Abstract
Background:
The most reliable suture technique for capsular closure after a capsulotomy remains unknown.
Purpose:
To determine which suture technique best restores native stability after a 5-cm interportal capsulotomy.
Study Design:
Controlled laboratory study.
Methods:
Ten human cadaveric hip specimens were tested using a 6-degrees-of-freedom robotic arm in 7 states: intact, capsular laxity, 5-cm capsulotomy, standard suture, shoelace, double shoelace, and Quebec City slider (QCS). Rotational range of motion (ROM) was measured across 9 tests: flexion, extension, abduction, abduction at 45° of flexion, adduction, external rotation, internal rotation, anterior impingement, and log roll. Distraction (ie, femoral head translation [FHT]) was measured across a range of flexion and abduction angles.
Results:
When compared with the native state, the 5-cm capsulotomy state showed the largest laxity increases on all tests, specifically in external rotation ROM (+13.4°), extension ROM (+11.5°), and distraction FHT (+4.5 mm) (P < .001 for all). The standard suture technique was not significantly different from the 5-cm capsulotomy on any test and demonstrated significantly more flexion ROM than the double shoelace suture (+1.41°; P = .049) and more extension ROM (+5.51°; P = .014) and external rotation ROM (+6.03°; P = .021) than the QCS. The standard suture also resulted in significantly higher distraction FHT as compared with the shoelace suture (+1.0 mm; P = .005), double shoelace suture (+1.4 mm; P < .001), and QCS (+1.1 mm; P = .003). The shoelace, double shoelace, and QCS techniques significantly reduced hip laxity when compared with the 5-cm capsulotomy state, specifically in external rotation ROM (respectively, –8.1°, –7.8°, and –10.2°), extension ROM (–6.3°, –7.3°, and –8.1°), and distraction FHT (–1.8, –2.2, and –1.9 mm) (P ≤ .003 for all). These 3 techniques restored native stability (no significant difference from intact) on some but not all tests, and no significant differences were observed among them on any test.
Conclusion:
Hip capsule closure with the standard suture technique did not prevent postoperative hip instability after a 5-cm capsulotomy, and 3 suture techniques were found to be preferable; however, none perfectly restored native stability at time zero.
Clinical Relevance:
The shoelace, double shoelace, and QCS suture techniques are recommended when closing the hip capsule.
Keywords: hip capsule closure, shoelace suture, double shoelace suture, Quebec City slider, biomechanical study, hip arthroscopy, hip range of motion, hip distraction, iliofemoral ligament
Hip arthroscopy is a well-established, evolving tool for diagnosing and treating hip pathologies. This surgical intervention can correct bone abnormalities and fix associated intra-articular pathologies, such as labral tearing and cartilage delamination, 5,13 with favorable clinical outcomes. 7,8,20 Yet, Harris et al 11 performed a systematic review of 6134 hip arthroscopy procedures and found that 6.3% of patients needed reoperation, including conversion to total hip arthroplasty.
Multiple causes for poor outcomes and revision surgery have been identified, such as increased acetabular coverage and femoral pistol grip deformity, 10 overresection of cam impingement, 18 unaddressed or underresected cam or pincer-type deformity, 24 and iatrogenic hip instability caused by an untreated capsulotomy or excessive capsular debridement for visualization. 18 Bolia et al 3 compared midterm outcomes after capsulotomy repair versus nonrepair in patients undergoing hip arthroscopy and reported that patients who underwent capsulotomy repair had higher patient-reported outcomes and lower rates of conversion to total hip arthroplasty. Previous biomechanical studies of the hip found that interportal capsulotomy or a T capsulotomy increased range of motion (ROM). 1,12 Iatrogenic hip instability or joint laxity has been clinically identified as an existing pathology and potential risk factor for hip osteoarthritis. 4,6,31 Therefore, capsular closure has been recommended to treat patients with hip instability. 14,17
Several new suture techniques have recently been described for capsular closure. Menge et al 19 reported on the Quebec City slider (QCS) technique, while Kizaki et al 16 and Uchida et al 27 detailed the arthroscopic shoelace and double shoelace capsular closure techniques. However, the biomechanical efficacy of these techniques as compared with standard suture has not yet been evaluated, and it remains unknown which technique best prevents postoperative hip instability. More evidence is needed to establish how to best repair a capsulotomy in patients undergoing hip arthroscopy.
The purpose of this study was to compare the efficacy of 4 suture techniques in a capsulotomy state—standard, shoelace, double shoelace, and QCS—for treating a 5-cm interportal capsulotomy created during an arthroscopic procedure. We hypothesized that the shoelace, double shoelace, and QCS suture techniques would be superior to the standard suture in restoring hip stability.
Methods
Specimen Preparation
This study included 10 unpaired human cadaveric hemipelvises including intact femurs with no history of hip injury or surgery (mean age, 58.1 years [range, 51-62 years]; mean body mass index, 22.2 kg/m2 [range, 15.0-32.3 kg/m2]; 5 men, 5 women; 5 right, 5 left). Institutional review board approval was not required for this study, because deidentified human cadaveric specimens are exempt from review consideration at our institution. The cadaveric specimens utilized in this study were donated to a tissue bank for the purpose of medical research and then purchased by our institution. All specimens were dissected free of all soft tissues superficial to the hip capsule. Specimens were stored at –20°C and thawed at room temperature for approximately 24 hours before testing.
To achieve neutral positioning of the hip, the hemipelvis and femur were placed on a table in a supine position. The femoral condyles maintained contact with a horizontal surface that was elevated 110 mm above the plane of the table throughout the neutral-setting process, while the hemipelvis was rotated to achieve neutral alignment. Hip internal/external rotation was set to neutral by aligning the pubic symphysis vertically to the hemisacral cut in the transverse plane. Hip abduction/adduction was set to neutral by aligning the mechanical axis of the femur parallel to the longitudinal axis of the sacrum in the coronal plane. Hip flexion/extension (pelvic tilt) was set to neutral by aligning the anterior superior iliac spine with the posterior superior iliac spine vertically in the sagittal plane.
