Abstract
Background:
It remains unclear if young overhead athletes with isolated superior labrum anterior-posterior (SLAP) type 2 lesions benefit more from SLAP repair or subpectoral biceps tenodesis.
Purpose:
To evaluate clinical outcomes and return to sport in overhead athletes with symptomatic SLAP type 2 lesions who underwent either biceps tenodesis or SLAP repair.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A retrospective analysis of prospectively collected data was performed in patients who underwent subpectoral biceps tenodesis (n = 14) or SLAP repair (n = 24) for the treatment of isolated type 2 SLAP lesions. All patients were aged <35 years at time of surgery, participated in overhead sports, and were at least 2 years out from surgery. Clinical outcomes were assessed with the American Shoulder and Elbow Surgeons (ASES) score; Single Assessment Numerical Evaluation (SANE) score; Quick Disabilities of the Arm, Shoulder, and Hand (QuickDASH) score; and the 12-Item Short Form (SF-12) physical component score. Return to sport and patient satisfaction were documented. Clinical failures requiring revision surgery and complications were reported.
Results:
Preoperative baseline scores in both the tenodesis and SLAP repair groups were similar. There were no significant differences between the groups on any postoperative outcome measure: For biceps tenodesis versus SLAP repair, the ASES score was 92.7 ± 10.4 versus 89.1 ± 16.7, the SANE score was 86.2 ± 13.7 versus 83.0 ± 24.1, the QuickDASH score was 10.0 ± 12.7 versus 9.0 ± 14.3, and SF-12 was 51.2 ± 7.5 versus 52.8 ± 7.7. No group difference in return-to-sports rate (85% vs 79%; P = .640) was noted. More patients in the tenodesis group (80%) reported modifying their sporting/recreational activity postoperatively because of weakness compared with patients in the SLAP repair group (15%; P = .022). One patient in each group progressed to surgery for persistent postoperative stiffness, and 1 patient in the tenodesis group had a postoperative complication related to the index surgery.
Conclusion:
Both subpectoral biceps tenodesis and SLAP repair provided excellent clinical results for the treatment of isolated SLAP type 2 lesions, with a high rate of return to overhead sports and a low failure rate, in a young and high-demanding patient cohort. More patients reported modifying their sporting/recreational activity because of weakness after subpectoral tenodesis.
Keywords: superior labrum anterior-posterior (SLAP), SLAP repair, biceps tenodesis, outcomes
Superior labrum anterior-posterior (SLAP) lesions were first described by Andrews et al 2 in 1985 and classified by Snyder and colleagues 28 in 1990. Over the last decades, more attention was paid to the SLAP region and associated lesions as a pain generator, especially in the overhead athlete.
Based on the classification of Snyder et al, 28 type 2 SLAP lesions are the most common type, characterized by fraying and detachment of the biceps anchor from the superior glenoid. In case of a symptomatic SLAP type 2 lesion and failed nonoperative management, 15 surgical treatment options mainly include SLAP repair or biceps tenodesis (or tenotomy). Controversy exists about which procedure is superior in terms of clinical outcome. Boileau et al 3 found biceps tenodesis to be superior with 80% satisfaction in patients with a mean age of 37 years (range, 19-57 years) compared with SLAP repair, with only 40% patient satisfaction for the treatment of type 2 SLAP lesions. Comparing return-to-sports rates, 87% returned to their previous sport in the tenodesis group compared with only 20% in the SLAP repair group.
While the age of patients in this study included those up to 57 years, it can be assumed that these patients had a more degenerative lesion, which may result in inferior outcomes for SLAP repair when compared with biceps tenodesis.
Schroder et al, 25 Ek et al, 12 and Chalmers et al 7 have shown that both procedures result in similar clinical outcomes when compared with each other in patients in their 30s and 40s; however, there was a significant difference in favor of biceps tenodesis, with 81% of patients treated with biceps tenodesis and 64% of patients treated with SLAP repair who returned to sport. Reoperation rates have been reported to be 7% in patients treated with biceps tenodesis and 14% in patients treated with SLAP repair, as summarized by Hurley et al 18 in a systematic review and meta-analysis. While the literature indicates that patients in their 30s and 40s benefit more from biceps tenodesis in terms of higher rates of patient satisfaction and return to sport, it is still unknown which procedure is superior in patients aged 35 years and younger. Isolated SLAP type 2 lesions are particularly observed in young overhead athletes, who rely on the stabilizing effect of the long head of the biceps tendon with limitation of anterior and superior translation during abduction and external rotation (throwing motion). 4,5,13,17 Whether equal or better results can be achieved in this age- and activity-selected patient collective with biceps anchor–preserving SLAP repair remains unknown.
The purpose of this study was therefore to analyze clinical outcomes, return-to-sport rates, and failure rates in overhead athletes aged 35 years or younger treated with SLAP repair or subpectoral biceps tenodesis for isolated SLAP type 2 lesions with a minimum follow-up of 2 years. It was hypothesized that SLAP repair in this young population would result in similar outcomes when compared with subpectoral biceps tenodesis.
