Abstract
Background
Over the course of the COVID-19 pandemic, a variety of COVID-19-related misinformation has spread and been amplified online. The spread of misinformation can influence COVID-19 beliefs and protective actions, including vaccine hesitancy. Belief in vaccine misinformation is associated with lower vaccination rates and higher vaccine resistance. Attitudinal inoculation is a preventative approach to combating misinformation and disinformation, which leverages the power of narrative, rhetoric, values, and emotion.
Objective
This study seeks to test inoculation messages in the form of short video messages to promote resistance against persuasion by COVID-19 vaccine misinformation.
Methods
We designed a series of 30-second inoculation videos and conducted a quasi-experimental study to test the use of attitudinal inoculation in a population of individuals who were unvaccinated (N=1991). The 3 intervention videos were distinguished by their script design, with intervention video 1 focusing on narrative/rhetorical (“Narrative”) presentation of information, intervention video 2 focusing on delivering a fact-based information (“Fact”), and intervention video 3 using a hybrid design (“Hybrid”). Analysis of covariance (ANCOVA) models were used to compare the main effect of the intervention on the 3 outcome variables: ability to recognize misinformation tactics (“Recognize”), willingness to share misinformation (“Share”), and willingness to take the COVID-19 vaccine (“Willingness”).
Results
There were significant effects across all 3 outcome variables comparing inoculation intervention groups to controls. For the Recognize outcome, the ability to recognize rhetorical strategies, there was a significant intervention group effect (P<.001). For the Share outcome, support for sharing the mis- and disinformation, the intervention group main effect was statistically significant (P=.02). For the Willingness outcome, there was a significant intervention group effect; intervention groups were more willing to get the COVID-19 vaccine compared to controls (P=.01).
Conclusions
Across all intervention groups, inoculated individuals showed greater resistance to misinformation than their noninoculated counterparts. Relative to those who were not inoculated, inoculated participants showed significantly greater ability to recognize and identify rhetorical strategies used in misinformation, were less likely to share false information, and had greater willingness to get the COVID-19 vaccine. Attitudinal inoculation delivered through short video messages should be tested in public health messaging campaigns to counter mis- and disinformation.
Keywords: attitudinal inoculation, intervention, COVID-19 vaccine, vaccine hesitancy, COVID-19, vaccine, vaccination, public health, health intervention, misinformation, infodemiology, vaccine misinformation
Introduction
The study of misinformation and disinformation and how to counter them is not new. There are centuries-old examples of the challenges in rebutting misleading or manipulative information [1-3]. However, although false and manipulative media are not new, “the digital age has changed how such messages are created, circulated, and interpreted, as well as their potential effects” [4]. As features of the COVID-19 media ecosystem, misinformation and disinformation are functionally similar, in that both either contradict or distort the current scientific and public health consensus as to the nature of the virus and appropriate steps to combat it [5,6]. However, the 2 terms refer to separate phenomena insofar as concerns motive. “Misinformation” is unintentionally inaccurate, while “disinformation,” is intentionally inaccurate and meant to mislead [7]. In the context of public health, the term “infodemic” was coined to refer to “an overflow of information of varying quality that surges across digital and physical environments during an acute public health event” [8]. Infodemiology, as a field of study and intervention, dates back to 1996 [9,10]. Eysenbach defines infodemiology as the “science of distribution and determinants of information in an electronic medium, specifically the Internet, or in a population, with the ultimate aim to inform public health and public policy” [9]. As Eysenbach describes it, infodemiology rests on the premise that public health and patterns of communication are correlated, and perhaps even causally connected.
Since the pandemic’s beginning, a variety of COVID-19-related misinformation and disinformation has spread and been amplified online [11]. The content and spread of misinformation can influence COVID-19 beliefs and protective actions [12,13]. Despite the availability of the COVID-19 vaccine in the United States, hesitancy among the general population remains a challenge. In their review of 39 nationally representative polls taken in the first half of 2021, Steelfisher et al [14] found that nearly 30% of the population remains hesitant to get the COVID-19 vaccine. Belief in vaccine misinformation is associated with lower vaccination rates and higher vaccine resistance [15]. The spread of misinformation and disinformation online can increase COVID-19 vaccine hesitancy [16]. Studies conducted at varying time points in 2020 have found that reliance on social media is associated with higher levels of holding both conspiracy beliefs and higher levels of vaccine hesitancy [17-20].
Studies of how to address the current infodemic are nascent. The inaugural World Health Organization (WHO) Infodemiology Conference of 2021 called for more research on interventions to address the infodemic [11]. Countering misinformation is a critical piece of infodemic management because misinformation impacts protective actions and vaccine hesitancy. Infodemiology research has shown that quality health information can be elusive to the public, especially in evolving situations, such as a pandemic [21]. One common approach used by public health risk communicators focuses on “facts.” However, as Eysenbach [21] points out, in times of evolving science, factual information can be hard to determine, and initial reports and decisions are made based on the best information available at any given time. Currently, the most common approach to countering misinformation is to engage in fact checking. Research evaluating the utility of online fact checking suggests that even under less uncertain conditions, it remains an uneven but relatively effective counterstrategy to disinformation [22-26]. However, fact checking carries with it 2 challenges: asymmetry and volume. Feelings of social ostracism are shown to decrease receptivity to counter disinformation fact checking [27]. Media consumers with less overall political knowledge are likewise less receptive, as are political conservatives more generally [28]. Meanwhile, the sheer volume with which bad actors are increasingly equipped to “flood the zone” with mis- and disinformation [29] can exhaust most audience’s ability to sift good information from bad, apart from more formal, time-and-resource-intensive fact-checking projects. Human moderators cannot match the speed and volume of false information and, furthermore, require an ever-changing range of subject expertise that content moderators cannot reasonably be expected to acquire [30,31]. Studies into the relative efficacy of logic-based versus emotionally based public health communication have suggested that the use of narrative [32-34], appeals to values [35,36], and rhetoric of personal, lived experience [37-39] yield better persuasive outcomes than more abstract, fact-based, or logical counterparts. Per Maertens et al [40], this might relate to the “broad spectrum” of potential viewpoints that such approaches address. That is, fact checking’s narrower focus on specific content addresses fewer points of persuasive vulnerability than a broader focus on form offered by rhetoric, narrative, and values.
Attitudinal inoculation (or, simply, “inoculation”) is a preventative approach to combating misinformation and disinformation that leverages the power of narrative, rhetoric, values, and emotion. Inoculation theory promises that people can become resistant to persuasion if they perceive a threat from an attempt to change their beliefs or attitudes and if they receive information to refute this attempt [41]. It originates in the midcentury work of William McGuire [41-43]. It uses the biological metaphor of viral inoculation to propose that “[t]hrough exposing individuals to messages containing a weakened argument against an attitude they hold, it is possible to ‘inoculate’ the individuals against future attacks on the attitude” [44]. Inoculation consists of exposing someone to a persuasive message that contains weakened arguments against an established attitude, which develops resistance against stronger persuasive attacks in the future [41].
