Abstract
Rib hyperostosis has previously been described in conjunction with disorders causing excessive vertebral ossification due to osseous bridging across the costovertebral joint, such as in diffuse idiopathic skeletal hyperostosis. Hyperostosis is believed to be a reactive process due to altered forces across the affected rib as bridging osteophytes decrease mobility at the respective costovertebral joint. The imaging characteristics of rib hyperostosis can be highly suspicious for malignancy. We share 2 cases of biopsy-proven benign rib hyperostosis with imaging across multiple modalities in hopes of increasing awareness of this entity and its imaging characteristics. In the first case, a 62-year-old female without history of malignancy underwent rib biopsy after bone scintigraphy demonstrated intense radiotracer uptake along a posteromedial rib. In the second case, a 66-year-old male with history of recurrent prostate cancer underwent rib biopsy after interval development of intense radiotracer uptake on bone scintigraphy along a posteromedial rib, new compared to 6 months prior. Both cases were seen in the setting of osseous bridging at the respective costovertebral joint. Imaging findings include contiguous radiotracer uptake on bone scintigraphy confined to the rib and respective costovertebral joint, cortical bone thickening with osseous excrescence at the costovertebral joint on radiographic and cross-sectional imaging, and increased osseous edema-like change, postcontrast enhancement, and surrounding soft tissue edema on magnetic resonance imaging. By increasing awareness to these imaging features, we hope to improve diagnostic confidence and decrease unnecessary, expensive, and sometimes invasive workup for future patients.
Keywords: Hyperostosis, Ribs, Diffuse idiopathic skeletal hyperostosis, Benign, Malignancy
Introduction
Benign hyperostosis of the ribs has previously been described in the setting of disorders causing excessive vertebral ossification, including diffuse idiopathic skeletal hyperostosis and seronegative spondyloarthropathies. Rib hyperostosis can present a challenging diagnostic dilemma for radiologists due to its alarming appearance on imaging. The imaging hallmarks of thickening and sclerosis of the involved bone, sometimes with increased radiotracer uptake on bone scintigraphy, are particularly worrisome in patients with a history or suspicion of malignancy. To further characterize its imaging characteristics and to bring increased awareness to this benign phenomenon, we describe 2 cases of rib hyperostosis that led to biopsy out of concern for malignancy. Both cases were seen in the setting of excessive vertebral ossification resulting in osseous bridging across the respective costovertebral joint. By sharing these biopsy-proven cases, we hope to improve diagnostic confidence for radiologists facing similar dilemmas in order to avoid unnecessary, costly, and sometimes invasive workup for patients.
Case report
In the first case, a 62-year-old woman with no history of cancer initially presented with complaints of dyspnea on exertion, decreased exercise tolerance, and pain with deep breathing for over 1 year. She had previous diagnoses of severe obstructive sleep apnea and a remote diagnosis of suspected asthma. The patient had never previously used a regular maintenance inhaler, but began using a family member's albuterol nebulizer daily due to worsening dyspnea. Pulmonary function test demonstrated moderate restriction without obstruction, no reversibility, and moderately reduced diffusion capacity. High resolution chest computed tomography (CT) was performed for further evaluation of the abnormal pulmonary function test and due to family history of pulmonary fibrosis. The pulmonary parenchyma was normal but findings of exuberant diffuse idiopathic skeletal hyperostosis were appreciated. The patient's symptoms continued, along with worsening right-sided pleurodynia, and she subsequently underwent bone scintigraphy with SPECT to evaluate for presumed psoriatic spondylitis as a cause of her symptoms. The study demonstrated intense radiotracer uptake in the posteromedial aspect of the right fifth rib, which corresponded to the area of pain (Fig. 1). Due to concern for malignancy, the woman underwent CT-guided core biopsy of the rib, which showed sclerotic bone and no neoplasm. Retrospective review of the patient's imaging demonstrated a large osseous excrescence spanning the right fifth costovertebral joint with hyperostosis of the rib.
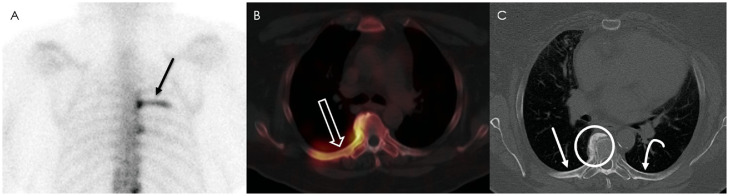
Fig. 1.
A 62-year-old female with rib hyperostosis in the setting of right-sided pleurodynia and concern for psoriatic spondylitis. Posterior view of the upper body from bone scintigraphy (A) and grayscale axial SPECT CT (B) demonstrate intense, contiguous radiotracer uptake spanning the right fifth costovertebral joint and posterior fifth rib (black arrow on A, open white arrow on B). Axial CT (C) demonstrates a large osseous excrescence at the right fifth costovertebral joint (white circle) with cortical thickening of the posterior fifth rib (straight white arrow). The adjacent left fifth costovertebral joint and posterior rib (curved white arrow) demonstrate no costovertebral bridging and normal cortical thickness.
