Abstract
Purpose
Femoral neck fractures (FNF) in adults are conventionally managed with surgical options. This paper is aimed to assess the safety, and functional outcomes of the novel Femoral neck system (FNS) for FNF treatment in adult population.
Methods
An organized quest of four literature databases (PubMed, Scopus, Web of Science, and Cochrane Library) was performed on March 1, 2022 using the term “femoral neck system”. Fixed or random-effect meta-analysis was used to analyse the outcome measures after selecting relevant studies and assessing their quality. Heterogeneity was considered when calculating pooled effect sizes and 95% confidence ranges.
Results
On comparing FNS with cannulated cancellous screws (CCS) or other methods, in a total of 762 patients (351 FNS and 411 CCS) in the 11 comparative studies considered for meta-analysis, blood loss was pointedly higher overall in the FNS group, mean difference 115.77 ml; 95% CI 3.11 ml, 28.42 ml; test of overall effect: z = 1.68, p = 0.09); with considerable heterogeneity. However, in the FNS group the operative time was substantially lower (Mean difference −7.91 min; 95% CI -15.01, −0.80; test of overall effect: z = 2.18, p = 0.03, with marked heterogeneity). Moreover, complications such as infections, non-union, osteonecrosis, implant cut-out were significantly lower in the FNS group with a Mantel Haenszel Odds ratio of 0.20 (95% CI 0.12, 0.34: Z = 6.01, p < 0.0001).
Conclusion
Keeping in mind the heterogenicity of the studies, -management of adult patients with FNF with FNS can provide results comparable to traditional fixation methods with significantly lower rate of complications.
Keywords: Hip fracture, Femoral neck fracture, Surgical management, Operative time, Complications, Outcomes
1. Introduction
Hip fractures are common injuries, with a substantial socio-economic burden both to patients and healthcare systems. Worldwide there are 1.6 million hip fractures with care provided to 63,284 people in the United Kingdom (UK) according to National Hip Fracture Database (NHFD).1,2 These figures are projected to rise to more than 6 million by 2050 worldwide.3
Femoral neck fractures (FNFs) account for roughly 50% of all hip fractures.4 FNFs have a higher incidence in elderly osteoporotic patients following simple falls, with multiple established treatment guidelines well documented in the literature, based on the fracture pattern and physiological assessment.5, 6, 7, 8, 9, 10 FNFs in the younger patient are less common, frequently manifests after high-energy trauma, with other associated injuries and management of such cases pose a great challenge to orthopaedic surgeons.11 The goals of treating FNFs in physiologically young individuals include preserving natural hip architecture, lowering the risk of osteonecrosis (AVN), and preventing non-union of femoral neck.4,12 Many different surgical devices have therefore been established and utilised to achieve the latter, with inconsistencies in the literature regarding the best treatment protocol.13 Often, this is based on the nature of the fracture and surgeon's preference.14 That being said, the efficacy of different surgical devices has been well documented in the literature.15, 16, 17, 18 The most common approach to fixing FNFs in younger patients is using cancellous cannulated screws (CCS), or in more unstable/comminuted fracture patterns, a Sliding Hip Screw (SHS) fixation may be favoured.13, 14, 15, 16
More recently, a novel, minimally invasive implant, known as the femoral neck system (FNS) has come into play, forming major advances in the treatment of FNFs. The FNS, established by DePuy Synthes®, Zuchwil, Switzerland, is designed to using a minimally invasive insertion approach, improved angular stability, and the possibility of extra intraoperative compression (if required) and postoperative dynamization across the fracture site.19
2. Materials and methods
2.1. Protocol and registration
PROSPERO (registration number: CRD42021278373; title: “Femoral neck system and its comparison with cannulated cancellous screws for fixation of femoral neck fractures: a systematic review and meta-analysis)”.
2.2. Eligibility criteria
We included studies involving FNF treated with the FNS. There were no restrictions on the types of study. All comparative studies were considered for meta-analysis, as feasible. Letters to the editors, commentaries, experimental studies, studies unrelated to femoral neck system and biomechanical studies were excluded for the purpose of qualitative summarisation. We also excluded preliminary studies, abstract-only papers and those without a full-text.
2.3. Data sources, literature search, study identification
A systematic search of four electronic medical databases (PubMed, Scopus, Web of Science, and Cochrane Library) was undertaken using the search term of “femoral neck system". The list of bibliography of the articles was also screened. Bibliographic references were then fed into EndNote web application to check for duplication, compilation and subsequent manual selection. The last date searched was March 1, 2022. We did not contact the authors for any additional information.
2.4. Information abstraction
Individually, two co-authors (KPI and MKP) conducted the searches, inspected the titles of the articles including their abstract sections, and appraised these. The whole content of studies that were possibly suitable for inclusion were individually examined. Any discrepancy was resolved by shared discussion and discussion with the senior co-author (VJ). A second round of screening was done by reviewing the full-text articles of the selected studies. For nonrandomised comparative studies, Newcastle and Ottawa scale was used for assessment of risk of bias. The senior co-author (VJ) used mutual arbitration to settle disagreements amongst reviewers on the risk of bias.
2.5. Statistical analysis
The findings from the included research were compiled into a narrative synthesis. Narrative data on patient attributes was compiled. For continuous variables, the median (range) or mean (standard deviation) were used to summarise the data, whereas for categorical variables, frequency/percentage were utilised. Predesigned forms were used for data extraction. Age, sex, operative time, blood loss, functional outcome (Harris Hip Score), and complications (non-union, osteonecrosis, implant cut-out etc.) were recorded for both groups (i.e., those treated with FNS and those treated with CCS and other methods).
