Abstract
On April 23, 2022, the Ministry of Health of the Democratic Republic of the Congo announced an EVD outbreak after discovering 2 confirmed cases and identifying 267 contacts. With collaboration from the WHO, the MoH are taking many interventions to prevent further expansion of this outbreak. Forty-six years ago, the Ebola virus was first discovered in 1976 near the Ebola River in the DRC. Since then, 13 outbreaks of EVD have occurred in the DRC and, in 2020, it witnessed the second largest EVD outbreak in the world, resulting in 3481 cases and 2299 mortalities. This article discusses the epidemiology of the current DRC outbreak by examining the etiology of EVD, the number of affected cases, and the subsequent case index. Considering these data, this paper discusses measures taken by the MoH, WHO, CDC, and UNICEF to mitigate the Ebola outbreak, such as supporting local teams to provide essential care, training medical staff, and raising awareness for vaccination. Finally, by comparing the gravity of the situation to current measures, this article provides recommendations for individuals and governments to protect themselves and mitigate future outbreaks.
Keywords: Ebola, Democratic Republic of Congo, Ebola virus, DRC, Ebola virus disease
Abbreviations
- EVD
Ebola Virus Disease
- MoH
Ministry of Health
- WHO
World Health Organization
- DRC
Democratic Republic of Congo
- IPC
Infection Prevention and Control
- CDC
Centers for Disease Control and Prevention
- RNA
Ribonucleic acid
- INRB
National Institute of Biomedical Research
- Gp:
Glycoprotein
- VP30
Viral protein 30
- EBV
Ebola virus
- UNICEF
United Nations International Children's Emergency Funds
- VHF
Viral hemorrhagic fever
1. Introduction
Ebola virus disease (EVD) is a serious, usually fatal, zoonotic disease that has spread sporadically in humans, vertebrates, and avians since its discovery in 1976 [1]. Due to increasing human contact from travel, immigration, displacement, and international trade, EVD epidemics have continued to spread and increase in the number [[2], [3], [4]]. The DRC announced its tenth outbreak on August 1, 2018. Between April 30, 2018, and November 17, 2019, 3296 cases and 2196 mortalities were reported among the five most affected areas, those being (1) Benin with 697 cases, (2) Katwa with 674, (3) Mabalako with 416, (4) Butembo with 288, and (5) Mandima with 344 [5,6]. This outbreak has become the second-largest EVD outbreak documented as it only follows the 2014–2016 West African outbreak, which resulted in 28 600 cases and 11 325 deaths. Consequently, since August 2018, the DRC Ministry of Health has collaborated with other parties, such as the World Health Organization (WHO), to contain future outbreaks and limit the risk of transmission throughout the country [6]. Despite these attempts, the Congolese Ministry of Health (MoH) declared its most recent EVD outbreak on April 23, 2022 after a 31-year-old male from Mbandaka began exhibiting symptoms of EVD [7].
2. Epidemiology and outbreak of Ebola virus in the Democratic Republic of Congo(DRC)
According to the WHO, the cumulative number of EVD cases since 1976 is over 34 710 worldwide. Although early supportive treatment with hydration and symptomatic relieving medication improves survival, fatality rates inconsistently vary from 25 to 90%, with an average of around 50% [8].
EBV is transmitted to humans via wild animals, particularly fruit bats, which are considered the natural host for EBV. From this, human to human transmission occurs through direct contact with blood, bodily secretions, and sharing of materials and surfaces (e.g. clothes, beds). Consequently, a high rate of infection is seen among health care workers due to their close contact with infected patients. Contacting the deceased body of an infected patient during funerals also contributes to the transmission of the disease, complicating its spread further [8].
As of May 2022, the DRC has encountered 13 outbreaks. Prior to the current 2022 outbreak, the most recent one began on October 8, 2021 and was officially declared over by the Ministry of Health on December 16, 2021. Among the eleven reported cases of EVD, six resulted in death, leading to a mortality rate of 55% [9,10]. The index case seems to be a three-year-old male presenting with a fever, physical weakness, loss of appetite, abdominal pain, difficulty breathing, dark stool, and blood in vomitus. EVD was confirmed by PCR test from the Rodolphe Mérieux INRB Laboratory, though the patient died on the same day. A father and his two children, who were neighbors to the index case, followed in symptoms and death [11]. Assuming that the index case may not have actually been the first infected individual, the CDC postulates that this outbreak could have resulted from a persistent infection in a previously infected patient during the 2018 outbreak, either due to transmission or disease relapse [11].
