Abstract
Introduction
There is increasing evidence that the prescription opioid crisis is spreading internationally. However, there is scarce literature comparing contemporary prescribing practices between units in different countries, particularly in the context of this evolving international problem. We sought to determine the patterns of postoperative opioid prescribing in three hospitals from geographically distinct regions.
Methods
This is a retrospective cohort study involving patients from three hospitals: XXX, Maine, USA; XXX, Scotland; and XXX, Australia. The health records, surgical details, and frequency and potency of discharge prescriptions were analyzed for 350 patients receiving surgery for isolated wrist or ankle fractures. Regression analysis was used to identify independent predictors of prescription opioid provision.
Results
Following ankle fracture surgery, Aberdeen patients (OR 6.0, 95% CI 3.0–11.5) and Adelaide patients (11.8, 95% CI 4.1–39.6) were significantly more likely to receive a prescription for opioids than those in Augusta (p < 0.001). For distal radius fractures, this was also the case (Aberdeen OR 21.2, 95% CI 7.2–79.3, Adelaide OR 21.6, 95% CI 7.3–81.3). For both fracture groups, the potency of prescription provided (measured in morphine milligram equivalents) was not significantly different. When opioids were included in the discharge prescription, Adelaide prescribers favored strong opioids, Aberdeen prescribers selected weak opioids, and prescribers in Augusta chose an even distribution of both types (p < 0.001). Multivariate analysis demonstrated that the odds of receiving prescription opioids were significantly influenced by geographic location and decreased by advancing patient age.
Conclusions
Geographic location is a key factor influencing the provision of postoperative opioids. We found no association with fracture type, patient demographic factors or intra-operative practices. Prescriber culture is likely an influential determinant of postoperative opioid provision. Emphasis on patient and prescriber education regarding the risks of prescription opioids and their potential long-term sequelae is key if we wish to change modifiable prescriber behavior.
Keywords: Fracture, Postoperative prescribing, Opioid
1. Introduction
An exaggeration of the benefits of prescription opioids by pharmaceutical companies, and the deliberate understatement of their risks and addictive potential, has led to an epidemic in the United States and Canada.1 The corresponding increase in rates of opioid overdose and overdose-related deaths has been termed the opioid crisis. There is evidence that in recent years the frequency of prescription opioid use has increased internationally.1
After orthopedic fracture surgery, there has historically been wide variation in patterns of opioid prescribing between hospitals in the United States and other regions of the world where opioids are used less frequently.2, 3, 4 However, there is scarce recent literature that documents comparison of contemporary prescribing practices between countries, particularly in the context of an evolving international prescription opioid problem. We therefore sought to determine the current patterns of postoperative opioid prescribing for fracture patients in three hospitals from geographically distinct regions.
Our primary aim was to define the frequency and potency of opioid medication prescription for patients recovering from extremity fracture surgery in the three hospitals. Our secondary aim was to identify patient, injury, surgical and anesthetic variables that might influence postoperative prescribing. We hypothesised that American patients continue to be prescribed opioids with greater potency, more frequently, and at higher doses than their Scottish and Australian counterparts.
2. Methods
Our study protocol was approved by the Institutional Review Boards at the participating hospitals. We followed the ‘Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)’ reporting guidelines for cohort studies.5
2.1. Study design and participants
We performed a retrospective cohort study involving 350 patients who had received operative treatment of an acute ankle (193) or distal radius (157) fracture at one of three hospitals in Augusta (Maine, USA), Aberdeen (Scotland) and Adelaide (Australia). We excluded patients with multiple fractures and those aged less than 16 years. Augusta (106) patients were treated by a single surgeon team from 2018 to 2020 at XXXX, a regional level 3 trauma centre treating public and private patients. Aberdeen patients (135) were treated by several surgeon teams in 2020 at XXXX, a major trauma centre Scotland treating public trauma patients from a large geographic area. Adelaide patients (109) received treatment from several surgeon teams in 2020 at XXXX, a major trauma centre in Australia treating predominantly public trauma patients.
