Abstract
Delaying routine health care has been prevalent during the COIVD-19 pandemic. Macro-level data from this period reveals that U.S. patients under-utilized routine health care services such as primary care visits, preventative tests, screenings, routine optometry care, dental appointments, and visits for chronic disease management. Yet, there is a gap in research on how and why patients understand risks associated with seeking or delaying routing health care during an infectious disease pandemic. Our research addresses this gap based on semi-structured interviews with 40 participants living in regions across the United States. By building upon Unger-Saldaña and Infante-Castañeda's model of delayed health care, we extend this model by articulating how health care delays happen during an infectious disease pandemic. Specifically, we show how perceptions of uncertainty and subjective risk assessments shape people's decisions to delay routine health care while they operate at two levels, internal and external to one's social bubble, interacting with each other.
Keywords: Delayed health care, COVID-19, Risk assessment, Decision making
1. Introduction
The global response to COVID-19 was marked by economic shutdowns with aims to mitigate the spread of COVID-19 by restricting people's interaction. Unlike some countries, the United States did not have a centralized response to COVID-19 (Park and Fowler, 2021). While many states implemented stay-at-home orders in response to rising COVID-19 cases, state and local crisis response efforts often placed a large amount of responsibility for risk management on the public, leading to wide discrepancies in individuals' understanding of risks associated with different behaviors (Chan et al., 2020). Within this broader context, a key area of decision making for individuals is seeking (or deferring) outpatient health care services, including primary health care, specialty health care, optometry, and dental care. In this study, we refer to these types of care as routine health care.
Researchers have found a broad trend towards deferring routine health care during COVID-19—as much as 48% in one study (Atherly et al., 2020). Overall, health services revenue in the United States fell 2.4% compared to 2019, and spending on health services fell sharply in March and April of 2020, with the largest drop in outpatient services (Cox et al., 2021). Dental providers saw a large decrease in revenue as well (Cox et al., 2021). This is a crucial topic not only because of the magnitude of delays that occurred during the pandemic; for example, breast cancer and colon cancer screenings dropped by more than 80% at the height of the pandemic (Vose, 2020), but also due to the exacerbating inequality in delaying health care (Mafi et al., 2022). This massive volume of delayed routine care will negatively impact quality of life, morbidity, and mortality for the U.S. population and likely impose additional as-yet-unknown negative consequences for many years to come (Woolf et al., 2020).
Decision making about seeking health care during the pandemic is complicated. This context is likely leading people to different decisions than would be made under normal circumstances, as evidenced by decreased health care utilization in 2020 and 2021 compared to those before the pandemic (Cox et al., 2021). However, how people make decisions about obtaining or delaying routine health care during the COVID-19 pandemic, and what factors shape these decisions, is under-studied. While prior models of health care delay are useful in explaining health care delay during COVID-19 (e.g., Unger-Saldaña and Infante-Castañeda, 2011), there is a limit to explainining how sociocultural and individual-level contexts interact with each other and with other societal and structural factors to shape decisions about delaying care. Part of the complexity in understanding the process of health care delay during COVID-19 stems from a lack of contextualized models or theories that describe people's decision making about delay when a public health crisis imposes new forms of risks. To fill this gap, our study answers the following research questions:
-
1.
How do people assess risks associated with seeking or delaying health care during the COVID-19 pandemic given existing uncertainty?
-
2.
How do people make decisions about health care delay based on their risk assessment?
Our research contributes to the interconnected health services, health policy, and health communications literature on delayed health care; the risk studies literature on risk perception and risk assessment; and the crisis informatics literature on how people behave during crises by contextualizing individuals’ risk assessment and health care delay within infectious disease crises. Specifically, we detail how and why people feel the need to delay health care during a pandemic and how they make those decisions. Based on empirical evidence, we develop a theoretical framework for understanding why participants made the decision to delay health care and delineate the social and personal factors that influence their decision making. This work will broaden our understanding of delayed health care during a public health crisis. The results will inform practitioners and policymakers as well by helping them examine how to best communicate risks to the public, such as helping people assess risks and receive in-person medical care.
2. Related work
2.1. Delaying health care
The literature on health care delay shows that delays are the result of complex interactions. As Unger-Saldaña and Infante-Castañeda (2011) describe, “delay is a result of the interplay between the patient's sociocultural context, individual characteristics that influence symptom interpretation and decision-making, interaction with the social network and types of support obtained, and aspects of the local health services” (p.1096). Individual-level characteristics which shape delays in health care include interpretations of one's health, such as experiences of bodily discomfort related to illness (Beedholm et al., 2019; Coventry et al., 2017; Nieminen et al., 2018), relative (mis)trust in the health care system and medical professionals (Kannan and Veazie, 2014; Powell et al., 2019; Simons et al., 2017), and perceptions or experiences of the difficulty in navigating the U.S. health care system (i.e., if navigation is highly frustrating, the decisions to delay health care increase) (Brunner et al., 2020; Percac-Lima et al., 2015; Sofaer, 2009). Social network features—such as a lack of social support—can also negatively affect individuals' ability to make timely decisions to seek medical attention (Dhand et al., 2019; Reisinger et al., 2018).
The sociocultural context of health care services can lead to delays in utilizing health care, because people tend to delay care when they lack the ability to access services, even when they otherwise want to access them (Lee et al., 2020; Taber et al., 2015). In contexts where health care services are unavailable—such as contexts where low-income individuals do not have access to adequate insurance coverage—delays in care are more likely (Jelani et al., 2020; Kent et al., 2013; Siminoff et al., 2014; Smolderen et al., 2010). Unavailability of services in the appropriate language or a culturally sensitive modality can also lead to delays in health care (Lightfoot et al., 2019; Simon et al., 2015). People may also decide to delay health carewhen they perceive that they will experience discrimination due to their gender (Chen et al., 2015; Galdas et al., 2010), race (Armenta and Sarabia, 2020; Attanasio and Hardeman, 2019; Gullatte et al., 2010), or identification within the LBGTQ community—specifically transgender patients (Jaffee et al., 2016; Lehavot et al., 2017; Macapagal et al., 2016)—often because they have heard accounts from others in their social networks about discriminatory treatment.