3. Etiology of Ebola virus infection
Ebola virus belongs to the Filoviridae family, which comprises three genera: Ebolavirus, Marburgvirus, and Cuevavirus [12]. This virus is a non-segmented, negative-stranded RNA virus, hence, it encodes a non-proofreading RNA-dependent RNA polymerase [12]. Therefore, the absence of proofreading predisposes EBV to higher frequencies of genetic mutations, thus promoting adaptability and expansion of the virus [13].
The three genera of EBV encompass five species, each concurring a degree of virulence that reflects its severity and fatality, those being (1) Taï Forest EBV, (2) Reston EBV, (3) Sudan EBV, (4) Bundibugyo EBV, and (5) Zaire EBV [14]. Among these five species, Zaire ebolavirus (EBOV) is classified as the most virulent type due to its lethality and degree of replication inside human cells [14,15].
Expanding on previously discussed methods of transmission, studies have shown that infection could specifically occur from direct contact with the bodily fluids of asymptomatic individual. This involves blood, urine, faeces, vomitus, saliva, sweat, breastmilk, and potentially semen [16,17]. Other transmission pathways also involve skin abrasions, contact with fomites, and inhalation of droplets, though airborne transmission seems to be much less likely [17,18]. Infection can also occur zoonotically, either through eating the meat of a carrier primate or being exposed to their bodily fluids [17]. Similarly, genetic sequencing has proven that the April 2022 outbreak seems to be due to a recent zoonotic spill-over event, as confirmed by the National Institute of Biomedical Research [19].
After infection, the incubation of EBV varies depending on the transmission method but usually lies between 2 and 21 days [16]. On average, symptoms arise after 8–10 days, though this time is sometimes shorter with blood-borne transmission [16,20]. The viral mechanism of invasion is complex but mainly targets phagocytes, such as dendritic cells and macrophages. Replication inside host cells is initiated by the attachment of Gp spikes, followed by binding of the transcriptional activator VP30 and, therefore, the start of viral transcription [21,20]. This inactivates the innate, adaptive, and intrinsic immune response, causing immune-mediated cell damage to organs such as the lungs, heart, kidney, liver, and gastrointestinal tract [18].
Initial symptoms of the disease typically present as flu-like symptoms, fever, myalgia, general malaise, vomiting, and diarrhea, with more severe symptoms including conjunctival hemorrhage and encephalopathy [20,22]. As dissemination of the virus progresses, cytokine storms emerge and, consequently exacerbate patient situations through bleeding, hypotension, and coagulation disorders [23].
4. Current efforts to mitigate Ebola virus in the Democratic Republic of Congo(DRC)
Ever since the emergence of Ebola's largest DRC outbreak in 2018, several international partners like the WHO, Center for Disease Control and Prevention (CDC), and United Nations International Children's Emergency Fund (UNICEF) have worked closely with the Congolese Government to curb the Ebola outbreak—having now been classified as a Public Health Emergency of International Concern [24].
The MoH and WHO have introduced measures of control to prevent the further spread of EBV. For instance, they have sent local teams to provide essential care to high-risk individuals who have come into contact with Ebola patients. Robust epidemiological analysis, active monitoring, and strengthening of the infection prevention and control (IPC) capacities were other health measures taken to reduce the impact of the outbreak. In addition, various multidisciplinary management measures, like providing psychological support to affected patients and raising awareness about Ebola prevention through the media, are also being promoted [25].
Additionally, the CDC has provided operational support and technical assistance in case investigation, border health, data management, vaccination, community engagement, and social mobilization. They have also made long term disease prevention strategies and capacity-building investments in the DRC by establishing permanent offices and national viral hemorrhagic fever (VHF) surveillance programs. Consequently, these programs have led to prompt identification and early isolation of suspected patients. Standardized IPC packages — including training sessions, technical support, and standard operating systems — have been developed to mitigate healthcare risks. The CDC and Red Cross have also supported local health authorities by assessing feedback from Ebola-affected communities [24].
Similarly, UNICEF has responded to the outbreak by assisting affected children and families. They have also worked with several religious leaders, psychosocial workers, and Ebola survivors to understand local fears and encourage health measures that are socio-culturally acceptable. Using these experiences, UNICEF has helped set up child care centers, hand washing units in schools, and distribute essential medical supplies — like thermometers and chlorine — to sterilize water to curb the spread [[26], [27], [28]].