2.2. Variables and definitions
We examined the inpatient electronic health records (EHR) of these patients to retrieve the following information: age, gender, history of anxiety or depression, surgical procedure, type of anesthesia used, length of hospital stay. We examined the hospital Picture Archiving and Communication System (PACS) to determine the fracture type according to the AO classification. For Augusta patients, a history of pre-injury prescription opioid use and details of postoperative opioid prescriptions were obtained from the Maine Prescription Drug Monitoring Program (PDMP). In Aberdeen and Adelaide, these data were obtained from the inpatient EHR. We defined a history of pre-injury opioid use as the existence of two or more filled opioid prescriptions provided for a separate diagnosis in the six months prior to injury. The drug type, strength and number of tablets for all postoperative opioid prescriptions was standardized to oral Morphine Milligram Equivalents (MMEs) to allow comparison.6,7
The sample size of patients chosen for each fracture group followed similar patient numbers chosen by Lindenhovius et al. in a similar study.3 All patients were advised to use over-the-counter paracetamol and NSAIDs routinely, unless contraindicated. Our definition of opioid pain medication included oral weak opioids (tramadol, codeine, dihydrocodeine) and oral strong opioids (oxycodone, hydrocodone). In Augusta, the provision of an immediate postoperative opioid prescription is the responsibility of the operating surgeon and their physician assistant. Any patient requests for additional or alternative medication are initiated by the patient calling the orthopaedic offices. In Aberdeen and Adelaide, postoperative prescribing is completed by ward based junior medical staff or the orthopaedic registrar. Additional patient requests following discharge are dealt with by primary care providers.
2.3. Statistical methods
Ankle fracture patients and distal radius fracture patients were analyzed as two distinct groups. The continuous variables patient age and MMEs followed an asymmetric distribution (Shapiro-Wilk test) for both fracture groups and are therefore presented as the median and range. Categorical variables are presented as proportions and ratios (with 95% CIs). Analysis was performed using statistical software (SPSS version 22, SPSS Inc., Chicago IL), with significance set at a p value less than 0.05.
Baseline characteristics of the Augusta, Aberdeen and Adelaide cohorts were compared using the Kruskal-Wallis test for continuous variables (age) and ordinal variables (fracture type, length of stay) and the chi-square test for categorical variables (gender, history of anxiety/depression, pre-injury prescription opioid use, anesthetic type, surgical approaches used). The primary aim of the study was evaluated by comparing the proportions of patients in each cohort provided with a postoperative opioid prescription using the chi-square test. The distributions of prescribed MMEs between cohorts were compared using the Kruskal-Wallis test.
In order to investigate the secondary research aim, regression analysis was used. We initially performed bivariate analyses to identify the association of independent variables with the dependent variable of interest (the presence of a postoperative opioid prescription), using the Mann-Whitney U test and the chi-square test for continuous and categorical variables, respectively. Independent variables displaying a near significant association (p value less than 0.1) or better were selected for inclusion in the regression analysis. We selected a binary logistic regression model to analyze the ability of the independent variables to influence the dependent variable, accounting for confounding. This kind of modeling produces a statistic called the Nagelkerke R square, which provides an approximation of the proportion of variation in the dependent variable that can be explained by the independent variables. In addition, the model output produces the exponentiation of the B coefficient, Exp(B), for each independent variable included. The Exp(B) is an odds ratio, representing the effect that a one-unit increase in the independent variable has upon the odds of producing the dependent outcome: each unit increase in “X” multiplies the odds of “Y outcome”, by Exp(B).