Methods
Patient Selection
This study was a retrospective review of prospectively collected data for patients who underwent either arthroscopic rotator cuff–sparing SLAP repair or arthroscopic long head of the biceps tendon tenotomy with extra-articular mini-open subpectoral tenodesis between October 2005 and December 2017. Institutional review board approval was received for the study protocol.
All patients were treated by a single surgeon (P.J.M.). Patients were included in this study if they (1) showed clinical (positive O’Brien and Yergason tests) signs of an isolated type 2 SLAP lesion, (2) showed radiological signs of an isolated type 2 SLAP lesion 21 (and confirmed during surgery), (3) were at least 2 years out of surgery, (4) participated in overhead sports defined by using the upper arm and shoulder in an arc overhead, and (5) were treated with one of the aforementioned procedures. Excluded were patients with type 1, 3, or 4 SLAP lesions or with pathologies of the long head of the biceps tendon, such as tendinitis or hourglass deformity. In addition, patients who had concomitant procedures such as rotator cuff repair or anterior or posterior labral repairs were also excluded.
Surgery was indicated for persistent pain, loss of strength, and impaired function of the affected arm that did not resolve under physical therapy for at least 3 months. Both procedures were performed in the beach-chair position. The indication for either SLAP repair or subpectoral biceps tenodesis was predominantly based on the tissue quality of the superior labrum by the treating surgeon. In case the bucket-handle–type configuration of the superior aspect of the labrum impressed solid, a repair was conducted. In the presence of degenerative multiple fraying of the superior labrum, a biceps tenodesis was preferred (in case of an unstable superior labral tear, an additional SLAP repair was performed, as mentioned below). 1
Arthroscopic SLAP Repair Technique
The SLAP repair technique 10 involved first establishing standard portals and performing a thorough evaluation of the SLAP and bicipital root to classify and confirm the type of labral tear.
Before anchor placement, the upper glenoid rim between 11 and 1 o’clock was debrided both the labrum and underlying bone by the help of an oscillating shaver and bur. The first of 2 single-loaded suture anchors was placed just anterior to the biceps tendon at the 1-o’clock position (for the right shoulder) on the apex of the glenoid rim via the anterosuperolateral portal. Similarly, the placement of the second anchor at the 11-o’clock position (for the right shoulder) on the apex of the glenoid rim was performed. The repair was finalized in a knotless fashion as illustrated in Figure 1.
Figure 1.

Right shoulder: viewing via the dorsal standard portal visualizing the final repair construct of a knotless SLAP repair.
After surgery, the patient is maintained in a sling for 4 weeks. Full passive range of motion is allowed as tolerated. Biceps loading is avoided. At 4 weeks postoperatively, the patient can begin full active range of motion, and at 6 weeks, the patient can start resistance training. When the patient is pain-free and full strength is restored—typically by the 4- to 5-month mark—unrestricted return to sport is allowed.
Subpectoral Biceps Tenodesis Technique
The subpectoral biceps tenodesis technique 23 involved creating posterior and standard rotator interval midglenoid portals and performing a thorough arthroscopic evaluation of the SLAP and bicipital root to classify and confirm the type of labral tear.
Next, the long head of the biceps tendon tenotomy was performed directly at the superior labral insertion, and the SLAP region was debrided by the use of a radiofrequency ablation device. Then, the arm was positioned in 90° of abduction and 90° of elbow flexion with the volar aspect of the forearm pointed downward and parallel to the floor. An incision was made extending from approximately 1 cm superior to 2 cm inferior to the inferior border of the pectoralis major tendon in the line of the axillary crease. The biceps tendon was identified and removed throughout the incision. The tendon was whipstitched with No. 2 nonabsorbable high-strength suture (FiberWire; Arthrex) beginning 2 cm proximal to the musculotendinous junction, and the excess tendon proximal was cut to the last suture stitch. The humeral fixation point was marked and freed from soft tissue with the use of an electrocautery. A 7-mm (female patient) or 8-mm (male patient) reamer was used to create a unicortical bone tunnel for a polyether-ether-ketone (PEEK) tenodesis screw (Figure 2). The suture limbs were cut flush, and the wound was irrigated and closed in a layered fashion.
Figure 2.