While past research on delaying care has examined features of sociocultural contexts that shape utilization or delay of care for different populations or individuals, the COVID-19 pandemic changed not only the sociocultural context of health care delivery in a rapid and broad manner, but also the roles of uncertainty and individuals' risk assessment. The decrease in health care utilization, primarily in ambulatory services, aligns with past public health crises, such as SARS which also saw declines in outpatient care (Chang et al., 2004). Any social interaction presents risk of COVID-19 transmission to individuals, so seeking health care itself has become a heightened risk from a sociocultural context perspective. Because these changes have altered people's decision-making processes about whether and how to seek or delay health care, past models of health care delay need to be adjusted under these new circumstances.
2.2. Individual's Risk Assessment and Perceived Vulnerability
The crisis informatics literature has previously identified multidimensional factors that drive decision making during times of crisis, thus can inform the study of decision making about treatment delay during crises. This literature has found that during crises, people's decisions are shaped by a desire to minimize (perceived) risks (Gui et al., 2018; Reuter et al., 2018; Wise et al., 2020). Further, decision making during crises tends to be more difficult, because individuals engage in sensemaking processes amidst heightened uncertainty (Pine et al., 2021; Kou et al., 2017; Huang et al., 2015).
Truly, it is increasingly incumbent on individuals to assess and manage risks, because risk-related decisions (e.g., assessing and understanding weighted risk, balancing risks, perceiving self and others' risk) require confronting an uncertain future. In other words, risk relates not to what is known to be happening in a current state, but what might happen in the future (Adam et al., 2000). Risk assessment is defined as enacting methods to minimize or prevent any potential negative outcomes from a hazard (Lupton, 1999). Much of the risk literature focuses on individual-level factors that shape decisions about risk. For example, research on health care decision making finds that intuition, emotion, and a desire to retain control over one's health are key factors in an individual's decision making about how to manage risks (Keshet and Popper-Giveon, 2018). Further, past research suggests that how patients view their own risk often influences their health care decisions. Oftentimes, when diagnosed with a health condition, clinicians ascribe and communicate risk status to patients. This new status alters patients' health identities, because the patient becomes aware of new threats to their health focused on risk of disease. This “measured vulnerability” (Gillespie, 2012)—defined as statistical measures that are used with patients to determine the risk of developing a disease—often produces increased uncertainty and anxiety in individuals labeled "statistically at-risk.” This also can make it difficult for patients to identify as a “healthy person,” and lead to a feeling of heightened vulnerability.
While individual characteristics clearly shape risk assessments and decisions, the risk literature shows that risk assessments and decisions are also deeply shaped by the contexts in which individuals are embedded. For example, an individual's cultural, political, and moral contexts shape decisions about whether or not to take vaccines (Kumar et al., 2016; Larson et al., 2015). Complicating the picture further, it is also clear that multiple risks coexist within the complex, overlapping sociocultural contexts in which individuals are embedded. This can create tensions for individuals who must assess each risk present as well as the interplay between risks, and balance risks against each other when making risk-related decisions.
2.3. Delaying health care during the COVID-19 pandemic
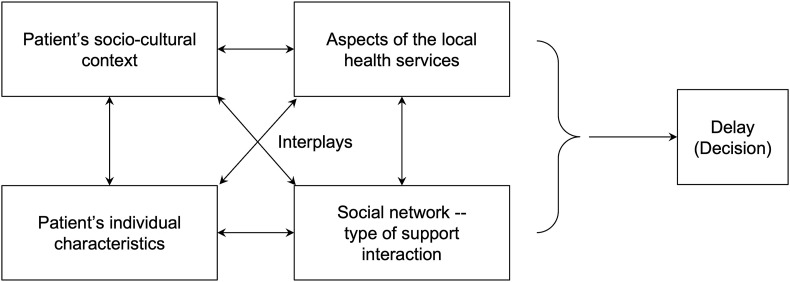
As described above, studies of health care delay delineate individual and contextual factors that shape decisions to delay health care. Also, they examine interplays between these factors that, taken together, lead to decisions to delay or utilize health care. To date, Unger-Saldaña and Infante-Castañeda’s (2011) model (Fig. 1 ) provides the most comprehensive theoretical framework of decisions to delay health care. They conceptualize decisions to delay health care as an interplay between a patient's individual characteristics, socio-cultural context, social network, and aspects of local health care services.
Fig. 1.
An illustration of the theoretical framework of decision making to delay health care (Unger-Saldaña and Infante-Castañeda, 2011).
However, Unger-Saldaña and Infante-Castañeda's (2011) theoretical framework has a limitation to explain health care delay during a global pandemic, because (1) the dimensions of uncertainty have been diversified and complicated (e.g. due to the nature of the infectious disease and new risks posed by the broader societal crisis such as economic risk and crumbling institutions) (Pine et al., 2021); (2) the existing framework is still very high-level and abstract, thus does not sufficiently describe decision making processes focused on delaying health care in the new pandemic context; and (3) it is unclear what the interplay between factors looks like between sociocultural context and social networks along with the interplay between individual characteristics and local health services. Through examining lived experiences of individuals making decisions about whether to utilize or delay routine care during the COVID-19 pandemic, this paper fills a pressing gap in the health care delay literature on how individuals assess risks and make risk-related decisions about delaying health care during a widespread pandemic. This paper also contributes to the crisis informatics literature, which, to date, has overlooked delay in routine health care as an impact of disasters.
3. Methods
Our research approach was inductive, meaning that we began with data and our theorized story arose from data (Charmaz, 2006). Our approach also had elements of abductive research (Timmermans and Tavory, 2012), because we began our research with a literature review and, upon identifying an existing multidimensional model of health care delay (Fig. 1), we used our analysis to bring our data into conversation with this existing model. This approach resulted in a refined model of health care delay oriented around risk assessment and risk-related decision making within the sociocultural context of a sweeping crisis, which is described in the findings and discussion.