When all 3 alignment conditions were met simultaneously, the joint was pinned in place using 2 K-wires driven from the lateral femoral shaft into the pubic bone and the ischium to stabilize the neutral position and eliminate rotation. Because the flexion/extension angle was dependent on the height of the femur, which was set arbitrarily for consistency during the initial neutral-setting process, this angle was re-set after the specimen was mounted to the robot by measuring the total arc of flexion-extension ROM and defining the neutral orientation such that 85% of the arc was flexion and 15% of the arc was extension. This pelvic tilt was based on findings from previous articles: (1) the hip flexion angle of the hips is the sum of the real hip joint flexion and posterior pelvic tilt2; (2) the rate of the pelvic contribution to the hip flexion angle is 20% to 30%2; and (3) the normal hip flexion angle is approximately 120°, and the normal hip extension angle is 15° with a fixed pelvis. 23 Based on these findings, the true hip joint flexion and extension represent 85% and 15% of total ROM, respectively, in the sagittal plane when pelvic tilt change during this motion is ignored. 2,23
Robotic Setup
Using a coordinate measuring machine (Romer Absolute Arm; Hexagon Manufacturing Intelligence), the relevant bony anatomy of the specimen was digitized to construct a joint coordinate system according to the International Society of Biomechanics standard. 29 Next, the femur and pelvis were individually potted in cylindrical molds of polymethyl methacrylate (Fricke Dental International Inc). The joint was then rigidly fixed to a 6-degrees-of-freedom robotic system (KUKA KR 60-3; KUKA Robotics) by securing the pelvis to the robot end effector and the femur to a rigid pedestal using custom fixtures. The pedestal was equipped with a 6-axis universal force/torque sensor. The software simVITRO (Version 5.2.1.74 Simulation Solutions) was used to control the robot and prescribe the desired forces and motions to the joint (Figure 1).
Figure 1.
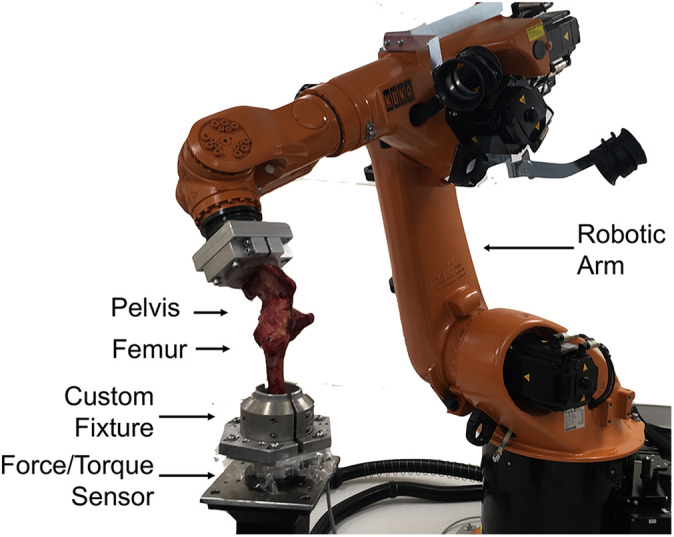
Biomechanical testing setup for a human cadaveric hip (right joint shown). The femur was secured within a custom fixture attached to the 6-axis force/torque sensor located on a static pedestal. The hemipelvis is mounted within a custom fixture attached to the effector of the KUKA KR-60 robotic arm.
Surgical Procedures
Each specimen underwent biomechanical testing in 7 states: intact (state 1), capsular laxity (state 2), standard suture (state 3), shoelace (state 4), double shoelace (state 5), QCS (state 6), and 5-cm capsulotomy (state 7). The 5-cm capsulotomy was created after the capsular laxity model (state 2), but it was immediately repaired without testing it first; the untreated capsulotomy (state 7) was tested last to avoid any tearing of soft tissue, which could affect subsequent states. The order of the capsular repairs (states 3-6) was randomized for each specimen. The capsular laxity model (state 2) was created using the protocol described by Jackson et al, 12 in which a 35-N·m extension torque for male specimens (or 25 N·m for female specimens) was applied to the hip for 1 hour. During this process the other rotation axes were kept in neutral under position control, and the forces were held at 60 N of compression and zero force in the anterior and lateral directions under force control. The laxity model was introduced to increase clinical relevance, based on the assumption that many patients undergoing hip arthroscopy experience capsular laxity before surgery.
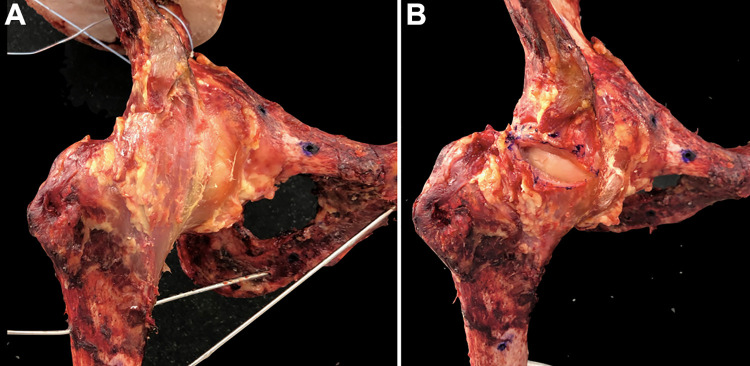
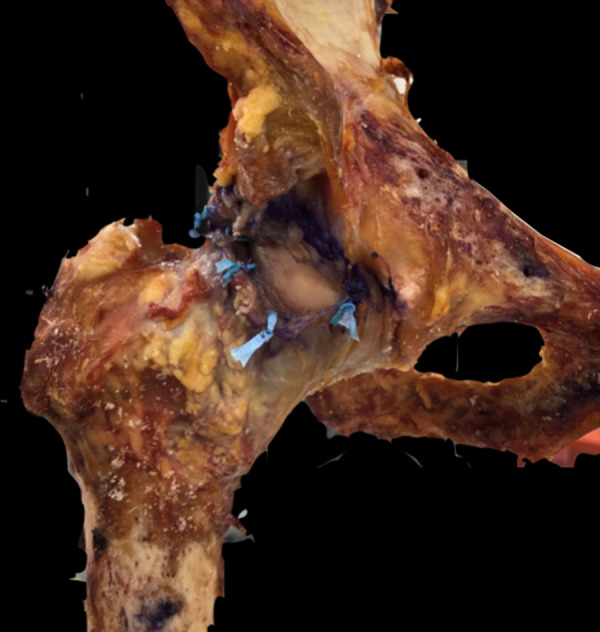
The 5-cm capsulotomy (state 7) was measured by marking a 5-cm line anteriorly from the superior capsule. The capsulotomy was then created along the line using a No. 10 blade scalpel. Care was taken to completely transect the iliofemoral ligament (IFL) in each specimen. The IFL margins were assessed visually by locating the iliocapsularis muscle and denoting the fibers deep to the muscle. The capsulotomy and transection of the IFL were performed and confirmed by 2 fellowship-trained orthopaedic surgeons (Y.M., N.F.) (Figure 2).