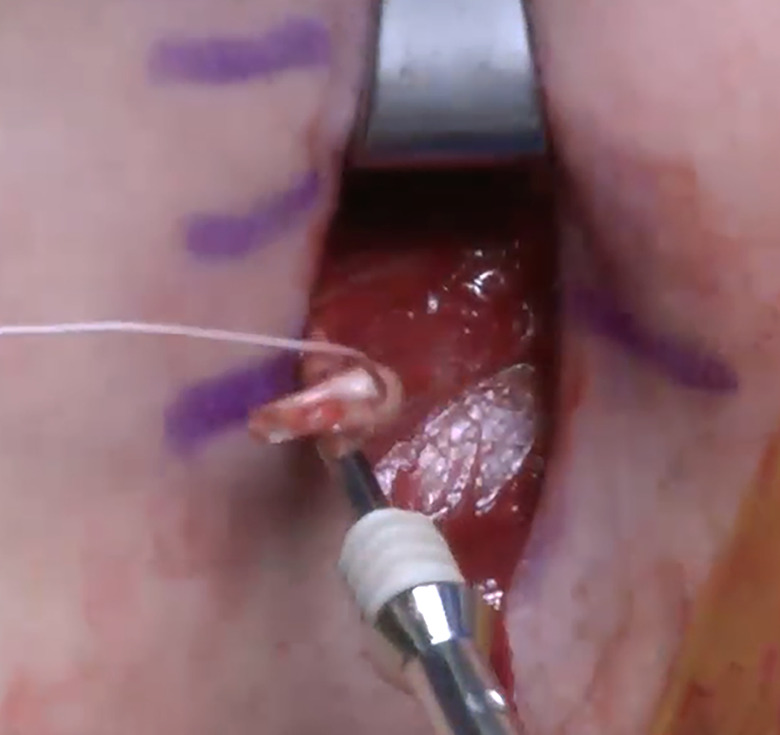
Right shoulder: view onto the axillary crease with the removed and whipstitched proximal biceps tendon placed on a tenodesis screw for later placement in a unicortical bone tunnel in the humeral shaft.
Postoperatively, sling immobilization for 2 weeks with immediate full active and passive range of motion was allowed. Patients were restricted from performing resisted elbow flexion maneuvers for at least 6 weeks after surgery. Overhead strengthening and heavy lifting were delayed for approximately 3 months.
Clinical and Functional Outcome Assessment
Preoperatively and at final follow-up, patients completed questionnaires (electronically or by paper) for the American Shoulder and Elbow Surgeons (ASES) score; Single Assessment Numerical Evaluation (SANE) score; Quick Disabilities of the Arm, Shoulder and Hand (QuickDASH) score; 12-Item Short Form (SF-12) physical component score; and patient satisfaction (on a 1-10 scale, with 10 representing “very satisfied”). Additional optional questions assessed patient participation in sports, both preoperatively and postoperatively. 22 These questions evaluated the functional ability to perform sports with the following possible answers: “unable,” “very difficult,” “somewhat difficult,” and “normal.” All answers except “unable” and “very difficult” were defined as able to return to sport. Patients were also asked to grade their sports participation level compared with their preinjury level, with “significantly below” or “cannot compete” considered as unable to return to the same level, while “moderately below” or “equal” to preinjury level were considered as successful return to sport. Questions specific to pain during sporting activity had the following possible answers: “none,” “mild,” “moderate,” or “severe.” Finally, any complications and clinical failures (defined as progressed to revision surgery) were reported.
Statistical Analysis
Continuous numerical data are presented as mean ± standard deviation, and categorical values are presented as percentages. Data were tested for normal distribution using the Kolmogorov-Smirnov test. An independent or paired t test was used for univariate analysis of normally distributed variables. For nonparametric data, Mann-Whitney tests were performed between the 2 groups. The Wilcoxon signed-rank test for the paired t test was used to compare baseline and postoperative scores. The chi-square test was used when comparing bivariates. Statistical analyses were performed with SPSS Version 11.0 (SPSS). Assuming an alpha level of 0.05 and a 2-tailed Mann-Whitney U test to compare postoperative patient-reported outcome scores, the known group sizes (n = 14 for patients who underwent biceps tenodesis with complete follow-up; n = 24 for patients who underwent SLAP repair with complete follow-up) were sufficient to detect an effect size of Cohen d = 0.99 with 80% statistical power.
Results
Patient Characteristics
Overall, 16 patients who underwent mini-open subpectoral biceps tenodesis (mean age, 28.6 years; range, 18-35 years) met the inclusion criteria, and 14 (87.5%) of these patients obtained minimum 2-year follow-up outcome scores (mean follow-up, 39.3 months; range, 24-71.9 months) (Table 1). Of those who were not included, 1 patient experienced shoulder dislocation and was treated with a Latarjet procedure before the 2-year follow-up, and 1 patient had a humeral shaft fracture at 1.2 years (classified as a postoperative complication), with 2-year data included in the analysis.
Table 1.
Summary of Patient Baseline Characteristics a
| Tenodesis Group, n = 16 | SLAP Repair Group, n = 28 | P | |
|---|---|---|---|
| Age at surgery, y, mean ± SD | 28.6 ± 6.1 | 24.4 ± 5.7 | .030 |
| Sex, female/male, n | 4/12 | 4/24 | .434 |
| Surgery on dominant arm, n (%) | 11 (68.9) | 17 (60.7) | .748 |
| Sports level at time of injury, n | .803 | ||
| High school | 1 | 1 | |
| Recreational | 9 | 18 | |
| College | 4 | 7 | |
| Professional | 2 | 2 | |
| Time from injury to surgery, mo, median (range) | 4.2 (0.5-218) | 14.9 (0.2-138) | .367 |
a Boldface P value indicates a statistically significant difference between groups (P < .05).
