable periods of development (Resnick, 2000).
Compas et al. have formulated a pediatric coping model that encompasses coping strategies under the categories of “primary” or active coping strategies, “secondary control” or accommodative coping strategies, and “disengagement” or passive coping strategies (definitions provided below; Compas et al., 2012; Compas & Harding Thomsen, 1999). The Compas model has shown to be a good framework for understanding coping with pain and stress in pediatric samples. For example, the coping categories reported above were validated via confirmatory factor analysis in a sample of youth with functional abdominal pain (Compas et al., 2006). These categories have also been utilized in questionnaire format in multiple studies on coping with stress and pain in youth (Compas et al., 2012; Compas & Harding Thomsen, 1999). However, the role of trauma and/or PTSS in youth with chronic pain has not yet explicitly been investigated via this well-validated model.
We aim to apply this model to traumatized youth with chronic pain to provide a focused and comprehensive lens in understanding coping and its subsequent impact on outcomes in these youth. The focus on coping in the identified population is particularly important given the evidence that coping is a critical factor in predicting long-term pain outcomes (Claar et al., 2008; Compas et al., 2012) and because more severe forms of stress such as trauma and/or PTSS are common in pediatric pain populations (Nelson et al., 2018; 2021; Nelson & Cunningham, 2020; Noel et al., 2016). Examining the role of particular coping styles in pain-related and psychosocial outcomes in youth with pain and trauma and/or PTSS is needed.
Aims of this scoping review center on supporting and refining a conceptual model informed by a systematic literature search and the framework presented by Compas et al., identifying important gaps in the field’s current understanding of coping in traumatized youth with a history of chronic pain, and providing avenues for future investigation and intervention development. This will be achieved through highlighting the relationship between trauma, PTSS, and pain, subsequent coping strategies in pediatric populations, and pain-related outcomes. The adapted coping model will highlight the unique considerations for enhancing coping support and intervention approaches for youth with a history of chronic pain and trauma and/or PTSS. Avenues for future investigation and intervention will then be discussed.
Methods
An unregistered protocol was created by the authors prior to searching to use for internal reviewer consistency. The methodology for conducting the search and reviewing articles is described using the PRISMA Scoping Review Extension reporting documentation (Tricco et al., 2018). It utilizes the scoping review methods practices outlined by the Joanna Briggs Institute Manual of Evidence Synthesis (Aromataris & Munn, 2020). The databases searched were PubMed (Medline and PubMed Central), Embase (including Medline), Cochrane Library (Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effectiveness, Cochrane Controlled Trials Register, Cochrane Review Methodology Database, and the Cochrane Collaboration), PsycInfo (including PsycAbstracts), and Sociological Abstracts. The most recent search was executed on September 20, 2021. This approach was developed in collaboration with the study author trained as a medical librarian (I. K-G.). Searches are presented in Supplementary Appendix 1 and include combinations of keywords and database-specific controlled vocabulary terms for children, chronic pain, trauma, posttraumatic stress disorder (PTSS), adverse childhood events, and coping strategies/behaviors. No date limits were used, and in PsycInfo and Sociological Abstracts, the ‘scholarly journals’ publication filter was applied.
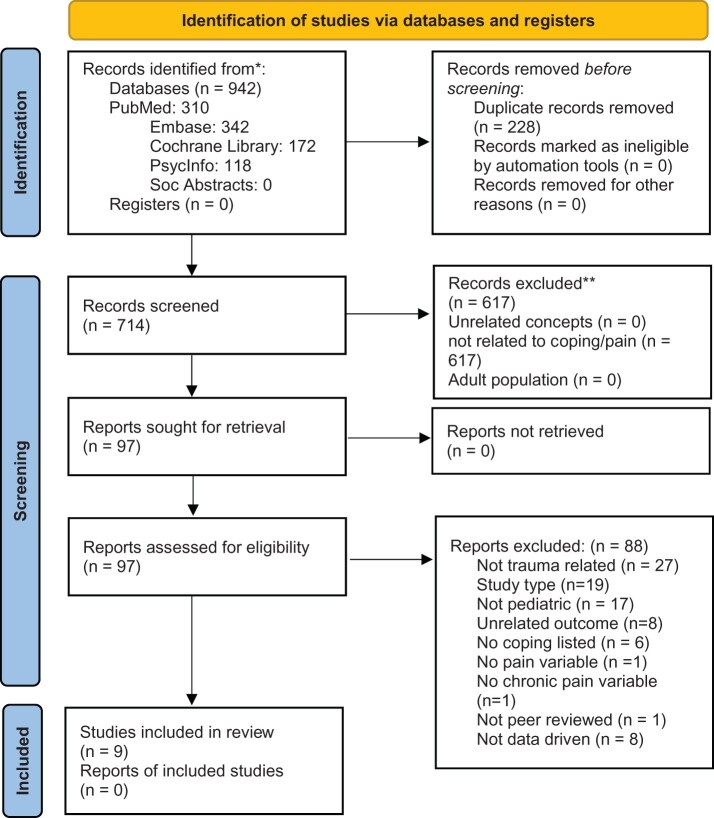
A total of 942 studies were exported from the databases searching and after deduplication 714 were reviewed (Figure 1). The articles included in this review were selected in a double-blind review by the authors (N. R. C., M. A., and S. N.) using Covidence (www.covidence.org). Any conflicts were resolved through collaborative discussion and critical review of the individual study aims. Data from the studies including demographics and study characteristics were put into tabular format (Table I). The eligibility criteria for including articles were primary research, data driven (i.e., quantitative studies only), a focus on child/adolescent subjects, experience of trauma or adverse childhood experiences in the context of pediatric chronic pain, and articles that discussed coping strategies. Articles focused on substance use, serious mental illness, or exclusively adult populations were excluded as these populations were deemed as being outside the scope of the review’s stated aims. Following an abstract-level review, articles without a stated focus on trauma and/or PTSS or pain in pediatric populations were reviewed and collaboratively decided on via author consensus for appropriateness for inclusion (e.g., if related to general pain or trauma coping, etc.). Data table shells were piloted using a sample of five articles from the full set and iteratively developed to ensure reviewer consistency and thoroughness. Data charting for articles was initially split evenly between all authors with final inclusion of articles verified by each author.
Figure 1.
PRISMA 2020 flow diagram for new systematic reviews which included searches of databases, registers, and other sources.
From: Page et al. (2021). For more information, visit: http://www.prisma-statement.org/.
Table I.