The chi square and I2 statistics were used for analysing the heterogeneity in effect measurements between the studies. Data were statistically pooled using either a random-effects meta-analysis (Der Simonian and Laird technique) or a fixed-effect meta-analysis (if I2 was less than 50%, a fixed-effect model was used, and if I2 was greater than 50%, a random-effects model was used). Forest plots and funnel plots were created that were suitable. Subgroup analyses were performed as per the age-group of the patients reported in studies. Pooled odds ratios (for categorical data) and Mean differences with 95% confidence intervals (for continuous data) were presented, along with those derived from each of the subgroups. Statistical significance was considered as a two-sided P value of less than of 0.05.
3. Results
3.1. Literature search
The PRISMA flow diagram has been shown in Fig. 1. The preliminary search generated 22 articles on PubMed, 28 on Scopus (All Fields), and 13 on Web of Science. No additional paper was found in the Cochrane library (All Text). Following the screening of duplicates and the exclusion of irrelevant articles based on title, 27 publications were considered for full text evaluation, and finally 27 papers were considered for this systematic review, all of which were published between 2021 and 2022. 11 papers reporting studies comparing FNS with other methods (including CCS) of femoral neck fracture stabilization were considered for qualitative summarisation of available data and meta-analysis.
Fig. 1.
Flow chart as per PRISMA guidelines.
3.2. Characteristics of the studies
The (Table 1, Table 2, Table 3) describes summary of the published studies.20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30 Nine studies were from China, and one each from Japan and Switzerland. A total of 762 patients (351 FNS and 411 CCS) were analyzed in the 11 comparative studies considered for meta-analysis. Two studies reported data from elderly cases only (one by Nabe Y et al. reported-on patients aged more than 65 years and another by Vazquez O et al. on patients aged more than 75 years), whereas seven studies (by Hu H et al., Zohu X et al., He C et al., Yan C et al., Yang J et al., Yang Y et al. and Zhang Y et al.) reported data on young patients (<65 years) only.
Table 1.
Characteristics, Demographics and findings of included studies on FNS.
| Authors/Year | Study Period/Country of study | Mean Age (Range in Years) Gender (Male Vs Female) |
Femoral neck system (FNS) usage | Other Implants used | Conclusion of the study | |
|---|---|---|---|---|---|---|
| 1 | Zhang Y et al., 2022 | 2019–2020 China |
54.9(28–66) years, 26 M 43F | 33 | 36 | FNS application linked to minimal surgical trauma, improved stability, and lesser complication |
| 2 | He C et al., 2021 | 2018–2020 China |
50.61 ± 10.30 vs 47.58 ± 10.31 years (18 M,15F vs 22 M,14F) |
33 | 36 | Compared to CS, the FNS decreased the frequency of peroperative imaging's, radiation exposure, and early complications such as shortening of the femoral neck and its nonunion. |
| 3 | Hu H et al., 2021 | 2017–2020 China |
50.45 ± 8.45 26 M vs 18F |
20 | 24 | FNS has a higher construct stability. No significant difference in the probability of AVN. Cut-out of screw and shortening of the neck was significantly lower in FNS group than in CCS group |
| 4 | Nibe Y et al., 2021 | 2006–2020 Japan |
79.5 11 M vs 41F |
25 | 27 | In older patients with Femoral neck fractures, FNS had a shorter operative duration and a reduced revision surgery. |
| 5 | Tang Y et al., 2021 | 2019–2020 China |
56.1 71 M vs 21F |
47 | 45 | FNS was comparable to CCS with regards to surgical time, length of incision, intraoperative blood loss, and complications. However, FNS group had better Harris hip score, shorter fracture healing time, and lesser neck shortening |
| 6 | Vazquez O et al., 2021 | 2015–2019 Switzerland |
84.9 ± 6.4 12 M vs 51F |
15 | 48 | FNS had significantly lower surgical duration and had equal efficacy to DHS and CCS |
| 7 | Zhou X et al., 2021 | 2019 China |
53.84 24 M vs 36F |
30 | 30 | FNS was costlier however more appropriate for treating Pauwels type-3 fractures as compare to CCS and had lesser soft tissue trauma speedy recovery lesser complication. |
| 8 | Yan C et al., 2021 | 2018–2020 China |
52(47–63)yrs vs 49(47–56)yrs, (10 M,14F vs 38 M,20F) | 24 | 58 | FNS could lead to faster fracture healing and rehabilitation, thereby reducing complications. |
| 9 | Yang J et al., 2021 | 2019–2020 China |
(47.8 ± 9.8) yrs vs (43.7 ± 13.1) yrs, (30 M,17F vs 26 M,21F) | 47 | 47 | Compared with CCS fixation, FNS fixation shortened operative time and fracture healing time, allowed patients to ambulate early after surgery, and better functional recovery of the hip(HHS). |
| 10 | Yang Y et al., 2021 | 2019–2020 China |
NA | 15 | 19 | Compared with CCS, FNS can reduce surgical trauma, intraoperative fluoroscopy frequency and obtain satisfactory short-term effectiveness. |
| 11 | Wei X et al., 2021 | 2019–2020 China |
(54 ± 13) yrs vs (53.2 ± 11.3) yrs, (38 M,24F vs 42 M,15F) | 62 | 57 | In comparison to CCS, FNS can significantly decreased intraoperative C arm exposure duration, reduced surgical and inpatient time. FNS fastened the fracture healing and promoted better functional recovery. |
Abbreviations: CCS= Cancellous Cannulated system; FNS= Femoral neck system; TS = Triple screw construct.