In the second case, a 66-year-old man with a history of metastatic prostate cancer and multiple pulmonary recurrences was found to have new intense radiotracer uptake along the posteromedial aspect of the right fifth rib that was new compared to an exam performed 6 months prior. Contrast-enhanced magnetic resonance imaging of the chest wall was subsequently performed, demonstrating a thickened appearance of the right fifth rib with increased T2 signal in the bone marrow, surrounding soft tissue edematous changes, and postcontrast enhancement of the rib and adjacent soft tissues (Fig. 2). CT-guided core biopsy was then performed with pathology demonstrating remodeling woven bone that was negative for malignant cells. On review of prior CTs, it was noted that a large right fifth costovertebral joint excrescence had significantly increased in size over the intervening 6 months between the prior CT and the most recent CT, resulting in progressive costovertebral ankylosis. In retrospect, subtle increase in posteromedial rib cortical thickness and density was appreciable on both CT exams, consistent with hyperostosis.
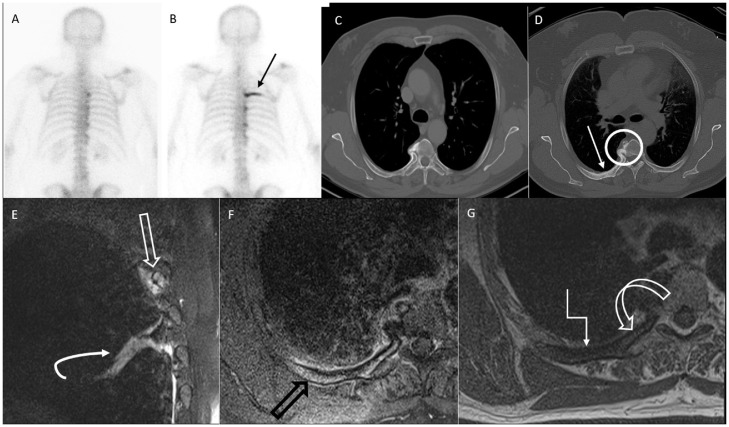
Fig. 2.
A 66-year-old male with rib hyperostosis in the setting of recurrent prostate cancer. Posterior views of the upper body from bone scintigraphy studies (A and B), image (A) obtained approximately 6 months prior to image (B). On image (B), there is new intense, contiguous radiotracer uptake spanning the right fifth costovertebral joint and posterior fifth rib (black arrow). Axial CT images (C and D) from the same patient, image (C) obtained approximately 6 months prior to image (D). On image (D), there is increased bony bridging across the right fifth costovertebral joint (white circle) compared to image (C) with cortical thickening of the posterior fifth rib (white arrow). Sagittal T2-weighted (E), axial postcontrast T1-weighted with fat suppression (F), axial precontrast T1-weighted (G) magnetic resonance images demonstrate edema-like signal of the posterior right fifth rib with adjacent soft tissue edema (open white arrow) on image (E), as well as posterior right fifth rib postcontrast osseous and adjacent soft tissue enhancement (open black arrow) on image (F). On image (G), there is decreased T1 signal in much of the rib due to marrow edema-like change (angled white arrow), but perseveration of normal marrow fat signal in the medial rib (curved open white arrow), importantly confirming the lack of a marrow-replacing process. There is incidental atelectasis (curved white arrow) noted on image (E).
Discussion
Rib hyperostosis is a finding often seen in association with disorders causing excessive vertebral ossification, including diffuse idiopathic skeletal hyperostosis, seronegative spondyloarthropathies, such as ankylosing spondylitis and psoriatic arthritis, and quadriplegia. Approximately 22% of patients with diffuse idiopathic skeletal hyperostosis have been found to have concurrent rib hyperostosis, along with approximately 10%-23% of patients with ankylosing spondylitis and 7% of patients with quadriplegia [1,2]. Hyperostosis is typically seen in the posteromedial aspect of the rib and is frequently seen in conjunction with a large osseous excrescence spanning the respective costovertebral joint and associated ossification of the radiate ligament, which attaches the rib head to the vertebral body [3]. It is hypothesized that ankylosis of the costovertebral joint produces increased loading forces on the rib due to loss of costovertebral joint mobility [1,2]. The resulting new strain on the affected rib leads to bony remodeling through Wolff's law that manifests as reactive hyperostosis on imaging [4].
Similarly, Macones et al. have previously reported stress-related hyperostosis of the posterior ribs and articular transverse processes in the chest radiographs of 80 asymptomatic patients. These authors examined the right-to-left rib involvement (9:1) and occupational histories and concluded that this hyperostosis occurs at sites most stressed with bending and rotation of the thorax [5].
They postulated that the radiographic rib changes observed might be due to altered biomechanics with resulting stress-related changes due to chronic pulling of the iliocostalis thoracis muscle and were of no clinical significance. They further concluded that the variation in ribs involved and lack of more widespread occurrence is probably due to either hyperreactivity of the iliocostalis thoracis muscle or a propensity for hyperostosis in the affected group. Our 2 cases differ in that the first patient was symptomatic and the second patient had metastatic prostate cancer. We also point out that although rib hyperostosis is a benign and frequently clinically insignificant finding, chest wall hypomobility in patients with diffuse idiopathic skeletal hyperostosis-associated rib hyperostosis has been shown to be a risk factor for poor prognosis after cervical spine injury [6].