A total of 28 patients who underwent arthroscopic SLAP repair (mean age, 28.6 years; range, 17-35 years) met the inclusion criteria, and 24 patients (85.7%) obtained minimum 2-year follow-up outcome scores (mean follow-up, 60.8 months; range, 24-120 months) (Table 1). Of those who were not included, 2 patients experienced shoulder dislocation without 2-year follow-up, 1 after trauma and the other after seizure. One patient refused to participate, and 1 patient died before the 2-year follow-up.
All patients in both groups actively participated in overhead sports before their injury (Table 2).
Table 2.
Listing of Sports by Level of Competition a
| Tenodesis Group, n = 16 | SLAP Repair Group, n = 28 | |||||||
|---|---|---|---|---|---|---|---|---|
| HS | Rec | College | Pro | HS | Rec | College | Pro | |
| Acrobatist | 1 | |||||||
| Baseball | 3 | 2 | 1 | 4 | 1 | |||
| Basketball | 3 | |||||||
| Climber | 3 | 4 | ||||||
| Fitness/Crossfit | 2 | |||||||
| Football | 1 | 1 | 1 | 4 | 1 | |||
| Kayaking/rafting | 1 | 1 | ||||||
| Lacrosse | 1 | |||||||
| MMA | 1 | |||||||
| Softball | 1 | |||||||
| Tennis | 1 | |||||||
| Volleyball | 1 | |||||||
| Weight lifting | 1 | 2 | ||||||
| Wrestling | 1 | 1 | ||||||
| Total | 1 | 9 | 4 | 2 | 1 | 18 | 7 | 2 |
a HS, high school; MMA, mixed martial arts; Pro, professional; Rec, recreational.
Clinical Outcomes
At the time of latest follow-up, patients in both groups saw significant improvement on most outcome scores when compared with the preoperative state. Patients who underwent tenodesis improved significantly from 72.1 to 92.7 for mean ASES score (P = .001), 68.9 to 86.2 for mean SANE score (P = .034), 26.9 to 10.0 for mean QuickDASH score (P = .028), and 49.2 to 51.2 for mean SF-12 (P = .084). Patients who underwent SLAP repair improved significantly from 70.6 to 89.1 for mean ASES score (P = .001), 66.1 to 83.0 for mean SANE score (P = .012), 28.9 to 9.0 for mean QuickDASH score (P = 002), and 45.3 to 52.8 for mean SF-12 (P = .001).
When outcome scores of SLAP repair were compared with subpectoral biceps tenodesis, no significant differences between both procedures in terms of any subjective outcome score were detected (all P > .05). The results of the group comparison of postoperative outcomes are given in Table 3.
Table 3.
Comparison of Patient-Reported Outcome Scores a
| Outcome Measure | Tenodesis Group, n = 14 | SLAP Repair Group, n = 24 | P |
|---|---|---|---|
| ASES | |||
| Preoperative | 72.1 ± 14.2 (50-93) | 70.6 ± 16.5 (40-100) | |
| Postoperative | 92.7 ± 10.4 (64.9-100) | 89.1 ± 16.7 (39.9-100) | .830 |
| P | .001 | .001 | |
| SANE | |||
| Preoperative | 68.9 ± 13.3 (49-89) | 66.1 ± 20.6 (0-89) | |
| Postoperative | 86.2 ± 13.7 (64-99) | 83.0 ± 24.1 (19-100) | .678 |
| P | .034 | .012 | |
| QuickDASH | |||
| Preoperative | 26.9 ± 18.4 (0-61) | 28.9 ± 10.2 (14-45) | |
| Postoperative | 10.0 ± 12.7 (0-38.6) | 9.0 ± 14.3 (0-43.1) | .332 |
| P | .028 | .002 | |
| SF-12 PCS | |||
| Preoperative | 49.2 ± 7.0 (34.2-57.8) | 45.3 ± 7.2 (33.8-58.5) | |
| Postoperative | 51.2 ± 7.5 (33.7-57.8) | 52.8 ± 7.7 (35.0-59.2) | .172 |
| P | .084 | .001 |
a Data are reported as mean ± SD (range). Boldface P values indicate a statistically significant difference between pre- and postoperative values (P < .05). ASES, American Shoulder and Elbow Surgeons score; QuickDASH, Quick Disabilities of the Arm, Shoulder and Hand score; SANE, Single Assessment Numerical Evaluation score; SF-12 PCS, 12-Item Short Form physical component score.