Table 2.
Operative, peri-operative parameters, Blood transfusion requirements, length of stay, follow-up and complications in patients undergoing FNS in the analysed studies.
| Authors/Year | Operative Time (in Minutes) | Peri-operative blood Loss (in millilitres) | Non-Union/Femoral Head Necrosis/Cut out etc. | Follow-up period (months) | Blood Transfusion | Length of stay (in days) | |
|---|---|---|---|---|---|---|---|
| 1 | Hu H et al., 2021 | 79.75 ± 26.35 | 69.45 ± 50.47 | 5 Patients | 12 | N/A | N/A |
| 2 | Nibe Y et al., 2021 | 42 ± 13 | 36 ± 25 | 0 | 13 | N/A | N/A |
| 3 | Tang Y et al., 2021 | 52.4 ± 11 | 50.6 ± 10.6 | 6 | >12 | N/A | N/A |
| 4 | Vazquez O et al., 2021 | 43.3 ± 10.1 | N/A | N/A | N/A | 1 | 10.3 |
| 5 | Zhou X et al., 2021 | 42.83 ± 4.69 | 99.73 ± 52.73 | 2 | Oct-22 | N/A | 5.07 ± 1.31 |
| 6 | Zhang Y et al., 2022 | 60 ± 12.44 | 13.7 ± 8.02 | Varus tilt 1, neck shortening 2 | 6 months | 7.57 ± 2.39 | |
| 7 | He C et al., 2021 | 49.94 ± 14.96 | NA | 1 cutout, 1 neck shortening | 12–24 months | NA | 5.12 ± 1.88 |
| 8 | Yan C et al., 2021 | 58.92 ± 6.97 | 79.17 ± 50.17 | 2 neck shortening | 3–12 months | NA | NA |
| 9 | Yang J et al., 2021 | 47.7 ± 9.4 | NA | NA | NA | NA | NA |
| 10 | Yang Y et al., 2021 | 39.4 ± 6.3 | 52.4 ± 10.4 | 1 unsatisfactory reduction, 2 neck shortening | NA | NA | NA |
| 11 | Wei X et al., 2021 | 45.2 ± 10.1 | NA | NA | NA | NA | NA |
Abbreviations: NA= Not available.
Table 3.
Operative, peri-operative parameters, Blood transfusion requirements, length of stay, follow-up and complications in patients undergoing CCS system in the analysed studies.
| Authors/Journal/Year of Publication | Operative Time (in Minutes) | Peri-operative blood Loss (in millilitres) | Non-Union/Femoral Head Necrosis/Cut out etc | Follow-up period (months) | Blood Transfusion | Length of stay (in days) | |
|---|---|---|---|---|---|---|---|
| 1 | Hu H et al., 2021 | 64.58 ± 18.56 | 23.71 ± 28.13 | 21 | 12 | N/A | N/A |
| 2 | Nibe Y et al., 2021 | 53 ± 21 | 41 ± 40 | 6 | 24 | N/A | N/A |
| 3 | Tang Y et al., 2021 | 42 ± 11.9 | 47.3 ± 9.3 | 12 | >12 | N/A | N/A |
| 4 | Vazquez O et al., 2021 | 68.8 | N/A | N/A | N/A | 1 | 12.3 |
| 5 | Zhou X et al., 2021 | 40.9 ± 5.22 | 30.27 ± 9.04 | 9 | Oct-22 | N/A | 5.33 ± 1.52 |
| 6 | Zhang Y et al., 2022 | 76.81 ± 13.31 | 16.58 ± 4.16 | Varus tilt 4. Neck shortening 5, need for implat removal 5 | 6 months | NA | 8.50 ± 1.95 |
| 7 | He C et al., 2021 | 56.11 ± 12.48 | NA | 2 non union, 2 nail retrest, 3 neck shortening, 2 cut out | 12–24 months | NA | 4.78 ± 1.55 |
| 8 | Yan C et al., 2021 | 88.38 ± 37.6 | 74.83 ± 42.73 | 2 osteonecrosis, 1 nonunion, 13 neck shortening | 6–18 months | NA | NA |
| 9 | Yang J et al., 2021 | 66.1 ± 3.8 | NA | NA | NA | NA | NA |
| 10 | Yang Y et al., 2021 | 41.6 ± 12.1 | 34.8 ± 26.0 | 1 unsatisfactory reduction, 1 implant cutout, 4 neck shortening | NA | NA | NA |
| 11 | Wei X et al., 2021 | 51.8 ± 11.7 | NA | NA | NA | NA | NA |
Abbreviations: NA= Not available.
