Abstract
Background:
Less than 1% adults in the United States who meet body mass index criteria undergo bariatric surgery. Our objective was to identify patient and provider perceptions of individual-level barriers to undergoing bariatric surgery.
Methods:
Adults with severe obesity and obesity care providers described their experiences with the bariatric surgery care process in semi-structured interviews. Using conventional content analysis, individual-level barriers were identified within Andersen’s Behavioral Model of Health Services Use.
Results:
Of the 73 individuals interviewed, 36 (49%) were female, and 15 (21%) were nonwhite. Six individual-level barriers were identified: fear of surgery, fear of lifestyle change, perception that weight had not reached its “tipping point,” concerns about dietary changes, lack of social support, and patient characteristics influencing referral.
Conclusions:
Patient and provider education should address patient fears of surgery and the belief that surgery is a “last resort.” Bariatric surgery programs should strengthen social support networks for patients.
Keywords: bariatric surgery, individual-level barriers, patient barriers, patient perceptions, provider perceptions
INTRODUCTION
An estimated 15% of U.S. adults meet body mass index (BMI) criteria for bariatric surgery (BMI ≥ 40 kg/m2 or ≥ 35 kg/m2 with an obesity-related health condition).1 Bariatric surgery is the most effective weight loss treatment when compared to behavioral weight management alone, leading to more sustained weight loss, greater co-morbidity resolution, and improved quality of life.2–5 Since the early 2000s, bariatric surgery mortality and complication rates have progressively improved to a serious adverse event rate less than 6% and perioperative mortality rate less than 0.2%.4 An appendectomy has similar adverse event and mortality rates.6
Despite the advances in bariatric surgery safety and efficacy, fewer than 1% of adults who meet the BMI criteria undergo bariatric surgery.1 Furthermore, less than 4% who meet BMI criteria and are actively participating in a behavioral weight management program undergo surgery.7 We have previously described barriers at the health system level, including care coordination and limited knowledge about bariatric surgery among referring providers.8 Individual-level barriers to bariatric surgery, such as fear of surgery or its complications, lack of interest in bariatric surgery, and financial concerns have been identified in quantitative studies, including surveys.9–12 To our knowledge, no investigators have used a qualitative study design that includes both patient and provider perspectives to investigate individual-level barriers to undergoing bariatric surgery.
Our objective was to identify patient and provider perceptions of individual-level barriers to undergoing bariatric surgery. To explore these themes, we performed semi-structured interviews with adults with severe obesity, primary care providers (PCPs), bariatric surgeons, registered dietitians (RDs), and health psychologists.
METHODS
Setting and population
Patients - Patients from two Veteran Affairs (VA) medical centers (VAMCs) in the Great Lakes Veterans Integrated Services Network (VISN) were eligible if they had attended behavioral or surgical weight management programs and met National Institute of Health (NIH) BMI criteria for bariatric surgery: 1) BMI ≥ 40 kg/m2, or 2) BMI ≥ 35 kg/m2 with an obesity-related health condition (coronary artery disease, gastroesophageal reflux disease, hypertension, obstructive sleep apnea, type 2 diabetes mellitus). Behavioral weight management program attendance was defined as participation in three or more MOVE! Weight Management Program (MOVE!) visits with the first visit in the 6–18 months preceding study initiation. MOVE! is the VA’s evidence-based program adapted from the Diabetes Prevention Program.13 Individual or group MOVE! visits are typically led by RDs and focus on improving nutrition, increasing physical activity, and implementing behavioral strategies, such as goal setting and self-monitoring.
Surgical weight management patients were adults (age ≥18 years) who had been referred for or undergone bariatric surgery and had participated in a MOVE! visit in the 1–6 years preceding study initiation. This timeframe permitted an adequate number of eligible bariatric surgery patients to be identified via electronic health record data and recruited for the study. Since some bariatric surgery programs exclude individuals based on age from bariatric surgery eligibility, we excluded patients older than 70 years of age.
Providers - PCPs, bariatric surgeons, RDs, and health psychologists were selected due to their involvement in the referral process and multidisciplinary management of bariatric surgery patients. Providers were included to ensure a holistic representation of perceived patient barriers to bariatric surgery. PCPs, RDs, and health psychologists were recruited from one of the three VAMCs in the Great Lakes VISN, which is one of 23 regional VA service networks. Eligible PCPs were defined as physicians, physician assistants, or nurse practitioners with a panel of more than 250 patients. We purposefully targeted bariatric surgeon recruitment from the five VHA regions (North Atlantic, Southeast, Midwest, Continental, and Pacific districts) that comprise all 21 bariatric surgery programs across the country.
The UW-Madison IRB and the William S. Middleton VA Research & Development Committee (VA R&D) approved the study. Written or verbal informed consent was obtained prior to all interviews. Other study procedures were performed in accordance with the Helsinki Declaration of 1975. The Consolidated Criteria for Reporting Qualitative Research (COREQ) reporting guidelines were followed (see document, Supplemental Digital Content 1).