Figure 2.
Right hip joint (A) in the intact state and (B) with a 5-cm capsulotomy.
The 4 capsular repairs (states 3-6) were all performed using No. 2 UltraTape (Smith & Nephew). The standard suture repair was performed using 5 evenly spaced simple interrupted sutures passed using a free needle and tied with alternating half-hitch knots. The single shoelace suture was performed using a suture passer (Accu-Pass; Smith & Nephew) to create stitches starting at the proximal end of the capsulotomy and ending at the distal end, traveling about 6 to 7 mm with each stitch in accordance with the previously described technique. 27 Once the capsulotomy was closed, the stitch was secured with alternating half-hitch knots.
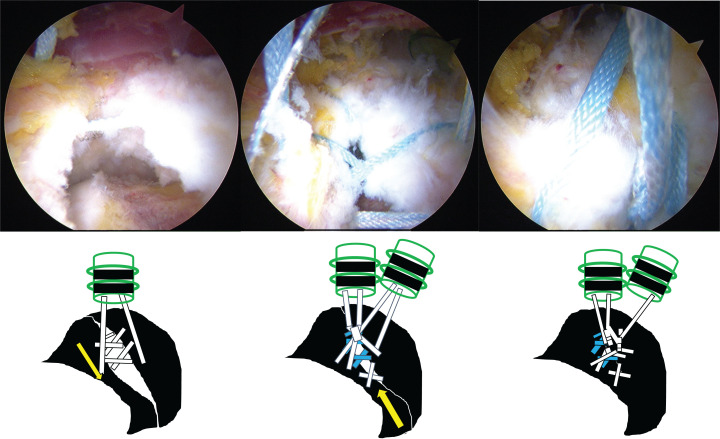
The double shoelace suture was performed using the same method as the single shoelace suture, with the addition of a second suture starting from the distal capsulotomy working proximally as described in the literature (Figure 3). 16 The QCS was performed using a double-limb UltraTape suture that was shuttled through the capsule using a free needle in the same way as the simple suture. Two fingers from each hand of the surgeon were placed within the 2 looped ends of the suture. Each hand was then pronated to form 2 separate loops. The 2 resultant loops were placed in one hand, and the free end of the suture was passed through both loops and pulled tight, in accordance with the previously described technique. 19 This stitch was secured with alternating half-hitch knots. Five QCS stitches were placed evenly to close the capsulotomy.
Figure 3.
Arthroscopic (top) and schematic (bottom) representation of the double shoelace suture technique.
Biomechanical Testing
Each specimen underwent 9 ROM tests in each state: flexion (test 1), extension (test 2), abduction (test 3), adduction (test 4), external rotation (test 5), internal rotation (test 6), abduction at 45° of flexion (test 7), anterior impingement (test 8), and log roll (test 9). The order of the tests was randomized in each state. All robotic tests were performed with the 3 translational axes in force control. Forces were minimized in the anterior and lateral directions, while a 60-N compressive force was applied in the superior direction to seat the joint.
Tests 1 to 6 were performed with the hip starting in neutral orientation. A 5-N·m torque was applied on the tested rotational axis, while the other 2 rotational axes were maintained at 0° in position control. The abduction test at 45° of flexion (test 7) was performed similarly to test 3 but with the hip maintained at 45° of flexion instead of 0° of flexion. The anterior impingement test (test 8) was performed with the hip starting in 95° of flexion, 5° of adduction, and 0° of internal rotation. The adduction and flexion angles were maintained constant throughout the test, while a 5-N·m internal rotation torque was applied to the joint. The log roll test was performed similarly to the internal rotation test, with the addition of an 88-N anterior force applied to the femur. For all ROM tests, the ROM (in degrees) on the torque-controlled axis and the femoral head translation (FHT; in millimeters) were recorded.
Each specimen underwent 6 distraction tests in each state. Distraction tests consisted of a 200-N distraction force oriented at a 45° angle between the inferior and lateral axes in the coronal plane. Forces were minimized along the anterior axis, and the hip was maintained in neutral internal rotation. The distraction tests were performed in the following hip positions: (1) neutral flexion, neutral adduction; (2) neutral flexion, 10° of adduction; (3) 10° of flexion, neutral adduction; (4) 10° of flexion, 10° of adduction; (5) 10° of extension, neutral adduction; and (6) 10° of extension, 10° of adduction. For all distraction tests, FHT (in millimeters) was recorded. The order of the distraction tests was randomized in each state, and the distraction tests were always run after the ROM tests.
Statistical Analysis
To match the repeated-measures experimental design, random-intercepts linear mixed effects models were used to compare capsule states. For the ROM tests, 1-factor linear mixed effects models were built to compare the ROM and FHT among capsule states during each simulated hip examination. For the distraction tests, a 3-factor model was built to compare the magnitude of FHT among capsule states while modeling the adduction and flexion angles. An unstructured covariance matrix was assumed for all linear mixed effects models. Estimated marginal means were reported, and the Tukey method was used to make all pairwise comparisons among the 7 hip capsule states. Residual diagnostics were inspected to ensure model fit, and those assumptions were met. The statistical software R was used for all plots and analyses (R Core Team version 4.0.0 with lmer and emmeans packages).
RESULTS
Table 1 shows the data from the 5-cm capsulotomy state and the repair states for increases in ROM and FHT versus the native state. Table 2 presents the data from the repair states for decreases in ROM and FHT as compared with the 5-cm capsulotomy state, discounting the anterior impingement test because no increase was demonstrated in the 5-cm capsulotomy state versus the intact state for that test. The results from the 6 distraction tests were analyzed using a 3-factor model: specimen state, flexion angle, and adduction angle. Therefore, FHT values in Tables 1 and 2 correspond to average increases and decreases across the range of flexion and adduction angles tested, and the P values apply to the range of flexion and adduction angles tested. Figure 4 shows box plots of all 9 ROM tests, while Appendix Figure A1 illustrates the results of the 3-factor mode for the distraction tests. Appendix Table A1 presents the mean ROM results in all states, and Appendix Table A2 contains the individual results from each distraction test.