Inoculation is preemptive, addressing audiences holding “healthy (ie, preferred) positions,” or agnostic and undecided [45]. It scales against the “flooded zone” of information, allowing individuals to bypass entire categories of misleading, manipulative, or simply distracting information. Inoculation is suited to address the needs of low-information audiences, ideologically polarized and conspiratorial groups, and groups that are traditionally difficult audiences to reach with corrections [46]. Inoculation may partially overcome the post hoc correction challenges of asymmetry and volume, while accounting for variations in the efficacy of fact-based versus narrative/rhetoric-based approaches.
Studies have supported the effectiveness of attitudinal inoculation as a tool for strengthening resistance to persuasion on public health topics, such as underage alcohol consumption, adolescent smoking initiation, deceptive nutrition-related food claims, unprotected sex, and child vaccine safety claims [47,48]. Additionally, attitudinal inoculation has been shown as an effective strategy for counterradicalization. In a foundational study, inoculation conferred resistance to persuasion by far-right and far-left extremist propaganda by reducing the credibility of the extremist groups that produced the propaganda and increasing reactance (the combination of anger and counterarguing) against the propaganda itself. By reducing source credibility and increasing reactance, inoculation ultimately reduced participant intentions to support the group that produced the propaganda [49].
The potential for attitudinal inoculation to combat COVID-19 vaccine misinformation was proposed by van der Linden et al [50]. Although attitudinal inoculation enjoys a rich body of literature, and infodemiology likewise can claim extensive source material, the specific application of both approaches to the crisis of the COVID-19 pandemic is scant at best. This study is among the first to answer the call made by van der Linden et al [50]. It not only sought to test the effectiveness of attitudinal inoculation against COVID-19 misinformation and disinformation but also attempted to address questions relating to persuasive communication, which bear direct relevance to the matter of public health communication in the pandemic. As described before, the relative efficacy of fact versus narrative or rhetoric in persuasive messaging has been studied across many dimensions of public health. Our study testing the use of video-based attitudinal inoculation to inoculate viewers against misinformation on COVID-19 vaccine injury is the first of its kind to compare the effectiveness of using facts versus narrative-rhetoric approaches to attitudinal inoculation messages relating to COVID-19 vaccine misinformation and disinformation. The goal of our research was to build upon the work of Braddock, van der Linden, and other inoculation theorists by using inoculation messages in the form of short video messages to promote resistance against persuasion by COVID-19 vaccine misinformation.
Methods
Identification of Antivax Narratives
This study was built upon our formative evaluation work that identified common rhetorical strategies and COVID-19 vaccine misinformation narratives and used formative surveys to explore their prevalence and validate select survey items that were used in this study [20,51,52]. The narratives were identified by analyzing 6 months of content from 10 online channels of antivaccine or COVID-19 denialist propaganda. These took the form of Twitter accounts, amateur videos, documentaries, Facebook groups, blogs, and Instagram pages. From these media sources, we created a list of 22 key narrative tropes and 16 rhetorical strategies, which represented the discursive foundation of the antivaccine and COVID-19 denialist media data collected, and created a codebook [53]. Narratives ranged from general claims that the COVID-19 vaccine could cause physical injury to the theory it was a bioweapon promoted by intelligence agencies for shadowy and perhaps even supernatural purposes. Some rhetorics framed their arguments along the lines of bodily autonomy by co-opting the language of women’s reproductive rights, while others relied on audio-visual cues, such as nauseating colors and low-frequency sounds, to cue unease in their audience.
Development of Inoculation Messages
Based on the identification of the antivax narratives, we selected a prominent metanarrative related to vaccine injury that was used to develop 3 different inoculation messages: (1) a fact-based video, focused on countering false statistics about the science and safety of vaccines; (2) a narrative and rhetoric-focused video, which “prebunked” (ie, practice of countering potential misinformation by warning people against it before it is disseminated) common antivaccine misinformation strategies; and (3) a hybrid video that tested a combination of factual rebuttal with narrative/rhetorical prebunking. These 3 approaches were selected in order to deepen understanding of the relative efficacy of fact-based and narrative/rhetoric-based persuasion. As discussed before, the relative efficacy of each approach has been addressed across a variety of fields, from extremist deradicalization to public health.
Development of Inoculation Videos
We designed a series of 30-second inoculation videos and conducted a quasi-experimental study to test the use of attitudinal inoculation in a population of individuals who were unvaccinated. We developed 3 inoculation videos. Each 30-second video contained a “microdose,” a weakened example of manipulation, which has been shown not to cause harm in a controlled research setting. The microdoses, while weakened, constitute an “active threat” that let people generate cognitive “antibodies” [40,54,55]. The differences between the 3 inoculation videos are shown in Table 1.
Table 1.
Description of video types.
| Video types | Purpose | Example of video script |
| Narrative and rhetoric inoculation | Inoculate viewers against vaccine misinformation strategies, such as manipulation, scapegoating, or conspiratorial reasoning. |
|
| Factual rebuttal inoculation | Counter false information about science and safety about vaccines. |
|
| Hybrid | Combine fact-based information and inoculation against misinformation strategies. |
|
Study Hypothesis
Based upon our prior research on the relationship between knowledge, attitude, and behavior, we posited 3 hypotheses:
Hypothesis 1: Relative to noninoculated participants, inoculated participants will demonstrate a greater ability to identify rhetorical strategies typically used in mis- and disinformation videos.
Hypothesis 2: Relative to noninoculated participants, inoculated participants will be less likely to report engaging in behaviors that support the spread of COVID-19 mis- and disinformation videos.
Hypothesis 3: Relative to noninoculated participants, inoculated participants will report greater intention to get vaccinated against COVID-19.
Study Design
We conducted a quasi-experimental study with a pre-post intervention questionnaire and control group using an organic sampling survey method between June 3 and 5, 2021 [56]. Using this method, 4 separate surveys were conducted for each of the video exposure interventions, and as such, randomization was not possible. We conducted our surveys through the Pollfish (an online survey company) survey platform. Participants were eligible to participate if they indicated they had not received a COVID-19 vaccine, were over the age of 18 years, and lived in the United States. In total, 500 US adults were recruited into each study arm by Pollfish via mobile technology. Respondents were recruited into 1 of 4 study arms, 1 for each type of inoculation message, plus a control group that received a video unrelated to inoculation or vaccines using the design outlined Figure 1.