Data collection
Recruitment letters and emails were sent to eligible patients or providers, respectively. Individuals were invited to participate in a semi-structured, 60-minute interview. Due to scheduling logistics or distance, provider interviews were either completed via telephone or in-person. Patient interviews were all conducted in-person. Interviews were conducted by 2 Master’s-level research team members (SAJ, CRB) from August 2016 to May 2017. Providers described their experiences managing adults with obesity and their perceptions of individual-level barriers to bariatric surgery (see document, Supplemental Digital Content 2). Patients described their experiences navigating weight loss treatment options, their motivations for pursuing either surgical or behavioral weight loss, any barriers or difficulties they encountered, and how their outcomes compared to their expectations (see document, Supplemental Digital Content 3). Following the interview, all participants completed a demographic survey that included age, education level, race/ethnicity, sex, and socioeconomic status.
Data analysis
Audio-recorded interviews were transcribed, de-identified, and uploaded to NVivo Version 11.14 Conventional content analysis with both emergent and a priori codes originating from research questions were used to analyze the data.15 The initial draft of codes was created independently by five research team members (SAJ, EA, RLG, CIV, LMF) using seven transcripts (approximately 10% of the total). These five members then met to identify themes, discuss their annotations, resolve differences, and determine the code definitions for the finalized codebook. Three coders (SAJ, EA, GES) used the finalized codebook to individually code approximately one-third of the remaining transcripts using constant comparison.16 Any areas of text that were unclear to the coder were brought to regular group coding meetings to discuss and reach consensus among the three coders. There were 15 codes from patient transcripts and 28 codes from provider transcripts used to identify data relating to bariatric surgery (see document, Supplemental Digital Content 4). Higher level analysis was performed by the entire research team using data matrices divided by codes as rows and participant group as columns (patient, PCP, bariatric surgeon, RD, or health psychologist).17 The resulting sub-themes were grouped according to Andersen’s model and used to formulate the six identified study themes (see document, Supplemental Digital Content 4). Purposeful sampling was used to achieve thematic saturation, and data triangulation between different stakeholder groups was used to ensure a comprehensive description of each studied phenomenon was obtained.
Research team backgrounds - To minimize bias during the coding process, we involved multiple clinical and non-clinical researchers with distinctive training backgrounds. SAJ is a white, female masters-level researcher with a background in anthropology. GES is a white, female graduate student with a background in social science. AF is a white, male medical student. RLG and JAM are white, female post-doctoral health-services research fellows and general surgery residents. EA is a white, female, PhD social scientist and director of the qualitative core in the Department of Surgery at UW-Madison. CIV is a white, female, PhD social psychologist and mixed methods health-services researcher. LMF is a white, male health-services researcher and bariatric surgeon. SDR is a white, female PhD in psychology and the National Director of the VA MOVE! program.
Andersen’s Behavioral Model of Health Services Use was used as a framework for generated themes because, our group has previously adopted this model for use in bariatric surgery18 and applied it to system-level bariatric surgery barriers.8 Andersen’s model is divided into contextual and individual determinants, health behaviors, and outcomes. In the current study, we focused on the individual determinants and personal health practices. Personal health practices are a subset of health behaviors that are performed by the individual and alter one’s health, such as diet, physical activity, medication adherence, and tobacco use. Individual determinants describe how service utilization is influenced by an individual’s need, health behaviors, and predisposing beliefs or social structure. Individual-level barriers also include patient and provider interactions. Andersen’s model uses three components to describe individual utilization of the health care system: 1) factors that prompt service use; 2) factors that impede or enable service utilization; and 3) need for medical treatment. Per Andersen’s model there are four types of “predisposing” individual characteristics (demographics, genetics, social structure, and beliefs), two types of individual “need” characteristics (perceived and evaluated), and two types of “enabling” individual characteristics (financing and organizational factors).19
RESULTS
Of the 1,091 patients and 229 providers assessed for study eligibility, 592 patients and 187 providers met inclusion criteria (Figure 1). Recruitment letters were sent to 271 patients and 182 providers. The remaining 321 patients were not contacted as we had reached thematic saturation. We interviewed 33 patients and 40 providers (15 PCPs, 13 bariatric surgeons, 6 RDs, 6 health psychologists). Bariatric surgeons from all five VHA regions were interviewed. Patient participants were predominantly male (79%), and providers were predominantly female (73%). More than half of the patients were married (55%), and 45% had a household income less than $50,000 (Table 1).
Figure 1: Flowchart detailing patient and provider recruitment.