Table 1.
Increases in Range of Motion and FHT Versus the Intact State a
| ROM Increase, deg (P Value) | |||||
|---|---|---|---|---|---|
| Test | 5-cm Capsulotomy | Standard Suture | Shoelace Suture | Double Shoelace | Quebec City Slider |
| Flexion | 2.6 (<.001) | 2.2 (<.001) | 1.0 (.348) | 0.8 (.604) | 0.9 (.405) |
| Extension | 11.5 (<.001) | 8.9 (<.001) | 5.1 (.028) | 4.2 (.122) | 3.4 (.330) |
| Abduction | 4.4 (<.001) | 3.8 (<.001) | 3.7 (<.001) | 3.1 (<.001) | 3.4 (<.001) |
| Adduction | 8.1 (<.001) | 5.5 (.002) | 4.9 (.006) | 3.8 (.064) | 3.2 (.174) |
| External rotation | 13.4 (<.001) | 9.2 (<.001) | 5.3 (.059) | 5.6 (.040) | 3.2 (.546) |
| Internal rotation | 3.7 (<.001) | 3.5 (<.001) | 3.5 (<.001) | 3.3 (<.001) | 3.5 (<.001) |
| Abduction at 45° of flexion | 3.2 (<.001) | 2.8 (<.001) | 2.6 (<.001) | 2.2 (<.001) | 2.4 (<.001) |
| Anterior impingement | 0.1 (.781) | 0.1 (.998) | 0.0 (>.999) | 0.0 (>.999) | 0.0 (.999) |
| Log roll | 2.9 (<.001) | 1.5 (.147) | 0.3 (.999) | 0.1 (>.999) | 0.3 (.999) |
| Significant increases b | 8/9 | 7/9 | 5/9 | 4/9 | 3/9 |
| FHT Increase, mm (P Value) | |||||
| Distraction | 4.5 (<.001) | 3.7 (<.001) | 2.7 (<.001) | 2.3 (<.001) | 2.7 (<.001) |
a Orange cells indicate a significant increase from the native state (bad), while green cells indicate no significant difference from the intact state (good). FHT, femoral head translation.
b Number of tests for which the corresponding state showed a significant increase from the native state (lower is better).
Table 2.
Decreases in Range of Motion and FHT Versus the 5-cm Capsulotomy State a
| ROM Decrease, deg (P Value) | ||||
|---|---|---|---|---|
| Test | Standard Suture | Shoelace Suture | Double Shoelace | Quebec City Slider |
| Flexion | 0.4 (.967) | 1.7 (.012) | 1.8 (.004) | 1.7 (.009) |
| Extension | 2.6 (.652) | 6.3 (.003) | 7.3 (<.001) | 8.1 (<.001) |
| Abduction | 0.6 (.618) | 0.7 (.363) | 1.3 (.009) | 1.0 (.100) |
| Adduction | 2.6 (.419) | 3.1 (.207) | 4.3 (.027) | 4.8 (.008) |
| External rotation | 4.1 (.247) | 8.1 (.001) | 7.8 (.001) | 10.2 (<.001) |
| Internal rotation | 0.1 (>.999) | 0.2 (>.999) | 0.4 (.980) | 0.2 (.999) |
| Abduction at 45° of flexion | 0.4 (.702) | 0.6 (.341) | 1.0 (.012) | 0.8 (.065) |
| Anterior impingement | 0.1 (.968) | 0.1 (.854) | 0.1 (.826) | 0.1 (.964) |
| Log roll | 1.4 (.187) | 2.6 (.001) | 3.0 (<.001) | 2.6 (<.001) |
| Significant decreases b | 0/9 | 4/9 | 7/9 | 5/9 |
| FHT Decrease, mm (P Value) | ||||
| Distraction | 0.8 (.053) | 1.8 (<.001) | 2.2 (<.001) | 1.9 (<.001) |
a Orange cells indicate no significant decrease from the 5-cm capsulotomy state (bad), while green cells indicate a significant decrease from the 5-cm capsulotomy state (good). FHT, femoral head translation.
b Number of tests for which the corresponding state showed a significant decrease from the 5-cm capsulotomy state (higher is better).
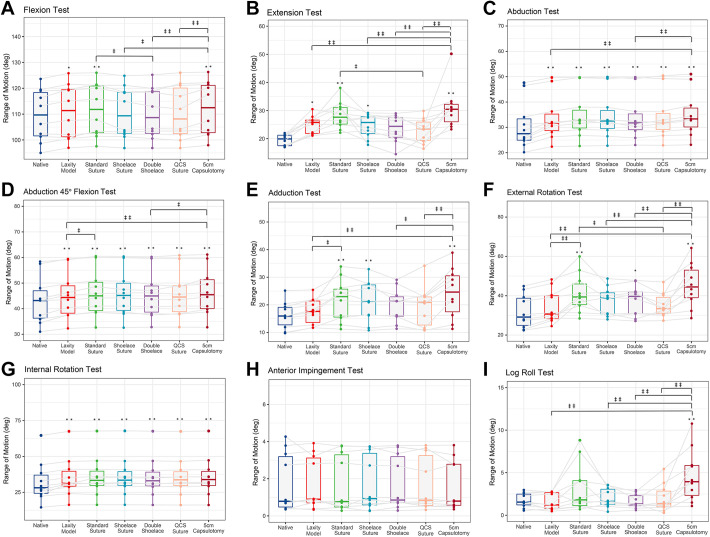
Figure 4.
Box plot graphs demonstrating range of motion in degrees during the 9 tests: (A) flexion, (B) extension, (C) abduction, (D) abduction at 45° of flexion, (E) adduction, (F) external rotation, (G) internal rotation, (H) anterior impingement, and (I) log roll. Dots represent individual specimen observations. Thick horizontal lines represent group medians, while top and bottom of boxes represent the 25th and 75th percentiles, respectively. Significantly different: ‡ P < .05. ‡‡ P < .01. Significantly different from native state: *P < .05. **P < .01. QCS, Quebec City slider.