A remarkable health response was also witnessed due to vaccination, infection prevention, and passive surveillance by frontline workers. Around 300 000 people have received Merck's rVSV-ZEBOV vaccine, and results have indicated efficacy of 97.5%. As a result, the vaccine has been licensed by four African nations, including the DRC, to prevent and diminish the spread of EBV [29].
5. Conclusion and recommendations
Since 1976, EBV outbreaks have taken a considerable toll on healthcare systems and yielded high mortality rates.
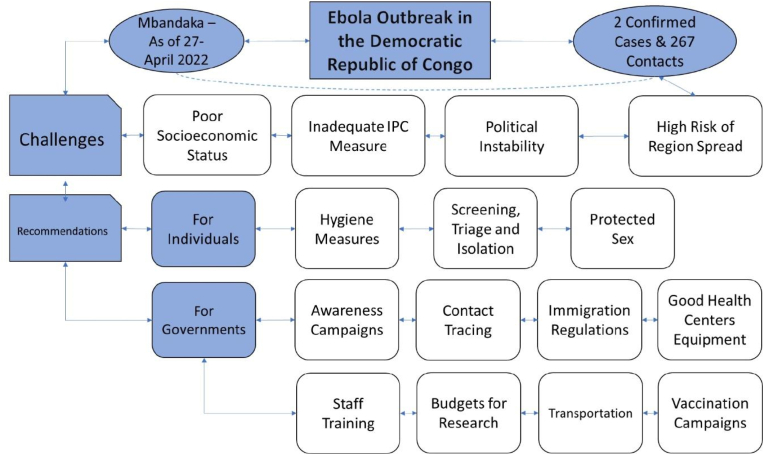
Due to the high risk of transmission from direct and indirect contact with infected persons through their bodily fluids and items, EBV has become dangerous and difficult to contain. Due to alarming rates of infection in the DRC, the WHO and the Congolese government have taken countless measures to control future outbreaks, such as contact tracing, strengthening infection prevention and control capacities, and raising awareness on protection and vaccination. Similarly, the CDC has provided technical assistance in case investigation and management; UNICEF has also assisted with establishing childcare centers for youth affected by Ebola. However, due to inadequate measures of IPC, poor economic status in the country, and political instability, the rate at which EBV spreads continues to accelerate. Therefore, in response to the continued spread of EBV outbreaks in the DRC and beyond, many measures could be adopted by governments and individuals to prevent further infections.
5.1. For individuals
Frequent handwashing with soap and clean water is essential. Individuals should avoid contact with infected persons' blood and bodily fluids (e.g. semen and saliva) until they recover from and test negative for EBV. Bodies of people who have died from Ebola should not be touched unless precautions and proper protocol are taken. Additionally, people should also avoid sharing materials and surfaces, such as clothes and needles, with others. The consumption of bushmeat (e.g., gorillas, chimpanzees) should also be avoided, and travel to countries with Ebola outbreaks should not be pursued, unless in urgent cases where vaccinations and precautions are taken.
Any person showing signs of infection should be referred for screening, triage, and isolation. Adhering to the most recent WHO recommendations, men who have survived EVD should practice safe sex for one year after exhibiting symptoms or until the semen tests negative for EBV twice [30].
5.2. For governments
Because vaccinations were able to contain the Ebola outbreak in Guinea in 2021, spreading awareness through vaccination campaigns could successfully prevent outbreaks in other areas. Additionally, authorities could temporarily impose immigration regulations on individuals from high-risk countries, as doing so would prevent the international spread of EBV. At the same time, countries should create fixed budgets and invest more in the development of healthcare facilities and research into vaccine treatments for infectious diseases. It is also crucial to ensure access to pure water, provide ample public spaces to avoid crowding, improve ways of transportation and communication, and introduce telemedicine to the healthcare system. Although these areas of improvement may be difficult to achieve for rural countries, efforts to overcome these encounters can reach cost-effective enhancement for disease diagnosis, treatment, and vaccination. Furthermore, health centers need to be equipped with more personal protective equipment, hygienic products, PCR kits, and medical supplies like masks and syringes. We also suggest training healthcare workers on EBV symptoms, detecting, and treating infected people (Fig. 1).
Fig. 1.