Scoping Review Results of Studies Examining Coping in Pain and/or Trauma Populations (N = 9).
| Publication year | First author | Participant age range | Participant race/ethnicity | Pain/Health population type | Coping area | Significant findings |
|---|---|---|---|---|---|---|
| 2021 | Beebe | Ages 8–17 | Not reported | Musculoskeletal, headache, neuropathic pain | Passive (disengagement) | Gait variability was significantly associated with fear of pain and avoidance behaviors. |
| 2021 | Patton | Ages 8–25 |
|
Cancer survivors | Accommodative (secondary control) | Higher posttraumatic stress and pain catastrophizing significantly predicted the presence of chronic pain. |
| 2020 | Soltani | Mean age = 14.20 (2.29) for pain and 13.49 (2.71) for control | Pain:
|
Chronic pain and healthy controls | Accommodative (secondary control) | Attentional bias towards pain was not found to be associated with clinical outcomes in chronic pain youth. |
Control:
| ||||||
| 2020 | Tsur | Ages 18–35 | “Majority Israeli” (otherwise not reported) | Chronic pain | Accommodative (secondary control) | The findings of two studies showed a significant association between child abuse and pain personification. |
| 2018 | Neville | Ages 8–18 |
|
Chronic pain | Accommodative (secondary control) | Child pain catastrophizing mediated the relationship between child PTSD symptoms and child pain. |
| 2018 | Soltani | Ages 8–18 |
|
Chronic pain | Accommodative (secondary control) | Benefit finding was significantly correlated with internalizing mental health symptoms, pain outcomes, and quality of life. |
| 2015 | Wojtowicz | Mean age = 15.84 (range not reported) | Not reported | Chronic pain | Passive (disengagement) | Passive and dependent coping styles were observed in youth with chronic pain. |
| 2009 | Smith | Ages 17–68 |
|
Chronic widespread pain and chronic fatigue |
|
Increased functional impairment was associated with increased avoidance and catastrophizing. |
| 2008 | Claar | Ages 12–17 | 90.7% White/Caucasian (otherwise not reported) | Chronic pain |
|
Profiles of pain coping differentiated pain patients by levels of symptoms, disability, and psychological impairment. |
Note. PTSD = posttraumatic stress disorder.
Results
Nine data-driven papers were selected for inclusion in this review and are overviewed in Table I. Among the included studies generated from our search, one study included an older adolescent/young adult age range (i.e., college students) and one study had children and adults in their sample. Notably, among the selected articles for the current review, all studies (where information was provided) reported a significant majority of participants as being White/Caucasian (70% or higher—see Table I) with five of those studies found either not reporting on participant race/ethnicity at all or providing very little detail.
Results were synthesized via author discussion into thematic (i.e., coping areas) groupings for the purposes of the current paper as outlined by the original Compas model and as described below. Of note, several papers identified focused on multiple aspects of coping and thus were included in more than one section of the model (see Table I).
The Co-occurrence of Psychological Trauma and/or Posttraumatic Stress (PTSS) and Pain in Pediatrics in the Context of Pain Coping
Previous research has clearly established the presence of various coping strategies in pediatric trauma and/or PTSS and pediatric pain populations (Claar et al., 2008; Cunningham et al., 2014; Dempsey et al., 2000). Research indicates that trauma and PTSS often have a bidirectional relationship due to the fact that PTSS requires a precipitating trauma and the presence of PTSS may put individuals at greater risk for re-traumatization (i.e., reminder or re-experiencing of past traumas) or novel traumatization (Lowe et al., 2014; Nader, 2016). In youth with chronic pain, certain methods of coping have been shown to be significantly indicative of optimized or poorer pain-related and psychosocial outcomes (Beebe et al., 2021; Claar et al., 2008). Similarly, youth with a history of trauma often employ coping strategies to manage the aftermath of a trauma experience, including a subset of those youth who may develop PTSS (Dempsey et al., 2000).
The results of our review suggests that a history of trauma (e.g., including some adverse childhood experiences, or ACEs) can contribute to poorer pain-related outcomes in youth via biopsychosocial constructs common to both experiences (Nelson et al., 2016). Youth with a history of ACEs tend to report increased somatic symptoms and fear of pain when compared to youth with pain and no or fewer ACEs exposures (Nelson et al., 2018; 2019). However, the impact of coping on short- and long-term functioning in youth with a history of trauma and/or PTSS and chronic pain remains unclear. For example, trauma symptoms (e.g., hypervigilance, trauma re-experiencing or avoidance, sleep disturbance [i.e., bad dreams about the event], emotional numbing, or increased guilt) may all individually or collectively affect youth’s ability to cope with pain episodes.
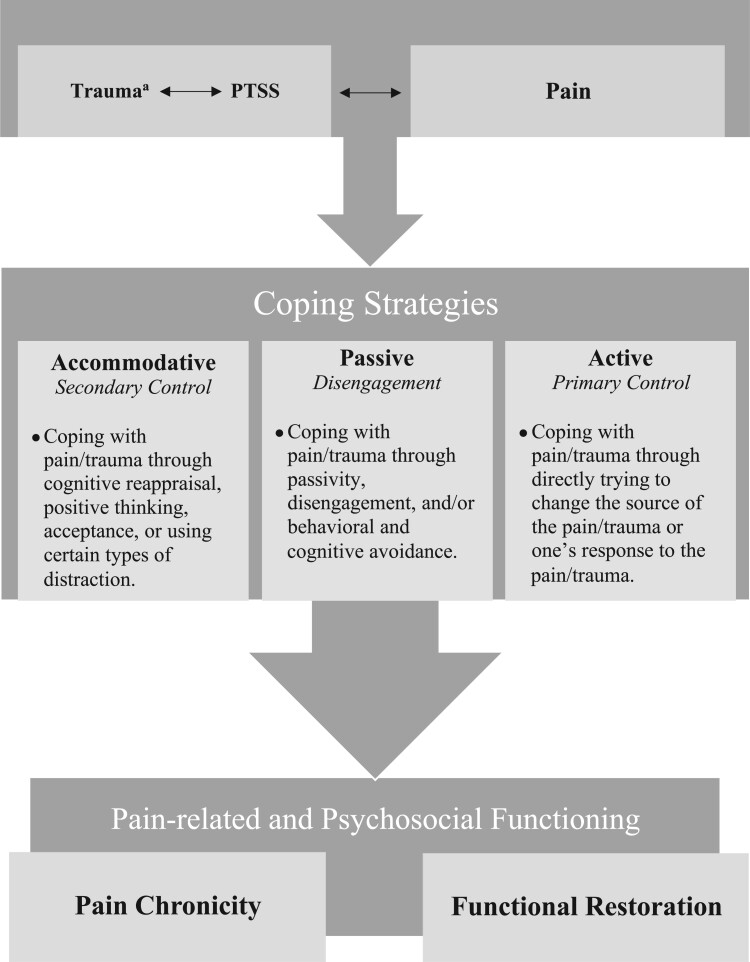
The Proposed Model
The proposed model of coping (Figure 2) was formulated using results of the conducted scoping review and is adapted from a model proposed by Compas et al. that has been previously applied to pediatric health populations (Compas et al., 2012; Compas & Harding Thomsen, 1999). The role of each coping strategy and their potential impact on functioning in youth with trauma/PTSS and pain will be considered in the context of prior pain and trauma research. When relevant, we also highlight related research that helps support the use of this model in understanding outcomes of pediatric chronic pain and trauma.
