Abstract
Background:
People with opioid use disorder and severe infections may complete their prolonged courses of outpatient parenteral antimicrobial therapy at a post-acute care facility due to adherence and safety concerns. We hypothesized that treatment with medications for opioid use disorder, such as methadone and buprenorphine, would increase antibiotic completion in these facilities.
Methods:
We performed a retrospective cohort study of people with opioid use disorder and severe infections who were discharged from the University of Maryland Medical Center to a post-acute care facility to complete intravenous antibiotic therapy. The primary outcome was completion of outpatient parenteral antimicrobial therapy. We compared the rate of antibiotic completion between patients prescribed and not prescribed medication for opioid use disorder at discharge from the acute care hospital.
Results:
A total of 161 patient encounters were included; the mean age was 43.4 years and 56% of patients were male. In 48% of the encounters, the patient was homeless and in 68% they recently injected drugs. The most common infectious syndrome was osteoarticular (44.1%). Medication for opioid use disorder was prescribed at discharge in 103 of 161 encounters and was newly started in 27 encounters. Similar rates of outpatient parenteral antimicrobial therapy completion were found in those who received (65/103) and did not receive (33/58) medication for opioid use disorder at discharge (odds ratio: 1.29; 95% confidence interval: 0.68–2.54; p = 0.44).
Conclusion:
Medication for opioid use disorder prescription at discharge was not associated with completion of outpatient parenteral antimicrobial therapy in a post-acute care facility. Our study is limited by possible selection bias and infrequent initiation of medication for opioid use disorder, which may have minimized the effect on antibiotic completion.
Keywords: injection drug use, medication for opioid use disorder, outpatient parenteral antimicrobial therapy, substance use disorder
Introduction
People with opioid use disorder (OUD) frequently have complicated bacterial and fungal infections such as osteomyelitis, infectious arthritis, and endocarditis,1,2 which are often treated with prolonged courses of intravenous (IV) antibiotics. Outpatient parenteral antimicrobial therapy (OPAT) allows patients to receive IV antibiotics outside the hospital, usually at home or in a post-acute care facility. People with OUD often complete OPAT in post-acute care facilities (such as skilled nursing or subacute rehabilitation facilities), instead of at home, due to concerns that they will not adhere to the antibiotic dosing schedule or will use the long-term IV access to inject non-prescribed drugs.3,4 In small studies, rates of successful completion of OPAT by people with OUD at post-acute care facilities are often lower than those receiving OPAT at other locations.5–7
Medications for opioid use disorder (MOUDs), such as buprenorphine and methadone, are effective for reducing symptoms of opioid withdrawal, OUD-related mortality, and illicit opioid use.8–10 Despite this benefit, MOUD are underutilized in acute care hospitals when people who inject drugs (PWIDs) are receiving care for complicated infections. 11 In people with OUD who received IV antibiotics only in the hospital (did not receive OPAT), use of MOUD was associated with higher rates of IV antibiotic completion. 12 Whether MOUD use can increase OPAT completion for people with OUD treated at a post-acute care facility is poorly understood. One retrospective study of people with OUD who completed IV or oral antibiotics at a medical respite facility did not demonstrate an association between a four-part intervention that included MOUD initiation and successful antibiotic completion. 13 This study was relatively small and did not report baseline MOUD use or antibiotic completion by discharge MOUD prescription.
We performed a retrospective cohort study, based on data from an established academic OPAT program, to test the hypothesis that, for people with OUD, prescription of methadone or buprenorphine at hospital discharge is associated with higher rates of OPAT completion at a post-acute care facility.
Methods
Patient encounters were identified through the OPAT program database at the University of Maryland School of Medicine. The OPAT program provides coordination of care and management of IV antibiotics by infectious disease (ID) nurses, an ID pharmacist, and an ID physician; receives and acts upon laboratory results; and coordinates in-person or remote follow-up with an ID physician. All patients in the OPAT program received ID and case management consultation during the acute care hospitalization. Consultation by the addiction psychiatry service during the hospitalization was provided only if ordered by the clinical team. Patients included in this study were discharged from two campuses of the University of Maryland Medical Center between 1 October 2017 and 31 April 2020.