Other differential diagnoses to consider in the setting of thickened or sclerotic ribs include fibrous dysplasia, Paget's disease, and renal osteodystrophy. Fibrous dysplasia can cause fusiform rib enlargement, but would demonstrate loss of normal trabeculation with possible ground glass matrix on CT and cortical thinning rather than thickening. Paget's disease uncommonly affects the ribs (1-4% of cases), but typically demonstrates cortical thickening and bone enlargement, like reactive hyperostosis. However, trabecular thickening is typically also seen, as well as imaging findings of Paget's disease throughout other areas of the skeleton. Renal osteodystrophy may also demonstrate bony sclerosis, but would cause diffuse changes rather than solitary or limited bone involvement [7,8]. Melorheostosis is an additional differential to consider in cases of rib thickening, though much more cortical thickening would typically be expected in melorheostosis compared to reactive hyperostosis [9].
As demonstrated in our 2 cases, the imaging appearance of rib hyperostosis can be highly concerning for malignancy. We suggest the following imaging features would support the diagnosis of benign rib hyperostosis rather than malignancy 1) solitary or limited bone scintigraphic changes confined to the posterior ribs only, 2) scintigraphic or SPECT activity starting at the vertebra extending contiguously outward without skip areas, 3) cortical hyperostosis with costovertebral ligamentous ossification on CT or radiography, 4) absence of destructive or permeative changes, and 5) absence of intramedullary osteoblastic changes. If these findings are present, a confident diagnosis of benign hyperostosis rather than malignancy can be made. Additionally, magnetic resonance imaging can demonstrate bone marrow edema-like signal, adjacent soft tissue edema, and postcontrast enhancement.
In both of our cases, findings of rib hyperostosis, initially found on bone scintigraphy, led to biopsy due to concern for malignant rib involvement. Awareness of rib hyperostosis, its associations, and its radiographic, cross-sectional, and scintigraphic features is important within the radiology community to avoid expensive, invasive, and unnecessary workup for this benign phenomenon.
Patient consent
Informed written consent was obtained from the subjects described in this report.
Footnotes
Competing Interests: The authors declare that there is no conflict of interest.
REFERENCES
- 1.Huang GS, Park YH, Taylor JAM, Sartoris DJ, Seragini F, Pathria MN, et al. Hyperostosis of ribs: association with vertebral ossification. J Rheumatol. 1993;20(12):2073–2076. [PubMed] [Google Scholar]
- 2.Frager L, Heaton D, Walker CM, Young K, Everist BM. Incidental posterior rib hyperostosis on chest CT: incidence and etiology. Skeletal Radiol. 2021;51(6):1173–1178. doi: 10.1007/s00256-021-03933-2. [DOI] [PubMed] [Google Scholar]
- 3.Saker E, Graham RA, Nicholas R, et al. Ligaments of the costovertebral joints including biomechanics, innervations, and clinical applications: a comprehensive review with application to approaches to the thoracic spine. Cureus. 2016;8(11):e874. doi: 10.7759/cureus.874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pearson OM, Lieberman DE. The aging of Wolff's “Law”: Ontogeny and responses to mechanical loading in cortical bone. Yearbook Phys Anthropol. 2004;47:63–69. doi: 10.1002/ajpa.20155. [DOI] [PubMed] [Google Scholar]
- 5.Macones AJ, Fisher MS, Locke J. Stress-related rib and vertebral changes. Radiology. 1989;170:117–119. doi: 10.1148/radiology.170.1.2783263. [DOI] [PubMed] [Google Scholar]
- 6.Sawakami K, Watanabe K, Sato T, Miura K, Katsumi K, Hosaka N, et al. Rib hyperostosis as a risk factor for poor prognosis in cervical spine injury patients with diffuse idiopathic hyperostosis. Spine. 2020;45:300–308. doi: 10.1097/BRS.0000000000003252. [DOI] [PubMed] [Google Scholar]
- 7.Guttentag AR, Salwen JK. Keep your eyes on the ribs: the spectrum of normal variants and diseases that involve the ribs. RadioGraphics. 1999;19:1125–1142. doi: 10.1148/radiographics.19.5.g99se011125. [DOI] [PubMed] [Google Scholar]
- 8.Levine BD, Motamedi K, Chow K, Gold RH, Seeger LL, et al. CT of rib lesions. AJR. 2009;193:5–13. doi: 10.2214/AJR.08.1216. [DOI] [PubMed] [Google Scholar]
- 9.Nasu K, Kuroki Y, Nawano S, Murakami K, Kuroki S, Sekiguchi R, et al. Thoracic cage extent of melorheostosis depicted by multislice CT. Skeletal Radiol. 2002;31:464–466. doi: 10.1007/s00256-002-0541-9. [DOI] [PubMed] [Google Scholar]