Figure 1.
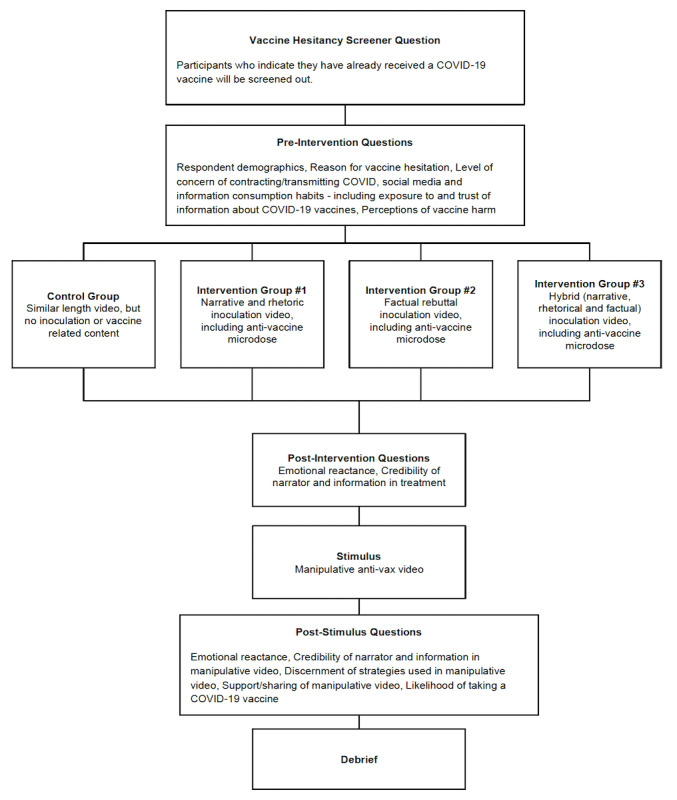
Study design.
All participants first answered questions about their demographics, social media and information consumption, exposure to and trust of information about COVID-19 vaccines, and perceptions of vaccine harm. Then, participants in the 3 treatment groups were “inoculated” by showing them a 30-second scripted video that highlights narrative or rhetorical tactics used in vaccine misinformation (intervention group 1, “Narrative,” n=500), contains factual rebuttal of vaccine misinformation (intervention group 2, “Fact,” n=500), or a hybrid of both (intervention group 3, “Hybrid,” n=500). The control group (n=500) watched a neutral video that described how to make a paper airplane. Participants were then asked a series of questions on their perceptions of the video.
After watching the inoculation video, participants were shown a video stimulus that utilizes the manipulation techniques participants were alerted to in the inoculation video. The same stimulus video was displayed to participants in the control group and all treatment groups. Participants were then asked the same series of questions on their perceptions of the video. The same questions were asked following the intervention/control video and the stimulus video in order to avoid alerting the respondent as to the type of video being assessed.
Ethical Considerations
The study protocol was approved by the American University Institutional Review Board (IRB-2022-295).
Variables of Interest
We had 3 hypotheses of interest. Each hypothesis corresponded to a different dependent variable below. The first hypothesis was related to the ability to identify misinformation, the second was related to willingness to share information, and the third was related to willingness to get vaccinated. The measures described below were designed to correspond to these 3 research questions, though the survey also included other items related to emotional reactance to the content.
Dependent Variables (Question Number - Variable Name)
We selected 3 particular outcomes of interest:
The ability to recognize rhetorical strategies in a video containing misinformation about the COVID-19 vaccine, such as unusual colors, scary music, and vague language (Q25 - Recognize)
Willingness to share the video containing misinformation about the COVID-19 vaccine (Q24 - Share)
Willingness to get vaccinated (Q26 - Willingness)
Independent Variables
We had the following independent variables:
Demographic variables: gender (male, female), age (continuous), race (non-Hispanic White, non-Hispanic Black, Hispanic, non-Hispanic Asian, other), income (continuous), education (less than high school, high school/General Educational Development (GED), some college, bachelor’s degree, postgraduate degree, other)
General vaccine attitude covariates: “Most vaccines do not cause immediate injuries or side effects,” “Most vaccines do not lead to long-term side effects,” “Vaccines cause more harm than benefit,” “Taking a vaccine is likely to give me a disease,” “Vaccination can protect me from getting a disease,” “Vaccines cause autism,” and “Vaccines are designed as a form of government control,” which was tested and then analyzed as a factor that controlled for vaccine attitudes (see analysis plan)
Statistical Analyses
The analyses included 3 steps: first, to conduct descriptive statistics of baseline sample characteristics; second, to analyze multi-item scale development; and third, to test the effect of the 3 interventions in comparison to controls on the endpoints collected after the second video. All final models were adjusted for demographics (age, gender, race, education, and income); baseline value, if available; and mean scores calculated about general attitudes toward vaccines.
Descriptive Statistics of Baseline Sample Characteristics
Baseline characteristics of the sample, including age, gender, race, income, education, and attitudinal variables, were described using means and SDs for continuous variables and counts and percentages for categorical variables. Descriptive statistics were calculated for the entire sample and by intervention group.
Multi-Item Scale Development
Principal component analysis (PCA) was used to test the dimensionality of multi-item scales, which included the scales for prior general vaccine attitudes and the 3 primary study outcomes, namely Recognize, Share, and Willingness. We planned to retain components associated with eigenvalues greater than 1 as long as factor loadings and internal consistency within components, as measured by Cronbach α, were acceptable (>.7). When more than 1 component was retained, the varimax rotation was applied to the model to aid in the interpretation of the factor loadings. For retained components, scores were created as the mean of their items.
Statistical Analysis of Effects of Interventions on Outcomes
Analysis of covariance (ANCOVA) models were used to compare the main effect of the intervention on the 3 outcome variables. The model for each outcome included the main effect of the intervention adjusted for age, gender, race, education, income, and the scores for prior general attitudes toward vaccines that was formed in the second step of our analysis. For the Share scale, the model also included the baseline Share score from after the first video. For the 3 outcomes, we were interested in testing the null hypothesis of no difference between intervention groups using a 2-tailed statistical test. To control the type 1 error rate resulting from multiple endpoints, we used the Holm method. For outcomes with a significant intervention group F test, we tested paired differences between the intervention groups and the control group and controlled for multiple comparisons using the Dunnett test. The power of the statistical test for an ANOVA with 3 intervention groups and 1 control group where the Dunnett test is used to compare each treatment mean with the control mean, one would require 477 subjects in each group in order to achieve 81% power to detect a mean difference of 0.33 between at least 1 pair of intervention and control groups, assuming an SD of 1.8 within each group and a family-wise type 1 error rate of .017, which corresponds to the first rejection level of the Holm method for this study.