Patient encounters were included if they were adults with a diagnosed substance use disorder (SUD) other than alcohol or nicotine, had a bacterial or fungal infection requiring OPAT and were managed by the University of Maryland School of Medicine OPAT program. Patients were excluded if they did not have a diagnosis of OUD, had inactive OUD, completed OPAT in a place other than a skilled nursing facility (e.g. at home, at residential drug treatment), or did not have information about MOUD at discharge. Multiple encounters from the same patient could be included.
Data abstraction was performed (by PRC) through analysis of the OPAT database, discrete variables exported from the medical record, and independent review of unstructured clinical notes (including admission notes, discharge notes, progress notes, and the addiction psychiatry and the ID consultation notes). Data were collected on age, sex, race, current experience of homelessness, current injection drug use (IDU), SUD diagnoses, past diagnosis of human immunodeficiency virus (HIV) infection, addiction psychiatry consultation, infectious syndromes, pathogens, OPAT antimicrobials, MOUD (buprenorphine or methadone) prior to acute care hospital admission and at the time of discharge, and outcome of OPAT treatment. Patients were characterized as having current IDU based on the assessment of the clinicians. SUD diagnoses were made by selection of International Classification of Diseases-9 (ICD-9) or ICD-10 codes (Supplemental Appendix A) and then confirmed by chart review. Patients were characterized as having inactive OUD if there were both (1) no illicit opioid use noted and/or inferred based on clinical notes and urine toxicology tests in the past year and (2) they were on treatment with MOUD. Patients were classified as prescribed MOUD prior to hospital admission or at hospital discharge based on the medication list, clinical notes, or the discharge instructions. The primary outcome was OPAT completion, defined as any of the following: documentation of cure, completion of planned therapy, or transition to suppressive antimicrobial therapy. Secondary outcomes included readmission within 30 days of OPAT completion and death.
We hypothesized that prescription of MOUD at discharge would increase the rate of OPAT completion. We also conducted an analysis to explore the effect of MOUD prior to admission. We compared baseline and outcome data by t-test for ratio data and chi-square or Fisher’s exact tests for nominal data. The odds ratio for the primary outcome was calculated by the Baptista–Pike method. Statistical tests were performed using GraphPad Prism 9 software.
Results
Out of 263 patient encounters that met the inclusion criteria, 102 encounters were subsequently excluded: 50 for discharge to somewhere besides a post-acute care facility (1 to acute rehabilitation, 1 to drug rehabilitation, and 48 to home), 37 who had inactive OUD, 13 for missing information on MOUD at discharge, and 2 who did not have a diagnosis of OUD. This left 161 encounters in the final analysis, representing 124 unique patients.
The mean age was 43.4 years and 56% of patients were male (Table 1). In 48% of the encounters, the patient was experiencing homelessness, and in 68%, they were currently injecting drugs. In 48% of encounters, patients had used other substances in addition to opioids and in 53% they were on MOUD prior to admission. Fourteen percent of the encounters involved patients with a diagnosis of HIV infection. Males were less likely to receive MOUD at discharge than females, but other baseline characteristics were similar. Most encounters (79%) included a consultation by the addiction psychiatry service. Infections were primarily osteomyelitis and/or septic arthritis (44.1%), followed by endocarditis (26.1%). Most infections involved a single Gram-positive organism (75.2%). Identified pathogens were commonly methicillin-resistant Staphylococcus aureus (39.8%), methicillin-sensitive Staphylococcus aureus (26.1%), or Streptococcus species (23.6%). Most OPAT treatments (90.1%) involved a single antibiotic, which was usually cephalosporin monotherapy (46.6%) or glycopeptide monotherapy (23.0%).