Return to Sport and Patient Satisfaction
At the time of final follow-up, 19 patients (79.2%) in the SLAP repair group and 12 patients (85.7%) in the tenodesis group had returned to their previous level of sporting activity. There was no significant difference between the 2 groups with respect to participation in sports preoperatively and return to sport postoperatively (P = .64 and P > .99). More patients in the tenodesis group (80%) reported modifying their sporting/recreational activity postoperatively because of weakness compared with the SLAP repair group (15%; P = .022). The sports participation level for the tenodesis group improved from a median of 3 (range, 2-5) to 2 (range, 1-6; P = .048), and for the SLAP repair group, it improved from a median of 5 (range, 1-6) to 2 (range, 1-5; P = .004). The mean patient satisfaction with postoperative outcomes was 9 (range, 1-10) for the SLAP repair group and 10 (range 3-10) for the tenodesis group. Results of the pre- to postoperative comparison of sports participation level for both study groups are shown in Table 4.
Table 4.
Postoperative Sports Participation Level Compared With Preoperative Level a
| Preoperative Level, Median | Postoperative Level, Median | P | |
|---|---|---|---|
| Tenodesis group | |||
| Level of sports participation b | 3 (moderately below preinjury) | 2 (slightly below or equal to preinjury) | .048 |
| Competition intensity c | 4 (25%-49% of preinjury) | 2 (75%-99% of preinjury) | .072 |
| Pain with competition d | 4 (moderate pain) | 3 (mild pain) | .088 |
| Shoulder function in sporting events e | 2 (somewhat difficult) | 3 (normal) | .028 |
| Normal shoulder function throwing a ball overhead 20 yards e | 2 (somewhat difficult) | 3 (normal) | .005 |
| Pain affects recreational activity f | 2 (moderate) | 1 (mild) | .062 |
| SLAP repair group | |||
| Level of sports participation b | 5 (cannot compete in usual sport) | 2 (slightly below preinjury) | .004 |
| Competition intensity c | 5 (<25% of preinjury) | 2 (75%-99% of preinjury) | .004 |
| Pain with competition d | 5 (severe pain) | 1 (no pain) | .065 |
| Shoulder function in sporting events e | 1 (very difficult) | 3 (normal) | .001 |
| Normal shoulder function throwing a ball overhead 20 yards e | 1 (very difficult) | 3 (normal) | .027 |
| Pain affects recreational activity f | 3 (severe) | 0 (none) | .004 |
a Boldface P values indicate a statistically significant difference between pre- and postoperative values (P < .05).
b Out of 6 categories: 1 = equal to or above preinjury level, 2 = slightly below preinjury level, 3 = moderately below preinjury level, 4 = significantly below preinjury level, 5 = cannot compete in usual sport, 6 = cannot compete in any sports.
c Out of 6 categories: 1 = same or better than preinjury, 2 = 75%-99% of preinjury level, 3 = 50%-74% of preinjury level, 4 = 25%-49% of preinjury level, 5 = <25% of preinjury level, 6 = no longer compete at any intensity.
d Out of 6 categories: 1 = no pain, 2 = pain after competition, 3 = mild pain with competition, 4 = moderate pain with competition, 5 = severe pain with competition, 6 = pain prevents competition.
e Out of 4 categories: 0 = unable, 1 = very difficult, 2 = somewhat difficult, 3 = normal.
f Out of 4 categories: 0 = none, 1 = mild, 2 = moderate, 3 = severe.
Complications and Clinical Failures
Postoperative complications occurred in both groups. One patient in each group was evaluated with postoperative stiffness, and both patients were revised with arthroscopic arthrolysis and ended up with satisfying postoperative clinical outcomes. There was 1 patient in the biceps tenodesis group who experienced a humeral shaft fracture at 1.2 years that was classified as a postoperative complication due to drilling for interference screw placement within the fracture line.
Discussion
The main finding of this study confirmed our initial hypothesis in that biceps tenodesis and SLAP repair both result in excellent and comparable patient-reported outcomes and complication rates in this young and high-demanding patient population in the short term. While biceps tenodesis showed a significant decrease in pain during competition, SLAP repair was superior in return to preinjury sports level and intensity. Both procedures showed a significant improvement in both shoulder function during throwing and pain relief during recreational activity. However, more patients reported modifying their sporting/recreational activity because of weakness after biceps tenodesis compared with after SLAP repair (80% vs 15%; P = .022).