3. Results
3.1. Ankle fracture patients
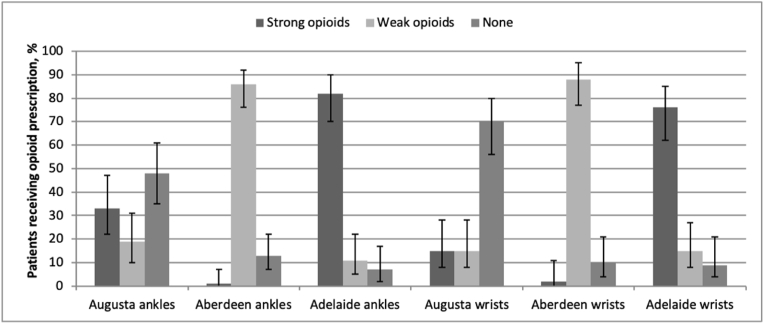
Adelaide patients were younger than those in Augusta and Aberdeen, and a smaller proportion had a history of anxiety or depression. Adelaide and Augusta patients used the most opioids pre-injury. None of the Aberdeen patients had a pre-injury history of strong opioid use, but a larger proportion used weak opioids. Augusta patients received regional anesthesia more frequently, and a greater number were discharged from hospital on the day of surgery. The distribution of patient gender, ankle fracture type and surgical approaches did not differ significantly between hospitals (Table 1). There was a statistically significant difference between postoperative opioid prescribing across the three hospitals. Augusta patients recovering from ankle fracture surgery received a prescription for opioid medication in 52% of cases, compared to 87% of patients in Aberdeen and 93% in Adelaide (Fig. 1). However, only 1% of Aberdeen prescriptions involved a strong opioid, compared with 64% of Augusta prescriptions and 88% of Adelaide prescriptions. Overall, the median MMEs per prescription was similar between all three groups (Table 3).
Table 1.
Baseline characteristics for patients with ankle fractures.
| ANKLE | Augusta (n = 54) | Aberdeen (n = 83) | Adelaide (n = 56) | p value |
|---|---|---|---|---|
| Age, median years (R) | 56 (22–82) | 52 (19–92) | 50 (16–92) | <0.001 |
| Gender, n (%) | ||||
| Male | 18 (33) | 35 (42) | 25 (45) | 0.439 |
| Female | 36 (67) | 48 (58) | 31 (55) | |
| Depression or anxiety, n (%) | 27 (50) | 25 (30) | 11 (20) | 0.003 |
| Pre-injury opioid use, n (%) | ||||
| Strong | 6 (11) | 0 | 7 (13) | 0.004 |
| Weak | 1 (2) | 8 (10) | 1 (2) | |
| Fracture type, n (%) | ||||
| A | 5 (9) | 6 (7) | 3 (5) | 0.389 |
| B | 34 (63) | 56 (68) | 33 (59) | |
| C | 15 (28) | 21 (25) | 20 (36) | |
| Anesthesia used, n (%) | ||||
| general only | 21 (39) | 36 (44) | 40 (71) | <0.001 |
| regional only | 1 (2) | 0 | 0 | |
| general plus regional | 29 (53) | 5 (6) | 14 (25) | |
| spinal plus regional | 1 (2) | 1 (1) | 1 (2) | |
| spinal only | 2 (4) | 40 (48) | 1 (2) | |
| missing values | 0 | 1 (1) | 0 | |
| Surgical approaches, n (%) | ||||
| Single | 20 (37) | 37 (45) | 29 (53) | 0.257 |
| Dual | 34 (63) | 46 (55) | 26 (47) | |
| Length of stay, days (%) | ||||
| same day | 40 (74) | 11 (13) | 5 (9) | <0.001 |
| 1 day | 8 (15) | 32 (39) | 30 (54) | |
| 2 or more days | 6 (11) | 40 (48) | 21 (37) | |
Fig. 1.
The proportion of patients provided with a postoperative opioid prescription. Error bars represent 95% CIs.
Table 3.
Postoperative opioid prescribing for patients recovering from a fracture of the ankle or distal radius. OR, odds ratio with 95% CIs; MMEs, oral morphine milligram equivalents, median and range.