Table 1.
Cohort characteristics.
| Total (n = 161) | No MOUD at discharge (n = 58) | MOUD at discharge (n = 103) | P value | |
|---|---|---|---|---|
| Demographics | ||||
| Mean age, years | 43.4 | 44.6 | 42.7 | 0.31 |
| Sex | ||||
| Male Female | 90 (55.9)71 (44.1) | 39 (67.2)19 (32.8) | 51 (49.5)52 (50.5) | 0.03 |
| Race | ||||
| White Black Latinx | 111 (68.9)48 (29.8)2 (1.2) | 40 (69.0)16 (27.6)2 (3.4) | 71 (68.9)32 (31.1)0 | 1.00 a |
| Homeless | 77 (47.8) | 27 (46.6) | 50 (48.5) | 0.81 |
| Injection drug use | 109 (67.7) | 36 (62.1) | 73 (70.9) | 0.25 |
| Additional SUD b | 77 (47.8) | 22 (37.9) | 55 (53.4) | 0.06 |
| HIV infection | 23 (14.3) | 8 (13.8) | 15 (14.6) | 0.89 |
| Addiction treatment | ||||
| MOUD treatment prior to admission | 85 (52.8) | 9 (15.5) | 76 (73.8) | <0.0001 |
| Addiction psychiatry consultation | 127 (78.9) | 41 (70.7) | 86 (83.5) | 0.06 |
| Infections | ||||
| Primary bacteremia Endocarditis Non-endocarditis endovascular infection Osteomyelitis or septic arthritis SSTI Other | 14 (8.7)42 (26.1)14 (8.7)71 (44.1)12 (7.5)8 (5.0) | 5 (8.6)15 (25.9)5 (8.6)28 (48.3)1 (1.7)4 (6.9) | 9 (8.7)27 (26.2)9 (8.7)43 (41.7)11 (10.7)4 (3.9) | ND |
| Pathogens | ||||
| Gram-positive monomicrobial Other (single or multiple Gram-positive, Gram-negative, and/or fungi) No pathogen identified | 107 (66.5)41 (25.5)13 (8.1) | 42 (72.4)13 (22.4)3 (5.2) | 65 (63.1)28 (27.2)10 (9.7) | 0.41 |
| MRSA MSSA | 64 (39.8)42 (26.1) | 24 (41.4)14 (24.2) | 40 (38.8)28 (27.2) | 0.91 |
| Streptococcus species | 38 (23.6) | 11 (19.0) | 27 (26.2) | 0.30 |
| Antibiotics | ||||
| Single antibiotic Multiple antibiotic | 145 (90.1)16 (9.9) | 54 (93.1)4 (6.9) | 91 (88.3)12 (12.7) | 0.42 |
| Penicillin (class) only Cephalosporin only Carbapenem only Glycopeptide only Lipopeptides only | 7 (4.3)75 (46.6)7 (4.3)37 (23.0)18 (11.2) | 3 (5.2)32 (55.2)3 (5.2)9 (15.5)6 (10.3) | 4 (3.9)43 (41.7)4 (3.9)28 (27.2)12 (11.7) | ND |
HIV: human immunodeficiency virus; MOUD: medication for opioid use disorder; MRSA: methicillin-resistant Staphylococcus aureus; MSSA: methicillin-sensitive Staphylococcus aureus; ND: comparison not done due to low numbers in some subgroups; OUD: opioid use disorder; SSTI: skin and soft tissue infection; SUD: substance use disorder.
Comparison between White and (Black + Latinx) due to low numbers of Latinx.
In addition to OUD, excluding nicotine and alcohol.