3.3. Meta-analysis of primary studies comparing FNS with CCS or other fixation methods
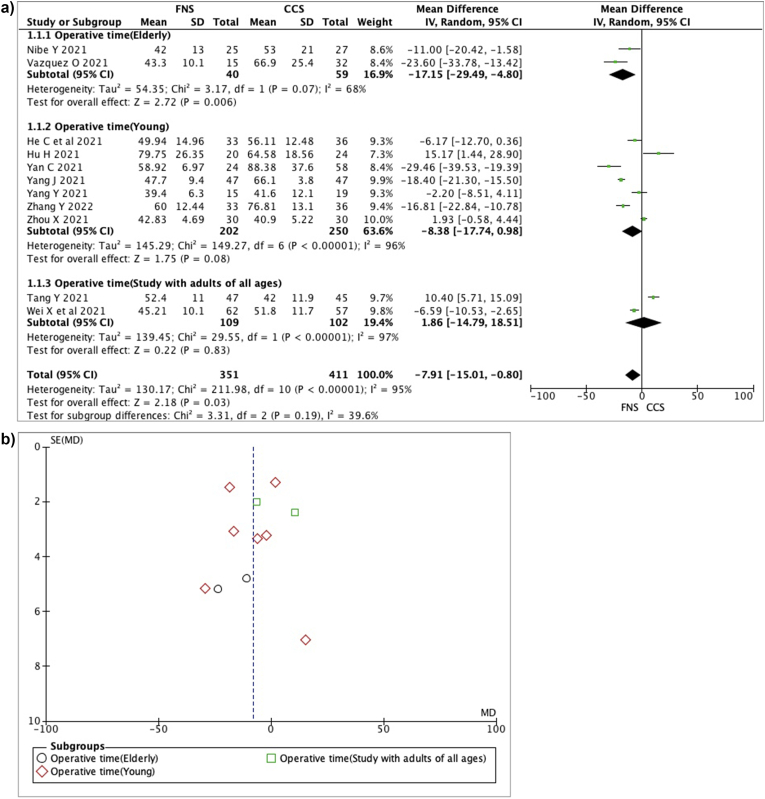
a) Surgical duration: On metanalysis of available data in the 11 studies; significantly lower operative time was observed in the FNS group, as compared to the CCS group (Mean difference −7.91 min; 95% CI -15.01 min, −0.80 min; test of overall effect: z = 2.18, p = 0.03). There was a considerable heterogeneity amongst the studies (Chi square = 211.98, p < 0.0001, I2 = 95%) requiring the further analysis. Moreover, the operative time was significantly lower in the FNS group, as compared to other group in the metanalysis of 2 studies on elderly patients (Mean difference −17.15 min; 95% CI -29.49 min, −4.80 min; test of overall effect: z = 2.72, p = 0.006). The test for subgroup difference was not significant with Chi square-3.31, I2 = 39.6%, p = 0.19. No funnel plot asymmetry was observed, indicating lack of publication bias (Egger's test; Z = −0.345, p = 0.73). (Fig. 2A and B).
Fig. 2.
A. Figure showing operative time (in min) forest plot, B. Funnel plot.
b) Blood loss: On metanalysis of available data assessing blood loss in the 7 studies; significantly higher blood loss was observed in the FNS group, as compared to the CCS group; mean difference 15.41 ml; 95% CI 3.99 ml, 26.83 ml; test of overall effect: z = 2.64, p = 0.008); and there was a considerable heterogeneity among both the studies (Chi square = 73.57, I2 = 92%, p < 0.00001). No significant subgroup differences were observed. (Fig. 3A and B).
Fig. 3.
A. Figure showing blood loss utilizing Forest plot (in ml) found in the studies, B. Funnel Plot.
c) Complications: Infections, non-union, osteonecrosis, implant cut-out, and other problems were compared between the two groups, and the number of complications was shown to be significantly lower in the FNS group overall. In the metanalysis of 7 studies reporting relevant data regarding complications (total 23 complications out of 227 FNS cases) versus other group (total 93 complications out of 275 cases), we found a Mantel Haenszel Odds ratio (MH-OR) of 0.20 (95% CI 0.12, 0.34; Z = 6.01, p < 0.0001; and Chi square = 7.07, p = 0.42, I2 = 1%; so fixed effects model was used). No significant subgroup effect was observed. (Fig. 4A and B).
Fig. 4.
A. Complications shown in a Forest plot., B. Funnel Plot.
d) Harris hip score: On metanalysis of 7 studies presenting relevant data on Harris hip score (HHS), significantly higher HHS was observed at last follow up. Data presented in the FNS group, as compared to the CCS group showed a mean difference of 8.55; 95% CI 3.10, 14.00; and a test of overall effect: z = 3.08, p = 0.002). There was a considerable heterogeneity among both the studies (Chi square = 222.58, I2 = 97%, p < 0.00001), so random effects model was used. (Fig. 5A and B).
Fig. 5.
A. Forest plot showing Harris hip score B. Funnel Plot.
e) Length of stay: On metanalysis of 4 studies presenting relevant data no significant difference was observed in length of hospital stay between the FNS group and the CCS group; mean difference −0.23; 95% CI -0.70, 0.25; test of overall effect: z = 0.93, p = 0.35); and there no significant heterogeneity amongst the studies (Chi square = 4.41, I2 = 32%, p = 0.22), so fixed effects model was used. (Fig. 6).
Fig. 6.
Forest plot showing length of stay.
f) Fluoroscopy time: On metanalysis of 4 studies presented number of time fluoroscopies used, a significantly lower frequency was found in the FNS group as compared to CCS group, mean difference −8.47; 95% CI -10.02, −6.92; test of overall effect: z = 10.72, p < 0.00001); with significant heterogeneity amongst the studies (Chi square = 15.44, I2 = 81%, p = 0.001), so random effects model was used (Fig. 7).