Results
Sample Characteristics
This analysis included 1991 subjects. Although 500 (25.1%) subjects were enrolled in each intervention group, not all subjects completed the survey questionnaire, leaving an analysis population of 495 (24.9%) participants in the control group and 480 (24.1%) in the narrative-rhetorical, 489 (24.6%) in the factual, and 489 (24.6%) in the hybrid video intervention groups. Overall, the study population had a mean age of 40.7 (SD 11.8) years, and 968 (50%) were female, 1439 (74%) were non-Hispanic White, 1173 (60%) had a bachelor’s degree or higher education, and 773 (40%) reported an income of US $100,000 or more. A summary of baseline characteristics for the entire sample and by intervention group is given in Table 2.
Table 2.
Baseline characteristics.
| Characteristic | All groups (N=1953) | Controls (N=495) | Narrative (N=495) | Fact (N=489) | Hybrid (N=489) | P valuea | ||
| Age (in years), mean (SD) | 40.8 (11.8) | 41.0 (11.7) | 36.6 (11.6) | 41.6 (11.4) | 43.6 (11.4) | <.001 | ||
| Female gender, n (%) | 968 (50) | 248 (50) | 234 (49) | 243 (50) | 243 (50) | .98 | ||
| Race, n (%) | .03 | |||||||
|
|
Non-Hispanic White | 1439 (74) | 380 (77) | 347 (72) | 356 (73) | 356 (73) | N/Ab | |
|
|
Non-Hispanic Black | 206 (11) | 29 (6) | 59 (12) | 59 (12) | 59 (12) | N/A | |
|
|
Hispanic/Latino | 98 (5) | 35 (7) | 21 (4) | 21 (4) | 21 (4) | N/A | |
|
|
Non-Hispanic Asian | 73 (4) | 13 (3) | 20 (4) | 20 (4) | 20 (4) | N/A | |
|
|
Other | 137 (7) | 38 (8) | 33 (7) | 33 (7) | 33 (7) | N/A | |
| Income (US $), n (%) | .02 | |||||||
|
|
<25,000 | 238 (12) | 76 (15) | 54 (11) | 54 (11) | 54 (11) | N/A | |
|
|
25,000-49,999 | 245 (12) | 75 (15) | 56 (11) | 57 (12) | 57 (11) | N/A | |
|
|
50,000-74,999 | 273 (14) | 48 (10) | 75 (15) | 75 (15) | 75 (15) | N/A | |
|
|
75,000-99,999 | 310 (16) | 74 (15) | 78 (16) | 79 (16) | 79 (16) | N/A | |
|
|
100,000-124,999 | 170 (9) | 42 (8) | 42 (9) | 43 (9) | 43 (9) | N/A | |
|
|
125,000-149,999 | 200 (10) | 51 (10) | 47 (10) | 51 (10) | 51 (10) | N/A | |
|
|
≥150,000 | 403 (21) | 83 (17) | 106 (22) | 107 (22) | 107 (22) | N/A | |
|
|
Prefer not to say | 114 (6) | 46 (9) | 22 (5) | 23 (5) | 23 (5) | N/A | |
| Education, n (%) | <.001 | |||||||
|
|
Less than high school | 164 (8) | 17 (3) | 49 (10) | 49 (10) | 49 (10) | N/A | |
|
|
High school/GEDc | 290 (15) | 103 (21) | 61 (13) | 63 (13) | 63 (13) | N/A | |
|
|
Some college | 254 (13) | 104 (21) | 50 (10) | 50 (10) | 50 (10) | N/A | |
|
|
Bachelor’s degree | 405 (21) | 105 (21) | 100 (21) | 100 (20) | 100 (20) | N/A | |
|
|
Postgraduate degree | 768 (39) | 166 (34) | 196 (41) | 203 (42) | 203 (42) | N/A | |
|
|
Other | 72 (4) | 0 (0) | 24 (5) | 24 (5) | 24 (5) | N/A | |
aTest of significant intervention group effect using ANOVA model for Age and Pearson chi-square test for categorical variables.
bN/A: not applicable.
cGED: General Educational Development.
Results of Statistical Analysis of Scales
PCA of the 7 items measuring prior attitudes toward vaccines retained 2 factors that accounted for 65% of the variance in the data. All items had a high factor loading on 1 of the 2 factors, with loading in the range of 0.71-0.83, while also having small factor loadings of less than 0.2 on the other factor (Table 3). Items loading most heavily on the first component asked the level of agreement to the statements “Most vaccines do not cause immediate injuries or side effects,” “Most vaccines do not lead to long-term side effects,” and “Vaccination can protect me from getting a disease,” while the remaining items that asked “Vaccines cause more harm than benefit,” “Taking a vaccine is likely to give me a disease,” “Vaccines cause autism,” and “Vaccines are designed as a form of government control” loaded highly onto the second component. Cronbach α for the 3 items loading on the first component was .70, while the 4 items loading on the second component had a Cronbach α of .83, indicating good internal consistency within each set of items. Because these 7 items formed 2 distinct constructs with good reliability, we created 2 scores for general attitudes toward vaccines by taking a subject’s mean response to the questions that loaded highly onto each factor.
Table 3.
PCAa factor structure.
| Construct items | Factor 1 loading | Factor 2 loading | |||
| General attitudes toward vaccines | |||||
|
|
Most vaccines do not cause immediate injuries or side effects. | 0.79 | 0.13 | ||
|
|
Most vaccines do not lead to long-term side effects. | 0.69 | 0.11 | ||
|
|
Vaccines cause more harm than benefit. | 0.09 | 0.74 | ||
|
|
Taking a vaccine is likely to give me a disease. | 0.09 | 0.75 | ||
|
|
Vaccination can protect me from getting a disease. | 0.49 | 0.10 | ||
|
|
Vaccines cause autism. | 0.19 | 0.75 | ||
|
|
Vaccines are designed as a form of government control. | 0.14 | 0.66 | ||
| Recognize | |||||
|
|
Scary music | 0.78 | N/Ab | ||
|
|
Weird colors | 0.78 | N/A | ||
|
|
Vague language (words that are unclear or not specific) | 0.73 | N/A | ||
| Sharing | |||||
|
|
How likely are you to share this second video with people in your social media network? | 0.83 | N/A | ||
|
|
How likely are your friends to share this second video on their social media networks? | 0.81 | N/A | ||
|
|
If you could, how likely would you be to support the producer of this second video by following them (receiving future posts from them) on social media? | 0.88 | N/A | ||
|
|
If you could, how likely would you be to financially support the producer of this second video? | 0.82 | N/A | ||
|
|
How likely are you to check the facts on the second video you just watched? | 0.60 | N/A | ||
aPCA: principal component analysis.
bN/A: not applicable.