OPAT completion occurred in 33 encounters (57%) in which MOUD was not prescribed at discharge, compared to 65 encounters (63%) in which MOUD was prescribed on discharge (Table 2; odds ratio: 1.29, 95% confidence interval: 0.68–2.54). This difference was not statistically significant (p = 0.44). Patients were readmitted within 30 days of finishing OPAT in 13 encounters (22.4%) with no MOUD at discharge and in 27 encounters (26.2%) with MOUD at discharge (p = 0.59). No deaths occurred.
Table 2.
Outcomes by MOUD at discharge.
| No MOUD at discharge (n = 58) | MOUD at discharge (n = 103) | OR (95% confidence interval) | P value | |
|---|---|---|---|---|
| Antibiotic completion | 33 (56.9) | 65 (63.1) | 1.29 (0.68 – 2.54) | 0.44 |
| Readmission within 30 days | 13 (22.4) | 27 (26.2) | 1.230 (0.57 – 2.57) | 0.59 |
| Death | 0 | 0 |
MOUD: medication for opioid use disorder; OR: odds ratio.
Encounters were further analyzed by MOUD use prior to hospital admission and at discharge (Figure 1). MOUD use by encounter was categorized as ‘none’ if not used prior to admission or at discharge, ‘stopped’ if used prior to admission but not by discharge, ‘continued’ if used both prior to admission and at discharge, and ‘started’ if not used prior to admission but started by discharge. OPAT completion occurred in 28 of 49 encounters, in which no MOUD was used; 5 of 9 in which MOUD was stopped, 47 of 78 in which MOUD was continued, and 18 of 27 in which MOUD was started. OPAT completion was not associated with MOUD use prior to admission and at discharge in a multigroup comparison (p = 0.85); results were similar when comparing only the MOUD continued and started groups (p = 0.66).
Figure 1.
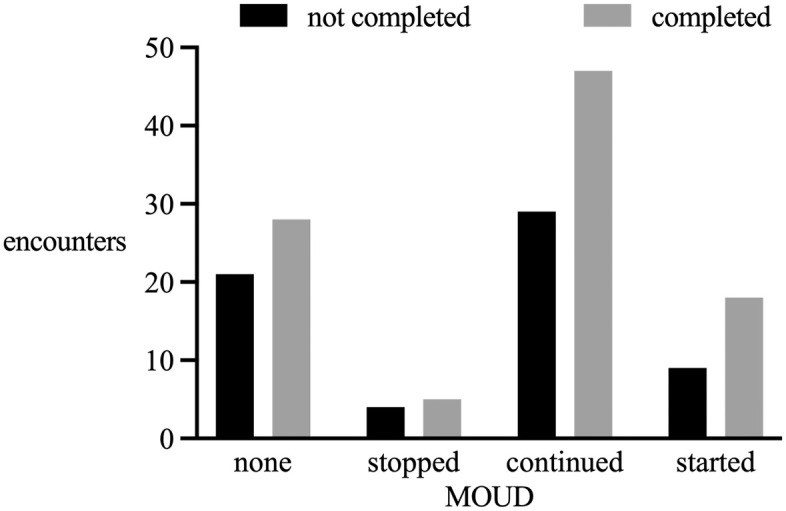
Antibiotic outcome events by MOUD use prior to admission and at discharge.
P value by chi-square of all groups = 0.85.
Discussion
We performed a retrospective cohort study of people with OUD who were receiving OPAT for severe infections at post-acute care facilities. Participants had high rates of IDU, homelessness, and multiple SUD diagnoses. Discharge to the post-acute care facility on methadone or buprenorphine was not associated with OPAT completion. A secondary analysis of MOUD prior to admission and at discharge also did not show an association with OPAT completion. Readmission was similar in both groups and no deaths occurred.
Our study found a similar level of overall OPAT completion (64%) as other studies of similar populations at skilled nursing facilities or SUD treatment facilities (49-73%).6,13–15 Rates of OPAT completion may be lower in PWID or those experiencing homelessness, 16 which was common in our study.