Figure 2.
Proposed model on the potential effects of trauma and/or posttraumatic stress symptoms (PTSS) on coping and pain-related outcomes in pediatric pain populations.
aA traumatic event (“trauma”), defined in the DSM 5, is an “actual or threatened death, serious injury, or sexual violence.” Following a trauma, some experience post-traumatic symptoms (PTSS). We have a bidirectional arrow between these factors as they can exacerbate the effect on the other (e.g., those who experience PTSS may be vulnerable to re-traumatization). Our model focuses those with pain and either exposure to traumatic event and/or PTSS, which is also represented by a bidirectional arrow as the factors of pain and trauma can co-occur and influence one another.
Accommodative Coping (Secondary Control)
Accommodative or secondary control coping is generally conceptualized as the effort to mitigate distress by managing one’s attention or cognitions related to the event(s) (Compas & Harding Thomsen, 1999) and can include strategies such as acceptance and cognitive restructuring/reframing (e.g., thinking more positively or helpfully). A total of seven studies relating to this area of coping were found using the scoping review methodology. In pain populations, preliminary research has found that attentional bias (i.e., overly attending) towards pain was not associated with poorer clinical pain outcomes (Soltani et al., 2020). Given the frequent occurrence of negative cognitions in the experience of pain (e.g., pain catastrophizing: “My pain will get worse if I move”) or PTSS (e.g., “I am not safe”, “This person is a threat to me”), adaptive secondary control coping may include cognitive coping strategies such as reframing how one thinks about their experience or their ability to manage their current surroundings (Claar et al., 2008). Emerging research also indicates that finding meaning or working towards acceptance of chronic pain, another example of secondary control coping, can increase positive outcomes and optimize resilience (Soltani et al., 2018).
Less frequent use of secondary control strategies may result in a prevalence of maladaptive thoughts related to pain and trauma/PTSS, contributing to more negative outcomes for pediatric pain populations. For example, research in adult populations suggests pain catastrophizing is associated with adverse outcomes in chronic pain including increased pain levels (Keogh et al., 2010), pain interference (Molton et al., 2009), and sleep disruption (de la Vega et al., 2019). Consistent with this, among studies within this review, it has also been found that increased functional impairment is significantly associated with increased pain catastrophizing in a sample of older adolescents and adults with chronic pain (Smith et al., 2009). In a sample of youth with chronic pain and trauma exposure, child pain catastrophizing mediated the relationship between child PTSD symptoms and child pain (Neville et al., 2018). Pain catastrophizing has been proposed as a mechanism through which child PTSD symptoms may influence pain outcomes (Holley et al., 2016). Indeed, in a sample of pediatric cancer survivors, pain catastrophizing was significantly predictive of chronic pain when occurring in concert with PTSS (Patton et al., 2021). Youth with a history of trauma and chronic pain may be more likely to have cognitions around chronic pain that relate to past history of trauma (Tsur, 2020), which may be maladaptive and contribute to negative pain-related and psychosocial outcomes. Pain-focused CBT should incorporate psychoeducation that specifically addresses how trauma can exacerbate maladaptive cognitive coping strategies relating to pain.
Passive Coping (Disengagement)
In the current model, disengagement or passive coping signifies active behavioral or cognitive strategies that help an individual avoid engaging with or thinking about distress (e.g., denial, distraction; Compas & Harding Thomsen, 1999; Connor-Smith et al., 2000). A total of four studies relating to this area of coping were found using the scoping review methodology. Findings on the use of disengagement coping for children with health conditions (which may or may not include pain) is mixed, with some studies showing fewer somatic complaints and lower levels of anxiety and depression whereas others finding the opposite (Compas et al., 2012). In research outside of this review, evidence suggests that when disengagement coping is defined as channeling attention toward positive activities or rewards, it is associated with positive trauma- and pain-related outcomes such as lower levels of trauma-related symptomology (Elzy et al., 2013). Evidence found in this review has supported the presence of passive and dependent coping styles in youth with chronic pain (Wojtowicz & Banez, 2015) with specific research indicating that disengagement coping behavior can be associated with maladaptive changes in movement (e.g., irregular gait) for children with chronic pain (Beebe et al., 2021) and that avoidant coping is associated with increased functional disability associated with chronic pain (Smith et al., 2009). It was also found that youth with chronic pain who engage in disengagement coping such as distraction or avoidance through use of social activities report higher levels of psychological impairment (e.g., depression, anxiety) and poorer physical functioning (Claar et al., 2008). In summary, disengagement coping may result in either positive and negative outcomes for youth experiencing both trauma/PTSS and chronic pain depending on how youth apply this particular coping strategy. Future research should further examine the use of these coping strategies in this population.
Active Coping (Primary Control)
Active or primary control coping encompasses active behavioral strategies (e.g., problem solving, emotional regulation, and expression) that are designed to directly address the cause of stress or feel a different way about it in order to minimize the negative emotional impact (Compas et al., 2012; Compas & Harding Thomsen, 1999; Endler & Parker, 2008). Primary control coping is frequently considered an adaptive method of coping, particularly in situations of “controllable stress” (e.g., school or social demands; Compas et al., 1991). In pediatric pain settings, research has found efficacy for teaching primary control strategies to youth with chronic pain and their parents (Kashikar-Zuck et al., 2013; Lynch-Jordan et al., 2014; Palermo et al., 2015) as a way to optimize outcomes; therefore, additional exploration of primary control coping in traumatized youth with chronic pain would be necessary to fully understand these constructs. In parallel, youth with a history of psychological trauma and/or PTSS (in the absence of pain) may employ similar primary control coping strategies to optimize functioning such as engaging in problem solving or emotional regulation strategies to optimize feelings of calm and safety (Hamblen & Barnett, 2016). As no studies were found using the scoping review methodology for the current paper that focused on these types of coping strategies, additional research is clearly needed. Accordingly, future research and in particular intervention development should focus on these methods of coping to optimize outcomes in youth with chronic pain and a history of trauma and/or PTSS.