For the 3 questions measuring the Recognize outcome, PCA showed the items to be unidimensional, with a single factor accounting for 72% of the variance. Factor loadings were all greater than 0.84, and Cronbach α was .81. PCA of the 5 items measuring the Share outcome also retained a single factor that accounted for 70% of the variance in the data. Factor loadings were high (0.70-0.89), and Cronbach α was .89.
Effect of Interventions on Outcomes of Interest
Hypothesis 1. The Ability to Recognize Rhetorical Strategies in a Video Containing Misinformation About the COVID-19 Vaccine (Recognize)
For the Recognize score, the ability to recognize rhetorical strategies, there was a significant intervention group effect (F(3,1929)=8.5, P<.001); see Table 4. Since this was the smallest of the intervention group effect P values among the 3 study endpoints, the Holm method rejected the null hypothesis of the no-intervention-group effect when P<.05/3=.02, which was achieved. The least squares (LS) means (SE) of the Recognize scale for controls and the 3 video intervention groups were 3.67 (0.09), 3.98 (0.09), 4.10 (0.09), and 4.14 (0.09), respectively. The LS mean differences between intervention groups (Narrative, Fact, and Hybrid) and controls were 0.31 (P=.01), 0.43 (P<.001), and 0.47 (P<0.001), respectively, with all P values being significant after adjusting for multiple comparison using the Dunnett test. These tests indicated that each intervention group had a statistically significant greater awareness of the tactics used to gain attention in the second video compared to controls.
Table 4.
ANCOVAa models’ estimated intervention effects, mean scores, and differences.
| Intervention LSb means and SEs | Differences from control intervention | |||||
| Outcome by intervention | F statistic P valuec | LS mean (SE)c | LS mean (SE) | Adjusted P valued | ||
| Recognition of rhetorical strategies (“Recognize”) | ||||||
|
|
Intervention effect | <.001 | N/Ae | N/A | N/A | |
|
|
Control | N/A | 3.67 (0.09) | N/A | N/A | |
|
|
Narrative | N/A | 3.98 (0.09) | 0.31 (0.11) | .01 | |
|
|
Fact | N/A | 4.10 (0.09) | 0.43 (0.10) | <.001 | |
|
|
Hybrid | N/A | 4.14 (0.09) | 0.47 (0.10) | <.001 | |
| Willingness to share misinformation content (“Share”) | ||||||
|
|
Intervention effect | .017 | N/A | N/A | N/A | |
|
|
Control | N/A | 4.11 (0.08) | N/A | N/A | |
|
|
Narrative | N/A | 3.90 (0.07) | –0.21(0.09) | .03 | |
|
|
Fact | N/A | 3.90 (0.07) | –0.22 (0.09) | .022 | |
|
|
Hybrid | N/A | 3.89 (0.07) | –0.22 (0.09) | .019 | |
| Willingness to get vaccinated (“Willingness”) | ||||||
|
|
Intervention effect | .006 | N/A | N/A | N/A | |
|
|
Control | N/A | 2.77 (0.09) | N/A | N/A | |
|
|
Narrative | N/A | 3.05 (0.09) | 0.28 (0.10) | .012 | |
|
|
Fact | N/A | 3.05 (0.09) | 0.28 (0.10) | .011 | |
|
|
Hybrid | N/A | 3.05 (0.09) | 0.28 (0.10) | .01 | |
aANCOVA: analysis of covariance.
bLS: least squares.
cF statistic, LS mean, and SE were obtained from an ANCOVA model for each outcome, with the intervention group as the main effect and adjusting for age, gender, race, education, income, and scores from 2 scales of general attitudes toward vaccines.
dP value adjusted for multiple comparisons between controls and intervention groups using the Dunnett test after finding a significant main effect for intervention.
eN/A: not applicable.
Hypothesis 2. Support for Sharing the Video Containing Misinformation About the COVID-19 Vaccine (Sharing)
For the Share scale, support for sharing the mis- and disinformation, the intervention group main effect was statistically significant (F(3,1928)=3.4, P=.02) using the Holm P value threshold of .05. For the control and intervention groups (Narrative, Fact, and Hybrid), the LS means (SE) were 4.11 (0.08), 3.90 (0.07), 3.90 (0.07), and 3.89 (0.07), respectively. The LS means for the difference between the control group and the 3 intervention groups were 0.21 (P=.03), 0.22 (P=.022), and 0.22 (P=.019) lower than that for the control group, respectively, indicating lower support for sharing/supporting the second video in each intervention group compared to controls.
Hypothesis 3. Willingness to Get vaccinated (Willingness)
The intervention group effect for the Willingness scale, willingness to get the vaccine, had the second smallest P value (F(3,1929)=4.1, P=.01) among the 3 study endpoints, which was significant at the Holm method adjusted cut-off of 0.05/2=.03. The LS means (SE) for the willingness scale for the control and 3 intervention groups were 2.77 (0.09), 3.05 (0.09), 3.05 (0.09), and 3.05 (0.09), respectively. The difference between the control groups and the 3 intervention groups (Narrative, Fact, and Hybrid) were 0.28 (P=.012), 0.28 (P=.011), and 0.28 (P=.01) points higher than that for the controls, respectively, indicating that subjects in the intervention groups were more willing to get the COVID-19 vaccine compared to controls.
Discussion
Principal Findings
The purpose of this study was to identify the effect of attitudinal inoculation videos on the ability to identify misinformation, willingness to share misinformation, and willingness to vaccinate. We found there was a significant effect of having been exposed to an inoculation video compared to a control video across each outcome of interest. Our results support our initial hypotheses that inoculation messaging can increase the ability to identify misinformation, decrease willingness to share misinformation, and increase willingness to vaccinate.
Our study explored not only whether there is an effect of inoculating participants but also whether inoculating against a narrative/rhetorical strategy or against factual misinformation is more effective. We also tested a hybrid video that combined fact-based and narrative/rhetorical strategies within the inoculation message. Past studies into the relative efficacy of narrative/rhetoric compared to fact-based appeals have suggested that narrative approaches are more likely to be persuasive to viewers [32-34,37-39,55]. However, we did not find significant differences across the 3 active intervention groups, suggesting that the content of the intervention video (narrative/rhetoric, fact based, or hybrid) does not impact the effect of the intervention. This may be attributable to the nuanced differences in the scripts used, which might have been difficult to distinguish in such a short time frame. Additionally, because there was only 1 video for each video script strategy, it is not possible to say whether there may be differences in other videos that used these same strategies. It is even possible that the cinematographic and casting choices behind each video (ie, the production and the medical workers who narrated them) themselves made indirect narrative and rhetorical appeals to viewers. These appeals include, for example, clean sets, approachable body language, hopeful music, and other emotionally engaging features of the videos. This, in turn, might have produced a “flattening” effect, rendering the appeals of the videos more uniform.