Five-Centimeter Capsulotomy
When compared with the native state, the 5-cm capsulotomy state demonstrated the largest magnitude of increases in ROM and FHT, with significant increases in 9 of 10 tests (all but anterior impingement). The largest significant ROM increases appeared in external rotation (+13.4°; P < .001) and extension (+11.5°; P < .001). This state also presented the largest FHT increase in distraction (+4.5 mm; P < .001). Because the anterior impingement test did not result in any significant increases in the 5-cm capsulotomy state versus the native state, it was excluded from the number of significant decreases when repairs were compared with the 5-cm capsulotomy in Table 2. Indeed, it would not be desirable for the repairs to reduce the ROM in this test, given that the 5-cm capsulotomy did not increase ROM in the first place and no significant differences were found in the anterior impingement test across all testing states.
Standard Suture
When compared with the native state, the standard suture repair demonstrated significant increases in 8 of 10 tests, with the largest significant ROM differences appearing in external rotation (+9.2°; P < .001) and extension (+8.9°; P < .001). The distraction test had the highest increase in FHT among the repair states (+3.7 mm; P < .001). As compared with the 5-cm capsulotomy, the standard suture repair resulted in significant decreases in ROM and FHT in 0 of 9 tests. In 4 of 10 specimens, the knots in the standard sutures did not withstand biomechanical testing and were found to be undone after the standard suture state, as shown in Figure 5.
Figure 5.
Photograph of a right hip after failure of the standard suture technique.
Shoelace Suture
When compared with the native state, the shoelace suture repair demonstrated significant increases in 6 of 10 tests with the largest significant ROM differences appearing in extension (+5.1°; P = .028) and adduction (+4.9°; P = .006). The distraction test yielded a significant increase versus the native state (+2.7 mm; P < .001). As compared with the 5-cm capsulotomy state, the shoelace suture reduced ROM in 4 of 9 tests.
Double Shoelace Suture
When compared with the native state, the double shoelace repair demonstrated significant increases in ROM in 4 of 9 tests with the largest significant differences appearing in external rotation (+5.6°; P = .040) and internal rotation (+3.3°; P < .001). In the distraction test, the double shoelace suture reflected the smallest increase in FHT (+2.3 mm; P < .001). As compared with the 5-cm capsulotomy state, the double shoelace suture significantly reduced ROM in 7 of 8 tests (all but the internal rotation test).
Quebec City Slider
When compared with the native state, the QCS yielded significant increases in ROM in 4 of 10 tests, with the largest significant differences appearing in internal rotation (+3.5°; P < .001) and abduction (+3.4° P < .001). In the distraction test, the QCS had a significant increase in FHT versus the native state (+2.7 mm; P < .001). As compared with the 5-cm capsulotomy, the QCS significantly reduced ROM in 5 of 9 tests.
Comparisons Among Repairs
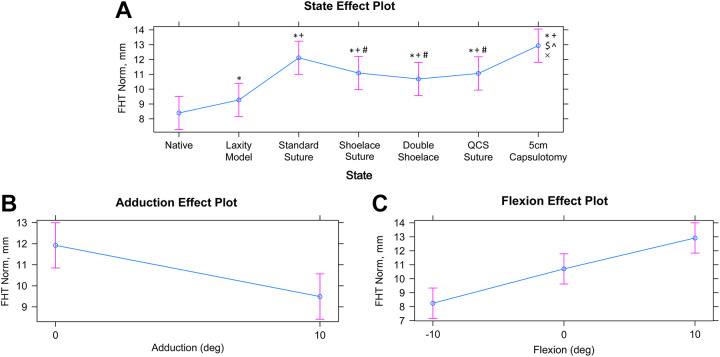
Despite the slight variations among shoelace suture, double shoelace suture, and QCS in their differences from the intact and 5-cm capsulotomy cut states, no significant differences were directly observed among these 3 repairs in any test. In contrast, the standard suture had significantly more ROM than the double shoelace suture in the flexion test (+1.41° P = .049) and from the QCS in the extension test (+5.51°; P = .014) and external rotation test (+6.03°; P = .021) (Figure 4). The standard suture also had significantly higher FHT in the distraction test than the shoelace suture (+1.0 mm; P = .005), double shoelace suture (+1.4 mm; P < .001), and QCS (+1.1 mm; P = .003) (Appendix Figure A1).
Discussion
The most important findings of this study were that a 5-cm capsulotomy with complete IFL transection caused hip joint instability during ROM and distraction testing when left untreated and that the standard suture technique did not significantly reduce this instability in any test. Repairs with standard sutures, while widely used in hip arthroscopy, may be insufficient to treat a 5-cm capsulotomy, thereby suggesting the need for more robust suture techniques.
The shoelace suture, double shoelace suture, and QCS techniques showed no significant differences from one another, and all contributed to reducing hip instability after 5-cm capsulotomy with complete transection of the IFL. Of these techniques, the QCS was the fastest and simplest to perform (although it was significantly more complex than the standard suture technique), and the double shoelace suture was the most complex and time-consuming. However, no repair restored native kinematics in the internal rotation, abduction, abduction at 45° of flexion, or distraction test, indicating that a complete return to native kinematics may not be possible prior to biological healing. Further research is necessary to investigate the potential benefits of smaller capsulotomies that partially preserve the IFL and to determine whether suture techniques involving capsular plication could fully stabilize the joint in the setting of large capsulotomies without causing loss of ROM.
In line with the results of the present study, Khair et al 15 reported that the creation of an interportal capsulotomy significantly reduced the force required for hip distraction in a cadaveric hip model. However, contrary to the present study, Khair et al showed that capsular repair with standard sutures restored hip stability, increasing the force required to distract the hip back to the native state. This difference in findings may be because of differences in the biomechanical testing setup—specifically, the biaxial load frame in position control in the Khair et al study versus the 6-degrees-of-freedom robotic arm in force control in the present study, the difference of distraction force, and the existence of a laxity model. It may also be owing to differences in the surgical technique, suture materials, and knots used; for instance, standard sutures pulled loose in 4 of 10 specimens in the present study, but all held tight in the Khair et al study.