Ecological and Developmental Considerations in the Conceptualization of Coping in Traumatized Pain Populations
As mentioned above, certain coping strategies can be considered either adaptive or maladaptive when observed in various contexts. In both pain and trauma contexts, secondary control coping (e.g., distraction) can be adaptive when performed over shorter periods of time in conjunction with appropriate functional activities (e.g., school, sports, social time, etc.; (Claar et al., 2008; Compas et al., 2012; Wohlheiter & Dahlquist, 2013). However, when relied upon as a long-term coping strategy in the absence of primary control coping strategies (e.g., problem solving, emotion regulation), functional and/or psychosocial disability can continue (Kashikar-Zuck et al., 2019; Palermo et al., 2015). Disengagement coping (i.e., avoidance) in certain contexts may be considered protective in the short-term for both pain and traumatized populations as well. When a pediatric pain patient avoids school, anxiety and stress surrounding tolerating pain in the school environment while keeping up with work is minimized in addition to the physical demands on the body. Similarly, for traumatized youth, avoiding certain people or situations that remind them of their trauma(s) (e.g., being around parents that fight) can minimize distress and increase feelings of safety. Regardless, across both settings, cultivating long-term use of these strategies in certain situations can cause overreliance on certain coping strategies across settings and in turn, may maintain disability and provide strong roadblocks towards health and wellness (Hamblen & Barnett, 2016; Holley et al., 2016; Wilson & Keane, 2004).
Relatedly, there are several developmental and cultural aspects of coping that require consideration. To begin, in contrast to adults, pediatric patients with pain and/or trauma are often less able to exercise autonomy in choosing the most adaptive coping strategy for them (Seiffge-Krenke & Pakalniskiene, 2011; Skinner & Wellborn, 2019). For example, a pediatric pain patient who wants to avoid school may be forced to attend by their parents (in the absence of appropriate supports to facilitate success) or conversely, told to stay home from school when they may have been up for the task. Similarly, a child who is traumatized may, in certain situations, be unable to avoid the source or reminder of their trauma (e.g., if it’s in their home environment). This lack of autonomy surrounding coping may be compounded in youth with a history of both pain and trauma, thus likely impacting their use of strategies that promote function. Previous research has shown that aiding parents in supporting their child with coping is crucial to their overall success (Lynch-Jordan et al., 2013; Simons et al., 2010). In a setting with pediatric patients who are managing both pain and trauma, education and support for parents may be particularly vital given the nuances in support that are required.
Cultural considerations are also significantly important in these situations. Several cultures hold strong views on seeking support and the traditional coping strategies recommended may not always align with values within that culture (Cauce et al., 2002; Liang et al., 2016). These considerations are notable in the context of research that indicates family factors (e.g., parent/guardian response to pain; Lipani & Walker, 2006; Lynch-Jordan et al., 2013; Sil et al., 2013) to be significantly predictive in overall pediatric pain coping. For example, in Black/African American and Asian families, problems are often solved within the family milieu (Barksdale & Molock, 2009; Rastogi et al., 2014). In terms of coping, several behaviors that would be considered maladaptive methods of coping (e.g., avoidance), as mentioned above, may be considered protective in certain culture contexts when violence or danger are present. Placing extra burden on parents to support their children with coping may also be ill advised at times given the fact that many racial/ethnic minority parents are overstressed and overworked (Nomaguchi & House, 2013). Future research should better seek to understand these avenues for individualized intervention. The findings related to the lack of reporting on participant sample demographics underscore the fact that research should put stronger emphasis on transparent reporting of racial/ethnic factors and examine relevant constructs in diverse populations to increase generalizability of results. Further, future research should be performed to validate known methods of coping assessment in diverse populations. For example, the Responses to Stress Questionnaire (RSQ) has been validated in several diverse samples (e.g., Navajo and Chinese youth; Wadsworth et al., 2004; Xiao et al., 2010) but these efforts should be expanded to additional racial/ethnic minority youth samples (e.g., black/African American, Hispanic/Latino, etc.). Known methods of coping and their correlates with pain and related impairment should also be examined in populations with greater racial/ethnic and socioeconomic diversity given that a significant majority of research to date has been performed in treatment-seeking youth, who are predominantly White/Caucasian (King et al., 2011).
Treatment Considerations for Youth With a History of Pain and Trauma and/or PTSS
Given the preliminary evidence that youth with chronic pain and PTSD may experience decreased response to pain-focused CBT when compared to their non-traumatized peers (Nelson & Cunningham, 2020), the formulation and/or consideration of biobehavioral interventions that capture the unique biopsychosocial facets of pain and trauma symptomatology is warranted. Previous research has also suggested that traditional pain-focused psychotherapies fail to target the impact that stressful or traumatic life events can have on individuals (Lumley & Schubiner, 2019b). A recent review proposed consideration of utilizing trauma-focused psychosocial interventions in youth with chronic pain with particular attention in narrative-exposure (i.e., trauma-focused cognitive behavioral therapy: TF-CBT) or mindfulness-based interventions (Nelson et al., 2021). Directly addressing maladaptive coping strategies in these youth (Nelson et al., 2020) through tailored interventions has the potential to greatly optimize treatment outcomes for this unique population.
In particular, as proposed in previous conceptual research (Nelson et al., 2021), many components of TF-CBT are common to CBT for pain but some are specifically designed to enhance trauma-based coping across multiple domains of child/adolescent functioning (e.g., cognitive, behavioral, emotional, etc.; Mannarino et al., 2014; Palermo, 2012). For example, recognizing the presence and potential impact of a trauma and/or PTSS history on current functioning through focused and deliberate assessment will allow catered intervention response. Engaging in narrative construction relating to pain or trauma history (which is currently lacking in pain-focused CBT; Palermo, 2012) may also more effectively address disengagement coping (i.e., distraction, avoidance) that may occur in response to trauma reminders or pain flares.
In complement, coping strategies commonly taught in both pain- and trauma-focused therapy may include taking steps to increase comfort and decrease stress in daily settings (e.g., maintaining preferential seating in the classroom, identifying a trusted resource at school for daily check-ins). Psychoeducation across pain and trauma contexts reduces perception of threat or danger surrounding the experience of pain or PTSS itself (e.g., “There is something dangerous going on inside my body”, “I am unsafe”; Mannarino et al., 2014), which may be considered a secondary control coping strategy. Thus, teaching trauma-focused cognitive coping (a primary element of TF-CBT; Mannarino et al., 2014) in youth who are also experiencing chronic pain could help optimize adaptive coping strategies in response to these experiences and contribute to more positive functioning long-term.