Some surgeons may be cautious about performing SLAP repair in young overhead athletes, as the repair construct experiences high loads during the arm cocking and deceleration phases. Walch et al 31 introduced the concept of the posterosuperior impingement during the cocking phase, which occurs when the posterior aspect of the SLAP region is exposed to a mechanical impingement between the posterior rotator cuff and the humeral head. Burkhart et al 6 further described the peel-back mechanism, in which the biceps anchor–SLAP region refrains a twist and pull off the glenoid. Thus, there is concern over potentially higher complication rates that may occur after SLAP repair because of the higher biomechanical load placed on this region, specifically in overhead athletes. However, these beliefs were refuted in this study, as no significant difference in failure rates was seen between the SLAP repair and biceps tenodesis groups. One patient with persistent postoperative stiffness was observed in each group, which may have been caused by prolonged restrictions during postoperative rehabilitation. Moreover, in the biceps tenodesis group, 1 major complication with a spiral humeral shaft fracture after a fall also occurred. This fracture pattern may have resulted from the 7- to 8-mm drilling of the humeral shaft for interference screw placement during biceps tenodesis and might have been avoided with use of an onlay technique for subpectoral biceps tenodesis. 14,19,20,26
In contrast to previously reported studies, 16,27 a higher rate of sports modification was seen in overhead athletes after biceps tenodesis than seen for SLAP repair (80% vs 15%; P = .022). This may imply that the long biceps tendon and its stabilizing function should not be neglected, especially in overhead athletes. When checking for numbers of baseball players who tended to react sensitively to interventions on the proximal aspect of the biceps tendon, we saw an even distribution (5 vs 5 players) in both groups for this cohort. Despite excellent return-to-sports rates even for this heterogenous cohort of overhead athletes, including climbers, weight lifters, and football players, SLAP repair has been shown to significantly influence the level of previous sporting/recreational activity. This is in line with Smith et al, 27 who investigated the return-to-play rates in Major League Baseball pitchers showing a return-to-play rate of 62.5% after SLAP repair. Those who successfully returned to play were able to achieve the level of prior performance in 86.7%. Similar data were presented by Gilliam et al, 16 comparing pitchers and nonpitchers. The authors demonstrated an overall success rate of return to sport in 62%. When comparing pitchers with nonpitchers, these numbers have started to differ, showing a successful return to sport in 59% versus 76%, respectively.
In the evaluation of return-to-sport rate, the biceps tenodesis group was slightly superior when compared with the SLAP repair group (85% vs 79%; P > .64), but this was not statistically significant and showed the restrictions/modifications mentioned above. Despite similar return-to-sports rates for both groups, the SLAP repair group had a statistically significant improvement in level of sports participation. Overall, the results of this study are encouraging for overhead athletes hoping to return to their preinjury level of sport.
The findings of the current study are comparable to recent results in the literature. 3,8,11,25,29,30 In 2018, Hurley et al 18 summarized in their systematic review and meta-analysis functional outcomes after SLAP repair versus biceps tenodesis. Among 234 patients in 5 studies, the authors found higher rates of patient satisfaction (96% vs 76%) and return to sport (81% vs 64%) in favor of biceps tenodesis when compared with SLAP repair. 18 There was no statistically significant difference in complication rates, rates of reoperation, or functional outcomes. However, the mean age of 35 to 52 years in this systematic review, 18 and previous outcome reports, 3,8,11,25 is a slight limitation in the applicability to the present study’s findings.
Interestingly, Cvetanovich and colleagues 9 showed that SLAP repair is favored predominantly in younger patients, but that the overall trend of performing SLAP repair has decreased in total, as shown with data from the database of the American Board of Orthopaedic Surgery. The trend toward performing biceps tenodesis versus SLAP repair in SLAP type 2 lesions as patients age may be because of the more degenerative nature of the SLAP lesions (vs a lesion of traumatic origin), which would predict poor healing potential. This is supported by findings of Provencher et al, 24 who analyzed outcomes and factors associated with success and failure after labral repair in a prospective evaluation of 179 type 2 SLAP repairs. The authors showed that a patient older than 36 years was associated with a higher chance of failure. 24 Further, some may trend toward biceps tenodesis versus SLAP repair because of the rates of stiffness seen after SLAP repair. In the current study, similar numbers for postoperative stiffness were observed for both groups.
While biceps tenodesis may be superior in an aging population, Chalmers et al 7 called attention to compromised results in overhead athletes (baseball pitchers) by finding a reduced rate of return to professional play. The authors assessed for rate of return to prior level of play among the population of 17 professional baseball players, showing that only 35% returned to their preinjury level. This may indicate that especially in overhead athletes, the long head of the biceps tendon may play a more important role influencing performance. 7 Schroder et al 25 impressively demonstrated in a 3-armed randomized controlled trial (40 patients per group; mean age, 40 years) that 89% of patients who underwent either SLAP repair or biceps tenodesis had excellent clinical outcomes, while sham surgery had the highest rates of revision (sham surgery 36% vs biceps tenodesis 15% vs SLAP repair 10%).
Respecting the results of the current and previous studies, SLAP repair and biceps tenodesis for overhead athletes should be considered as an option in the treatment of symptomatic SLAP type 2 lesions only if nonoperative treatment has failed. Athletes should be informed about the chances of returning to their previous sport and level of performance.