3.1. Participants
Our study included 40 participants, who ranged in age from 21 to 70 with a mean age of 40. Participants resided in 14 states (AZ, CA, IL, IN, TX, WA, WI, TN, MA, MN, VT, NJ, OR. CT) where 50% of participants resided in Arizona. This was due to an easier level of recruitment based on the research team's networks. Participants were recruited via a study flier disseminated through multiple nationwide nonprofit listservs to which we had access and through social media. Individuals interested in the study were directed to complete a short screening questionnaire. The study team selected 40 participants from these responses with an aim to create a participant pool that was diverse in age, location, and perceived health risk from COVID-19. 20 participants considered themselves to have elevated health risk from COVID-19 due to age or underlying health conditions. 9 considered themselves to be at economic risk due to lack of employment, inability to find work or had a household member financially impacted. 10 were essential workers and were required to interact in-person with community members at work. We did not collect income or ethnic information on participants, because comparison of experiences across ethnic and socioeconomic groups was not the focus of the study. Also, these data can be sensitive to collect, and we did not want to raise concerns about privacy that may prevent participants from consenting to be re-interviewed at a later time. However, through interviews, we learned that participants have varied incomes from very low income to upper middle-class as well as diverse ethnic backgrounds (e.g., Black, LatinX, Asian, and White).
3.2. Data collection
We conducted the first round of semi-structured interviews with all 40 participants via phone or zoom (between April and June 2020). Interviews lasted roughly 60 min and were recorded and transcribed. Each participant was given a $20 gift card for their participation. The interview guide was designed to understand individuals’ lived experiences of risks in relation to the COVID-19 pandemic, risk-related decisions, information sources that informed risk assessment and risk-related decision making, and challenges with accessing appropriate information. A subsection of the interview questions focused explicitly on utilization of routine health care during the pandemic.
We conducted a second round of interviews with 15 participants between December 2020 and March 2021 (pre-vaccine rollout). During the first round of interviews, we noted that many participants described delaying routine health care due to perceived risk of utilizing health care during the pandemic. Thus, the second interview guide probed more deeply the decision-making process to delay health care, and also asked about participant experiences with telemedicine (the data on telemedicine experiences are outside the scope of the current paper and will be reported elsewhere).
3.3. Data analysis
Data analysis began while we were still conducting the first round of interviews, so that preliminary analyses could shape ongoing data collection. Transcribed interviews were uploaded to a web-based qualitative analytic software program, Dedoose, to facilitate the coding process. Open coding was for capturing emerging themes from data without predefined themes. After the completion of the first round of interviews and open coding on all first-round interview transcripts, the authors used the open codes to create a structured code set and re-coded data using it. Structured coding included condensing initial codes into overarching themes along with memo writing. Memos consisted of initial ideas about trends emerging through the structured codes (Charmaz, 2006). Transcripts from the second round of interviews were analyzed using the structured code set. This allowed us to discover emerging patterns during the first round of interviews and allowed for further development of the research questions.
Through open and structured coding, we found common experiences emerging from the data surrounding delayed health care. We utilized the constant comparative method (Glaser, 1965) throughout data collection and analysis to theorize how people made decisions to seek or delay health care during COVID-19. This resulted in a set of themes and an extension of the current model of health care delay decisions, presented next.
4. Findings
4.1. Subjective risk assessment in utilizing in-person health care
Of 40 participants, 15 reported that they had delayed routine health care (i.e., appointments related to chronic conditions or preventative health care) during one or both interviews. Broadly, participants’ decisions to delay were centered on perceived risks of seeking in-person health care. As we illustrate below, all participants—whether they delayed health care or not—believed that seeking health care in person presented a danger of COVID-19 infection. Yet, while the perception of seeking in-person health care during the pandemic was considered hazardous by all participants, some decided to delay routine care while others did not.
Our analysis uncovered the complex risk assessment that individuals carried out based on their perceptions of the relative risks embedded in either receiving or delaying routine in-person care. Specifically, in assessing COVID-19 risks, participants developed complex understandings of vulnerability to COVID-19 infection. We call this unique positioning of COVID-19 risks a “self-defined locus of risk,” which we define as a personal risk calculus that takes into account both one's own vulnerability as well as the vulnerabilities of those that they come into physical contact with (e.g., those they live with or otherwise come into close physical contact with, such as those they are in a “pod” with). We call these other people in which individuals will factor into their risk assessment the “social bubble.” A “locus” is a particular position, point, or place.
Because COVID-19 is a highly infectious disease that can be easily passed from one person to another and exerts outsized effects on people with certain characteristics, participants allocated risks of infection and sickness posed by COVID-19 at the intersection of their own perceived health vulnerabilities and the health vulnerabilities of those they were in close, unprotected physical proximity to. Further, we found that the self-defined locus of risk was shaped by certain factors including health communications, historical perceptions of vulnerability (of self and others), perceived risks of bodily harm posed by COVID-19, and uncertainty about the risks posed by seeking health care during COVID-19. Finally, we found that people weighed the risks of delaying routine health care against the risk of being exposed to COVID-19, a calculus that was colored by 1) their self-defined locus of risk, and 2) the availability of alternate “lower risk” options for health care treatment such as telemedicine.
4.2. Perceived uncertainty related to external factors
Perceptions of uncertainty about risk related to receiving in-person health care stemmed from two sources: factors internal and external to oneself or one's social bubbles. All participants that were interviewed saw seeking in-person health care as presenting a high risk for contracting COVID-19 for a multitude of reasons, all of which hinged on uncertainty. People were uncertain about the cleanliness of medical offices, medical offices' access to safety measures or adherence to safety protocols, how many people would be at the office, and whether or not they would encounter someone sick with the virus. All participants described medical offices as places that presented high uncertainty and little control over sources of risk. For example, P1 described:
“People go to the doctor’s office when they’re not feeling good, and they may or may not have a compromised immune system already, and then goin’ into the doctor … [J]ust because I’m doing everything that I can [to take care of myself], doesn’t mean the people in the office are doing everything they can. I think medical staff would, but I’m not very trusting with [the patients].”
Similarly, P2 described a decision to delay an eye appointment:
“Doctors see a lotta people. Who are they touching? What precautions are they taking? I didn’t wanna expose myself to that at all at the time because I didn’t know enough. I still wouldn’t today 'cause it’s not that important to me. I can wait a year …”
As these quotes indicate, perceived lack of transparency about safety precautions from health care facilities exacerbated perceptions of risk associated with health care. However, even when medical offices clearly communicated safety precautions (e.g., cleaning procedures) to patients, some participants still saw getting in-person health care as a source of risk that they were not willing to take on. As P3 said, “Yes, they've cleaned it and so on, but let's just reduce risk as much as we possibly can [by not utilizing health care at all].” P3, a parent, pointed out that taking children to get medical care multiplied the risk of exposure:
“When I make [a medical] appointment, ‘cause I’m a single parent, I bring all five kids at one time ….to me, it’s double the exposure, double the risk. It just doesn’t make sense. I’m not gonna do that, so I just waited and delayed. They said we can come in now because I wanted to get everyone the flu shot, but we … haven't gone back."