Fig. 7.
Forest plot showing Fluoroscopy time frequency.
g) Fracture healing time: Fracture heling time was significantly lower in FNS group On metanalysis of 5 studies presenting relevant data; standardised mean difference(SMD) −1.05, 95% CI -2.03, −0.08; test of overall effect: z = 2.11, p = 0.03); with significant heterogeneity amongst the studies (Chi square = 70.41, I2 = 94%, p < 0.00001), so random effects model was used, SMD was used as some studies by reported healing time in weeks and others in months(Fig. 8).
Fig. 8.
Healing time on Forest plot.
5.Study quality: As per Newcastle and Ottawa scale the study by Zhu X et al. had a score of 8, the studies by He C et al., Hu h et al. and Tang Y has a score of 7. The rest of studies under consideration had a score of 6. The preoperative matching was performed only in study by Zhu X et al.
4. Discussion
In younger patients with FNF, closed or open reduction with internal fixation is still the recommended therapeutic option, as preserving the femoral head remains a primary goal.31, 32, 33 The ideal implant for fixation of FNF in adult patients has always posed a challenge to orthopaedic surgeons, across the world. Currently, CCS and Sliding hip screw (SHS) fixations have been the mainstay treatment to fix these fractures, with variable outcomes reported in the literature. SHS also called dynamic hip screw (DHS) implants are known to be more biomechanically stable and utilised in displaced/unstable (Pauwels II-III, posterior comminution) and basicervical pattern of fractures. CCS is less intrusive and more commonly used in Pauwels I or minimally displaced fractures.34 However, these implants are not without complications, which may involve implant failure, non-union and avascular necrosis of the femoral head often requiring revision surgery.35
A novel implant, the FNS, has been innovated, with the aim to provide a minimally invasive and biomechanically stable fixation of FNFs. The implant is ingeniously devised and includes a small side plate that rests on the femoral shaft. The plate provides angular stability and designed to provide a minimized implant footprint. The shaft plate has a proximal cylindrically designed bolt to allow the passage of Antirotation-Screw (ARScrew) and deliver guided collapse. The whole construct thus provides an angular and rotationally stable construct by allowing the screw to slide, along the barrel plate for a controlled dynamic impaction.36 FNS thus aims to combine the advantages of both dynamic hip screw system and cannulated cancellous screw system. Several studies have focused on ascertaining the biomechanical stability of the FNS,16,19,20,37 demonstrating an overall exceptional biomechanical performance and a significantly higher construct stability when compared to the CCS, with somewhat comparable results with DHS fixation. On biomechanical testing, Stoffel K et al. discovered that Internal fixation with three CCS is inferior to FNS in terms of overall structural stability.16 In comparison to Hansson Pins, Schopper et al. found that FNS demonstrated greater resistance and improved stability to varus deformation in the management of FNF.19 Furthermore, a recent finite element study utilising FNS on Pauwels type III FNF found that positioning the bolt tip towards the subchondral bone increases stability. With caudal placement, the interfragmentary sliding distance, shear and compressive, stress all increased.38 However, another recent biomechanical analysis has found that FNS may not as stable as reported earlier.39
Recently however, the focus has shifted towards the clinical outcomes of the FNS, which are equally as important to understand. This systematic review evaluates the quantifiable outcomes of the FNS vs other models used to fix FNFs.
Clinical outcomes of the FNS are governed by a multitude of variables including procedure time, intraoperative blood loss, post-operative functional outcomes, and risk of post-operative complications. Overall, our results showed a significant decrease in the rate of complications associated with the FNS when compared to CCS, correlating well with the literature.20,28,40 However, despite this, a few recent studies have illustrated a higher rate of reoperations, avascular necrosis and cut-out of devices in adults more than 65 years of age stabilized by FNS therefore, it was concluded that age greater than 65 years may be considered as an exclusion regarding patient selection while using FNS.28,40 Also, our metanalysis showed that significantly higher Harris hip score (HHS) was achieved in the FNS group, as compared to the CCS group.
Another major advantage of the FNS was that it allowed patients to start early rehabilitation, physiotherapy and weight bearing, furthermore, improving functional outcomes. Studies have shown an improvement in the post-operative VAS scores, and high Harris scores at the last follow up. This likely to be related rate of fracture healing, occurring earlier with the FNS in comparison to other fixation constructs.28
It is a consensus that prolonged operative durations is related with a higher chance in the risk of complications, and surgeons should always aim to reduce the surgical timings41 Our study revealed that the operative time was substantially lower in the FNS group. Moreover, the operative time was found to be even more shorter in the FNS group when compared to other group in the metanalysis of 2 studies on elderly patients.