A summary of challenges and recommendations for containment of Ebola virus outbreak in the Democratic Republic of Congo. (Figure 1. was drawn and analyzed by authors Hadi Kassem1,5 and Olivier Uwishema1,3,4∗)
The MoH should also work to identify all contact activities of the two confirmed cases in the current outbreak; to date, 267 contact persons have been identified, though more are to be discovered.
More laboratories should be established in Mbandaka, as this will facilitate case identification and contact tracing. Furthermore, the WHO should facilitate the shipping of Ervebo vaccines to Mbandaka as ring vaccination has already started on April 27 in the province [30]. Moreover, 20 courses of monoclonal antibodies were received in this area against Ebola, and more courses should be continued for patients at high risk [30]. Working on initiation and maintenance of IPC by training health care workers supporting health centers and rehabilitation of the water resources are essential measures to prevent further spread of infection.
Additionally, the CDC should be prepared to employ epidemiologists, infectious diseases specialists, and ICU-trained nurses to help in outbreak response efforts [[31], [32], [33]]. Neighboring provinces should also be on alert to detect any cases spreading to their territories through border screenings and temperature monitoring in public areas [31].
In conclusion, public health systems should be made ready to contain future EBV outbreaks by applying many measures on both individual and governmental basis.
Ethics approval
Not Applicable.
Funding
We have not received any financial support for this manuscript.
Authors’ contribution
Olivier Uwishema: Conceptualization, Project administration, Writing-review and Designing, All authors: Data collection and Assembly, Olivier Uwishema: Reviewed and edited the first draft, Jeffrey Sun: Reviewed and edited the second draft, Olivier Uwishema: Reviewed and edited the third draft, Helen Onyeaka: Reviewed and edited the final draft, Jeffrey Sun: Reviewed and edited the final draft, Helen Onyeaka: Supervision, Manuscript writing: All authors Final approval of manuscript: All authors.
Conflicts of interest
No conflicts of interest declared.
Acknowledgement
None.
Financial support
None.
Data availability statement
Not Applicable.
Consent for publication
Not Applicable.
All co-authors approved the final manuscript.
All co-authors have read and approved the submission.
Provenance and peer review
Not commissioned, externally peer reviewed.
Ethical approval
Not Applicable.
Please state any sources of funding for your research
None.
Please state any conflicts of interest
No conflicts of interest declared.
Registration of research studies
Name of the registry: Not Applicable
Unique Identifying number or registration ID: Not Applicable
Hyperlink to your specific registration (must be publicly accessible and will be checked): Not Applicable
Consent
Not Applicable.
Guarantor
Not Applicable.
Contributor Information
Jeffrey Sun, Email: sun72@mcmaster.ca.
Olivier Uwishema, Email: uwolivier1@ktu.edu.tr.
Hadi Kassem, Email: Hadi.station@hotmail.com.
Mortada Abbass, Email: abbassmortada7@gmail.com.
Lama Uweis, Email: Uweis.lama@gmail.com.
Anushree Rai, Email: iamanushree99@gmail.com.
Rayyan El Saleh, Email: rayyan-elsaleh@hotmail.com.
Irem Adanur, Email: iremadanur@gmail.com.
Helen Onyeaka, Email: h.onyeaka@bham.ac.uk.