The IFL contributes to hip joint stability as the primary static stabilizer, 28,29 as it is the strongest of the capsular ligaments and resists anterior translation and external rotation of the hip. 21 Telleria et al 26 examined an anatomic arthroscopic description of the capsular ligaments and reported that IFL runs from the 12:45 clockface position to the 3-o’clock position. This places the IFL in the path of both arthroscopic portals, with the anterolateral portal piercing the IFL just inside the lateral border and the anterior portal piercing the IFL just inside the medial border. 22 The present study showed that a 5-cm capsulotomy with complete transection of the IFL caused major hip instability. However, it is possible to perform smaller capsulotomies that partially preserve the IFL, and additional research is necessary to determine the extent of the associated benefits to hip stability.
Abrams et al 1 examined the effectiveness of complete repair of T-capsulotomy using 7 fresh-frozen cadaveric hip specimens. They observed that although a T-capsulotomy showed significantly increased external rotation when compared with an interportal capsulotomy, repairing the T-capsulotomy restored native external rotation. Further research is necessary to determine whether the type and size of the capsulotomy affect the ability to restore native biomechanics using capsular closure techniques. One of the most critical factors demonstrating poor clinical outcomes is hip instability, a characteristic associated with developmental dysplasia of the hip (DDH) or borderline DDH (BDDH). 9,24,25 Arthroscopic surgery results in increased capsular laxity and could therefore exacerbate this risk factor in patients with BDDH. 30 Kizaki et al 16 and Uchida et al 27 described that the indication of shoelace or double shoelace sutures was DDH or BDDH with capsular laxity (Beighton score >6), atraumatic instability, and hyperlaxity. However, additional research is necessary to determine the efficacy of the newly proposed suture techniques in these specific patient groups, including the option of utilizing capsular plication to tighten the capsule beyond its preoperative state.
Limitations
This study had certain limitations. Being a time-zero cadaveric study, the effects of healing are not accounted for. With the limited tests and increased specimen age (mean age, 58.1 years; range, 51-62 years), the results may not fully represent the younger patient population that typically undergoes hip arthroscopy. The simulated examinations of the hip may not replicate the manual clinical examination perfectly, especially given the lack of pain as an endpoint in cadaveric testing. Only interportal capsulotomy was investigated even though many surgeons perform a T-capsulotomy. Techniques involving capsular plication were not investigated in this study, despite the introduction of capsular laxity before creating the 5-cm capsulotomy. We used a freehand technique for capsular suture. The standard sutures pulled loose in 4 of 10 specimens, and because the order of tests was randomized, it is unknown which specific test caused the sutures to fail and when in the testing order this event occurred (it was simply observed a posteriori). However, the results from these specimens were still included in the analysis, as we believe that suture failure is an important result clinically. Future studies should be conducted to investigate clinically relevant methods for characterizing hip stability after surgical intervention and to explore the connection among ROM, distractive FHT, and clinical symptoms.
Conclusion
Hip capsule closure with the standard suture technique did not prevent postoperative hip instability after a 5-cm capsulotomy, and 3 recently developed suture techniques (Shoelace, Double Shoelace and Quebec City Slider) were preferable.
Appendix
Appendix Figure A1.
Modeled independent effect plots for 3-factor linear mixed effects models of FHT norm in millimeters. Effect plots: (A) state, (B) adduction, and (C) flexion. Dots represent model estimates for each state when adduction and flexion effects are averaged. Error bars represent 95% CIs for the estimate. *Significant from native. +Significant from laxity. #Significant from standard. $Significant from shoelace. ^Significant from double shoelace. ×Significant from QCS. FHT, femoral head translation; QCS, Quebec City slider.
Appendix Table A1.
Results of Range of Motion Testing by State
| Range of Motion, deg | |||||||
|---|---|---|---|---|---|---|---|
| Test | Native | Laxity Model | Standard Suture | Shoelace Suture | Double Shoelace Suture | Quebec City Slider Suture | 5-cm Capsulotomy |
| Flexion | |||||||
| Mean ± SD | 109.5 ± 3.2 | 110.9 ± 3.2 | 111.7 ± 3.2 | 110.5 ± 3.2 | 110.3 ± 3.2 | 110.4 ± 3.2 | 112.1 ± 3.2 |
| 95% CI | 98.4 to 120.7 | 99.8 to 122.1 | 100.6 to 122.9 | 99.3 to 121.6 | 99.2 to 121.4 | 99.3 to 121.6 | 101 to 123.3 |
| Extension | |||||||
| Mean ± SD | –19.5 ± 1.5 | –24.9 ± 1.5 | –28.4 ± 1.5 | –24.6 ± 1.5 | –23.7 ± 1.5 | –22.9 ± 1.5 | –30.9 ± 1.5 |
| 95% CI | –24.6 to –14.3 | –30.1 to –19.8 | –33.5 to –23.2 | –29.7 to –19.5 | –28.8 to –18.5 | –28.0 to –17.7 | –36.1 to –25.8 |
| Abduction | |||||||