The intervention videos were designed to protect people against being misled by flawed argumentation used in common online mis- and disinformation, such as conspiracy theories [57,58]. In practice, this means that watching a video with an inoculation message and a weakened microdose of manipulation techniques allows viewers to discern more readily subsequent misinformation that makes use of similar flawed argumentation techniques. In this study, we were able to achieve this in videos that were only 30 seconds in duration. This is critical because 30 seconds is consistent with short attention spans for online video consumption on social media and the length of many ads online, enabling such a video to be shown in ad slots. Prior inoculation studies have tested longer-form videos or text [49,51,58]. These findings for the effects of 30-second videos have implications for the ability to disseminate inoculation messages in social media ad slots.
Furthermore, online platforms are a viable place to disseminate these interventions to affect perceptions and behavior, because information on vaccine injury is viewed and spread on social media and exposure to online misinformation is associated with lower vaccination intentions [17,59,60]. Social media platforms that may hesitate at the prospect of hosting inoculation videos containing a microdose of misinformation might be reassured that in the proper context of an inoculation message, these microdoses are vital to the overall discrediting of misinformation and disinformation.
Limitations
This study has limitations. First, the study sample was not representative of the general population but rather was more highly educated, mobile app users. Testing the effects of the intervention with a broader audience and determining whether there are differential effects among particular subsamples of the population will add to the understanding of the effect of these types of videos. Second, as described before, further investigation is needed to explore whether there may be meaningful differences in narrative versus fact versus hybrid models that could not be detected in this study due to the study design; however, in general, our results suggest that fact-based rhetorical strategies can be as effective as a narrative-rhetoric or hybrid approach.
Conclusion
As an infodemic management strategy, approaches that go beyond fact checking, and do not simply focus on countering 1 piece of content, may be valuable. We found that attitudinal inoculation in video-based messages may be an intervention strategy that can be used in designing public health messaging campaigns to counter mis- and disinformation. Online dissemination of these videos could be a viable strategy to increase vaccine uptake and can be tried more broadly. Videos that use attitudinal inoculation to combat COVID-19 vaccine misinformation should be tested with a broader audience beyond the United States and on social media platforms, such as YouTube and TikTok. More research is needed to understand how videos with attitudinal inoculation perform when individuals are in a typical information consumption environment and faced with competing demands for attention.
Abbreviations
- ANCOVA
analysis of covariance
- GED
General Educational Development
- LS
least squares
- PCA
principal component analysis
Footnotes
Conflicts of Interest: None declared.
References
- 1.Plato . In: The Gorgias of Plato. Woolsey TD, Stallbaum G, editors. Boston, MA: J. Munroe & Company; 1848. [Google Scholar]
- 2.Clem S. Post-truth and vices opposed to truth. J Soc Christ Ethics. 2017;37(2):97–116. [Google Scholar]
- 3.Aquinas T. Summa theologica. Complete English ed. TX: Christian Classics; 1981. [Google Scholar]
- 4.Freelon D, Wells C. Disinformation as political communication. Polit Commun. 2020 Feb 14;37(2):145–156. doi: 10.1080/10584609.2020.1723755. [DOI] [Google Scholar]
- 5.Sell T, Hosangadi D, Smith E, Trotochaud M, Vasudevan P, Gronvall G, Rivera Y, Sutton J, Ruiz A, Cicero A. National Priorities to Combat Misinformation and Disinformation for COVID-19 and Future Public Health Threats: A Call for a National Strategy. [2022-05-31]. https://www.centerforhealthsecurity.org/our-work/pubs_archive/pubs-pdfs/2021/210322-misinformation.pdf .
- 6.Bernardo T, Sobkowich KE, Forrest RO, Stewart LS, D'Agostino M, Perez Gutierrez E, Gillis D. Collaborating in the time of COVID-19: the scope and scale of innovative responses to a global pandemic. JMIR Public Health Surveill. 2021 Feb 09;7(2):e25935. doi: 10.2196/25935. https://publichealth.jmir.org/2021/2/e25935/ v7i2e25935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kapantai E, Christopoulou A, Berberidis C, Peristeras V. A systematic literature review on disinformation: toward a unified taxonomical framework. New Media Soc. 2020 Sep 20;23(5):1301–1326. doi: 10.1177/1461444820959296. [DOI] [Google Scholar]
- 8.Directorate-General for Communications Networks, Content and Technology (European Commission) A Multi-dimensional Approach to Disinformation: Report of the Independent High Level Group on Fake News and Online Disinformation. [2022-05-31]. https://op.europa.eu/en/publication-detail/-/publication/6ef4df8b-4cea-11e8-be1d-01aa75ed71a1 .