References
- 1.Passi D., Sharma S., Dutta S.R., Dudeja P., Sharma V. Ebola virus disease (the killer virus): another threat to humans and bioterrorism: brief review and recent updates. J. Clin. Diagn. Res. 2015;9:LE01. doi: 10.7860/JCDR/2015/13062.6100. –LE08. [Google Scholar] [CrossRef] [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aceng J.R., Ario A.R., Muruta A.N., Makumbi I., Nanyuja M., Komakech I., Bakainaga A.N., Talisuna A.O., Mwesigye C., Mpairwe A.M., et al. Uganda's experience in Ebola virus disease outbreak preparedness. Glob. Health. 2020;16:24. doi: 10.1186/s12992-020-00548-5. 2018–2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lesmanawati D.A.S., Veenstra P., Moa A., Adam D.C., Raina C., MacIntyre R. A rapid risk analysis tool to prioritize response to infectious disease outbreak. BMJ Glob. Health. 2020;5 doi: 10.1136/bmjgh-2020-002327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chippaux J.P. Outbreaks of Ebola virus disease in Africa: the beginnings of the tragic saga. J. Venom. Anim. Toxins Incl. Trop. Dis. 2014;20:44. doi: 10.1186/1678-9199-20-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maganga G.D., Kapetshi J., Berthet N., Kebela Ilunga B., Kabange F., Mbala Kingebeni P., Mondonge V., Muyembe J.J., Bertherat E., Briand S., Cabore J., Epelboin A., Formenty P., Kobinger G., González-Angulo L., Labouba I., Manuguerra J.C., Okwo-Bele J.M., Dye C., Leroy E.M. Ebola virus disease in the democratic Republic of Congo. N. Engl. J. Med. 2014;371(22):2083–2091. doi: 10.1056/NEJMoa1411099. [DOI] [PubMed] [Google Scholar]
- 6.Aruna A., Mbala P., Minikulu L., Mukadi D., Bulemfu D., Edidi F., Bulabula J., Tshapenda G., Nsio J., Kitenge R., Mbuyi G., Mwanzembe C., Kombe J., Lubula L., Shako J.C., Mossoko M., Mulangu F., Mutombo A., Sana E., Tutu Y. Vol. 68. 2019. Ebola Virus Disease Outbreak - Democratic Republic of the Congo, August 2018-November 2019. MMWR. Morbidity and mortality weekly report; pp. 1162–1165. CDC ebola response. 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. (n.d.). Ebola Virus Disease – Democratic Republic of the Congo. World Health Organization. Retrieved May 2, 2022, from https://www.who.int/emergencies/disease-outbreak- news/item/ebola-virus-disease-democratic-republic-of-the-congo_1.
- 8.World Health Organization . February 23rd 2021. Ebola Virus Disease.https://www.who.int/news-room/fact-sheets/detail/ebola-virus-disease Accessed on the 28th of April 2022. [Google Scholar]
- 9.World Health Organization, Democratic Republic of Congo Declares Ebola Outbreak over, December 16th 2021. https://www.afro.who.int/news/democratic-republic-congo-declares-ebola-outbreak-over.
- 10.Centers for Disease Control and Prevention . February 22nd 2021. History of Ebola Virus Disease Outbreaks.https://www.cdc.gov/vhf/ebola/history/chronology.html [Google Scholar]
- 11.World Health Organization . October 10th 2021. Ebola Virus Disease- Democratic Republic of the Congo.https://www.who.int/emergencies/disease-outbreak-news/item/ebola-virus-disease-democratic-republic-of-the-congo_1 [Google Scholar]
- 12.Khadka S., Williams C.G., Sweeney-Gibbons J., Basler C.F. Marburg and ebola virus mRNA 3' Untranslated regions contain negative regulators of translation that are modulated by ADAR1 editing. J. Virol. 2021;95(19) doi: 10.1128/JVI.00652-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Whitfield Z.J., Prasad A.N., Ronk A.J., Kuzmin I.V., Ilinykh P.A., Andino R., Bukreyev A. Species-specific evolution of ebola virus during replication in human and bat cells. Cell Rep. 2020;32(7) doi: 10.1016/j.celrep.2020.108028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baseler L., Chertow D.S., Johnson K.M., Feldmann H., Morens D.M. The pathogenesis of ebola virus disease. Ann. Rev. Pathol. 2017;12:387–418. doi: 10.1146/annurev-pathol-052016-100506. [DOI] [PubMed] [Google Scholar]
- 15.Jacob S.T., Crozier I., Fischer W.A., 2nd, Hewlett A., Kraft C.S., Vega M.A., Soka M.J., Wahl V., Griffiths A., Bollinger L., Kuhn J.H. Ebola virus disease. Nat. Rev. Dis. Prim. 2020;6(1):13. doi: 10.1038/s41572-020-0147-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kourtis A.P., Appelgren K., Chevalier M.S., McElroy A. Ebola virus disease: focus on children. Pediatr. Infect. Dis. J. 2015;34(8):893–897. doi: 10.1097/INF.0000000000000707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Judson S., Prescott J., Munster V. Understanding ebola virus transmission. Viruses. 2015;7(2):511–521. doi: 10.3390/v7020511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel P.R., Su Shah. StatPearls Publishing; 2022 Jan. Ebola Virus.https://www.ncbi.nlm.nih.gov/books/NBK560579/ [Updated 2022 Feb 13]. In: StatPearls [Internet]. Treasure Island (FL) Available from. [Google Scholar]