Another participant (P5) pointed to urgent care and emergency departments as especially “high risk” settings: “… taking anyone into an urgent care or an ER is extremely risky, because you don't know who's walking in next to you and what you can potentially be exposed to.” Uncertainty also surrounded the dangers COVID-19 might impose on them or those they were in contact with, because COVID-19 itself acts in unpredictable ways and impacts different people differently. P6 had previously contracted COVID-19 and was sedated and placed on a ventilator in a hospital for treatment. Although he learned a lot from his first-hand experience with COVID-19, he felt that “it turned out pretty well” and thought he was “in decent shape all things considered.” He still faced uncertainty about his long-term symptoms (for example, his blood oxygen levels still dipped to dangerously low levels at night, and he was not sure if that would ever go back to normal), whether his infection gave him any immunity against future COVID-19 infections, or how future infections might further affect his health. Additionally, there was uncertainty not only about how a COVID-19 infection would impact a specific person medically, but also what the social and economic effects of a severe infection might be. The uncertainty surrounding COVID-19 contributed to fear, anxiety, and an increased sense of danger, as P7 described:
“Well, my biggest thing is the fear of the unknown. I over-think literally everything. My whole thing has been … ‘What if I have to not live in my apartment anymore?’ ‘What if I don’t get a job after this?’ ‘What if I go into debt?’ … Then just the whole, everything already feeling weird was definitely increasing all of that anxiety.”
4.3. Perceived uncertainty related to internal factors
Although participants by and large saw receiving in-person health care as hazardous, some participants did in fact choose to seek in-person routine health care. Therefore, the dynamics of determining one's self-defined locus of risk weighed the most heavily in people's decision making about whether or not to delay health care during the COVID-19 pandemic. Participants' self-defined locus of risk was based on their understanding of how COVID-19 worked, who was most affected, what health vulnerabilities they possessed, and what health vulnerabilities existed within their social bubble. For example, P8 told us, “I'm a retired firefighter, so I'm always worried about my lungs.” He reported that he never had any lung issues but knew that his job made him prone to greater risk of serious respiratory problems. He considered this vulnerability when making decisions that might involve exposure to COVID-19, including receiving in-person health care. Participants with certain pre-existing conditions—including asthma, diabetes, and cancer—perceived that these conditions put them at greater risk for more severe disease. For example, P17 said “I have asthma, so that is a pre-existing condition … I'm definitely mindful that if I get sick, it's not good.”
Prior to the pandemic, decisions to utilize or delay health care centered on the self. COVID-19 changed the equation. Because COVID-19 is an infectious disease with a high transmission rate and is spread through the air, participants described how they had to take into account the health (and relative vulnerability) of those in their social bubbles when making decisions to utilize or delay routine health care. For example, a new father (P9) stated that he and his wife were delaying health care for themselves as they had a newborn baby at home.
“… Obviously [the baby’s] immune system is nonexistent in many ways. The idea of what this could do to the family, along with people in my life that are all in their 70s or 80s, it's terrifying. There's a lot of concern about what this could do to myself, to my immediate family, and the next circle out."
Another participant (P10), a college student, considered herself to be at low risk for a severe case of COVID-19 but made decisions that considered her parents, who she lived with. Both were older and at high risk due to underlying health conditions, which shaped her decisions about delaying health care:
“I have canceled some appointments or refrained from scheduling certain appointments that I've needed, canceled the blood test like three different times because it always happened to. I was about to schedule it right when there were surges of cases and so I figured I'll just cancel it for now and do it later.”
Overall, participants described how they weighed the risks of delaying particular routine health care against the risk of being exposed to COVID-19 in terms of their self-defined locus of risk. Those who perceived high levels of vulnerability to COVID-19 for themselves or those in their social bubbles felt increased fear and anxiety about receiving in-person care, and often felt that the risks of receiving in-person care outweighed the risks of delaying routine health care—even when that health care was (under normal circumstances) deemed necessary, and the risks of delaying it would not be tolerated under other conditions. P11, who had asthma as a pre-existing condition, stated:
“I have the fear that if I ever come in contact with this virus that I would be a goner. That’s definitely my top anxiety right now." [She goes on to detail that she is avoiding chronic care for her allergies as she is trying to be cautious due to her asthma] “I definitely need to talk to somebody eventually, but like I said, I’m being risk-averse, things I think I’m allergic to or I try to stay away from."
4.4. ‘Should I go to my appointment or delay it?’ How People Made Decisions About Whether to Utilize or Delay Routine Health Care
Our participants described weighing uncertainty stemming from external factors (e.g., the risks posed by going to a medical facility) against their self-defined locus of risk. For example, P11 above described how she needed the health care services she was delaying, but considering the fact that she had asthma—which she believed made her extremely vulnerable to COVID-19, and the uncertain risks posed by going to a health care facility—she believed she was being “risk averse” by delaying health care. The risk, from her (and other participants') perspectives, stemmed from health care itself, not from delaying needed health care. Interestingly, for many of our participants, the ‘risk calculus’ that resulted in decisions to delay health care did not accord much weight to the risk of delaying health care. This indicates that our participants perceived that the risk of contracting COVID-19 from health care services was much greater than the risks posed by delaying care. These patterns can be found in examples of chronic care visits and preventive care visits: P12 described delaying her yearly breast exam, even though her mother had a history of breast cancer: “I'm okay with whatever risk I'm putting my own self in because I'm not going there right now.” For another example, P13, who had a newborn at home, explained his decision to delay a cardiac monitoring test he routinely receives for a chronic cardiac condition:
“I made the decision to delay it, because I'd have to go into a clinic [multiple times] I think I have to go four times, morning and night, for them to put it on, take it off, put it on, take it off, and I was just like, '‘No, that's, that's too much.’ I'll wait another month or two and then get it done”
Similarly, participants felt that it was acceptable to cancel yearly eye and dental appointments, as well as yearly physical exams. P14 stated:
“Yeah, I think I had an eye doctor’s appointment that I was pushing back … I mean, of course the doctor was wearing a mask and everything, but still. I didn’t feel comfortable with them being that close to your face. I had pushed that back for a while, but then my glasses broke. and I had to go in. Dental care, too … I don’t know how comfortable I feel yet … I know they're doing everything they can to be safe, but again, just having the whole process with the dentist and my mouth being open and—I don’t know. I'm just cautious and nervous about seeking dental care at this point.”