| Augusta |
Aberdeen |
Adelaide |
p value | |
|---|---|---|---|---|
| ANKLE | n = 54 | n = 83 | n = 56 | |
| Postoperative opioid prescription, n (%) | ||||
| strong | 18 (33) | 1 (1) | 46 (82) | <0.001 |
| weak | 10 (19) | 71 (86) | 6 (11) | |
| none | 26 (48) | 11 (13) | 4 (7) | |
| OR of prescription opioid | 1 | 6.0 (3.0–11.5) | 11.8 (4.1–39.6) | – |
| MMEs per prescription (mg) | 75 (30–225) | 84 (84–210) | 75 (30–150) | 0.162 |
| Variables contributing to receiving a prescription: location; patient age | ||||
|
| ||||
| DISTAL RADIUS | n = 52 | n = 52 | n = 53 | |
| Postoperative opioid prescription, n (%) | ||||
| strong | 8 (15) | 1 (2) | 40 (76) | <0.001 |
| weak | 8 (15) | 46 (88) | 8 (15) | |
| none | 36 (70) | 5 (10) | 5 (9) | |
| OR of prescription opioid | 1 | 21.2 (7.2–79.3) | 21.6 (7.3–81.3) | – |
| MMEs per prescription (mg) | 90 (50–150) | 84 (84–84) | 75 (30–150) | 0.433 |
| Variables contributing to receiving a prescription: location; patient age; fracture type A | ||||
3.2. Predictors of postoperative opioid prescription for ankle fracture patients
Bivariate analyses revealed location (p < 0.001), patient age (p = 0.002) and the use of regional anesthetic block (p < 0.001) as variables displaying a significant association with the provision of a postoperative opioid prescription. Past history of anxiety or depression and pre-injury prescription opioid use showed no association.
The resultant binary logistic regression model accounted for 29% of the variability in postoperative opioid prescribing (Nagelkerke R square, p < 0.001), and included location and patient age as statistically significant predictors. Patients in Augusta were 90% less likely to receive a prescription (Exp[B] 0.10, 95%CI 0.03–0.33, p < 0.001). For each one year increase in patient age, the odds of receiving an opioid prescription decreased by 3% (Exp[B] 0.97, 95%CI 0.95–0.99, p = 0.010). Of note, the use of regional anesthetic block was not a statistically significant predictor of outcome (p = 0.103) after controlling for confounding.
3.3. Distal radius fracture patients
The Adelaide cohort was younger and made up of a larger proportion of male patients than the Augusta and Aberdeen groups. A greater proportion of Type B fractures was seen in Aberdeen. A past history of depression or anxiety and pre-injury prescription opioid use was seen more frequently in Augusta patients. Americans were also more likely to receive regional anesthesia and be discharged on the day of surgery (Table 2). Thirty percent of Augusta patients recovering from surgery for a distal radius fracture received a prescription for opioid medication, compared to 90% of Aberdeen patients and 91% in Adelaide (Fig. 1). Only 2% of Aberdeen prescriptions involved a strong opioid, compared with 50% in Augusta and 83% in Adelaide. Overall, the median MMEs per prescription did not differ between groups (Table 3).
Table 2.
Baseline characteristics for patients with distal radius fractures.
| DISTAL RADIUS | Augusta (n = 52) | Aberdeen (n = 52) | Adelaide (n = 53) | p value |
|---|---|---|---|---|
| Age, median years (R) | 61 (27–86) | 61 (16–81) | 47 (18–83) | <0.001 |
| Gender, n (%) | ||||
| male | 10 (19) | 17 (33) | 27 (49) | 0.003 |
| female | 42 (81) | 35 (67) | 26 (51) | |
| Depression or anxiety, n (%) | 25 (48) | 10 (19) | 5 (9) | <0.001 |
| Pre-injury opioid use, n (%) | ||||
| strong | 7 (13) | 0 | 2 (4) | 0.034 |
| weak | 2 (4) | 5 (10) | 3 (6) | |
| Fracture type, n (%) | ||||
| A | 29 (56) | 9 (17) | 22 (42) | <0.001 |
| B | 4 (8) | 29 (56) | 19 (36) | |
| C | 19 (36) | 14 (27) | 12 (23) | |
| Anesthesia used, n (%) | ||||
| general only | 18 (35) | 41 (79) | 43 (81) | <0.001 |
| regional only | 10 (19) | 6 (11) | 3 (6) | |
| general plus regional | 24 (46) | 5 (10) | 7 (13) | |
| Surgical approaches, n (%) | ||||
| single | 45 (87) | 48 (92) | 51 (96) | 0.194 |
| dual | 7 (13) | 4 (8) | 2 (4) | |
| Length of stay, days (%) | ||||
| same day | 47 (90) | 27 (52) | 18 (34) | <0.001 |
| 1 day | 4 (8) | 22 (42) | 26 (49) | |
| 2 or more days | 1 (2) | 3 (6) | 11 (17) | |
3.4. Predictors of postoperative opioid prescription for distal radius fracture patients
Bivariate analyses revealed location (p < 0.001), patient age (p < 0.001), gender (p = 0.004), history of anxiety/depression (p = 0.011), pre-injury prescription opioid use (p = 0.065), fracture type (p < 0.001) and the use of regional anesthetic block (p < 0.001) as variables displaying a significant or near significant association with the provision of a postoperative opioid prescription.