Furthermore, the standard approach utilised for insertion of the FNS is like that of the DHS, although less invasive and usually incorporates an incision that is much smaller in length; a direct lateral incision starting a few centimetres proximal to the central axis of femoral neck. To reach the femur, several structures, including the fascia and muscle must be split. Hence, it is not uncommon to encounter bleeding. Theoretically speaking, this is usually more than bleeding encountered during a CCS procedure, which is often done using a percutaneous approach.42,43 Our meta-analysis also revealed that the CCS group had lower blood loss while the FNS group had increased blood loss, correlating well with the literature, despite the fact that there was a trend for less blood loss, in the study by Nibe Y et al. on elderly patients in the FNS group.21 Moreover, a recent retrospective comparative study has shown that the use of FNS is linked to a reduction in surgical trauma, lesser blood loss, lesser radiation exposure for patients and staff, stouter stability, and decreased post-operative complications such as shortness and varus tilt of femoral neck, and implant removal incidences than CCS treatment, in young patients authors suggested that in femoral neck fractures, FNS could be a viable treatment option.26 A recent case series of 34 patients treated with femoral neck system demonstrated that the FNS has the potential to be both safe and effective. Failures were higher in patients aged more than 65 years and females. According to the authors, age (65 years) is a significant aspect to consider while choosing patients for CRIF because it is linked to a decreased probability of failure.40 In contrast, a latest study indicated that FNS is more effective than hemiarthroplasty in elderly patients with undisplaced neck femur fractures, and the authors recommend it as a treatment choice for these individuals.44
5. Limitations
We do acknowledge limitations to this study. First, it is important to highlight the quite a smaller number of papers included in this review with significant heterogeneity. Moreover, since the FNS fixation is somewhat novel, the follow up time was variable and, in most studies, it was relatively short, which may have an impact on the assessment of clinical outcomes.
6. Conclusion
This systematic review and metanalysis highlights the clinical efficacy of FNS in comparison to other modes of fixation for FNF based on the most up to date available studies. These studies have revealed an overall improvement in perioperative and postoperative complication rates, Harris Hip Scores, fracture healing time, with a generally superior functional outcome compared to other fixation methods. No statistically significant difference was noted with respect to procedure time and intraoperative blood loss on meta-analysis. Further, larger multicentre randomised controlled studies with longer lengths of follow-up periods are necessary to corroborate our findings.
Ethical approval
The current submitted article is not a clinical study and does not involve any patients.
Authors contributions
VKJ, MKP, SS, RB and AS involved in Conceptualization, literature search, manuscript writing and editing. AS, MKP, VKJ and KPI Literature search, manuscript writing, references, data analysis and editing. All authors read and agreed the final draft submitted.
Funding
None.
Declaration of competing interest
The authors declare no conflict of interest.
Contributor Information
Ahmed Saad, Email: ahmed.saad3@nhs.net.
Mohit Kumar Patralekh, Email: mohitkumarpatralekh@gmail.com.
Vijay Kumar Jain, Email: drvijayortho@gmail.com.
Sagaurav Shrestha, Email: sagaurav.shrestha@nhs.net.
Rajesh Botchu, Email: drbrajesh@yahoo.com.
Karthikeyan. P. Iyengar, Email: kartikp31@hotmail.com.
References
- 1.Johnell O., Kanis J.A. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int. Nov. 2004;15(11):897–902. doi: 10.1007/s00198-004-1627-0. [DOI] [PubMed] [Google Scholar]
- 2.National hip fracture database (NHFD) annual report 2021. Royal college of physicians. https://www.rcplondon.ac.uk/projects/outputs/national-hip-fracture-database-nhfd-annual-report-2021 Available at:
- 3.Cooper C., Campion G., Melton L.J., 3rd Hip fractures in the elderly: a world-wide projection. Osteoporos Int. Nov. 1992;2(6):285–289. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 4.Pauyo T., Drager J., Albers A., Harvey E.J. Management of femoral neck fractures in the young patient: a critical analysis review. World J Orthop. 2014;5(3):204–217. doi: 10.5312/wjo.v5.i3.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roberts K.C., Brox W.T., Jevsevar D.S., Sevarino K. Management of hip fractures in the elderly. J Am Acad Orthop Surg. Feb. 2015;23(2):131–137. doi: 10.5435/JAAOS-D-14-00432. [DOI] [PubMed] [Google Scholar]
- 6.Szita J., Cserháti P., Bosch U., Manninger J., Bodzay T., Fekete K. Intracapsular femoral neck fractures: the importance of early reduction and stable osteosynthesis. Injury. Dec. 2002;33(Suppl 3):C41–C46. doi: 10.1016/s0020-1383(02)00330-3. [DOI] [PubMed] [Google Scholar]
- 7.Krischak G., Beck A., Wachter N., Jakob R., Kinzl L., Suger G. Relevance of primary reduction for the clinical outcome of femoral neck fractures treated with cancellous screws. Arch Orthop Trauma Surg. Oct. 2003;123(8):404–409. doi: 10.1007/s00402-003-0571-3. Epub 2003 Aug 12. [DOI] [PubMed] [Google Scholar]