Finally, we found that information sources have impacted individuals’ risk calculus for utilizing or delaying in-person care. For example, P16 stated that she made decisions about delaying routine health care based on current COVID-19 information in her local community.
“I have canceled some appointments or refrain from scheduling certain appointments that I've needed, canceled the blood test like three different times … I was about to schedule it right when there was a surge of cases and so I figured I'll just cancel it for now and do it later."
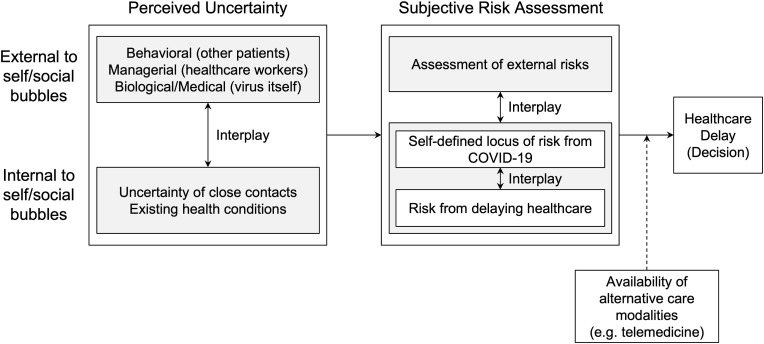
Based on our findings, we developed a preliminary model of individuals’ decision making to utilize or delay routine health care during the COVID-19 pandemic (Fig. 2 ). This model captures the interplay between perceived uncertainty both external and internal to the self and social bubbles. Further, we find that these different sources of perceived uncertainty interact to shape subjective risk assessments, which are formed based on an interplay between assessments of external risks, self-defined locus of risk, and risk from delaying health care (although, as described above, risk from delaying health care is not weighed heavily in these risk assessments). Uncertainty about COVID-19 interacts with these subjective risk assessments to result in a decision about utilizing or delaying in-person health care. It is important to note that some participants had alternatives to in-person health care available to them—although this varied based on the condition, location, health care coverage, etc. Many participants chose to take advantage of alternatives to in-person health care such as telemedicine, indicating that the presence of such alternatives may prevent the need to delay routine health care. However, alternatives to in-person care were not available in many circumstances.
Fig. 2.
A preliminary model of decision making to delay health care during the COVID-19 pandemic.
5. Discussion
5.1. Multi-level structures of the model for delayed health care
Unger-Saldaña and Infante-Castañeda (2011) developed their multidimensional model of health care delay, one of the most widely adopted models about delayed health care, using the context of health care delay related to breast cancer (Fig. 1). This model indicates that delay prior to receiving care is primarily due to the patient, and delay after receiving care is both affected by the health care provider and other influencing factors.
Our study of health care delay during COVID-19 allows us to extend Unger-Saldaña and Infante-Castañeda's (2011) model by distinguishing external and internal factors that give rise to people's decision to delay health care (Fig. 2), because our findings clearly show that people weigh uncertainty and risk that exist in both external environments (e.g., other patients' risk management practices, the nature of the virus) and themselves and their families (e.g., one's health condition, family status). Conceptual distinction between these two kinds of factors provides meaningful implications for both theories and methods. Theoretically, the multi-level model of health care delay can provide a more systematic understanding of an individual's decision-making process to delay health care. The hierarchical, muti-level model makes it easier for researchers to focus on micro- and macro dynamics separately, reducing the complexity that stems from different scopes of risk management practices and the surrounding environments. Methodologically, future studies can benefit from the new model by leveraging hierarchical, multi-level analysis methods such as multi-level regressions or agent-based modeling in quantitatively studying the dynamics of health care delay.
Because each of the internal and external factors has its own dynamics (e.g., family situation and one's own health condition could be seen as being multi-level within the internal factors), the model needs to be developed and refined further through future studies that focus on a particular level of factors. While the proposed model still provides an abstract understanding of only a few types of factors in the multi-level structures, we believe the proposed model can be an initial effort to extend the theory of health care delay.
5.2. Interplays: Where Tensions in Managing Risk are Created
As the Unger-Saldaña and Infante-Castañeda (2011) model shows, sociocultural factors, patients' individual factors, and other characteristics that are associated with health care practices create tensions that risk workers (i.e., both health care workers and patients) have to manage throughout their risk assessment practices. While this model can explain interactions between different factors and their roles in delaying health care, oftentimes patients interact with their sociocultural contexts at different levels (e.g., chronic disease patients' assessments of risks are shaped by both organizational norms and broader community cultures). In other words, individuals tend to enact practices within pre-defined institutional structures, and in so doing practices re-shape the institutional structures and logics within which they are enacted (Giddens, 1991; Thornton et al., 2012). Although these dynamics can still be explained through interplays between different factors as depicted in Fig. 1, the Unger-Saldaña and Infante-Castañeda (2011) model may provide limited explanations about the procedural aspect of health care delay from a risk assessment perspective. Also, abstracting the complex co-constitution of practice and structure may result in a loss of the nuance about how different practices and structures come into tension in shaping health care delay decisions. These theoretical challenges are further amplified during the COVID-19 pandemic, because lay people's burden to assess risks has increased due to a lack of medical resources and unclear risk assessment guidelines from health authorities (Pine et al., 2021).
Resolving part of these theoretical challenges, the proposed model details the locations of tensions that can be created between key factors associated with health care delay at different levels. The findings show some of these interplays clearly, such as the interplay between external uncertainty and internal conditions (e.g., balancing between the uncertainty of health care providers' health and safety practices and the unpredictability of individuals' own health conditions), which in turn leads to their subjective risk assessment and, thus, the decision to delay health care. For example, before they reached the self-assessment of risks, many participants were balancing between different uncertainties that existed on different entities and practices (e.g., comparing uncertainty of one's health condition and that of medical facility's risk prevention practices). This pattern demonstrates that the tensions exist between uncertainties inherent to people's small world networks (i.e., factors internal to self/social bubbles) and those that exist outside of one's social boundaries (i.e., factors external to self/social bubbles).