Relatedly, there is a larger movement of implementing trauma-informed care across pediatric health settings. It has been proposed that trauma-informed care models may improve coping in the management of pain in acute inpatient settings (Agoston et al., 2020) but minimal research has investigated this in the context of pediatric chronic pain. Outside of pain, a trauma-informed protocol developed by Marsac et al. (2016) has been shown to promote patient’s emotional wellbeing and recovery by attending to D-E-F: reduce Distress, promote Emotional support, and remember the Family. This intervention may serve to address distress related to pain and support adaptive coping in pediatric pain samples. Pain Reprocessing Therapy, an intervention that has been studied in adults, may also be worthy of consideration of youth with chronic pain and a history of trauma. Authors originally formulated the intervention using a trauma-informed model and it has shown significant promise in treating pain complaints in adult populations (Ashar et al., 2021; Lumley & Schubiner, 2019a, 2019b). Future research should examine this model and its potential for adaptation to pediatric pain populations.
Limitations
The scoping review method of this paper has several limitations. The search was limited to published, peer-reviewed literature found in traditional abstracting and indexing databases. Gray literature was not searched, and the study could have missed relevant examples of this type of scholarship. Given that the focus of this literature search and coping model was on pediatric populations, findings may also be limited in generalization for more diverse pediatric samples (as mentioned above).
Conclusions and Future Directions
Parallel lines of research indicate that styles of coping may be more deleteriously impacted in youth with chronic pain and a history of psychological trauma and/or PTSS. For example, youth with pain who have been exposed to trauma may be less able to employ adaptive pain coping strategies in certain situations due to perceived or actual threat. The presence of cognitive distortions surrounding pain and trauma may also impact coping strategies. These examples highlight the strong importance of considering a history of trauma and/or PTSS in the prevention and treatment of impairment in youth with chronic pain. Across these populations, certain methods of coping such as cognitive coping or benefit finding (Claar et al., 2008; Soltani et al., 2018) may be more effective in contributing to positive outcomes whereas other more passive tactics may generally compound risk for poorer physical and psychosocial outcomes long-term.
Long-Term Pain Outcomes via Adaptive or Maladaptive Coping
Several studies indicate that certain coping styles, including disengagement strategies, are significantly predictive in the long-term of poorer physical and psychosocial outcomes in youth with chronic pain (Claar et al., 2008; Compas et al., 2012; Kashikar-Zuck et al., 2002). Research also suggests that subjective management of psychological trauma (i.e., coping) is more significantly predictive of chronic PTSS than objective or physical management of the event(s) (Mouthaan et al., 2014). Therefore, it may be that those youth with chronic pain and a history of psychological trauma and/or PTSS experience compounded risk for poorer physical and psychosocial impairment in response to maladaptive coping strategies such as overuse of disengagement strategies, and in turn, greater pain chronicity long-term. Alternatively, research indicates that the use of certain coping strategies like problem-solving or emotion regulation or specific types of distraction (when not used as avoidance coping) can lead to increased wellbeing and optimized or restorative functioning in both pain and trauma populations (Birnie et al., 2014; Mc Elroy & Hevey, 2014; Smith et al., 2016). Future research is needed, most notably longitudinal studies and those focused on measuring active or primary control coping strategies, to better understand the complexities of the relationships and potential trajectories of impairment or function between coping, physical status (e.g., pain), and psychosocial functioning (PTSS, anxiety, depression, stress) in at-risk populations.
Implications for Future Research
The unique impact that a history of trauma and/or PTSS has on the coping of youth with a concurrent chronic issue, such as chronic pain remains unclear. Previous research has highlighted the overall complexities of the relations between biopsychosocial factors contributing to pain chronicity (Gatchel et al., 2007; Nelson et al., 2016). For example, factors such as age, sex, parent pain behaviors, school engagement, and symptoms of anxiety/depression (Claar et al., 2008; Compas et al., 2012; Cunningham et al., 2014; Kashikar-Zuck et al., 2002), can all strongly predict methods of coping in pediatric pain populations. However, these studies have not been performed in populations in which a history of trauma and/or PTSS was an explicit focus, and therefore, our understanding of these factors in this context may be limited. Included in the necessary research going forward, investigations should be undertaken which specifically examine the nuanced relationships between these constructs and coping in pediatric populations with chronic pain and trauma. Using validated coping assessments such as the RSQ (Connor-Smith et al., 2000) in youth with pain and trauma and/or PTSS, qualitative methodology to better allow these patients to report on their experiences with coping with both issues, and research with explicit assessment of trauma and/or PTSS (e.g., semistructured clinical interview, etc.) and analyses to examine the direct and/or indirect relationships (e.g., mediation, moderation, etc.) between trauma and coping in youth with pain would also significantly contribute to our understanding of these constructs. Focusing future research efforts on adaptive coping modalities such as primary control strategies will allow us to better understand and capitalize on those aspects of pain and trauma coping that contribute to increased function and resiliency.
The purported overlap between coping models in pediatric trauma and pain populations also underscores the importance of targeted intervention to optimize outcomes (see treatment considerations detailed above). As mentioned above, preliminary research indicates that certain methods of coping such as cognitive coping or benefit finding may lead towards increased outcomes and potentially resilience in individuals with a pain and trauma history (Claar et al., 2008; Soltani et al., 2018). Methods of resilience in general in pediatric and adult populations is an understudied area and one which needs further understanding to optimize outcomes for these at-risk individuals (Palit et al., 2021). In particular, longitudinal investigations in pediatric populations that include measurement of pain, trauma exposure and PTSS (Wilson & Keane, 2004), coping (e.g., using Compas’ model), and resilience (e.g., optimism; Cousins et al., 2015) are needed.
Supplementary Data
Supplementary data can be found at: https://academic.oup.com/jpepsy.
Funding
The current study was funded by the National Center for Complementary and Integrative Health-NCCIH 1K23AT010643 (to Dr. Nelson) and the National Center for Complementary and Integrative Health-NCCIH K23AT009458 (to Dr. Cunningham).
Conflicts of interest: None.