- 19.World Health Organization Disease outbreak news; ebola virus disease- Democratic Republic of the Congo. 27 April 2022. https://www.who.int/emergencies/disease-outbreak-news/item/2022- DON377 Available at:
- 20.Zawilińska B., Kosz-Vnenchak M. General introduction into the Ebola virus biology and disease. Folia Med. Cracov. 2014;54(3):57–65. [PubMed] [Google Scholar]
- 21.Zhu W., Banadyga L., Emeterio K., Wong G., Qiu X. The roles of ebola virus soluble glycoprotein in replication, pathogenesis, and countermeasure development. Viruses. 2019;11(11):999. doi: 10.3390/v11110999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Olukitibi T.A., Ao Z., Mahmoudi M., Kobinger G.A., Yao X. Dendritic cells/Macrophages-Targeting feature of ebola glycoprotein and its potential as immunological facilitator for antiviral vaccine approach. Microorganisms. 2019;7(10):402. doi: 10.3390/microorganisms7100402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marcinkiewicz J., Bryniarski K., Nazimek K. Ebola haemorrhagic fever virus: pathogenesis, immune responses, potential prevention. Folia Med. Cracov. 2014;54(3):39–48. [PubMed] [Google Scholar]
- 24.Centre for Disease Control and Prevention . June 19, 2019. Viral Hemorrhagic Fevers, Ebola Virus Disease, Outbreaks, 2018 Eastern Democratic Republic of the Congo.https://www.cdc.gov/vhf/ebola/outbreaks/drc/what-cdc-is-doing.html [Google Scholar]
- 25.World Health Organization, Disease Outbreak News, Ebola virus disease - Democratic Republic of the Congo, December 16, 2021 https://www.who.int/emergencies/disease-outbreak-news/item/2021-DON351.
- 26.United Nations International Children's Emergency Funds, Eastern and South Africa, Ebola Preparedness and Response, Focus Countries: Uganda, South Sudan, Rwanda & Burundi https://www.unicef.org/esa/ebola-preparedness-and-response.
- 27.Uwishema O., Okereke M., Onyeaka H., Hasan M.M., Donatus D., Martin Z., Oluwatomisin L.A., Mhanna M., Olumide A.O., Sun J., Adanur I. Threats and outbreaks of cholera in Africa amidst COVID-19 pandemic: a double burden on Africa's health systems. Trop. Med. Health. 2021;49(1):93. doi: 10.1186/s41182-021-00376-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Uwishema O., Taylor C., Lawal L., Hamiidah N., Robert I., Nasir A., Chalhoub E., Sun J., Akin B.T., Adanur I., Mwazighe R.M., Onyeaka H. The syndemic burden of HIV/AIDS in Africa amidst the COVID-19 pandemic. Immun. Inflamm. Dis. 2022;10(1):26–32. doi: 10.1002/iid3.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Khan F.M.A., Hasan M.M., Kazmi Z., et al. Ebola and COVID-19 in Democratic Republic of Congo: grappling with two plagues at once. Trop. Med. Health. 2021;49:67. doi: 10.1186/s41182-021-00356-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Health Organization Disease outbreak news; ebola virus disease- Democratic Republic of the Congo. 27 April 2022. https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON377 Available at:
- 31.The Democratic Republic of Congo Declared Ebola Virus Disease (EVD) Outbreak in Mbandaka, Equateur Province. Africa CDC. 2022, April 25. https://africacdc.org/news-item/the-democratic-republic-of-congo-declared-ebola-virus-disease-evd-outbreak-in-mbandaka-equateur-province/ Retrieved May 2, 2022, from. [Google Scholar]
- 32.Uwishema O., Alshareif B., Yousif M., Omer M., Sablay A., Tariq R., Zahabioun A., Mwazighe R.M., Onyeaka H. Lassa fever amidst the COVID-19 pandemic in Africa: A rising concern, efforts, challenges, and future recommendations. J. Med. Virol. 2021;93(12):6433–6436. doi: 10.1002/jmv.27219. [DOI] [PubMed] [Google Scholar]
- 33.Uwishema O., Nnagha E.M., Chalhoub E., Nchasi G., Mwazighe R.M., Akin B.T., Adanur I., Onyeaka H. 11th. Vol. 93. J. Med. Virol.; 2021. Dengue fever outbreak in Cook Island: A rising concern, efforts, challenges, and future recommendations; pp. 6073–6076. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not Applicable.