- 9.Davison K, Guan S. The quality of dietary information on the World Wide Web. J Can Diet Assoc. 1996;57(4):137–141. [Google Scholar]
- 10.Eysenbach G. Infodemiology and infoveillance: framework for an emerging set of public health informatics methods to analyze search, communication and publication behavior on the Internet. J Med Internet Res. 2009;11(1):e1157. doi: 10.2196/jmir.1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Calleja N, AbdAllah A, Abad N, Ahmed N, Albarracin D, Altieri E, Anoko JN, Arcos R, Azlan AA, Bayer J, Bechmann A, Bezbaruah S, Briand SC, Brooks I, Bucci LM, Burzo S, Czerniak C, De Domenico M, Dunn AG, Ecker UKH, Espinosa L, Francois C, Gradon K, Gruzd A, Gülgün BS, Haydarov R, Hurley C, Astuti SI, Ishizumi A, Johnson N, Johnson Restrepo D, Kajimoto M, Koyuncu A, Kulkarni S, Lamichhane J, Lewis R, Mahajan A, Mandil A, McAweeney E, Messer M, Moy W, Ndumbi Ngamala P, Nguyen T, Nunn M, Omer SB, Pagliari C, Patel P, Phuong L, Prybylski D, Rashidian A, Rempel E, Rubinelli S, Sacco P, Schneider A, Shu K, Smith M, Sufehmi H, Tangcharoensathien V, Terry R, Thacker N, Trewinnard T, Turner S, Tworek H, Uakkas S, Vraga E, Wardle C, Wasserman H, Wilhelm E, Würz A, Yau B, Zhou L, Purnat TD. A public health research agenda for managing infodemics: methods and results of the first WHO Infodemiology Conference. JMIR Infodemiol. 2021;1(1):e30979. doi: 10.2196/30979. http://europepmc.org/abstract/MED/34604708 .v1i1e30979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Akpan I, Aguolu O, Kobara Y, Razavi R, Akpan A, Shanker M. Association between what people learned about COVID-19 using web searches and their behavior toward public health guidelines: empirical infodemiology study. J Med Internet Res. 2021;23(9):e28975. doi: 10.2196/28975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bridgman A, Merkley E, Loewen PJ, Owen T, Ruths D, Teichmann L, Zhilin O. The Causes and Consequences of COVID-19 Misperceptions: Understanding the Role of News and Social Media. [2022-05-31]. https://misinforeview.hks.harvard.edu/article/the-causes-and-consequences-of-covid-19-misperceptions-understanding-the-role-of-news-and-social-media/
- 14.Allington D, Duffy B, Wessely S, Dhavan N, Rubin J. Health-protective behaviour, social media usage and conspiracy belief during the COVID-19 public health emergency. Psychol Med. 2021;51(10):1763–1769. doi: 10.1017/S003329172000224X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.SteelFisher GK, Blendon R, Caporello H. An uncertain public - encouraging acceptance of Covid-19 vaccines. N Engl J Med. 2021 May 22;384(16):1483–1487. doi: 10.1056/NEJMp2100351. [DOI] [PubMed] [Google Scholar]
- 16.Ognyanova K, Lazer D, Baum M, Druckman J, Green J, Perlis R. The COVID States Project #60: COVID-19 vaccine misinformation: from uncertainty to resistance. OSF Preprints. 2021 doi: 10.31219/osf.io/xtjad. [DOI] [Google Scholar]
- 17.Loomba S, de FA, Piatek S, de GK, Larson H. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat Hum Behav. 2021;5(3):337–348. doi: 10.1038/s41562-021-01056-1. [DOI] [PubMed] [Google Scholar]
- 18.Romer D, Jamieson K. Patterns of media use, strength of belief in COVID-19 conspiracy theories, and the prevention of COVID-19 from March to July 2020 in the United States: survey study. J Med Internet Res. 2021;23(4):e25215. doi: 10.2196/25215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Romer D, Jamieson K. Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc Sci Med. 2020;263:113356. doi: 10.1016/j.socscimed.2020.113356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Piltch-Loeb R, Savoia E, Goldberg B, Hughes B, Verhey T, Kayyem J. Examining the effect of information channel on COVID-19 vaccine acceptance. PLOS ONE. 2021;16(5):e0251095. doi: 10.1371/journal.pone.0251095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eysenbach G. How to fight an infodemic: the four pillars of infodemic management. J Med Internet Res. 2020 Jun 29;22(6):e21820. doi: 10.2196/21820. https://www.jmir.org/2020/6/e21820/ v22i6e21820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hameleers M, Powell TE, Van Der Meer TG, Bos L. A picture paints a thousand lies? The effects and mechanisms of multimodal disinformation and rebuttals disseminated via social media. Polit Commun. 2020 Feb 05;37(2):281–301. doi: 10.1080/10584609.2019.1674979. [DOI] [Google Scholar]
- 23.Pérez-Escolar M, Ordóñez-Olmedo E, Alcaide-Pulido P. Fact-checking skills and project-based learning about infodemic and disinformation. Think Skills Creat. 2021 Sep;41:100887. doi: 10.1016/j.tsc.2021.100887. [DOI] [Google Scholar]
- 24.Wood T, Porter E. The elusive backfire effect: mass attitudes’ steadfast factual adherence. Polit Behav. 2018 Jan 16;41(1):135–163. doi: 10.1007/s11109-018-9443-y. [DOI] [Google Scholar]
- 25.Zimmermann F, Kohring M. Mistrust, disinforming news, and vote choice: a panel survey on the origins and consequences of believing disinformation in the 2017 German parliamentary election. Polit Commun. 2020;37(2):215–237. [Google Scholar]
- 26.Rodríguez-Pérez C, Paniagua-Rojano F, Magallón-Rosa R. Debunking political disinformation through journalists’ perceptions: an analysis of Colombia’s fact-checking news practices. Media Commun. 2021;9(1):264–275. [Google Scholar]
- 27.Garrett L. COVID-19: the medium is the message. Lancet. 2020;395(10228):942–943. doi: 10.1016/S0140-6736(20)30600-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Graves L, Nyhan B, Reifler J. Understanding innovations in journalistic practice: a field experiment examining motivations for fact-checking. J Commun. 2016 Jan 08;66(1):102–138. doi: 10.1111/jcom.12198. [DOI] [Google Scholar]
- 29.Nemr C, Gangware W. Weapons of Mass Distraction: Foreign State-Sponsored Disinformation in the Digital Age. [2022-05-31]. https://www.state.gov/wp-content/uploads/2019/05/Weapons-of-Mass-Distraction-Foreign-State-Sponsored-Disinformation-in-the-Digital-Age.pdf .
- 30.Newton C. The Trauma Floor: The Secret Lives of Facebook Content Moderators in America. [2022-05-31]. https://www.theverge.com/2019/2/25/18229714/cognizant-facebook-content-moderator-interviews-trauma-working-conditions-arizona .