People with SUD who require OPAT may be treated at home, at a post-acute care facility, or at other locations, including residential SUD facilities. Multiple factors may determine the location for OPAT, and it is difficult to compare non-randomized outcomes among patients in different locations. Multiple studies have demonstrated that home OPAT can be effective in people with OUD or IDU. Vazirian et al. 14 found similar OPAT outcomes for a small number of PWID and matched controls. Price et al. 5 reported 100% completion of home OPAT in a highly selected cohort of PWID. D’Couto et al. 6 found higher OPAT completion at home compared to a post-acute care facility in people with SUD (81% vs. 64%), and a small randomized study of home OPAT or in-hospital IV antibiotics by Fanucchi et al. 17 reported 100% antibiotic completion in both groups, but less drug use in the home OPAT group. These studies support the hypothesis that home OPAT may be the most supportive environment for select people.
Despite the demonstrated success of OPAT at home in certain people with SUD, people with SUD and serious infections are more likely to be discharged to a post-acute care facility. 18 They may be more medically complex, may require physical or occupational therapy, or may not have a suitable private home for complicated treatments, such as OPAT. In addition, some people requiring OPAT may be discharged to a facility because they are unjustly and illegally excluded from home OPAT due to their substance use. 19 Given the frequency that people with OUD and serious infections are treated in post-acute care facilities, approaches to improve OPAT completion are critical.
Many groups have reported innovative strategies to improve OPAT care for people who use drugs, with mixed success. Attempts to coordinate OPAT at residential SUD treatment facilities have been met with low uptake by patients.20,21 One program reported significantly lower antibiotic completement rates for PWID with infective endocarditis treated at a SUD treatment facility (46%) compared to a historical control group treated in the hospital (74%), although with similar readmission and mortality outcomes. 22 Improving prescription of MOUD during hospitalizations for severe infections may reduce early patient-directed discharge 23 and post-discharge mortality, 24 although many studies have reported difficulty improving the rate of MOUD use even with dedicated programs.25,26
Beieler et al. 13 performed a small but innovative study of four different interventions (ID consultation, addiction consultation, case management, and MOUD at discharge) in people with OUD experiencing homelessness who were treated with mostly (86%) IV antibiotics at a residential SUD treatment facility. The investigators found that use of all four interventions was associated with improved clinical cure of infection and retention in addiction treatment. However, neither the four-intervention combination nor MOUD alone were associated with increased antibiotic completion. In fact, none of the individual interventions, except case management, improved antibiotic completion, despite rates of MOUD uptake (50% of encounters with new MOUD start) that were much higher than in our study. In comparison, our larger study featured universal case management consultation and reported higher rates of overall antibiotic completion. The study by Beieler et al. and this study suggest that improvement of antibiotic completion requires multiple complex interventions.
Our study is limited by infrequent initiation of MOUD, which may have minimized the effect of MOUD on antibiotic completion. MOUD initiation and titration are limited by the current regulatory environment. Under current US Drug Enforcement Administration (DEA) regulations, methadone cannot be administered for a patient in a post-acute care facility unless the patient is already enrolled in an outpatient methadone treatment program. In addition, regulations from the Substance Abuse and Mental Health Services Administration limit the starting dose of methadone and may discourage up-titration to effective doses in acute hospital settings. 27 Clinical considerations also limit the rate of dose increases, which may prohibit the prescription of an effective dose by the time of hospital discharge. Different regulations restrict buprenorphine use. Outpatient buprenorphine prescribing is limited to providers who have a special DEA certification. Outpatient buprenorphine prescribers may not be available to patients admitted to a post-acute care facility.