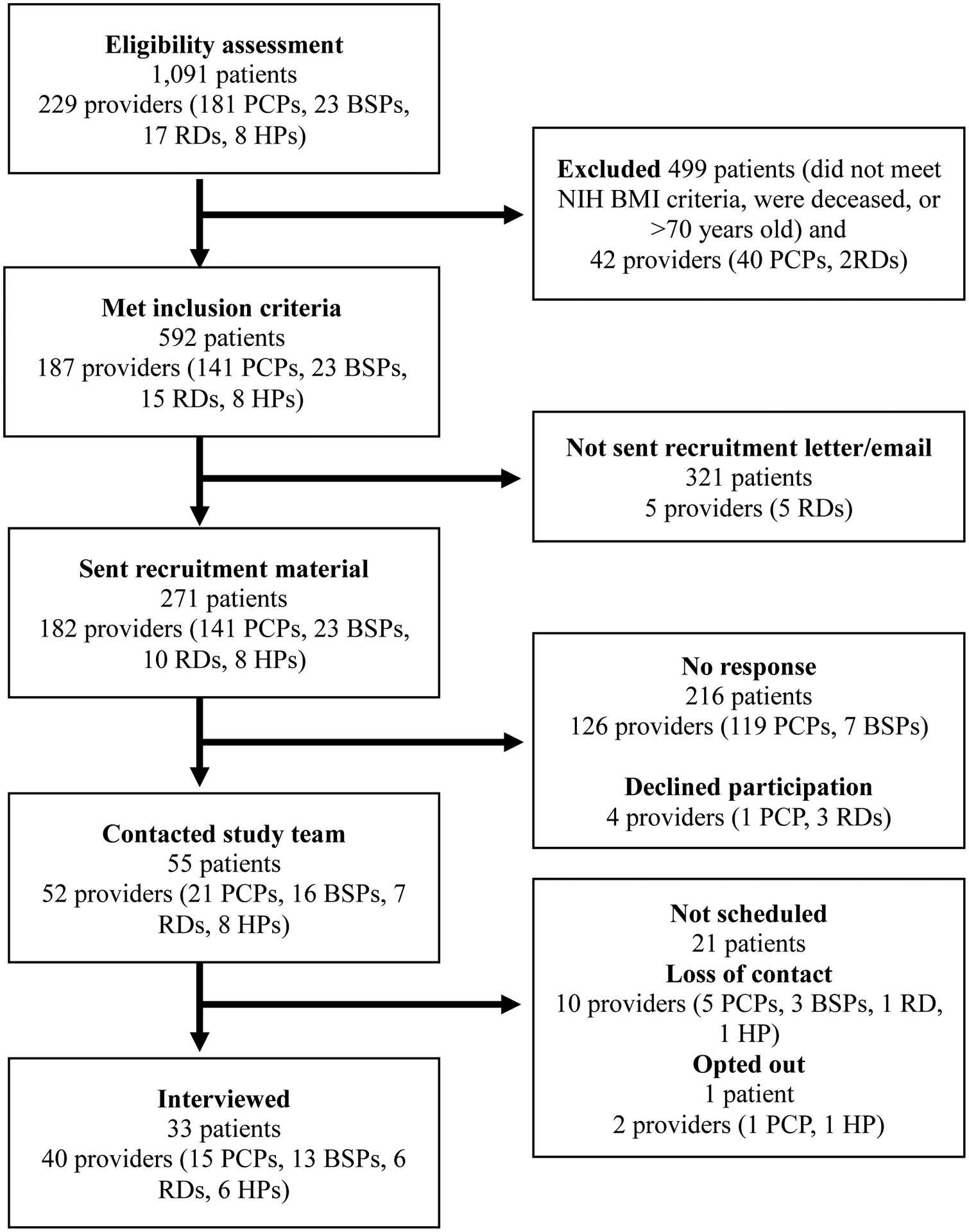
PCP: Primary care providers; HP: Health psychologist; BSP: Bariatric surgery provider; RD: Registered dietician
Table 1.
Study participant demographics
| Patients (n=33) | Providers (n=40) | |
|---|---|---|
| Age (mean, SD) | 58.5 (±8.4) | 44.0 (±9.9) |
| Gender (n, %) | ||
| Male | 26 (79) | 11 (27) |
| Female | 7 (21) | 29 (73) |
| Race (n, %) | ||
| White | 25 (76) | 31 (78) |
| Black or African American | 7 (21) | 0 |
| Hispanic | 1 (3) | 1 (2.5) |
| Other | 0 | 8 (20) |
| Marital status (n, %) | ||
| Married | 18 (55) | |
| Single, never married | 9 (27) | |
| Divorced/Separated | 6 (18) | |
| Years in practice (mean, SD) | 13.7 (±9.3) | |
| Dual appointment at university (n, %) | 17 (43) | |
| Highest level of education (n, %) | ||
| Graduate or postgraduate | 7 (21) | |
| Bachelor’s degree, Associate Degree or Trade/Technical/vocati onal school | 8 (24) | |
| High school graduate or some college credit but no degree | 16 (49) | |
| Some high school | 2 (6) | |
| Current work status (n, %) | ||
| Employed or student | 9 (27) | |
| Unemployed, searching for work | 1 (3) | |
| Retired | 10 (30) | |
| Disabled | 13 (40) | |
| Annual household income (n, %) | ||
| Greater than $100,000 | 4 (12) | |
| $50,000–$99,999 | 13 (40) | |
| Less than $50,000 | 15 (45) | |
| Declined to answer | 1 (3) | |
Six themes were identified and mapped to Andersen’s Behavioral Model of Health Services Use (Table 2). Table 3 displays the identified themes by the provider or patient group that expressed them. Representative patient and provider quotes for each theme are included in Table 4. The six study themes were:
Table 2.