- 31.Roberts S. Behind the Screen. New Haven, CT: Yale University Press; 2019. [Google Scholar]
- 32.Adebayo A, Davidson Mhonde R, DeNicola N, Maibach E. The effectiveness of narrative versus didactic information formats on pregnant women's knowledge, risk perception, self-efficacy, and information seeking related to climate change health risks. Int J Environ Res Public Health. 2020 Sep 23;17(19):6969. doi: 10.3390/ijerph17196969. https://www.mdpi.com/resolver?pii=ijerph17196969 .ijerph17196969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu S, Yang JZ. The role of temporal distance perception in narrative vs. non-narrative persuasion related to e-cigarettes. J Health Commun. 2020 Jul 02;25(7):543–553. doi: 10.1080/10810730.2020.1788678. [DOI] [PubMed] [Google Scholar]
- 34.Murphy ST, Frank LB, Chatterjee JS, Moran MB, Zhao N, Amezola de Herrera P, Baezconde-Garbanati LA. Comparing the relative efficacy of narrative vs nonnarrative health messages in reducing health disparities using a randomized trial. Am J Public Health. 2015 Oct;105(10):2117–2123. doi: 10.2105/ajph.2014.302332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Falk E, Scholz C. Persuasion, influence, and value: perspectives from communication and social neuroscience. Annu Rev Psychol. 2018 Jan 04;69(1):329–356. doi: 10.1146/annurev-psych-122216-011821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bryan CJ, Yeager DS, Hinojosa CP. A values-alignment intervention protects adolescents from the effects of food marketing. Nat Hum Behav. 2019 Jun;3(6):596–603. doi: 10.1038/s41562-019-0586-6. http://europepmc.org/abstract/MED/30988478 .10.1038/s41562-019-0586-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen M, Bell RA. A meta-analysis of the impact of point of view on narrative processing and persuasion in health messaging. Psychol Health. 2022 May 06;37(5):545–562. doi: 10.1080/08870446.2021.1894331. [DOI] [PubMed] [Google Scholar]
- 38.de Wit JBF, Das E, Vet R. What works best: objective statistics or a personal testimonial? An assessment of the persuasive effects of different types of message evidence on risk perception. Health Psychol. 2008 Jan;27(1):110–115. doi: 10.1037/0278-6133.27.1.110.2008-00647-015 [DOI] [PubMed] [Google Scholar]
- 39.Gilkey M, Grabert B, Malo T, Hall M, Brewer N. Physicians' rhetorical strategies for motivating HPV vaccination. Soc Sci Med. 2020;266:113441. doi: 10.1016/j.socscimed.2020.113441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Maertens R, Roozenbeek J, Basol M, van der Linden S. Long-term effectiveness of inoculation against misinformation: three longitudinal experiments. J Exp Psychol Appl. 2021;27(1):1–16. doi: 10.1037/xap0000315. [DOI] [PubMed] [Google Scholar]
- 41.McGuire WJ. Inducing resistance to persuasion. Some contemporary approaches. In: Haaland CC, Kaelber WO, editors. Self and Society. An Anthology of Readings. Lexington, MA: Ginn Custom; 1981. pp. 192–230. [Google Scholar]
- 42.McGuire WJ, Papageorgis D. The relative efficacy of various types of prior belief-defense in producing immunity against persuasion. J Abnorm Soc Psychol. 1961 Mar;62(2):327–337. doi: 10.1037/h0042026. [DOI] [PubMed] [Google Scholar]
- 43.McGuire WJ. The effectiveness of supportive and refutational defenses in immunizing and restoring beliefs against persuasion. Sociometry. 1961;24(2):184–197. [Google Scholar]
- 44.Banas JA, Rains SA. A meta-analysis of research on inoculation theory. Commun Monogr. 2010 Sep;77(3):281–311. doi: 10.1080/03637751003758193. [DOI] [Google Scholar]
- 45.Braddock K. Vaccinating against hate: using attitudinal inoculation to confer resistance to persuasion by extremist propaganda. Terror Polit Violence. 2019:1–23. [Google Scholar]
- 46.Roozenbeek J, van der Linden S, Nygren T. Prebunking Interventions Based on the Psychological Theory of “Inoculation” Can Reduce Susceptibility to Misinformation Across Cultures. [2022-05-31]. https://misinforeview.hks.harvard.edu/article/global-vaccination-badnews/
- 47.Compton J, Jackson B, Dimmock JA. Persuading others to avoid persuasion: inoculation theory and resistant health attitudes. Front Psychol. 2016;7:122. doi: 10.3389/fpsyg.2016.00122. doi: 10.3389/fpsyg.2016.00122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cook J, Lewandowsky S, Ecker U. Neutralizing misinformation through inoculationxposing misleading argumentation techniques reduces their influence. PLOS ONE. 2017;12(5):e0175799. doi: 10.1371/journal.pone.0175799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Braddock K, Hughes B, Goldberg B, Miller-Idriss C. Subversive online activity predicts susceptibility to persuasion by far-right extremist propaganda. MediArXiv. doi: 10.33767/osf.io/c734s. Preprint posted online June 1, 2021. [DOI] [Google Scholar]
- 50.van DLS, Dixon G, Clarke C, Cook J. Inoculating against COVID-19 vaccine misinformation. EClinicalMedicine. 2021:33. doi: 10.1016/j.eclinm.2021.100772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hughes B, Braddock K, Miller-Idriss C, Goldberg B, Criezis M, Dashtgard P. Inoculating against persuasion by scientific racism propaganda: the moderating roles of propaganda form and subtlety. SocArXiv. Preprint posted online July 31, 2021 https://osf.io/preprints/socarxiv/ecqn4/download. [Google Scholar]
- 52.Savoia E, Piltch-Loeb R, Goldberg B, Miller-Idriss C, Hughes B, Montrond A, Kayyem J, Testa MA. Predictors of COVID-19 vaccine hesitancy: socio-demographics, co-morbidity, and past experience of racial discrimination. Vaccines (Basel) 2021 Jul 09;9(7):767. doi: 10.3390/vaccines9070767. https://www.mdpi.com/resolver?pii=vaccines9070767 .vaccines9070767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hughes B, Miller-Idriss C, Piltch-Loeb R, Goldberg B, White K, Criezis M. Development of a codebook of online anti-vaccination rhetoric to manage COVID-19 vaccine misinformation. Int J Environ Res Public Health. 2021;18(14):7556. doi: 10.3390/ijerph18147556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Roozenbeek J, van der Linden S. Fake news game confers psychological resistance against online misinformation. Palgrave Commun. 2019;5(1):1–10. [Google Scholar]
- 55.Ooms J, Hoeks J, Jansen C. "Hey, that could be me": the role of similarity in narrative persuasion. PLOS ONE. 2019;14(4):e0215359. doi: 10.1371/journal.pone.0215359. https://dx.plos.org/10.1371/journal.pone.0215359 .PONE-D-18-21702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rothschild D, Konitzer T. Random Device Engagement (RDE) with Organic Samples. New York, NY: Pollfish; 2022. [Google Scholar]
- 57.Lewandowsky S, Yesilada M. Inoculating against the spread of Islamophobic and radical-Islamist disinformation. Cogn Res Princ Implic. 2021 Aug 19;6(1):57. doi: 10.1186/s41235-021-00323-z. http://europepmc.org/abstract/MED/34410513 .10.1186/s41235-021-00323-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.van der Linden S, Leiserowitz A, Rosenthal S, Maibach E. Inoculating the public against misinformation about climate change. Glob Chall. 2017 Mar 27;1(2):1600008. doi: 10.1002/gch2.201600008. doi: 10.1002/gch2.201600008.GCH2201600008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lazer D, Green J, Ognyanova K, Baum M, Lin J, Druckman J. The COVID States Project #57: social media news consumption and COVID-19 vaccination rates. OSF Preprints. 2021 [Google Scholar]
- 60.Basch CE, Basch CH, Hillyer GC, Meleo-Erwin ZC, Zagnit EA. YouTube videos and informed decision-making about COVID-19 vaccination: successive sampling study. JMIR Public Health Surveill. 2021 May 06;7(5):e28352. doi: 10.2196/28352. https://publichealth.jmir.org/2021/5/e28352/ v7i5e28352 [DOI] [PMC free article] [PubMed] [Google Scholar]