| Mean ± SD | –30.8 ± 2.9 | –33.7 ± 2.9 | –34.6 ± 2.9 | –34.5 ± 2.9 | –33.9 ± 2.9 | –34.2 ± 2.9 | –35.2 ± 2.9 |
| 95% CI | –40.6 to –21 | –43.5 to –23.9 | –44.4 to –24.8 | –44.3 to –24.6 | –43.7 to –24.1 | –44.0 to –24.4 | –45.0 to –25.4 |
| Abduction at 45° of flexion | |||||||
| Mean ± SD | –43.3 ± 2.9 | –45.1 ± 2.9 | –46.1 ± 2.9 | –45.9 ± 2.9 | –45.5 ± 2.9 | –45.7 ± 2.9 | –46.5 ± 2.9 |
| 95% CI | –53.3 to –33.3 | –55.1 to –35.2 | –56.1 to –36.1 | –55.9 to –36 | –55.5 to –35.6 | –55.7 to –35.7 | –56.5 to –36.6 |
| Adduction | |||||||
| Mean ± SD | 16.2 ± 2.2 | 17.7 ± 2.2 | 21.7 ± 2.2 | 21.2 ± 2.2 | 20.0 ± 2.2 | 19.5 ± 2.2 | 24.3 ± 2.2 |
| 95% CI | 8.7 to 23.7 | 10.2 to 25.2 | 14.2 to 29.2 | 13.7 to 28.7 | 12.5 to 27.5 | 12 to 27 | 16.8 to 31.8 |
| External rotation | |||||||
| Mean ± SD | –32.0 ± 2.7 | –34.4 ± 2.7 | –41.2 ± 2.7 | –37.3 ± 2.7 | –37.5 ± 2.7 | –35.2 ± 2.7 | –45.3 ± 2.7 |
| 95% CI | –41.2 to –22.7 | –43.7 to –25.1 | –50.5 to –31.9 | –46.6 to –28 | –46.8 to –28.4 | –44.5 to –25.9 | –54.6 to –36 |
| Internal rotation | |||||||
| Mean ± SD | 32.3 ± 4.4 | 35.3 ± 4.4 | 35.8 ± 4.4 | 35.8 ± 4.4 | 35.6 ± 4.4 | 35.8 ± 4.4 | 36.0 ± 4.4 |
| 95% CI | 17 to 47.6 | 19.9 to 50.6 | 20.5 to 51.2 | 20.5 to 51.2 | 20.2 to 50.9 | 20.4 to 51.1 | 20.6 to 51.3 |
| Anterior impingement | |||||||
| Mean ± SD | 1.8 ± 0.5 | 1.7 ± 0.5 | 1.7 ± 0.5 | 1.7 ± 0.5 | 1.8 ± 0.5 | 1.7 ± 0.5 | 1.6 ± 0.5 |
| 95% CI | 0.1 to 3.4 | 0.1 to 3.3 | 0.1 to 3.3 | 0.1 to 3.4 | 0.1 to 3.4 | 0.1 to 3.3 | 0.01 to 3.2 |
| Log roll | |||||||
| Mean ± SD | 1.8 ± 0.6 | 1.6 ± 0.6 | 3.2 ± 0.6 | 2.0 ± 0.6 | 1.6 ± 0.6 | 2.0 ± 0.6 | 4.6 ± 0.6 |
| 95% CI | –0.3 to 3.8 | –0.4 to 3.6 | 1.2 to 5.2 | 0 to 4 | –0.4 to 3.7 | 0 to 4 | 2.6 to 6.6 |
Appendix Table A2.
Results of Distraction Testing by State
| Femoral Head Translation, mm, Mean ± SD | |||||||
|---|---|---|---|---|---|---|---|
| Abduction: Flexion, deg | Native | Laxity Model | Standard Suture | Shoelace Suture | Double Shoelace Suture | Quebec City Slider Suture | 5-cm Capsulotomy |
| 0° abduction | |||||||
| –10° flexion | 7.1 ± 1.3 | 8.1 ± 1.3 | 10.6 ± 2.5 | 9.2 ± 1.4 | 8.9 ± 1.6 | 9.2 ± 2.1 | 11.4 ± 2.9 |
| 0° flexion | 9.8 ± 0.9 | 10.6 ± 1.0 | 13.1 ± 2.4 | 12.2 ± 1.6 | 11.9 ± 1.7 | 12.1 ± 1.9 | 13.8 ± 2.8 |
| 10° flexion | 12.0 ± 0.9 | 12.9 ± 0.8 | 15.2 ± 2.3 | 14.4 ± 1.6 | 14.1 ± 1.6 | 14.4 ± 1.9 | 15.9 ± 2.7 |
| 10° abduction | |||||||
| –10° flexion | 4.7 ± 1.3 | 5.7 ± 1.2 | 9.2 ± 3.8 | 7.8 ± 1.9 | 7.0 ± 1.4 | 8.2 ± 3.9 | 10.3 ± 4.0 |
| 0° flexion | 6.5 ± 1.4 | 7.4 ± 1.4 | 10.9 ± 3.8 | 9.7 ± 2.4 | 9.3 ± 2.1 | 9.6 ± 3.2 | 11.8 ± 4.1 |
| 10° flexion | 9.0 ± 1.3 | 9.7 ± 1.4 | 12.8 ± 3.5 | 12.1 ± 2.5 | 11.6 ± 2.2 | 11.9 ± 3.0 | 13.6 ± 3.8 |
Footnotes
Final revision submitted January 6, 2022; accepted January 21, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: S.U. has received research support from Smith & Nephew and consulting fees from ConMed and Smith & Nephew. M.J.P. has received research support from Ossur, Siemens, Smith & Nephew, and Vail Valley Medical Center; consulting fees from Smith & Nephew; speaking fees from Synthes; and royalties from Arthrosurface, Bledsoe, ConMed Linvatec, DJO, and Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Abrams GD, Hart MA, Takami K, et al. Biomechanical evaluation of capsulotomy, capsulectomy, and capsular repair on hip rotation. Arthroscopy. 2015;31(8):1511–1517. [DOI] [PubMed] [Google Scholar]
- 2. Bohannon RW, Bass A. Research describing pelvifemoral rhythm: a systematic review. J Phys Ther Sci. 2017;29(11):2039–2043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bolia IK, Fagotti L, Briggs KK, Philippon MJ. Midterm outcomes following repair of capsulotomy versus nonrepair in patients undergoing hip arthroscopy for femoroacetabular impingement with labral repair. Arthroscopy. 2019;35(6):1828–1834. [DOI] [PubMed] [Google Scholar]
- 4. Canham CD, Domb BG, Giordano BD. Atraumatic hip instability. JBJS Rev. 2016;4(5):e3. [DOI] [PubMed] [Google Scholar]
- 5. Casp A, Gwathmey FW. Hip arthroscopy: common problems and solutions. Clin Sports Med. 2018;37(2):245–263. [DOI] [PubMed] [Google Scholar]
- 6. Chandrasekaran S, Vemula SP, Martin TJ, Suarez-Ahedo C, Lodhia P, Domb BG. Arthroscopic technique of capsular plication for the treatment of hip instability. Arthrosc Tech. 2015;4(2):e163–e167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Clapp IM, Nwachukwu BU, Beck EC, Jan K, Gowd AK, Nho SJ. Comparing outcomes of competitive athletes versus nonathletes undergoing hip arthroscopy for treatment of femoroacetabular impingement syndrome. Am J Sports Med. 2020;48(1):159–166. [DOI] [PubMed] [Google Scholar]
- 8. Duchman KR, Westermann RW, Glass NA, Bedard NA, Mather RC, 3rd, Amendola A. Who is performing hip arthroscopy? An analysis of the American Board of Orthopaedic Surgery Part-II Database. J Bone Joint Surg Am. 2017;99(24):2103–2109. [DOI] [PubMed] [Google Scholar]
- 9. Fukui K, Trindade CA, Briggs KK, Philippon MJ. Arthroscopy of the hip for patients with mild to moderate developmental dysplasia of the hip and femoroacetabular impingement: outcomes following hip arthroscopy for treatment of chondrolabral damage. Bone Joint J. 2015;97B(10):1316–1321. [DOI] [PubMed] [Google Scholar]