Our retrospective study is also subject to selection bias between the MOUD groups and due to exclusion of patients who completed antibiotic therapy in the hospital. Selection bias may explain the less-frequent MOUD prescription at discharge for male patients (Table 1). There are also possible unmeasured confounders, including a risk that those not prescribed MOUD had less-severe OUD or less-severe infections and were therefore more likely to complete antibiotics than those prescribed MOUD. There are also limits to the accuracy of data gathered from the clinical record, especially characterization of SUD diagnoses and current IDU. We excluded people with inactive OUD based on clinical and laboratory assessments, since MOUD may be less likely to benefit them, but this may have incorrectly excluded some people with ongoing use that was unknown to the clinical team. Use of ICD codes to select the cohort may miss those with incomplete documentation and may erroneously select patients who use prescribed opioids in the absence of an SUD. We were also unable to measure continuation of MOUD at post-acute care facilities; it is possible those who managed to continue MOUD would have better outcomes. Readmission or deaths may not have been captured in the available records. Our findings are from one urban academic medical center, which limits generalizability.
The use of MOUD in appropriate patients with serious infections is only one of many elements that may improve care. New treatment paradigms of oral or long-acting IV antibiotics can allow effective treatment without the issues related to prolonged IV access, including safety concerns, and possible requirement for treatment within a facility. 28 Prolonged antibiotic treatment of people with OUD requires careful coordination to continue the treatment of OUD during care transitions. These efforts may be aided by changes to the regulatory framework for MOUD. Intensive and collaborative clinical care and coordination by dedicated, expert teams, in the style of tumor boards, can ameliorate some of the challenges of the fragmented health and social support systems. 29
Improving antibiotic treatment for people with SUD and severe infections is critical. Solutions to deliver effective and dignified treatment of infections in people with SUD will likely require complex, multimodal approaches, and will need to be tailored to individual patient circumstances.
Supplemental Material
Supplemental material, sj-docx-1-tai-10.1177_20499361221103877 for Medication for opioid use disorder at hospital discharge is not associated with intravenous antibiotic completion in post-acute care facilities by Edward C. Traver, Patrick R. Ching and Shivakumar Narayanan in Therapeutic Advances in Infectious Disease
Footnotes
Ethics approval and consent to participate: This study was approved by the University of Maryland, Baltimore Institutional Review Board (approval number HP00093828) with a waiver of informed consent.
Consent for publication: N/A
Author contributions: Edward C. Traver: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Writing – original draft; Writing – review & editing.
Patrick R. Ching: Data curation; Methodology; Writing – original draft; Writing – review & editing.
Shivakumar Narayanan: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Supervision; Writing – original draft; Writing – review & editing.
ORCID iDs: Edward C. Traver  https://orcid.org/0000-0001-7127-3872
https://orcid.org/0000-0001-7127-3872
Patrick R. Ching  https://orcid.org/0000-0001-6106-2799
https://orcid.org/0000-0001-6106-2799
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest statement: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of data and materials: Data and materials are not publically available.
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Edward C. Traver, University of Maryland Medical Center, 22 S. Greene St, Baltimore, MD 21201, USA.
Patrick R. Ching, Division of Infectious Diseases, Department of Medicine, School of Medicine, Washington University in St. Louis, St. Louis, MO, USA
Shivakumar Narayanan, Division of Clinical Care and Research, Institute of Human Virology, School of Medicine, University of Maryland School of Medicine, Baltimore, Maryland, USA.