Individual-level barriers to bariatric surgery (per Andersen’s Behavioral Model of Health Services Use)
| Individual determinant | Individual determinant description according to Andersen’s Model | Study theme |
|---|---|---|
| Predisposing: Social structure | Social networks and interactions, education, occupation | 1. Lack of social support |
| Predisposing: Health beliefs | Underlying attitudes, values, and knowledge of the healthcare system | 2. Fear of surgery and its outcomes (e.g. scared of surgery, complications, excess skin, or possibility of weight regain or sub-optimal results) 3. Fear of lifestyle change (e.g., dietary, lifelong process) 4. Patient characteristics influencing provider referral (e.g., mental illness, substance abuse, perceived patient motivation) |
| Need: Perceived | An individual’s perceived need for healthcare based on their own health, functional state, symptoms and whether they judge the problem warrants help | 5. Perception that weight had not reached its “tipping point” (i.e., not life threatening or severely impacting quality of life) |
| Health behaviors: Personal health practices | An individual’s practices that influence health status such as diet, stress management, and adherence to medical advice | 6. Concerns about adhering to recommended dietary changes |
Table 3.
Individual-level barriers to bariatric surgery from patient and provider perspectives
| Individual determinant | Theme | PCP | Bariatric surgeon | Registered dietitian | Health psychologist | Patient |
|---|---|---|---|---|---|---|
| Social | 1. Lack of social support | X | X | X | ||
| Beliefs | 2. Fear of surgery and its outcomes | X | X | X | X | |
| 3. Fear of lifestyle change | X | X | X | X | ||
| 4. Patient characteristics influencing provider referral | X | X | X | |||
| Need | 5. Perception that weight had not reached its “tipping point” | X | X | X | X | X |
| Personal Health Practices | 6. Concerns about adhering to recommended dietary changes | X | X | X | X |
X indicates the barrier was identified as a theme during interviews with that type of study participant
Table 4.
Representative patient and provider quotes regarding individual-level barriers to bariatric surgery
| Theme | PCP | Bariatric surgeon | Registered dietitian | Health psychologist | Patient |
|---|---|---|---|---|---|
| 1. Lack of social support | “If they don’t have stability in their life, mentally and socially…then it’s not going to be as successful.” | “The best candidates had a lot of social support from family and friends and people who wouldn’t look at bariatric surgery as somehow cheating or lazy.” | “I just didn’t have the support to help me out after surgery” | ||
| 2. Fear of surgery and its outcomes | “There is the terror of surgery …that they could have a complication of it. That they might have chronic diarrhea or something like that or chronic reflux.” | “On the patient side it’s a …lack of understanding of what the risks actually are, and maybe potential unfounded fear in having bariatric surgery. I think those are kind of the biggest boundaries to referral.” | “Often they say they want surgery and they don’t really know the long- term ramifications of that. So, we do some instruction up front about what are the different surgeries, what are the risks? Sometimes people are like, ‘oh, no, never mind, that’s not for me.’” | “I’m going to take a perfectly good organ and frickin’ mangle it…half the reason why I backed out of that surgery” | |
| 3. Fear of lifestyle change | “I think that there is a fear that they won’t be able to eat the way they eat now.” | “I’ll get some patients who start the process, and they’re just, when they learn more what the changes they have to adhere to, just know they couldn’t do it” | “Specifically with carbonated beverages, you’re going to have to give up for rest of your life. Is that something that you’re willing to do? ‘Cause I do have some patients that I ask that question to already, and I get the answer “no”. That’s a big deterrent for them having surgery” | “I know you have to change your lifestyle. But I just didn’t feel like I wanted to do it that way.” | |
| 4. Patient characteristics influencing provider referral | “I feel like they haven’t put in the effort to try… their diabetes is not controlled, they’re not using their CPAP machines… all those little issues which will provide you with lack of motivation, which will make them more like less motivated, so I try to discourage” | “… patients that have had previous substance abuse have learned a lot of coping mechanisms to help with sobriety. I never thought that they would be good candidates, but what I’m finding is that they’re actually really good candidates.” | “Sometimes patients are in a real rush to get the surgery but aren’t from a behavioral standpoint really ready” | ||
| 5. Perception that weight had not reached its “tipping point” | “Well most of them really don’t [get surgery] unless they have a life threatening…reason.” | “Everybody who canceled their surgery said, “You know what I think I can do this on my own.” | “I would say that they see it as kind of life or death at that point. They have such a poor quality of life being morbidly obese, they’ve tried everything under sun, that this surgery is their last option to try to take some control of their life back.” “People have surprised me and said “I don’t need it” |
“We often also see a number of patients…who have in their minds that the surgery is sort of last resort for them.” | “I wanted to do it on my own, because I really didn’t want to alter my body.” “I just felt like there should have been a bridge. Before you go through this diet and gastric bypass there should be something like, “okay try this medication or something and see if this helps”” |
| 6. Concerns about adhering to recommended dietary changes | “I know a lot of people do have a hard time maintaining the diet. Several of my patients just kind of graze all day.” | “We say three months of weight management needs to occur [before surgery], so not every patient can do that” | “Food is a source of comfort…but if they use it as a coping tool, their relationship with it has to change. And that can be challenging.” | “You know I don’t mind eating less food, but to tell me to not be able to eat certain things or drink certain things…it just seemed not worthwhile for me.” |
1. Fear of surgery and its outcomes
Patients described a reluctance to pursue surgery due to prior negative experiences with other surgical procedures, stories from acquaintances with adverse outcomes after bariatric surgery, or from Internet research. One patient described needing to “accept that [surgery] could be my time” to die prior to pursuing. Providers perceived these sentiments as a “fear of surgery.” Providers and patients voiced concerns regarding complications from the surgery. Patients were concerned about the invasiveness of the procedure and the alteration of a “healthy organ.” One patient canceled his scheduled surgery because he didn’t want to mangle a “perfectly good organ,” and another did not believe in “altering the body manually.” Patients were not convinced that surgery would achieve weight loss or comorbidity resolution; they did “not want to alter [their] body” without a guarantee of success. Patients were concerned that additional surgery would be required, for instance plastic surgery to remove excess skin. Given these concerns, some patients considered surgery as a “last resort;” providers had a similar perception of patient views that surgery was the last option to “take some control of their life back.” Notably, health psychologists did not discuss fear of surgery as a patient barrier.