- 10. Haefeli PC, Albers CE, Steppacher SD, Tannast M, Buchler L. What are the risk factors for revision surgery after hip arthroscopy for femoroacetabular impingement at 7-year followup? Clin Orthop Relat Res. 2017;475(4):1169–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Harris JD, McCormick FM, Abrams GD, et al. Complications and reoperations during and after hip arthroscopy: a systematic review of 92 studies and more than 6,000 patients. Arthroscopy. 2013;29(3):589–595. [DOI] [PubMed] [Google Scholar]
- 12. Jackson TJ, Peterson AB, Akeda M, et al. Biomechanical effects of capsular shift in the treatment of hip microinstability: creation and testing of a novel hip instability model. Am J Sports Med. 2016;44(3):689–695. [DOI] [PubMed] [Google Scholar]
- 13. Jamil M, Dandachli W, Noordin S, Witt J. Hip arthroscopy: indications, outcomes and complications. Int J Surg. 2018;54(pt B):341–344. [DOI] [PubMed] [Google Scholar]
- 14. Kalisvaart MM, Safran MR. Hip instability treated with arthroscopic capsular plication. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):24–30. [DOI] [PubMed] [Google Scholar]
- 15. Khair MM, Grzybowski JS, Kuhns BD, Wuerz TH, Shewman E, Nho SJ. The effect of capsulotomy and capsular repair on hip distraction: a cadaveric investigation. Arthroscopy. 2017;33(3):559–565. [DOI] [PubMed] [Google Scholar]
- 16. Kizaki K, Hatakeyama A, Utsunomiya H, Philippon MJ, Uchida S. Arthroscopic double shoelace capsular plication technique for the treatment of borderline hip dysplasia associated with capsular laxity. Arthrosc Tech. 2019;8(8):e923–e927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Levy DM, Grzybowski J, Salata MJ, Mather RC, 3rd, Aoki SK, Nho SJ. Capsular plication for treatment of iatrogenic hip instability. Arthrosc Tech. 2015;4(6):e625–e630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Locks R, Bolia I, Utsunomiya H, Briggs K, Philippon MJ. Current concepts in revision hip arthroscopy. Hip Int. 2018;28(4):343–351. [DOI] [PubMed] [Google Scholar]
- 19. Menge TJ, Chahla J, Soares E, Mitchell JJ, Philippon MJ. The Quebec City slider: a technique for capsular closure and plication in hip arthroscopy. Arthrosc Tech. 2016;5(5):e971–e974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Murata Y, Uchida S, Utsunomiya H, Hatakeyama A, Nakamura E, Sakai A. A comparison of clinical outcome between athletes and nonathletes undergoing hip arthroscopy for femoroacetabular impingement. Clin J Sport Med. 2017;27(4):349–356. [DOI] [PubMed] [Google Scholar]
- 21. Myers CA, Register BC, Lertwanich P, et al. Role of the acetabular labrum and the iliofemoral ligament in hip stability: an in vitro biplane fluoroscopy study. Am J Sports Med. 2011;39:85s–91s. [DOI] [PubMed] [Google Scholar]
- 22. Ortiz-Declet V, Mu B, Chen AW, et al. Should the capsule be repaired or plicated after hip arthroscopy for labral tears associated with femoroacetabular impingement or instability? A systematic review. Arthroscopy. 2018;34(1):303–318. [DOI] [PubMed] [Google Scholar]
- 23. Prather H, Harris-Hayes M, Hunt DM, Steger-May K, Mathew V, Clohisy JC. Reliability and agreement of hip range of motion and provocative physical examination tests in asymptomatic volunteers. PM R. 2010;2(10):888–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sardana V, Philippon MJ, de Sa D, et al. Revision hip arthroscopy indications and outcomes: a systematic review. Arthroscopy. 2015;31(10):2047–2055. [DOI] [PubMed] [Google Scholar]
- 25. Sharfman ZT, Grundshtein A, Paret M, Amit L, Amar E, Rath E. Surgical technique: arthroscopic osteoplasty of anterior inferior iliac spine for femoroacetabular impingement. Arthrosc Tech. 2016;5(3):e601–e606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Telleria JJ, Lindsey DP, Giori NJ, Safran MR. A quantitative assessment of the insertional footprints of the hip joint capsular ligaments and their spanning fibers for reconstruction. Clin Anat. 2014;27(3):489–497. [DOI] [PubMed] [Google Scholar]
- 27. Uchida S, Pascual-Garrido C, Ohnishi Y, et al. Arthroscopic shoelace capsular closure technique in the hip using UltraTape. Arthrosc Tech. 2017;6(1):e157–e161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. van Arkel RJ, Amis AA, Cobb JP, Jeffers JR. The capsular ligaments provide more hip rotational restraint than the acetabular labrum and the ligamentum teres: an experimental study. Bone Joint J. 2015;97B(4):484–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Walters BL, Cooper JH, Rodriguez JA. New findings in hip capsular anatomy: dimensions of capsular thickness and pericapsular contributions. Arthroscopy. 2014;30(10):1235–1245. [DOI] [PubMed] [Google Scholar]
- 30. Wilkin GP, Ibrahim MM, Smit KM, Beaule PE. A contemporary definition of hip dysplasia and structural instability: toward a comprehensive classification for acetabular dysplasia. J Arthroplasty. 2017;32(9):S20–S27. [DOI] [PubMed] [Google Scholar]
- 31. Yeung M, Memon M, Simunovic N, Belzile E, Philippon MJ, Ayeni OR. Gross instability after hip arthroscopy: an analysis of case reports evaluating surgical and patient factors. Arthroscopy. 2016;32(6):1196–1204.e1191. [DOI] [PubMed] [Google Scholar]