Supplementary Material
References
- Agoston A. M., Basu R. K., Nelson S. (2020). A universal, trauma-informed approach to pediatric hospital medicine. Hospital Pediatrics, 10(11), 1017–1019. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Association Publishing. [Google Scholar]
- Aromataris E. M. Z. E., & , MunnZ. (2020). JBI manual for evidence synthesis. JBI. [Google Scholar]
- Ashar Y. K., Gordon A., Schubiner H., Uipi C., Knight K., Anderson Z., & , Flood T. F. (2021). Effect of pain reprocessing therapy vs placebo and usual care for patients with chronic back pain: A randomized clinical trial. JAMA Psychiatry. Advance online publication. 10.1001/jamapsychiatry.2021.2669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barksdale C. L., Molock S. D. (2009). Perceived norms and mental health help seeking among African American college students. The Journal of Behavioral Health Services & Research, 36(3), 285–299. [DOI] [PubMed] [Google Scholar]
- Beebe J. A., Kronman C., Mahmud F., Basch M., Hogan M., Li E., Ploski C., Simons L. E. (2021). Gait variability and relationships with fear, avoidance, and pain in adolescents with chronic pain. Physical Therapy, 101(4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birnie K. A., Chambers C. T., Fernandez C. V., Forgeron P. A., Latimer M. A., McGrath P. J., Cummings E. A., Finley G. A. (2014). Hospitalized children continue to report undertreated and preventable pain. Pain Research and Management, 19(4), 198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonilla S., Saps M. (2013). Early life events predispose the onset of childhood functional gastrointestinal disorders. Revista de Gastroenterologia de Mexico, 78(2), 82–91. [DOI] [PubMed] [Google Scholar]
- Casey C. Y., Greenberg M. A., Nicassio P. M., Harpin R. E., Hubbard D. (2008). Transition from acute to chronic pain and disability: A model including cognitive, affective, and trauma factors. Pain, 134(1-2), 69–79. [DOI] [PubMed] [Google Scholar]
- Cauce A. M., Domenech-Rodríguez M., Paradise M., Cochran B. N., Shea J. M., Srebnik D., Baydar N. (2002). Cultural and contextual influences in mental health help seeking: A focus on ethnic minority youth. Journal of Consulting and Clinical Psychology, 70(1), 44–55. [DOI] [PubMed] [Google Scholar]
- Claar R. L., Baber K. F., Simons L. E., Logan D. E., Walker L. S. (2008). Pain coping profiles in adolescents with chronic pain. Pain, 140(2), 368–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas B. E., Banez G. A., Malcarne V., Worsham N. (1991). Perceived control and coping with stress: A developmental perspective. Journal of Social Issues, 47(4), 23–34. [Google Scholar]
- Compas B. E., Boyer M. C., Stanger C., Colletti R. B., Thomsen A. H., Dufton L. M., Cole D. A. (2006). Latent variable analysis of coping, anxiety/depression, and somatic symptoms in adolescents with chronic pain. Journal of Consulting and Clinical Psychology, 74(6), 1132–1142. [DOI] [PubMed] [Google Scholar]
- Compas B. E., Harding Thomsen A. (1999). Coping and response s to stress among children with recurrent abdominal pain. Journal of Developmental and Behavioral Pediatrics, 20(5), 323–324. [DOI] [PubMed]
- Compas B. E., Jaser S. S., Dunn M. J., Rodriguez E. M. (2012). Coping with chronic illness in childhood and adolescence. Annual Review of Clinical Psychology, 8, 455–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor-Smith J. K., Compas B. E., Wadsworth M. E., Thomsen A. H., Saltzman H. (2000). Responses to stress in adolescence: Measurement of coping and involuntary stress responses. Journal of Consulting and Clinical Psychology, 68(6), 976–992. [PubMed] [Google Scholar]
- Cousins L. A., Cohen L. L., Venable C. (2015). Risk and resilience in pediatric chronic pain: Exploring the protective role of optimism. Journal of Pediatric Psychology, 40(9), 934–942. [DOI] [PubMed] [Google Scholar]
- Cunningham N. R., Lynch-Jordan A., Barnett K., Peugh J., Sil S., Goldschneider K., Kashikar-Zuck S. (2014). Child pain catastrophizing mediates the relation between parent responses to pain and disability in youth with functional abdominal pain. Journal of Pediatric Gastroenterology and Nutrition, 59(6), 732–738. 10.1097/MPG.0000000000000529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de la Vega R., Miró J., Esteve R., Ramírez-Maestre C., López-Martínez A. E., Jensen M. P. (2019). Sleep disturbance in individuals with physical disabilities and chronic pain: The role of physical, emotional and cognitive factors. Disability and Health Journal, 12(4), 588–593. [DOI] [PubMed] [Google Scholar]
- Dempsey M., Stacy O., Moely B. (2000). “Approach” and “avoidance” coping and PTSD symptoms in innercity youth. Current Psychology, 19(1), 28–45. [Google Scholar]
- Edwards R. R., Dworkin R. H., Sullivan M. D., Turk D. C., Wasan A. D. (2016). The role of psychosocial processes in the development and maintenance of chronic pain. The Journal of Pain, 17(9 Suppl), T70–T92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elzy M., Clark C., Dollard N., Hummer V. (2013). Adolescent girls’ use of avoidant and approach coping as moderators between trauma exposure and trauma symptoms. Journal of Family Violence, 28(8), 763–770. [Google Scholar]
- Endler N., Parker J. D. (2008). Coping inventory for stressful situations [Database record]. APA PsycTests.