2. Fear of lifestyle change
Patients described fear of commitment to a “life-long process.” This fear of commitment was linked to the irreversible nature of bariatric surgery and concern regarding negative consequences if lifestyle changes were not adhered to (e.g., pain after overeating). One patient in his 60s felt he was too old to incorporate the lifestyle changes and stated he would have considered surgery more if he had been younger. Bariatric surgeons, RDs and PCPs perceived that patients’ feared lifestyle changes and having to adhere to a new diet. Providers described some patients as unwilling to incorporate dietary changes, such as limiting carbohydrates or eliminating soda. Health psychologists did not perceive patient fear of lifestyle change as a barrier.
3. Perception that weight had not reached its “tipping point”
Patients and all provider groups did not perceive a need for surgery until obesity was “lifethreatening” or until co-morbidities limited physical function to an unacceptable degree. Patients were not convinced that their obesity severity required an intervention as invasive as surgery. Furthermore, patients maintained the belief that they could lose weight on their own. Many patients spoke of surgery as “too extreme;” they would rather try medications or other nonsurgical options for weight loss. Once weight reached its “tipping point,” patients and providers described severe obesity and its associated comorbidities as a motivational factor. Until the “tipping point” was reached, patients often adapted to physical changes caused by their weight gain; as one patient who did not pursue surgery said, “I’m at a point now where okay, I have the cane, I deal with the cane.” Some felt that learning to ambulate with a cane, wearing a continuous positive airway pressure (CPAP), or starting insulin was preferable to undergoing bariatric surgery.
4. Concerns about adhering to recommended dietary changes
Adhering to dietary changes was described as a barrier by patients, PCPs, bariatric surgeons, and RDs. Providers perceived that patients lacked motivation to adhere to recommended dietary changes. One patient who did not pursue surgery said “there’s no way I could ever maintain that diet.” Providers also noted that patients with prior failed weight loss attempts felt discouraged from trying again. Providers and patients described food as a coping mechanism with one patient stating “when I got free from drugs, I turned to food. That was my drug.” Other patients described using food as a “crutch,” making it difficult to adhere to dietary changes in the long-term. Post-operatively, one participant described feeling like a “trapped animal” due to the constant hunger from his psychiatric medications competing with the pain he experienced when eating. Patients described meal preparation taking too long or difficulty finding healthy food options in food pantries or for affordable prices as barriers.
5. Lack of social support
The attitude of the patients’ family and friends toward bariatric surgery influenced the decision to pursue surgery, with those describing surgery as “somehow cheating or lazy” unlikely to pursue surgery. Patients, PCPs, and health psychologists described the importance of a stable social support network capable of providing post-operative care and emotional support. One patient who did not pursue surgery said “half the reason why [he] backed out was [his] mother and sister not getting along, and after surgery you have to depend on somebody.” Registered dieticians and bariatric surgeons did not discuss social support networks. Providers viewed patients without social support as unlikely to be successful surgical candidates.
6. Patient characteristics influencing provider referral
Some PCPs, RDs, and health psychologists described older age and a history of mental illness or substance abuse as a barrier to referral. However, providers within each group had different views. One RD described a history of substance abuse as a characteristic associated with improved adherence, since patients in remission are more likely to have coping skills that make them more successful after surgery. Providers used patient reliability and appointment attendance as a proxy for motivation to undergo bariatric surgery. For example, one PCP described poorly controlled diabetes or poor CPAP therapy compliance as indicative of a lack of patient motivation and would discourage those patients from surgery.
DISCUSSION
The patients and providers who participated in this qualitative study described numerous individual-level barriers to bariatric surgery. All types of participant groups reported the perception that weight had not reached its “tipping point” as a barrier. Patients and multiple provider groups noted that fear of surgery, fear of change, and concerns about adhering to the recommended diet were obstacles to bariatric surgery.
Patients and providers cited concerns over bariatric surgery safety and its potential complications as reasons for not pursuing surgery. Other studies have reported similar perceptions that bariatric surgery is high risk. In a survey of 284 patients interested in bariatric surgery, respondents cited the following reasons for not pursuing bariatric surgery: fear of complications from surgery (51%), fear of dying (25%), and fear of surgery in general (24%).9 In our study and elsewhere in the literature, bariatric surgery was described as a method of “last resort” and “‘too extreme.”10,20,21 Interestingly, there seems to be a disconnect between the risk patients are willing to accept and the actual risk of bariatric surgery. In a survey study involving 654 U.S. patients interested in bariatric surgery, the mean acceptable mortality risk was 6.7% with 20% of the cohort willing to undertake a risk of >10%.22 This is substantially higher than the current bariatric surgery mortality rate of <0.1%.4 Our study suggests that there may be a “tipping point” where patients decided surgery was beneficial. At that point, co-morbidities and other factors, such as decreased mobility, being able to play with grandchildren, and fear of dying, became motivations for pursuing bariatric surgery.