In a similar vein, another type of tension could be created within the subjective risk assessment processes. Risk can be identified and assessed either external to one's social bubbles or internal to their own conditions. For example, many participants assessed their risk based on their own chronic health risk as opposed to the risk of prevalent virus outside of their social circles, which led them to decide whether they would delay their health care or not. The interplay between internal and external risk assessments are partly shaped by their understanding of uncertainty that exists in both sides of the social worlds, and ultimately became the basis for the decision to delay health care. As such, by articulating the kinds of tensions that exist in different levels and stages of the decision-making processes, the proposed model can complement the initial model suggested by Unger-Saldaña and Infante-Castañeda (2011).
Meanwhile, the interplays between key factors associated with risk assessment need to be examined further to refine the theoretical model. While the model provides more detailed descriptions about what the interplays look like along people's risk assessment processes, each dimension of perceived uncertainty and subjective risk assessment comes with a multiplicity of factors, which can create their own tensions within each construct. For example, people not only manage tensions between external and internal risks, but also between different kinds of internal risks such as between their own health condition and their family's vulnerability. These kinds of micro-dynamics are implicitly presented in the proposed model. Further studies that investigate such dynamics within each category of risk assessment processes will make the model more concrete and comprehensive.
5.3. The Roles of Availability of Alternative Cares and the Implications for the Proposed Model
According to our findings, the availability of alternative care modalities such as telemedicine can be an important factor that moderates individuals' decision to delay health care. Even if people can assess presenting risks internal or external to their social bubbles, their decision to delay health care could depend on the availability of alternative care methods. In other words, people's risk assessment would be often moderated by material resources at the moment of decision-making practices (depicted as a dashed line in Fig. 2). Because our current analysis does not provide an extensive understanding of material resources such as different tyeps of alternative care modalities, future studies need to design protocols more in detail to capture how and why alternative cares moderate people's risk assessment processes differently given multiple tensions of existing conditions and factors.
The moderating role of the availability of alternative care modalities is also related to the theories of health care delay. The original model of health care delay was based on the structural understanding of health care practices where diverse actors and public sphere characteristics interact with each other (Unger-Saldaña and Infante-Castañeda, 2011). By distinguishing the subjective assessment of risks from the perceived uncertainty and the effects of material resources (i.e., alternative cares), the model highlights the procedural aspects of health care delay rather than the ontological view of the complexity in health care practices. Although the proposed model weakly captures the co-shaping dynamics between the structural and behavioral aspects of health-related practices (Giddens, 1991), this process model provides a more comprehensive understanding of how and why the decision for health care delay is made than the previous model does from an analytic perspective. To further incorporate the roles of the availability of alternative care modalities in the proposed model, future studies would need to focus on (1) what kinds of alternative care modalities exist and (2) how different characteristics of alternative care modalities moderate people's risk assessment in making decisions to delay health care.
5.4. Practical implications of model
The proposed model (Fig. 2) can provide health care providers with useful vocabularies and procedural knowledge when communicating risk to their patients and the public. As seen through the COVID-19 pandemic, risk decisions are often nuanced and involve many competing factors. This model may also be useful for health care providers for understanding how and why patients delay care during a crisis. Our research suggests that participants make decisions to seek in-person care that are fueled by anxiety, uncertainty, and fear. Additionally, participants often feel that there is a lack of information about what seeking care in-person would look like during the pandemic. Participants express concerns about the amount of people they would be in contact with, general cleanliness of the medical office, and the risk of contracting and passing the disease on to anyone else. This suggests a need for a better framework that details low- and high-risk behaviors, so that the public can make better informed decisions. The proposed framework and knowledge will be a basis for public health guidance that instills the confidence that seeking in-person care is safe and necessary to maintain effective continuity of care.
Detailed pamphlets or PSAs, for example, can be developed informed by this model by articulating possible risks of delaying health care versus seeking health care. As the model describes, self-defined locus of risk plays an important role in determining whether a patient will delay health care or not. This locus of risk may include both self-risk due to occupational hazard and pre-existing conditions, along with the risk of the general household. The targeted communication such as pamphlets could consider including both types of risks and explain what seeking health care means for a person who has to balance between the risks.
Finally, understanding that availability of alternative care modalities often moderates the perceived uncertainty can help health authorities develop a comprehensive communication about available health resources that can complement individuals’ health care. In other words, the targeted communication through customized websites, apps, or pamphlets can include not only different types of uncertainties, risks, and their interpretations, but also available resources that can mitigate the adverse effects of delaying routine health care. We believe that developing this approach based on the proposed model will be an initial effort to help health care providers and potential patients navigate the complex risk information environment during a public health crisis.
Credit author statement
Prakriti Shukla: Data curation, Writing – original draft, Myeong Lee: Conceptualization, Writing – review & editing, Supervision, Visualization, Samantha Whitman: Data curation, Investigation, Writing – review & editing, Kathleen Pine: Supervision, Writing – review & editing, Investigation.
Declaration of competing interest
None.