The binary logistic regression model accounted for 54% of the variability in postoperative opioid prescribing (Nagelkerke R square, p < 0.001). Only three of the seven variables remained as statistically significant predictors: location, patient age and fracture type. Patients in Augusta were 94% less likely to receive a prescription (Exp[B] 0.06, 95%CI 0.02–0.22, p < 0.001). For each one year increase in patient age, the odds of receiving an opioid prescription decreased by 4% (Exp[B] 0.96, 95%CI 0.93–0.99, p = 0.030). Suffering a Type A distal radius fracture decreased the odds of receiving a prescription by 70% (Exp[B] 0.30, 95%CI 0.09–0.95, p = 0.041).
4. Discussion
The opioid crisis in the United States has prompted the implementation of strategies aimed at reducing opioid prescribing. Many hospitals and orthopaedic practices have introduced strict upper limits to prescriptions.8, 9, 10 Over half of the 50 states have passed mandatory prescription limits, with the effect of decreasing rates of opioid provision.11,12 All states except Missouri now monitor prescriber behavior via a Prescription Drug Monitoring Program. The Orthopaedic Trauma Association has published clinical practice guidelines on the rational use of opioids following surgery.13 These strategies, and increased awareness of the problem, has culminated in the Center for Disease Control and Prevention reporting a 19% reduction in annual opioid prescribing rates between 2006 and 2017.14
Unfortunately, the opposite trend is being reported in other countries. In Australia, one systematic review of 20 studies evaluating prescription opioid rates has shown a 15-fold increase in the 20 years up to 2017, predominantly driven by a sharp rise in oxycodone use.15 There are fewer data available from the United Kingdom, but an increase in opioid prescribing for all causes of non-cancer pain by primary care providers has been demonstrated, in particular a five-fold increase in the use of weak opioids such as codeine, dihydrocodeine and tramadol.16 Such is the level of concern internationally, that Levy and colleagues recently published a multidisciplinary consensus statement with recommendations aimed at preventing opioid-related harm in surgical patients.17
In this study, we chose to evaluate the patterns of postoperative opioid prescribing at hospitals in these three geographically distinct regions. We found marked differences in prescribing for a matched group of patients receiving similar surgery for ankle and distal radius fractures. We feel the greater proportion of Type B distal radius fractures observed in the Aberdeen cohort potentially reflects the current preference in the United Kingdom for nonoperative treatment of Type A fractures and many Type C injuries with a non-displaced articular component. The observed differences in pre-injury anxiety and depressive disorders between cohorts is less easily explained, but could be linked to socio-economic deprivation or regional preferences in the management of mental health disorders.
In contrast to our hypothesis, Augusta patients received opioids less frequently (30–52%) than those in Aberdeen (87–90%) and Adelaide (91–93%), despite being discharged from hospital earlier. In the event of an opioid prescription being provided, however, there was no significant difference in the overall potency between groups (Table 3). Adelaide prescriptions contained the greatest proportion of strong opioids (oxycodone, hydrocodone), whereas Aberdeen prescribers preferred weak opioids almost exclusively (dihydrocodeine). Augusta patients were provided with similar proportions of strong or weak preparations (oxycodone, tramadol). Our multivariate analyses showed that the odds of receiving prescription opioids were significantly influenced by geographic location and were decreased by advancing patient age. Notably, the use of regional anesthetic techniques had no significant influence. However, this study has not quantified the use of local anesthetic used by the surgeon intra-operatively.