- 8.Heetveld M.J., Raaymakers E.L., Luitse J.S., Gouma D.J. Rating of internal fixation and clinical outcome in displaced femoral neck fractures: a prospective multicenter study. Clin Orthop Relat Res. Jan. 2007;454:207–213. doi: 10.1097/01.blo.0000238867.15228.8d. PMID: 17031315. [DOI] [PubMed] [Google Scholar]
- 9.Estrada L.S., Volgas D.A., Stannard J.P., Alonso J.E. Fixation failure in femoral neck fractures. Clin Orthop Relat Res. Jun. 2002;(399):110–118. doi: 10.1097/00003086-200206000-00013. PMID: 12011699. [DOI] [PubMed] [Google Scholar]
- 10.Gjertsen J.E., Vinje T., Engesaeter L.B., et al. Internal screw fixation compared with bipolar hemiarthroplasty for treatment of displaced femoral neck fractures in elderly patients. J Bone Joint Surg Am. Mar. 2010;92(3):619–628. doi: 10.2106/JBJS.H.01750. PMID: 20194320. [DOI] [PubMed] [Google Scholar]
- 11.Protzman R.R., Burkhalter W.E. Femoral-neck fractures in young adults. J Bone Joint Surg Am. Jul. 1976;58(5):689–695. PMID: 932067. [PubMed] [Google Scholar]
- 12.Ly T.V., Swiontkowski M.F. Treatment of femoral neck fractures in young adults. Instr Course Lect. 2009;58:69–81. [PubMed] [Google Scholar]
- 13.Slobogean G.P., Sprague S.A., Scott T., McKee M., Bhandari M. Management of young femoral neck fractures: is there a consensus? Injury. Mar. 2015;46(3):435–440. doi: 10.1016/j.injury.2014.11.028. Epub 2014 Nov 27. [DOI] [PubMed] [Google Scholar]
- 14.Fletcher J.W.A., Sommer C., Eckardt H., Knobe M., Gueorguiev B., Stoffel K. Intracapsular femoral neck fractures-A surgical management algorithm. Medicina (Kaunas) 2021;57(8):791. doi: 10.3390/medicina57080791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen C., Yu L., Tang X., et al. Dynamic hip system blade versus cannulated compression screw for the treatment of femoral neck fractures: a retrospective study. Acta Orthop Traumatol Turc. Oct. 2017;51(5):381–387. doi: 10.1016/j.aott.2017.07.006. Epub 2017 Aug 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stoffel K., Zderic I., Gras F., Sommer C., Eberli U., Mueller D. Biomechanical evaluation of the femoral neck system in unstable Pauwels III femoral neck fractures: a comparison with the dynamic hip screw and cannulated screws. J Orthop Trauma. 2017;31(3):131–137. doi: 10.1097/BOT.0000000000000739. [DOI] [PubMed] [Google Scholar]
- 17.Panteli M., Rodham P., Giannoudis P.V. Biomechanical rationale for implant choices in femoral neck fracture fixation in the non-elderly. Injury. 2015;46(3):445–452. doi: 10.1016/j.injury.2014.12.031. [DOI] [PubMed] [Google Scholar]
- 18.Slobogean G.P., Sprague S.A., Scott T., Bhandari M. Complications following young femoral neck fractures. Injury. Mar; 2015;46(3):484–491. doi: 10.1016/j.injury.2014.10.010. Epub 2014 Oct 31. [DOI] [PubMed] [Google Scholar]
- 19.Schopper C., Zderic I., Menze J., et al. Higher stability and more predictive fixation with the Femoral Neck System versus Hansson Pins in femoral neck fractures Pauwels II. J Orthop Translat. 2020:88–95. doi: 10.1016/j.jot.2020.06.002. Jul 22;24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hu H., Cheng J., Feng M., Gao Z., Wu J., Lu S. Clinical outcome of femoral neck system versus cannulated compression screws for fixation of femoral neck fracture in younger patients. J Orthop Surg Res. 2021;16(1):370. doi: 10.1186/s13018-021-02517-z. Published 2021 Jun 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nibe Y., Matsumura T., Takahashi T., Kubo T., Matsumoto Y., Takeshita K. A comparison between the femoral neck system and other implants for elderly patients with femoral neck fracture: a preliminary report of a newly developed implant. J Orthop Sci. Jun. 2021;2(21):S0949–S2658. doi: 10.1016/j.jos.2021.04.016. pp.00153–6. [DOI] [PubMed] [Google Scholar]
- 22.Tang Y., Zhang Z., Wang L., et al. Femoral neck system versus inverted cannulated cancellous screw for the treatment of femoral neck fractures in adults: a preliminary comparative study. J Orthop Surg Res. 2021;16:504. doi: 10.1186/s13018-021-02659-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vazquez O., Gamulin A., Hannouche D., Belaieff W. Osteosynthesis of non-displaced femoral neck fractures in the elderly population using the femoral neck system (FNS): short-term clinical and radiological outcomes. J Orthop Surg Res. 2021;16(1):477. doi: 10.1186/s13018-021-02622-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhou X.Q., Li Z.Q., Xu R.J., et al. Comparison of early clinical results for femoral neck system and cannulated screws in the treatment of unstable femoral neck fractures. Orthop Surg. Aug. 2021;13(6):1802–1809. doi: 10.1111/os.13098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang Y., Ma T., Zhang X., Luo X., Fan T., Wang Y. [Short-term effectiveness of femoral neck system in the treatment of femoral neck fracture] Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2021;35(5):539–543. doi: 10.7507/1002-1892.202012097. PMID: 33998204; PMCID: PMC8175206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang Y.Z., Lin Y., Li C., et al. A comparative analysis of femoral neck system and three cannulated screws fixation in the treatment of femoral neck fractures: a six-month follow-up. Orthop Surg. 2022 doi: 10.1111/os.13235. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.He C., Lu Y., Wang Q., et al. Comparison of the clinical efficacy of a femoral neck system versus cannulated screws in the treatment of femoral neck fracture in young adults. BMC Musculoskelet Disord. Nov 29. 2021;22(1):994. doi: 10.1186/s12891-021-04888-0. PMID: 34844578; PMCID: PMC8630835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yan C., Wang X., Xiang C., et al. [Comparison of effectiveness of femoral neck system and cannulate compression screw in treatment of femoral neck fracture in young and middle-aged patients] Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2021;35(10):1286–1292. doi: 10.7507/1002-1892.202103099. PMID: 34651482; PMCID: PMC8505931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yang J., Zhou X., Li L., et al. [Comparison of femoral neck system and inverted triangle cannulated screws fixations in treatment of Pauwels type Ⅲ femoral neck fractures] Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. Sep 15. 2021;35(9):1111–1118. doi: 10.7507/1002-1892.202102046. PMID: 34523275; PMCID: PMC8444134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xiong Wei, Yi Min, Cheng Long, et al. [A comparative study of femoral neck system versus inverted triangle cannulated compression screws in fixation of adult femoral neck fracture] Chin J Orthop Trauma. 2021;23(9):748–753. doi: 10.3760/cma.j.cn115530-20210822-00388. [DOI] [Google Scholar]
- 31.Szita J., Cserháti P., Bosch U., Manninger J., Bodzay T., Fekete K. Intracapsular femoral neck fractures: the importance of early reduction and stable osteosynthesis. Injury. 2002;33(Suppl 3):C41–C46. doi: 10.1016/s0020-1383(02)00330-3. [DOI] [PubMed] [Google Scholar]
- 32.Krischak G., Beck A., Wachter N., Jakob R., Kinzl L., Suger G. Relevance of primary reduction for the clinical outcome of femoral neck fractures treated with cancellous screws. Arch Orthop Trauma Surg. 2003;123(8):404–409. doi: 10.1007/s00402-003-0571-3. [DOI] [PubMed] [Google Scholar]
- 33.Heetveld M.J., Raaymakers E.L., Luitse J.S., Gouma D.J. Rating of internal fixation and clinical outcome in displaced femoral neck fractures: a prospective multicenter study. Clin Orthop Relat Res. 2007;454:207–213. doi: 10.1097/01.blo.0000238867.15228.8d. [DOI] [PubMed] [Google Scholar]
- 34.Chen Z., Wang G., Lin J., et al. Efficacy comparison between dynamic hip screw combined with anti-rotation screw and cannulated screw in treating femoral neck fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2011;25(1):26–29. [PubMed] [Google Scholar]
- 35.Xia Y., Zhang W., Zhang Z., Wang J., Yan L. Treatment of femoral neck fractures: sliding hip screw or cannulated screws? A meta-analysis. J Orthop Surg Res. Jan 14. 2021;16(1):54. doi: 10.1186/s13018-020-02189-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xiao Y.P., Shu D.P., Bei M.J., Ji T., Kan W.S., Li S.G. The clinical application of a novel method of internal fixation for femoral neck fractures-dynamic locking compression system. J Orthop Surg Res. 2018;13(1):131. doi: 10.1186/s13018-018-0827-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cha Y.H., Yoo J.I., Hwang S.Y., et al. Biomechanical evaluation of internal fixation of Pauwels type III femoral neck fractures: a systematic review of various fixation methods. Clin Orthop Surg. Mar; 2019;11(1):1–14. doi: 10.4055/cios.2019.11.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jung C.H., Cha Y., Yoon H.S., et al. Mechanical effects of surgical variations in the femoral neck system on Pauwels type III femoral neck fracture: a finite element analysis. Bone Joint Res. Feb. 2022;11(2):102–111. doi: 10.1302/2046-3758.112.BJR-2021-0282.R1. PMID: 35168366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Xia Y., Zhang W., Hu H., Yan L., Zhan S., Wang J. Biomechanical study of two alternative methods for the treatment of vertical femoral neck fractures - a finite element analysis. Comput Methods Programs Biomed. Nov. 2021;211 doi: 10.1016/j.cmpb.2021.106409. Epub 2021 Sep 9. PMID: 34560605. [DOI] [PubMed] [Google Scholar]
- 40.Stassen R.C., Jeuken R.M., Boonen B., Meesters B., de Loos E.R., van Vugt R. First clinical results of 1-year follow-up of the femoral neck system for internal fixation of femoral neck fractures. Arch Orthop Trauma Surg. Nov. 2021;3 doi: 10.1007/s00402-021-04216-0. Epub ahead of print. PMID: 34734328. [DOI] [PubMed] [Google Scholar]
- 41.Cheng H., Clymer J.W., Po-Han Chen B., et al. Prolonged operative duration is associated with complications: a systematic review and meta-analysis. J Surg Res. Sep. 2018;229:134–144. doi: 10.1016/j.jss.2018.03.022. [DOI] [PubMed] [Google Scholar]
- 42.Bout C.A., Cannegieter D.M., Juttmann J.W. Percutaneous cannulated screw fixation of femoral neck fractures: the three-point principle. Injury. Mar. 1997;28(2):135–139. doi: 10.1016/s0020-1383(96)00161-1. [DOI] [PubMed] [Google Scholar]
- 43.Khoo C., Haseeb A., Ajit Singh V. Cannulated screw fixation for femoral neck fractures: a 5-year experience in A single institution. Malays Orthop J. 2014;8(2):14–21. doi: 10.5704/MOJ.1407.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cintean R., Pankratz C., Hofmann M., Gebhard F., Schütze K. Early results in non-displaced femoral neck fractures using the femoral neck system. Geriatr Orthop Surg Rehabil. 2021;12 doi: 10.1177/21514593211050153. PMID: 34733579; PMCID: PMC8559200. [DOI] [PMC free article] [PubMed] [Google Scholar]