In our analysis, patients felt that their obesity and its associated co-morbidities was not severe enough to warrant bariatric surgery. They considered bariatric surgery as a “last resort.”Other studies have noted a similar incongruence between the severity of patients’ obesity and comorbid conditions and bariatric surgery interest.10,23 Furthermore, individuals with overweight and obesity tend to underestimate their weight, and this is associated with decreased surgical interest.10 In a survey study of 657 adults with overweight and obesity, 55% of men and 31% of women did not correctly self-identify as having overweight and less than 10% correctly identified themselves as having obesity or “very overweight.”24 Patient and provider education is needed to improve the identification of obesity and the understanding of the associated risks.
Participants were also worried they would undergo an invasive procedure and subsequently not lose enough weight initially or later regain weight. The evidence indicates that 80–90% of patients demonstrate optimal weight loss after one year, defined as >50% excess weight loss (EWL).25,26 Yet, numerous studies have reported that bariatric surgery candidates have unrealistic pre- and post-operative weight loss expectations; thus, they are disappointed even with a good weight loss outcome.26,27 Patients in one survey study of 284 prospective bariatric surgery patients stated that 99% EWL would be ideal and 52% EWL, which is considered a successful surgical outcome, would be disappointing.27
Setting realistic attainable expectations for weight management before surgery may be associated with improved patient satisfaction and behavioral maintenance adherence after surgery.28,29 One innovative approach to setting appropriate weight-loss expectations was recently described by Varban and colleagues, who used state-wide bariatric registry data to predict weight loss one year after surgery.30 Implementation of these types of predictive models may help identify patients who need additional post-operative behavioral treatment to optimize weight loss.
Patients and provider groups voiced concerns about the ability to adhere to recommended dietary changes. Dietary noncompliance after bariatric surgery affects a significant proportion of patients post-operatively, with a prospective clinical follow-up of 100 bariatric surgery patients finding 40% of patients were noncompliant with dietary recommendations within one year of surgery.31 Grazing behaviors and loss of controlled eating habits are major contributors to weight regain.32,33 Furthermore, there is a growing body of literature on the importance of disordered eating and food addiction in the management of obesity and prevention of weight regain.34,35 In our study, several patients and RDs discussed using food as a “crutch” or an alternative to substance abuse.
Individualized weight treatment plans and improved behavior maintenance skills may help improve adherence to recommended behavioral changes after surgery. In 2016, our group conducted a 16-week behavioral intervention involving video and telephone visits focused on behavior maintenance skills after bariatric surgery. Patients in the intervention arm gained less weight and adhered to a healthier diet.36 Dissemination and implementation of this type of postbariatric surgery behavioral program may help provide patients the long-term dietary support they need.
Our study has several limitations. First, some barriers faced by our study participants may not be applicable to patients outside the VHA. Veterans are more likely to have a higher comorbidity burden, be more socioeconomically disadvantaged, and have higher rates of mental illness and substance abuse compared to non-Veterans.37,38 Second, our interviews may not reflect patient and provider sentiments in other regions of the country as the patients, PCPs, RDs, and health psychologists are from the Midwest. Furthermore, males comprised the majority of our patient participants, so our findings may not capture differing perceptions of barriers among genders. Third, our interview guides did not address all the individual determinants within Andersen’s Behavioral Model of Health Services as some determinants (e.g., genetics) were not conducive to interviews. Alternative research designs are needed to analyze the contribution of these other determinants. Fourth, the themes identified during the coding process could have been biased since most transcripts were coded individually and reflected the perspectives of coders who were white. We attempted to minimize bias in the coding process by coding the initial 10% of transcripts and identifying broader themes with contributions from the entire study team. Finally, recall bias may have impacted our results, although multiple participant groups expressed each of the identified themes.
In conclusion, low bariatric surgery utilization is influenced by patients’ fear of surgery and change, along with hesitation regarding the need for bariatric surgery and incorporation of the recommended lifestyle changes. Providers should address these factors when educating and referring patients who are candidates for bariatric surgery. Behavioral interventions are needed to optimize longitudinal, multidisciplinary programmatic support as patients change their personal health practices.
Supplementary Material
Supplemental Digital Content 1: Consolidated criteria for reporting qualitative studies (COREQ): 32-item checklist.
Supplemental Digital Content 2: Provider Interview Guide.
Supplemental Digital Content 3: Patient Interview Guides.
Supplemental Digital Content 4: Bariatric surgery qualitative analysis codes.
Highlights.
Patients and providers identified 6 individual-level barriers to bariatric surgery
Surgery was feared and felt to be an extreme measure to address obesity
Patients feared change and committing to a new diet for rest of life
Fear of judgement & unstable support networks influenced decision to pursue surgery
Education and longitudinal support are needed to address the barriers
ACKNOWLEDGEMENTS
Sources of Funding:
Effort on this study and manuscript was made possible by an American College of Surgeons George H.A. Clowes Memorial Research Career Development Award and a VA HSR&D Career Development Award to Dr. Funk (CDA 015-060), as well as a VA Research Career Scientist award to Dr. Voils (RCS 14-443). Further funding was through the NIH Metabolism and Nutrition Training Program T32 (DK007665) to Dr. Murtha. The views represented in this study represent those of the authors and not those of the Department of Veterans Affairs or the U.S. Government. The authors declare no conflicts of interest related to these funding sources.