Limitations
While the current study demonstrated interesting findings in this age- and activity-selected cohort, there are limitations that must be mentioned. No clinical examination at final follow-up was performed to assess minor range of motion deficits or biceps strength. No performance metrics were analyzed to objectively assess the athlete’s performance. The patient-reported outcome measures used in this study may not have been the best for high-level athletes. This is a short-term follow-up study, and possible clinical differences between both groups at mid- and long-term follow-up might exist. Also, since the patient number is small and included a mixture of sports, statistical differences and the informative value of this study might be clearer with a larger number of cases. All eligible patients from a prospectively enrolled research database were included in this study. A power calculation assuming this study’s fixed sample size indicated that effect sizes more subtle than d = 0.99 cannot be ruled out by this study. Moreover, there was selection bias, as this was not a randomized study. Although this indicates that the groups are not ideally comparable, this retrospective study aimed to report a continuous and rare series of young overhead athletes affected by SLAP type 2 lesions treated with either SLAP repair or biceps tenodesis.
Conclusion
This study showed that subpectoral biceps tenodesis and SLAP repair provided excellent clinical results with a high rate of return to overhead sports and a low failure rate in a young and high-demanding patient cohort for the treatment of isolated SLAP type 2 lesions. However, more patients reported modifying their sporting/recreational activity because of weakness after biceps tenodesis.
Footnotes
Final revision submitted February 9, 2022; accepted February 23, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: The positions of L.L. and P.C.N. at the Steadman Philippon Research Institute were supported by AGA, via Arthrex, for 1 calendar year. T.J.D. has received educational or grant support from Smith & Nephew, CGG Medical, and DJO. P.J.M. has received research support from Arthrex, Ossur, Siemens, and Smith & Nephew; consulting fees from Arthrex; royalties from Arthrex, Medbridge, and Springer; and hospitality payments from Arthrosurface, Merz Pharmaceuticals, Sanofi-Aventis, and Stryker; and has stock/stock options in VuMedi. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Vail Health Hospital (protocol No. 2018-69).
References
- 1. Altintas B, Pitta R, Fritz EM, Higgins B, Millett PJ. Technique for type IV SLAP lesion repair. Arthrosc Tech. 2018;7(4):e337–e342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Andrews JR, Carson WG, Jr, McLeod WD. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med. 1985;13(5):337–341. [DOI] [PubMed] [Google Scholar]
- 3. Boileau P, Parratte S, Chuinard C, Roussanne Y, Shia D, Bicknell R. Arthroscopic treatment of isolated type II SLAP lesions: biceps tenodesis as an alternative to reinsertion. Am J Sports Med. 2009;37(5):929–936. [DOI] [PubMed] [Google Scholar]
- 4. Braun S, Horan MP, Elser F, Millett PJ. Lesions of the biceps pulley. Am J Sports Med. 2011;39(4):790–795. [DOI] [PubMed] [Google Scholar]
- 5. Braun S, Millett PJ, Yongpravat C, et al. Biomechanical evaluation of shear force vectors leading to injury of the biceps reflection pulley: a biplane fluoroscopy study on cadaveric shoulders. Am J Sports Med. 2010;38(5):1015–1024. [DOI] [PubMed] [Google Scholar]
- 6. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology Part I: pathoanatomy and biomechanics. Arthroscopy. 2003;19(4):404–420. [DOI] [PubMed] [Google Scholar]
- 7. Chalmers PN, Erickson BJ, Verma NN, D’Angelo J, Romeo AA. Incidence and return to play after biceps tenodesis in professional baseball players. Arthroscopy. 2018;34(3):747–751. [DOI] [PubMed] [Google Scholar]
- 8. Chalmers PN, Monson B, Frank RM, et al. Combined SLAP repair and biceps tenodesis for superior labral anterior-posterior tears. Knee Surg Sports Traumatol Arthrosc. 2016;24(12):3870–3876. [DOI] [PubMed] [Google Scholar]
- 9. Cvetanovich GL, Gowd AK, Frantz TL, Erickson BJ, Romeo AA. Superior labral anterior posterior repair and biceps tenodesis surgery: trends of the American Board of Orthopaedic Surgery database. Am J Sports Med. 2020;48(7):1583–1589. [DOI] [PubMed] [Google Scholar]
- 10. Dekker TJ, Lacheta L, Goldenberg B, Grantham WJ, Millett PJ. Rotator cuff sparing arthroscopic SLAP repair with knotless all-suture anchors. Arthrosc Tech. 2019;8(9):e993–e998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Denard PJ, Ladermann A, Parsley BK, Burkhart SS. Arthroscopic biceps tenodesis compared with repair of isolated type II SLAP lesions in patients older than 35 years. Orthopedics. 2014;37(3):e292–e297. [DOI] [PubMed] [Google Scholar]