References
- 1. Schranz AJ, Fleischauer A, Chu VH, et al. Trends in drug use: associated infective endocarditis and heart valve surgery, 2007 to 2017. Ann Intern Med 2019; 170: 31, http://annals.org/article.aspx?doi=10.7326/M18-2124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Larney S, Peacock A, Mathers BM, et al. A systematic review of injecting-related injury and disease among people who inject drugs. Drug and Alcohol Dependence 2017; 171: 39–49, https://linkinghub.elsevier.com/retrieve/pii/S0376871616310444 [DOI] [PubMed] [Google Scholar]
- 3. Fanucchi L, Leedy N, Li J, et al. Perceptions and practices of physicians regarding outpatient parenteral antibiotic therapy in persons who inject drugs. J Hosp Med 2016; 11: 581–582. [DOI] [PubMed] [Google Scholar]
- 4. Rapoport AB, Fischer LS, Santibanez S, et al. Infectious diseases physicians’ perspectives regarding injection drug use and related infections, United States, 2017. Open Forum Infect Dis 2018; 5: ofy132, https://academic.oup.com/ofid/article/doi/10.1093/ofid/ofy132/5034859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Price CN, Solomon DA, Johnson JA, et al. Feasibility and safety of outpatient parenteral antimicrobial therapy in conjunction with addiction treatment for people who inject drugs. J Infect Dis 2020; 222: S494–S498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. D’Couto HT, Robbins GK, Ard KL, et al. Outcomes according to discharge location for persons who inject drugs receiving outpatient parenteral antimicrobial therapy. Open Forum Infect Dis 2018; 5: ofy056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Suzuki J, Johnson J, Montgomery M, et al. Outpatient parenteral antimicrobial therapy among people who inject drugs: a review of the literature. Open Forum Infect Dis 2018; 5: ofy194, https://academic.oup.com/ofid/article/doi/10.1093/ofid/ofy194/5067551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Liebschutz JM, Crooks D, Herman D, et al. Buprenorphine treatment for hospitalized, opioid-dependent patients. JAMA Intern Med 2014; 174: 1369–1376, http://archinte.jamanetwork.com/article.aspx?doi=10.1001/jamainternmed.2014.2556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Larochelle MR, Bernson D, Land T, et al. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality. Ann Intern Med 2018; 169: 137–145, http://annals.org/article.aspx?doi=10.7326/M17-3107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dunlap B, Cifu AS. Clinical management of opioid use disorder. JAMA 2016; 316: 338–339, http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.2016.9795 [DOI] [PubMed] [Google Scholar]
- 11. Rosenthal ES, Karchmer AW, Theisen-Toupal J, et al. Suboptimal addiction interventions for patients hospitalized with injection drug use-associated infective endocarditis. Am J Med 2016; 129: 481–485. [DOI] [PubMed] [Google Scholar]
- 12. Marks LR, Munigala S, Warren DK, et al. A comparison of medication for opioid use disorder treatment strategies for persons who inject drugs with invasive bacterial and fungal infections. J Infect Dis 2020; 222: S513–S520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Beieler AM, Klein JW, Bhatraju E, et al. Evaluation of bundled interventions for patients with opioid use disorder experiencing homelessness receiving extended antibiotics for severe infection. Open Forum Infect Dis 2021; 8: ofab285, https://academic.oup.com/ofid/article/doi/10.1093/ofid/ofab285/6288523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Vazirian M, Jerry JM, Shrestha NK, et al. Outcomes of outpatient parenteral antimicrobial therapy in patients with injection drug use. Psychosomatics 2018; 59: 490–495. [DOI] [PubMed] [Google Scholar]
- 15. Jewell C, Weaver M, Sgroi C, et al. Residential addiction treatment for injection drug users requiring intravenous antibiotics. J Addict Med 2013; 7: 271–276, https://journals.lww.com/01271255-201307000-00008 [DOI] [PubMed] [Google Scholar]