Our reported frequency of prescription opioid provision for Augusta patients is lower than that documented in recent comparable American series,11,18 as well as studies performed at the peak of the epidemic,3,19,20 where opioid prescriptions were almost universally provided for patients recovering from ankle or distal radius fracture surgery. We are not aware of any previous Scottish or Australian orthopedic fracture literature with which to compare our findings.
In our study, there was less frequent use of strong opioids for Augusta patients than previously reported in the United States. Dwyer et al. reported 73% of prescriptions were for strong opioids after distal radius fracture surgery in Burlington, Massachusetts in 2016.18 By comparison, strong opioids were preferred for 50% of Augusta prescriptions. Helmerhorst et al. noted that 100% of prescriptions were for strong opioids after ankle fracture surgery in Boston, Massachusetts in 2006.19 This compares with 64% (Augusta), 1% (Aberdeen) and 88% (Adelaide) in our study. We are aware of one comparable study reporting prescribed MMEs. Reid et al. evaluated prescribing patterns for two consecutive patient groups recovering from ankle and distal radius fracture surgery in Providence, Rhode Island in 2017.11 The first group received prescriptions before the introduction of mandatory state prescription limits, the second group after the legislation was in place. Mean first prescription MMEs fell from 374 to 172 for distal radius surgery and 417 to 167 after ankle surgery. By comparison, the median prescribed MMEs for all three locations in our study was 90 or less, irrespective of fracture type.
One fundamental influence on the choice of postoperative prescription in Aberdeen and Adelaide is the availability of ready-labeled analgesic medications for postoperative patients. In Adelaide, the prescriber may issue a predetermined ‘starter pack’ of oxycodone 5 mg, tramadol 50 mg or codeine/paracetamol 30/500 mg. In Aberdeen, UK legislation (The Misuse of Drugs Act 1971 [amendment] Order 2014) inhibits the availability of strong opioids via this ready-labeled route, and the prescriber may issue dihydrocodeine 30 mg or codeine/paracetamol 30/500 mg: the prescription of strong opioids is therefore inherently more convoluted and time consuming. By contrast, Augusta patients are prescribed medications electronically for collection at their preferred pharmacy and starter packs are not used.
In our attempt to identify variables that might influence postoperative prescribing we were able to construct regression models which accounted for 29% (ankle) and 54% (distal radius) of the variation in opioid prescribing patterns. The most influential variable was geographic location, even after accounting for numerous patient, injury and anesthetic factors. Location, or regional prescribing culture, is the product of prescriber factors (training, attitudes to pain, attitudes to opioids, institutional protocols and limits) and patient factors (past experiences, expectations of pain relief, attitudes to pain and opioids, preference for specific medications). The remaining variation may be related to numerous psychosocial factors not measured in our study. We attempted to control for psychological distress (anxiety and/or depressive disorder), but did not control for the influence of life stressors (life roles, personal relationships, housing, employment), cognitive bias (catastrophic thinking) and other mental and social health issues, all of which are known to be involved in a patients perception of pain and their perceived requirement for pain relief.21
Our study results should be interpreted in the context of relevant limitations. Of particular note is that the surgeon prescriber in Augusta is a UK trained orthopedic surgeon. His prescribing patterns are unlikely to be representative of other US trained surgeons in Maine, although he is of course subject to the same regulations. Our Augusta findings might therefore be interpreted as ‘cross-cultural’, i.e. the product of non-regional prescriber factors and regional patient factors, as outlined above. In addition, the dates of the study period across the three sites are not uniform. To better compare the three regions, we selected continuous time periods to give equivalent patients numbers. This improved the strength of our study, allowing more patients to be compared across the three sites, but there may have been changes in prescribing habits with time which we have not accounted for. Finally, and importantly, this study is retrospective in nature and the results should be interpreted bearing in mind the limitations inherent to this kind of research.