References
- Chen S.I., Wang Y., Dreyer R., Strait K.M., Spatz E.S., Xu X., et al. Insurance and prehospital delay in patients ≤ 55 years with acute myocardial infarction. Am. J. Cardiol. 2015;116(12):1827–1832. doi: 10.1016/j.amjcard.2015.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macapagal K., Bhatia R., Greene G.J. Differences in healthcare access, use, and experiences within a community sample of racially diverse lesbian, gay, bisexual, transgender, and questioning emerging adults. LGBT Health. 2016;3(6):434–442. doi: 10.1089/lgbt.2015.0124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisinger M.W., Moss M., Clark B.J. Is lack of social support associated with a delay in seeking medical care? A cross-sectional study of Minnesota and Tennessee residents using data from the Behavioral Risk Factor Surveillance System. BMJ Open. 2018;8(7) doi: 10.1136/bmjopen-2017-018139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adam B., Beck U., Van Loon J., Adam B., van Loon J. The Risk Society and beyond: Critical Issues for Social Theory. first ed. SAGE Publications; essay: 2000. Introduction: repositioning risk; the challenge for social theory; pp. 10–39. [Google Scholar]
- Armenta A., Sarabia H. Receptionists, doctors, and social workers: examining undocumented immigrant women's perceptions of health services. Soc. Sci. Med. 2020;246 doi: 10.1016/j.socscimed.2020.112788. [DOI] [PubMed] [Google Scholar]
- Atherly A., Van Den Broek-Altenburg E., Hart V., Gleason K., Carney J. Consumer reported care deferrals due to the COVID-19 pandemic, and the role and potential of telemedicine: cross-sectional analysis. JMIR Publ. Health Surveil. 2020;6(3) doi: 10.2196/21607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attanasio L.B., Hardeman R.R. Declined care and discrimination during the childbirth hospitalization. Soc. Sci. Med. 2019;232:270–277. doi: 10.1016/j.socscimed.2019.05.008. [DOI] [PubMed] [Google Scholar]
- Beedholm K., Andersen L.S., Lorentzen V. From bodily sensations to symptoms: health care–seeking practices among people affected by acute coronary syndrome. Qual. Health Res. 2019;29(11):1651–1660. doi: 10.1177/1049732319857057. [DOI] [PubMed] [Google Scholar]
- Brunner J., Rose D.E., Chuang E., Canelo I., Yano E.M. The role of healthcare system hassles in delaying or forgoing care. Healthcare. 2020;8(No. 2) doi: 10.1016/j.hjdsi.2020.100411. Elsevier. [DOI] [PubMed] [Google Scholar]
- Chan H.F., Skali A., Savage D.A., Stadelmann D., Torgler B. Risk attitudes and human mobility during the COVID-19 pandemic. Sci. Rep. 2020;10(1):1–13. doi: 10.1038/s41598-020-76763-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang H.J., Huang N., Lee C.H., Hsu Y.J., Hsieh C.J., Chou Y.J. The impact of the SARS epidemic on the utilization of medical services: SARS and the fear of SARS. Am. J. Publ. Health. 2004;94(4):562–564. doi: 10.2105/ajph.94.4.562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charmaz K. Sage; 2006. Constructing Grounded Theory: A Practical Guide through Qualitative Analysis. [Google Scholar]
- Coventry L.L., van Schalkwyk J.W., Thompson P.L., Hawkins S.A., Hegney D.G. Myocardial infarction, patient decision delay and help‐seeking behaviour: a thematic analysis. J. Clin. Nurs. 2017;26(13–14):1993–2005. doi: 10.1111/jocn.13607. [DOI] [PubMed] [Google Scholar]
- Cox Cynthia, Amin Krutika, Kamal Rabah. How have health spending and utilization changed during the coronavirus pandemic? [Internet] Health System Tracker. 2021 https://www.healthsystemtracker.org/chart-collection/how-have-healthcare-utilization-and-spending-changed-so-far-during-the-coronavirus-pandemic/ Available from: [Google Scholar]
- Dhand A., Luke D., Lang C., Tsiaklides M., Feske S., Lee J.M. Social networks and risk of delayed hospital arrival after acute stroke. Nat. Commun. 2019;10(1):1–8. doi: 10.1038/s41467-019-09073-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galdas P.M., Johnson J.L., Percy M.E., Ratner P.A. Help seeking for cardiac symptoms: beyond the masculine–feminine binary. Soc. Sci. Med. 2010;71(1):18–24. doi: 10.1016/j.socscimed.2010.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giddens A. In: Giddens' Theory of Structuration. A Critical Appreciation. Bryant C., Jary D., editors. Routledge; London: 1991. Structuration theory. Past, present and future; pp. 55–66. [Google Scholar]
- Gillespie C. The experience of risk as ‘measured vulnerability’: health screening and lay uses of numerical risk. Sociol. Health Illness. 2012;34(2):194–207. doi: 10.1111/j.1467-9566.2011.01381.x. [DOI] [PubMed] [Google Scholar]
- Glaser B.G. The constant comparative method of qualitative analysis. Soc. Probl. 1965;12(4):436–445. [Google Scholar]
- Gui X., Kou Y., Pine K., Ladaw E., Kim H., Suzuki-Gill E., Chen Y. Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems. ACM; 2018. Multidimensional risk communication: Public discourse on risks during an emerging epidemic; pp. 1–14. [Google Scholar]
- Gullatte M.M., Brawley O., Kinney A., Powe B., Mooney K. Religiosity, spirituality, and cancer fatalism beliefs on delay in breast cancer diagnosis in African American women. J. Relig. Health. 2010;49(1):62–72. doi: 10.1007/s10943-008-9232-8. [DOI] [PubMed] [Google Scholar]
- Huang Y.L., Starbird K., Orand M., Stanek S.A., Pedersen H.T. Proceedings of the 18th ACM conference on computer supported cooperative work & social computing. 2015. Connected through crisis: emotional proximity and the spread of misinformation online; pp. 969–980. [Google Scholar]
- Jaffee K.D., Shires D.A., Stroumsa D. Discrimination and delayed health care among transgender women and men. Med. Care. 2016;54(11):1010–1016. doi: 10.1097/MLR.0000000000000583. [DOI] [PubMed] [Google Scholar]
- Jelani Q.U.A., Jhamnani S., Spatz E.S., Spertus J., Smolderen K.G., Wang J., et al. Financial barriers in accessing medical care for peripheral artery disease are associated with delay of presentation and adverse health status outcomes in the United States. Vasc. Med. 2020;25(1):13–24. doi: 10.1177/1358863X19872542. [DOI] [PubMed] [Google Scholar]
- Kannan V.D., Veazie P.J. Predictors of avoiding medical care and reasons for avoidance behavior. Med. Care. 2014:336–345. doi: 10.1097/MLR.0000000000000100. [DOI] [PubMed] [Google Scholar]