- Gatchel R. J., Peng Y. B., Peters M. L., Fuchs P. N., Turk D. C. (2007). The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychological Bulletin, 133(4), 581–624. 10.1037/0033-2909.133.4.581 [DOI] [PubMed] [Google Scholar]
- Hamblen J., Barnett E. (2016). PTSD in children and adolescents. National Center for PTSD. www.ncptsd. org [Google Scholar]
- Holley A. L., Wilson A. C., Noel M., Palermo T. M. (2016). Post-traumatic stress symptoms in children and adolescents with chronic pain: A topical review of the literature and a proposed framework for future research. European Journal of Pain (London, England), 20(9), 1371–1383. 10.1002/ejp.879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashikar-Zuck S., Cunningham N., Peugh J., Black W. R., Nelson S., Lynch-Jordan A. M., Pfeiffer M., Tran S. T., Ting T. V., Arnold L. M., Carle A., Noll J., Powers S. W., Lovell D. J. (2019). Long-term outcomes of adolescents with juvenile-onset fibromyalgia into adulthood and impact of depressive symptoms on functioning over time. Pain, 160(2), 433–441. 10.1097/j.pain.0000000000001415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashikar-Zuck S., Sil S., Lynch-Jordan A. M., Ting T. V., Peugh J., Schikler K. N., Hashkes P. J., Arnold L. M., Passo M., Richards-Mauze M. M., Powers S. W., Lovell D. J. (2013). Changes in pain coping, catastrophizing, and coping efficacy after cognitive-behavioral therapy in children and adolescents with juvenile fibromyalgia. The Journal of Pain, 14(5), 492–501. 10.1016/j.jpain.2012.12.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashikar-Zuck S., Vaught M. H., Goldschneider K. R., Graham T. B., Miller J. C. (2002). Depression, coping, and functional disability in juvenile primary fibromyalgia syndrome. The Journal of Pain, 3(5), 412–419. https://www.ncbi.nlm.nih.gov/pubmed/14622745 [DOI] [PubMed] [Google Scholar]
- Keogh E., Book K., Thomas J., Giddins G., Eccleston C. (2010). Predicting pain and disability in patients with hand fractures: Comparing pain anxiety, anxiety sensitivity and pain catastrophizing. European Journal of Pain (London, England), 14(4), 446–451. [DOI] [PubMed] [Google Scholar]
- King S., Chambers C. T., Huguet A., MacNevin R. C., McGrath P. J., Parker L., MacDonald A. J. (2011). The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain, 152(12), 2729–2738. 10.1016/j.pain.2011.07.016 [DOI] [PubMed] [Google Scholar]
- Lami M. J., Martínez M. P., Miró E., Sánchez A. I., Guzmán M. A. (2018). Catastrophizing, acceptance, and coping as mediators between pain and emotional distress and disability in fibromyalgia. Journal of Clinical Psychology in Medical Settings, 25(1), 80–92. [DOI] [PubMed] [Google Scholar]
- Lazarus R. S., Folkman S. (1984). Stress, appraisal, and coping. Springer publishing company. [Google Scholar]
- Liang J., Matheson B. E., Douglas J. M. (2016). Mental health diagnostic considerations in racial/ethnic minority youth. Journal of Child and Family Studies, 25(6), 1926–1940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipani T. A., Walker L. S. (2006). Children's appraisal and coping with pain: Relation to maternal ratings of worry and restriction in family activities. Journal of Pediatric Psychology, 31(7), 667–673. 10.1093/jpepsy/jsj038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe S. R., Walsh K., Uddin M., Galea S., Koenen K. C. (2014). Bidirectional relationships between trauma exposure and posttraumatic stress: A longitudinal study of Detroit residents. Journal of Abnormal Psychology, 123(3), 533–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley M. A., Schubiner H. (2019a). Emotional awareness and expression therapy for chronic pain: Rationale, principles and techniques, evidence, and critical review. Current Rheumatology Reports, 21(7), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley M. A., Schubiner H. (2019b). Psychological therapy for centralized pain: An integrative assessment and treatment model. Psychosomatic Medicine, 81(2), 114–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch-Jordan A. M., Kashikar-Zuck S., Szabova A., Goldschneider K. R. (2013). The interplay of parent and adolescent catastrophizing and its impact on adolescents' pain, functioning, and pain behavior. The Clinical Journal of Pain, 29(8), 681–688. 10.1097/AJP.0b013e3182757720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch-Jordan A. M., Sil S., Peugh J., Cunningham N., Kashikar-Zuck S., Goldschneider K. R. (2014). Differential changes in functional disability and pain intensity over the course of psychological treatment for children with chronic pain. Pain, 155(10), 1955–1961. 10.1016/j.pain.2014.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannarino A. P., Cohen J. A., Deblinger E. (2014). Trauma-focused cognitive-behavioral therapy. In S. Timmer, & A. Urquiza (Eds.), Evidence-based approaches for the treatment of maltreated children (pp. 165–185). Springer. [Google Scholar]
- Marsac M. L., Kassam-Adams N., Hildenbrand A. K., Nicholls E., Winston F. K., Leff S. S., Fein J. (2016). Implementing a trauma-informed approach in pediatric health care networks. JAMA Pediatrics, 170(1), 70–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maujean A., Gullo M. J., Andersen T. E., Ravn S. L., Sterling M. (2017). Post-traumatic stress symptom clusters in acute whiplash associated disorder and their prediction of chronic pain-related disability. Pain Reports, 2(6), e631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mc Elroy S., Hevey D. (2014). Relationship between adverse early experiences, stressors, psychosocial resources and wellbeing. Child Abuse & Neglect, 38(1), 65–75. [DOI] [PubMed] [Google Scholar]
- Molton I. R., Stoelb B. L., Jensen M. P., Ehde D. M., Raichle K. A., Cardenas D. D. (2009). Psychosocial factors and adjustment to chronic pain in spinal cord injury: Replication and cross-validation. Journal of Rehabilitation Research and Development, 46(1), 31–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouthaan J., Sijbrandij M., Luitse J. S., Goslings J. C., Gersons B. P., Olff M. (2014). The role of acute cortisol and DHEAS in predicting acute and chronic PTSD symptoms. Psychoneuroendocrinology, 45, 179–186. [DOI] [PubMed] [Google Scholar]
- Nader K. (2016). Assessment of trauma in youths: Understanding issues of age, complexity, and associated variables. Routledge. [Google Scholar]
- Nelson S., Beveridge J. K., Mychasiuk R., Noel M. (2021). Adverse childhood experiences (ACEs) and internalizing mental health, pain, and quality of life in youth with chronic pain: A longitudinal examination. The Journal of Pain, 22(10), 1210–1220. [DOI] [PubMed] [Google Scholar]
- Nelson S., Borsook D., Enlow M. B. (2021). Targeting the stress response in pediatric pain: Current evidence for psychosocial intervention and avenues for future investigation. Pain Reports, 6(3), e953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson S., Burns M., McEwen B., Borsook D. (2020). Stressful experiences in youth: “Set-up” for diminished resilience to chronic pain. Brain, Behavior, & Immunity-Health. 100095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson S., Cunningham N. (2020). The impact of posttraumatic stress disorder on clinical presentation and psychosocial treatment response in youth with functional abdominal pain disorders: An exploratory study. Children, 7(6), 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson S., Cunningham N., Kashikar-Zuck S. (2016). A conceptual framework for understanding the role of adverse childhood experiences in pediatric chronic pain. Clinical Journal of Pain. 10.1097/AJP.0000000000000397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson S., Simons L., Logan D. (2018). The incidence of Adverse Childhood Experiences (ACEs) and their association with pain-related and psychosocial impairment in youth with chronic pain. The Clinical Journal of Pain, 34(5), 402–408. [DOI] [PubMed] [Google Scholar]