- 16. Beieler A, Magaret A, Zhou Y, et al. Outpatient parenteral antimicrobial therapy in vulnerable populations: people who inject drugs and the homeless. J Hosp Med 2019; 14: 105–109, https://www.journalofhospitalmedicine.com/jhospmed/article/193132/hospital-medicine/outpatient-parenteral-antimicrobial-therapy-vulnerable [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fanucchi LC, Walsh SL, Thornton AC, et al. Outpatient parenteral antimicrobial therapy plus buprenorphine for opioid use disorder and severe injection-related infections. Clinical Infectious Diseases 2020; 70: 1226–1229, https://academic.oup.com/cid/article/70/6/1226/5538253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kim J-H, Fine DR, Li L, et al. Disparities in United States hospitalizations for serious infections in patients with and without opioid use disorder: a nationwide observational study. PLoS Medicine 2020; 17: e1003247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jawa R, Rozansky H, Clemens D, et al. Rethinking home-based outpatient parenteral antibiotic therapy for persons who inject drugs. J Addict Med 2022; 16: e70–e72, https://journals.lww.com/10.1097/ADM.0000000000000856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fanucchi LC, Lofwall MR, Nuzzo PA, et al. In-hospital illicit drug use, substance use disorders, and acceptance of residential treatment in a prospective pilot needs assessment of hospitalized adults with severe infections from injecting drugs. J Subst Abuse Treat 2018; 92: 64–69, https://linkinghub.elsevier.com/retrieve/pii/S0740547218300497 [DOI] [PubMed] [Google Scholar]
- 21. Englander H, Wilson T, Collins D, et al. Lessons learned from the implementation of a medically enhanced residential treatment (MERT) model integrating intravenous antibiotics and residential addiction treatment. Subst Abus 2018; 39: 225–232, https://www.tandfonline.com/doi/full/10.1080/08897077.2018.1452326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gelman SS, Stenehjem E, Foster RA, et al. A novel program to provide drug recovery assistance and outpatient parenteral antibiotic therapy in people who inject drugs. Open Forum Infect Dis 2022; 9: ofab629, https://academic.oup.com/ofid/article/doi/10.1093/ofid/ofab629/6459163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nolan NS, Marks LR, Liang SY, et al. Medications for opioid use disorder associated with less against medical advice discharge among persons who inject drugs hospitalized with an invasive infection. J Addict Med 2021; 15: 155–158, https://journals.lww.com/10.1097/ADM.0000000000000725, PMID: 32804690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kimmel SD, Walley AY, Li Y, et al. Association of treatment with medications for opioid use disorder with mortality after hospitalization for injection drug use: associated infective endocarditis. JAMA Netw Open 2020; 3: e2016228, https://jamanetwork.com/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Paras ML, Wolfe SB, Bearnot B, et al. Multidisciplinary team approach to confront the challenge of drug use-associated infective endocarditis. J Thorac Cardiovasc Surg. Epub ahead of print 4 November 2021. DOI: 10.1016/j.jtcvs.2021.10.048. [DOI] [PubMed] [Google Scholar]
- 26. Eaton EF, Lee RA, Westfall AO, et al. An integrated hospital protocol for persons with injection-related infections may increase medications for opioid use disorder use but challenges remain. J Infect Dis 2020; 222: S499–S505, https://academic.oup.com/jid/article/222/Supplement_5/S499/5900602 [DOI] [PubMed] [Google Scholar]
- 27. Pytell JD, Sharfstein JM, Olsen Y. Facilitating methadone use in hospitals and skilled nursing facilities. JAMA Intern Med 2020; 180: 7–8, https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2754811 [DOI] [PubMed] [Google Scholar]
- 28. Lewis S, Liang SY, Schwarz ES, et al. Patients with serious injection drug use related infections who experience patient directed discharges on oral antibiotics have high rates of antibiotic adherence but require multidisciplinary outpatient support for retention in care. Open Forum Infect Dis 2022; 9: ofab633, https://academic.oup.com/ofid/advance-article/doi/10.1093/ofid/ofab633/6499353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sikka MK, Gore S, Vega T, et al. ‘OPTIONS-DC’, a feasible discharge planning conference to expand infection treatment options for people with substance use disorder. BMC Infect Dis 2021; 21: 772, https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-021-06514-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-tai-10.1177_20499361221103877 for Medication for opioid use disorder at hospital discharge is not associated with intravenous antibiotic completion in post-acute care facilities by Edward C. Traver, Patrick R. Ching and Shivakumar Narayanan in Therapeutic Advances in Infectious Disease