- Kent E.E., Forsythe L.P., Yabroff K.R., Weaver K.E., de Moor J.S., Rodriguez J.L., Rowland J.H. Are survivors who report cancer‐related financial problems more likely to forgo or delay medical care? Cancer. 2013;119(20):3710–3717. doi: 10.1002/cncr.28262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keshet Y., Popper-Giveon A. The undisciplined patient in neoliberal society: conscious, informed and intuitive health behaviours. Health Risk Soc. 2018;20(3–4):182–199. [Google Scholar]
- Kou Y., Gui X., Chen Y., Pine K. Conspiracy talk on social media: Collective sensemaking during a public health crisis. Proceedings of the ACM on Human-Computer Interaction. 2017;1(CSCW):1–21. 61. [Google Scholar]
- Kumar D., Chandra R., Mathur M., Samdariya S., Kapoor N. Vaccine hesitancy: understanding better to address better. Isr. J. Health Pol. Res. 2016;5(1):1–8. doi: 10.1186/s13584-016-0062-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson H.J., Schulz W.S., Tucker J.D., Smith D.M. Measuring vaccine confidence: introducing a global vaccine confidence index. PLoS Curr. 2015;7 doi: 10.1371/currents.outbreaks.ce0f6177bc97332602a8e3fe7d7f7cc4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee A.A., James A.S., Hunleth J.M. Waiting for care: chronic illness and health system uncertainties in the United States. Soc. Sci. Med. 2020;264 doi: 10.1016/j.socscimed.2020.113296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehavot K., Katon J.G., Simpson T.L., Shipherd J.C. Transgender veterans' satisfaction with care and unmet health needs. Med. Care. 2017;55(Suppl. 9 2):S90. doi: 10.1097/MLR.0000000000000723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lightfoot A.F., Thatcher K., Simán F.M., Eng E., Merino Y., Thomas T., et al. What I wish my doctor knew about my life”: using photovoice with immigrant Latino adolescents to explore barriers to healthcare. Qual. Soc. Work. 2019;18(1):60–80. doi: 10.1177/1473325017704034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupton D., editor. Risk and sociocultural theory: New directions and perspectives. Cambridge University Press; 1999. [Google Scholar]
- Mafi J.N., Craff M., Vangala S., Pu T., Skinner D., Tabatabai-Yazdi C., et al. Trends in US ambulatory care patterns during the COVID-19 pandemic, 2019-2021. JAMA. 2022;327(3):237–247. doi: 10.1001/jama.2021.24294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nieminen M., Aro K., Jouhi L., Bäck L., Mäkitie A., Atula T. Causes for delay before specialist consultation in head and neck cancer. Acta Oncol. 2018;57(12):1677–1686. doi: 10.1080/0284186X.2018.1497297. [DOI] [PubMed] [Google Scholar]
- Park S., Fowler L. Political and administrative decentralization and responses to COVID-19: comparison of the United States and South Korea. Int. J. Organ. Theor. Behav. 2021;24(4):289–299. [Google Scholar]
- Percac-Lima S., Cronin P.R., Ryan D.P., Chabner B.A., Daly E.A., Kimball A.B. Patient navigation based on predictive modeling decreases no‐show rates in cancer care. Cancer. 2015;121(10):1662–1670. doi: 10.1002/cncr.29236. [DOI] [PubMed] [Google Scholar]
- Pine K.H., Lee M., Whitman S.A., Chen Y., Henne K. Proceedings of the 2021 CHI Conference on Human Factors in Computing Systems. ACM; 2021. Making sense of risk information amidst uncertainty: Individuals’ perceived risks associated with the COVID-19 pandemic; pp. 1–15. [Google Scholar]
- Powell W., Richmond J., Mohottige D., Yen I., Joslyn A., Corbie-Smith G. Medical mistrust, racism, and delays in preventive health screening among African-American men. Behav. Med. 2019;45(2):102–117. doi: 10.1080/08964289.2019.1585327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuter C., Hughes A.L., Kaufhold M.A. Social media in crisis management: an evaluation and analysis of crisis informatics research. Int. J. Hum. Comput. Interact. 2018;34(4):280–294. [Google Scholar]
- Siminoff L., Thomson M., Dumenci L. Factors associated with delayed patient appraisal of colorectal cancer symptoms. Psycho Oncol. 2014;23(9):981–988. doi: 10.1002/pon.3506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon M.A., Tom L.S., Nonzee N.J., Murphy K.R., Endress R., Dong X., Feinglass J. Evaluating a bilingual patient navigation program for uninsured women with abnormal screening tests for breast and cervical cancer: implications for future navigator research. Am. J. Publ. Health. 2015;105(5):e87–e94. doi: 10.2105/AJPH.2014.302341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons G., Lumley S., Falahee M., Kumar K., Mallen C.D., Stack R.J., Raza K. The pathway to consultation for rheumatoid arthritis: exploring anticipated actions between the onset of symptoms and face-to-face encounter with a healthcare professional. BMC Muscoskel. Disord. 2017;18(1):1–9. doi: 10.1186/s12891-017-1619-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smolderen K.G., Spertus J.A., Nallamothu B.K., Krumholz H.M., Tang F., Ross J.S., et al. Health care insurance, financial concerns in accessing care, and delays to hospital presentation in acute myocardial infarction. JAMA. 2010;303(14):1392–1400. doi: 10.1001/jama.2010.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sofaer S. Navigating poorly charted territory. Med. Care Res. Rev. 2009;66(1_Suppl. l):75S–93S. doi: 10.1177/1077558708327945. [DOI] [PubMed] [Google Scholar]
- Taber J.M., Leyva B., Persoskie A. Why do people avoid medical care? A qualitative study using national data. J. Gen. Intern. Med. 2015;30(3):290–297. doi: 10.1007/s11606-014-3089-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornton P.H., Ocasio W., Lounsbury M. Oxford University Press on Demand; 2012. The Institutional Logics Perspective: A New Approach to Culture, Structure, and Process. [Google Scholar]
- Timmermans S., Tavory I. Theory construction in qualitative research: from grounded theory to abductive analysis. Socio. Theor. 2012;30(3):167–186. [Google Scholar]
- Unger-Saldaña K., Infante-Castañeda C.B. Breast cancer delay: a grounded model of help-seeking behaviour. Soc. Sci. Med. 2011;72(7):1096–1104. doi: 10.1016/j.socscimed.2011.01.022. [DOI] [PubMed] [Google Scholar]
- Vose J. 34(9) Williston Park; NY: 2020. Delay in cancer screening and diagnosis during the COVID-19 pandemic: what is the cost? (Oncology). 343-343. [DOI] [PubMed] [Google Scholar]
- Wise T., Zbozinek T.D., Michelini G., Hagan C.C. 2020. Changes in Risk Perception and Protective Behavior during the First Week of the COVID-19 Pandemic in the United States. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf S.H., Chapman D.A., Sabo R.T., Weinberger D.M., Hill L. Excess deaths from covid-19 and other causes, March-April 2020. JAMA. 2020;324(5):510. doi: 10.1001/jama.2020.11787. [DOI] [PMC free article] [PubMed] [Google Scholar]