- Nelson S., Smith K., Sethna N., Logan D. (2019). Youth with chronic pain and a history of adverse childhood experiences in the context of multidisciplinary pain rehabilitation. The Clinical Journal of Pain, 35(5), 420–427. [DOI] [PubMed] [Google Scholar]
- Neville A., Soltani S., Pavlova M., Noel M. (2018). Unravelling the relationship between parent and child PTSD and pediatric chronic pain: The mediating role of pain catastrophizing. The Journal of Pain, 19(2), 196–206. [DOI] [PubMed] [Google Scholar]
- Noel M., Wilson A. C., Holley A. L., Durkin L., Patton M., Palermo T. M. (2016). Posttraumatic stress disorder symptoms in youth with vs without chronic pain. Pain, 157(10), 2277–2284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nomaguchi K., House A. N. (2013). Racial-ethnic disparities in maternal parenting stress: The role of structural disadvantages and parenting values. Journal of Health and Social Behavior, 54(3), 386–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olff M., Langeland W., Gersons B. P. (2005). The psychobiology of PTSD: Coping with trauma. Psychoneuroendocrinology, 30(10), 974–982. [DOI] [PubMed] [Google Scholar]
- Page M. J., McKenzie J. E., Bossuyt P. M., Boutron I., Hoffmann T. C., Mulrow C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., McGuinness, L. A. ... Moher, Det al. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palermo T. M. (2012). Cognitive-behavioral therapy for chronic pain in children and adolescents. Oxford University Press. [Google Scholar]
- Palermo T. M., Law E. F., Zhou C., Holley A. L., Logan D., Tai G. (2015). Trajectories of change during a randomized controlled trial of internet-delivered psychological treatment for adolescent chronic pain: How does change in pain and function relate? Pain, 156(4), 626–634. 10.1097/01.j.pain.0000460355.17246.6c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palit S., Palermo T. M., Fillingim R. B., Bartley E. J. (2021). Topical review: Examining multidomain pain resilience in late adolescents and young adults. Journal of Pediatric Psychology, 46(3), 280–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton M., Forster V. J., Forbes C., Stokoe M., Noel M., Carlson L. E., Birnie K. A., Reynolds K., Schulte F. (2021). Characterizing pain in long-term survivors of childhood cancer. Supportive Care in Cancer. 10.1007/s00520-021-06386-4 [DOI] [PubMed] [Google Scholar]
- Rastogi P., Khushalani S., Dhawan S., Goga J., Hemanth N., Kosi R., Sharma R. K., Black B. S., Jayaram G., Rao V. (2014). Understanding clinician perception of common presentations in South Asians seeking mental health treatment and determining barriers and facilitators to treatment. Asian Journal of Psychiatry, 7, 15–21. [DOI] [PubMed] [Google Scholar]
- Resnick M. D. (2000). Protective factors, resiliency, and healthy youth development. Adolescent Medicine (Philadelphia, Pa.), 11(1), 157–164. [PubMed] [Google Scholar]
- Rimsza M. E., Berg R. A., Locke C. (1988). Sexual abuse: Somatic and emotional reactions. Child Abuse & Neglect, 12(2), 201–208. [DOI] [PubMed] [Google Scholar]
- Seiffge-Krenke I., Pakalniskiene V. (2011). Who shapes whom in the family: Reciprocal links between autonomy support in the family and parents’ and adolescents’ coping behaviors. Journal of Youth and Adolescence, 40(8), 983–995. [DOI] [PubMed] [Google Scholar]
- Sil S., Lynch-Jordan A., Ting T. V., Peugh J., Noll J., Kashikar-Zuck S. (2013). Influence of family environment on long-term psychosocial functioning of adolescents with juvenile fibromyalgia. Arthritis Care & Research), 65(6), 903–909. 10.1002/acr.21921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons L. E., Logan D. E., Chastain L., Cerullo M. (2010). Engagement in multidisciplinary interventions for pediatric chronic pain: Parental expectations, barriers, and child outcomes. The Clinical Journal of Pain, 26(4), 291–299. 10.1097/AJP.0b013e3181cf59fb [DOI] [PubMed] [Google Scholar]
- Skinner E. A., Wellborn J. G. (2019). Coping during childhood and adolescence: A motivational perspective. In D. L. Featherman, R. M. Lerner, & M. Perlmutter (Eds.), Life-span development and behavior (pp. 91–134). Routledge. [Google Scholar]
- Smith M. M., Saklofske D. H., Keefer K. V., Tremblay P. F. (2016). Coping strategies and psychological outcomes: The moderating effects of personal resiliency. The Journal of Psychology, 150(3), 318–332. [DOI] [PubMed] [Google Scholar]
- Smith W. R., Strachan E. D., Buchwald D. (2009). Coping, self-efficacy and psychiatric history in patients with both chronic widespread pain and chronic fatigue. General Hospital Psychiatry, 31(4), 347–352. [DOI] [PubMed] [Google Scholar]
- Soltani S., Neville A., Hurtubise K., Hildenbrand A., Noel M. (2018). Finding silver linings: A preliminary examination of benefit finding in youth with chronic pain. Journal of Pediatric Psychology, 43(3), 285–293. [DOI] [PubMed] [Google Scholar]
- Soltani S., van Ryckeghem D. M., Vervoort T., Heathcote L. C., Yeates K. O., Sears C., Noel M. (2020). Clinical relevance of attentional biases in pediatric chronic pain: An eye-tracking study. Pain. Advance online publication. 10.1097/j.pain.0000000000002346 [DOI] [PubMed] [Google Scholar]
- Tricco A. C., Lillie E., Zarin W., O'Brien K. K., Colquhoun H., Levac D., Moher D., Peters M. D. J., Horsley T., Weeks L., Hempel S., Akl E. A., Chang C., McGowan J., Stewart L., Hartling L., Aldcroft A., Wilson M. G., Garritty C., Straus S. E. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. [DOI] [PubMed] [Google Scholar]
- Tsur N. (2020). Chronic pain personification following child abuse: The imprinted experience of child abuse in later chronic pain. Journal of Interpersonal Violence. Advance online publication. 10.1177/0886260520944529. [DOI] [PubMed] [Google Scholar]
- Wadsworth M. E., Rieckmann T., Benson M. A., Compas B. E. (2004). Coping and responses to stress in Navajo adolescents: Psychometric properties of the Responses to Stress Questionnaire. Journal of Community Psychology, 32(4), 391–411. [Google Scholar]
- Wilson J. P., Keane T. M. (2004). Assessing psychological trauma and PTSD. Guilford Press. [Google Scholar]
- Wohlheiter K. A., Dahlquist L. M. (2013). Interactive versus passive distraction for acute pain management in young children: The role of selective attention and development. Journal of Pediatric Psychology, 38(2), 202–212. [DOI] [PubMed] [Google Scholar]
- Wojtowicz A. A., Banez G. A. (2015). Adolescents With chronic pain and associated functional disability: A descriptive analysis. Journal of Child Health Care, 19(4), 478–484. [DOI] [PubMed] [Google Scholar]
- Xiao J., Yao S., Zhu X., Zhang C., Auerbach R. P., McWhinnie C. M., Abela J. R. (2010). The responses to stress questionnaire: Construct validity and prediction of depressive and social anxiety symptoms in a sample of Chinese adolescents. Stress and Health, 26(3), 238–249. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.