- 12. Ek ET, Shi LL, Tompson JD, Freehill MT, Warner JJ. Surgical treatment of isolated type II superior labrum anterior-posterior (SLAP) lesions: repair versus biceps tenodesis. J Shoulder Elbow Surg. 2014;23(7):1059–1065. [DOI] [PubMed] [Google Scholar]
- 13. Elser F, Braun S, Dewing CB, Giphart JE, Millett PJ. Anatomy, function, injuries, and treatment of the long head of the biceps brachii tendon. Arthroscopy. 2011;27(4):581–592. [DOI] [PubMed] [Google Scholar]
- 14. Euler SA, Smith SD, Williams BT, Dornan GJ, Millett PJ, Wijdicks CA. Biomechanical analysis of subpectoral biceps tenodesis: effect of screw malpositioning on proximal humeral strength. Am J Sports Med. 2015;43(1):69–74. [DOI] [PubMed] [Google Scholar]
- 15. Fedoriw WW, Ramkumar P, McCulloch PC, Lintner DM. Return to play after treatment of superior labral tears in professional baseball players. Am J Sports Med. 2014;42(5):1155–1160. [DOI] [PubMed] [Google Scholar]
- 16. Gilliam BD, Douglas L, Fleisig GS, et al. Return to play and outcomes in baseball players after superior labral anterior-posterior repairs. Am J Sports Med. 2018;46(1):109–115. [DOI] [PubMed] [Google Scholar]
- 17. Giphart JE, Elser F, Dewing CB, Torry MR, Millett PJ. The long head of the biceps tendon has minimal effect on in vivo glenohumeral kinematics: a biplane fluoroscopy study. Am J Sports Med. 2012;40(1):202–212. [DOI] [PubMed] [Google Scholar]
- 18. Hurley ET, Fat DL, Duigenan CM, Miller JC, Mullett H, Moran CJ. Biceps tenodesis versus labral repair for superior labrum anterior-to-posterior tears: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2018;27(10):1913–1919. [DOI] [PubMed] [Google Scholar]
- 19. Lacheta L, Imhoff AB, Siebenlist S, Scheiderer B. Subpectoral biceps tenodesis: all-suture anchor onlay technique. Arthrosc Tech. 2020;9(5):e651–e655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lacheta L, Rosenberg SI, Brady AW, Dornan GJ, Millett PJ. Biomechanical comparison of subpectoral biceps tenodesis onlay techniques. Orthop J Sports Med. 2019;7(10):2325967119876276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nam EK, Snyder SJ. The diagnosis and treatment of superior labrum, anterior and posterior (SLAP) lesions. Am J Sports Med. 2003;31(5):798–810. [DOI] [PubMed] [Google Scholar]
- 22. O’Holleran JD, Kocher MS, Horan MP, Briggs KK, Hawkins RJ. Determinants of patient satisfaction with outcome after rotator cuff surgery. J Bone Joint Surg Am. 2005;87(1):121–126. [DOI] [PubMed] [Google Scholar]
- 23. Pogorzelski J, Horan MP, Hussain ZB, Vap A, Fritz EM, Millett PJ. Subpectoral biceps tenodesis for treatment of isolated type II SLAP lesions in a young and active population. Arthroscopy. 2018;34(2):371–376. [DOI] [PubMed] [Google Scholar]
- 24. Provencher MT, McCormick F, Dewing C, McIntire S, Solomon D. A prospective analysis of 179 type 2 superior labrum anterior and posterior repairs: outcomes and factors associated with success and failure. Am J Sports Med. 2013;41(4):880–886. [DOI] [PubMed] [Google Scholar]
- 25. Schroder CP, Skare O, Reikeras O, Mowinckel P, Brox JI. Sham surgery versus labral repair or biceps tenodesis for type II SLAP lesions of the shoulder: a three-armed randomised clinical trial. Br J Sports Med. 2017;51(24):1759–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Siebenlist S, Lenich A, Buchholz A, et al. Biomechanical in vitro validation of intramedullary cortical button fixation for distal biceps tendon repair: a new technique. Am J Sports Med. 2011;39(8):1762–1768. [DOI] [PubMed] [Google Scholar]
- 27. Smith R, Lombardo DJ, Petersen-Fitts GR, et al. Return to play and prior performance in Major League Baseball pitchers after repair of superior labral anterior-posterior tears. Orthop J Sports Med. 2016;4(12):2325967116675822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Snyder SJ, Karzel RP, Del Pizzo W, Ferkel RD, Friedman MJ. SLAP lesions of the shoulder. Arthroscopy. 1990;6(4):274–279. [DOI] [PubMed] [Google Scholar]
- 29. Tahal DS, Katthagen JC, Vap AR, Horan MP, Millett PJ. Subpectoral biceps tenodesis for tenosynovitis of the long head of the biceps in active patients younger than 45 years old. Arthroscopy. 2017;33(6):1124–1130. [DOI] [PubMed] [Google Scholar]
- 30. Vap AR, Katthagen JC, Tahal DS, et al. Isolated biceps reflection pulley tears treated with subpectoral biceps tenodesis: minimum 2-year outcomes. Arthroscopy. 2017;33(10):1788–1794. [DOI] [PubMed] [Google Scholar]
- 31. Walch G, Boileau P, Noel E, Donell ST. Impingement of the deep surface of the supraspinatus tendon on the posterosuperior glenoid rim: an arthroscopic study. J Shoulder Elbow Surg. 1992;1(5):238–245. [DOI] [PubMed] [Google Scholar]