Conflict of Interest
Effort on this study and manuscript was made possible by an American College of Surgeons George H.A. Clowes Memorial Research Career Development Award and a VA HSR&D Career Development Award to Dr. Funk (CDA 015-060), as well as a VA Research Career Scientist award to Dr. Voils (RCS 14-443). The views represented in this study represent those of the authors and not those of the Department of Veterans Affairs or the U.S. Government. Further funding was through the NIH Metabolism and Nutrition Training Program T32 (DK007665).The authors declare no conflicts of interest related to these funding sources.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Campos GM, Khoraki J, Browning MG, Pessoa BM, Mazzini GS, Wolfe L. Changes in Utilization of Bariatric Surgery in the United States From 1993 to 2016. Ann Surg. 2020;271(2):201–209. 10.1097/sla.0000000000003554 [DOI] [PubMed] [Google Scholar]
- 2.Chang S-H, Stoll CRT, Song J, Varela JE, Eagon CJ, Colditz GA. The Effectiveness and Risks of Bariatric Surgery. JAMA Surg. 2014;149(3):275. 10.1001/jamasurg.2013.3654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet. 2015;386(9997):964–973. 10.1016/s0140-6736(15)00075-6 [DOI] [PubMed] [Google Scholar]
- 4.Arterburn DE, Telem DA, Kushner RF, Courcoulas AP. Benefits and Risks of Bariatric Surgery in Adults. JAMA. 2020;324(9):879. 10.1001/jama.2020.12567 [DOI] [PubMed] [Google Scholar]
- 5.Coleman KJ, Fischer H, Arterburn DE, et al. Effectiveness of Gastric Bypass Versus Gastric Sleeve for Cardiovascular Disease: Protocol and Baseline Results for a Comparative Effectiveness Study. JMIR Res Protoc. 2020;9(4):e14936. 10.2196/14936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jenkins PC, Oerline MK, Mullard AJ, Englesbe MJ, Campbell DA, Hemmila MR. Hospital variation in outcomes following appendectomy in a regional quality improvement program. Am J Surg. 2016;212(5):857–862. 10.1016/j.amjsurg.2016.02.011 [DOI] [PubMed] [Google Scholar]
- 7.Maciejewski ML, Arterburn DE, Berkowitz TSZ, et al. Geographic Variation in Obesity, Behavioral Treatment, and Bariatric Surgery for Veterans. Obesity. 2019;27(1):161–165. 10.1002/oby.22350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Funk LM, Alagoz E, Jolles SA, et al. A Qualitative Study of the System-level Barriers to Bariatric Surgery Within the Veterans Health Administration. Ann Surg. 2020. 10.1097/sla.0000000000003982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fung M, Wharton S, Macpherson A, Kuk JL. Receptivity to Bariatric Surgery in Qualified Patients. J Obes. 2016;2016:1–6. 10.1155/2016/5372190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wharton S, Serodio KJ, Kuk JL, Sivapalan N, Craik A, Aarts MA. Interest, views and perceived barriers to bariatric surgery in patients with morbid obesity. Clin Obes. 2016;6(2):154–160. 10.1111/cob.12131 [DOI] [PubMed] [Google Scholar]
- 11.Afonso BB, Rosenthal R, Li KM, Zapatier J, Szomstein S. Perceived barriers to bariatric surgery among morbidly obese patients. Surg Obes Relat Dis. 2010;6(1):16–21. 10.1016/j.soard.2009.07.006 [DOI] [PubMed] [Google Scholar]
- 12.Iuzzolino E, Kim Y. Barriers impacting an individuals decision to undergo bariatric surgery: A systematic review. Obes Res Clin Pract. 2020;14(4):310–320. 10.1016/j.orcp.2020.07.001 [DOI] [PubMed] [Google Scholar]
- 13.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. 10.1056/NEJMoa012512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.QSR International (1999) NVivo Qualitative Data Analysis Software [computer program]. Version 12. [Google Scholar]
- 15.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 16.Charmaz K Constructing Grounded Theory: a practical guide through qualitative analysis. London: SAGE Publications; 2006. [Google Scholar]
- 17.Miles M, Huberman AM. Qualitative Data Analysis: an expanded sourcebook. 1994. Published Second Edition. [Google Scholar]
- 18.Imbus JR, Voils CI, Funk LM. Bariatric surgery barriers: a review using Andersen’s Model of Health Services Use. Surg Obes Relat Dis. 2018;14(3):404–412. 10.1016/j.soard.2017.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Babitsch B, Gohl D, von Lengerke T. Re-revisiting Andersen’s Behavioral Model of Health Services Use: a systematic review of studies from 1998–2011. Psychosoc Med. 2012;9:Doc11. 10.3205/psm000089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roberson DW, Neil JA, Pories ML, Rose MA. Tipping point: factors influencing a patient’s decision to proceed with bariatric surgery. Surg Obes Relat Dis. 2016;12(5):1086–1090. 10.1016/j.soard.2016.01.009 [DOI] [PubMed] [Google Scholar]