We believe that prescriber culture is a strong determinant of postoperative opioid provision. There is good evidence that education of surgeon and resident prescribers can be influential in this regard, encouraging responsible and rational prescribing behavior.22, 23, 24
In this study we have reported details of opioid prescription provision, not opioid consumption, and have no data on the actual numbers of tablets consumed by each patient. Additionally, inpatient opioid use has not been documented. This may influence discharge medications and therefore this may alter the MMEs between groups if taken into account. Clinicians need to be aware of inpatient use, as much as discharge medication, in order to minimize the risk of long-term addiction.1 Future prospective work will measure patient-reported outcomes (postoperative pain and satisfaction scores) of the prescribing patterns presented here, as we attempt to define the optimal strength and duration of analgesic treatment for patients recovering from isolated extremity fracture surgery.
5. Conclusions
The results of this study suggest geographic location is a key factor influencing the provision of postoperative opioids. We found no association with fracture type, patient demographic factors or intra-operative practices. We feel prescriber culture is likely an influential determinant of postoperative opioid provision. If we wish to change modifiable prescriber behavior then perhaps greater emphasis might be placed on patient and prescriber education regarding the risks of prescription opioids and their potential long-term sequelae.
Source of funding
None.
Declaration of competing interest
None.
References
- 1.Helmerhorst G.T., Teunis T., Janssen S.J., Ring D. An epidemic of the use, misuse and overdose of opioids and deaths due to overdose, in the United States and Canada: is Europe next? bone & joint j. 2017;99-B:856–864. doi: 10.1302/0301-620X.99B7.BJJ-2016-1350.R1. [DOI] [PubMed] [Google Scholar]
- 2.Carragee E.J., Vittum D., Truong T.P., Burton D. Pain control and cultural norms and expectations after closed femoral shaft fractures. Am J Orthop (Belle Mead NJ) 1999;28:97–102. [PubMed] [Google Scholar]
- 3.Lindenhovius A.L., Helmerhorst G.T., Schnellen A.C., Vrahas M., Ring D., Kloen P. Differences in prescription of narcotic pain medication after operative treatment of hip and ankle fractures in the United States and The Netherlands. J Trauma. 2009;67:160–164. doi: 10.1097/TA.0b013e31818c12ee. [DOI] [PubMed] [Google Scholar]
- 4.Young J.D., Bhashyam A.R., Qudsi R.A., et al. Cross-cultural comparison of postoperative discharge opioid prescribing after orthopaedic trauma surgery. J Bone Jt Surg Am Vol. 2019;101:1286–1293. doi: 10.2106/JBJS.18.01022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.von Elm E., Altman D.G., Egger M., et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 6.https://fpm.ac.uk/opioids-aware-structured-approach-opioid-prescribing/dose-equivalents-and-changing-opioids
- 7.Svendsen K., Borchgrevink P., Fredheim O., Hamunen K., Mellbye A., Dale O. Choosing the unit of measurement counts: the use of oral morphine equivalents in studies of opioid consumption is a useful addition to defined daily doses. Palliat Med. 2011;25:725–732. doi: 10.1177/0269216311398300. [DOI] [PubMed] [Google Scholar]
- 8.Bhashyam A.R., Basilico M., Weaver M.J., Harris M.B., Heng M. Using historical variation in opioid prescribing immediately after fracture surgery to guide maximum initial prescriptions. J Orthop Trauma. 2019;33:e131–e136. doi: 10.1097/BOT.0000000000001392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Teunis T., Stoop N., Park C.J., Ring D. What factors are associated with a second opioid prescription after treatment of distal radius fractures with a volar locking plate? Hand (N Y) 2015;10:639–648. doi: 10.1007/s11552-015-9767-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wyles C.C., Hevesi M., Ubl D.S., et al. Implementation of procedure-specific opioid guidelines: a readily employable strategy to improve consistency and decrease excessive prescribing following orthopaedic surgery. JB JS Open Access. 2020;5 doi: 10.2106/JBJS.OA.19.00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reid D.B.C., Shah K.N., Shapiro B.H., Ruddell J.H., Akelman E., Daniels A.H. Mandatory prescription limits and opioid utilization following orthopaedic surgery. J Bone Jt Surg Am Vol. 2019;101:e43. doi: 10.2106/JBJS.18.00943. [DOI] [PubMed] [Google Scholar]
- 12.Sedney C.L., Khodaverdi M., Pollini R., Dekeseredy P., Wood N., Haggerty T. Assessing the impact of a restrictive opioid prescribing law in West Virginia. Subst Abuse Treat Prev Pol. 2021;16:14. doi: 10.1186/s13011-021-00349-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hsu J.R., Mir H., Wally M.K., Seymour R.B. Orthopaedic trauma association musculoskeletal pain task F. Clinical practice guidelines for pain management in acute musculoskeletal injury. J Orthop Trauma. 2019;33:e158–e182. doi: 10.1097/BOT.0000000000001430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.https://cdc.gov/drugoverdose/data/prescribing/prescribing-practices.html
- 15.Donovan P.J., Arroyo D., Pattullo C., Bell A. Trends in opioid prescribing in Australia: a systematic review. Aust Health Rev. 2020;44:277–287. doi: 10.1071/AH18245. [DOI] [PubMed] [Google Scholar]
- 16.Jani M., Birlie Yimer B., Sheppard T., Lunt M., Dixon W.G. Time trends and prescribing patterns of opioid drugs in UK primary care patients with non-cancer pain: a retrospective cohort study. PLoS Med. 2020;17 doi: 10.1371/journal.pmed.1003270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levy N., Quinlan J., El-Boghdadly K., et al. An international multidisciplinary consensus statement on the prevention of opioid-related harm in adult surgical patients. Anaesthesia. 2021;76:520–536. doi: 10.1111/anae.15262. [DOI] [PubMed] [Google Scholar]
- 18.Dwyer C.L., Soong M., Hunter A., Dashe J., Tolo E., Kasparyan N.G. Prospective evaluation of an opioid reduction protocol in hand surgery. J Hand Surg Am. 2018;43:516–522 e1. doi: 10.1016/j.jhsa.2018.01.021. [DOI] [PubMed] [Google Scholar]
- 19.Helmerhorst G.T., Lindenhovius A.L., Vrahas M., Ring D., Kloen P. Satisfaction with pain relief after operative treatment of an ankle fracture. Injury. 2012;43:1958–1961. doi: 10.1016/j.injury.2012.08.018. [DOI] [PubMed] [Google Scholar]
- 20.Kim N., Matzon J.L., Abboudi J., et al. A prospective evaluation of opioid utilization after upper-extremity surgical procedures: identifying consumption patterns and determining prescribing guidelines. J Bone Jt Surg Am Vol. 2016;98:e89. doi: 10.2106/JBJS.15.00614. [DOI] [PubMed] [Google Scholar]
- 21.Brown L.E., Fatehi A., Ring D. Talking points for the safe and effective alleviation of pain. bone & joint j. 2020;102-B:1122–1127. doi: 10.1302/0301-620X.102B9.BJJ-2020-0091.R1. [DOI] [PubMed] [Google Scholar]
- 22.Bhashyam A.R., Young J., Qudsi R.A., Parisien R.L., Dyer G.S.M. Opioid prescribing patterns of orthopedic surgery residents after open reduction internal fixation of distal radius fractures. J Hand Surg Am. 2019;44:201–207 e2. doi: 10.1016/j.jhsa.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 23.Goel A., Feinberg A., McGuiness B., et al. Postoperative opioid-prescribing patterns among surgeons and residents at university-affiliated hospitals: a survey study. Can J Surg J canadien de chirurgie. 2020;63:E1–E8. doi: 10.1503/cjs.016518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hopkins R.E., Bui T., Konstantatos A.H., et al. Educating junior doctors and pharmacists to reduce discharge prescribing of opioids for surgical patients: a cluster randomised controlled trial. Med J Aust. 2020;213:417–423. doi: 10.5694/mja2.50812. [DOI] [PubMed] [Google Scholar]