- 21.Wysoker A The Lived Experience of Choosing Bariatric Surgery to Lose Weight. J Am Psychiatr Nurses Assoc. 2005;11(1):26–34. 10.1177/1078390305275005 [DOI] [Google Scholar]
- 22.Wee CC, Hamel MB, Apovian CM, et al. Expectations for Weight Loss and Willingness to Accept Risk Among Patients Seeking Weight Loss Surgery. JAMA Surg. 2013;148(3):264. 10.1001/jamasurg.2013.1048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wee CC, Huskey KW, Bolcic-Jankovic D, Colten ME, Davis RB, Hamel M. Sex, Race, and Consideration of Bariatric Surgery Among Primary Care Patients with Moderate to Severe Obesity. J Gen Intern Med. 2014;29(1):68–75. 10.1007/s11606-013-2603-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnson F, Beeken RJ, Croker H, Wardle J. Do weight perceptions among obese adults in Great Britain match clinical definitions? Analysis of cross-sectional surveys from 2007 and 2012. BMJ Open. 2014;4(11):e005561. 10.1136/bmjopen-2014-005561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Livhits M, Mercado C, Yermilov I, et al. Preoperative predictors of weight loss following bariatric surgery: systematic review. Obes Surg. 2012;22(1):70–89. 10.1007/s11695-011-0472-4 [DOI] [PubMed] [Google Scholar]
- 26.Karmali S, Brar B, Shi X, Sharma AM, De Gara C, Birch DW. Weight recidivism postbariatric surgery: a systematic review. Obes Surg. 2013;23(11):1922–1933. 10.1007/s11695-013-1070-4 [DOI] [PubMed] [Google Scholar]
- 27.Kaly P, Orellana S, Torrella T, Takagishi C, Saff-Koche L, Murr MM. Unrealistic weight loss expectations in candidates for bariatric surgery. Surg Obes Relat Dis. 2008;4(1):610. 10.1016/j.soard.2007.10.012 [DOI] [PubMed] [Google Scholar]
- 28.Baldwin AS, Rothman AJ, Jeffery RW. Satisfaction with Weight Loss: Examining the Longitudinal Covariation Between People’s Weight-loss-related Outcomes and Experiences and Their Satisfaction. Ann Behav Med. 2009;38(3):213–224. 10.1007/s12160-009-9148-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rothman AJ. Toward a theory-based analysis of behavioral maintenance. Health Psychol. 2000;19(1s):64–69. 10.1037/0278-6133.19.suppl1.64 [DOI] [PubMed] [Google Scholar]
- 30.Varban OA, Bonham AJ, Stricklen AL, et al. Am I on Track? Evaluating Patient-Specific Weight Loss After Bariatric Surgery Using an Outcomes Calculator. Obes Surg. 2021. 10.1007/s11695-021-05397-8 [DOI] [PubMed] [Google Scholar]
- 31.Elkins G, Whitfield P, Marcus J, Symmonds R, Rodriguez J, Cook T. Noncompliance with Behavioral Recommendations Following Bariatric Surgery. Obes Surg. 2005;15(4):546–551. 10.1381/0960892053723385 [DOI] [PubMed] [Google Scholar]
- 32.Colles SL, Dixon JB, O’Brien PE. Grazing and loss of control related to eating: two highrisk factors following bariatric surgery. Obesity (Silver Spring). 2008;16(3):615–622. 10.1038/oby.2007.101 [DOI] [PubMed] [Google Scholar]
- 33.Freire RH, Borges MC, Alvarez-Leite JI, Toulson Davisson Correia MI. Food quality, physical activity, and nutritional follow-up as determinant of weight regain after Rouxen-Y gastric bypass. Nutrition. 2012;28(1):53–58. 10.1016/j.nut.2011.01.011 [DOI] [PubMed] [Google Scholar]
- 34.Hebebrand J, Albayrak Ö, Adan R, et al. “Eating addiction”, rather than “food addiction”, better captures addictive-like eating behavior. Neurosci Biobehav Rev. 2014;47:295–306. 10.1016/j.neubiorev.2014.08.016 [DOI] [PubMed] [Google Scholar]
- 35.Subramaniam K, Low WY, Lau PC, et al. Eating Behaviour Predicts Weight Loss Six Months after Bariatric Surgery: A Longitudinal Study. Nutrients. 2018;10(11). 10.3390/nu10111616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Voils CI, Adler R, Strawbridge E, et al. Early-phase study of a telephone-based intervention to reduce weight regain among bariatric surgery patients. Health Psychol. 2020;39(5):391–402. 10.1037/hea0000835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McCance-Katz E 2018 National Survey on Drug Use and Health: Veterans. In: Services USDoHaH, ed2018. [Google Scholar]
- 38.Rogers WH, Kazis LE, Miller DR, et al. Comparing the health status of VA and non-VA ambulatory patients: the veterans’ health and medical outcomes studies. J Ambul Care Manage. 2004;27(3):249–262. 10.1097/00004479-200407000-00009 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1: Consolidated criteria for reporting qualitative studies (COREQ): 32-item checklist.
Supplemental Digital Content 2: Provider Interview Guide.
Supplemental Digital Content 3: Patient Interview Guides.
Supplemental Digital Content 4: Bariatric surgery qualitative analysis codes.


